Escolar Documentos
Profissional Documentos
Cultura Documentos
Case Study Preeclampsia
Enviado por
Claudia SanchezDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Case Study Preeclampsia
Enviado por
Claudia SanchezDireitos autorais:
Formatos disponíveis
Initial History and Assessment
At 0600 Jennie is brought to the Labor and Delivery triage area by her sister. The client complains of a pounding headache for the last 12 hours unrelieved by acetaminophen (Tylenol), swollen hands and face for 2 days, and epigastric pain described as bad heartburn. Her sister tells the nurse, "I felt like that when I had toxemia during my pregnancy." Admission assessment by the nurse reveals: today's weight 182 pounds, T 99.1 F, P 76, R 22, BP 138/88, 4+ pitting edema, and 3+ protein in the urine. Heart rate is regular, and lung sounds are clear. Deep tendon reflexes (DTRs) are 3+ biceps and triceps and 4+ patellar with 1 beat of ankle clonus. The nurse applies the external fetal monitor, which shows a baseline fetal heart rate of 130, absent variability, positive for accelerations, no decelerations, and no contractions. The nurse also performs a vaginal examination and finds that the cervix is 1 cm dilated and 50% effaced, with the fetal head at a 2 station. In reviewing Jennie's history, the nurse is correct in concluding that Jennie is in jeopardy of developing a hypertensive disorder due to which risk factors? To accurately assess this client's condition, what information from the prenatal record is most important for the nurse to obtain?
Pathophysiology of Preeclampsia
There is no definitive cause of preeclampsia, but the pathophysiology is distinct. The main pathogenic factor is poor perfusion as a result of arteriolar vasospasm. Function in organs such as the placenta, liver, brain, and kidneys can be depressed as much as 40 to 60%. As fluid shifts out of the intravascular compartment, a decrease in plasma volume and subsequent increase in hematocrit is seen. The edema of preeclampsia is generalized. Virtually all organ systems are affected by this disease, and the mother and fetus suffer increasing risk as the disease progresses. Preeclampsia develops after 20 weeks gestation in a previously normotensive woman. Elevated blood pressure is frequently the first sign of preeclampsia. The client also develops proteinuria. While no longer considered a diagnostic measurement of preeclampsia, generalized edema of the face, hands, and abdomen that is not responsive to 12 hours of bedrest is often present. Preeclampsia progresses along a continuum from mild to severe preeclampsia, HELLP syndrome, or eclampsia. A client may present to the labor unit anywhere along that continuum. What is the pathophysiology responsible for Jennie's complaint of a pounding headache and the elevated DTRs? Jennie's sister is very concerned about the swelling (edema) in her sister's face and hands because it seems to be worsening rapidly. She asks the nurse if the healthcare provider will prescribe some of "those water pills" (diuretics) to help get rid of the excess fluid. Which response by the nurse is correct?
Admission to the Labor and Delivery Unit
At 0630 the nurse calls to report to the healthcare provider, who prescribes the following: admit to labor and delivery, bed rest with bathroom privileges (BRP), IV D5LR at 125 ml/hr, CBC with platelets, clotting studies, liver enzymes, chemistry panel, 24-hour urine collection for protein and uric acid, ice chips only by mouth, nonstress test, hourly vital signs, and DTRs. While awaiting the lab results, which nursing intervention has the highest priority? Which technique is best for the nurse to use when evaluating Jennie's blood pressure while she is on bed rest? The nurse performs a nonstress test to evaluate fetal well-being.
HELLP Syndrome
At 0800, physical assessment and labs reveal the following: the client is still complaining of a headache but the epigastric pain has slightly decreased. While resting in a left lateral position, the vital signs are BP 146/94, P 75, R 18. Hyperreflexia continues with one beat of clonus. The baseline fetal heart rate is 140 with average long-term variability and no decelerations. Since completion of a reactive nonstress test, no further accelerations have occurred. Lab results include: hemoglobin - 13.1 g/dl, hematocrit - 40.5 g/dl, platelets - 120,000 mm3, aspartate aminotransferase (AST) - slightly elevated, alanine aminotransferase (ALT) - normal for pregnancy, 0 burr cells on slide, clotting studies normal for pregnancy. The healthcare provider diagnoses Jennie with preeclampsia rather than HELLP syndrome, a variant of severe preeclampsia.
