Escolar Documentos
Profissional Documentos
Cultura Documentos
Celiac Adime Final
Enviado por
api-287759747Descrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Celiac Adime Final
Enviado por
api-287759747Direitos autorais:
Formatos disponíveis
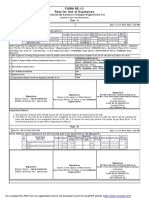
ADIME
Celiac
Disease
Date
Pertinent
information
provided
by
patient
Age; Gender; Dx; PMH
Ht; Wt; UBW/%UBW;
IBW; %IBW; BMI
Assessment
Labs
Positive test for:
TTG (indicator of Celiac disease)
EMA antibodies antiendomysial (indicator of Celiac disease)
Meds
GI
I/O
Physical Assessment
Skin
EER; EPR;
Fluid requirements
Current
Diet
PES
#1
Diagnosis
May 27, 2015
Patient states she is hungry all of the time and when she eats (especially large amounts) she
usually has immediate diarrhea. Patient states when eating fried foods or beef her diarrhea
worsens. She does not claim to be vomiting or nausea.
Age: KM 36 yo, female
Diet history: Patient states she eats noodle soups, chicken, crackers, sprite, fried foods, and beef.
Admitting diagnosis: celiac disease
Malabsorption; anemia
Height: 53; 160 cm.
Current Weight: 92 lbs 41.8 kg (82% of UBW; 80% of IBW)
UBW: 112 lbs (1 month ago) 50.9 kg
18% weight loss in 1 month; severe weight loss
IBW: 115 lbs 52.3 kg
BMI: 16.3 Underweight
Albumin 2.9g/dL (low)
Prealbumin 14mg/dL (low)
Hgb 10.5 g/dL (low)
Hct 35% (low)
Ferritin 12 micrograms/dL (low)
PES #2
NA
Bowel biopsy results: flat mucosa, villus atrophy, and hyperplastic crypts-inflammatory infiltrate
in lamina propia.
NPO
NA
NA
EER: 1,569 kcal/day (based on 30kcal/kg of IBW
Protein: 41 g/day (.8g/kg based on IBW)
Fluid: 1,500 ml (1ml/kcal based on EER for IBW)
NPO
AEB
Unintended
R/T
severe
weight
weight
loss
diarrhea
and
loss
of
18%
(20
malabsorption
lbs.
of
UBW)
in
1
month.
AEB
Impaired
Low
ferritin
(12
nutrient
micrograms/dL),
utilization
hemoglobin
R/T
(10.5
g/dL),
and
altered
GI
hematocrit
function
(35%)
levels;
bowel biopsy of
flat mucosa,
villus atrophy,
and hyperplastic
PES #3
Monitoring/
Evaluation
Intervention
Nutrition Prescription
Treatment
plan:
nutrition
therapy,
education,
acquisition
of
additional
information
Plan(s) for evaluating
outcomes of
interventions listed
above; plan for follow-
up
Signature (& name)
cryptsinflammatory
infiltrate in
lamina propia
(damage to
intestinal
mucosa).
AEB
Undesirable
diet
history
of
R/T
food
choices
consuming
foods
knowledge
with
gluten,
deficit
reported
by
patient.
After
approval
of
PO,
recommend/order
gluten-free
and
lactose
free
diet
order
by
avoiding
wheat,
rye,
barley,
malt,
oats,
and
dairy.
Restrict
lactose
(milk
and
dairy)
foods
until
damaged
intestinal
villi
are
regenerated,
and
then
add
lactose
to
diet
as
tolerated.
Increase
caloric
needs
to
2000
per
day
until
IBW
of
115
lbs.
(1-2
lb.
gain
per
week)
is
reached,
then
1500
kcal/day.
Increase
iron
intake
to
18mg/day.
Before
dismissal,
educate
patient
on
foods
with
gluten
and
lactose
by
teaching
her
how
to
read
food
labels
in
order
to
identify
products
with
gluten
and
lactose.
Have
patient
keep
food
diary
and
write
down
any
GI
symptoms
(diarrhea,
nausea,
and
vomiting).
Provide
client
with
iron
rich
food
sources.
In
hospital,
collaborate
with
nursing
unit
to
monitor
weight
gain
and
tolerance
of
foods
with
I/O.
Monitor
intake
with
calorie
count.
Evaluate
change
in
hematocrit,
hemoglobin,
and
ferritin
levels.
After
dismissal,
at
home,
measure
weight
weekly.
Patients
weight
will
stabilize
at
IBW
of
115
lbs.
