Escolar Documentos
Profissional Documentos
Cultura Documentos
Disabilities Modalities and Activity Paper
Enviado por
api-293515530Descrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Disabilities Modalities and Activity Paper
Enviado por
api-293515530Direitos autorais:
Formatos disponíveis
Running head: DISABILITIES, MODALITIES AND ACTIVITIES
Disabilities, Modalities and Activity Adaptations Assignment Paper
Soraya Russell
Florida International University
LEI 3703
DISABILITIES, MODALITIES AND ACTIVITIES
Disabilities, Modalities and Activity Adaptations Assignment Paper
With the prevalence of different disabilities in the world today, it is important to have an
understanding of what they are and how they affect people. The categories of disabilities include
developmental, cognitive, psychological, orthopedic, neurological, sensory, and social
impairments. The two disabilities discussed in this paper fall into the categories of
developmental and neurological impairments; they are autism and multiple sclerosis. Also,
discussed are the modalities and activity adaptions associated with these.
Disabling Condition Description
Autism and Autism Spectrum Disorder (ASD) are general terms for a complex group of
disorders in brain development. ASDs are developmental disabilities that cause significant
challenges in social, communication and behavioral abilities (Center for Disease Control [CDC],
2015). The associated disorders are autistic disorder, childhood disintegrative disorder, pervasive
developmental disorder-not otherwise specified (PDD-NOS) and Asperger syndrome. Previously
these were identified as distinct subtypes; however, with the release of the Diagnostic and
Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) all autism disorders were merged
under one diagnostic umbrella term called ASD (Autism Speaks, 2015).
People with ASD often do not look different than other people, but may communicate,
interact, behave, and learn in different ways from most. The thinking, learning, and problemsolving abilities can range from gifted to severely challenged. Some with ASD need considerable
help with daily activities; others need less (CDC, 2015). According to Foose and Ardovino
(2007), Specific characteristics include lack of social or emotional reciprocity, stereotyped or
repetitive motions, and lack of varied or spontaneous make-believe play (p. 137).
DISABILITIES, MODALITIES AND ACTIVITIES
These symptoms may range from mild to severe forms involving communication
problems, unusual play with toys or other objects, difficulty with changes in routine or
surroundings, and unusual responses to noises and lights (i.e., sensory integration) (Foose &
Ardovino, 2007). While most people associate autism with an intellectual disability, not all
persons with autism have limited intellectual capacity. Some have a very high IQ and even excel
in art, music and math. These were previously considered as having high-functioning autism
(Autism Speaks, 2015).
The prevalence of autism has greatly increased over the years. As of February 2015,
about 1 in 68 children has been identified with ASD. It occurs in all racial, ethnic, and
socioeconomic groups and is almost 5 times more common among boys (1 in 42) than among
girls (1 in 189) (CDC, 2015). Almost half the children identified with ASD have an average to
above average intellect (CDC, 2015).
For many years the cause of autism was unknown, but advanced research has provided
possible causes. Most scientists agree genes are one factor making a person more likely to
develop ASD. Children with Down syndrome, fragile X syndrome, tuberous sclerosis, or other
genetic and chromosomal are more at risk for developing ASD (CDC, 2015). Having a sibling
with ASD also puts one at higher risk. Children conceived by older parents, maternal illness
during pregnancy and difficulties with oxygen deprivation to the babys brain at birth are also
factors (Autism Speaks, 2015).
Because autism primarily affects an individuals social and verbal communication skills,
it can result in a wide range of secondary conditions. These can include social impairment,
speech and language difficulties, attention disorders, gross and fine motor skill impairments,
deficits in sensory processing, anxiety and depression, and epilepsy (Swann-Guerrero & Mackey,
DISABILITIES, MODALITIES AND ACTIVITIES
2007). Foose and Ardovino (2007) stated, 25% to 33% of people with autism have epileptic
seizures (p.137). It is important to note which secondary condition(s) affect the client especially
if they are prone to having seizures.
Because no child with autism has the exact same limitations and strengths as another, as a
Certified Therapeutic Recreation Specialist (CTRS), it is essential to assess the client. However,
it is safe to say that most people with autism have significant social impairment. Children can
often suffer in school because of this. This is where recreational therapy services would be of
useful. A CTRS would benefit from including a child with autism with those who do not have
disabilities so as to provide a model of appropriate behavior.