Plan of Care: Magnesium Sulfate Administration
Prior to initiating the healthcare provider's prescription, the nurse must first obtain consent for vaginal and cesarean birth, analgesia and anesthesia, and blood transfusion. The nurse is aware that pregnant adolescents are considered emancipated minors. Therefore, Jennie can sign the consent forms herself. The healthcare provider prescribes this plan of care for Jennie: 1. Obtain permits for vaginal birth, cesarean birth, analgesia/anesthesia, and blood transfusion. 2. Start on magnesium sulfate (4 gm bolus over 20 min, then 1 gm/hr per pump) per unit protocol. (The recommended bolus is 4 to 6 grams) 3. Follow standing magnesium sulfate protocol (may vary by hospital): o Primary IV: Lactated Ringer's solution o Total fluid volume: 150 ml/hour o Insert Foley catheter with urimeter attachment for hourly I&O o Bedrest o Vital signs & DTRs hourly after stabilized on magnesium sulfate o Continuous uterine and fetal monitoring o Calcium gluconate at bedside 4. Begin oxytocin (Pitocin) induction per protocol. What is the primary action of magnesium sulfate when given in preeclampsia?
Which assessment finding would indicate to the nurse that a client is experiencing magnesium sulfate toxicity?
A Legal Issue
The nurse asks Jennie if the healthcare provider has discussed labor and delivery processes, potential complications, and the management of those complications with her, and if she understands them. Jennie replies, "I think so," then asks for a pen. Which action should the nurse take? Jennie's sister offers to sign the consent forms for her because Jennie is so young and just isn't feeling well right now. Which response by the nurse is correct?
Evaluation
The 0900 assessment reveals: Jennie reports that her headache has decreased slightly, but the epigastric pain has increased. Complaints of scotoma began about 5 minutes ago. Reflexes are 4+ biceps and patellar and 3+ triceps with 3 beats of ankle clonus. Vital signs are: T 99 F, P 80, R 19, BP 144/96. The most recent blood magnesium level is 2 gm/dl. Intake since admission (@0600) is 150 ml and output is 300 ml. The healthcare provider increases the magnesium sulfate prescription to 2 gm/hr. Fetal monitor tracing reveals a baseline fetal heart rate in the 120s, minimal long-term variability, no accelerations, and no decelerations. Uterine contractions are occurring every 4 to 5 minutes and they are moderate quality upon palpation. Cervical exam indicates the cervix is now 3 cm dilated and 80% effaced, with the presenting part (cephalic) at -1 station. Jennie reports mild discomfort with contractions but does not want anything for pain at this time. Jennie's partner and sister are at the bedside helping her use relaxation breathing through each contraction. Jennie is in the right lateral position with the head of the bed slightly elevated. Jennie asks why the magnesium sulfate was increased. What explanation should the nurse provide? When the nurse evaluates the fetal monitor strip, she notes a decrease in the fetal heart rate longterm variability.
A Complication Occurs
At 0930 Jennie's sister rings the call bell and yells, "Come quickly, Jennie is shaking all over." The nurse determines that Jennie is experiencing an eclamptic seizure. Which nursing intervention takes priority?
After the seizure ends, the nurse assesses the status of membranes, which may have ruptured with the seizure, as well as the fetal heart rate and the contraction status. The nurse observes the following pattern on the external fetal monitor: Contractions occur every 3 minutes and last 60 seconds. The baseline fetal heart rate is 130 beats per minute, and there is minimal long-term variability. At the peak of each contraction, the fetal heart rate gradually decreases to 117 beats per minute, then returns to the baseline 15 seconds after the contraction ends. What type of periodic fetal heart rate change is occurring? Jennie is lying on her left side. Oxygen is being administered via mask at 10 liters per minute. Both of these actions incorporate principles of intrauterine resuscitation. Intrauterine resuscitation is directed toward improving uterine blood flow and increasing maternal oxygenation and cardiac output. What should the nurse do next to ensure intrauterine resuscitation?
