Escolar Documentos
Profissional Documentos
Cultura Documentos
Feasibility Study On Birthing Clinic
Enviado por
Kristine AgpalzaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Feasibility Study On Birthing Clinic
Enviado por
Kristine AgpalzaDireitos autorais:
Formatos disponíveis
1
INTRODUCTION
Our country today faces serious problem specifically on health sector and
giving birth at home is one of the problems that should be given importance by
the Philippine government since giving birth at home meets several complication
and untoward problems that will cause mortality.
According to the Department of Health, maternal mortality report, updated
in June 2010, hypertension complicated by pregnancy comprises 29 percent of
the causes of maternal deaths, and partum hemorrhage 15 percent - the second
and third leading causes of maternal death. Others are sepsis, obstructed labor
and complications around unsafe abortion and giving births at home - most of
which are preventable with proper diagnosis and intervention.
According to the National Demographic Health Survey (NDHS) of 2008,
only 44 percent of births in the Philippines occur in health facilities; 56 percent of
children are still delivered at home.
Under Philippine law, licensed midwives are authorized to carry out the
supervision and care of women during pregnancy, labor and management of
normal deliveries, including the administration of an oxytocin drug to prevent and
treat hemorrhage after the delivery of the placenta.
At present, Department of Health made a memorandum that there will no
more pregnant mother to deliver children at home due to unsafe and risk delivery.
Thus, as licensed midwives and proponents of this feasibility study aims to
establish a birthing center, to be named as Mother Choice Birthing Center to
establish a safe and sustainable birth center and increase woman with access to
healthcare provider and health care facility at lower cost and access to Philhealth
is available.
In addition, proponents are encourage to open a birthing center since not
all pregnant woman can access to hospital at the same time, hospital addresses
different cases of health problems while birthing center only focus on parturient
cases at the same time cheaper.
Objectives of the Study
Generally, this study will be of great help to achieve the vision of the
Mothers Choice Birthing Center, which is to be an effective partner in sustaining
and maintaining quality of care to our clients through excellent birthing center
service with full clients satisfaction.
Significance of the Study
To the Researchers
The result of this study will be very significant to the researcher. This is
because it can give them better idea about starting a business about birthing
center.
To the Client
The positive result of the study will provide them a birthing clinic with
utmost consideration on the safety and security of pregnant woman and newborn
babies.
To the School
The school administration will be proud of the brilliant researched studies
added to the College Library and Research Department for the useful reference
for future researchers.
To the Government
The government will surely support the study because of the situation of
health in our country today. If the study will be materialized it will be a big help to
the community in general.
THE FEASIBILITY STUDY
This chapter presents the four (4) components of a project feasibility
study, namely: management, marketing, technical and financial.
This project
feasibility study is prepared to ascertain if the project, as initially designed, will
have a chance in the niche market when implemented.
Management Feasibility
This aspect includes a study of the basic organization, form of business,
organizational chart and project operation schedules.
This aspect helps to
determine the effectiveness of the organization and the qualification of the
individuals which will make-up the organization of the business.
Form of Business
The business will be registered and recognized under the name: Mothers
Choice Birthing Center as universal-limited partnership and will be registered with
the Securities and Exchange Commission (SEC). A partnership duly formed
under the law is a juridical person separate and distinct from each of the partner.
The proponents are Registered Midwife (RM), to wit: Marites C. Bahian, Mary
Jane Beleno, Aubrey D. Nuez, Roselie A. Rodicol and Susan L. Suralta.
The form of the business is an association of two or more persons to carry
on as co-owners of a business for profit and as a result of a specific contractual
agreement among the owners or partners.
It is agreed that partners have
specified duties and responsibilities to the business activities (as presented in the
organizational chart). Other positions left require hiring of workers to work for the
company.
All partners finished from the two-year Diploma in Midwifery, passed the
Board of Midwifery Licensure Examination and will finish their degree in Bachelor
of Science in Midwifery. Thus, they have enough knowledge and skills to run the
business.
Organizational Structure
The proponents agreed that they will join force in managing their business
considering that the company has limited resources. However, once the birthing
center will expand, they will hire additional staff to assist the business operation.
Next page is the designed organizational structure outlining the position
involves.
Mothers Choice Birthing Center
ROSELIE C.
RODICOL
PRINCIPAL-
PEDIATRICIAN
ON-CALL
OBSTETRICIAN
ON-CALL
SONOLOGIST
ON-CALL
MARITES C.
BAHIAN
MIDWIFE
MARY JANE C.
BELENO
MIDWIFE
AUBREY D.
NUEZ
SUSAN L.
SURALTA
MIDWIFE
MIDWIFE
WACTHMAN
STUDENT
INTERN
Note: Additional staff will be hired once the business is already established.
Business Experiences and Qualifications of Proponents
The experiences, trainings and seminar attended by the proponents are
considered excellent factors in business success.
The course taken by the
proponents are in line with birthing management which will be a big factor in the
success of business.
Through their experience, the proponents believe that
these can give them that much needed self-confidence to enable them to carry
their individual task.
Table 1. Unit Management Personnel
Unit Management
Time to be
Personnel
devoted to the
project and duties
Principal Midwife
-12 hours
-Manages and
oversees the
operation of the
business
Pediatrician
on-call
-24 hour cover of
the clinic
-Manage the
immediate
newborn care
OB-Gyne
On-call
Consultant
-24 hour cover of
the clinic
-Manage the
maternal care
Ultrasound
Part-time
Sonologist
- 8 hours duty
- Ultrasound Incharge
Skilled Midwife
-12 hours
- responsible for
maternal and
immediate new
born care
Qualification
Compensation
- Masters Degree
holder, BSM, RM
-Competent
Personality
P 10,000.00
plus fringe
benefits
-License Pediatric
Medicine
Physician
-Competent
Personality
Php 500 per new
born
-License OB-Gyne
Medicine
Physician
-Competent
Personality
-License
Sonologist
Php 3,500 per
mother or 500 per
consultation
Licensed Midwife
Php8,000 per
month plus fringe
benefit
Php 200 per
ultrasound
Table 2. Labor Skills Requirement
Labor Skills
Number of
Required
Required Skilled
Labor
Watchman
1
Qualification
High School
Graduate
Basic Police
Training
Compensation
P 4,000.00 per
month plus fringe
benefit
Student Intern: Second year Midwifery SAIT student
Protocol:
*Observe
*Assist
*Research
*Experience
Support groups:
Womens League
SAIT -school
Shift rotations:
Staff are divided according to schedule (12 hours per duty)
Eight hours only for security and housekeeper
Recruitment Program
The recruitment will be simple. In case the clinic is under staff, the center
will hire on-call midwife to facilitate under staff while hiring is undertaking. Hiring
scheme will be post in the internet and applicants will submit their application,
bio-data
and
requirements
via
at
motherschoicebirthingcenter@yahoo.com. The applicants will undergo a written
and practical examination to gauge their mental capacity and know if they had
the skills to carry out the work. Once they will pass, the principal midwife will
conduct character reference of the person. Lastly, there will be a final interview
to choose the best applicant for the position.
