Escolar Documentos
Profissional Documentos
Cultura Documentos
Ebp Poster
Enviado por
api-2835405940 notas0% acharam este documento útil (0 voto)
40 visualizações1 páginaHistorically, nurses have provided change of shift reports to the oncoming shift at nurses stations or secluded rooms away from the patients. Specific patient problems that are often overlooked include assessments such as specific wound observation, IV sites, or fluids. Non bed side reports were noted to be around 35-40 minutes in length on average, interrupted and disorganized.
Descrição original:
Título original
ebp poster (1)
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PPT, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoHistorically, nurses have provided change of shift reports to the oncoming shift at nurses stations or secluded rooms away from the patients. Specific patient problems that are often overlooked include assessments such as specific wound observation, IV sites, or fluids. Non bed side reports were noted to be around 35-40 minutes in length on average, interrupted and disorganized.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
40 visualizações1 páginaEbp Poster
Enviado por
api-283540594Historically, nurses have provided change of shift reports to the oncoming shift at nurses stations or secluded rooms away from the patients. Specific patient problems that are often overlooked include assessments such as specific wound observation, IV sites, or fluids. Non bed side reports were noted to be around 35-40 minutes in length on average, interrupted and disorganized.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
Você está na página 1de 1
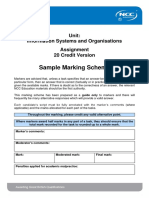
Increasing Patient Satisfaction and Safety Through Bed Side Reporting
Jodie Gayton, RN Heather McLemore, RN Kateri Pletcher, RN
Statement of the Problem
Historically, nurses have provided change of shift reports to the
oncoming shift at nurses stations or secluded rooms away from the
patients. Little to no patient or family involvement in patient plan of
care during shift change allows for potential gaps in care. Specific
patient problems that are often overlooked include assessments such
as specific wound observation, IV sites, or fluids. Sentinel events such
as falls or rapid condition changes are more likely to occur during
change of shift. Standardization of information provided is not widely
used during reporting and as a result important information can be
overlooked.
The Joint Commissions 2009 and 2010 National Patient Safety Goals
included a requirement to encourage patients to be involved actively in
their care and to implement a standardized handoff communication
process when a change of care providers occurs.
Presentation and critical appraisal of the
evidence
Non bed side reports were noted to be around 35-40 minutes in
length on average, interrupted and disorganized.
Often reports on all patients were given to all nurses in a group
setting.
Surveys that were used in studies: retrospective and prospective.
Likert scales were implemented in surveys.
Surveys and studies were approved by institutional review boards.
Data was analyzed by statisticians and appropriate software.
SBART (Situation, Background, Assessment, Recommendations,
Thanks).
Clinical Question
Does implementing bedside shift reports lead to greater patient
satisfaction with care when compared to traditional shift change
reports at the nurses station?
Suggestions for Future Research
Additional randomized controlled trials.
Meta-analysis of literature.
Further research on pediatric floors.
Standardized report formats for all department types.
Research for optimal ways to wake up patient/family.
Post implementation studies to evaluate continued
effectiveness over several years.
Effective and success program modifications.
Training seminars on management of the implementation.
Appropriate training durations prior to implementation.
Search for Evidence
Studies and research on this topic were located through CINHAL.
The articles were searched for using these terms: bedside
reporting and shift reporting. Results were limited to the last 5 to 10
years. A combinations of 22 research articles, reports and pilot
studies were selected for review. References from articles were
also used to locate and select additional literature. Research
literature covered various nursing practices ranging from pediatrics,
medical/ surgical units, telemetry/cardiology units, mother/baby
units and birthing centers.
Clinical Practice Implications
Promotes patient safety by ensuring bed alarms, bed rails, call
lights, in place, patients are seen sooner.
Timely interventions during shift change especially for rapid
changes in condition, reducing potential sentinel events and
perception that no one is around during shift change.
Provides an opportunity for patients/family to meet oncoming staff,
to ask questions, receive clarification, collaborate and participate in
their plan of care, and correct inaccuracies.
Patients report higher satisfaction ratings that translates into loyal
customers who are more likely to return for follow-up care and
services and evidence shows they are less likely to litigate.
Decreases patient/family anxiety.
Sensitive issues can be handled outside the room prior to entering.
Avoids subjective discussions, chit chat/social time and promotes
staff accountability by visualizing the room and ensuring certain tasks
are completed rather than discovering issues after prior shift has left.
Decreased medication errors by reviewing prior shift medications
and allergies in room.
Nurses report higher satisfaction with reporting, ability to leave on
time resulting in financial savings in terms of overtime since time
spent in report decreases to 2-7 minutes per patient (acuity
dependent).
Provides oncoming nurses faster patient recognition and ability to
prioritize care earlier.