Prevention and Treatment of Medication Complications
No further seizures occur, and at 1000 the nursing assessment reveals that Jennie is groggy but responsive with hand grasp weak bilaterally. Her DTRs are 1+ biceps, triceps, and patellar with no ankle clonus. Vital signs: BP 138/88, P 82, R 14. The most recent magnesium level is 8 gm/dl. The hourly intake is 175 ml, and the output is 25 ml. The baseline fetal heart rate via external monitor is baseline 130 with minimal, but improving, longterm variability. There are no accelerations, and the decelerations have ceased. Spontaneous rupture of the amniotic membranes (SROM) occurred with the seizure, and the fluid is clear. Contractions are occurring every 3 minutes and lasting 60 seconds. The contractions are strong to palpation. Vaginal exam by the healthcare provider reveals that the cervix is dilated 7 cm and is 100% effaced and that the fetal head is at 0 station. The healthcare provider makes the decision to continue labor rather than perform a cesarean section because both mother and baby are stabilizing, and the cervix is changing. Jennie is crying with each contraction and requests something for pain. After consultation with the anesthesia provider, the healthcare provider prescribes an epidural using a local anesthetic agent as opposed to an opioid analgesic. What medication should be readily available as an antidote for magnesium sulfate? Which complication is Jennie most at risk for following the epidural with a local anesthestic, such as bupivacaine or ropivacaine?
Client Teaching: Pushing Technique
At 1130 Jennie complains of rectal pressure and an urge to push. Her headache is worsening, but she reports no scotoma and no epigastric pain. Her vital signs are: T 98.4 F, P 70, R 16, BP 130/83. DTRs are 1+ biceps and triceps; unable to elicit patellar, no clonus. Intake for the last hour is 150 ml, and output is 30 ml.
The baseline fetal heart rate is 120 with minimal long-term variability, positive for accelerations and mild variable decelerations. Strong contractions lasting 70 seconds are occurring every 2 to 3 minutes. Jennie's cervix is now 10 cm dilated, and the fetal head is at +3 station. The nurse informs the healthcare provider. Because Jennie is completely dilated and has the urge to push, the nurse reviews the proper pushing technique with Jennie and her partner.
1200: A Baby is Born
Jennie gives birth vaginally to a baby girl. The Apgar score is 2 at 1 minute, 6 at 5 minutes, and 7 at 10 minutes. After Jennie and her partner hold the baby for a few minutes, the baby is taken to the neonatal intensive care unit (NICU) for observation. The placenta is delivered spontaneously, and Jennie remains in the labor/delivery/recovery room. The NICU nurse anticipates and prepares for which complications in the newborn related to treatment of the mother with magnesium sulfate?
Post-birth Care
Jennie remains on magnesium sulfate. No further seizures have occurred, and she is stable at the present time. The anesthesia provider has released Jennie from the postanesthesia care unit. Which room and nursing staff assignments should be made for Jennie? Jennie's partner asks if some friends can come and watch television with him now that the baby has been born." Which response by the nurse is most appropriate?
The nurse is aware that continued magnesium sulfate puts Jennie at risk for postpartum hemorrhage even though Pitocin is infusing. Which medication is safest for Jennie if a second one is needed to treat postpartum hemorrhage?
Case Outcome
By 36-hours postpartum Jennie is diuresing and has decreased edema. She also has decreased CNS irritability and a slight decrease in her BP. All of these are signs that the preeclampsia is resolving. She is transferred to the Mother/Baby unit as is her newborn, who is also stable. Breastfeeding is successfully initiated. On the fourth postpartum day, both are discharged home with follow-up planned in one week. Since the risk for preeclampsia recurrence in subsequent pregnancies is 30%, the nurse emphasizes the importance of sharing her history of the disease during this pregnancy with healthcare providers during any future pregnancies.
