Escolar Documentos
Profissional Documentos
Cultura Documentos
Atherosclerosis Pathophysiology
Enviado por
Candice ChengDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Atherosclerosis Pathophysiology
Enviado por
Candice ChengDireitos autorais:
Formatos disponíveis
http://ang.sagepub.
com/
Angiology
Atherosclerosis Pathophysiology and the Role of Novel Risk Factors: A Clinicobiochemical Perspective
V. Mallika, Binita Goswami and Medha Rajappa ANGIOLOGY 2007 58: 513 DOI: 10.1177/0003319707303443 The online version of this article can be found at: http://ang.sagepub.com/content/58/5/513
Published by:
http://www.sagepublications.com
Additional services and information for Angiology can be found at: Email Alerts: http://ang.sagepub.com/cgi/alerts Subscriptions: http://ang.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav Citations: http://ang.sagepub.com/content/58/5/513.refs.html
>> Version of Record - Nov 16, 2007 What is This?
Downloaded from ang.sagepub.com at MCMASTER UNIV LIBRARY on February 1, 2013
Angiology
Volume 58, Number 5, 2007
513
Atherosclerosis Pathophysiology and the Role of Novel Risk Factors: A Clinicobiochemical Perspective
V. Mallika,* Binita Goswami, and Medha Rajappa, New Delhi, India
Atherosclerosis is the root cause of the biggest killer of the 21st century. Mechanisms contributing to atherogenesis are multiple and complex. A number of theoriesincluding the role of dyslipidemia, hypercoagulability, oxidative stress, endothelial dysfunction, and inflammation and infection by certain pathogenshave been propounded from time to time explain this complex phenomenon. Recently it has been suggested that atherosclerosis is a multifactorial, multistep disease that involves chronic inflammation at every step, from initiation to progression, and that all the risk factors contribute to pathogenesis by aggravating the underlying inflammatory process. A better understanding of the pathogenesis of atherosclerosis will aid in devising pharmaceutical and lifestyle modifications for reducing mortality resulting from coronary artery disease (CAD). A comprehensive literature search was conducted using the Web sites of the National Library of Medicine (http:// www.ncbl.nlm.nih.gov/) and PubMed Central, the US National Library of Medicines digital archive of life sciences literature (http:// www.pubmedcentral.nih.gov/). The data were accessed from books and journals in which relevant articles in this field were published. The whole spectrum of coronary artery disease evolves through various events that lead to the formation and progression of atherosclerotic plaque and finally its complications. Atherosclerosis is the culprit behind coronary artery disease, cerebral vascular disease, and peripheral vascular disease. The pathogenic mechanisms are varied and complex. Of late, the role of lipoprotein (a), homocysteine, and inflammation and infection as prime culprits in pathogenesis of CAD is the subject of intense research and debate. The appreciation of the role of inflammation in atherosclerosis provides a mechanistic framework to understand the clinical benefits of newer therapeutic strategies, and a better understanding of pathogenesis aids in formulating preventive and therapeutic strategies in reducing mortality resulting from CAD. An in-depth knowledge of the various pathogenic mechanisms involved in atherosclerosis can help in substantiating the current existing knowledge about the CAD epidemic. This knowledge will help clinicians to better manage the disease, which affects Indians in its most severe form.
Angiology 58:513522, October/November 2007 From the *Department of Biochemistry, G.B. Pant Hospital, New Delhi, India, the Department of Biochemistry, Maulana Azad Medical College, New Delhi, India, and the Department of Ocular Biochemistry, Dr. R.P. Centre for Ophthalmic Sciences, AIIMS, New Delhi, India. Address correspondence to: Dr. V. Mallika, Director Professor and Head, Department of Biochemistry, G.B. Pant Hospital, New Delhi -110002, India; phone: 91-11- 23231289; e-mail: drvmallika@gmail.com. DOI: 10.1177/0003319707303443 2007 Sage Publications
Coronary artery disease (CAD) has been recognized as the leading cause of morbidity and mortality in developed as well as developing countries. In more than 90% of cases, the cause of myocardial ischemia is reduction of coronary blood flow owing to atherosclerotic coronary arterial obstruction. Actually, 70% to 85% of all myocardial infarctions occur in the face of < 30% stenosis. The actual cause of angina/ischemia is regional blood flow differences.1 An in-depth knowledge of atherosclerosis and its pathogenesis is therefore
Downloaded from ang.sagepub.com at MCMASTER UNIV LIBRARY on February 1, 2013
514
Angiology
Volume 58, Number 5, 2007
imperative in ascertaining the etiology of CAD and devising pharmacological interventions accordingly.
What Is Atherosclerosis?
The term atherosclerosis is derived from the Greek word athero, meaning gruel or porridge, and sclerosis, meaning hardening. It affects all sized blood vessels, including the medium-sized, elastic arteries. The main arteries affected are the aorta and the coronary, cerebral, and popliteal arteries.2 Atherosclerosis is a progressive disease process that generally begins in childhood and has clinical manifestation in middle to late adulthood. It occurs as a result of 3 fundamental processes.2-4 These processes are accumulation of intimal smooth muscle cells (SMC), together with variable numbers of accumulated macrophages and T lymphocytes; formation by the proliferated SMC of large amounts of connective tissue matrix including collagen, elastin fibers, and proteoglycans; and accumulation of lipids, principally in the form of cholesterol esters and free cholesterol within the cells, as well as in the surrounding connective tissue. The earliest lesions of atherosclerosis can be found in young children and infants in the form of a lesion called the fatty streak, whereas the advanced lesion, the fibrous plaque, generally appears during early adulthood and progresses with age.4
to the potent vasodilator nitric oxide (NO). In normal blood vessels, NO and acetylcholine induce vasodilation, but with endothelium damage, disruption of the cell state negates normal function and the actions of potent vasodilators. The damaged endothelium causes abnormal responses from acetylcholine by increasing the production of vasoconstricting agents such as thromboxane A2 and prostaglandins, in addition to eliciting the development of abnormal intracellular signaling mechanisms, which cause an increase in intracellular Ca2+ and endothelinderived vasoconstricting factors. Endothelial damage also triggers platelets to adhere and aggregate at the site of the damage, which causes monocytes to enter the tunica intima and proliferate within the tunica-media junction of the artery. This effect causes the arterial wall to herniate at this site. With increased monocyte invasion into arteries and continual herniation, the lumen of the artery can become progressively reduced. This combination of biochemical and anatomical alterations contributes to oxidative stress and increased vascular damage, the so-called precursors for atherogenic changes within arteries.
Oxidation hypothesis
The prerequisite for macrophage uptake and cellular accumulation of cholesterol is oxidative modification of low-density lipoproteins (LDL). The initiation of the oxidation process is induced by the intracellular generation of lipoperoxides, which are transferred to LDL through the development of O2-derived free radicals. These species later initiate a series of chemical reactions that are generally referred to as lipid peroxidation. These chemical reactions are maintained by the conversion of lecithin to lyso-lecithin, catalyzed by the plasma membrane-bound enzyme phospholipase A2. Lipid peroxidation contributes to the destruction of the lipid components of the plasma membrane and enhances the release of fatty acids through fatty acid fragmentation and the formation of the reactive intermediate species, referred to as lipoperoxides. These overwhelm LDL and are generated continuously by Cu2+ ions in conjunction with peroxy radicals. Lipoperoxides are toxic to plasma membranes, as they rearrange the chemical structure of the double bonds found in fatty acids. They also combine with apolipoprotein B (apo B) and phospholipids to prevent LDL from binding to the LDL receptor.
