Escolar Documentos
Profissional Documentos
Cultura Documentos
Comprehensive Case Study Final - Adjusted
Enviado por
api-174496267Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Comprehensive Case Study Final - Adjusted
Enviado por
api-174496267Direitos autorais:
Formatos disponíveis
1 Amanuel Negussie Compiled Case Study August 2013 Effectiveness of IMRT vs.
VMAT in sparing the mandible, larynx, and parotid glands for oropharyngeal cancer treatment Abstract: Introduction: This study aims to compare and contrast sparing of the mandible, larynx, and parotid glands in treatment of oropharyngeal cancer using IMRT and VMAT techniques. Case Description: A treatment with IMRT or VMAT using multiple boost techniques was demonstrated in the following 3 cases. Patient 1 represents a case of 3 target volumes treated for a postoperative squamous cell carcinoma of the base of tongue using IMRT plus 3DCRT. Patient 2 represents a case of three target volumes treated for a postoperative squamous cell carcinoma of the tonsil using VMAT alone. Patient 3 represents a case of two target volumes treated for squamous cell carcinoma of the base of tongue using VMAT plus 3DCRT as a definitive treatment. Conclusion: Each case was individually evaluated on how well normal structures were spared and whether the plan met the objectives. The plans were evaluated based on RTOG and QUANTEC guidelines. Oropharyngeal cancer treatments using IMRT plus 3DCRT, VMAT alone, and VMAT plus 3DCRT have been demonstrated on how well the ipsilateral parotid, larynx, and mandible can be spared with optimal target coverage. Key Words: oropharyngeal cancer, 3DCRT, IMRT, VMAT, mandible, parotid glands, larynx Introduction The anatomy of oropharynx extends inferiorly to the hyoid bone and includes the base of tongue and tonsil.1 Oropharyngeal cancer commonly occurs in the base of tongue and tonsil and is less common in the soft palate and posterior pharyngeal wall.2 About 60% of oropharyngeal cancers are caused by human papilloma virus (HPV).3 The management of oropharyngeal cancer is multidisciplinary, which may include surgery, radiation therapy, or chemotherapy. The type of
2 treatment chosen for each patient may vary based on the stage and patients status. Radiation therapy is one of the most important treatment approaches that can either be used as a definitive treatment or as an adjuvant postoperative treatment. Radiation therapy alone is a standard approach for early staged oropharyngeal tumors.4 Radiation therapy alone or with chemotherapy is also more effective in HPV related oropharyngeal tumors.3 Since oropharyngeal cancers are often approached with a curative intent and are treated with high dose radiation, normal organ preservation is essential. The presence of various radiosensitive structures in the head and neck region make treatment planning a difficult task. Advanced treatment techniques such as intensity modulated radiation therapy (IMRT) and volumetric modulated radiation therapy (VMAT) are becoming standard treatment methods due to their ability to reduce dose to normal structures. Even with these techniques radiation therapy treatments can cause significant acute and late toxicities.5 Late reactions mainly includes xerostomia, dysphagia, and osteonecrosis.5 As a result, special attention must always be given to the parotid glands, mandible, and larynx when planning oropharyngeal cancer treatments. Maintaining salivary flow by preserving salivary glands is fundamental in oropharyngeal cancer treatments. Studies from University of Michigan showed that IMRT can reduce contralateral parotid dose to 32% compared with 93% using standard traditional technique.6 According to a study by Blanco et al.7, patients with bilateral parotid mean dose greater than 25 gray (Gy) have poor salivary function; whereas, decreased xerostomia was recorded when one or both parotids received a mean dose less than 25 Gy. Although sparing the contralateral parotid is of utmost important, the significance of sparing the ipsilateral parotid is debatable.8 Current radiation therapy oncology group (RTOG) and quantitative analysis of normal tissue effects in the clinic (QUANTEC) guidelines require minimizing mean dose for parotid below 26 Gy (Table 1). The incidence of osteonecrosis after oropharyngeal cancer treatment is 5-15% depending on the dose to mandible and patients dental hygiene.5 This can be reduced by dental extraction and limiting the dose to mandible below 60 Gy.5 A large number of patients who undergo surgery and radiation treatment for oropharyngeal cancer benefit from implant supported prosthesis. High dose radiation to the anterior mandible can lead to prosthesis implant failure to this region.9 Compared to other head and neck sites, the dose to the mandible is higher in oropharyngeal cancer treatments.10 Generally, risk of osteonecrosis is dependent on the volume of mandible
