Escolar Documentos
Profissional Documentos
Cultura Documentos
September Case Study
Enviado por
api-174496267Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
September Case Study
Enviado por
api-174496267Direitos autorais:
Formatos disponíveis
1 Amanuel Negussie September Case Study Sep.
15, 2013 VMAT for Cancer of Base of Tongue History of Present Illness: BS is a 56-year-old gentleman who had pain in his right ear, right throat and had experienced right sided headaches for a number of months. He also had difficulty swallowing food. As the pain started to get worse, BS saw his primary physician and was referred to an otolaryngologist. An indirect laryngoscopy was performed in which a mass extending from the hypopharynx into the epiglottis was detected. A computed tomography (CT) of the neck was also performed and demonstrated an ulcerated base of tongue (BOT) mass that extended more into the right floor of mouth. It also extended into the vallecula and free margins of the epiglottis; but the remainder of the supraglottic larynx, preepiglottic fat, and area of glottis folds appeared uninvolved. However, the mass seemed to include the right and left geniohypid muscles and the right hyoglossus muscles. There was also a possibility of involvement of the right anterior belly of the digastrics. There were several left level II and III lymph nodes that were suspicious for metastatic disease with extracapsular spread. A positron emission tomography (PET) also demonstrated involvement of level II lymph nodes. There was no clear evidence of any metastatic disease. Biopsies were obtained and showed moderately differentiated squamous cell carcinoma. The tumor was positive for human papilloma virus (HPV). About 60% of oropharyngeal cancers are caused by HPV.1 The tumor was staged IVA T3 (stage 3 primary tumor) N2 (stage 2 regional lymph nodes) Mx (unknown metastasis). Past Medical History: BS has a history of hemochromatosis, which was treated with phlebotomies. Social History: BS is single and works as a carpenter. He has a history of smoking, 40 packs per year, but quit smoking a month ago. The patient reported that his brother had esophageal cancer at age 62. He has no other family history of cancer. Medications: BS currently uses the following medications: Duragesic, Lexapro, Nystatin, Oxycodone, mouthwash, multivitamin, and nicotine patch. Diagnostic Imaging: BS had a CT scan of the head and neck that demonstrated a mass in the BOT. The mass measured 4.4 x 4.4 x 4.1 centimeter (cm). The left level IIA lymph node measured 2.5 cm. There was a second adjacent node that measured 1.8 cm. The level III lymph
2 node measured 1.4 cm. DS also had a PET scan that showed tumor in the BOT with a standardized uptake value (SUV) of 9.4. There was an activity in the left level II lymph node with an SUV of 5.7 and left level III lymph nodes with an SUV of 5.9. There was also a right level II lymph node with an SUV of 3.8, which was under the size of 1 cm. Radiation Oncologist Recommendations: BS was recommended a concurrent chemoradiation treatment. The radiation oncologist discussed the typical radiation treatment course that will last 7 weeks with chemotherapy every 3 weeks. Possible acute side effects including skin irritation, sore throat, swallowing difficulties, loss of taste, dry mouth, nausea, and significant weight loss were explained to the patient. Potential long-term side effects including dry mouth, stiffness of the jaw or neck, damage to spinal cord, hypothyroidism, and prolonged swallowing issues were also explained. The benefit of prophylactic feeding tube versus placing one when needed was thoroughly discussed. The radiation oncologist recommended doing image guided radiation therapy (IGRT) with daily cone beam CT (CBCT) in order to minimize margins and minimize risk of side effects. The patient was recommended and had his teeth extracted before treatment. In oropharyngeal cancer, dental extraction prior to radiation treatment can reduce the incidence of osteonecrosis.2 The Plan (Prescription): After examining the patient and reviewing the diagnostic findings, the radiation oncologist decided to proceed with volumetric modulated arc therapy (VMAT). The treatment was prescribed to 6000 centigray (cGy) in 30 fractions to the right oropharynx and involved