Doctors report satisfaction with nurses able to answer questions
sooner.
Uses a standardized form to communicate such as SBART.
Você também pode gostar
- Comprehensive Discharge Planning-Ebp PowerpointDocumento45 páginasComprehensive Discharge Planning-Ebp Powerpointapi-24187790Ainda não há avaliações
- Managing Change Towards Bedside Shift ReportDocumento12 páginasManaging Change Towards Bedside Shift Reportapi-438607141Ainda não há avaliações
- Komunikasi Efektif Dan Keselamatan Pasien - Bahan Bu TikaDocumento44 páginasKomunikasi Efektif Dan Keselamatan Pasien - Bahan Bu TikaZara Yuliani PutriAinda não há avaliações
- Transitions of CareDocumento3 páginasTransitions of Caredelap05Ainda não há avaliações
- NUR4103 Communication Skills For Nurses-2Documento17 páginasNUR4103 Communication Skills For Nurses-2debbiekissoon1Ainda não há avaliações
- Relationshipbasedcarepaper - NSG 4040-1Documento13 páginasRelationshipbasedcarepaper - NSG 4040-1api-314231356Ainda não há avaliações
- Improving Bedside Shift-To-shift Nursing Report ProcessDocumento34 páginasImproving Bedside Shift-To-shift Nursing Report ProcessJaypee Fabros Edra100% (2)
- Strategies To Improve Handoff CommunicationDocumento2 páginasStrategies To Improve Handoff CommunicationJames SimmonsAinda não há avaliações
- Nursing ReportDocumento25 páginasNursing ReportikaverayantiAinda não há avaliações
- Icu InnovationDocumento5 páginasIcu InnovationAmber ThompsonAinda não há avaliações
- Nursing Report: By: Ni Luh Putri Rahayu (18.321.2895) A12-BDocumento25 páginasNursing Report: By: Ni Luh Putri Rahayu (18.321.2895) A12-Bputri rahayuAinda não há avaliações
- Nurse Case StudyDocumento6 páginasNurse Case Studyprateeksha16Ainda não há avaliações
- Managing Patient Expectations at Emergency Department TriageDocumento15 páginasManaging Patient Expectations at Emergency Department TriageHans GrobakAinda não há avaliações
- Evidence Based Standards For Measuring Nurse Staffing and PerformanceDocumento208 páginasEvidence Based Standards For Measuring Nurse Staffing and Performancemr_jamzAinda não há avaliações
- The Role of Nurse Practitioners in Care Coordination and TransitionDocumento10 páginasThe Role of Nurse Practitioners in Care Coordination and Transitionapi-312364579Ainda não há avaliações
- Nursng ReportDocumento19 páginasNursng ReportNgurahAinda não há avaliações
- Leadership AnalysisDocumento8 páginasLeadership Analysisapi-260554694Ainda não há avaliações
- Research ForumDocumento34 páginasResearch ForumJustine May GervacioAinda não há avaliações
- Evidence Based Standards For Measuring Nurse Staffing and PerformanceDocumento208 páginasEvidence Based Standards For Measuring Nurse Staffing and PerformanceA As'ad MaoAinda não há avaliações
- Journal Article Critique Nursing 665Documento5 páginasJournal Article Critique Nursing 665api-214213767Ainda não há avaliações
- The COAT & Review Approach: How to recognise and manage unwell patientsNo EverandThe COAT & Review Approach: How to recognise and manage unwell patientsNota: 5 de 5 estrelas5/5 (1)
- Unit 4 Assessment: Literature ReviewDocumento5 páginasUnit 4 Assessment: Literature Reviewyetunde badruAinda não há avaliações
- Question of Acute CareDocumento11 páginasQuestion of Acute CareKuberAiranAinda não há avaliações
- 1.1 Background Nursing Documentation Is The Record of Nursing Care That Is Planned and Delivered ToDocumento13 páginas1.1 Background Nursing Documentation Is The Record of Nursing Care That Is Planned and Delivered Toari cendani prabawatiAinda não há avaliações
- Patients' Waiting Time: Indices For Measuring Hospital EffectivenessDocumento18 páginasPatients' Waiting Time: Indices For Measuring Hospital Effectivenessmr kevinAinda não há avaliações
- Documentation: Siji M. SunnyDocumento5 páginasDocumentation: Siji M. SunnySUNNY__SIJIAinda não há avaliações
- Nur 410 Bedside Shift ReportDocumento8 páginasNur 410 Bedside Shift Reportapi-448827323Ainda não há avaliações
- Physical Therapist As Patient ManagerDocumento25 páginasPhysical Therapist As Patient ManagerUmer QureshiAinda não há avaliações