Check
food
diary
to
determine
compliance
with
gluten-free
diet,
iron
content,
and
daily
kcals.
Have
patient
meet
with
doctor
to
check
for
stable
lab
values
of
hematocrit,
hemoglobin,
and
ferritin.
Liz
Neahring
Você também pode gostar
- Nutr302l NCP NotesDocumento14 páginasNutr302l NCP Notesapi-271284613Ainda não há avaliações
- Adime Malnutrition and OncolgyDocumento6 páginasAdime Malnutrition and Oncolgyapi-300587226100% (1)
- Kidney AdimeDocumento2 páginasKidney Adimeapi-287591907Ainda não há avaliações
- Adime Note GDMDocumento2 páginasAdime Note GDMapi-242547654100% (1)
- 3 Adime Form For Diabete Case 1Documento2 páginas3 Adime Form For Diabete Case 1api-309275032Ainda não há avaliações
- Malnutrition AdimeDocumento2 páginasMalnutrition Adimeapi-508953960Ainda não há avaliações
- Adime For DiabetesDocumento2 páginasAdime For Diabetesapi-383891195Ainda não há avaliações
- Oncology AdimeDocumento2 páginasOncology Adimeapi-299929867Ainda não há avaliações
- Adime HenryDocumento4 páginasAdime Henryapi-486579190Ainda não há avaliações
- Diabetes AdimeDocumento3 páginasDiabetes Adimeapi-330880468100% (3)
- Case Study 11 AdimeDocumento3 páginasCase Study 11 Adimeapi-347141638Ainda não há avaliações
- Adime-Kidney Disease PortfolioDocumento4 páginasAdime-Kidney Disease Portfolioapi-477636568Ainda não há avaliações
- Case Study 31 Adime NoteDocumento3 páginasCase Study 31 Adime Noteapi-533641139Ainda não há avaliações
- Diabetes Mandatory Case Study AdimeDocumento2 páginasDiabetes Mandatory Case Study Adimeapi-434982019Ainda não há avaliações
- Case Study Adime NoteDocumento2 páginasCase Study Adime Noteapi-240616135Ainda não há avaliações
- Ntrs 415a Adime Note 1Documento2 páginasNtrs 415a Adime Note 1api-287590844100% (1)
- Adime Note Allison 2Documento3 páginasAdime Note Allison 2api-457873289Ainda não há avaliações
- Hypertension and Dyslipidemia Case StudyDocumento14 páginasHypertension and Dyslipidemia Case Studyapi-435771794Ainda não há avaliações
- Adime 1Documento1 páginaAdime 1api-308400395Ainda não há avaliações
- Case Study 7 AdimeDocumento2 páginasCase Study 7 Adimeapi-300889147100% (2)
- Cancer Adime NoteDocumento4 páginasCancer Adime Noteapi-299079787Ainda não há avaliações
- Adime 2 UchcDocumento9 páginasAdime 2 Uchcapi-307029735Ainda não há avaliações
- Sample Case StudyDocumento10 páginasSample Case Studyapi-702059884Ainda não há avaliações
- Adime NoteDocumento2 páginasAdime Noteapi-383891195Ainda não há avaliações
- CVD Case StudyDocumento4 páginasCVD Case Studyapi-435010651Ainda não há avaliações
- 4 Diabetes Nutrition Care PlanDocumento5 páginas4 Diabetes Nutrition Care Planapi-309275032Ainda não há avaliações
- Malnutrition Case Study-2Documento5 páginasMalnutrition Case Study-2dakota100% (1)
- Case Study OutlineDocumento3 páginasCase Study OutlineExcel MarieAinda não há avaliações
- Adime NoteDocumento3 páginasAdime Noteapi-298471603100% (2)
- ADIME+Example 2Documento3 páginasADIME+Example 2schmekshy1Ainda não há avaliações
- Clinical Case Studies DiabetesDocumento8 páginasClinical Case Studies Diabetesapi-434982019Ainda não há avaliações
- Ncma215 Course Task 5Documento2 páginasNcma215 Course Task 5AngelaAinda não há avaliações
- PRESENTE AdolescentDocumento2 páginasPRESENTE AdolescentKasangga IsaganiAinda não há avaliações
- Porter Obesity Adime 2Documento3 páginasPorter Obesity Adime 2api-538657643Ainda não há avaliações
- Nutrition ReviewDocumento23 páginasNutrition ReviewMonice Robinson Williams0% (2)
- Adime 4Documento9 páginasAdime 4api-253944123100% (2)