high-risk regions. A simultaneous prescription of 5400 cGy in 30 fractions was prescribed to elective nodal regions. A boost of 1000 cGy in 5 fractions was prescribed to involved nodes and right oropharynx for a total of 7000 cGy in 35 fractions. Patient Setup/Immobilization: BS was simulated in a supine position with his head towards the scanner. His head was fixed in a neutral position on an accufoam (Figure 1). An aquaplast mask was made by warming a thermoplastic mesh in a warm bath and stretching it over the patients face, neck, and shoulders (Figure 1). The customized mask was used to reproduce the same head position and restrict movement during treatment. A shoulder strap was used to pull the shoulders away from the treatment area (Figure 1). BS had a sponge under his knees for comfort. No bite block was used to immobilize the tongue. In patients who are being treated for the BOT with IMRT and where the contralateral neck is clinically negative, bite blocks should not be used
3 in order to spare the contralateral parotid gland.3 A General Electric (GE) CT unit was used for the simulation. The head and neck images were taken at 0.25 cm slices. Anatomical Contouring: After the simulation was completed, the CT slices were imported into the Varian Eclipse version 10 treatment planning system (TPS). The medical dosimetrist contoured most of the normal structures including the brain, brainstem, eyes, lenses, lungs, mandible, and spinal cord. The radiation oncologist contoured the parotids, oral cavity, gross tumor volume (GTV), clinical target volume (CTV), and planning target volume (PTV). The PTVs included PTV54, PTV60, and PTV 70 (Figure 2). The dental artifacts were contoured and assigned a density equivalent to water. Metal artifacts can distort dose distribution by creating cold and hot spots.4 This correction method can help reduce such complications. The spinal cord was expanded by 0.3 cm in all directions. Avoidance structures were created for organs at risk (OR) that overlapped with the target with 0.2 cm margin around PTV60. This included left parotid, right parotid, mandible, and oral cavity. An avoidance structure was also created for each shoulder. A 1 cm wide ring was constructed 2 cm away from the PTV60. The PTV54 was enlarged 0.1 cm in all direction for optimization purpose. The purpose of the ring was reduce beam streaking and increase dose conformity.
Beam Isocenter/Arrangement: A Varian 21 IX linear accelerator (Linac) was used to treat the patient. During simulation, the radiation oncologist set an isocenter within the treatment site. Three rotational arcs were arranged for the initial treatment, two in clockwise (CC) direction and one in counter clockwise (CCW) direction. The first beam rotated from 200o to 160o with 10o collimator angle and 15 x 17.2 cm field size (Figure 3). The second beam rotated from 200o to 160o with 300o collimator angle and 15 x 20.6 cm field size (Figure 4). The third beam rotated from160o to 200o with 350o collimator angle and 15 x 17.2 cm field size (Figure 5). The boost plan contained two arcs, CC and CCW direction. The CC beam rotated from 200o to 160o with 10o collimator angle and 14.5 x 10.3 cm field size (Figure 6). The CCW beam rotated from160o to 200o with 350o collimator angle and 14.5 x 10.3 cm field size (Figure 7). The couch rotation was set at 0o for all arcs. A 6 mega volt (MV) photon beam was used for all arcs. Treatment Planning: The medical dosimetrist started the initial plan by setting the appropriate gantry rotation, collimator angle, and field size. These were carefully arranged to allow full PTV exposure for each arc. The inverse planning process included clinical goals to the PTVs and
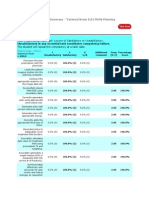