Potential Triggers
A number of hypotheses3 have been proposed from time to time to identify the triggering factors for atherosclerosis. Among these hypotheses are the response to injury hypothesis1-5 and the oxidation hypothesis.2,3,5
Response to injury hypothesis
This hypothesis states that the endothelium helps to regulate homeostasis of the cardiovascular system. This proposal was supported by the fact that an intact endothelium is capable of releasing antithrombic and fibrinolytic factors in addition
Downloaded from ang.sagepub.com at MCMASTER UNIV LIBRARY on February 1, 2013
Mallika
Atherosclerosis Pathophysiology and Novel Risk Factors
515
LDL can undergo acetylation to an oxidized form, which is then unable to bind onto native receptors. Oxidized LDL (Ox-LDL) contains lyso-phosphatidylcholine, which is a potent chemo-attractant for macrophages. Lyso-phosphatidylcholine up-regulates the expression of vascular cell adhesion molecules such as intercellular adhesion molecule-1 (ICAM1), which is present within the endothelium and increases monocyte adhesion. Available LDL uses the macrophage as a scavenger molecule. It binds onto and internalizes the LDL. Internalized, oxidized LDL then inhibits monocyte motility. Macrophages that have phagocytosed LDL are referred to as foam cells, owing to their lipid-like appearance on microscopy.
Atherosclerotic Risk Factors3,6,7
Modifiable risk factors, controlled by lifestyle, include cigarette smoking, obesity, and physical inactivity. Modifiable risk factors corrected by pharmacotherapy and/or lifestyle modifications include lipid disorders, hypertension, diabetes mellitus, and insulin resistance. Unmodifiable risk factors include age, gender, and family history/genetics. Newer risk factors include lipoprotein (a) (Lp [a]), homocysteine, thrombotic risk factors, and inflammatory risk factors. Now we will review in detail the role of each of the factors that lead to the pathogenesis of atherosclerosis.
LDLhave now been implicated in the atherosclerotic process. Studies have shown that TRLPs are taken up by the vascular intima and initiate smooth muscle cell proliferation and extracellular matrix deposition.15-18 Therefore, apo B assays can provide valuable information regarding the risk of CAD, as apo B is a common lipoprotein of both cholesterol-rich and triglyceride-rich lipoproteins.19,20 Apolipoprotein C-III (apo C-III) in very lowdensity lipoprotein (VLDL) is associated with denser, smaller VLDL subclasses and is believed to be particularly atherogenic.21 Remnants associated with apo C-III are more related to the development of atherosclerosis than are triglycerides per se. Fasting remnant lipoproteins could reflect postprandial remnant lipoproteins and predict future clinical coronary events independently of other risk factors.22 Peroxisome proliferator-activated receptor- (PPAR-) agonism increases the synthesis of apo A-I, the main apolipoprotein of high-density lipoprotein (HDL), a particle that protects against lesion formation, probably owing to its role in reverse cholesterol transport (removing cholesterol from the artery wall and delivering it to the liver). Other laboratory studies have established that PPAR- agonists also possess anti-inflammatory properties of potential relevance to atherogenesis. For example, these agents can reduce vascular cell adhesion molecule-1 (VCAM-1) and tissue factor gene expression by cells found in atheroma. Interference with the activation of nuclear factor-B (NF-B), resulting from competition for coactivators, may explain part of this anti-inflammatory action of PPAR- agonism.23-25 Role of postprandial hyperlipidemia. It is important to acknowledge that triglyceride-rich particles are produced mainly postprandially.26 In the postprandial state, because of the limited availability of lipoprotein lipase, competition at the level of this enzyme will occur, resulting in the accumulation of triglyceride-rich parlicles.27 It has been shown that, among all patients with premature CAD, 40% have normal fasting plasma lipids, although many have impaired clearance of postprandial lipoprotein.28,29 It is for this reason that atherosclerosis has been considered to be a postprandial phenomenon.30 Lipoprotein (a). Lipoprotein (a) has been identified as an independent risk factor for CAD,
Role of lipids
The lipogenic hypothesis states that both lesion initiation and progression in atherosclerosis appear to be associated with markedly increased levels of plasma LDL. Proliferated smooth muscle cells within lesions are filled with cholesterol oleate and become necrotic, leading to the formation of plaque.2,4 Epidemiological studies have shown a positive relationship between total cholesterol concentrations and mortality from CAD.8 Small, dense LDL particles are more atherogenic than large, buoyant LDL particles, and oxidation of LDL also increases its atherogenicity.9-14 Triglyceride-rich lipoproteins (TRLPs) besides the conventional, cholesterol-containing
Downloaded from ang.sagepub.com at MCMASTER UNIV LIBRARY on February 1, 2013
516
Angiology
Volume 58, Number 5, 2007
especially in the Indian context. Lp (a) particles contain apo(a) and apo B in a 1:1 molar ratio. apo(a) contains a Kringle-5 domain and a protease domain with 85% amino acid identity with the plasminogen protease domain.31,32 The mechanisms implicated in the atherogenicity of Lp (a) include3 the tendency to self-aggregate and precipitate; greater capacity to bind to glycosaminoglycans and other structures in the vascular wall; impaired fibrinolysis owing to its structural homology with plasminogen and its regulation of synthesis of plasminogen activator inhibitor-1 (PAI-1); and induction of smooth muscle cell proliferation.33-36 Role of metabolic syndrome. Metabolic syndrome is characterized by obesity, atherosclerosis insulin resistance and hyperinsulinemia, hyperlipidemia, essential hypertension, type 2 diabetes mellitus, and coronary heart disease. Other features include hyperfibrinogenemia, increased PAI-1, and a proinflammatory state.3,37 This metabolic derangement is also characterized by a low-grade inflammatory state, which is suggested by the high levels of C-reactive protein, tumor necrosis factor- (TNF-) and other pro-inflammatory mediators.3,38 Adipose tissue itself can give rise to cytokines that worsen insulin sensitivity and provide a systemic pro-inflammatory stimulus. In metabolic syndrome, LDL levels often remain in the average range, although the particles may have qualitative alterations that render them small and dense, making them particularly prone to oxidation and hence evoking inflammation. The low levels of HDL that characteristically accompany the elevated triglycerides in metabolic syndrome blunt another endogenous anti-inflammatory, and hence atheroprotective, mechanism.39 Persistent hyperglycaemia in diabetes can accelerate the formation of advanced glycation end products, yet another trigger to arterial inflammation.40 Hence, metabolic syndrome is a very important proatherogenic condition. Role of coagulation cascade and fibrinolytic system3. The acute manifestations of CAD such as acute myocardial infarction are triggered by complications of atherosclerotic plaquethrombosis, occlusion, or rupturebecause of alteration in the delicate balance between fibrinogenesis and fibrinolysis.41 Exposure of the subendothelial thrombogenic milieu to circulating blood allows