3 irradiated to high radiation dose. RTOG guideline recommends limiting the maximum dose for the mandible to below 66 Gy (Table 1). Sparing larynx is also essential in oropharyngeal cancer treatments to prevent dysphagia and aspiration. IMRT can be used in two different methods to achieve this; junctioned IMRT (JIMRT) and whole field IMRT (WF-IMRT). In J-IMRT, the upper portion of the target is treated with IMRT matched to an anterior (AP) field with a laryngeal block to treat the lower portion of the target.11 In WF-IMRT, the entire target is treated with IMRT fields.11 Multiple studies have shown that WF-IMRT can significantly reduce the mean dose for larynx when compared to JIMRT.11 QUANTEC recommends limiting the maximum dose for the larynx to below 66 Gy and the mean dose to below 50 Gy (Table 1). RTOG recommends the maximum dose to be kept below 45 Gy (Table 1). Methods and Materials Patient selection Patient 1 is a 63 year old male with a stage T2 (stage 2 primary tumor) N0 (no regional lymph nodes) M0 (no metastasis) squamous cell carcinoma of the base of tongue (BOT). The patient was initially treated with left hemiglossectomy and left selective neck dissection. The radiation therapy plan was designed to target two planning target volumes (PTV) with single IMRT dose painted plan followed by a boost to a third PTV with 3 dimensional radiation therapy (3DCRT). The first PTV targeted the bilateral nodal chains. The second PTV targeted the primary tumor bed plus regions of grossly involved lymphadenopathy. The third PTV targeted regions that are high risk for recurrence. Patient 2 is a 61 year old male with HPV positive stage T1 (stage 1 primary tumor) N2 (stage 2 regional lymph nodes) M0 squamous cell carcinoma of the left tonsil. The patient was initially treated with tonsillectomy and neck dissection. The radiation therapy plan was designed to target three PTVs with separate VMAT plans. The first PTV targeted the bilateral nodal chains. The second PTV targeted the primary tumor bed plus regions of grossly involved lymphadenopathy. The third PTV targeted regions that are high risk for recurrence. Patient 3 is an 82 year old male with a stage T3 (stage 3 primary tumor) N2 M0 squamous cell carcinoma of BOT. The patient was not a surgery candidate due to his respiratory condition.
4 Therefore, radiation therapy was given as a definitive treatment. The radiation therapy plan was designed to target two PTVs initially with VMAT followed by a boost with 3DCRT. The first PTV targeted the bilateral nodal chains. The second PTV targeted the tumor and involved lymph nodes. Patient Set-up All three patients were scanned in a supine position on a head support. Patient 3 was positioned with this head and chest slightly inclined using a breast board due to his inability to lay flat on the computer tomography (CT) couch. In all 3 cases, an aquaplast mask was used to immobilize the head, neck, and shoulders. A shoulder strap was used for patients 2 and 3 to ensure the shoulders were pulled away from the treatment area. A bite block was used for patient 2 but not for patients 1 and 3. In patients treated for a base of tongue where the contralateral neck is clinically negative, bite blocks should not be used in order to spare the contralateral parotid gland.12 A wire was placed on the surgical scar for patients 1 and 2. Target Delineation The Pinnacle3 treatment planning system (TPS) version 9 was used for patient 1 and Eclipse TPS version 10 was used for patients 2 and 3. The CT scan was obtained for all three patients in the described treatment position. The CT images were taken at 3 millimeter (mm) slices for patient 1 and 2.5 mm for patients 2 and 3. The variation in slice thickness is due to different departmental preferences. Two CT scans were obtained for patient 1, with and without non-iodinated intravenous (IV) contrast. The two scans were fused, the scan without an IV contrast being the primary planning scan. The structures contoured by the medical dosimetrist included: the surgical scar, spinal cord, brainstem, and mandible. The radiation oncologist contoured the brachial plexus, parotid glands, esophagus, larynx, oral cavity, and the targets. The PTVs included: PTV 54 (the PTV receiving 54 Gy), PTV 60 (the PTV receiving 60 Gy), and PTV66 (the PTV receiving 66 Gy). For patient 2, no diagnostic images were fused with the planning CT scans. The medical dosimetrist contoured the eyes, lenses, lungs, inner ears, optic nerves, and mandible. The radiation oncologist contoured the parotid glands, oral cavity, optic chiasm, pituitary gland, submandibular gland, thyroid, and targets. The PTVs included: PTV 50 (the PTV receiving 50 Gy), PTV 64 (the PTV receiving 64 Gy), and PTV 70 (the PTV receiving 70 Gy).
