Escolar Documentos
Profissional Documentos
Cultura Documentos
Hsci 480 Research Paper
Enviado por
api-253401555Descrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Hsci 480 Research Paper
Enviado por
api-253401555Direitos autorais:
Formatos disponíveis
Running head: BRIDGING THE GAP FOR PATIENTS WITH MENTAL ILLNESSES
Bridging the Gap for Patients with Mental Illnesses
Through the Process of Self-Management
Nicolle L. Quenga
HSCI 480
California State University San Bernardino
BRIDGING THE GAP FOR PATIENTS WITH MENTAL ILLNESSES
Table of Contents
Abstract..3
Introduction...4
Identifying the Problem..4,5
Conflict in the Health Care System...6
Breaking Down the Barriers6,7
Experimenting with Direct Care.7,8
Experimenting with Indirect Care.8
Conclusion.8
References9,10
BRIDGING THE GAP FOR PATIENTS WITH MENTAL ILLNESSES
Abstract
To achieve and mental stability is one of the single most important things we can do for our
health. There is not nearly enough emphasis placed on the common mental disorders such as
anxiety and depression. The barriers present in the health care system, medical personnel, and
assigned intervention/treatment method need to be addressed. The improvement of a patients
mental health condition can be made through strategic approaches in direct and indirect care.
This paper explores the possibilities of assigning nurses to patients based on their aptitude and
web-based programs. I found that both options proved to significantly improve a persons
symptoms and overall mental health status.
Keywords: anxiety, depression, mental health, direct, indirect, aptitude, wed-based
BRIDGING THE GAP FOR PATIENTS WITH MENTAL ILLNESSES
Bridging the Gap for Patients with Mental Illnesses
Through the Process of Self-Management
The number of people suffering from mental illness is dramatically increasing and
becoming a global concern. There are multiple barriers such as: conflicts in the current health
care system, inaccurate disorder recognition factors, and physician incentives/disincentives that
prevent patients from receiving the appropriate treatment interventions. It is crucial to our safety
that these areas of concern be addressed and modified to improve the overall mental health of our
communities. I chose this topic because I strongly believe that management and intervention play
a crucial role in the improved outcomes of mental illnesses. The barriers need to be magnified,
inspected and depleted to reach those in need of treatment. It is important to experiment with
different methods of intervention to see which are most beneficial for patients in their given
condition.
Identifying the Problem
Over the last five years, shootings have managed to make their way into the news
headlines numerous times. Research has found that a majority of the shooters had some
documented medical history of mental illness or presented obvious indicators of illness for a
length of time. Their irrational and violent behavior, however, suggests a serious lack in the
proper treatment of their condition. The National Institute of Mental Health (NIMH) lists
neuropsychiatric disorders as the number one leading disease in 2010. It conservatively
estimates the total costs associated with serious mental illness to be in excess of $300 billion per
year (SAMHSA, 2002). The gaps in our mental health system are costing lives and billions of
dollars. In order to fill these gaps, health care providers and patients alike must develop a clear
understanding of what a mental illness is and how to effectively address it.
BRIDGING THE GAP FOR PATIENTS WITH MENTAL ILLNESSES
Anxiety and depression are two of the most common mental disorders (CMDs) in our
society today. The clinical definition for depression according to WebMD is feelings of intense
sadness -- including feeling helpless, hopeless, and worthless -- last for many days to weeks and
keep you from functioning normally. Anxiety is being in a constant state of feeling anxious or
nervous which can cause such distress that it interferes with a person's ability to lead a normal
life. It is vital for people to be aware of their feelings and be able to recognize when those
feelings become too overwhelming. A daily log that tracks mood, thoughts and activities can
indicate whether any major changes are occurring. Without sufficient knowledge and selfmonitoring, the symptoms can become more serious and possibly result in suicide. 30% to 70%
of suicide victims suffer from major depression or bipolar (manic-depressive) disorder (Mental
Health America). And considering suicide is the eleventh leading cause of death in the U.S., this
is an important correlation that cannot be ignored. Even though mental illness contributes greatly
to the suicide rates, it has the potential to dramatically lower them through an early diagnosis and
attentive medical treatment program.
In regards to mental illnesses, San Bernardino County presents itself as a primary area for
concern. Due to a large majority of this county being low-income, health care is less accessible.