4 planning constraints to the ring, the avoidance structures, and OR. The progressive resolution optimizer (PRO) algorithm within the Eclipse software generated an ideal intensity map with optimal weighting of each control point. The MLC segments, the gantry speeds, and the dose rates of each control point were generated from the ideal intensity map. The plan was reviewed after each optimization and weightings of the objectives were adjusted based on the information retrieved from the dose volume histogram (DVH) and the isodose lines. The final three dimension (3D) dose distribution was evaluated using DVH analysis as well as viewing the 3D dose distribution in multi-plane view and on individual CT slices. The final dose calculation was performed using the analytical anisotropic algorithm (AAA). The plan was finalized with the 95% isodose line covering the PTV54 with a mean dose of 5087 cGy and maximum dose of 5643 cGy located within the PTV and PTV60 with a mean dose of 6138 cGy and maximum dose of 6474 cGy (Figure 8). All of the clinical goals and planning objectives were met (Figure 9). After careful review, the physician accepted the treatment plan. BS had 23 fractions of the initial treatment, but was re-simulated due to weight loss. The simulation was done with the same setup position and slice thickness as the initial simulation. However, a new thermoplastic mask was constructed. All OR and PTVs were re-contoured. The same approach was taken to plan the remaining 7 fractions. The avoidance structures included the parotids, mandible, oral cavity, and shoulders. The PTV54 was enlarged 0.1 cm in all direction and a 1 cm wide ring was constructed 2 cm away from PTV60. The plan was optimized with clinical goals set for the avoidance structures, OR, and PTVs. It was finalized with the 95% isodose line covering the PTV 54 with a mean dose of 1155 cGy and a maximum dose of 1292 cGy and PTV 60 with a mean dose of 1427 cGy and maximum dose of 1530 cGy (Figure 10). All of the clinical goals and planning objectives were met (Figure 11). The optimization for the boost plan was conducted with a new avoidance structures for the mandible and parotids 0.2 cm away from PTV70. A new 1 cm wide ring was also created 2 cm away from PTV70. PTV70 was enlarged 0.1 cm in all directions for optimization purposes. The plan was optimized multiple times with the necessary changes made to obtain the utmost OR sparing and target coverage. The plan was finalized with the 95% isodose line covering PTV70 with a mean dose of 1022 cGy and maximum dose of 1078 cGy (Figure 12). All of the clinical goals and planning objectives were met (Figure 13). The cumulative dose to the parotids, spinal cord, brainstem, oral cavity, and mandible was kept below their dose limit (Figure 14).
5 Quality Assurance (QA)/Physics Check: A monitor unit (MU) check was performed with RadCalc. At this facility, a 5% deviation in MU is the tolerance for all plans. Anything outside of this range needs to be re-calculated and fixed by the medical dosimetrists or physicists prior to the first treatment. Both the initial plans and the boost plan were approved with an individual MU difference less than 3% (Figures 15, 16, and 17). The rapid arc QAs were generated using the AAA of each arc. The intensity maps were calculated in a flat solid water phantom. The intensity maps were exported to be compared to measurements obtained with the SunNuclear MapCheck device. The initial plan passed the QA with 99.7%; the re planned initial plan with 98.4%; and the boost plan with 98.4%. Conclusion: One of the major challenges this plan presented was a change of contours due to patients weight loss. Weight loss during treatment may cause underdosage of tumor volumes and/or overdosage of OR.5 After a discussion with the physicist and medical dosimetrist, the radiation oncologist decided re-simulating and re-planning the remaining treatment was crucial. The patient was re-simulated with similar setup position and same immobilization devices. However, constructing a new aquaplast mask was necessary since the original mask was loose and not fitting well. All the normal structures and tumor volumes were re-contoured. The physician re-contoured the PTVs as close as the initial contours. A similar approach was taken to plan the remaining fractions. The composite plan that included the initial plan, the re-plan, and the boost plan was carefully assessed to assure that the constraints to all OR were met. Repeating the simulation and re-planning the treatment was the appropriate approach for this case as it allowed an adequate dose to the PTVs and a safe dose to OR.
6 Figures
Figure 1. Patients setup position with accufoam, aquaplast mask, and shoulder strap
Figure 2. Transverse, coronal, and sagittal view of the PTV. Green represents PTV70, blue represents PTV60, and brown represents PTV54.