5 For patient 3, the planning CT was fused with a diagnostic magnetic resonance imaging (MRI) of the head and neck. The normal structures contoured by the medical dosimetrist were the brain, brainstem, eyes, lenses, lungs, inner ears, optic nerves, and mandible. The radiation oncologist contoured the parotid glands, optic chiasm, oral cavity, and the targets. The PTVs included PTV 50 and PTV 70. Treatment Planning The dose prescription and planning parameters are presented for each case in Table 2. For patient 1, dose objectives were set for PTV 60, PTV 54, spinal cord, spinal cord planning organ at risk volume (PRV) (spinal cord + 5 mm), brain stem, brain stem PRV (brain stem + 5mm), parotids, larynx, and mandible. RTOG 0920 protocol was used as a guide to map out the plan. More priority was given to meet the spinal cord and brainstem constraints. Many attempts were made to minimize the dose to the rest of the normal structures. Two off cord lateral beams were used for the PTV 66 boost plan in an effort to minimize the dose to the brainstem and spinal cord. For patient 2, the initial treatment for PTV 50 was planned with dose objectives set for PTV 50, spinal cord PRV, brain stem, parotid glands, oral cavity, mandible, submandibular glands, and the shoulders. A precaution was taken to carefully minimize the dose to the normal structures and leave room for the boost dose contribution. The QUANTEC guidelines were used to map out the plan. The dose objectives set for the boost plan included PTV 64, PTV 70, and all the normal structures used in the initial plan. For patient 3, the initial plan for PRV 50 was planned with dose objectives set for PTV 50, spinal cord PTV, brain stem, parotid glands, oral cavity, mandible, submandibular glands, and shoulders. A precaution was taken to minimize the dose to the ipsilateral parotid and leave room for dose distribution from the boost plan. The boost to PTV 70 was planned with two off cord lateral beams in an attempt to minimize the dose to the spinal cord and brainstem. In each case, the medical dosimetrists approached the plan with an effort to create an optimal PTV coverage with the dose constraints for OR meeting RTOG or QUANTEC guidelines. The maximum dose for each plan was also kept below 110%. For the normal structures that overlapped with the target, the tissues within the PTV were cropped out with 2 mm margin for optimization purpose. The structures included: mandible, parotids, submandibular glands, and larynx. This technique helped the medical dosimetrists to manipulate the dose to the normal
6 structures without affecting the PTV coverage. In order to increase dose conformality around the target, a 1 centimeter (cm) ring created 2 cm away from the PTV was used during the optimization process of patients 2 and 3 VMAT plans. Plan Analysis & Evaluation The most notable difference between VMAT and IMRT is a variation in monitor unit (MU) and treatment time. Various studies have presented that VMAT can provide lower MU per fraction with shorter delivery time. VMAT is also known to provide better dose conformity than IMRT. However, IMRT can generate plans with better dose homogeneity.12 A study by Clemente et al12 showed that, in oropharyngeal cancers, higher larynx sparing can be achieved with IMRT but better ipsilateral parotid sparing can be achieved with VMAT. Another study by Teoh et al13 demonstrated a lower contralateral parotid sparing can be achieved with VMAT than IMRT. Patient 1s treatment was planned based on RTOG guidelines. The ipsilateral parotid gland was spared with a mean dose of 17.3 Gy. The maximum dose constraint for the mandible was met with 63.3 Gy. The mean dose for the mandible was 39.7 Gy and did not meet the goal. The larynx also did not meet RTOG guidelines and was finalized with a mean dose of 36.6 Gy and a maximum dose of 56.8 Gy. All targets were well covered with the 95% isodose line and a maximum dose less than 110% (Figure 1 and Table 3). The plan was acceptable to the physician since a large volume of both the mandible and larynx overlapped with the targets. Patient 2s treatment was planned based on QUNTEC guidelines. The constraints for both the ipsilateral was met. The mean dose for the left parotid was 