Escolar Documentos
Profissional Documentos
Cultura Documentos
Jan Case Study
Enviado por
api-212894050Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Jan Case Study
Enviado por
api-212894050Direitos autorais:
Formatos disponíveis
1
Megan Whitley January Case Study January 25, 2013 Clinical Practicum I Medical Dosimetry Treatment for Infiltrating Ductal Carcinoma with 4-field Tangentials History of Present Illness: Patient LS is a 48 year old female of Caucasian ethnicity. She has been diagnosed with an Infiltrating Ductal Carcinoma (IDC). In 2011 LS went for her yearly mammogram and an area of concern was seen. In response to this, her doctor of obstetrics and gynecology (OBGYN) had a digital picture taken, per LS, and no concerns were revealed. The following year, in 2012, LS went in for her mammogram, and the area had changed. Upon mammogram, although her breast tissue is naturally dense, a nodule was visualized which required a subsequent ultrasound (US). After US, the patient was scheduled for a biopsy which was her worst experience throughout this whole thing. The experience was bad, not due to the biopsy results of grade 2 IDC, but because the doctor had no bed side manner, frightened her with the news, and sent her home from the biopsy without any care instructions, information, or plans for further communication. The carcinoma was found to be progesterone and Human Estrogen Receptor (HER2) positive. At this point, LS sought assistance from friends and family and changed doctors. The patient then had magnetic resonance imaging (MRI) scheduled by her new surgeon. The MRI revealed a single focus uptake in the upper inner quadrant of the left breast. A lumpectomy and a sentinel lymph node biopsy were then performed confirming a 9 millimeter (mm) grade 2 infiltrating ductal carcinoma. There was evidence of extensive intraductal component, but no evidence of angiolymphatic space invasion. This means that there was no blood and lymph channel involvement. Three lymph nodes were submitted for testing and all were negative for invasion. The margins around the lumpectomy site were initially concerning, but proved to be negative at 5 millimeters (mm) from ductal carcinoma in situ. A MammaPrint was done at the time of lumpectomy and revealed low risk, represented by a low MammaPrint score. MammaPrint is the first cancer recurrent assay that provides early-stage breast cancer patients with a test to establish the risk of distant recurrence following surgery.1 The surgeon then referred LS to a radiation oncologist where she and I met.
Past Medical History: Malignant melanoma treated with excision alone in 2003. Past Surgical History: Melanoma surgery in 2003, and breast biopsy and lumpectomy December 2012. Social History: LS is a stay at home mom. She is married and has 3 children. She is a nonsmoker and a nondrinker. Medications: Vitamin D, multivitamin, calcium, magnesium, and cod liver oil. Family History: Father had prostate cancer at age 70. Gynecological History: The patient is gravida 4, para 3, premenopausal female. She began menstruating at the age of 13. She did suffer 1 miscarriage. She was on oral contraceptives for 3 years. Radiation Oncologists Recommendations: The radiation oncologist recommended LS for adjuvant radiation therapy following breast conservation surgery. Three different treatment regimens were discussed. The first was whole breast irradiation with a boost either in standard fractionation or hypofractionation. Also discussed was the potential for a trial/protocol study. The RTOG 1005 randomizes patients between sequential and concurrent boosts, and LS would be eligible due to her age of less than 50 years. The last option was brachytherapy. In this case a SAVI (strut adjusted volume implant), that utilizes multiple catheters within the lumpectomy cavity, would be placed for customized volumetric irradiation.2 The SAVI is a partial breast
treatment mechanism meant as part of breast conservation therapy. Side effects of radiation for all of these options were discussed. The patient and radiation oncologist came to the conclusion that due to an upcoming vacation to Hawaii, the medical oncology consult required to be on protocol, would delay treatment too far. Furthermore, after a computed tomography (CT) scan was performed to evaluate her tumor site, it was determined that her cavity was not viable for SAVI placement. Thus, a prescription was written for 4256 centigray (cGy) to be delivered 266cGy/day for 16 fractions. After this original dose a boost plan will be developed that will take the overall dose to 5256 cGy, rendering the boost prescription at 1000 cGy to be delivered 250 cGy/day for 4 fractions. The patient will meet with medical oncology after returning from vacation for follow-up adjuvant therapy. Patient Setup/Immobilization: The therapist retrieved the patient from the dressing room and escorted them to the CT scanner, a GE LightSpeed. Before the complex simulation, the procedure was explained extensively to LS and the consent was signed. A timeout was taken