- Nur Final PaperDocumento9 páginasNur Final Paperapi-404050277Ainda não há avaliações
- Using Client Outcome Monitoring As A Tool For SupervisionDocumento5 páginasUsing Client Outcome Monitoring As A Tool For SupervisionDianaSantiago100% (1)
- Application Project - Team 11Documento30 páginasApplication Project - Team 11api-601587526Ainda não há avaliações
- Documentation, Nursing Rounds, Manual & ProtocolDocumento22 páginasDocumentation, Nursing Rounds, Manual & ProtocolSUNNY__SIJIAinda não há avaliações
- Nurse Change-Of-Shift Report PolicyDocumento2 páginasNurse Change-Of-Shift Report Policyapi-235633705Ainda não há avaliações
- Quality and Synthesis PaperDocumento6 páginasQuality and Synthesis Paperapi-253093073Ainda não há avaliações
- Diabetes Mellitus Autoimmune Insulin Beta Cells Pancreas Polyuria Polydipsia PolyphagiaDocumento37 páginasDiabetes Mellitus Autoimmune Insulin Beta Cells Pancreas Polyuria Polydipsia PolyphagiaVishuAinda não há avaliações
- Final Revised!!!!!!Documento44 páginasFinal Revised!!!!!!Far Daurong100% (1)
- Evidenced Based Nursing PracticeDocumento7 páginasEvidenced Based Nursing PracticeKim ViñasAinda não há avaliações
- Hourly Rounding and The Effects On Patient Safety and Satisfaction ArtifactDocumento29 páginasHourly Rounding and The Effects On Patient Safety and Satisfaction Artifactapi-310375757Ainda não há avaliações
- Quality and Safety Synthesis PaperDocumento6 páginasQuality and Safety Synthesis Paperapi-252807964Ainda não há avaliações
- Nursing DiagnosisDocumento38 páginasNursing DiagnosisJR Rolf NeuqeletAinda não há avaliações
- Handing and Taking OverDocumento6 páginasHanding and Taking OverRuthraaadi Rameshkumar75% (4)
- Canadian Triage Acuity Scale (CTAS)Documento32 páginasCanadian Triage Acuity Scale (CTAS)Ciecilia Stefanny Sistandria Mahesta100% (3)
- Tammy Tarner Journal Club EntryDocumento1 páginaTammy Tarner Journal Club Entryapi-357707616Ainda não há avaliações
- Open VsDocumento16 páginasOpen Vsapi-482726932Ainda não há avaliações
- CQI by CommitteeDocumento6 páginasCQI by CommitteeJhOy XiAinda não há avaliações
- Quality Improvement Proposal PaperDocumento7 páginasQuality Improvement Proposal Paperapi-533686691Ainda não há avaliações
- Psychology and Health Notes - CIE Psychology A-LevelDocumento18 páginasPsychology and Health Notes - CIE Psychology A-LevelRajasekar KrishnasamyAinda não há avaliações
- Running Head: Reflection in Nursing 1Documento21 páginasRunning Head: Reflection in Nursing 1joseeAinda não há avaliações
- Final Paper Nur410Documento10 páginasFinal Paper Nur410api-598929897Ainda não há avaliações
- Capstone Scholarly PaperDocumento5 páginasCapstone Scholarly Paperapi-592369059Ainda não há avaliações
- He U.S. Hospital System Suffers From ShortfallsDocumento8 páginasHe U.S. Hospital System Suffers From Shortfallsjoy gorreAinda não há avaliações
- ResearchDocumento6 páginasResearchKrishoban BaskaranAinda não há avaliações
- The Maximally Efficient and Optimally Effective Emergency Department: One Good Thing A DayNo EverandThe Maximally Efficient and Optimally Effective Emergency Department: One Good Thing A DayAinda não há avaliações
- Medical Home: Care Coordination: The Patient-CenteredDocumento23 páginasMedical Home: Care Coordination: The Patient-CenteredDwi Suranto100% (1)
- Baccountingackground Researc1Documento6 páginasBaccountingackground Researc1Noor Ul AinAinda não há avaliações
- Nursing AssessmentDocumento28 páginasNursing AssessmentKierstine Joy YamatAinda não há avaliações
- A Study of Proactive Ethics Consultation For CriticallyDocumento18 páginasA Study of Proactive Ethics Consultation For CriticallyJENIFER KARINA PUTZ LORENZIAinda não há avaliações
- Data Makes the Difference: The Smart Nurse's Handbook for Using Data to Improve CareNo EverandData Makes the Difference: The Smart Nurse's Handbook for Using Data to Improve CareAinda não há avaliações
- Group 4 - Team B - Health DiagnosticsDocumento9 páginasGroup 4 - Team B - Health DiagnosticsVihang VasaAinda não há avaliações