Training Program
The goal of the training program in the company is to develop specific
skills, attitude and capacities to maximize the individuals job performance.
Virtually, every employee in the company will undergo some degree of training
programs, either formal or informal.
MDG trainings include: Partograph, IV
insertion, neonatal resuscitation, breastfeeding, basic life support, post partum
hemorrhage and immediate newborn care.
Fringe Benefits
Below are the fringe benefits offered by the company will be as follows:
-
Full coverage on SSS, Philhealth and Pag-IBIG
Annual vacation leave and sick leave for 15 days with pay
13th month bonus
Retirement Package
Commission
Facilities
The facilities of the birthing clinic based on Department of Health (DOH)
requirement will be the following:
Toilet and bathing facilities for mother and baby
24 hour supply of clean and hot water
10
Electricity supply (including emergency lighting)
24 hour refrigerator for storing medicines
Equipment in satisfactory condition
One patient bed per room for private type
Seven pt. in ward with curtain and dividers to provide patient privacy for
each room
Each room must have bright lighting
Oxygen tank and supply available in the delivery room, must be secured
to solid object
Adequate prevention from occupational hazards
No animals in the clinic
All windows and doors should be covered with a minimum in a net
covering
Sufficient ventilation
Absolutely no smoking on the premises with an obvious sign at front desk
11
Table 3. Pre-Operating Activities
Activities
Number of Weeks
Preparation of the Project Feasibility Study
4
Registration of the Business (SEC, DTI, Philhealth)
4
Business Permit
2
Construction of the Building
24
Purchase of the Equipment
4
Setting-up of the Equipment
4
Purchases of facilities and office supplies
4
Hiring of workers
2
Note: It is expected by the proponents that at the end of one year preparation,
the birthing center will fully operate after the completion of pre-operating
activities.
Table 4. Pre-operating Expenses
Activities
Preparation of the Project Feasibility Study
Registration of the Business (SEC, DTI, Philhealth)
Business Permit
Renovation of the Building
Purchase of the Equipment
Setting-up of the Equipment
Purchases of facilities and office supplies
Purchases of Medicine
Hiring of workers
Initial Total Amount Needed
Initial Amount Needed
P
5,000.00
2,500.00
5,000.00
480,000.00
21,620.00
4,000.00
3,000.00
1,690.00
1,000.00
P 523,810.00
12
MARKETING FEASIBILITY
This aspect is considered as the lifeblood of virtually projected feasibility
study for the extent of the data and information gathering because the
succeeding aspects depend largely on it.
This serves as the basis of the
financial section through projected demand. It includes the following information:
demand and supply gap analysis, marketing program and the projected number
of clients. The objective of this study is to determine the quantity of clients
needed to maintain the operation of the mothers choice birthing center.
Below is the presentation of Bukidnon map highlighting Maramag,
Bukidnon where proponents would like to serve South Poblacion where Camp 1
is located.
The said area has no available birthing center and far from the
hospitals and clinic in Poblacion, Maramag, Bukidnon.
In addition, Camp 1,
13
Maramag, Bukidnon is a cross section between Quezon and Don Carlos,
Bukidnon with a bigger population.
Table 5. Supply and Demand Gap Analysis
Area
Population
Pregnant
(2010)
Woman
Maramag
90,901
7,635
Quezon
94,584
7,945
Don Carlos
64,334
5,404
Source: NSO January 2013 Quickstat
Potential
Clients
3,054
3,178
2,161
Potential Clients
Share
275
286
194
Assumptions:
It is expected that 8.4% of the total female population gave birth in a year
It is expected that there will be 40% potential clients, since it is already
prohibited by DOH to deliver the baby at home.
With 40% potential clients to be served by birthing clinic, the proponents
will serve 9% only during the first year of its operation.
Major Clients
14
Catchment Area: Camp 1, Maramag Bukidnon and the nearby community
living 20 km in diameter, approximately. These will include the nearby barangays
of Don Carlos and Quezon, Bukidnon. In addition, clients served are those who
cannot afford to give birth in the hospitals and can only afford the birthing center
rates.
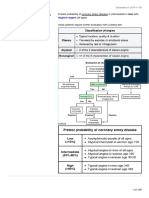
Criteria for Admission to Birthing Center (Based on Phil health Mandate)
Low risk pregnancies only
Age 19-45
Gestation 37-41 weeks
No significant co-morbidities
No previous caesarean sections
No current pregnancy complications
Have pre-natal during 1st trimester, 2nd trimester and twice in 3rd trimester
Has had all the necessary blood tests and investigations e.g. full blood
count, urea and electrolytes, and infection screening
With or without Phil health
Criteria for disqualification for admission in Birthing Center
15
(Based on Phil health Mandate)
*With high blood pressure
*With diabetes
*Malformation
*Multi-pregnancy
*With previous caesarean section
*With previous complication (below is the detailed list)
Table 6. Enumeration of Previous Complications
Previous
complications
Unexplained stillbirth/neonatal death or previous
death related to intrapartum difficulty
Previous baby with neonatal encephalopathy
Pre-eclampsia requiring preterm birth
Placental abruption with adverse outcome
Eclampsia
Uterine rupture
Primary postpartum hemorrhage requiring
additional treatment or blood transfusion
Retained placenta requiring manual removal in
theatre
Shoulder dystocia
History of previous baby more than 4.5 kg
Extensive vaginal, cervical, or third- or fourthdegree perineal trauma
Placenta previa
Abruptio placenta
16
Still birth
Quality of Service
The proponents will ensure that the proposed birthing center will provide
the best quality service. Price offered is affordable compared to hospitals. (note:
specific services are put into detail in the technical feasibility study section)
Terms of Payment
For Phil health patient, the clients full payment will be charged from their
Phil health Insurance.
For Non-Phil health patient, the clients may pay partial down payment
during admittance or full payment will be made before patient will be discharged.
Location of the Birthing Center
Mothers Choice Birthing Center will be located in Camp 1, Maramag,
Bukidnon.
Emergency Vehicle
24 hour availability of vehicle to allow prompt transfer to hospital in case of
complications or complex care.
Thus, collaboration is deemed necessary.
Collaboration for transfer, partner with nearby hospitals: BPH Maramag.
17
Moreover, the proponents will provide a 24/7 transportation facilities for
immediate response for those patient who would like to be picked-up.
Promotional or Advertising Scheme to be adopted
The promotional or advertising schemes to be adopted by the proponents
are the following: leafleting in the nearby Barangay for the information about the
mothers choice birthing center, referral fee of Php 500.00 per referral and radio
advertisement for the first month of operation.