deposition of platelets, which initiates coagulation leading to thrombosis and/or occlusion of the vessel lumen.42 Fibrinogen, the main coagulation protein in plasma, has been identified as a risk factor for CAD.43 Decreased fibrinolytic activity has been observed in CAD patients. The level of PAI-1 is significantly increased. The thrombosis in situ leads to thrombin generation, which, in addition to cleaving fibrinogen, can potently stimulate smooth muscle migration and proliferation. Thrombin triggers platelet release of growth factors such as platelet-derived growth factor (PDGF) from their granules, further stimulating smooth muscle migration and proliferation.3 Activated platelets also elaborate transforming growth factor- (TGF-), the most potent stimulus known for interstitial collagen synthesis by smooth muscle cells. In this manner, a silent microvascular haemorrhage within the atherosclerotic intima could give rise to a growth spurt in the evolution of the plaque.42,44 Role of platelet aggregability. Platelets play a critical role in the pathogenesis of thrombus formation and thromboembolic events and may serve as source of circulating immumoreactive tissue factor. Results of over 400 clinical trials have demonstrated that any antiplatelet drug offers significant protection against cardiovascular events. It is therefore essential to thoroughly evaluate the risk associated with platelet hyperfunction in precipitating acute coronary events. In spite of decades of research in this field, the role of platelets in the initiation of inflammation and endothelial dysfunction is not very well defined. Activation of platelets by various agonists like adenosine diphosphate (ADP) and epinephrine leads to a number of effects through the activation of signaling pathways.3 Up-regulation of these pathways will increase the risk for clinical complications associated with acute coronary syndromes (ACSs). ACSs can also be triggered by platelet-induced thrombus formation, release of growth factors, bacterial infections,45 and inflammatiory mediators. In addition, they activate other cells such as monocytes and macrophages and promote the expresson of tissue factor and TNFs. They also modulate the function of leukocytes and the expression of chemotactic factors and adhesive properties of endothelial cells. CD40L expression by platelets plays a pivotal role in plaque progression.41,46
Downloaded from ang.sagepub.com at MCMASTER UNIV LIBRARY on February 1, 2013
Mallika
Atherosclerosis Pathophysiology and Novel Risk Factors
517
When the prevailing fibrinolytic mechanisms outweigh the procoagulant pathways, a limited mural thrombus, rather than an occlusive and sustained blood clot, forms. With healing, however, resorption of the mural thrombus and the release of PDGF and the anti-inflammatory mediator TGF- combine to engender a healing response that leads to fibrous tissue formation.3 The consequent smooth muscle accumulation and collagen accretion allow rapid evolution of a fatty lesion to one of more fibrous character.47,48 Role of endothelial dysfunction. The normal, healthy endothelium regulates vascular tone and structure and exerts anticoagulant, antiplatelet, and fibrinolytic properties. The maintenance of vascular tone is accomplished by the release of numerous dilator and constrictor substances,3,49 for example, NO, prostacyclin, endothelin, and angiotensin II. Damage to the endothelium upsets the balance between vasoconstriction and vasodilation and initiates a number of events and processes including increased endothelial permeability, platelet aggregation, leukocyte adhesion and generation of cytokines,50that promote or exacerbate atherosclerosis. Decreased production or activity of NO, manifested as impaired vasodilation, may be one of the earliest signs of atherosclerosis.51 Role of free radicals. Free radical-mediated injury to the vessel wall has been implicated in the pathogenesis of atherosclerosis.52 Free radicals cause the peroxidation of the lipids being carried by LDL, producing Ox-LDL. OxLDL is taken up much faster by the endothelial cell and macrophages, thereby accelerating the atherosclerotic process.53 Oxidized Lp(a) is 10 times more atherogenic than Ox-LDL. OxLDL has many characteristics that potentially promote atherosclerosis3,54-58: Taken up rapidly by macrophages to form foam cells Chemo-attractant for circulating monocytes and T cells Promotes the differentiation of monocytes and release of macrophage colony stimulating factor from endothelial cells
Immunogenic Cytotoxic to various cell types, including endothelial cells Activates metalloproteinases Induces proatherogenic genes PDGF, COX, and e-NOS Induces apoptosis of SMCs Stimulates expression of CD40/CD40L Role of inflammation and infection. Atherosclerosis is a multifactorial, multistep disease that involves chronic inflammation at every stage, from initiation to progression and eventually plaque rupture.59 Adhesion molecules expressed by inflamed endothelium recruit leukocytes, including monocytes which then penetrate into the intima, predisposing the vessel wall to lipid accretion or vasculitis. Inflammatory mediators enhance uptake of modified lipoprotein particles and formation of lipid-filled macrophages. T cells also enter the intima and secrete cytokines, which subsequently amplify the proliferation of intimal SMCs. Later in the process, inflammatory mediators can weaken the protective fibrous cap of the atheroma, possibly leading to thrombosis and the occurrence of ACS.60,61 Epidemiological studies suggest an association between some pathogens45 and atherosclerosis including Chlamydia pneumoniae, cytomegalovirus, Helicobacter pylori, and bacteria associated with periodontal disease.62,63 It has been suggested that these pathogens influence atheroma biology by modulating macrophagelipoprotein interactions. They increase LDL oxidation, expression of adhesion molecules and inflammatory cytokines, and prothrombotic activity. Chlamydial heat shock protein-60 (HSP-60) has independent atherogenic properties.63,64 Cytomegalovirus produces a protein that binds to and inactivates p53, resulting in cell proliferation. It also causes upregulation of scavenger receptors, increased Lp(a) production, and impaired fibrinolysis.65 Role of leucocytes and adhesion molecules in atherosclerosis. The normal arterial endothelium resists prolonged contact with leukocytes, including the blood monocyte. When endothelial cells undergo inflammatory activation, they increase their expression of various leukocyte
Downloaded from ang.sagepub.com at MCMASTER UNIV LIBRARY on February 1, 2013
518
Angiology
Volume 58, Number 5, 2007
adhesion molecules. In the context of monocyte recruitment to the atheroma, VCAM-1 seems to have a major role. Once adherent to the activated endothelial layer, the monocyte diapedeses between intact endothelial cells to penetrate into the tunica intima, or innermost layer of the arterial wall. This directed migration requires a chemoattractant gradient.66,67 Various chemokines seem to participate in this process, particularly interaction of monocyte chemoattractant protein1 (MCP-1)3 with its receptor CCR2. Notably, the foam cell secretes proinflammatory cytokines3 that amplify the local inflammatory response in the lesion, as well as reactive oxygen species. The activated mononuclear phagocyte has a key role in the thrombotic complications of atherosclerosis by producing matrix metalloproteinases (MMPs) that can degrade the extracellular matrix that lends strength to the plaques fibrous cap.68 Lymphocytes enter the intima facilitated by binding to adhesion molecules including VCAM-1 and in response, chemoattractants selective for lymphocytes. Known chemoattractants include a trio of interferon- (IFN-)inducible chemokines of the CXC family including inducible protein-10 (IP10), monokine induced by IFN- (Mig), and IFNinducible T cell -chemoattractant (I-TAC). These chemokines bind to chemokine receptor CXCR3 expressed by T cells in the atherosclerotic lesion. Once resident in the arterial intima, the T cell may encounter antigens such as Ox-LDL and HSPs of endogenous or microbial origin, among others. On activation by engagement of the receptor and antigen, the T cell can produce cytokines3 that can influence the behavior of other cells present in the atheroma. Notably, CD40 binding to the CD40 ligand, particularly on macrophages, may induce the expression of tissue factor, MMPs, and pro-inflammatory cytokines. The production of these mediators provides an amplification loop resulting from crosstalk between the prototypical cell of acquired immunity (the T lymphocyte) and that of innate immunity (the mononuclear phagocyte). Within the atheroma, as in other tissues, the helper T cells can polarize into those secreting generally pro-inflammatory cytokines (known as TH1 cells) and/or those secreting predominantly anti-inflammatory cytokines (denoted TH2 cells). In general, TH1 cells predominate in the atheroma.69,70 In addition to its leukocyte