16.4 Gy. For the larynx, the mean dose was 51 Gy and the maximum dose was 72.8 Gy. Although QUANTEC does not have a dose limit for the mandible, the plan was finalized with a mean dose of 38.4 Gy and maximum dose of 65 Gy. This does not meet RTOG guidelines. All targets were covered with the 95% isodose line and a maximum dose less than 110% (Figure 2 and Table 3). The plan was acceptable to the physician since the parotid, larynx, and the rest of OR were effectively spared. For patient 3, QUANTEC guidelines were used for planning. The constraints for both the parotid was met. The mean dose for the ipsilateral parotid was 19.6 Gy. The mean dose for the larynx was 69.4 Gy and the maximum dose was 74.1 Gy. The plan was finalized with the mean dose for mandible being 40.3 Gy and the maximum dose being 69.3. All targets were well covered with the 95% isodose line and a maximum dose less than 110% (Figure 3 and Table 3). Although the
7 dose to mandible did not meet RTOGs constraint, the plan was acceptable to the physician since the rest of OR were spared effectively. All the constraints for the remaining OR including the brainstem, oral cavity, and spinal cord were met in all three cases (Table 3). The ipsilateral parotid gland was spared with a mean dose less than 20 Gy for all three plans. The parotid was spared the most in Patient 2 where the entire plan was carried out using VMAT (Table 3). A similar study by Clemente et al13 also showed that VMAT is better in sparing the ipsilateral parotid gland. In Patients 1 and 3, since the final boost was carried out with 3DCRT, the parotid was spared the most in the initial plans. This was done purposely to leave room for dose contribution from the boost plans. Since QUANTEC guidelines were used to evaluate Patients 2 and 3s plan, less priority was given for the mandible. From the three cases, the only plan that met RTOGs constraints for mandible was patient 2. Patient 1 met one of the two constraints but Patient 3 did not meet either of the constraints. All three cases have very similar mean dose with patient 2 being the lowest. The lowest maximum dose for the mandible was achieved for Patient 1 treated with IMRT plus 3DCRT (Table 3). Early onset necrosis mainly occurs if the maximum dose is above 70 Gy.10 In all three cases, the maximum dose was kept below 70 Gy (Table 3). QUANTEC and RTOG have different constraints for larynx (Table 1). All three cases met QUANTECs constraint but not RTOGs (Table 3). The larynx presented the greatest challenge for the medical dosimetrists since a large volume of it lies in between the targets. Comparatively, patient 1 has the lowest mean and maximum dose (Table 3). The larynx for Patient 3 was spared the least. This may be due to the boost, which was planned with right and left lateral beams targeting PTV70. In analyzing Table 3, all three techniques, IMRT plus 3DCRT, VMAT alone, and VMAT plus 3DCRT provided clinically acceptable plans. An overall average lower mean dose for the OR was achieved with the IMRT plus 3DCRT technique (Table 3). Note that in this plan the 3DCRT was used to deliver only 6 Gy of the final boost to PTV66. A lower mean and maximum dose to OR was achieved with VMAT alone than VMAT plus 3DCRT (Table 3). The dose contribution from 3DCRT increased the OR dose in Patient 3. Results and Discussion
8 The three cases demonstrated different techniques of approaching oropharyngeal cancer treatment. The ipsilateral parotid, mandible, and larynx are the three important structures that presented the greatest challenge in the planning process of each treatment. This is mainly due to the fact that these structures overlapped with the targets. In such cases, minimizing the dose to the OR and meeting their constraints may not be possible without affecting the PTV coverage. If PTV coverage is more important than sparing the overlapped OR, then the medical dosimetrist has to make sure that the maximum dose does not fall within the overlapped region. Difference in prescription between Patient 1 versus Patients 2 and 3 may be a limitation for a comparison among the three cases. In addition, difference in dose calculation algorithms, planning approaches, and departmental preferences can be another limitation.