Você também pode gostar
- Medical Surgical Nursing With MnemonicsDocumento110 páginasMedical Surgical Nursing With MnemonicsJerome F. Adorable, RN92% (76)
- Aloe VeraDocumento25 páginasAloe VeraClaudia Sanchez100% (2)
- CHARACTER FORMATION 1 PrelimDocumento15 páginasCHARACTER FORMATION 1 PrelimAiza Minalabag100% (1)
- Pregnancy Induced Hypertension (Pih)Documento56 páginasPregnancy Induced Hypertension (Pih)shandi23100% (5)
- Schizophrenia and Psychotic Disorders PPT Chap 21Documento46 páginasSchizophrenia and Psychotic Disorders PPT Chap 21Claudia SanchezAinda não há avaliações
- Schizophrenia and Psychotic Disorders PPT Chap 21Documento46 páginasSchizophrenia and Psychotic Disorders PPT Chap 21Claudia SanchezAinda não há avaliações
- PreeclampsiaDocumento58 páginasPreeclampsiarhyanne100% (8)
- Preeclampsia Case StudyDocumento30 páginasPreeclampsia Case Studysamangelo94Ainda não há avaliações
- Unit 1 Module 3 Rep in PlantsDocumento26 páginasUnit 1 Module 3 Rep in Plantstamesh jodhanAinda não há avaliações
- Hyperbilirubinemia Case StudyDocumento7 páginasHyperbilirubinemia Case Studyr_ramos0759Ainda não há avaliações
- Dysfunctional Labor and BirthDocumento167 páginasDysfunctional Labor and BirthKristel Joy Sarmiento AsuncionAinda não há avaliações
- 5 - Abortion or MiscarriageDocumento43 páginas5 - Abortion or Miscarriageasifdawar2011Ainda não há avaliações
- Gestational HypertensionDocumento17 páginasGestational HypertensionRubinaAinda não há avaliações
- Preeclampsia, Severe, UncontrolledDocumento22 páginasPreeclampsia, Severe, UncontrolledLharra Cagulada-PostranoAinda não há avaliações
- Pregnancy Induced Hypertension (PIH) : Case Scenario 4Documento4 páginasPregnancy Induced Hypertension (PIH) : Case Scenario 4Mae Arra Lecobu-anAinda não há avaliações
- Pregnancy Induced Hypertension (PIH)Documento3 páginasPregnancy Induced Hypertension (PIH)Susan HepziAinda não há avaliações
- Severe PreeclampsiaDocumento84 páginasSevere PreeclampsiaJm Bernardo50% (2)
- Case AGNDocumento66 páginasCase AGNMohaima PanditaAinda não há avaliações
- Gestational HypertensionDocumento6 páginasGestational HypertensionDimitrisSoulisAinda não há avaliações
- Genil v. Rivera DigestDocumento3 páginasGenil v. Rivera DigestCharmila SiplonAinda não há avaliações
- Gestational HypertensionDocumento72 páginasGestational HypertensionYn El100% (1)
- Government College of Nursing Jodhpur (Raj.) : Procedure On-Cordiotocography Subject-Obstetrics & Gynecology Specialty-IDocumento6 páginasGovernment College of Nursing Jodhpur (Raj.) : Procedure On-Cordiotocography Subject-Obstetrics & Gynecology Specialty-Ipriyanka100% (1)
- Case Study Placenta Previa This Is It 1Documento71 páginasCase Study Placenta Previa This Is It 1Homework Ping100% (1)
- Final Copy For Pre-EclampsiaDocumento60 páginasFinal Copy For Pre-EclampsiaSheena ClaireAinda não há avaliações
- Preeclampsia Case StudyDocumento9 páginasPreeclampsia Case StudyVanet100% (2)
- Hypertension in Pregnancy CompiledDocumento67 páginasHypertension in Pregnancy CompiledRaiza Love Caparas-PablicoAinda não há avaliações
- In Partial Fulfillment of The Requirements in Care of Mother and Child and Adolescent 217 Related Learning ExperienceDocumento28 páginasIn Partial Fulfillment of The Requirements in Care of Mother and Child and Adolescent 217 Related Learning ExperienceAllyssa BunagAinda não há avaliações