prior to the beginning of the simulation to verify the patients name, that she knew why she was having a scan, and to verify the breast to be treated. Photos were also taken to be uploaded into the patients electronic chart. The patient was placed on the breast board (see Figure 1). The breast board was placed on the table top with the wingboard, a Vac-Lok, and B headrest on the wingboard (see Figure 2). The patient was placed supine with knee wedge for her knees, both arms extended above her head and holding handles in the B1 position. The radiation oncologist came in to mark the extent of the breast tissue (superior, inferior, medial, lateral), lumpectomy scar marker, and a nipple marker. Then the laser origin was marked with 3 bbs. The scan then began in 2.5 millimeter (mm) slices totaling 121 images. After the scan was complete, the radiation oncologist came in and set the isocenter, the table was shifted, and the treatment isocenter was marked on the patient. The images were then transferred to the picture archiving and communication system (PACS) software and then on to the Eclipse treatment planning software (TPS). Contouring: After the patient was pulled in to Eclipse for planning, contouring was done of both the lungs separately, and then a structure that combines them, as well as the heart, the body, the scar and all of the field delineating wires, and the thyroid gland. The radiation oncologist was then called to contour the clinical target volume (CTV), which is the cavity, or balloon, and the clips remaining post operatively to designate the extent of the tumor cavity. Treatment Planning: After the beams were added. The plan began with two tangential beams, a left medial tangent, and a left lateral tangent. The energy was set to 6 megavoltage (MV) until an initial calculation was performed and the CTV was not fully covered. Then two more 18MV beams were added to push the dose deeper into the tissue. To make a decision between these energies, the penetrability of each energy must be considered. 18MV gives depth to the treatment, while 6MV delivers treatment more superficially. To determine whether to use 6MV or 18MV, the separation is taken between the medial and lateral breast tissue borders. If the separation is 18-21 centimeters (cm) use 6MV, but if it is over 25 cm, use 18MV. But if you are treating inflammatory disease within the breast, is important to remember to keep the skin dose relatively high to avoid recurrence. Dose tolerance to the skin is around 27 Gy dosing at 180cGy/day, so as long as its kept below this level, the dose is considered radiobiologically effective. Next the weighting is determined. This plan kept the weight much lighter on the 18MV beams because the tumor bed was relatively shallow, causing a need for more 6MV.
Distribution of the weight always totals 1.0. In this plan, the 6MV beams were evenly weighted at .45 each. By adding the weight of the medial 18MV beam of .06 and the lateral beam of .04, the total reaches 1.0. Then, electronic compensators (ECs) were applied to the 6MV beams. When using ECs you have the ability to edit the fluence or the dose cloud. Once the changes are made, the EC is expected to determine how to move the MLCs (multi-leaf collimators) to create the chosen fluence. MLCs influence these doses by choreographed movements that increase or decrease the transmission to the CTV. EC are never used with 18MV energy because of the neutron production created. After the plan has the V20 per lung less than 20%, and the heart maximum dose at 22Gy, the dosimetrist works with the plan until the hot spot is decreased as far a possible without effect the coverage to the CTV. The radiation oncologist approved the plan once this was achieved, the approved plan was sent to Mosaiq, a quality assurance (QA) plan was developed, digitally reconstructed radiographs were provided for the first day of treatment, and a backup calculation was performed in RadCalc (see Figure 4). Physics: Once the plan was approved and ready for treatment, the final step was to run a trial fraction to make sure that the information accurately transferred to the record and verify software, and that the plan would behave in the manner in which it was meant. A QA plan was created by the physicist to run on the Delta4. The fluence that registered within the Delta4 was compared to the approved treatment plan fluence. The Delta4 functions from a gamma analysis. The absolute dose evaluation and gamma analysis of the fluence were performed and compared to the measured dose delivered against the calculated phantom plan. For the plan to pass QA, 95% of all the points tested within the phantom must have a 3% more or less deviation from the predetermined dose. This plan passed QA. Conclusion/Impact: I enjoyed this case study. LS was a great first case study because she was very communicative, and a great insight to the patient perspective. When I initially met this patient, she had recently been through a negative experience with a doctor and their practice. Her fear was plain to see and her trust was difficult to gain. But, through this experience, I learned to enjoy my work environment from the patients perspective, as well as my new employee perspective. Together, we were able to learn both what the center had to offer, and the clinic surroundings. Furthermore, in the beginning, I thought that this plan was going to be less attractive due to its simple nature. Fortunately, since it was a simple setup, yet a complex
treatment plan, I was able to learn how to use ECs, MLCs, and the Delta4. I was also introduced to the work flow of the clinic. It helped me to better learn my new atmosphere, and it introduced me to other professionals involved in the patients daily care. This case also introduced me to the nuances in day-to-day dosimetry planning, that I can undertake immediately and help out within the department (i.e. importing and exporting, entering patient information into Mosaiq, and assisting with proper documentation).