Figure 3. Collimator angle and field size of the first arc for the initial plan covering PTV54 and PTV60.
Figure 4. Collimator angle and field size of the second arc for the initial plan covering PTV54 and PTV60.
Figure 5. Collimator angle and field size of the third arc for the initial plan covering PTV54 and PTV60.
Figure 6. Collimator angle and field size of the first arc for the boost plan covering PTV70.
Figure 7. Collimator angle and field size of the first arc for the boost plan covering PTV70.
Figure 8a. Transverse view of dose distribution for the initial plan. The 95% isodose line (blue) and 90% isodose line (orange) conformity around PTV54 and PTV60.
10
Figure 8b. Coronal view of dose distribution for the initial plan. The 95% isodose line (blue) and 90% isodose line (orange) conformity around PTV54 and PTV60.
Figure 8c. Sagittal view of dose distribution for the initial plan. The 95% isodose line (blue) and 90% isodose line (orange) conformity around PTV54 and PTV60.
11
Figure 9. DVH of the initial plan demonstrating dose distribution to PTVs and OR.
Figure 10a. Transverse view of dose distribution for the re-planned initial treatment. The 95% isodose line (blue) and 90% isodose line (orange) conformity around PTV54 and PTV60.
12
Figure 10c. Coronal view of dose distribution for the re-planned initial treatment. The 95% isodose line (blue) and 90% isodose line (orange) conformity around PTV54 and PTV60.
Figure 10c. Sagittal view of dose distribution for the re-planned initial treatment. The 95% isodose line (blue) and 90% isodose line (orange) conformity around PTV54 and PTV60.
13
Figure 11. DVH of the re-planned initial treatment demonstrating dose distribution to PTVs and OR
Figure 12a. Transverse view of dose distribution for the boost plan. The 95% isodose line (blue) conformity around PTV70.
14
Figure 12b. Coronal view of dose distribution for the boost plan. The 95% isodose line (blue) conformity around PTV70.
15
Figure 12c. Sagittal view of dose distribution for the boost plan. The 95% isodose line (blue) conformity around PTV70.
Figure 13. DVH of the boost plan demonstrating dose distribution to PTV and OR.
16
Figure 14. DVH of the plan sum demonstrating dose distribution to PTVs and OR.
17
Figure 15. MU check of the initial plan
18
Figure 16. MU check of the re-planned treatment
19
Figure 17. MU check of the boost plan
20 References 1. Hong AM, Dobbins TA, Lee CS, et al. Human papilloma virus predicts outcome in oropharyngeal cancer in patients treated primarily with surgery or radiation therapy. Br J Canc. 2010;103:1510-1517. 2. Bhide SA, Newbold KL, Harrington KJ, et al. Clinical evaluation of intensity-modulated radiotherapy for head and neck cancers. Br J Radiol. 2012;85:487-494. 3. Harrison LB, Sessions RB, Hong WK. Head and Neck Cancer: A Multidisciplinary Approach. 3rd ed. Philadelphia, PA. Lippincott Williams and Wilkins; 2009:331-332. 4. Kim Y, Tome WA, Todd MB, et al. The impact of metal artifacts on head and neck IMRT dose distribution. Radiother Oncol.2006;79(2):198-202. 5. Hansen EK, Bucci MK, Quivey JM, et al. Repeat CT imaging and replanning during the course of IMRT for head-and-neck cancer. Int J Radiat Oncol Biol Phy. 2006;64(2):355-362.