Table 7. Promotional or Advertising Scheme to be adopted
Particulars
Leafleting
Radio Advertisement
Referral Fee per month
Total Amount
Amount
P 1,000.00
4,000.00
2,000.00
P 7,000.00
Contribution to the Philippine Economy
The opening of the Mothers Choice Birthing Center in Camp 1, Maramag
Bukidnon will provide birthing facility in the South of Poblacion, Maramag,
Bukidnon and will provide more convenience and basic health services needed
by pregnant woman who needs more attentive care during the nine months of
pregnancy as well as the immediate care for newborn babies.
18
Government will be facilitated by lowering the percentage of pregnant
woman and new born child from mortality rate and additional tax for the operation
of the said birthing center.
The immediate community will be given full health access for pregnant
woman and new born babies at a very affordable price.
TECHNICAL FEASIBILITY
This aspect determines to what extent the project meets the technical
soundness criteria. The technical requirements of the project will be analyzed.
Description of the Project
The project will be named as Mothers Choice Birthing Center under the
management of licensed and experienced midwives with the assistance of
licensed and experienced pediatrician and ob-gyne physicians.
Description of the Area
Minimum of 300 x 15 square feet
(building and facility requirements is under the Department of Health prescription)
Toilet and adequate bathing facilities for mother and baby
24 hour supply of clean and hot water and electricity supply (including
emergency lighting)
24 hour refrigerator for storing medicines
19
Equipment in satisfactory condition
One patient bed per room for private type
Seven pt. in ward with curtain and dividers to provide patient privacy for
each room
Each room must have bright lighting
Oxygen tank and supply to the delivery room, must be secured to solid
object
Adequate prevention from occupational hazards
No animals in the clinic
All windows and doors should be covered with a minimum of a net
covering
Sufficient ventilation
Absolutely no smoking on the premises with an obvious sign at front desk
Cleaning and Sanitation:
Daily thorough cleaning of facilities with the use of a regimented checklist
20
Cleaning of individual patient areas after every use e.g. wiping down beds
and cleaning up any spillage of body fluids
Individual disposal bins for sharp equipment, clinical waste and household
general waste with ideally a safe and environmentally friendly method of
discard
Sufficient plumbing and drainage facilities
Hand washing sinks and alcohol gel to be located near clinical workstation
A dirty utility room for dirty linen and sanitary waste
A clean linen closet and laundry bag
A sterile laundry facility
Adequate method of sterilization of reusable instruments e.g. autoclave
Thorough hand washing with water and soap before and after each and
every patient contact including before and after each patient intervention
or procedure.
Alcohol gel to be applied on entering and leaving the
birthing center
Mothers Choice Birthing Center Confidentiality Statement
21
At Mothers Choice Birthing Center, our goal is to provide the best possible
security and privacy measures for each patient. All patient reports, documents,
lab values, and information will be kept confidential by the staff of Mothers
Choice Birthing Center. Prior to the release of any information, the patient will
first be asked for permission to disclose sensitive material to external parties.
Staff members not associated with the patients care are not allowed to review
records. All records will be kept for the duration of the patients life, after which
time the records will be destroyed to protect confidentiality. All records will be
kept in a locked, secure area of the clinic with no public access.
Antenatal Care
Patients should be given a choice at outset of care to have their birth at
Mother Choice Birthing Center or in the hospital. They should be educated that if
something goes wrong during their labor, outcomes for the woman and baby may
be better in an obstetrics unit at hospital. Obstetric units may be able to provide
direct access to obstetricians, anesthetists, neonatologists and other specialized
care, including epidural analgesia. At any point during pregnancy or delivery,
they may need to be transferred to a hospital for emergency treatment.
Antenatal Guidelines
First Visit: When the mother first realizes she is pregnant
Patient Screening Questionnaire
22
Education for the Mother:
How the baby develops during pregnancy government poster
General Advice About What to Expect During a Healthy Pregnancy
Keeping Healthy While Pregnant
Danger Signs during Pregnancy
Birth plan
Laboratory Test Requirements:
Hemoglobin
Hepatitis B
Blood glucose
Vitamin Supplementation and Medications
Folic Acid 400 mcg per day until the 12th week of pregnancy: this helps
prevent neural tube defects
Iron supplements should not be offered routinely: give only if anemic or
hemoglobin <11g/100mL
Multivitamins
Second Visit: Between 18-20 Weeks
Follow up with first visit and make sure patient has completed required
tests.
23
Continue to record observations, VS, weight, fundal height, and any
problems or concerns the expecting mother may have.
Labs: Blood Glucose.
Make plan for next visit.
Third Visit: Between 24-28 weeks
Follow-up with second visit
Continue Antenatal Flow Chart and record observations, vital signs,
weight, fundal height, and any problems or concern the expecting mother
may have.
Laboratory Test Requirement:
Hemoglobin
Urine: proteinurea
Blood glucose
Oral Glucose Tolerance Test (OGTT)
Ultrasound
Fourth Visit: Between 32-36 Weeks
Follow up with third visit
Continue record observations, vital signs, weight, fundal height, and fetal
presentation.
24
If fetus is found to be malpositioned through palpation, a confirmation must
be done by ultrasound.
If it is confirmed by ultrasound, give the woman a choice to follow up in one
to two weeks for a repeat ultrasound to check fetal position. If at that time the
fetus is still malpositioned the woman should be referred to the nearest hospital
and told she may not give birth at the clinic; however all post natal care from the
6 week baby check on are still available to her.
Laboratory Test Requirement:
Hemoglobin:
Normal: >10.
If hemoglobin <10, the woman should be referred to hospital for her birth, as low
Hb signifies a greater probability of bleeding during birth and the possible need
for blood products which the clinic cannot provide
Discuss upcoming delivery with the woman and go over any concerns or
questions she may have.
Encourage financial planning and discuss costs.
Encourage prompt mobilization towards the birthing centre as soon as
they feel the beginning stages of labor.
25
Discuss the possibility that they may not be able to give birth at the clinic,
should there any complications with their labor.
Other Visits:
Reasons for extra visits include, but are not limited to: high blood
pressure, pain in abdomen, and extra blood sugar checks
Other visits should be at the discretion of the patient and the SBA
providing antenatal care
Intrapartum Care
Admission only if in established labor
Sign consent form for admission.
First Stage of Labor
Definitions:
Latent first stage of labor: A period of time, not necessarily continuous,
when: there are painful contractions and some cervical change, including
cervical effacement and dilatation up to 4 cm.
Established first stage of labor: When there are regular painful
contractions and progressive cervical dilatation from 4 cm.