selectivity, other features of VCAM-1 make it an interesting candidate. Endothelial cells express VCAM-1 in response to cholesterol feeding selectively in areas prone to lesion formation.71 In addition, VCAM-1 rises before leukocyte recruitment begins in both rabbit and mouse models of cholesterol-induced lesion formation.72 In addition to VCAM-1, P- and E-selectin also seem to contribute to leukocyte recruitment in atherosclerosis-susceptible mice.73,74 Constituents of modified lipoprotein particles, among them certain oxidized phospholipids and short-chain aldehydes arising from lipoprotein oxidation, can induce transcriptional activation of the VCAM-1 gene mediated in part by NF-B. Pro-inflammatory cytokines such as interleukin-1 (IL-1) or TNF- induce VCAM-1 expression in endothelial cells by this pathway. Human atherosclerotic lesions contain these cytokines.3 Thus, pro-inflammatory cytokines may link hypercholesterolemia to VCAM-1 expression.75 Monocyte chemoattractant protein-1 (MCP-1), overexpressed in human and experimental atheroma, can recruit the mononuclear phagocytes that characteristically accumulate in the nascent atheroma.68 IL-8 may have a similar role as a leukocyte chemoattractant during atherogenesis.76 Atheroma overexpress other chemokines that may contribute to lymphocyte recruitment, including a trio of CXC chemokines induced by interferon (IFN- ). 77 Chemoattraction of mast cells found in atheroma may depend on eotaxin, a CC chemokine also overexpressed in these lesions.78 Eotaxin, a chemoattractant that interacts with the chemokine receptor CCR3, may mediate the transendothelial migration of this specialized leukocyte. Once resident in the intima, the mast cell can undergo degranulation, releasing preformed TNF-, heparin with its anti-coagulant and potentially growth-inhibitory effects on smooth muscle cells, and the serine proteinases tryptase and chymase. These proteinases may activate the inactive zymogen forms of MMPs to their proteolytic forms. Chymase may also generate active forms of angiotensin from their precursor, angiotensin-I.78 Two processes related to inflammation may participate in endothelial desquamation. The first, endothelial cell death (perhaps by apoptosis) may result from local production of
Downloaded from ang.sagepub.com at MCMASTER UNIV LIBRARY on February 1, 2013
Mallika
Atherosclerosis Pathophysiology and Novel Risk Factors
519
inflammatory mediators or cytolytic attack by activated killer T cells.3 Additionally, inflammatory mediators and oxidized lipoproteins can stimulate the expression and activation of MMPs specialized in degrading components of the subendothelial basement membrane. Thus, inflammatory stimulation may promote the production by endothelial cells of enzymes that degrade the extracellular matrix constituents to which they adhere under normal circumstances.3,79 We therefore stand on the threshold of clinical application of the basic biology of inflammation in atherosclerosis that could fundamentally alter the way in which we practice preventive medicine80 and prove immeasurably beneficial to the public as well. Role of homocysteine81 The role of homocysteine in the pathogenesis of CAD was first reported by Wilcken and Wilcken in 1976.82 It is a product of methionine metabolism.
expression, and elicits DNA damage response, which induces apoptosis in neurons.
Genetic factors
Numerous genes for 10 apolipoproteins and 4 lipoproteins have been isolated from chromosomes 1, 2, 3, 6, 8, 11, 15, 16, and 19, with the gene for the LDL receptor located on chromosome 19. Mutants of this gene have been associated with familial hypercholesterolemia. This genetic condition occurs in individuals who inherit a mutant gene or are heterozygotes and possess less than 50% of the required LDL receptors. Heterozygotes possess 1 normal gene but inherit a mutant gene that contains the genetic code responsible for the LDL receptor protein. These individuals synthesize about 50% of the usual quantity of LDL receptors and can bind and degrade 50% of the normal rate of LDL. Roughly 1 in 500 people are affected by this mutation. Plasma LDL levels are high, and a large proportion of patients will suffer from a cardiac incident by the age of 35 years. In contrast, the homozygotes possess 2 mutant genes or possess a genetic predisposition to hypercholesterolemia. These inherited defective LDL receptor genes are incapable of synthesizing normal receptor and maintain an abnormally high LDL concentration owing to an increased production of LDL and decreased removal of LDL.93
Mechanism involved in the atherothrombotic effects of homocysteine80
Effects of platelet function and thrombosis83-85 include stimulation of platelet generation of thromboxane A2; activation of factor V and interference with protein C activation and thrombomodulin expression; and interference with the bioavailability of prostacyclin and expression of heparin sulfate. Effects on endothelial and smooth muscle function86-88 include endothelial cell desquamation, smooth muscle cell proliferation, and intimal thickening. Homocysteine inhibits DNA synthesis in vascular endothelial cells and arrests their growth in the G1 phase. It also induces mitogenesis in smooth muscle cells by stimulating the MAP kinase pathway and by induction of the c-fos gene, encourages interaction between neutrophils and endothelial cells, and enhances metalloproteinase activity. Effects on oxidantantioxidant dynamics 89,90 are that homocysteine oxidizes LDL, promotes generation of free radicals; inhibits intracellular antioxidant enzymes; reduces bioavailability of NO; and activates poly-ADPribose polymerase, an important mediator of endothelial dysfunction. Effects at the genetic level 91,92 include that homocysteine alters the methylation status of genes, thus contributing to altered gene
Conclusion
A deep insight into the pathogenesis of atherosclerosis will be of tremendous help in reducing the morbidity and mortality from this deadly disease. The explanation by Fleming that vascular disease is the result of inflammation was first established in 1995 in Helsinki, Finland, and the complete details were laid out in 2000.80 The discovery of these novel risk factors is a great step forward. The appreciation of the role of inflammation in atherogenesis provides a mechanistic frame work to understand clinical benefits of newer preventive and therapeutic strategies, thereby proving immensely
Downloaded from ang.sagepub.com at MCMASTER UNIV LIBRARY on February 1, 2013
520
Angiology
Volume 58, Number 5, 2007
beneficial to CAD-prone populations, including the Indian population.
and inflammatory cytokines (AIR study). Arterioscler Thromb Vasc Biol 22:1162-1167, 2002. 15. Havel RJ. Role of triglyceride rich lipoproteins in progression of atherosclerosis. Circulation 81:694-696, 1990.