- The Positive Impact of Continuous ImprovementDocumento15 páginasThe Positive Impact of Continuous ImprovementMane DaralAinda não há avaliações
- BMG 871Documento9 páginasBMG 871omotola52paseAinda não há avaliações
- Six Sigma QuizDocumento37 páginasSix Sigma QuizSSH11Ainda não há avaliações
- Questionnaire DesignDocumento18 páginasQuestionnaire DesignRohan Purohit100% (1)
- FINAL ANG VN Dossiers Conf EnglishDocumento196 páginasFINAL ANG VN Dossiers Conf Englishlangtu_sitinh_902002Ainda não há avaliações
- Discussion For Bradford AssayDocumento2 páginasDiscussion For Bradford Assayniewaznekto100% (2)
- 2nd Quarter Exam PRactical Research 2Documento3 páginas2nd Quarter Exam PRactical Research 2Geraldine LauronAinda não há avaliações
- 21st Century Skills ReportDocumento20 páginas21st Century Skills Reportapi-396616332Ainda não há avaliações
- Statistics and Standard DeviationDocumento50 páginasStatistics and Standard DeviationRon April Custodio Frias100% (10)
- Champy LLLDocumento25 páginasChampy LLLandi arfandiAinda não há avaliações
- Ancient Engineering: Selective Ceramic Processing in The Middle Balsas Region of Guerrero, Mexico.Documento370 páginasAncient Engineering: Selective Ceramic Processing in The Middle Balsas Region of Guerrero, Mexico.Citlalii BaronAinda não há avaliações
- Daing DissertationDocumento73 páginasDaing DissertationJesusima Bayeta AlbiaAinda não há avaliações
- 06 L5DB Information Systems and Organisations ISO Sample Assignment MSDocumento8 páginas06 L5DB Information Systems and Organisations ISO Sample Assignment MSpreeyalAinda não há avaliações
- GEC 112 Module 3, Lesson 5Documento10 páginasGEC 112 Module 3, Lesson 5James PotenteAinda não há avaliações
- Policy Analysis: A Systematic Approach To Supporting Policymaking in The Public SectorDocumento18 páginasPolicy Analysis: A Systematic Approach To Supporting Policymaking in The Public SectorBereket DesalegnAinda não há avaliações
- Ankush Project Report MDRADocumento60 páginasAnkush Project Report MDRAKrishna GoelAinda não há avaliações
- Mba HRM Dissertation TopicsDocumento6 páginasMba HRM Dissertation TopicsPaySomeoneToWriteAPaperForMeCanada100% (1)
- BeaconhandbookDocumento30 páginasBeaconhandbookchris husonAinda não há avaliações
- LESSON - Literature & Statement of The ProblemDocumento13 páginasLESSON - Literature & Statement of The ProblemHomer Kurt BugtongAinda não há avaliações
- Community Assessment of Police Practices Community Satisfaction SurveyDocumento86 páginasCommunity Assessment of Police Practices Community Satisfaction SurveyTorontoistAinda não há avaliações
- Master Thesis In-Depth InterviewsDocumento5 páginasMaster Thesis In-Depth Interviewsrqopqlvcf100% (1)
- NegOr Q3 EAPP Module7 v2Documento27 páginasNegOr Q3 EAPP Module7 v2Cyrah BrionAinda não há avaliações
- Nps Thesis DatabaseDocumento5 páginasNps Thesis Databasekathymillerminneapolis100% (2)
- Rajiv Gandhi University of Health Sciences, Karnataka, Bangalore Annexure - Ii Name of The Candidate and Address (In Block Letters)Documento18 páginasRajiv Gandhi University of Health Sciences, Karnataka, Bangalore Annexure - Ii Name of The Candidate and Address (In Block Letters)subiAinda não há avaliações
- Sto. Niño National High School: Background of The StudyDocumento27 páginasSto. Niño National High School: Background of The StudyKyran LisacaAinda não há avaliações
- Research 3 Quarter 3 - MELC 1 Week 1-2 Inferential StatisticsDocumento39 páginasResearch 3 Quarter 3 - MELC 1 Week 1-2 Inferential StatisticsHanna nicole JapsayAinda não há avaliações
- BIblio GuidelinesDocumento4 páginasBIblio GuidelinesR-Chian Jose GermanpAinda não há avaliações
- Generative Phonology D Kumpulkan Hari IniDocumento6 páginasGenerative Phonology D Kumpulkan Hari IniMidori MakibouAinda não há avaliações
- Chapter 3 and 4 Research PaperDocumento21 páginasChapter 3 and 4 Research PaperEva Lumanta100% (3)
- Is 9214 1979Documento25 páginasIs 9214 1979Hajarath Prasad AbburuAinda não há avaliações
- Fet 500 TheodoliteDocumento2 páginasFet 500 TheodoliteSony Zebua100% (1)