Approximately 65,000 low-income residents of San Bernardino County were estimated to have
a serious mental illness and need mental health services in 2012/13 (sb county). Those who are
experiencing symptoms of mental illness or have been diagnosed with a disorder are not
receiving adequate resources to manage it. The county did a report on the number of people from
2008-2013 expressing an immediate need for mental health services. This bar graph shows there
is a consistent rise in numbers and demonstrates the desperate call for a solution.
BRIDGING THE GAP FOR PATIENTS WITH MENTAL ILLNESSES
Conflict in the Health Care System
The critical flaws in our health care system are the main reasons why people with mental
disorders are being neglected. Physician turnover is one that has negatively impacted the entire
system of patient care. An annual Physician Retention Survey from Cejka Search and the
American Medical Group Association (AMGA) finds that medical groups had an average
physician turnover rate of 6.8 percent in 2012, up from 6.5 percent in 2011 and the highest rate
since 2005 (RWJF). The California Physician Facts and Figures Almanac points to age as being
one of the main causes. California has the largest percentage of physicians over the age of 60. In
comparison to other states, we take the lead at a staggering 30% (CHCF, 2010). When the
availability of PCPs in an area decreases, so does the availability of care. The Inland Empire is
experiencing this problem firsthand. The almanac provides statistical evidence supporting the
fact that the area falls below national recommendations for the number of providers and
specialists per 100,000 population. It has always been a challenge for the desert area to attract
and maintain skilled physicians and specialists. It is not considered an ideal area to practice
medicine because of its physical location and low economic stability. Fewer health providers also
results in a high patient to physician ratio. Those practitioners who remain in the area are forced
to take on a surplus of new patients, shorten their visitation times and outwardly extend their
scheduling of appointments. All of these combined creates restrictions on various aspects of
patient care for both doctors and their staff.
Breaking Down the Barriers. Amidst the obstacles that exist regarding the preventative
and treatment options of people with mental illnesses, there are solutions available. One is
identifying the incentives and disincentives that influence a medical practice. According to
Incentives and Disincentives for the Treatment of Depression and Anxiety: A Scoping Review,
BRIDGING THE GAP FOR PATIENTS WITH MENTAL ILLNESSES
there are six: (1) attitudes and beliefs, (2) training and core competencies, (3) leadership, (4)
organizational, (5) financial, and (6) systemic (Ashcroft, 2014). The objective is to use these
variables interchangeably in such a way that they encourage health organizations to adopt
various approaches in treatment and promote interest in mental health. Their research findings
highlight the fact that disincentives are equally as important to understand when trying to
accomplish goals. A second solution is training doctors and nurses to recognize the signs and
symptoms of CMDs. Their ability to distinguish between which symptoms match with which
disorder is beneficial to both the patient and professional. I have had the pleasure of working
beside a PCP/cardiologist for five years. In this time, I have personally experienced the major
flaws associated with mental health assessment. It is common for a patient to express their
feelings of distress, anxiety and depression but still be ignored. Sometimes physicians will
simply prescribe them medication or refer them to a psychiatrist. Depending on the severity of
the disorder, these methods of treatment are not always the best solution. The patient must
develop a comfortable relationship with their physician and trust that they will be provided the
best medical advice for their life.
Experimenting with Direct Care. In terms of treatment for depressed patients, one
study conducted in Belgium offers a unique approach. Ordinarily, a person that is admitted to
their psychiatric unit of a hospital or residential home is assigned one nurse for the entire stay.
Researchers wanted to test whether matching nurses based on their aptitude of knowledge for
different depressive stages would be more effective. Nurses were ranked as novice, proficient or
master. This factor determined which displayed behaviors they were most suited to manage. In
this study, various nurse aptitudes showed several statistically significant associations with
changes in a patients depressive feelings, whereas antidepressant medication did not
BRIDGING THE GAP FOR PATIENTS WITH MENTAL ILLNESSES
(HASPESLAGH). This treatment method would require regular strategic planning and
evaluation from managers/nurses in an organization.
Experimenting with Indirect Care. Web-based programs are a more practical
intervention method for those physicians with a high patient volume. A study called Impact of a
Mobile Phone and Web Program on Symptom and Functional Outcomes for People with Mildto-Moderate Depression, Anxiety and Stress, demonstrates the technologys ability to facilitate in
the self-management of people with CMDs. It is convenient, readily accessible and highly
effective in improving a patients condition. The study utilizes a program called myCompass.