Duration of the first stage labor:
Nulliparous: 8-18 hours
26
Multiparous: 5-12 hours
Assessment
Initial Assessment of a woman in labor should include:
Listening to her story and review clinical records
Physical observation: temperature, pulse, blood pressure, urinalysis
Length, strength and frequency of contractions
Abdominal palpation: fundal height, lie, presentation, position and station
Vaginal loss: show, liquor, blood
Assessment of pain
FHR auscultated for a minimum of 1 minute immediately after a
contraction
Vaginal examination should be offered if woman is in established labor
IV Fluid access
2 large cannula (at least 18G/Green) to be inserted into a patients veins
on admission
Assessment
27
A pictorial record of labor (partograph) should be used once labor is
established
World Health Organization recommends 4-hour action line on partograph,
should one be used
Observations or Labor watch
Temperature and blood pressure every four hours
Pulse every hour
Documentation of frequency of contractions every thirty minutes
Frequency of emptying the bladder
Vaginal examination offered every four hours or where there is concern
about progress or in response to the womans wishes (after abdominal
palpation and assessment of vaginal loss).
Intermittent auscultation of the fetal heart after a contraction should occur
for at least one minute, every fifteen minutes, and the rate should be
recorded as an average. The maternal pulse should be palpated if a FHR
abnormality is detected to differentiate the two heart rates. Intermittent
auscultation can be undertaken by Doppler ultrasound.
Second Stage of Labor
28
Definitions:
Passive second stage of labor: The finding of full dilatation of the cervix
prior to or in the absence of involuntary expulsive contractions.
Onset of the active second stage of labor: The baby is visible with
expulsive contractions and a finding of full dilatation of the cervix or other
signs of full dilatation of the cervix. As well as active maternal effort
following confirmation of full dilatation of the cervix in the absence of
expulsive contractions.
Duration of the second stage labor
Nulliparous: Birth would be expected to take place within 3 hours of the
start of the active second stage in most women.
A diagnosis of delay in the active second stage should be made when it
has lasted 2 hours and women should be referred to a healthcare
professional trained to undertake an operative vaginal birth if birth is not
imminent.
Multiparous: Birth would be expected to take place within 2 hours of the
start of the active second stage in most women.
A diagnosis of delay in the active second stage should be made when it
has lasted 1 hour and women should be referred to a healthcare
29
professional trained to undertake an operative vaginal birth if birth is not
imminent.
Observations
Blood pressure and pulse every hour
Temperature every four hours
Vaginal examination offered every hour in the active second stage or in
response to the womans wishes (after abdominal palpation and
assessment of vaginal loss)
Documentation of the frequency of contractions every hour
Frequency of emptying the bladder
Ongoing consideration of the womans emotional and psychological
needs.
Assessment of progress should include maternal behavior, effectiveness
of pushing and fetal wellbeing, taking into account fetal position and
station at the onset of the second stage. These factors will assist in
deciding the timing of further vaginal examination and the need for
obstetric review.
30
Intermittent auscultation of the fetal heart should occur after a contraction
for at least one minute, at least every five minutes. The maternal pulse
should be palpated if there is suspected fetal bradycardia or any other
FHR anomaly to differentiate the two heart rates.
Ongoing consideration should be given to the womans position, hydration,
coping strategies and pain relief throughout the second stage.
Womens Position and Pushing in the Second Stage
Women should be discouraged from lying supine or semi-supine in the
second stage of labor and should be encouraged to adopt any other
position that they find most comfortable.
Women should be informed that in the second stage they should be
guided by their own urge to push.
If pushing is ineffective or if requested by the woman, strategies to assist
birth can be used, such as support, change of position, emptying of the
bladder and encouragement.
Reducing Perineal Trauma
Perineal massage should not be performed by healthcare professionals in
the second stage of labor.
31
Either the hands on (guarding the perineum and flexing the babys head)
or the hands poised (with hands off the perineum and babys head but in
readiness) technique can be used to facilitate spontaneous birth.
Lidocaine spray should not be used to reduce pain in the second stage of
labor.
A routine episiotomy should not be carried out during spontaneous vaginal
birth.
Women with a history of severe perineal trauma should be informed that
their risk of repeat severe perineal trauma is not increased in a
subsequent birth, compared with women having their first baby.
Third Stage of Labor
Definitions:
Third stage of labor: the time from the birth of the baby to the expulsion of
the placenta and membranes.
Prolonged third stage: over 30 minutes
Observations
Blood pressure and pulse
32
Womans general physical condition, as shown by her color, respiration
and her own report of how she feels
Vaginal blood loss
Recommendation
Active management of the third stage is recommended, which includes the
use of oxytocin (10 international units [IU] by intramuscular injection),
followed by early clamping and cutting of the cord and controlled cord
traction.
Women should be informed that active management of the third stage
reduces the risk of maternal hemorrhage and shortens the third stage.
Pulling the cord or palpating the uterus should only be carried out after
administration of oxytocin as part of active management.
Start completing Postnatal Notes
Immediate Cord Care after Birth
When the child the cord pulses and is fat and blue, do not cut at this time.
Place the bay on the mothers chest wrapped in a warm blanket.
After a while, feel the cord if the pulsation stops then cut.
33
Change gloves for the n next procedure.
Indications for Transfer to More Advanced Healthcare Facility via Ambulance
Need for continuous electronic fetal monitoring or EFM, indicated by:
Significant meconium-stained liquor, and this change should also be
considered for light meconium-stained liquor
Abnormal FHR detected by intermittent auscultation: less than 110 beats
per minute, greater than 160 bpm, any decelerations after a contraction; or
uncertainty of presence of fetal heartbeat
Maternal pyrexia: 38.0C once or 37.5C on two occasions 2 hours apart
Fresh bleeding starting in labor
The womans request to be transferred
Delay in the first or second stages of labor, diagnosed by:
Cervical dilatation of less than 2 cm in 4 hours for first labor
Cervical dilatation of less than 2 cm in 4 hours or a slowing in the progress
of labor for second or subsequent labors
Changes in the strength, duration and frequency of uterine contractions.
34
Request for epidural pain relief
Obstetric emergency antepartum hemorrhage, cord
presentation/prolapsed, postpartum hemorrhage, maternal collapse or a
need for advanced neonatal resuscitation
Retained placenta that cannot be extracted by manual intervention
Malpresentation or breech presentation diagnosed for the first time at the
onset of labor, taking into account imminence of birth
Either raised diastolic blood pressure: over 90 mmHg; or raised systolic
blood pressure: over 140 mmHg; on two consecutive readings taken 30
minutes apart
Third- or fourth-degree tear or other complicated perineal trauma requiring
suturing
If premature rupture of membranes occurred over 24 hours before onset
of labor
Care of Mother and Baby Immediately After Birth
Care of baby
35
APGAR scores at 1 and 5 minutes should be recorded for all births. If no
respirations, stimulate baby, if stimulation ineffective, begin neonatal
resuscitation.
