Escolar Documentos
Profissional Documentos
Cultura Documentos
Newborn Assessment
Enviado por
api-232728488Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Newborn Assessment
Enviado por
api-232728488Direitos autorais:
Formatos disponíveis
Newborn Assessment
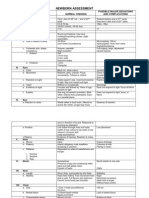
Newborn Physical Assessment Please use the following code:
Sara Staffen
+ = Present/normal
= Not present
NA = Not applicable
Admission data (This will be obtained from the babys chart!): Temp __36.6____ HR __140___ Resp __48___ Bld glucose __NA___ APGAR Score 1 min __8__ 5 min __9__ Resuscitation measures: _____NA______ ____________________________________________________________________ Ilotycin _11:45_ (time) Vit K __11:45___ (time) Nursed in L&D Y N
After you have read the infants chart and gathered the information, give your assessment of this infants status when it was 1 hour after birth (give details, not good)
Length __19 in___ Wt. ___8 lb 3 oz.___
- Vital signs stable; within normal parameters - Regular respiration rate and pattern, non-labored breathing - Heart sounds strong S1 & S2 audible - Pink color, consistent with race, clear skin - Capillary refill < 3 seconds - Even, round head, minimal caput and molding - Appears to be nursing well NOW YOU ARE READY TO DO A PHYSICAL ASSESSMEDNT ON THIS BABY (to be completed by you the day you are caring for the baby): Temp __36.7__ HR __130___ Resp __52___ Color: Pink ___+___ Pale ______ Mottles ______ Plethoric ______ Jaundice ______ Stained ______ Acrocyanosis ______ Skin: Clear ___+___ Pressure marks ______ Abrasions ______ Dry ______ Ecchymosis ______ Petechiae ______ Nevi ______ Milia ______ Rash ______ Lanugo ______ Vernix ___+___ Mongolian spots ______ Respirations: Regular __+___ Grunting ______ Abdominal ______ Retracting ______ Shallow ______ Nasal flaring ______ Sighing ______ Other ______ Cry: Lusty ___+__ Weak ______ Shrill ______ Head: Symmerty/shape __round, even_ Molding ______ Cephalhematoma _____
Caput succedaneum ___+_minimal___ ISE mark _____ Other ______ Anterior fontanel: Flat __+___ Full ______ Depressed ______ Posterior fontanel: Flat __+___ Full ______ Depressed ______ Sutures Coronal Sagittal Lambdoidal Overriding ________ ________ ________ Separated ________ ________ ________ Approximated _____+_____ _____+_____ _____+_____
Ears: (describe exact location & how you determined if it was normal) Position: Normal __+___ Abnormal ______ Describe normal position _ between the eyes and mouth._____ Skin tags _____ Nose: Symmetry ___+___ Flaring _____ Patent: Left __+__ Right __+__ Eyes: (describe what you found) Right Subconjunctive hemorrhage Nevi on lids Edema Red reflex Other ____ ____ ____ _NA_ _NA_ Left ____ ____ ____ _NA_ _NA_ evenly spaced
Mouth: Mucous membranes: Pink ___+__ Pale ______ Cyanotic ______ Teeth _____ Epsteins pearls _____ Hard palate: Intact ___+___ Abnormal ______________________________ Soft palate: Intact ____+__ Abnormal ______________________________ Lips: Cleft _____ Drooping _____ Symmetry __+___ Anterior chest: Symmetrical __+___ Shape _round_ Clavicles: Intact __+___ Fracture ____________________________ Breasts: Palpable tissue __+____ Engorgement ______ Heart sound: RRR ___+_____ Other ________
Genitals: Female: Labia majora: Completely covers minora __+__ Partially covers minora _____ Labia minora protruding _____ Vaginal discharge _____ Hymenal tag ____ Posterior: Pilonidal dimple ____ Truft of hair _____ Spinal column: Symmetry ___+___ Intact __+___ Anal patency: Y N Stool Y N Type __NA__
Anterior Abd: Symmetry ___+___ Other _NA___ Cord: # of vessels ___3___ Protruding base _____ Extremities: Right Symmetry Movement Digits (number) Flexion creases Palmar creases Sole creases Hips: Intact Right Left __+ __+ Dislocated/subluxation __ __ __+ __+ __5___ __+ __+ __+ Left __+ __+ __5___ __+ __+ __+ (10 fingers and toes)
Neuro-muscular: Tone: Normal ____+
Lethargic ______ Rigid ______ Tremors ______
What is your overall assessment and prognosis for this infant (do not say good): - Overall all assessment is positive; the newborns Apgar scores were eight and nine. Newborn reflexes present, strong heart and lung sounds with regular rate and rhythms, positive bowel sounds, creases on palms and soles. Newborn is tolerating breast feeding well. - Prognosis: the infant is healthy and should be able to go home with parents two days after delivery.