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Ec 102 Eclipseinverseplanningimrtandrapidarcv 13 CamanuelnegussieDocumento1 páginaEc 102 Eclipseinverseplanningimrtandrapidarcv 13 Camanuelnegussieapi-174496267Ainda não há avaliações
- Amanuel Negussie: Certificate of AttendanceDocumento1 páginaAmanuel Negussie: Certificate of Attendanceapi-174496267Ainda não há avaliações
- PhotonDocumento3 páginasPhotonapi-174496267Ainda não há avaliações
- Fall EvalsDocumento6 páginasFall Evalsapi-212894050Ainda não há avaliações
- ResumeDocumento2 páginasResumeapi-174496267Ainda não há avaliações
- Fall EvalsDocumento6 páginasFall Evalsapi-212894050Ainda não há avaliações
- Joe RTDocumento1 páginaJoe RTapi-174496267Ainda não há avaliações
- V 13 RtsummaryonsitetrainingworkshopfamanuelnegussieDocumento1 páginaV 13 Rtsummaryonsitetrainingworkshopfamanuelnegussieapi-174496267Ainda não há avaliações
- Amanuel Final 5 1 14Documento19 páginasAmanuel Final 5 1 14api-174496267Ainda não há avaliações
- ImrtDocumento3 páginasImrtapi-174496267Ainda não há avaliações
- BrachytherapyDocumento3 páginasBrachytherapyapi-174496267Ainda não há avaliações
- ElectronDocumento2 páginasElectronapi-174496267Ainda não há avaliações
- ConferenceDocumento7 páginasConferenceapi-174496267Ainda não há avaliações
- Fall EvalsDocumento6 páginasFall Evalsapi-212894050Ainda não há avaliações
- Case Log FallDocumento2 páginasCase Log Fallapi-174496267Ainda não há avaliações
- Monthly EvalDocumento2 páginasMonthly Evalapi-174496267Ainda não há avaliações
- Tally 1Documento2 páginasTally 1api-174496267Ainda não há avaliações
- For E-PortfolioDocumento14 páginasFor E-Portfolioapi-174496267Ainda não há avaliações
- ComptotalsDocumento3 páginasComptotalsapi-174496267Ainda não há avaliações
- ConferencesDocumento4 páginasConferencesapi-174496267Ainda não há avaliações
- Conference LogsDocumento1 páginaConference Logsapi-174496267Ainda não há avaliações
- Comprehensive Case Study - AnDocumento31 páginasComprehensive Case Study - Anapi-174496267Ainda não há avaliações
- PT Case LogsDocumento2 páginasPT Case Logsapi-174496267Ainda não há avaliações
- Comprehensive Case Study Final - AdjustedDocumento17 páginasComprehensive Case Study Final - Adjustedapi-174496267Ainda não há avaliações
- August Citation AssignmentDocumento2 páginasAugust Citation Assignmentapi-174496267Ainda não há avaliações
- July Case StudyDocumento18 páginasJuly Case Studyapi-174496267Ainda não há avaliações
- October Case StudyDocumento15 páginasOctober Case Studyapi-174496267Ainda não há avaliações
- May EvalDocumento6 páginasMay Evalapi-174496267Ainda não há avaliações
- 2nd Rotation PallDocumento3 páginas2nd Rotation Pallapi-174496267Ainda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- T.N.T. health hazards of munitions workDocumento3 páginasT.N.T. health hazards of munitions workLetícia LamasAinda não há avaliações
- Virtual Pig Dissection Worksheet 06-07 2Documento6 páginasVirtual Pig Dissection Worksheet 06-07 2api-255054890Ainda não há avaliações
- Aesthetic Facial Anatomy Essentials For Injections-CRC Press (2020)Documento259 páginasAesthetic Facial Anatomy Essentials For Injections-CRC Press (2020)stella95% (22)
- (José Almeida) Atlas of Endovascular Venous SurgeDocumento516 páginas(José Almeida) Atlas of Endovascular Venous SurgeTa TaAinda não há avaliações
- DR Asia ResumeDocumento2 páginasDR Asia ResumeAasiya TarannumAinda não há avaliações