9 Figures
Contours: light blue = PTV54, blue = PTV60 Isodose lines: blue = 51.3 Gy, red = 57 Gy
Contours: red = PTV 66 Isodose line: yellow = 5.7 Gy
Figure 1. Patient 1: Target Delineation, Dose Distribution, and DVH
10
Contour: light blue = PTV50 Isodose line: blue = 47.5 Gy
Contours: pink = PTV64, red PTV70 Isodose line: orange = 60.8, green = 66.5
DVH of the initial plan showing the dose distribution to ipsilateral parotid, mandible, and PTV
11
DVH of the boost plans showing the dose distribution to the ipsilateral parotid, and PTVs Figure 2. Patient 2: Target Delineation, Dose Distribution, and DVH
12
Contour: blue = PTV 50 Isodose line: 47.5 Gy
Contour: light blue = PTV 70 Isodose line: orange = 66.5 Gy
Figure 3. Patient 3: Target Delineation, Dose Distribution, and DVH
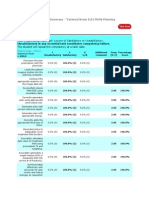
13 Tables Table 1: RTOG and QUANTEC dose constraints for parotid glands, mandible, and larynx. Organ Volume Bilateral whole parotid glands Parotid Unilateral whole parotid gland Dmean < 20 Gy Dmean < 26 Gy V50 < 30Gy QUANTEC14 Dmean < 25 Gy RTOG15 20 cc < 20 Gy
Mandible
N/A
Dmax < 66 Gy Dmean < 38 Gy
Whole organ Whole organ Larynx Whole organ
Dmax < 66 Gy Dmean < 50 Gy [Aspiration] Dmean < 44 Gy [Edema]
Dmax < 45 Gy
Whole organ *Note: Dmean (mean dose), Dmax (maximum dose)
V50 < 27%
Table 2: Prescription and Treatment Planning Parameters Prescription and Treatment Planning Parameters Case Site Patient 1 BOT Prescription Technique Fractionation IMRT (SIB)+3DCRT Standard Fractionation Beam Energy Dose to PTV1 Dose to PTV2 Dose to PTV3 6 MV 54 Gy 60 Gy 66 Gy VMAT Standard Fractionation 6 MV 50 Gy 64 Gy 70 Gy VMAT+3DCRT Standard Fractionation 6 MV 50 Gy 70 Gy Patient 2 Tonsil Patient 3 BOT
Treatment Planning Parameters
14 Beam Arrangement (9) Co-planar beams for the initial fields (2) Co-plannar beams for the boost fields (3) Co-planar arc beams for PTV1 (2) Co-planar arc beams for PTV2 and PTV3 Gantry Angles/Rotations Initial 160o, 120o, 80o, 40o, 0o, 320o, 280o, 240o, 200o Boost (PTV3) 270o and 90o PTV1 205o - 155o coll 5o 155o - 205o coll 355o 205o - 155o coll 5o PTV2 210o -179o coll 10o 179o - 210o coll 350o PTV3 210o - 150o coll 20o 150o - 210o coll 340o *Note: BOT (base of tongue), MV (megavoltage), SIB (simultaneous integrated boost,) coll (collimator) Table 3. Plan Analysis and Evaluation Plan Analysis and Evaluation Structures Patient 1 (Gy) Dmean PTV1 PTV2 PTV3 Ipsilateral parotid Mandible Larynx Brain stem Spinal cord 58.4 61.7 64.6 17.3 39.7 36.6 1.65 23.3 Dmax 64.6 64.6 61.6 58.8 63.3 56.8 9.99 45.2 Dmean 51 65.3 71.4 16.4 38.4 51 4.4 26.3 55 69.8 76.3 63 65 67.8 31.5 35.3 Patient 2 (Gy) Dmax 49 69.7 N/A 19.6 40.3 69.4 13.5 22.7 Dmean Patient 3 (Gy) Dmax 52.2 73.7 N/A 70.4 69.3 74.1 40 38.5 PTV1 235o - 105o coll 5o 105o - 235o coll 355o 235o 105o coll 5o PTV2 270o and 90o (3) Co-planar arc beams for PTV1 (2) Co-planar beams for PTV2
15 Oral cavity 30.2 59.2 37.8 52 37.2 53
*Note: the Dmean and Dmax shown here represent the result of the composite plan