Recreational Therapy (RT) Modalities
Williams (2007) described the term treatment modality as recreation or other activities
used to help clients meet therapeutic goals (p. 70). A review of the modalities specific to the
clients needs must be considered. A comprehensive understanding of these needs and interest are
critical to the overall success of the intervention. Since children with autism usually have
restricted interests, a major goal of a CTRS is to expand their recreational therapy
services/modalities. Some of these modalities include: music therapy, aquatic therapy, play
therapy, animal assisted therapy, and exercise.
Music therapy involves the study and use of music through singing, playing and listening
to assist with the individuals physical, cognitive, emotional, and social needs. It can promote
communication, emotional health and expression in addition to memory retention (Dattilo &
McKenney, 2011). Aquatic therapy includes passive or active water exercises and swimming. It
is intended to provide physical and psychological benefits, while encouraging individuals to
achieve independent leisure participation as well (Dattilo & McKenney, 2011).
DISABILITIES, MODALITIES AND ACTIVITIES
Play therapy is a technique that allows a child to naturally express their feelings and
thinking through play while improving cognition, social and physical skills. Using play as a
therapeutic medium involves nondirective and directive play therapy (Dattilo & McKenney,
2011). Animal assisted therapy improves lives through interactions with animals in conjunction
with a therapist. A variety of techniques are used such as contact with animals and caring for
them (Dattilo & McKenney, 2011). Therapeutic use of exercise involves implementing a daily
routine of physical activity to meet treatment goals such as improved coordination, strength,
mobility, balance and relaxation (Dattilo & McKenney, 2011). Yoga is a very common exercise
used for calming and relaxing (Swann-Guerrero & Mackey, 2007).
The modality I chose to research was aquatic therapy. The discussion begins with the
historical background. It has been an international topic of study for many years. Used by
Greeks, Romans, Egyptians, Hindus, Japanese and Chinese; it has been appreciated for the
therapeutic results. It was not until the nineteenth century that aquatic therapy made progress in
the United States. Today its value is gaining recognition, as more practitioners are educated in
the beneficial effects of aquatic therapy (Dattilo & McKenney, 2011).
The purpose of the modality is to promote the transfer of medical treatment efficiently
into the community setting and to build health maintenance as a lifestyle (Dattilo & McKenney,
2011, p. 69). It also provides psychological and physiological improvements while encouraging
independent leisure participation (Dattilo & McKenney, 2011). In order for a CTRS to be able to
perform aquatic therapy they must have certain qualifications. In addition to basic aquatic
therapy training it is recommended that a CTRS have Aquatic Therapy and Rehabilitation
industry Certification (ATRIC), Aquatic Exercise Association instructor certification, Arthritis
DISABILITIES, MODALITIES AND ACTIVITIES
Aquatic instructor certification, and Multiple Sclerosis instructor certification (Dattilo &
McKenney, 2011).
Some of the most common aquatic techniques are swimming, Halliwick, Dolan and
Watsu. Swimming can be adapted to meet each individuals needs. It involves the body as a
whole and encourages social interaction. The Halliwick method uses the holistic approach in
teaching comfort and balance. It involves four steps of instruction, which include mental
adjustment, rotational control, inhibition and facilitation (Dattilo & McKenney, 2011).
The Dolan method was developed specifically for persons with autism. It teaches them
how to swim by placing Styrofoam floats on their back and swim fins on their feet. The
instructor imitates the movements and praises the participant when the do it correctly. As they
progress the Styrofoam floats and fins are removed. Watsu uses stretching and joint movement to
induce deep relaxation while floating participants are rocked back and forth in warm water
(Dattilo & McKenney, 2011).
Aquatic therapy provides children with autism a safe and supported environment. Since
these children have significant deficits in sensory processing they can over or under react to
stimuli in their environment. The hydrostatic water pressure can be soothing for them, which
relaxes their muscles (Jake, 2003). It is also believed to facilitate language development and
self-concept, and to improve adaptive behavior and provide an appropriate setting for early
educational intervention (Pan, 2010, p. 11). The buoyancy of the water also allows independent
movement that may not be achieved on land and as a result enhances motor performance (Pan,
2010).
An assessment is required to determine which children would benefit most from aquatic
therapy. Children with attention disorders, difficulty with range of motion, sensory impairments
DISABILITIES, MODALITIES AND ACTIVITIES
and show an interest in water would benefit from aquatic therapy. In planning the exercise
certain goals have to be targeted. The goals most appropriate in this situation are sensory
stimulation, improvement of range of motion, balance, response to visual cues and relaxation.
The facilitation techniques necessary to implement this modality are briefing, leading and
debriefing. Before beginning the activity the client should be informed of the expectations and
established goals. When leading the activity, the CTRS works to ensure the program stays
consistent with the targeted goals. Debriefing takes place after the activity has been completed.