Reflexes: Reflex: Describe what you observed Rooting: __+
The rooting reflex helps to ensure successful breastfeeding. Lightly touch the corner of the newborns mouth or cheek. Normal newborn babies automatically turn their face toward the stimulus and make sucking (rooting) motions with the mouth when the cheek or lip is touched. Describe the procedures Describe normal responses
Sucking: __+
Touch the roof of the newborn's mouth and they will begin to suck.
Sucking response on finger.
Moro: __+__
Witnessed spontaneously when the newborn was startled by a loud sound or possibly by her own crying.
The infant will have a startled look and the arms will fling out sideways with the palms up and the thumbs flexed.
Stepping: did not assess
NA
Newborn appears to take steps or dance when held upright with his/her feet touching a solid surface.
Grasp/hand: __+__
Stroke newborns hand or just place your finger in their hand.
Stroking the palm of a newborn's hand causes them to close their fingers in a grasp. The newborns toes flex, or curl under and grasp
Grasp/foot: __+__
Stoke up the middle of the newborns foot.
On the basis of your assessment, list at least TWO nursing diagnosis for this baby and all the teaching interventions you would use for each nursing diagnosis. Please include the rationale for your actions. You must have at least two references besides your textbooks for your rationales. Be sure your assessment and interventions correspond to your Nursing Diagnosis.
Nursing Diagnosis
Necessary Assessments/Interventions
Assess: signs of infections, elevated body temperature, listlessness, difficulty feeding, and irritability. 1. Monitor neonates condition, including vital signs.
Rationale
High risk for infection r/t maternal factors & immune system deficiency
Effective Breastfeeding
Mother tested GBS positive, antibiotics were administered during labor. Mother is not vaccinated against any communicable diseases including Pertussis. Infant was vaccinated against Hep B after delivery. A fever tends to be more clinically relevant in neonates and 2. Provide education to the parents regarding infants younger than three months, because they are observation for signs of infection. immunologically immature and incompletely vaccinated. Including any fever in infants less than (Snyder, Kivlehan, & Collopy, 2011) Studies have shown that three months. infants younger than three months lack innate immunity 3. Ensure that all equipment used for infant therefore are at an increased risk for serious bacterial is sterile, scrupulously clean. infection, bacteremia and occult bacteremia, making the 4. Administer prophylactic antibiotics and/or parental recognition of fever and follow-up actions to seek vaccinations as per Doctors order. medical attention extremely important. (Snyder, Kivlehan, & Collopy, 2011) Assess mothers knowledge and Breastfeeding not only provides essential nutrition, it is also experience with breastfeeding and an important mechanism in the formation of the newborns infants ability to latch on to breast emotional development and building a trusting relationship through correct positioning and assess between the newborn and the mother. (Kailaiselv, 2011). presence of rooting reflex. According to Kailaiselv (2011), breastfeeding has many 1. Monitor infants height and weight to properties that benefit both the mother and newborn. ensure standards of development and Breastfeeding releases Oxytocin which aids in uterine
growth are being met.
2. Educate mother and support person
3.
4.
Ineffective thermoregulation r/t immature compensation for changes in environmental 1. temperature. AEB postpartum axillary temperature of 36.3 C. 2. 3. 4.
about breastfeeding techniques to encourage the success of breastfeeding. Teach mother how to break suction to avoid chaffed nipples and other interventions that decrease engorgement and tenderness. Ensure that infant is nursing every 2-3 hours, stooling 1-6 times and wetting 6-8 diapers daily. Assess temperature frequently, initial rectally, repeating axillary temperature every 15 minutes during rewarming. Desired outcome: axillary temperature within 36.5-37.3 C. Place neonate in radiant heat warmer or skin-to-skin contact with mother. Place hat on neonates head. Utilize heat lamps during any procedures. Ensure neonates clothing and bed linens are dry and warm.
involution, it also encourages strong mother-newborn bonding through skin-to-skin contact and its cost effective. For the newborn, breast milk provides immunologic properties, meets nutritional needs, promotes neurological development, and is easily digested with less allergenic properties.