The program contains 12 skill-building modules derived from CBT, Interpersonal
Psychotherapy, Problem-solving Therapy and Positive Psychology that cover topics such as
Managing Fear and Anxiety, Tackling Unhelpful Thinking, Managing Loss and Major Life
Change, and Solving Problems (Proudfoot). Assuming that the subjects used the program as
instructed, they experienced a significant reduction in their symptoms. If this type of program
could be implemented by PCPs, it has great potential to improve the health of those with mental
illnesses.
Conclusion
The purpose of this paper is to bring awareness to mental illnesses and explain its
immediate need for restructure in the mental health care system. There are numerous barriers that
prevent people from receiving adequate care. Health care systems must be designed so that there
is the appropriate amount of PCPs available to treat a countys patient population. All medical
personnel should be trained on the subject of mental disorders to accurately diagnose and treat an
individual. It takes a team effort from all persons involved to pinpoint a disorder and decide on
the right treatment method.
BRIDGING THE GAP FOR PATIENTS WITH MENTAL ILLNESSES
References
Annual Total Direct and Indirect Costs of Serious Mental Illness (2002). (2002, January
1). Retrieved November 10, 2014, from
http://www.nimh.nih.gov/health/statistics/cost/index.shtml
Ashcroft, R. , Silveira, J. , Rush, B. , & McKenzie, K. (2014). Incentives and
disincentives for the treatment of depression and anxiety: A scoping review. Canadian Journal of
Psychiatry, 59(7), 385-392.
HASPESLAGH, M. , EECKLOO, K. , & DELESIE, L. (2012). Aptitude-based
assignment of nurses to depressed patients. Journal of Psychiatric & Mental Health Nursing,
19(6), 492-499.
Physician Supply. July (2010). In California Health Care Almanac. California Physician
Facts and Figures (pp. 1-33).
Physician Turnover at Highest Rate Since 2005. (2013, March 21). RWJF. Retrieved
November 17, 2014, from http://www.rwjf.org/en/blogs/human-capitalblog/2013/03/physician_turnovera.html
Proudfoot, J. , Clarke, J. , Birch, M. , Whitton, A. , Parker, G. , et al. (2013). Impact of a
mobile phone and web program on symptom and functional outcomes for people with mild-tomoderate depression, anxiety and stress: A randomised controlled trial. BMC Psychiatry, 13, .
San Bernardino County Community Indicators Report. (2014). Community Health and
Wellness, 50-52. Retrieved November 8, 2014, from
http://cms.sbcounty.gov/Portals/21/Resources Documents/CIR_2014_Report.pdf
BRIDGING THE GAP FOR PATIENTS WITH MENTAL ILLNESSES
Suicide. (n.d.). Retrieved November 10, 2014, from
http://www.mentalhealthamerica.net/suicide
10
Você também pode gostar
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Epilepsy & BehaviorDocumento5 páginasEpilepsy & BehaviorRirin RamadhanyAinda não há avaliações
- EAT 26 ScoringDocumento1 páginaEAT 26 ScoringRezza Hary100% (1)
- Clinical Psychiatry (Kraepelin, 6th Ed. 1902)Documento478 páginasClinical Psychiatry (Kraepelin, 6th Ed. 1902)Ricardo R. Ricardo100% (1)
- The Dissociation Theory of Pierre JanetDocumento12 páginasThe Dissociation Theory of Pierre Janetvalentina chistrugaAinda não há avaliações
- MENTOR OET Writing Session 10 MR Ming Zang Oet For NursingDocumento4 páginasMENTOR OET Writing Session 10 MR Ming Zang Oet For NursingAnjana Varghese50% (2)
- Intro Psychological DisordersDocumento39 páginasIntro Psychological DisordersMary Jo LegaspiAinda não há avaliações
- 1 Being and The Death Drive: The Quality of Green's ThinkingDocumento10 páginas1 Being and The Death Drive: The Quality of Green's ThinkingDaysilirionAinda não há avaliações