Figures:
1. This is the CT scanner with the breast board, the wing board, the B head rest, and the knee wedge, being prepared for the patients daily setup.
2. The VacLok has been added and conformed to the patients body to provide a reproducible daily setup. Also, the laser are visible, and available to mark the patient.
3. This is a copy of the patients beam data a details for all 4 of her fields.
4. This is the print out from the backup calculation software, RadCalc, verifying that the calculations fall within a 3% tolerance of their originally calculated dose.
5. This is an en face view of the dose cloud with the skin turned on.
10
6. This is a visual representation of the fields showing both the ECs and the dose.
10
11
7. This is the dose volume histogram (DVH) that represents the dose received by both the CTV and the organs at risk (OARs).
11
12
8. This is the dose represented in color wash. In this view you can clearly visualize the depth provided by the 18X beams, as well as the dose contributed to the skin from the 6X beams.
12
13
References:
1. Agendia. MammaPrint Provides Individualized Metastasis Risk Assessment for Your Breast Cancer Patients. Agendia website. http://www.agendia.com/pages/mammaprint/21.php 2011. Accessed January 25, 2013. 2. Cianna Medical. Less Toxicity. More Patients. Now That's SAVI. http://www.ciannamedical.com/ 2012. Accessed January 25, 2012.
13
Você também pode gostar
- Megan Whitley Resume Nov 2017Documento4 páginasMegan Whitley Resume Nov 2017api-212894050Ainda não há avaliações
- Budget ActivityDocumento2 páginasBudget Activityapi-247490129Ainda não há avaliações
- New Patient Flow ChartDocumento1 páginaNew Patient Flow Chartapi-212894050Ainda não há avaliações
- Master Comp ListDocumento1 páginaMaster Comp Listapi-212894050Ainda não há avaliações
- March Case StudyDocumento13 páginasMarch Case Studyapi-212894050Ainda não há avaliações
- Megan FinalDocumento20 páginasMegan Finalapi-212894050Ainda não há avaliações
- Megan FinalDocumento20 páginasMegan Finalapi-212894050Ainda não há avaliações
- Fall EvalsDocumento6 páginasFall Evalsapi-212894050Ainda não há avaliações
- Fall EvalsDocumento6 páginasFall Evalsapi-212894050Ainda não há avaliações
- Fall EvalsDocumento6 páginasFall Evalsapi-212894050Ainda não há avaliações
- Conference Report For MeganDocumento5 páginasConference Report For Meganapi-212894050Ainda não há avaliações
- Professional VolunteeringDocumento3 páginasProfessional Volunteeringapi-212894050Ainda não há avaliações
- September Case StudyDocumento10 páginasSeptember Case Studyapi-212894050Ainda não há avaliações
- Extra Credit Problems Submit Upto 20 QuesDocumento7 páginasExtra Credit Problems Submit Upto 20 Quesapi-174496267Ainda não há avaliações
- Feb Case StudyDocumento12 páginasFeb Case Studyapi-212894050Ainda não há avaliações
- Ama Challenge 2012Documento3 páginasAma Challenge 2012api-174496267Ainda não há avaliações
- Master Comp ListDocumento1 páginaMaster Comp Listapi-212894050Ainda não há avaliações
- Dos 425 Planning Practice Problems 2011Documento3 páginasDos 425 Planning Practice Problems 2011api-213108684Ainda não há avaliações
- RedgroupwikiassignmentsDocumento2 páginasRedgroupwikiassignmentsapi-212894050Ainda não há avaliações
- Composite Case StudyDocumento27 páginasComposite Case Studyapi-212894050Ainda não há avaliações
- October Case StudyDocumento8 páginasOctober Case Studyapi-212894050Ainda não há avaliações
- Practice ProblemsDocumento7 páginasPractice Problemsapi-174496267Ainda não há avaliações
- July Case StudyDocumento13 páginasJuly Case Studyapi-212894050Ainda não há avaliações
- Summary of The Guest LectureDocumento1 páginaSummary of The Guest Lectureapi-212894050Ainda não há avaliações
- June Case StudyDocumento12 páginasJune Case Studyapi-212894050Ainda não há avaliações
- Interview of MoeDocumento4 páginasInterview of Moeapi-212894050Ainda não há avaliações
- May Ec Case StudyDocumento11 páginasMay Ec Case Studyapi-212894050Ainda não há avaliações