During a postpartum assessment, the neonates axillary temperature was repeated twice with results of 36.3 C both times. A final rectal temperature reading was 36.4 C; therefore rewarming interventions were performed. Adaptation of the neurological system to extrauterine life may be inadequate, despite being a full-term infant. Hypothermia predisposes infant to cold stress, utilization of nonrenewable brown fat stores, and reduced sensitivity to increased levels of carbon dioxide, hypercapnia, or decreased oxygen levels, hypoxia. (Nurse Care Plan, 2012). Therefore it is important to monitor the neonate for presence of tachypnea or apnea, generalized cyanosis, bradycardia, poor cry, and lethargy. These signs indicate cold stress leading to increased oxygen consumption and possible acidosis. Rewarming the infant too rapidly has been associated with apneic states as well. (Nurse Care Plan, 2012).
References: Kalaiselv, K. (2011). Leifer: Newborn Feeding. Retrieved from http://elsevieradvantage.com/samplechapters/9780323083478/11[1].pdf Ladwig, G.B., & Ackley, B.J. (2011). Mosbys Guide to Nursing Diagnosis. Maryland Heights, MO: Mosby Inc. & Elsevier Inc. Nurse Care Plan. (2012). Ineffective Thermoregulation: Nursing Diagnosis Infant. Retrieved from http://www.nurse-careplan.com/2012/06/ineffective-thermoregulationnursing.html Snyder, S. R., Kivlehan, S., & Collopy, K. (2011). Fever in the Neonate and Young Infant. EMS World, 40(6), 57-61.
Você também pode gostar
- NEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideNo EverandNEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideAinda não há avaliações
- LOW RISK NEONATAL NURSING: Passbooks Study GuideNo EverandLOW RISK NEONATAL NURSING: Passbooks Study GuideAinda não há avaliações
- Maternity Care Plan - Template 1 - 21 - 09Documento9 páginasMaternity Care Plan - Template 1 - 21 - 09Steven BerschaminskiAinda não há avaliações
- Newborn Assessment ToolDocumento5 páginasNewborn Assessment ToolReana AbillarAinda não há avaliações
- Assessment of NeonateDocumento11 páginasAssessment of NeonateAbhishek GirdharAinda não há avaliações
- Newborn AssessmentDocumento3 páginasNewborn AssessmentValerie Ybañez Peñalber100% (2)
- New Born CareDocumento22 páginasNew Born Caredexter100% (8)
- Assessment of The Normal NewbornDocumento6 páginasAssessment of The Normal Newborndhalal100% (2)
- Initial Newborn AssessmentDocumento14 páginasInitial Newborn Assessmentaclark831Ainda não há avaliações
- Newborn Assessment ChecklistDocumento57 páginasNewborn Assessment Checklistmuiz muhammadAinda não há avaliações
- Essential Newborn Care GuideDocumento120 páginasEssential Newborn Care Guidejuly3ciaAinda não há avaliações
- Assessment of NewbornDocumento33 páginasAssessment of Newbornmehta shivaniAinda não há avaliações
- 01 - Newborn Physical ExamDocumento2 páginas01 - Newborn Physical Examgerald_valeriano0% (1)
- Electronic Fetal MonitoringDocumento4 páginasElectronic Fetal MonitoringMauZungAinda não há avaliações
- Care of The NewbornDocumento5 páginasCare of The Newbornbuzz Q100% (2)
- 986 Assessment of New Born NursingDocumento91 páginas986 Assessment of New Born NursingkrishnaAinda não há avaliações
- Complete newborn exam guideDocumento123 páginasComplete newborn exam guideSarahAinda não há avaliações
- High Risk Newborn2Documento15 páginasHigh Risk Newborn2Catherine Villanueva Sta Monica100% (1)
- Ob Clinical Worksheet - IntrapartumDocumento8 páginasOb Clinical Worksheet - Intrapartumcandice lavigneAinda não há avaliações