This is when the CTRS reviews the events that occurred, how the client reacted and the
progression made toward the goal (Long, 2007). When evaluating the client in this therapy
program, it would be beneficial to note if the target goal was met or how close it was to being
reached. The specialist should also note what the client had to say during the program, such as, if
the water temperature was comfortable or the flotation devices were effective. The client should
be evaluated each time the activity takes place.
The specific activities found under the modality of aquatic therapy to be discussed are:
blowing balls, giant steps, bells, passing the ball, and balancing with turbulence. Blowing balls
and giant steps fit under this modality because both are activities, which assist the participant in
adjusting to the water (Dattilo & McKenney, 2011). It is important, both for safety and comfort,
that the participant be calm at ease when in the water. Bells and passing the ball both fit under
this modality because they assist in lateral, vertical and supine rotation to increase controlled
movement in the water. Balancing with turbulence also fits under this modality because of its
focus on improving balance and controlled movement (Dattilo & McKenney, 2011). All of these
fulfill the purpose of aquatic therapy in that their goal is to increase range of motion and balance.
DISABILITIES, MODALITIES AND ACTIVITIES
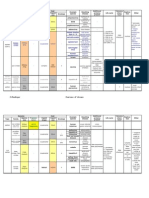
Activity Description and Activity Analysis Form Summary
The activity I chose to further discuss and complete my Activity Analysis Form (AAF) on
is bells. The overall purpose of this activity is to facilitate vertical rotation and motor
performance. When conducting aquatic therapy exercises it is important to know the participants
strengths, weaknesses, and how much room is required to complete the activity safely. With that
being said, the bell activity is designed for individuals whose goal is to increase their range of
motion and are not prone to epileptic seizure or have it under control.
The number of participants ranges from 1-3 and there should be sufficient space between
participants (about arms length apart). If the activity is done with just one participant then he/she
is placed in a circle formation using a long or short arm hold. The therapist and participant are in
alternating positions. The therapist then instructs the participant to bend their knees to the chest
and place the head back slowly. When this is done correctly, the participant is told to bring their
head forward and blow. If the individual is in need of assistance, they can use the therapists arm
to support their body (Dattilo & McKenney, 2011).
Now, the participant is encouraged to imitate the wind, sun and rain. When its time to
imitate the wind, the instructor says, Blow like the wind, and then the participant blows toward
the middle of the circle. When imitating the sun, the instructor says, The sun comes out, which
lets the participant know to place their head back and lie out in the sun. Lastly, the instructor
says, Make rain, and this is when the participant kicks their legs in the water (Dattilo &
McKenney, 2011).
If there is more than one participant, the activity can be done in a line formation. When
the instructor tells the group to walk forward, they let their legs go behind them and blow. After,
the instructor will walk backwards and instruct the participants to pull their knees up to their
DISABILITIES, MODALITIES AND ACTIVITIES
chests, place their heads back and extend their whole body lengthwise. Repeat instructions until
the instructor says its over (Dattilo & McKenney, 2011).
Completing the AFF for the bells activity included the following functional domains:
physical, social, cognitive, affective and administrative. Under the physical aspects, the primary
body position needed is to be lying down (floating) in the water and bent at the waist when
pulling the knees to the chest. The use of the whole body is needed. The activity requires
bending, standing and stretching. Sight and hearing are the primary senses required. Much
movement energy and flexibility is required, but not necessarily a high degree of hand-eye
coordination, strength, speed or endurance.
Under social aspects, the primary social interaction pattern for this activity is aggregate,
which is where a persons actions are directed toward another object while in the company of
another person. The participants should wear swimwear. There is close proximity and much
physical contact between instructor and participant. Cognitive aspects include a low amount of
complex rules, long-term, and short-term memory. No concrete or abstract thinking, math
reading, writing or spelling is required in this activity. It is important though, for the participant
to know their body parts and directionality.
Because the bells activity focuses more on physiological improvements and inward
feeling of relaxation, the affective aspects of this activity dont allow for much outward
expression. This activity is supposed to be fun and joyful. This is not a time for expressing guilt,
pain, anger fear or frustration. Under the administrative domain, the type of leadership style that
is requires is a supervisor and specific activity-skill expertise. There is not specific environment
required and the only equipment needed is a pool. The activity ends naturally and includes 1-3
participants.