REFERENCES
1. Fleming RM: Angina and coronary ischemia are the result of coronary regional blood flow differences. J Amer Coll Angiol 1:127-42, 2003. 2. Schoen FJ. The Heart in Robbins Pathological Basis of Disease. 5th ed. New York: W.B. Saunders Co.; 1994:517-582. 3. Fleming RM. The Pathogenesis of Vascular Disease. Textbook of Angiology. New York: Springer-Verlag; 1999:787-798. 4. Braunwald E. Heart Disease. A Textbook of Cardiovascular Disease. Vol 2, 5th ed. New York: W.B. Saunders Co.; 1997:1105-1160. 5. Alexander RW, Schlant RC, Fuster V, ORouke RA, Roberts R, Sonnenbuck EH. Hursts. The Heart Arteries and Veins. Vol. 1, 9th ed. New York: McGraw-Hill; 1998:1139-1196. 6. Boon NA, Fox KAA, Bloomfield P, Bradbuny A. Cardiovascular Disease in Davidsons Principles and Practice of Medicine. 19th ed. New York: Churchill Livingstone; 2002;357-782. 7. Fauci AS, Braunwald E, Isselbacher KJ, et al. Harrisons Principles of Internal Medicine. Vol. 1, 15th ed. New York: McGraw-Hill; 2003:1377-1398. 8. Austin MA, King MC, Varnizan KM: Atherogenic lipoprotein phenotype: a proposed genetic marker for coronary heart disease risk. Circulation 82:495-506, 1990. 9. Lamarche B, St. Pierre AC, Ruel IL. A prospective population based study of low density lipoprotein particle size as a risk factor for ischemic heart disease in men. Can J Cardiol 17:859-865, 2001. 10. Blake GJ, Tvos JD, Rifai N. Low density lipoprotein particle concentration and size as determined by nuclear magnetic resonance spectroscopy as predictors of cardiovascular disease in women. Circulation 106:1930-1937, 2002. 11. Lamarche B, Lemieux I, Despres JP. The small dense LDL phenotype and the risk of coronary heart disease: epidemiology pathophysiology and therapeutic aspects. Diabetes Metab 25:199-211, 1999. 12. Vakkilainen J, Steiner G, Ansauer JC: Relationships between low density lipoprotein particle size, plasma lipoproteins, and progression of coronary artery disease: the Diabetes Atherosclerosis Intervention Study (DAIS). Circulation 107:1733-1737, 2003. 13. Holvoet P, Mertens A, Verhamme P. Circulating oxidized LDL is a useful marker for identifying patients with coronary artery disease. Arterioscler Thromb Vasc Biol 21:844-848, 2001. 14. Hulthe J, Iagerberg B. Circulating oxidized LDL is associated with subclinical atherosclerosis development
16. Krauss RM. Atherogenicity of triglyceride-rich lipoproteins. Am J Cardiol 13B-17B, 1998. 17. Hodis HN, Mack WJ, Azen SP. Triglyceride and cholesterol rich lipoproteins have a differential effect on mild/moderate and severe lesion progression as assessed by quantitative coronary angiography in a controlled trial of lovastatin. Circulation 90:42-49, 1994. 18. Alanpovic P, Mack WJ, Knight-Gibson C. The role of triglyceride rich lipoprotein families in the progression of atherosclerotic lesions as determined by sequential coronary angiography from a controlled clinical trial. Arterioscler Thromb Vasc Biol 17:715-722, 1997. 19. Sigurdsson G, Baldursdottir A, Sigvaldason H. Predictive value of apolipoproteins in a prospective survey of coronary artery disease in men. Am J Cardiol 62:1251-1254, 1992. 20. Walldius G, Jungner I, Holmer I. High apolipoprotein B, low apolipoprotein A-I, and improvement in the prediction of fatal myocardial infarction (AMORIS study): a prospective study. Lancet 358:2026-2033, 2001. 21. Sacks FM, Alaupovic P, Moye LA: VLDL, apolipoproteins B, C III and E, and risk of recurrent coronary events in the cholesterol and recurrent events (CARE) trial. Circulation 102:1886-1892, 2000. 22. Schaefer EJ, McNamara JR, Shan PK: Elevated remnantlike particle cholesterol and triglyceride levels in diabetic men and women in the Framingham Offspring Study. Diabetes Care 25:989-994, 2002. 23. Marx N, Sukhova GK, Collins T, Libby P, Plutzky J: PPAR activators inhibit cytokine-induced vascular cell adhesion molecule-1 expression in human endothelial cells. Circulation 99:3125-3131, 1999. 24. Neve BP: PPAR agonists inhibit tissue factor expression in human monocytes and macrophages. Circulation 103:207-212, 2001. 25. Delerive P: Peroxisome proliferator-activated receptor negatively regulates the vascular inflammatory gene response by negative crosstalk with transcription factors NF-kB and AP-I. J Biol Chem 274:32048-32054, 1999. 26. Castro Cabezas M, Halkes CJ, Meijjssen S: Diurnal triglyceride profiles: a novel approach to study triglyceride changes. Atherosclerosis 155:219-228, 2001. 27. Lewis GF, OMeara NM, Soltys PA: Fasting hypertriglyceridemia in noninsulin-dependent diabetes mellitus is an important predictor of postprandial lipid and lipoprotein abnormalities. J Clin Endocrinol Metab 72:934-944, 1991. 28. Patsch JR, Miesenback G, Hopferwieser T: Relation of triglyceride metabolism and coronary artery disease. Studies in the postprandial state. Arterioscler Thromb 12:1336-1345, 1992. 29. Weintraub MS, Grosskopf I, Rassin T: Clearance of chylomicron remnants in normolipidemic patients with coronary artery disease: Case control study over three years. BMJ 312:936-939, 1996.
Downloaded from ang.sagepub.com at MCMASTER UNIV LIBRARY on February 1, 2013
Mallika
Atherosclerosis Pathophysiology and Novel Risk Factors
521
30. Zilversmit DB: Atherogenesis: A postprandial phenomenon. Circulation 60:473-485, 1979. 31. Loscalzo J: Lipoprotein (a): a unique risk factor for atherothrombotic disease. Arteriosclerosis 10:672-679, 1990. 32. Loscalzo J, Weinfeld M, Flees GM, Scanu AM, Fogelman AM: Lipoprotein (a), fibrin binding and plasminogen activation. Arteriosclerosis 10:240-245, 1990. 33. Lawn RM: Lipoprotein (a) in heart disease. Sci Am 266:54-60, 1992. 34. Dalen GH, Guyton JR, Mohammad A: Association of levels of lipoprotein (a), plasma lipids and other lipoproteins with coronary arteries documented by angiography. Circulation 74:758-765, 1986. 35. Mbewu AD, Duington PN: Lipoprotein (a) structure, properties, and possible involvement in thrombogenesis and atherogenesis. Atherosclerosis 85:1-14, 1990. 36. Galle J, Bengen J, Schollmeyer P, Wanner C. Impairment of endothelium-dependent diation of rabbit renal arteries by oxidized lipoprotein (a). Circulation 92:1582-1589, 1995. 37. Rosenson RS: Assessing risk across the spectrum of patients with the metabolic syndrome. Am J Cardiol 96:8E-10E, 2005. 38. Sorrentino MJ: Implications of the metabolic syndrome the new epidemic. Am J Cardiol 96:3E-7E, 2005. 39. Navab M: High density lipoprotein associated enzymes: their role in vascular biology. Curr Opin Lipidol 9:449456, 1998. 40. Schmidt AM, Yan SD, Wautier JL, Stern D: Activation of receptor for advanced glycation end products: a mechanism for chronic vascular dysfunction in diabetic vasculopathy and atherosclerosis. Cri Res 84:489-497, 1999. 41. Miller GJ: Hemostasis and cardiovascular risk. The British and European experience. Arch Pathol Lab Med 116:1318-1321, 1992. 42. Meade TW, Ruddock V, Sterling Y: Fibrinolytic activity, clotting factors and long term incidence of ischemic heart disease in the Northwick Park Heart Study. Lancet 342:1076, 1993. 43. Erdste E: Plasma fibrinogen an independent cardiovascular risk factor. J Intern Med 227:365-372, 1990. 44. Juhan-Vague I, Allesi MC: Plasminogen activator inhibitor and atherothrombosis. Thromb Haemost 70:138-143, 1993. 45. Fleming RM. Using C-reactive protein as a marker of bacterially aggravated atherosclerosis in acute coronary syndromes. J Amer Coll Angiol 2003;1:165-171, 2003. 46. Fuster V, Fayad ZA, Badimon JJ: Acute coronary syndromes: biology. Lancet 353:S115-S119, 1999. 47. Saksela O, Rifkin DB: Cell-associated plasminogen activation/regulation and physiological functions. Annu Rev Cell Biol 4:93-126, 1988. 48. Libby P: Inflammation in atherosclerosis. Nature 420:868-874, 2002. 49. Drexler H: Factors involved in the maintenance of endothelial function. Am J Cardiol 82:35-45, 1998.