- Research Article 1 1Documento10 páginasResearch Article 1 1api-212894050Ainda não há avaliações
- Certificate of CompletionDocumento1 páginaCertificate of Completionapi-212894050Ainda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- TB Microscopy Handbook - FinalDocumento88 páginasTB Microscopy Handbook - FinalMigori Art100% (1)
- Vaccine Card - 20231120 - 175739 - 0000Documento2 páginasVaccine Card - 20231120 - 175739 - 0000MarilynAinda não há avaliações
- Extended and Expanded Roles of Nurses 4Documento1 páginaExtended and Expanded Roles of Nurses 4Sivaprasad SAinda não há avaliações
- Bertino2022 Book ClinicalEthicsForConsultationPDocumento181 páginasBertino2022 Book ClinicalEthicsForConsultationPJonatán Pérez RochaAinda não há avaliações
- Mycoplasma MBBS lectureDocumento19 páginasMycoplasma MBBS lectureSajjal Ali50% (2)
- Pioglitazone Hydrochloride Monograph For Professionals - DrugsDocumento13 páginasPioglitazone Hydrochloride Monograph For Professionals - DrugssilvanaanggraeniAinda não há avaliações
- Efektifitas Latihan Progressive Muscle Relaxation (PMR) Terhadap Mual Muntah Kemoterapi Pasien Kanker OvariumDocumento8 páginasEfektifitas Latihan Progressive Muscle Relaxation (PMR) Terhadap Mual Muntah Kemoterapi Pasien Kanker OvariumMutmin AnsariAinda não há avaliações
- Spotters 1Documento10 páginasSpotters 1elavarkuzhali2019Ainda não há avaliações
- CHD Indian GuidelinesDocumento15 páginasCHD Indian GuidelinesDhiraj Kr GauravAinda não há avaliações
- Drug Profile: ChlorpheniramineDocumento16 páginasDrug Profile: ChlorpheniramineMuhammad Ali RizviAinda não há avaliações
- ProP - Differentiating Nuclear Sclerosis From CataractsDocumento6 páginasProP - Differentiating Nuclear Sclerosis From CataractsDita TaepangAinda não há avaliações
- Diploma in DiabetologyDocumento8 páginasDiploma in Diabetologydawood260Ainda não há avaliações
- Missouri Counties Sue Drug Companies Over Opioid CrisisDocumento274 páginasMissouri Counties Sue Drug Companies Over Opioid CrisisSam ClancyAinda não há avaliações
- Natural Perineal Tears vs EpisiotomyDocumento9 páginasNatural Perineal Tears vs Episiotomydg_tajudinAinda não há avaliações
- PDF DIR 456Documento6 páginasPDF DIR 456Fauzan MaulanaAinda não há avaliações
- 018 Vs 022Documento3 páginas018 Vs 022kkorina5100% (2)
- Blood Culture Manual MT - SinaiDocumento41 páginasBlood Culture Manual MT - SinaiAvi Verma100% (1)
- Acne or Rosacea Infographic PDFDocumento1 páginaAcne or Rosacea Infographic PDFHegde sharma100% (1)
- Patient Discharge SummaryDocumento1 páginaPatient Discharge SummaryampalAinda não há avaliações
- IPCR Form - Mos'Documento2 páginasIPCR Form - Mos'Jay-Ann AlcideraAinda não há avaliações
- CIPD FactsDocumento2 páginasCIPD FactsStephen BowlesAinda não há avaliações
- Kdigo 2013. CKDDocumento110 páginasKdigo 2013. CKDcvsmed100% (1)
- POC CHWO HW Solutions PDFDocumento5 páginasPOC CHWO HW Solutions PDFakashkr619Ainda não há avaliações
- Angie ResumeDocumento2 páginasAngie Resumeapi-270344093Ainda não há avaliações
- Major Incidents and Mass Casualty EventsDocumento99 páginasMajor Incidents and Mass Casualty EventsJose Damian Cortes FernandezAinda não há avaliações
- Chemotherapy Extravasation: Establishing A National Benchmark For Incidence Among Cancer CentersDocumento9 páginasChemotherapy Extravasation: Establishing A National Benchmark For Incidence Among Cancer CentersRiri AmalinaAinda não há avaliações
- SilosDocumento3 páginasSilosapi-548205221100% (1)
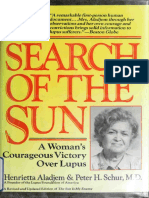
- Aladjem - The Sun Is My Enemy - in Search of The Sun - A Woman's Courageou - Aladjem, Henrietta, 1917 (Orthomolecular Medicine)Documento310 páginasAladjem - The Sun Is My Enemy - in Search of The Sun - A Woman's Courageou - Aladjem, Henrietta, 1917 (Orthomolecular Medicine)Anonymous gwFqQcnaX100% (1)
- General Surgery (Must Know)Documento93 páginasGeneral Surgery (Must Know)Binit BharatiAinda não há avaliações
- Cytokine StormDocumento1 páginaCytokine StormLAinda não há avaliações