- Principles of Postpartum Nursing CareDocumento2 páginasPrinciples of Postpartum Nursing CareZaire DylanAinda não há avaliações
- High Risk Newborn Conditions Present at BirthDocumento47 páginasHigh Risk Newborn Conditions Present at BirthChinchu ChinchuAinda não há avaliações
- Birth asphyxia causes and neonatal resuscitationDocumento20 páginasBirth asphyxia causes and neonatal resuscitationinne_fAinda não há avaliações
- New Born Care 1Documento12 páginasNew Born Care 1Tsuyoshi BangAinda não há avaliações
- Newborn exam checklist under 40 charsDocumento2 páginasNewborn exam checklist under 40 charsWajid Hussein0% (1)
- Newborn Assessment 2.16Documento16 páginasNewborn Assessment 2.16rrbischofbergerAinda não há avaliações
- Hypertension in Pregnancy Classification and ManagementDocumento44 páginasHypertension in Pregnancy Classification and ManagementIrfandy Chairi Sulaiman Lubis100% (1)
- Postpartum Care of NewbornDocumento8 páginasPostpartum Care of NewbornSara rose100% (1)
- Newborn CareDocumento282 páginasNewborn CarecikiricaAinda não há avaliações
- Newborn Assessment Head to ToeDocumento17 páginasNewborn Assessment Head to Toemarycris100% (2)
- Obstetric ExaminationDocumento26 páginasObstetric Examinationshofa nur rahmannisaAinda não há avaliações
- AntepartumDocumento32 páginasAntepartumphoenix180100% (1)
- Newborn AssessmentDocumento15 páginasNewborn Assessmentmarie97% (35)
- Newborn AssessmentDocumento24 páginasNewborn Assessmentvincentsharon100% (2)
- Kayla Flaskerud Vsim BP Concept Map, Isbar, ClincialDocumento12 páginasKayla Flaskerud Vsim BP Concept Map, Isbar, ClincialCameron Janzen100% (1)
- Newborn AssessmentDocumento7 páginasNewborn AssessmentMJ Amarillo100% (6)
- PrematurityDocumento37 páginasPrematuritySolomon AmosAinda não há avaliações
- Complications of LaborDocumento54 páginasComplications of Laborallie-jones-6489100% (2)
- Thermoregulation in NewbornDocumento14 páginasThermoregulation in NewbornSamsiah ChaAinda não há avaliações
- Immediate Newborn CareDocumento9 páginasImmediate Newborn CareLj FerolinoAinda não há avaliações
- Neonatal ResuscitationDocumento5 páginasNeonatal Resuscitationabdirahiim ahmedAinda não há avaliações
- Newborn AssessmentDocumento5 páginasNewborn Assessmentlanilyn aquinoAinda não há avaliações
- Admission of Neonates in Nicu & Nursing ManagementDocumento30 páginasAdmission of Neonates in Nicu & Nursing ManagementMonika shankarAinda não há avaliações
- Nursing Care Management - 107: de La Salle Lipa College of NursingDocumento3 páginasNursing Care Management - 107: de La Salle Lipa College of NursingThe Blue and Gold RvdAinda não há avaliações
- Basic Newborn Resuscitation ChecklistDocumento2 páginasBasic Newborn Resuscitation ChecklistMidhu50% (2)
- Newborn Assessment NORMALDocumento2 páginasNewborn Assessment NORMALVanessaMUellerAinda não há avaliações
- Maternal and Child Health Nursing Care of The NewbornDocumento5 páginasMaternal and Child Health Nursing Care of The NewbornJeanilynTanAinda não há avaliações
- Rubella and PregnancyDocumento6 páginasRubella and PregnancyKABERA RENEAinda não há avaliações
- Worksheet To Accompany FHR Review Video: Emerald Spangler May 6, 2021Documento3 páginasWorksheet To Accompany FHR Review Video: Emerald Spangler May 6, 2021Emerald SpanglerAinda não há avaliações
- Abnormal LaborDocumento20 páginasAbnormal Laborأ.م.د. إنعام فيصل محمدAinda não há avaliações
- Pediatric Drug AdministrationDocumento32 páginasPediatric Drug AdministrationNobleScarletAinda não há avaliações
- OB Care Plan: Assessment DataDocumento12 páginasOB Care Plan: Assessment Dataapi-520985654Ainda não há avaliações