16 References 1. Arruda FF, Puri DR, Zhung J, et al. Intensity-modulated radiation therapy for the treatment of oropharyngeal carcinoma: The Memorial Sloan Kettering Cancer Center experience. Int J Radiat Oncol Biol Phy. 2006;64(2):363-373. doi:10.1016/j.ijrobp.2005.03.006 2. Haigentz M, Silver CE, Corry J, et al. Current trends in initial management of oropharyngeal cancer: the declining use of open surgery. Eur Arch Oto-Rhino-L. 2009;266(12):1845-1855. doi:10.1007/s00405-009-1109-2 3. Hong AM, Dobbins TA, Lee CS, et al. Human papilloma virus predicts outcome in oropharyngeal cancer in patients treated primarily with surgery or radiation therapy. Br J Canc. 2010;103:1510-1517. doi:10.1038/sj.bjc.6605944 4. Hong TS, Tome WA, Harari PM. Heterogeneity in head and neck IMRT target design and clinical practice. Radiother Oncol. 2012;103(1):92-98. doi: 10.1016/j.radonc.2012.02.010 5. Bhide SA, Newbold KL, Harrington KJ, et al. Clinical evaluation of intensity-modulated radiotherapy for head and neck cancers. Br J Radiol. 2012;85(1013):487-494. doi:10.1259/bjr/85942136 6. Eisbrush A, Ship JA, Martel MK, et al. Parotid gland sparing in patients undergoing bilateral head and neck irradiation: techniques and early results. Int J Radiat Oncol Biol Phys. 1996;36:469-480. doi:10.1016/S0360-3016(96)00264-7 7. Blanco AI, Chao C, Naqa IE, et al. Dose volume modeling of salivary functioning patient with head and neck cancer receiving radiotherapy. Int J Radiat Oncol Biol Phys. 2005;62(4):1055-1069. doi:10.1016/j.ijrobp.2004.12.076 8. Claus F, Duthoy W, Boterberg T, et al. Intensity modulated radiation therapy for oropharyngeal and oral cavity tumors: clinical use and experience. Oral Oncol. 2002;38(6):597-604. doi:10.1016/S1368-8375(01)00111-7 9. Verdonck HWD, De Jong JMA, Granzier MEPG, et al. Intensity-modulated radiation therapy for oropharyngeal cancer: Radiation dosage constraint at anterior mandible. Radiat Oncol. 2009;45(6):511-514. doi:10.1016/j.oraloncology.2008.07.007 10. Nguyen NP, Vock J, Chi A, et al. Effectiveness of intensity modulated and image guided radiotherapy for spare the mandible from excessive radiation. Oral Oncol. 2012:48(7);653657 doi:10.1016/j.oraloncology.2012.01.016
17 11. Ad VB, Lin H, Hwang WT, et al. Larynx-sparing techniques using intensity-modulated radiation therapy for oropharyngeal cancer. Med Dosim. 2012;37(4):383-386. doi:10.1016/j.meddos.2012.02.004 12. Harrison LB, Sessions RB, Hong WK. Head and Neck Cancer: A Multidisciplinary Approach. 3rd ed. Philadelphia, PA. Lippincott Williams and Wilkins; 2009:331-332. 13. Clemente S, Wu BB, Giuseppe S, et al. Smartarc based volumetric modulated arc therapy for oropharyngeal cancer: a dosimetric comparison with both intensity modulated radiation therapy and helical tomotherapy. Int J Radiat Oncol Biol Pys. 2011;80(4):1248-1255. doi:10.1016/j.ijrobp.2010.08.007 14. Teoh M, Beveridge S, Wood K, et al. Volumetric-modulated arc therapy (RapidArc) vs. conventional fixed field intensity modulated radiotherapy for F-FDG-PET-guided dose escalation in oropharyngeal cancer: A planning study. Med Dosim. 2013;38(1):18-24. doi: 10.1016/j.meddos.2012.05.002 15. Marks LB, Yorke ED, Jackson A, et al. Use of normal tissue complication probability models in clinic. Int J Radiat Oncol Biol Phys. 2010;76(3):S10-S19. doi:10.1016/j.ijrobp.2009.07.1754 16. Machtay M. A phase III study of postoperative radiationtherapy (IMRT)+/- Cetuximab for locally advanced resected head and neck cancer. http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0920. 2013. Accessed August 1, 2013.