Obtain babys vital signs, see Newborn Vital Signs
Skin-skin contact as soon as possible after birth
Baby dried and covered in warm dry blanket
Initial breastfeeding should be as soon as possible
Measurement of head circumference, body temperature and birth weight
should be measured soon after the 1st hour
An examination of the baby should be carried out to ensure no physical
abnormality
Apply Erythromycin ointment 0.5-1% or Tetracycline ointment 1% to both
eyes within 1 hour of birth
Administer Vitamin K 0.5 mg IM, within 1 hour of birth
Complete Postnatal Notes
Administer BCG immunization prior to discharge.
36
Needs hemoglobin check before discharge
Care of Woman
Measure temperature, pulse, blood pressure, uterine contractions, lochia
Examine placenta and membranes: assessment of their condition,
structure, cord vessels and completeness
Early assessment of maternal emotional/psychological condition
Record successful voiding of the womans bladder within 6 hours post
delivery
Perineum Assessment and Repair
Complete Postnatal Notes
Mothers who arrive in the immediate postnatal phase
Ensure patient has been known the antenatal period, has attended all the
required antenatal appointments and has had all the necessary
investigations
If not, then immediately send mother and baby to nearest hospital via
emergency transportation
37
If vital signs and observations within normal limits, mother and baby may
stay at clinic for further management
If any of the following occur, mother and baby should be transferred to
nearest hospital
Maternal systolic blood pressure greater than 140, less than 90, or
diastolic blood pressure greater than 90
Postpartum hemorrhage, with blood loss greater than 500 ml.
See
Management of Postpartum Hemorrhage
Maternal collapse
Maternal Pyrexia, defined by a temperature of 38C or greater
Retained placenta
Third or fourth degree perineal tear
Abnormality of baby
Neonatal resuscitation required at any point
Please ensure patient and baby stabilized before transferring to hospital
e.g. IV cannula inserted, fluid resuscitation
38
Postnatal Care
Postnatal Care of the Mother
Please complete Initial Mother Assessment form in Postnatal Notes
Give oral and demonstrational teaching on breastfeeding within 24 hours
of birth, prior to discharge from birthing centre
Breastfeeding:
Mother should educate about the important of breastfeeding
Perineal Care
Assess mother for perineal pain, discomfort or stinging, offensive perineal
odor or dyspareunia.
If the mother is experiencing discomfort, she should be taught that topical
cold therapy provides effective perineal pain relief.
Encourage perineal hygiene, such as frequent sanitary pad changes,
frequent hand washing, and daily bathing to keep the perineum clean.
General Advice
See to it of keeping healthy after giving birth
Postnatal Care of the Baby
Complete Initial Baby Assessment form in Postnatal Notes
39
Complete full body assessment of baby, if any gross abnormalities,
especially jaundice, within first 24 hours, baby may need to be referred to
hospital of choice
Prior to Discharge
Provide mother with chance to ask any questions she may have before
leaving the clinic.
Provide mother with documentation and help if necessary to fill out the
appropriate government forms to be reimbursed for the delivery of her
baby.
Postnatal Follow Up
Appointment at First Week
Follow Up for the Mother
Ask about any issues experienced and problems encounter like:
Signs of mastitis: flu-like symptoms, red, tender and painful breasts, if
present, encourage gentle massage of breast, continued feeding, paracetamol
for discomfort and increased fluid intake
Constipation and hemorrhoids: if no bowel movement three days after birth,
give patient a gentle laxative, encourage increased dietary fiber and fluid
40
consumption in both cases, and encourage cold packs and paracetamol for pain
management
Urinary incontinence: if this is an issue, give teaching on Keagel exercises
Fatigue: if experiencing excessive fatigue, review birthing events and
antepartum history, if any signs indicate hemorrhage, check mothers
hemoglobin.
Emotional wellbeing: encourage the mother to communicate any changes in
mood, emotional state or behavior that seem abnormal to her
Discuss plans for contraception following birth and encourage the mother
to abstain from sexual intercourse for six weeks postpartum
Follow Up for the Baby
Babies should be assessed for: temperature, heart rate, respiratory rate,
color, regular urination and stooling, general appetite and breast milk
intake, body tone, and irritability.
Assess for jaundice, pale stools and dark urine. If present assess severity,
if acute jaundice present, refer to hospital.
41
Appointment at Sixth Week -for immunization
Perform a complete physical assessment of the baby, as outlined in the
Complete Physical Assessment of the Baby and assess social smiling and
visual fixing at this time as well.
Ask about any concerns the mother has had about her child since the last
appointment
Administer OPV 1, Pentavalent 1 and Rotarex 1
Appointment at Tenth Week
Follow Up for the Mother
Ask about any concerns the mother has had since the previous
appointment
Continue to manage concerns that have arisen previously
Follow Up for the Baby
Ask about any concerns the mother has had about the child since the last
appointment
Continue to manage concerns that have arisen previously
42
Measure and plot height and weight on growth chart
Administer OPV 2 , Pentavalent 2 and Rotarex 2
Appointment at Fourteenth Week
Administer OPV 3and Pentavalent 3
Appointment at Sixth Month
Measure and plot babys height and weight in growth chart
Appointment at Ninth Month
Administer Measles immunization to baby and vitamin A
Actual Building of the Mothers Choice Birthing Center
43
Proposed Floor Plan 12-Bed Ward
44
Table 7. Expected Attainable Clients
Area
Jun
Jul
Aug
Sep
Oct
Nov
Dec
Jan
Feb
Mar
Apr
May
Total
11
11
11
11
11
11
11
11
11
11
11
11
132
12
12
12
12
12
12
12
12
12
12
12
12
144
96
Total
31
31
31
31
31
31
31
31
31
31
31
31
372
Assumptions:
An increase of 16% of clients per year or an equivalent of additional 4
clients in a year will be realized on the second year.
Effect of Layout on Work Flow
The effect of layout on work flow will be smooth, convenient, thus resulting
for efficient and effective care for mother and baby.
45
Provision for Expansion
During the five years initial operations, partners agreed to focus more on
area penetration and long-term profit maximization and established good
relationship toward the clients to address and respond immediately to their need
and demand. Provision for expansion will be planned as business will grow and
become stable.
Structure
The structure will be fully concreted and will be build according to
government requirement to prevent hazard.
Waste Disposal
There will be a separate trash can for biodegradable, non-biodegradable
and infectious items. Biodegradable waste will be disposed in a compose pit.
Non-biodegradable waste will be sold in junk shops.
For Infectious Items
(Sharps and Biohazard Disposal) will be disposed as follows: All sharps including
needles, finger sticks, glass, ampules, IV supplies, and specimen containers will
be disposed of in a puncture proof plastic container provided by the clinic. Each
container when full will be disposed of in a 3 meter deep hole, at least 20 meters
from the nearest water supply and building, as recommended by DOH.
Biohazardous material including blood and birthing by-products should be
46
disposed of via incineration, or disposed of by the same method as detailed
above.