- CP On Pre-EclampsiaDocumento152 páginasCP On Pre-Eclampsiakathy100% (2)
- CP Preeclampsia RevisedDocumento32 páginasCP Preeclampsia RevisedTessa Grace PugonAinda não há avaliações
- JMDocumento45 páginasJMDana Fajardo RezanoAinda não há avaliações
- Pre Eclampsia - FinalDocumento54 páginasPre Eclampsia - Finalsupernurse02Ainda não há avaliações
- Pre Eclampsia Case StudyDocumento39 páginasPre Eclampsia Case StudyAnton RossiniAinda não há avaliações
- New Case of Pre-EclampsiaDocumento13 páginasNew Case of Pre-EclampsiaKristine AlejandroAinda não há avaliações
- Case Study PreeclampsiaDocumento3 páginasCase Study PreeclampsiaRima Christa Ulin SitepuAinda não há avaliações
- Case Study On Ob Ward PreeclampsiaDocumento12 páginasCase Study On Ob Ward PreeclampsiaNimrod83% (6)
- Case3 Case StudyDocumento6 páginasCase3 Case StudyKrizzia Angela BacotocAinda não há avaliações
- Case - Eclampsia FinalDocumento84 páginasCase - Eclampsia FinalKimberley Anne SantosAinda não há avaliações
- Case Study: Acute GlomerulonephritisDocumento19 páginasCase Study: Acute GlomerulonephritisKuruma Maricar SorianoAinda não há avaliações
- GastroschisisDocumento19 páginasGastroschisiskunaidongAinda não há avaliações
- Case Study Ob 3Documento10 páginasCase Study Ob 3matahfakahAinda não há avaliações
- CHN Case Analysis Case ScenarioDocumento7 páginasCHN Case Analysis Case ScenarioNathalie kate petallarAinda não há avaliações
- Obesity Prevention and Education For School Nurses Community Health NursingDocumento66 páginasObesity Prevention and Education For School Nurses Community Health NursingGabrielaAinda não há avaliações
- Normal Spontaneous DeliveryDocumento1 páginaNormal Spontaneous DeliveryGi GiAinda não há avaliações
- Case Pres AutosavedDocumento21 páginasCase Pres AutosavedJaysellePuguonTabijeAinda não há avaliações
- Mechanism of LaborDocumento12 páginasMechanism of LaborSaidatul Safarah Md HassanAinda não há avaliações
- Hydatidiform Mole: PGI Sia, Kevin PGI Tan, SheilaDocumento80 páginasHydatidiform Mole: PGI Sia, Kevin PGI Tan, SheilaSheila Mary TanAinda não há avaliações
- Premature Rupture of MembranesDocumento3 páginasPremature Rupture of MembranesSheena Kunkel100% (2)
- Pre EclampsiaDocumento13 páginasPre EclampsiaEniamrahs DnalonAinda não há avaliações
- Pregestational DiabetesDocumento7 páginasPregestational Diabetesraisya farah monicaAinda não há avaliações
- A Case Presentation On Pregnancy Induced HypertensionDocumento7 páginasA Case Presentation On Pregnancy Induced Hypertensionzygote_23100% (1)
- Eclampsia Nursing Case AnalysisDocumento38 páginasEclampsia Nursing Case AnalysisMary Justine Nuyad-AfricaAinda não há avaliações
- Case Study - Incomplete Abortion Related To APSDocumento8 páginasCase Study - Incomplete Abortion Related To APSRomeo ReyesAinda não há avaliações
- PREECLAMPSIA Case ScenarioDocumento2 páginasPREECLAMPSIA Case Scenariosabao kizuiteAinda não há avaliações
- ALTERED POST PARTUM Complications Nursing Lecture and Care PlanDocumento13 páginasALTERED POST PARTUM Complications Nursing Lecture and Care PlanKristelle Joy Capili SicatAinda não há avaliações