- 11-Immediate Care of NewbornDocumento112 páginas11-Immediate Care of NewbornJiela CarbonillaAinda não há avaliações
- PARTOGRAMDocumento17 páginasPARTOGRAMKrutthivaasa PriyaAinda não há avaliações
- Postpartum Physiology, What's Normal: Starting at Her HeadDocumento26 páginasPostpartum Physiology, What's Normal: Starting at Her HeadyogurtAinda não há avaliações
- Common Diseases of NewbornDocumento162 páginasCommon Diseases of NewbornMichelle ThereseAinda não há avaliações
- Newborn AssessmentDocumento10 páginasNewborn Assessmentapi-508446364Ainda não há avaliações
- Care of The Normal Newborn: M. Rogers-Walker, MSN/Ed, RNDocumento28 páginasCare of The Normal Newborn: M. Rogers-Walker, MSN/Ed, RNyanetp01Ainda não há avaliações
- Pediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)No EverandPediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)Ainda não há avaliações
- NEONATAL NURSE PRACTITIONER: Passbooks Study GuideNo EverandNEONATAL NURSE PRACTITIONER: Passbooks Study GuideAinda não há avaliações
- Final ResumeDocumento2 páginasFinal Resumeapi-232728488Ainda não há avaliações
- Weebly Introductions 3Documento1 páginaWeebly Introductions 3api-232728488Ainda não há avaliações
- Sara Staffen - Research PosterDocumento1 páginaSara Staffen - Research Posterapi-232728488Ainda não há avaliações
- Weebly Introductions 6Documento1 páginaWeebly Introductions 6api-232728488Ainda não há avaliações
- Theory in PracticeDocumento5 páginasTheory in Practiceapi-232728488Ainda não há avaliações
- Sara Staffen - Cover LetterDocumento1 páginaSara Staffen - Cover Letterapi-232728488Ainda não há avaliações
- Reference Letter - ColleyDocumento1 páginaReference Letter - Colleyapi-232728488Ainda não há avaliações
- Weebly Introductions 2Documento1 páginaWeebly Introductions 2api-232728488Ainda não há avaliações
- Weebly Introductions 4Documento1 páginaWeebly Introductions 4api-232728488Ainda não há avaliações
- Proof of CompletionDocumento1 páginaProof of Completionapi-232728488Ainda não há avaliações
- 350 Scholarship Day PosterDocumento1 página350 Scholarship Day Posterapi-232728488Ainda não há avaliações
- Osp LeadershipDocumento9 páginasOsp Leadershipapi-232728488Ainda não há avaliações
- Review of Research PaperDocumento10 páginasReview of Research Paperapi-232728488Ainda não há avaliações
- Family AssessmentDocumento10 páginasFamily Assessmentapi-232728488Ainda não há avaliações
- Sara Staffen Service Learning Journals 1-5Documento10 páginasSara Staffen Service Learning Journals 1-5api-232728488Ainda não há avaliações
- Health Nutrition Throughout PregnancyDocumento4 páginasHealth Nutrition Throughout Pregnancyapi-232728488Ainda não há avaliações
- Service Learning ProposalDocumento8 páginasService Learning Proposalapi-232728488Ainda não há avaliações
- Bfitgrouppresentation Sexualhealth 1Documento21 páginasBfitgrouppresentation Sexualhealth 1api-232728488Ainda não há avaliações
- Winshield SurveryDocumento8 páginasWinshield Surveryapi-232728488Ainda não há avaliações
- Smoking During Pregnancy FinalDocumento14 páginasSmoking During Pregnancy Finalapi-232728488Ainda não há avaliações
- Ebp Orthostatic Vital Signs Quality Patient CareDocumento7 páginasEbp Orthostatic Vital Signs Quality Patient Careapi-232728488Ainda não há avaliações
- FSRH Ukmec Summary September 2019Documento11 páginasFSRH Ukmec Summary September 2019Kiran JayaprakashAinda não há avaliações
- Controle de Abastecimento e ManutençãoDocumento409 páginasControle de Abastecimento e ManutençãoHAROLDO LAGE VIEIRAAinda não há avaliações