FINANCIAL FEASIBILITY
This chapter shows the financial performance and resources of the
proposed project. This includes: financial statements and financial ratios that
enable the proponents to determine the liquidity, profitability, stability of the
project and the proponents ability to pay its financial obligations. It will give
substantial information as basic for the establishment of the proposed project.
Table 8. Monthly Projected Cost
Particulars
Ultrasound Rental
Building Amortization (Finance)
Lot Rental
Water and Electricity Bill
Midwife Salary (5)
Principal Midwife
Ob-Gyne (Consultation)
Pediatrician (consultation)
Supplies
Watchman
Total
Unit Cost per Patient
Unit Cost
= Total Cost / Total no. of clients
= 98,000/31
= 3,161.29
Mark-up
= 253%
Amount (in Php)
2,000.00
1,600.00
2,000.00
5,500.00
40,000.00
10,000.00
15,500.00
15,500.00
1,900.00
4,000.00
98,000.00
47
Unit Price per Patient = 8,000.00
Table 8. Equipment
Particulars
Qty
Monthly
NSVD set
Stethoscope
500.00
500.00
Weighing scale
1000.00
1000.00
Blood pressure
apparatus
500.00
500.00
Thermometer
300.00
300.00
Doppler
15,000.00
15,000.00
Measuring tape
20.00
20.00
Kelly pad
200.00
200.00
Goose neck lamp
300.00
300.00
Tourniquet
50.00
50.00
P 21,870.00
P 21,870.00
Total
4000.00
Yearly
P
4000.00
Table 9. Supply
Particulars
mask
soap
Qty
Monthly
P
50.00
100.00
Yearly
P
600.00
1,200.00
48
bleach
70.00
840.00
paper
150.00
1,800.00
50.00
600.00
cotton
100.00
1,200.00
gauze
100.00
1,200.00
glove
100.00
1,200.00
50.00
600.00
alcohol
100.00
1,200.00
Ky jelly
100.00
600.00
syringe
150.00
1,800.00
P 1,120.00
P 13,440.00
Monthly
90.00
Yearly
ball pen
umbilical cord
Total
Table 10. Medicine
Particulars
Paracetamol
Qty
P
P
Anti-inflammatory
1,080.00
300.00
3,600.00
Antiemetic
200.00
2,400.00
49
Oxytocin
500.00
6,000.00
Vit. k
200.00
Erythromycin
300.00
Albendazole
100.00
2,400.00
3,600.00
1,200.00
Total
P 1,690.00
20,280.00
Table 11. Rental Expense
Particulars
Ultrasound Rental
Monthly
2,000.00
Yearly
P
Land Rental
24,000.00
2,000.00
24,000.00
Amortization (Building)
2,000.00
24,000.00
Total
P 6,000.00
72,000.00
Note:
Ultrasound will be lend from GE company at Php 2,000.00/month payable
for 20 years
Old Building will be renovated through Land Bank loan amounting to Php
480,000.00
Table 12. Ultrasound Income
Particulars
First Tri @ 600
Qty
31
Second Tri @ 450
31
13,950.00
Third Tri @ 450
31
13,950.00
Monthly
18,600.00
Yearly
P 223,200.00
167,400.00
167,400.00
Total
46,500.00
558,000.00
50
Less:
Sonologist Fee
31
18,600.00
P 223,200.00
Net Income
27,900.00
334,800.00
Less: Rental
2,000.00
24,000.00
Net Income after Rental Fee
25,900.00
310,800.00
Table 13.Schedule for Salaries and Wages
Particulars
Principal Midwife
Qty
1
Monthly
P 10,000.00
Yearly
P 120,000.00
Midwives
40,000.00
480,000.00
Watchman
8,000.00
96,000.00
Pediatrician
15,500.00
186,000.00
Ob-Gyne
15,500.00
186,000.00
Sonologist
18,600.00
223,200.00
Total
P 107,600.00
P 1,291,200.00
Mothers Choice Birthing Center
Projected Income Statement
For 1 year
Table 14. Projected Income Statement of Mothers Choice Birthing Center
Particulars
Year 1
Gross Profit
3,224,000.00
Add: Ultrasound Income
558,000.00
51
Total Gross Profit
Less: Expenses
Salaries and Wages
Advertising
Rental Expense
Amortization Expense
Ultrasound Rental
Equipment
Supply
Medicine
Total Expenses
Net Income
Less: Income Tax (30%)
Net Income after Tax
3,782,000.00
1,291,200.00
7,000.00
48,000.00
24,000.00
24,000.00
21,870.00
13,440.00
20,280.00
1,449,790.00
2,332,210.00
699,663.00
1,632,547.00
Mothers Choice Birthing Center
Projected Cash Flow Statement
For 1 year
Table 15. Projected Cash Flow Statement of Mothers Choice Birthing Center
Particulars
Pre-operating Period
Year 1
Cash Inflow
Owners Capital
523,810.00
Gross Profit
3,782,000.00
Total Cash Inflow
4,305,810.00
Less: Cash Outflow
Salaries and Wages
1,291,200.00
Advertising
7,000.00
Rental Expense
48,000.00
Amortization Expense
24,000.00
Ultrasound Rental
24,000.00
Equipment
21,870.00
Supply
13,440.00
Medicine
20,280.00
Income Tax
699,663.00
Total Cash Outflow
2,149,453.00
Cash Balance Ending
2,156,357.00
52
Mothers Choice Birthing Center
Projected Balance Sheet
For 1 year
Table 15. Projected Balance Sheet of Mothers Choice Birthing Center
Particulars
Amount (Php)
Cash on Bank
2,000,000.00
Cash on Hand
156,357.00
Total Assets
2,156,357.00
Liabilities
Add: Capital
Add: Net Income
Total Liabilities and Capital
480,000.00
43,810.00
1,632,547.00
2,156,357.00
Financial Analysis and Interpretation:
Profit Margin
= Net Income
Sales
= 1,632,547.00
3,782,000.00
= 0.4317 or 43.17%
Analysis and Interpretation:
The profit margin shows that for every 1.00 sales, there is a net profit
margin of .43 centavo. This means that during the first year of operation the
birthing center will be able to earn 43% net profit considering also that various
expenses were incurred during the pre-operating period.
53
Return on Investment
= Net Income
Investment
= 1,632,547.00
523,810.00
= 3.11
Analysis and Interpretation
It is expected that for every 1.00 peso invested by the proponents, the
birthing center can return 3.11 pesos during the first year of operation.
Payback Period
= Investment
Annual Cash Returns
=
523,810.00
3,782,000.00
= 0.138 or 13.8%
It reflects that the company can repay its invested capital during the first
year of its operation.
Conclusions:
54
Based on the presentation of this study, the following conclusion was
made:
Birthing Center is feasible in Camp 1, Maramag, Bukidnon since there is
no available birthing center in the area including the nearby barangays.