- Incomplete AbortionDocumento18 páginasIncomplete AbortionAra DirganAinda não há avaliações
- COURSE in The WARD Interhospital FinalDocumento8 páginasCOURSE in The WARD Interhospital Finalkimadlo656Ainda não há avaliações
- Severe Pre EclampsiaDocumento110 páginasSevere Pre EclampsiaJachel Kathleen LaguioAinda não há avaliações
- Case Stude NNJDocumento6 páginasCase Stude NNJmuzamirAinda não há avaliações
- Acute Glomerulonephritis (AGN)Documento35 páginasAcute Glomerulonephritis (AGN)jennalyn_dejelo100% (1)
- Acute PyelonephritisDocumento24 páginasAcute PyelonephritisChristine Karen Ang Suarez100% (1)
- Ob Case Presentation GDMDocumento78 páginasOb Case Presentation GDMmarsphinx50% (4)
- Nursing Care Plan: Obstetrics and Gynecology Nursing RotationDocumento8 páginasNursing Care Plan: Obstetrics and Gynecology Nursing RotationMary Justine Nuyad-AfricaAinda não há avaliações
- Case Study MiscariageDocumento14 páginasCase Study MiscariagesexiiimammaAinda não há avaliações
- West Avenue, Molo, Iloilo City NCM 109 Rle: Care of Mother, Child at Risk or With Problems (Acute and Chronic)Documento3 páginasWest Avenue, Molo, Iloilo City NCM 109 Rle: Care of Mother, Child at Risk or With Problems (Acute and Chronic)snow.parconAinda não há avaliações
- Management of Eclampsia: Baha M. SibaiDocumento9 páginasManagement of Eclampsia: Baha M. SibaiPiyawan Fern YodpetchAinda não há avaliações
- Case Scenario 3Documento2 páginasCase Scenario 3Winter KimAinda não há avaliações
- Standards FAQ Details - Joint CommissionDocumento5 páginasStandards FAQ Details - Joint CommissionClaudia SanchezAinda não há avaliações
- Lecture Outline: Reproductive Choices: Making Responsible DecisionsDocumento51 páginasLecture Outline: Reproductive Choices: Making Responsible DecisionsClaudia SanchezAinda não há avaliações
- 271 Physical AssessmentDocumento4 páginas271 Physical AssessmentClaudia SanchezAinda não há avaliações
- Shoulder DystociaDocumento37 páginasShoulder DystociaClaudia SanchezAinda não há avaliações
- Nasal Cannula Use in NICUDocumento2 páginasNasal Cannula Use in NICUClaudia SanchezAinda não há avaliações
- Domestic Abuse Outline COMPLETE-4Documento5 páginasDomestic Abuse Outline COMPLETE-4Claudia SanchezAinda não há avaliações
- "Making The Best of A Bad Situation": Shoulder DystociaDocumento37 páginas"Making The Best of A Bad Situation": Shoulder DystociaClaudia SanchezAinda não há avaliações
- Exam 1Documento1 páginaExam 1Claudia SanchezAinda não há avaliações
- Chapter 25 CardiacDocumento66 páginasChapter 25 CardiacClaudia SanchezAinda não há avaliações
- FHWA Guidance For Load Rating Evaluation of Gusset Plates in Truss BridgesDocumento6 páginasFHWA Guidance For Load Rating Evaluation of Gusset Plates in Truss BridgesPatrick Saint-LouisAinda não há avaliações
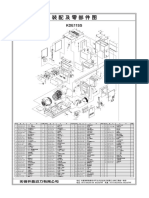
- Colfax MR Series CompresorDocumento2 páginasColfax MR Series CompresorinvidiuoAinda não há avaliações
- Test Bank For Psychology 6th Edition Don HockenburyDocumento18 páginasTest Bank For Psychology 6th Edition Don HockenburyKaitlynMorganarwp100% (42)
- Caring For Women Experiencing Breast Engorgement A Case ReportDocumento6 páginasCaring For Women Experiencing Breast Engorgement A Case ReportHENIAinda não há avaliações