DISABILITIES, MODALITIES AND ACTIVITIES
10
Activity Adaptation
Activity modifications or adaptations are important when dealing with any disability. It is
one of the most important ways to facilitate inclusion. Before the ADA was passed people with
disabilities were often excluded from activities because the adapted equipment we now have
today, was not available to them. However, because of the many advocates people with
disabilities have gained over the years, many attitudinal and architectural barriers can be
overcome. Now that the disability and activity have been assessed through thorough research and
the use of the AAF form, I have thought of a few ways that the activity can be adapted. Due to
the broad range of characteristics of autism, I will discuss the many possible limitations the child
may have.
When addressing the cognitive aspects of the activity, it would be beneficial to evaluate
the complexity of the rules and strategy used. This activity does not require complex rules, but it
is important to note the level of cognitive ability of the participant. As mentioned earlier, about
half of those with autism have an intellectual disability. For those with a low cognitive ability,
the instructor may need to lead by example and show the participant what to do instead of saying
it verbally. For those with a higher cognitive ability, the instructor can make the rules a little
more complicated to challenge them.
In the physical domain of this activity, it is important to remember that the whole body is
used in this activity. If the participant has difficulty with motor skills and is one of their goals,
the instructor can work their way up to stretching the body lengthwise. The first time the activity
is done they can just work on bringing the legs up to the knees and with each session progress to
stretching out and kicking. Also, for a child that has problems with sensory integration and have
sensitivity to noise, it would be beneficial to keep the pool quiet (Jake, 2003).
DISABILITIES, MODALITIES AND ACTIVITIES
11
Aquatic therapy also provides opportunity for social integration. The nature of the
activity is aggregate; however, for those with social impairments, it would be beneficial to
include up to two more participants so as to increase acceptable social behaviors (Pan, 2010).
The participants included should be children without disabilities so they can serve as a model. If
an individual has a secondary condition of epilepsy, the parents and doctors should approve of
him/her receiving aquatic therapy (Jake, 2003). This may require a closer physical proximity and
contact on the part of the instructor to ensure the safety of the participant (Jake, 2003). It may
also be necessary to have a second instructor assisting with the activity and both should be
trained in handling seizures.
Since those with autism dont necessarily have physical disabilities, there is not much
needed in the area of adapted equipment. However, there are a few simple devices that can be
used. If the individual has severe difficulty with visual cues, the instructor may set this as a goal.
So instead of using verbal cues, laminated or waterproofed picture cards can be used instead as
visual cues (Jake, 2003). A video camera may also prove useful. Video prompting is when a
video clip of one step of a task to show an individual and then giving that individual the
opportunity to perform that step before the next step is shown (Yanardag, Akmanoglu &
Yilmaz, 2013). Using this can be an effective way to help children with autism reach their
desired target skills (Yanardag, et. al, 2013).
Using reinforcers to encourage correct behavior is a great tool to remember to use when
dealing with children with autism. Clap or give them a toy when they complete the activity
correctly to further encourage correct behavior. This activity will be evaluated by measuring the
degree to which the goal was met. It is also important to receive feedback from the participant
about what they did and did not enjoy, so as to know what further changes can be made.
DISABILITIES, MODALITIES AND ACTIVITIES
12
Second Disabling Condition and Activity Adaptation
Description & Overview
The second disabling condition I chose to discuss is multiple sclerosis (MS). MS is the
most common disease of the nervous system affecting young adults. It is a demyelinating
disease, meaning it damages the myelin sheath that surrounds and protects the nerves (SwannGuerrero & Mackey, 2007). The myelin sheath allows the neural pathways to send impulses or
signals to and from the brain. MS affects the central nervous system (CNS). This includes the
brain, spinal cord, and optic nerve (Swann-Guerrero & Mackey, 2007).
According to Swann-Guerrero & Mackey (2007), MS affects about 400,000 Americans
most of them being women. Because MS is common among young adults, it is usually diagnoses
between the ages of 20 and 50, although some have been diagnosed even younger. The four types
of MS include: relapsing-remitting, primary progressive, secondary progressive and progressive
relapsing. Relapsing-remitting is the most common form of MS and occurs when the condition
exacerbates, then there is partial or complete recovery. Primary progressive involves a
continuous worsening of the disease. Secondary progressive involves the initial period of
relapsing-remitting and a steady exacerbation, with or without flare-ups or remissions.
Progressive relapsing involves a steady decline of the disease from the beginning with or without
recovery between relapses (Swann-Guerrero & Mackey, 2007).
Persons with MS may lose the ability to walk independently or at all because of
tightening in the muscle groups, including chest, hips, hamstrings, and calves. They experience
intense fatigue during rigorous physical activities. There is also a limited tolerance for heat,
which may further increase fatigue. Some may have paresis or paralysis because of muscle
weakness in the lower extremities. Other impairments include: range of motion, balance and
DISABILITIES, MODALITIES AND ACTIVITIES
13
coordination, painful or blurry loss of vision, rapid eye movement, numbness, tingling and pain
(Swann-Guerrero & Mackey, 2007).