- Case Study About Type II Diabetes MellitusDocumento82 páginasCase Study About Type II Diabetes MellitusKristine YoungAinda não há avaliações
- NCMA 215 Dysphagia Nursing Care PlanDocumento2 páginasNCMA 215 Dysphagia Nursing Care PlanGina PrancelisoAinda não há avaliações
- Final Adime Note AnemiacasestudyDocumento2 páginasFinal Adime Note Anemiacasestudyapi-253526841Ainda não há avaliações
- Dietary TherapyDocumento48 páginasDietary TherapyVanetAinda não há avaliações
- Definition of Modified DietDocumento20 páginasDefinition of Modified Dietmisbah67% (3)
- Case Study QuestionDocumento16 páginasCase Study QuestionLloyd The UnicornAinda não há avaliações
- 5 NFSC 470 - Case Study Adime Note Celiac DiseaseDocumento2 páginas5 NFSC 470 - Case Study Adime Note Celiac Diseaseapi-242530221Ainda não há avaliações
- Adime AssessmentDocumento3 páginasAdime Assessmentapi-302346627Ainda não há avaliações
- Imbalanced NutritionDocumento2 páginasImbalanced NutritionRizza 이 동해 Ocampo100% (1)
- Nutrition Care PlanDocumento6 páginasNutrition Care Planapi-340025372Ainda não há avaliações
- Nutr 510 - Counseling Session 2Documento4 páginasNutr 510 - Counseling Session 2api-240740872Ainda não há avaliações
- Adime 3Documento9 páginasAdime 3api-279537861Ainda não há avaliações
- Nutrition Support in Severe Sepsis and Morbid ObesityDocumento6 páginasNutrition Support in Severe Sepsis and Morbid ObesitydakotaAinda não há avaliações
- Adime RenalDocumento3 páginasAdime Renalapi-508953960Ainda não há avaliações
- Adime 2 UchcDocumento11 páginasAdime 2 Uchcapi-307103979100% (1)
- Young and Middle Adulthood Nutrition ReportDocumento50 páginasYoung and Middle Adulthood Nutrition ReportFabby Vitacion TanAinda não há avaliações
- Nutrition Guidelines for Chronic DiseasesDocumento59 páginasNutrition Guidelines for Chronic DiseasesPattAinda não há avaliações
- Tube Feeding Worksheet #1: 2040 835/1000 1703.4 ML of Free WaterDocumento6 páginasTube Feeding Worksheet #1: 2040 835/1000 1703.4 ML of Free WaterLatifah AlsahaleyAinda não há avaliações
- Malnutriton Case StudyDocumento4 páginasMalnutriton Case Studyapi-302848761Ainda não há avaliações
- Case Study For DMDocumento5 páginasCase Study For DMJermeLou Bao100% (1)
- Nutrition Care Process and ModelDocumento82 páginasNutrition Care Process and ModelNoci M. FrenkAinda não há avaliações
- Nutrition Therapy For Renal Disorders Case QuestionsDocumento9 páginasNutrition Therapy For Renal Disorders Case QuestionspeytonAinda não há avaliações
- Adime Lgi PDFDocumento3 páginasAdime Lgi PDFapi-2802318020% (1)
- Fiber Handout EnglishDocumento3 páginasFiber Handout Englishapi-287759747Ainda não há avaliações
- Parkinsons Presentation Case StudyDocumento33 páginasParkinsons Presentation Case Studyapi-287759747Ainda não há avaliações
- 410 ResearchfinalpaperDocumento52 páginas410 Researchfinalpaperapi-287759747Ainda não há avaliações
- Sodexo ResumeDocumento2 páginasSodexo Resumeapi-287759747Ainda não há avaliações
- Annamalai International Journal of Business Studies and Research AijbsrDocumento2 páginasAnnamalai International Journal of Business Studies and Research AijbsrNisha NishaAinda não há avaliações
- Casting Procedures and Defects GuideDocumento91 páginasCasting Procedures and Defects GuideJitender Reddy0% (1)
- Multiple Choice: CH142 Sample Exam 2 QuestionsDocumento12 páginasMultiple Choice: CH142 Sample Exam 2 QuestionsRiky GunawanAinda não há avaliações
- Level 3 Repair PBA Parts LayoutDocumento32 páginasLevel 3 Repair PBA Parts LayoutabivecueAinda não há avaliações