Você também pode gostar
- V 13 RtsummaryonsitetrainingworkshopfamanuelnegussieDocumento1 páginaV 13 Rtsummaryonsitetrainingworkshopfamanuelnegussieapi-174496267Ainda não há avaliações
- Ec 102 Eclipseinverseplanningimrtandrapidarcv 13 CamanuelnegussieDocumento1 páginaEc 102 Eclipseinverseplanningimrtandrapidarcv 13 Camanuelnegussieapi-174496267Ainda não há avaliações
- Amanuel Negussie: Certificate of AttendanceDocumento1 páginaAmanuel Negussie: Certificate of Attendanceapi-174496267Ainda não há avaliações
- Amanuel Final 5 1 14Documento19 páginasAmanuel Final 5 1 14api-174496267Ainda não há avaliações
- Joe RTDocumento1 páginaJoe RTapi-174496267Ainda não há avaliações
- ResumeDocumento2 páginasResumeapi-174496267Ainda não há avaliações
- ImrtDocumento3 páginasImrtapi-174496267Ainda não há avaliações
- ConferenceDocumento7 páginasConferenceapi-174496267Ainda não há avaliações
- Comprehensive Case Study - AnDocumento31 páginasComprehensive Case Study - Anapi-174496267Ainda não há avaliações
- PhotonDocumento3 páginasPhotonapi-174496267Ainda não há avaliações
- Fall EvalsDocumento6 páginasFall Evalsapi-212894050Ainda não há avaliações
- Fall EvalsDocumento6 páginasFall Evalsapi-212894050Ainda não há avaliações
- BrachytherapyDocumento3 páginasBrachytherapyapi-174496267Ainda não há avaliações
- ElectronDocumento2 páginasElectronapi-174496267Ainda não há avaliações
- Fall EvalsDocumento6 páginasFall Evalsapi-212894050Ainda não há avaliações
- Monthly EvalDocumento2 páginasMonthly Evalapi-174496267Ainda não há avaliações
- For E-PortfolioDocumento14 páginasFor E-Portfolioapi-174496267Ainda não há avaliações
- ComptotalsDocumento3 páginasComptotalsapi-174496267Ainda não há avaliações
- Case Log FallDocumento2 páginasCase Log Fallapi-174496267Ainda não há avaliações
- September Case StudyDocumento20 páginasSeptember Case Studyapi-174496267Ainda não há avaliações
- ConferencesDocumento4 páginasConferencesapi-174496267Ainda não há avaliações
- Tally 1Documento2 páginasTally 1api-174496267Ainda não há avaliações
- October Case StudyDocumento15 páginasOctober Case Studyapi-174496267Ainda não há avaliações
- May EvalDocumento6 páginasMay Evalapi-174496267Ainda não há avaliações
- July Case StudyDocumento18 páginasJuly Case Studyapi-174496267Ainda não há avaliações
- Conference LogsDocumento1 páginaConference Logsapi-174496267Ainda não há avaliações
- August Citation AssignmentDocumento2 páginasAugust Citation Assignmentapi-174496267Ainda não há avaliações
- PT Case LogsDocumento2 páginasPT Case Logsapi-174496267Ainda não há avaliações
- 2nd Rotation PallDocumento3 páginas2nd Rotation Pallapi-174496267Ainda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Syllabus For Bachelor of Physiotherapy (BPT) Academic ProgrammeDocumento36 páginasSyllabus For Bachelor of Physiotherapy (BPT) Academic ProgrammevikasmaeAinda não há avaliações
- 2022-Brochure Neonatal PiccDocumento4 páginas2022-Brochure Neonatal PiccNAIYA BHAVSARAinda não há avaliações
- Food Processing NC II - SAGDocumento4 páginasFood Processing NC II - SAGNylmazdahr Sañeud DammahomAinda não há avaliações
- Biochem Nucleic Acid ReviewerDocumento5 páginasBiochem Nucleic Acid ReviewerGabrielle FranciscoAinda não há avaliações
- HVAC (Heating, Ventilation and Air Conditioning) : SRS PrecautionsDocumento1 páginaHVAC (Heating, Ventilation and Air Conditioning) : SRS PrecautionssoftallAinda não há avaliações