50. Ross R: Atherosclerosis. An inflammatory disease. N Engl J Med 340:115-126, 1999. 51. Davignon J, Ganz P: Role of endothelial dysfunction in atherosclerosis. Circulation 109(III):III-27III-32, 2002. 52. Harrison D, Griending KK, Landmesser U: Role of oxidative stress in atherosclerosis. Am J Cardiol 91:7A11A, 2003. 53. ODonnell VB: Free radicals and lipid signaling in endothelial cells. Antioxid Redox Signal 5:195-203, 2003. 54. Li D, Yang B, Mehta JL: Ox-LDL induces apoptosis in human coronary artery endothelial cells: role of PKC, PTK, Bcl2, and Fas. Am J Physiol 275:H568-H576, 1998. 55. Inoue M, Itoh H, Tanaka T. Oxidised LDL regulates vascular endothelial growth factor expression in human macrophages and endothelial cells through activation of peroxisome proliferator activator receptor gamma. Arterioscler Thromb Vasc Biol 21:560-566, 2001. 56. Auge N, Garcia V, Maupas-Schwalm F: Oxidized LDL induced smooth muscle cell proliferation involves the EGF receptor/PI-3 Kinase/Akt and the sphingolipid signaling pathways. Arterioscler Thromb Vasc Biol 22:1990-1995, 2002. 57. Li D, Liu L, Chen H, Sawamura T, Ranganathan S, Mehta JL: Lox-I mediates OX-LDL induced expression of matrix metalloproteinase in human coronary artery endothelial cells. Circulation 107:612-617, 2003. 58. Li D, Liu L, Chen H, Sawamura T, Mehta JL: Lox-1, an oxidized LDL endothelial receptor, induces CD40/ CD40L signaling in human coronary artery endothelial cells. Arterioscler Thromb Vasc Biol 23:816-821, 2003. 59. Libby P, Ridker PM, Maseri A: Inflammation and atherosclerosis. Circulation 105:1135-1143, 2002. 60. Shah PK: Plaque disruption and thrombosis: potential role of inflammation and infection. Cardiol Clin 17:271-281, 1999. 61. Ross R: The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 362:801-809, 1993. 62. Cheng JWN, Rivera NG: Infection and atherosclerosis focus on cytomegalovirus and chlamydia pneumoniae. Ann Pharmacother 32:1310-1316, 1998. 63. Mehta JL, Saldeen TGP, Rand K: Interactive role of infection, inflammation and traditional risk factors in atherosclerosis and coronary disease. J Am Coll Cardiol 31:1217-1225, 1998. 64. Kalayoglu MV, Libby P, Byrne GI: Chlamydia pneumoniae as an emerging risk factor in cardiovascular disease. JAMA 288:2724-2731, 2002. 65. Fabricant CG, Fabricant J, Litrenta MM: Virus induced atherosclerosis. J Exp Med 148:335-340, 1978. 66. Gerrity RG: The role of the monocyte in atherogenesis. Transition of blood borne monocytes into foam cells in fatty lesions. Am J Pathol 103:181-190, 1981. 67. Plutzky J: Inflammatory pathways in atherosclerosis and acute coronary syndrome. Am J Cardiol 88:10K15K, 2001.
Downloaded from ang.sagepub.com at MCMASTER UNIV LIBRARY on February 1, 2013
522
Angiology
Volume 58, Number 5, 2007
68. Pober JS, Cotxao RS: Cytokines and endothelial cell biology. Physiol Rev 70:427-451, 1990. 69. Mehta JL, Nichols WW, Mehta P: Neutrophils as potential participants in acute myocardial ischemia. J Am Coll Cardiol 11:1309-1316, 1988. 70. Hansson GK, Jonasson L, Seifert PS, Stemme S: Immune mechanisms in atherosclerosis. Arteriosclerosis 9:567-578, 1989. 71. Cybulsky MI, Gimbrone MA: Endothelial expression of a mononuclear leucocyte adhesion molecule during atherogenesis. Science 251:788-791, 1991. 72. Li H, Cybulsky MI, Gimbrone MA, Libby P: An atherogenic diet rapidly induces VCAM-1, a cytokine mononuclear leukocyte adhesion molecule, in rabbit endothelium. Arterioscler Thromb 13:197-204, 1993. 73. Johnson RC. Absence of P-selectins delays fatty streak formation in mice. J Clin Invest 99:1037-1043, 1997. 74. Dong ZM: The combined role of P-and E-selectins in atherosclerosis. J Clin Invest 102:145-152, 1998. 75. Collins T, Cybulsky MI: NF-KB: pivotal mediator or innocent bystander in atherogenesis? J Clin Invest 107:255-264, 2001. 76. Boisvert WA, Santiago R, Curtiss LK, Terkeltaub RA: A leucocyte homologue of the IL-8 receptor CXCR-2 mediates the accumulation of macrophages in atherosclerotic lesions of LDL receptor deficient mice. J Clin Invest 101:353-363, 1998. 77. Mach F: Differential expression of three T-lymphocyte activating CXC chemokines by human atheroma associated cells. J Clin Invest 104:1041-1050, 1999. 78. Haley KJ: Overexpression of eotaxin and the CCR3 receptor in human atherosclerosis: using genomic technology to identify a potential novel pathway. Circulation 102:2185-2189, 2000. 79. Rajavashisth TB: Inflammatory cytokines and oxidized low density lipoproteins increase endothelial cell expression of membrane type 1 matrix metalloproteinase. J Biol Chem 274:11924-11929, 1999. 80. Fleming RM: The effect of high, moderate and low fat diets on weight loss and cardiovascular disease risk factors. Preventive Cardiol 5:110-118, 2002. 81. Fleming RM: The influence of diet on homocysteine. Fourth International Homocysteine Conference; Basel, Switzerland, June 2003. 82. Wilcken DEL, Wilcken B: The pathogenesis of coronary artery disease. A possible role for methionine metabolism. J Clin Invest 57:1079-1082, 1976. 83. Harpel PC, Chang VT, Borth W: Homocysteine and other sulfhydryl compounds enhance the binding of lipoprotein (a) to fibrin. A potential biochemical link between thrombosis, atherogenesis and sulfhydryl compound metabolism. Proc Natl Acad Sci USA 89:10193-10197, 1992. 84. Lentz SR, Sadler JE: Inhibition of thrombomodulin surface expression and protein C activation by the thrombogenic agent homocysteine. J Clin Invest 88:1096-1914, 1991. 85. Nishinaga M, Ozawa T, Shimado K: Homocysteine, a thrombogenic agent, suppresses anticoagulant heparin
sulphate expression in cultured porcine aortic endothelial cells. J Clin Invest 92:1381-1386, 1993. 86. Haynes WG: Hyperhomocysteinemia. Vascular functions and atherosclerosis: effect of vitamins. Cardiovasc Drugs Ther 16:391-399, 2002. 87. Wall R, Harlan JM, Harker LA, Striker GE: Homocysteine induced endothelial cell injury in vivo: a review. Thromb Res 18:113-121, 1980. 88. Dudman NPB, Temple SE, Guo XW, Fu WY, Perry MA: Homocysteine enhances neutrophil endothelial interactions in vivo. Cir Res 84:409-416, 1999. 89. Heinecke JW, Rosen H, Suzuki LA, Chait A: The role of sulphur containing amino acids in super oxide production and modification of low density lipoprotein in arterial smooth muscle cells. J Biol Chem 262:1009810103, 1987. 90. Upchurch GR, Welch GN, Fabian AJ: Homocysteine decreases bioavailable Nitric Oxide by a mechanism involving glutathione peroxidase. J Biol Chem 272:17012-17017, 1997. 91. Hiltunen MO, via-Herttual S: DNA methylation, smooth muscle cells and atherogenesis. Arterioscler Thromb Vasc Biol 20:1557-1564, 2000. 92. Krumkan II, Culmsee C, Chan SL, et al: Homocysteine elicits a DNA damage response in neurons that promotes apoptosis and hypersensitivity to excitotoxins. J Neurosci 20:6920-6926, 2000. 93. Toyota Y, Yamamura T, Miyake Y, Yamamoto A: Low density lipoprotein (LDL) binding affinity for the LDL receptor in hyperlipoproteinemia. Atherosclerosis 147:77-86, 1999.