Recommendation:
The following recommendations were drawn:
Birthing Center is commendable in the areas far from hospitals.
Você também pode gostar
- Feasibility Study On Birthing ClinicDocumento48 páginasFeasibility Study On Birthing ClinicKay D. Beredo100% (1)
- Amalachukwu Maternity Home Health CareDocumento11 páginasAmalachukwu Maternity Home Health CareIgbani Victory100% (1)
- Lyiny inDocumento11 páginasLyiny inSi Kaye100% (3)
- Feasibility Study of Birthing Center in Tuguegarao CityDocumento14 páginasFeasibility Study of Birthing Center in Tuguegarao CityUmma Eugenio Agustin75% (4)
- Feasibility Study of Birthing Center in Tuguegarao CityDocumento14 páginasFeasibility Study of Birthing Center in Tuguegarao CityCharisse Woo100% (1)
- Business Plan EditedDocumento24 páginasBusiness Plan EditedEduardo Anerdez86% (14)
- Draft Ordinance (Birthing Homes Regulation)Documento8 páginasDraft Ordinance (Birthing Homes Regulation)Zimm BasubasAinda não há avaliações
- Executive Summary Maternity Clinic Bus PlanDocumento6 páginasExecutive Summary Maternity Clinic Bus PlanSimu Jemwa100% (4)
- Mayo Clinic Maternity Ward FinalDocumento18 páginasMayo Clinic Maternity Ward Finalapi-240147836Ainda não há avaliações
- Policies, Standards Requirements For Licensing Birthing ClinicDocumento46 páginasPolicies, Standards Requirements For Licensing Birthing ClinicMatt Lao Dionela83% (24)
- Pains and Gains of Birth Clinic OwnersDocumento33 páginasPains and Gains of Birth Clinic OwnersNamoAmitofou100% (3)
- Clinic Feasibility StudyDocumento20 páginasClinic Feasibility StudyJeff Bergosh100% (3)
- Feasibility Study - Medical Supply and EquipmentsDocumento22 páginasFeasibility Study - Medical Supply and EquipmentsEduardo Salazar71% (7)
- Family Planning DohDocumento441 páginasFamily Planning DohWiston Ilagan100% (11)
- EINC - A Step-By-Step GuideDocumento41 páginasEINC - A Step-By-Step GuideAlejandro Aricheta91% (11)
- Birthing Homes ReqDocumento10 páginasBirthing Homes ReqMi Lagro100% (2)
- Feasibility Study For A Hospital Management SystemDocumento7 páginasFeasibility Study For A Hospital Management SystemMuhammad Saad Ashrafi100% (1)
- Kalarikal Pharmacy Business Plan: Submitted By, N.P.Vinide S3 MbaDocumento17 páginasKalarikal Pharmacy Business Plan: Submitted By, N.P.Vinide S3 MbaVinide Vineeth100% (7)
- Medical Equipment - Supplies Business PlanDocumento50 páginasMedical Equipment - Supplies Business PlanMurali33% (3)
- The Health Care Delivery SystemDocumento114 páginasThe Health Care Delivery SystemBea Bianca CruzAinda não há avaliações
- Clinic Business PlanDocumento41 páginasClinic Business PlanIshaan Kamal100% (6)
- Family Planning Service Record Form IDocumento4 páginasFamily Planning Service Record Form IBarangay Lam-anAinda não há avaliações
- Guidelines Setting Up Family Planning Services HospitalsDocumento36 páginasGuidelines Setting Up Family Planning Services HospitalsRNdrei dela Cruz100% (1)
- Family PlanningDocumento55 páginasFamily PlanningRNdrei dela Cruz94% (18)
- Dialysis Center in BPDHDocumento29 páginasDialysis Center in BPDHXien Cadiz100% (5)
- Unang Yakap DOH EINCDocumento20 páginasUnang Yakap DOH EINCLore Anne Mhae Santos100% (1)
- Feasibility ExampleDocumento105 páginasFeasibility ExampleJho Marie RomeroAinda não há avaliações
- The Anatomy of The Philippine Health Care SystemDocumento43 páginasThe Anatomy of The Philippine Health Care SystemMark Reynie Renz Silva100% (1)
- Policies, Standard Requirements For Licensing Birthing ClinicDocumento25 páginasPolicies, Standard Requirements For Licensing Birthing ClinicAl YsSa Ricafort Millabas100% (3)
- Institute of Arts Business and FinanceDocumento91 páginasInstitute of Arts Business and Finance`ynah100% (1)
- Feasibility Study Birthing ClinicDocumento38 páginasFeasibility Study Birthing ClinicMicah Langiden100% (1)
- Feasibility StudyDocumento2 páginasFeasibility StudyJessica Ddw Fianza100% (13)
- Ao2019 0026Documento5 páginasAo2019 0026alissalvqs100% (2)
- Aschiana: Afghan Children and New Approach Project ProposalDocumento6 páginasAschiana: Afghan Children and New Approach Project Proposalsaher8901100% (1)
- Essential Intrapartum and Newborn Care (EINC) Bulletin 1Documento10 páginasEssential Intrapartum and Newborn Care (EINC) Bulletin 1maxicap7386% (7)
- Feasibility Study ISKO LOUNGE CHAPTER 1 PDFDocumento157 páginasFeasibility Study ISKO LOUNGE CHAPTER 1 PDFAdrian JamesAinda não há avaliações
- The Comparative Study of Pastil Restaurant in General Santos CityDocumento8 páginasThe Comparative Study of Pastil Restaurant in General Santos CityLaurabelle Nueva Palabao Amoguis - Dinglasa100% (1)
- A Project Feasibility StudyDocumento6 páginasA Project Feasibility StudySaramee Inosanto86% (7)
- Hemorrhage Uterine AtonyDocumento59 páginasHemorrhage Uterine Atonygorres100% (1)
- Midwifery EntrepreneurshipDocumento2 páginasMidwifery EntrepreneurshipRoland Acebedo82% (17)
- Elizabeth Retail Pharmacy Business Plan2Documento14 páginasElizabeth Retail Pharmacy Business Plan2believe daniel100% (3)
- Project Proposal On Child Nutrition For Sustainable Health and Prenatal ClinicDocumento6 páginasProject Proposal On Child Nutrition For Sustainable Health and Prenatal Clinicczeremar chan100% (2)
- Internal Examination: Prepared By: Lester D. Bongabong BSN Ii - BDocumento9 páginasInternal Examination: Prepared By: Lester D. Bongabong BSN Ii - BJustine Cagatan100% (1)
- FHSIS Form TCL Pre NatalDocumento11 páginasFHSIS Form TCL Pre NatalEden Vblagasy100% (5)
- FPCBT Level 1 For FacilitatorsDocumento519 páginasFPCBT Level 1 For FacilitatorsMichael Villavert100% (1)