- Pradhan Mantri Gramin Digital Saksharta Abhiyan (PMGDISHA) Digital Literacy Programme For Rural CitizensDocumento2 páginasPradhan Mantri Gramin Digital Saksharta Abhiyan (PMGDISHA) Digital Literacy Programme For Rural Citizenssairam namakkalAinda não há avaliações
- Report Emerging TechnologiesDocumento97 páginasReport Emerging Technologiesa10b11Ainda não há avaliações
- 15 - 5 - IoT Based Smart HomeDocumento6 páginas15 - 5 - IoT Based Smart HomeBhaskar Rao PAinda não há avaliações
- Maverick Brochure SMLDocumento16 páginasMaverick Brochure SMLmalaoui44Ainda não há avaliações
- C6 RS6 Engine Wiring DiagramsDocumento30 páginasC6 RS6 Engine Wiring DiagramsArtur Arturowski100% (3)
- Phys101 CS Mid Sem 16 - 17Documento1 páginaPhys101 CS Mid Sem 16 - 17Nicole EchezonaAinda não há avaliações
- 8dd8 P2 Program Food MFG Final PublicDocumento19 páginas8dd8 P2 Program Food MFG Final PublicNemanja RadonjicAinda não há avaliações
- Web Api PDFDocumento164 páginasWeb Api PDFnazishAinda não há avaliações
- UAPPDocumento91 páginasUAPPMassimiliano de StellaAinda não há avaliações
- Accomplishment Report 2021-2022Documento45 páginasAccomplishment Report 2021-2022Emmanuel Ivan GarganeraAinda não há avaliações
- Service and Maintenance Manual: Models 600A 600AJDocumento342 páginasService and Maintenance Manual: Models 600A 600AJHari Hara SuthanAinda não há avaliações
- Why Genentech Is 1Documento7 páginasWhy Genentech Is 1panmongolsAinda não há avaliações
- S5-42 DatasheetDocumento2 páginasS5-42 Datasheetchillin_in_bots100% (1)
- Motor Master 20000 SeriesDocumento56 páginasMotor Master 20000 SeriesArnulfo Lavares100% (1)
- Evaluating Sources IB Style: Social 20ib Opvl NotesDocumento7 páginasEvaluating Sources IB Style: Social 20ib Opvl NotesRobert ZhangAinda não há avaliações
- Exp 8 - GPG - D12B - 74 PDFDocumento4 páginasExp 8 - GPG - D12B - 74 PDFPRATIKSHA WADIBHASMEAinda não há avaliações
- Skuld List of CorrespondentDocumento351 páginasSkuld List of CorrespondentKASHANAinda não há avaliações
- Sentinel 2 Products Specification DocumentDocumento510 páginasSentinel 2 Products Specification DocumentSherly BhengeAinda não há avaliações
- Striedter - 2015 - Evolution of The Hippocampus in Reptiles and BirdsDocumento22 páginasStriedter - 2015 - Evolution of The Hippocampus in Reptiles and BirdsOsny SillasAinda não há avaliações
- Nursing Care Management of a Client with Multiple Medical ConditionsDocumento25 páginasNursing Care Management of a Client with Multiple Medical ConditionsDeannAinda não há avaliações
- Prof Ram Charan Awards Brochure2020 PDFDocumento5 páginasProf Ram Charan Awards Brochure2020 PDFSubindu HalderAinda não há avaliações
- Electronics Ecommerce Website: 1) Background/ Problem StatementDocumento7 páginasElectronics Ecommerce Website: 1) Background/ Problem StatementdesalegnAinda não há avaliações
- Account Statement From 30 Jul 2018 To 30 Jan 2019Documento8 páginasAccount Statement From 30 Jul 2018 To 30 Jan 2019Bojpuri OfficialAinda não há avaliações
- Manual Analizador Fluoruro HachDocumento92 páginasManual Analizador Fluoruro HachAitor de IsusiAinda não há avaliações
- Instrumentation Positioner PresentationDocumento43 páginasInstrumentation Positioner PresentationSangram Patnaik100% (1)
- Unit 1 TQM NotesDocumento26 páginasUnit 1 TQM NotesHarishAinda não há avaliações
- Sarvali On DigbalaDocumento14 páginasSarvali On DigbalapiyushAinda não há avaliações
- Biagioli Did Galileo Copy The TelescopeDocumento28 páginasBiagioli Did Galileo Copy The TelescopeGregory HooAinda não há avaliações