Downloaded from ang.sagepub.com at MCMASTER UNIV LIBRARY on February 1, 2013
Você também pode gostar
- s121 Cpnre Study GuideDocumento3 páginass121 Cpnre Study GuideCandice Cheng64% (14)
- Nursing Lab 3 Skill Performance Checklist Administering A Blood Transfusion S U NP CommentsDocumento2 páginasNursing Lab 3 Skill Performance Checklist Administering A Blood Transfusion S U NP CommentsCandice Cheng88% (8)
- Aan 202 CourseworkDocumento17 páginasAan 202 CourseworkCris GalendezAinda não há avaliações
- Physiology of Drowning PDFDocumento63 páginasPhysiology of Drowning PDFPeter PhelpsAinda não há avaliações
- Dr. Rabi Dhakal 1 Year MD Resident Department of PediatricDocumento29 páginasDr. Rabi Dhakal 1 Year MD Resident Department of PediatricRabi Dhakal100% (1)
- Acute Myocardial InfarctionDocumento20 páginasAcute Myocardial InfarctionDavid Christian CalmaAinda não há avaliações
- Anatomy and Physiology Case Study 2bDocumento4 páginasAnatomy and Physiology Case Study 2bDylle Lorenzo ClaudioAinda não há avaliações
- AtherosclerosisDocumento56 páginasAtherosclerosisJohn Matley Caampued100% (8)
- Malaria MEQDocumento6 páginasMalaria MEQMuvenn KannanAinda não há avaliações
- Rheumatology Cases Fall Clinics 2019Documento85 páginasRheumatology Cases Fall Clinics 2019NaziBrola TsivadzeAinda não há avaliações
- Multiple SclerosisDocumento6 páginasMultiple SclerosisandrearuzziAinda não há avaliações
- Stratethon Case PDFDocumento3 páginasStratethon Case PDFRajat YadavAinda não há avaliações
- The Aging AdultDocumento6 páginasThe Aging Adultlaryn dodd100% (2)
- Pathophysiology of Congestive Heart Failure: Cardiovascular SystemDocumento3 páginasPathophysiology of Congestive Heart Failure: Cardiovascular SystemMon GabrielAinda não há avaliações
- DB13 - Pathophysiology of AtherosclerosisDocumento2 páginasDB13 - Pathophysiology of Atherosclerosisi_vhie03Ainda não há avaliações
- Genetic DisordersDocumento9 páginasGenetic Disordersamerica25Ainda não há avaliações
- Pa Tho PhysiologyDocumento11 páginasPa Tho PhysiologyJonathan CuaAinda não há avaliações
- Role of The Kidney in Long Term RegulationDocumento19 páginasRole of The Kidney in Long Term RegulationMelisa NovitasariAinda não há avaliações
- Concept MapDocumento5 páginasConcept MapRon OpulenciaAinda não há avaliações
- Pathophysiology OrthoDocumento2 páginasPathophysiology OrthoAlexis Jean Calib-og BasconAinda não há avaliações
- TuberculomaDocumento7 páginasTuberculomaAdeleAinda não há avaliações
- Glycogen Storage Disorders PDFDocumento4 páginasGlycogen Storage Disorders PDFAHMEDAinda não há avaliações
- Portal Vein Thrombus ChildrenDocumento11 páginasPortal Vein Thrombus ChildrenViswas ChhapolaAinda não há avaliações
- Check ListDocumento11 páginasCheck ListtetarwalAinda não há avaliações
- Components of BloodDocumento10 páginasComponents of BloodTeYya NHikowl AguilarAinda não há avaliações
- Department of Kriyasharir: Mahatma Gandhi Ayurved College Hospital & Research Centre Salod (H), WardhaDocumento39 páginasDepartment of Kriyasharir: Mahatma Gandhi Ayurved College Hospital & Research Centre Salod (H), WardhaAvanti ShendurjaneAinda não há avaliações
- Anterior Pituitary DisordersDocumento4 páginasAnterior Pituitary DisordersJe LynAinda não há avaliações
- Diabetic Emergencies Case StudiesDocumento32 páginasDiabetic Emergencies Case StudiesLamria Maloni Siahaan0% (1)
- Hepatomegaly 1Documento5 páginasHepatomegaly 1Bobby ParksAinda não há avaliações
- Paget's Disease & Osteopetrosis AssignmentDocumento14 páginasPaget's Disease & Osteopetrosis AssignmentMustafa KhandgawiAinda não há avaliações
- Pathophysiology of InfectionDocumento3 páginasPathophysiology of Infectionchristianemmanuel18Ainda não há avaliações
- Metabolic Syndrome DR - Yunus, SPPDDocumento15 páginasMetabolic Syndrome DR - Yunus, SPPDMariaEllyNobetaHutabarat100% (1)
- Pathophysiology of AtherosclerosisDocumento27 páginasPathophysiology of AtherosclerosisAmira Paguyo QuilapioAinda não há avaliações
- Pathophysiology 2Documento92 páginasPathophysiology 2Princess AgarwalAinda não há avaliações
- Avascular NecrosisDocumento3 páginasAvascular Necrosisahmad shaltoutAinda não há avaliações
- Pathophysiology of MalariaDocumento20 páginasPathophysiology of Malariamelia100% (1)
- Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis - Pathogenesis, Clinical Manifestations, and Diagnosis - UpToDateDocumento41 páginasStevens-Johnson Syndrome and Toxic Epidermal Necrolysis - Pathogenesis, Clinical Manifestations, and Diagnosis - UpToDateDicky SangadjiAinda não há avaliações
- Distributive Shock PDFDocumento8 páginasDistributive Shock PDFAdreiTheTripleAAinda não há avaliações
- RicketsDocumento3 páginasRicketsLoverMind CabaronAinda não há avaliações
- Stevens Johnson DiseaseDocumento5 páginasStevens Johnson DiseaseShammy RNAinda não há avaliações
- Nutritional Support of Stroke Patients: ESPEN Congress Lisbon 2015Documento40 páginasNutritional Support of Stroke Patients: ESPEN Congress Lisbon 2015Risma SaroyaAinda não há avaliações
- Pathophysiology of OsteoarthritisDocumento1 páginaPathophysiology of OsteoarthritisGLADYS GARCIAAinda não há avaliações
- Aneurysm Final (Bentals Procedure)Documento55 páginasAneurysm Final (Bentals Procedure)tejuteju067100% (1)
- Pathophysiology of StrokeDocumento22 páginasPathophysiology of StrokeKingman844100% (3)
- Testicular CancerDocumento24 páginasTesticular CancerJulianne LeeAinda não há avaliações
- Pathophysiology ErDocumento3 páginasPathophysiology ErAlexa A. AldayAinda não há avaliações
- Heart FailureDocumento10 páginasHeart Failureurmila prajapatiAinda não há avaliações
- Rhabdomyolysis Case Study WeeblyDocumento18 páginasRhabdomyolysis Case Study Weeblyapi-241865788Ainda não há avaliações
- Rheumatoid ArthritisDocumento19 páginasRheumatoid ArthritisLiya AnjelinaAinda não há avaliações
- Myocardial InfarctionDocumento15 páginasMyocardial InfarctionameerAinda não há avaliações
- Agis Mira Dewi, S.kedDocumento35 páginasAgis Mira Dewi, S.kedAgiish EMdeAinda não há avaliações
- Poststreptococcal Glomerulonephritis - UpToDateDocumento21 páginasPoststreptococcal Glomerulonephritis - UpToDateHandre Putra100% (1)
- Bone Fracture Concept MapDocumento1 páginaBone Fracture Concept MapJette Charmae OlboAinda não há avaliações
- Acute Kidney InjuryDocumento37 páginasAcute Kidney InjuryLani BuenaventuraAinda não há avaliações
- Concept Map MI 2Documento1 páginaConcept Map MI 2nicole barcenaAinda não há avaliações