- Normal Spontaneous Delivery Case StudyDocumento5 páginasNormal Spontaneous Delivery Case StudyJerwin Ogoy50% (10)
- Feasibility Study (Raw File)Documento9 páginasFeasibility Study (Raw File)khengamer100% (6)
- Unang YakapDocumento14 páginasUnang YakapIrwan M. IskoberAinda não há avaliações
- Project ProposalDocumento5 páginasProject ProposalainjelAinda não há avaliações
- Maternal, Newborn and Child Health and Nutrition Strategy (Manual of Operations)Documento235 páginasMaternal, Newborn and Child Health and Nutrition Strategy (Manual of Operations)Misyel AvelinoAinda não há avaliações
- Tarpaulin PrintingDocumento29 páginasTarpaulin PrintingChristian Lim75% (4)
- Loi MbfhiDocumento11 páginasLoi MbfhiAnsams Fats100% (2)
- A Sample Hospital Business Plan Template - ProfitableVentureDocumento15 páginasA Sample Hospital Business Plan Template - ProfitableVentureMacmilan Trevor Jamu100% (1)
- BEmONC & CEmONCDocumento39 páginasBEmONC & CEmONCYuuki Chitose (tai-kun)100% (3)
- Feasibility Study - TheyCare Child Care CenterDocumento61 páginasFeasibility Study - TheyCare Child Care Centeritscristinavi93% (15)
- Laws Related To Family PlanningDocumento17 páginasLaws Related To Family PlanningMary Chris Bacnis CabuangAinda não há avaliações
- Postpartum Nurse ResumeDocumento5 páginasPostpartum Nurse Resumeafiwgzsdf100% (2)
- Medical Billing & Coding Demystified, 2nd EditionNo EverandMedical Billing & Coding Demystified, 2nd EditionNota: 4 de 5 estrelas4/5 (1)
- Feasibility Study On Birthing ClinicDocumento50 páginasFeasibility Study On Birthing ClinicbillyjopalmaofficialAinda não há avaliações
- Laporan Praktikum Faal Aplikasi PDFDocumento13 páginasLaporan Praktikum Faal Aplikasi PDFSilvi ApreliaAinda não há avaliações
- Team Work EssayDocumento7 páginasTeam Work Essayezknbk5h100% (2)
- UNICEF Innocenti Prospects For Children Global Outlook 2023Documento53 páginasUNICEF Innocenti Prospects For Children Global Outlook 2023sofiabloemAinda não há avaliações
- Ardc 2Documento1 páginaArdc 2Camille GuintoAinda não há avaliações
- Simplified ACLS AlgorithmDocumento1 páginaSimplified ACLS AlgorithmBrianAinda não há avaliações
- Antihypertensive Drugs - Classification and SynthesisDocumento14 páginasAntihypertensive Drugs - Classification and SynthesisCường NguyễnAinda não há avaliações
- Acute Pyelonephritis - Salido, Reyes 3CDocumento24 páginasAcute Pyelonephritis - Salido, Reyes 3Cmena inezAinda não há avaliações
- Social Perspectives - Unit 10 - Task 1 - Copy 123Documento13 páginasSocial Perspectives - Unit 10 - Task 1 - Copy 123zxko24Ainda não há avaliações
- Patients With Acid, High Fat and Low Protein Diet Have Higher Laryngopharyngeal Reflux Episodes at The Impedance PH MonitoringDocumento10 páginasPatients With Acid, High Fat and Low Protein Diet Have Higher Laryngopharyngeal Reflux Episodes at The Impedance PH MonitoringLucien HaAinda não há avaliações
- 10-05 Roster GWG and PAsDocumento1 página10-05 Roster GWG and PAsCalifornia Stem Cell ReportAinda não há avaliações
- H02E Assignment 8Documento4 páginasH02E Assignment 8Good ChannelAinda não há avaliações
- SirkulasiDocumento17 páginasSirkulasiJessica VanyaAinda não há avaliações
- W 26882Documento53 páginasW 26882Jose GueraAinda não há avaliações
- Supervivencia Dental A Largo Plazo Después Del Tratamiento Regenerativo de Defectos IntraóseosDocumento7 páginasSupervivencia Dental A Largo Plazo Después Del Tratamiento Regenerativo de Defectos IntraóseosAgustin BuryakAinda não há avaliações
- Research Article: An Effective LSTM Recurrent Network To Detect Arrhythmia On Imbalanced ECG DatasetDocumento11 páginasResearch Article: An Effective LSTM Recurrent Network To Detect Arrhythmia On Imbalanced ECG DatasettestAinda não há avaliações
- 0529 Protocol Update 6.2.09 PDFDocumento57 páginas0529 Protocol Update 6.2.09 PDFTowhidulIslamAinda não há avaliações
- Meeting 9.Documento6 páginasMeeting 9.Ida NursantiAinda não há avaliações
- The Colloidal Silver Cure For Cheyletiella MitesDocumento10 páginasThe Colloidal Silver Cure For Cheyletiella MitesduhitijeloAinda não há avaliações
- COVID-19 Prevention & IEC Committee, PGIMER Chandigarh: Tentative Webinar Schedule For Healthcare ProfessionalsDocumento3 páginasCOVID-19 Prevention & IEC Committee, PGIMER Chandigarh: Tentative Webinar Schedule For Healthcare Professionalsvarshasharma05Ainda não há avaliações
- Considerations For The Design of Antibody-Based TherapeuticsDocumento30 páginasConsiderations For The Design of Antibody-Based TherapeuticsDaniel CastanAinda não há avaliações
- Sample TranscriptDocumento2 páginasSample TranscriptTejas Shah67% (3)
- The Powerful Impact of StressDocumento19 páginasThe Powerful Impact of StressMichael Angelo SeñaAinda não há avaliações
- HEALTH-TEACHING-PLAN sUGATON EVALDocumento9 páginasHEALTH-TEACHING-PLAN sUGATON EVALPrincess Faniega SugatonAinda não há avaliações
- Zanki Step 2 - Cardiovascular SystemDocumento129 páginasZanki Step 2 - Cardiovascular SystemChunlei WangAinda não há avaliações
- CHN SummaryDocumento20 páginasCHN SummaryFaith ManingoAinda não há avaliações
- CIPD Mental Health & Wellbeing Briefing For Managers May 2020Documento23 páginasCIPD Mental Health & Wellbeing Briefing For Managers May 2020bya*boAinda não há avaliações
- 2014 Group Case StudyDocumento42 páginas2014 Group Case StudyBrian100% (1)
- InclusivnessDocumento183 páginasInclusivnessmollalgnAinda não há avaliações
- Basic Ethical Principles 1. StewardshipDocumento5 páginasBasic Ethical Principles 1. Stewardshipmitsuki_sylph83% (6)
- Surgical Sponges - Towels WebDocumento20 páginasSurgical Sponges - Towels WebDa Josh MarienellaAinda não há avaliações