- RARE Manual For Training Local Nature GuidesDocumento91 páginasRARE Manual For Training Local Nature GuidesenoshaugustineAinda não há avaliações
- (Sat) - 072023Documento7 páginas(Sat) - 072023DhananjayPatelAinda não há avaliações
- SCERT Kerala State Syllabus 9th Standard English Textbooks Part 1-1Documento104 páginasSCERT Kerala State Syllabus 9th Standard English Textbooks Part 1-1Athulya ThondangattilAinda não há avaliações
- John DrydenDocumento3 páginasJohn DrydenDunas SvetlanaAinda não há avaliações
- Been There, Done That, Wrote The Blog: The Choices and Challenges of Supporting Adolescents and Young Adults With CancerDocumento8 páginasBeen There, Done That, Wrote The Blog: The Choices and Challenges of Supporting Adolescents and Young Adults With CancerNanis DimmitrisAinda não há avaliações
- Introduction To EthicsDocumento18 páginasIntroduction To EthicsMarielle Guerra04Ainda não há avaliações
- VRPIN 01843 PsychiatricReportDrivers 1112 WEBDocumento2 páginasVRPIN 01843 PsychiatricReportDrivers 1112 WEBeverlord123Ainda não há avaliações
- UNIT 5-8 PrintingDocumento17 páginasUNIT 5-8 PrintingNOODAinda não há avaliações
- Total Physical Response (G4)Documento3 páginasTotal Physical Response (G4)Aq Nadzrul LarhAinda não há avaliações
- AMICO Bar Grating CatalogDocumento57 páginasAMICO Bar Grating CatalogAdnanAinda não há avaliações
- The Scope and Method of Economics: © 2007 Prentice Hall Business Publishing Principles of Economics 8e by Case and FairDocumento36 páginasThe Scope and Method of Economics: © 2007 Prentice Hall Business Publishing Principles of Economics 8e by Case and FairLangson phiriAinda não há avaliações
- CATaclysm Preview ReleaseDocumento52 páginasCATaclysm Preview ReleaseGhaderalAinda não há avaliações
- Hanwha Q Cells Data Sheet Qpeak L-g4.2 360-370 2017-10 Rev02 NaDocumento2 páginasHanwha Q Cells Data Sheet Qpeak L-g4.2 360-370 2017-10 Rev02 NazulfikarAinda não há avaliações
- Jul - Dec 09Documento8 páginasJul - Dec 09dmaizulAinda não há avaliações
- 25 Middlegame Concepts Every Chess Player Must KnowDocumento2 páginas25 Middlegame Concepts Every Chess Player Must KnowKasparicoAinda não há avaliações
- Universitas Tidar: Fakultas Keguruan Dan Ilmu PendidikanDocumento7 páginasUniversitas Tidar: Fakultas Keguruan Dan Ilmu PendidikanTheresia Calcutaa WilAinda não há avaliações
- Manuel SYL233 700 EDocumento2 páginasManuel SYL233 700 ESiddiqui SarfarazAinda não há avaliações
- Gis Data Creation in Bih: Digital Topographic Maps For Bosnia and HerzegovinaDocumento9 páginasGis Data Creation in Bih: Digital Topographic Maps For Bosnia and HerzegovinaGrantAinda não há avaliações
- KDE11SSDocumento2 páginasKDE11SSluisgomezpasion1Ainda não há avaliações
- Session 1Documento18 páginasSession 1Akash GuptaAinda não há avaliações
- XII CS Material Chap7 2012 13Documento21 páginasXII CS Material Chap7 2012 13Ashis PradhanAinda não há avaliações
- 0012 Mergers and Acquisitions Current Scenario andDocumento20 páginas0012 Mergers and Acquisitions Current Scenario andJuke LastAinda não há avaliações
- The Chemistry of The Colorful FireDocumento9 páginasThe Chemistry of The Colorful FireHazel Dela CruzAinda não há avaliações