- Deoferio vs. Intel Technology Philippines, Inc.Documento2 páginasDeoferio vs. Intel Technology Philippines, Inc.Jica GulaAinda não há avaliações
- McLean Hospital 2013 Annual ReportDocumento24 páginasMcLean Hospital 2013 Annual ReportmcleanhospitalAinda não há avaliações
- Black SwanDocumento6 páginasBlack SwanKASHISH DAGAAinda não há avaliações
- Psych GlossaryDocumento42 páginasPsych GlossaryVida Marie PaguiriganAinda não há avaliações
- DNB Psychiatry Thesis TopicsDocumento7 páginasDNB Psychiatry Thesis Topicscandicehimwarren100% (2)
- Suicide and Other Psychiatric EmergenciesDocumento32 páginasSuicide and Other Psychiatric EmergenciesGolda MeboyaAinda não há avaliações
- Understanding Eating DisordersDocumento10 páginasUnderstanding Eating DisorderspuchioAinda não há avaliações
- Internship Project Presentation - FinalDocumento18 páginasInternship Project Presentation - Finalapi-496055759Ainda não há avaliações
- Alcoholism Care PlanDocumento11 páginasAlcoholism Care Planilakkiya ilakkiyaAinda não há avaliações
- An Evaluation of The Applicability of The Tripartite Constructs To Social Anxiety in Adolescents Emily R. AndersonDocumento14 páginasAn Evaluation of The Applicability of The Tripartite Constructs To Social Anxiety in Adolescents Emily R. AndersonTripartite-ModelAinda não há avaliações
- Youth SuicideDocumento16 páginasYouth SuicideMohammedAhmedRazaAinda não há avaliações
- Comorbid Anxiety and Depression - Epidemiology, Clinical Manifestations, and Diagnosis PDFDocumento24 páginasComorbid Anxiety and Depression - Epidemiology, Clinical Manifestations, and Diagnosis PDFdreaming0% (1)
- Motivation: Add Keyword Search CPC Competition Search (Global) CPC (Global) Competition (Global)Documento2 páginasMotivation: Add Keyword Search CPC Competition Search (Global) CPC (Global) Competition (Global)hijas muhammedAinda não há avaliações
- Cognitive Behavioral Play Therapy Play Therapy: Why Learn More About CBT?Documento47 páginasCognitive Behavioral Play Therapy Play Therapy: Why Learn More About CBT?Anita Di Frangia100% (1)
- Assessment, Depersonalization, TDocumento3 páginasAssessment, Depersonalization, TsunkissedchiffonAinda não há avaliações
- 34 Jan 2011 PDFDocumento136 páginas34 Jan 2011 PDFNikita JoshiAinda não há avaliações
- Navigating The Space Between Brilliance and MadnessDocumento85 páginasNavigating The Space Between Brilliance and Madnessmirandota100% (1)
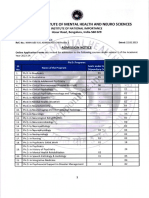
- NIMHANS MPHIL, PHD APPLICATION NOTIFICATION - PeppGuideDocumento6 páginasNIMHANS MPHIL, PHD APPLICATION NOTIFICATION - PeppGuideswathy sudheerAinda não há avaliações
- Anorexia Integrated TreatmentDocumento6 páginasAnorexia Integrated Treatmentmadequal2658Ainda não há avaliações
- Psychogenic Pain and Aggression: The Syndrome of The Solitary HunterDocumento11 páginasPsychogenic Pain and Aggression: The Syndrome of The Solitary HunterHikmat SatriaAinda não há avaliações
- List of Mental Health Practitioners For Young Adults at Nominal Fee/Free. Created by Mahima Kukreja. LGBTQ+ Friendly.Documento8 páginasList of Mental Health Practitioners For Young Adults at Nominal Fee/Free. Created by Mahima Kukreja. LGBTQ+ Friendly.Rahul SuhalkaAinda não há avaliações
- Review Test For Final Exam PSY 250 Abnormal PsychologyDocumento11 páginasReview Test For Final Exam PSY 250 Abnormal PsychologyJen CalaquiAinda não há avaliações
- Bipolar Spectrum Screening Quiz: The Goldberg Bipolar Screening QuestionnaireDocumento3 páginasBipolar Spectrum Screening Quiz: The Goldberg Bipolar Screening QuestionnaireIñaki Garmendia100% (1)