- Science and TechnologyDocumento21 páginasScience and TechnologyPat MillerAinda não há avaliações
- HUM110 Gilgamesh EssayDocumento4 páginasHUM110 Gilgamesh EssaynsmeganAinda não há avaliações
- Join Our Telegram Channel: @AJITLULLA: To Get Daily Question Papers & SolutionsDocumento24 páginasJoin Our Telegram Channel: @AJITLULLA: To Get Daily Question Papers & SolutionsNaveen KumarAinda não há avaliações
- Dr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFDocumento72 páginasDr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFagnesspratiwiAinda não há avaliações
- Comparative Pharmacology For AnesthetistDocumento162 páginasComparative Pharmacology For AnesthetistGayatri PalacherlaAinda não há avaliações
- Inlet Manifold Pressure - Test: Testing and AdjustingDocumento2 páginasInlet Manifold Pressure - Test: Testing and AdjustingAbdoulaye Boua BERTHEAinda não há avaliações
- 3 Activities For Adults To Practice Modeling SELDocumento10 páginas3 Activities For Adults To Practice Modeling SELDavid Garcia PerezAinda não há avaliações
- REV Description Appr'D CHK'D Prep'D: Tolerances (Unless Otherwise Stated) - (In)Documento2 páginasREV Description Appr'D CHK'D Prep'D: Tolerances (Unless Otherwise Stated) - (In)Bacano CapoeiraAinda não há avaliações
- 2019 06 28 PDFDocumento47 páginas2019 06 28 PDFTes BabasaAinda não há avaliações
- Heteropolyacids FurfuralacetoneDocumento12 páginasHeteropolyacids FurfuralacetonecligcodiAinda não há avaliações
- UK Tax SystemDocumento13 páginasUK Tax SystemMuhammad Sajid Saeed100% (1)
- Mushrooms and Religion: Amanita MuscariaDocumento8 páginasMushrooms and Religion: Amanita MuscariaGummyCola50% (2)
- Cover Letter UchDocumento1 páginaCover Letter UchNakia nakia100% (1)
- A Comprehensive Review of Cementitious Grouts - Composition, Properties, Requirements and Advanced PerformanceDocumento16 páginasA Comprehensive Review of Cementitious Grouts - Composition, Properties, Requirements and Advanced PerformanceiporrasAinda não há avaliações
- Bio411 C1Documento1 páginaBio411 C1Aqiena BalqisAinda não há avaliações
- NG Teng Fong Discharge DocumentsDocumento14 páginasNG Teng Fong Discharge DocumentsAnonymous yGwMIPJRawAinda não há avaliações
- Aldehydes, Ketones, Carboxylic Acids, and EstersDocumento11 páginasAldehydes, Ketones, Carboxylic Acids, and EstersNATURE COMPUTERAinda não há avaliações
- BV Lesson Plan 4Documento3 páginasBV Lesson Plan 4api-252119803Ainda não há avaliações
- Blueprint Huynh My Ky Duyen 2022 McDonald'sDocumento2 páginasBlueprint Huynh My Ky Duyen 2022 McDonald'sHuỳnh Mỹ Kỳ DuyênAinda não há avaliações
- Latest Low NOx Combustion TechnologyDocumento7 páginasLatest Low NOx Combustion Technology95113309Ainda não há avaliações
- Chewable: Buy Pepcid AC Packages, Get Pepcid AC 18'sDocumento2 páginasChewable: Buy Pepcid AC Packages, Get Pepcid AC 18'sMahemoud MoustafaAinda não há avaliações
- Viscoline Annular UnitDocumento4 páginasViscoline Annular UnitjoquispeAinda não há avaliações
- DX340LC: Crawler ExcavatorDocumento20 páginasDX340LC: Crawler ExcavatorFeristha Meriani TabitaAinda não há avaliações
- Current Concepts of Enzyme Histochemistry in Modern PathologyDocumento11 páginasCurrent Concepts of Enzyme Histochemistry in Modern PathologyRosa AquinoAinda não há avaliações
- Discharge PlanDocumento3 páginasDischarge PlanBALOGO TRISHA MARIEAinda não há avaliações