- Post Partum Care (Puerperium) : Iril I. Panes, RN, MANDocumento48 páginasPost Partum Care (Puerperium) : Iril I. Panes, RN, MANJonaPhieDomingoMonteroIIAinda não há avaliações
- PulpotecDocumento2 páginasPulpotecFeras Al-ZbounAinda não há avaliações
- Maternal and Child Health Is The Program of The Department of Health Created To Lessen The Death of Infants and Mother in The PhilippinesDocumento18 páginasMaternal and Child Health Is The Program of The Department of Health Created To Lessen The Death of Infants and Mother in The PhilippinesNicole Marin-ChingAinda não há avaliações
- Psoriasis and Parapsoriasis Literature ReviewDocumento2 páginasPsoriasis and Parapsoriasis Literature ReviewBetharlitha PurLikaAinda não há avaliações
- Review of Level 1 Hospital Floor PlansDocumento6 páginasReview of Level 1 Hospital Floor PlansBEA GAinda não há avaliações
- Awesome Birthe BookDocumento278 páginasAwesome Birthe BookOlga SilvaAinda não há avaliações
- Colorectal Cancer Screening: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Documento49 páginasColorectal Cancer Screening: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)StangPongritAinda não há avaliações
- Post Tpa Care SheetDocumento2 páginasPost Tpa Care SheetDewanggaWahyuPrajaAinda não há avaliações
- Paul Karason, Blue ManDocumento4 páginasPaul Karason, Blue ManAlphonse AlvkardAinda não há avaliações
- Case GNApsDocumento47 páginasCase GNApsAndhika Hadi WirawanAinda não há avaliações
- Hospital Management SoftwareDocumento2 páginasHospital Management SoftwareAnsar AhmadAinda não há avaliações
- Pedia Nicu NotesDocumento32 páginasPedia Nicu NotesChristian Noel Fernandez100% (2)
- Shierhana Awali Arasa: Trainings & SeminarsDocumento2 páginasShierhana Awali Arasa: Trainings & SeminarsShierhana Awali ArasaAinda não há avaliações
- Daftar Pustaka: Selma Mutiara Hani, Dr. Moh Nailul Fahmi, SP - OG Dr. Fatwa Sari Tetra Dewi, MPH., PH.DDocumento10 páginasDaftar Pustaka: Selma Mutiara Hani, Dr. Moh Nailul Fahmi, SP - OG Dr. Fatwa Sari Tetra Dewi, MPH., PH.DRohadatul Aisy Kurnia PutriAinda não há avaliações
- 123456Documento85 páginas123456Mario ŠaravanjaAinda não há avaliações
- Pediatric General Anesthesia for COVID-19 PatientDocumento4 páginasPediatric General Anesthesia for COVID-19 PatientHainey GayleAinda não há avaliações
- NP 12345 EyyyyDocumento133 páginasNP 12345 EyyyySjerwin Anthony Gianan100% (2)
- Pelvic Organ Prolapse GuideDocumento15 páginasPelvic Organ Prolapse GuidesaraeboAinda não há avaliações
- ResumeDocumento2 páginasResumeapi-283008119Ainda não há avaliações
- MDH Sustainability Report 2011Documento52 páginasMDH Sustainability Report 2011Jangshik BaboAinda não há avaliações
- Renal Scintigraphy Procedures and IndicationsDocumento18 páginasRenal Scintigraphy Procedures and IndicationsViorelVelenciucAinda não há avaliações
- Basic Splinting TechniquesDocumento5 páginasBasic Splinting TechniquesRicardo BragaAinda não há avaliações
- "Spiritual Midwifery" (2003), by Ina May Gaskin: Midwifery Is A Book AboutDocumento5 páginas"Spiritual Midwifery" (2003), by Ina May Gaskin: Midwifery Is A Book AboutEdwin IV DomendenAinda não há avaliações
- Medical Ethics Dissertation TopicsDocumento8 páginasMedical Ethics Dissertation TopicsThesisPaperHelpCanada100% (1)
- Osce-Stations - Blogspot.co - Id-Cervical Smear Amp ExamDocumento2 páginasOsce-Stations - Blogspot.co - Id-Cervical Smear Amp ExamPatrick BayuAinda não há avaliações