- 2nd Pornhub Awards - WikipediaaDocumento13 páginas2nd Pornhub Awards - WikipediaaParam SinghAinda não há avaliações
- Unit 1 - Gear Manufacturing ProcessDocumento54 páginasUnit 1 - Gear Manufacturing ProcessAkash DivateAinda não há avaliações
- Inorganica Chimica Acta: Research PaperDocumento14 páginasInorganica Chimica Acta: Research PaperRuan ReisAinda não há avaliações
- The European Journal of Applied Economics - Vol. 16 #2Documento180 páginasThe European Journal of Applied Economics - Vol. 16 #2Aleksandar MihajlovićAinda não há avaliações
- Customer Perceptions of Service: Mcgraw-Hill/IrwinDocumento27 páginasCustomer Perceptions of Service: Mcgraw-Hill/IrwinKoshiha LalAinda não há avaliações
- Social Media Exposure and Its Perceived Impact On Students' Home-Based Tasks ProductivityDocumento9 páginasSocial Media Exposure and Its Perceived Impact On Students' Home-Based Tasks ProductivityJewel PascuaAinda não há avaliações
- QuickTransit SSLI Release Notes 1.1Documento12 páginasQuickTransit SSLI Release Notes 1.1subhrajitm47Ainda não há avaliações
- Obstetrical Hemorrhage: Reynold John D. ValenciaDocumento82 páginasObstetrical Hemorrhage: Reynold John D. ValenciaReynold John ValenciaAinda não há avaliações
- Bluetooth TutorialDocumento349 páginasBluetooth Tutorialjohn bougsAinda não há avaliações
- LM1011 Global ReverseLogDocumento4 páginasLM1011 Global ReverseLogJustinus HerdianAinda não há avaliações
- PESO Online Explosives-Returns SystemDocumento1 páginaPESO Online Explosives-Returns Systemgirinandini0% (1)
- Udaan: Under The Guidance of Prof - Viswanathan Venkateswaran Submitted By, Benila PaulDocumento22 páginasUdaan: Under The Guidance of Prof - Viswanathan Venkateswaran Submitted By, Benila PaulBenila Paul100% (2)
- FSRH Ukmec Summary September 2019Documento11 páginasFSRH Ukmec Summary September 2019Kiran JayaprakashAinda não há avaliações
- AATCC 100-2004 Assesment of Antibacterial Dinishes On Textile MaterialsDocumento3 páginasAATCC 100-2004 Assesment of Antibacterial Dinishes On Textile MaterialsAdrian CAinda não há avaliações
- 5054 w11 QP 11Documento20 páginas5054 w11 QP 11mstudy123456Ainda não há avaliações
- GMWIN SoftwareDocumento1 páginaGMWIN SoftwareĐào Đình NamAinda não há avaliações
- 2014 mlc703 AssignmentDocumento6 páginas2014 mlc703 AssignmentToral ShahAinda não há avaliações
- Orc & Goblins VII - 2000pts - New ABDocumento1 páginaOrc & Goblins VII - 2000pts - New ABDave KnattAinda não há avaliações
- Case 5Documento1 páginaCase 5Czan ShakyaAinda não há avaliações
- India: Kerala Sustainable Urban Development Project (KSUDP)Documento28 páginasIndia: Kerala Sustainable Urban Development Project (KSUDP)ADBGADAinda não há avaliações
- Energy AnalysisDocumento30 páginasEnergy Analysisca275000Ainda não há avaliações
- Unit-1: Introduction: Question BankDocumento12 páginasUnit-1: Introduction: Question BankAmit BharadwajAinda não há avaliações
- Pita Cyrel R. Activity 7Documento5 páginasPita Cyrel R. Activity 7Lucky Lynn AbreraAinda não há avaliações
- 08 Sepam - Understand Sepam Control LogicDocumento20 páginas08 Sepam - Understand Sepam Control LogicThức Võ100% (1)
- Photographing Shadow and Light by Joey L. - ExcerptDocumento9 páginasPhotographing Shadow and Light by Joey L. - ExcerptCrown Publishing Group75% (4)
- Archlinux 之 之 之 之 Lmap 攻 略 ( 攻 略 ( 攻 略 ( 攻 略 ( 1 、 环 境 准 备 ) 、 环 境 准 备 ) 、 环 境 准 备 ) 、 环 境 准 备 )Documento16 páginasArchlinux 之 之 之 之 Lmap 攻 略 ( 攻 略 ( 攻 略 ( 攻 略 ( 1 、 环 境 准 备 ) 、 环 境 准 备 ) 、 环 境 准 备 ) 、 环 境 准 备 )Goh Ka WeeAinda não há avaliações