- Different Injuries of The Musculoskeletal System Its Management and CareDocumento113 páginasDifferent Injuries of The Musculoskeletal System Its Management and CareMaAn Castor Palcon TuzonAinda não há avaliações
- Crush Injury and Crush Syndrome PDFDocumento2 páginasCrush Injury and Crush Syndrome PDFMichael DrakeAinda não há avaliações
- Myocardialinfarction 150223043527 Conversion Gate02 PDFDocumento22 páginasMyocardialinfarction 150223043527 Conversion Gate02 PDFBhavika Aggarwal100% (1)
- Tuberculoma PDFDocumento9 páginasTuberculoma PDFselvie87Ainda não há avaliações
- Update On Cancer CachexiaDocumento4 páginasUpdate On Cancer CachexiaIyanAinda não há avaliações
- Avascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandAvascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNota: 4 de 5 estrelas4/5 (2)
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNo EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsAinda não há avaliações
- Pathophysiology and Pharmacotherapy of AtherosclerosisDocumento7 páginasPathophysiology and Pharmacotherapy of AtherosclerosisSandeep PooniaAinda não há avaliações
- Hypertrophic Pyloric StenosisDocumento3 páginasHypertrophic Pyloric StenosisCandice ChengAinda não há avaliações
- Tables of Normal ValuesDocumento6 páginasTables of Normal ValuesEunice BautistaAinda não há avaliações
- Easy Way To Learn ABGsDocumento13 páginasEasy Way To Learn ABGsMunaim TahirAinda não há avaliações
- Atherosclerosis As InflammationDocumento9 páginasAtherosclerosis As InflammationCandice Cheng0% (1)
- Human Sexuality Chapter 15 NotesDocumento7 páginasHuman Sexuality Chapter 15 NotesCandice ChengAinda não há avaliações
- Chest Pain NICEDocumento52 páginasChest Pain NICEAliya Batrisya AliyaAinda não há avaliações
- Acute Myocardial Infarction LANCETDocumento15 páginasAcute Myocardial Infarction LANCETSi vis pacem...Ainda não há avaliações
- Acute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesDocumento17 páginasAcute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesCandice ChengAinda não há avaliações
- Chapter 12Documento6 páginasChapter 12Candice ChengAinda não há avaliações
- FactsDocumento2 páginasFactsjanveeAinda não há avaliações
- Alzheimers Disease and Dental ManagementDocumento5 páginasAlzheimers Disease and Dental ManagementMalu OliveiraAinda não há avaliações
- Netter's Internal Medicine 2nd Ed 13Documento9 páginasNetter's Internal Medicine 2nd Ed 13Panagiotis SouldatosAinda não há avaliações
- Round Cell TumorsDocumento86 páginasRound Cell TumorsMadhura ShekatkarAinda não há avaliações
- The Practical Management of DepressionDocumento48 páginasThe Practical Management of Depressionpasha rashaAinda não há avaliações
- Cerebral Palsy Practice Essentials: Signs and SymptomsDocumento11 páginasCerebral Palsy Practice Essentials: Signs and SymptomsTahsinur RahmanAinda não há avaliações
- Evaluation and Prevention of Diabetic NeuropathyDocumento6 páginasEvaluation and Prevention of Diabetic Neuropathyvivek_win95Ainda não há avaliações
- Genetics and TeratologyDocumento21 páginasGenetics and Teratologypandem soniya0% (1)
- Pathology Notes HemalathaDocumento117 páginasPathology Notes HemalathapriyagerardAinda não há avaliações
- Thyroid ScintigraphyDocumento7 páginasThyroid ScintigraphyadaniAinda não há avaliações
- Ecart Medications and EquipmentDocumento9 páginasEcart Medications and EquipmentJan Philippe BelandoAinda não há avaliações
- 2021 Breeder-Management-Guide Cobb-Vantress (001-040)Documento40 páginas2021 Breeder-Management-Guide Cobb-Vantress (001-040)susey madelit apaza mamaniAinda não há avaliações
- Medical Examination Form: Tel Aviv University International International - Tau.Ac - IlDocumento6 páginasMedical Examination Form: Tel Aviv University International International - Tau.Ac - IlSiddaq SinghAinda não há avaliações
- Breasting FeedingDocumento46 páginasBreasting FeedingPriya bhattiAinda não há avaliações
- Book IV Medicine (De Medicina)Documento8 páginasBook IV Medicine (De Medicina)Marcus Annaeus LucanusAinda não há avaliações
- Hastening Death by VSED - Clinical Findings Panel HandoutsDocumento26 páginasHastening Death by VSED - Clinical Findings Panel HandoutsalmondpleasureAinda não há avaliações
- Splinting Techniques: by Madhumitha M, Aruna G, Abi P, Sakthivelayudham G, Sujidha R, Srivignesh MDocumento99 páginasSplinting Techniques: by Madhumitha M, Aruna G, Abi P, Sakthivelayudham G, Sujidha R, Srivignesh MSakthivelayudhamganesanAinda não há avaliações
- Point Scale: RUBRICS For Health Performance Jingle Making Programs and Policy On How To Prevent Non-Communicable DiseaseDocumento2 páginasPoint Scale: RUBRICS For Health Performance Jingle Making Programs and Policy On How To Prevent Non-Communicable Diseaseeliza cunananAinda não há avaliações
- Royal Medical Services Professional Training Division Logbook For Surgery ResidentsDocumento58 páginasRoyal Medical Services Professional Training Division Logbook For Surgery ResidentsMohammed SameerAinda não há avaliações
- Supervisi Berjenjang Di Era Pandemi Covid-19 Dalam Manajemen KeperawatanDocumento10 páginasSupervisi Berjenjang Di Era Pandemi Covid-19 Dalam Manajemen Keperawatanfebrian rahmatAinda não há avaliações
- Social Fluids: Metaphors and Meanings of Society: Bryan S. TurnerDocumento10 páginasSocial Fluids: Metaphors and Meanings of Society: Bryan S. TurnerWilliam wilsonAinda não há avaliações
- Fundamentals in Nursing TransDocumento14 páginasFundamentals in Nursing TransPia Gabrielle CabatanaAinda não há avaliações
- Ferdinand Marcos - Hero or NotDocumento3 páginasFerdinand Marcos - Hero or NotAsta AstaAinda não há avaliações
- History of HygieneDocumento24 páginasHistory of HygieneSama Al HayekAinda não há avaliações
- Rubella Virus Infection, The Congenital Rubella Syndrome, and The Link To AutismDocumento28 páginasRubella Virus Infection, The Congenital Rubella Syndrome, and The Link To AutismM Azzam SAinda não há avaliações
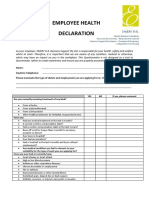
- Employee Health Declaration FormDocumento3 páginasEmployee Health Declaration FormKajal KumariAinda não há avaliações
- Anatomy and Physiology An Integrative Approach 2nd Edition Mckinley Solutions ManualDocumento26 páginasAnatomy and Physiology An Integrative Approach 2nd Edition Mckinley Solutions ManualEdwardStephensMDeqik100% (60)
- (Thi Có 06 Trang) TH I Gian Làm Bài: 60 Phút, Không K TH I Gian PHDocumento12 páginas(Thi Có 06 Trang) TH I Gian Làm Bài: 60 Phút, Không K TH I Gian PHNgọc HuyềnAinda não há avaliações