Activity Adaptation
Those with MS may find it more difficult to use land-based methods of exercising due to
the physical demands placed on the body because of gravity. As a result, more people are turning
to aquatic therapy as research has revealed its many benefits. The Multiple Sclerosis Association
of America (MSAA) (2014) stated, aquatic exercise is effective for improving flexibility and
range of motion, cardiovascular endurance, fatigue level, muscle strength, mobility function
(including gait and balance), quality of life, and psychological well-being (p. 3). But in order
for an individual to benefit from the bells activity listed above, some adaptions are necessary.
Depending on the level of mobility the individual has, some adaptive equipment might be
needed. If a person uses a wheelchair and has difficulty walking, a pool lift or floating stairs
should be used to assist in entering the pool. Mitts, paddles, bands, noodles, waist belts and other
flotation devices are available to use in the pool for those who have trouble standing (MSAA,
2014). Because this activity requires a lot of movement in the physical aspect, the instructor
should be aware of each individuals strengths and limitations so as to not tire them out. If the
goal is to work on muscle strengthening, the individual may wear devices on the limbs to create
resistance standing (MSAA, 2014).
In this activity, working with persons with autism turned out to be the complete opposite
for someone with MS. Persons with autism may need more assistance cognitively (e.g., using
visual cues), while a person with MS needs more assistance physically (e.g., using a pool lift).
Overall, this proved to be a very informative assignment in understanding and comparing the
various needs and adaptations of different disabilities.
DISABILITIES, MODALITIES AND ACTIVITIES
14
References
Autism Speaks (2015). What Is Autism? Retrieved from https://www.autismspeaks.org/whatautism
CentersforDiseaseControlandPrevention(CDC)(2015).FactsAboutASD.Retrievedfrom
http://www.cdc.gov/ncbddd/autism/facts.html
Dattilo, J., & McKenney, A. (2011). Facilitation Techniques in Therapeutic Recreation. State
College, PA: Venture Publishing, Inc.
Foose, A., & Ardovino, P. (2007). Therapeutic Recreation and Developmental Disabilities. In T.
Robertson & T. Long (Eds.), Foundations of Therapeutic Recreation (127-144).
Champaign, IL: Human Kinetics, Inc.
Jake, L. (2003). Autism and the role of Aquatic Therapy in Recreational Therapy Treatment
Services. Therapeutic Recreation Directory. Retrieved from
http://www.recreationtherapy.com/tx/stress.htm
Long, T. (2007). The Therapeutic Recreation Process. In T. Robertson & T. Long (Eds.),
Foundations of Therapeutic Recreation (79-97). Champaign, IL: Human Kinetics, Inc.
Multiple Sclerosis Association of America (MSAA) (2014). Aquatic Exercise & Multiple
Sclerosis: A Guide For Patients. Retrieved from http://mymsaa.org/PDFs/aqua-patientpub.pdf
Pan, C-Y (2010). Effects of water exercise swimming program on aquatic skills and social
behaviors in children with autism spectrum disorders. Autism: The International Journal
Of Research And Practice, 14(1), 928.
DISABILITIES, MODALITIES AND ACTIVITIES
15
Swann-Guerrero, S., & Mackey, C. (2007). Wellness Through Physical Activity. In T. Robertson
& T. Long (Eds.), Foundations of Therapeutic Recreation (199-214). Champaign, IL:
Human Kinetics, Inc.
Williams, R. (2007). Places, Models, and Modalities of Practice. In T. Robertson & T. Long
(Eds.), Foundations of Therapeutic Recreation (63-76). Champaign, IL: Human Kinetics,
Inc.
Yanardag, M., Akmanoglu, N., & Yilmaz, I. (2013). The effectiveness of video prompting on
teaching aquatic play skills for children with autism. Disability & Rehabilitation, 35(1),
47-56.
Você também pode gostar
- EMOTIONAL SELF-REGULATION AND ARTISTIC THERAPIESNo EverandEMOTIONAL SELF-REGULATION AND ARTISTIC THERAPIESNota: 5 de 5 estrelas5/5 (1)
- Thebestiimulti2022 004Documento11 páginasThebestiimulti2022 004Marcin ChłostaAinda não há avaliações
- Tia Langston - ProjectDocumento17 páginasTia Langston - Projectapi-460354727Ainda não há avaliações
- Final Research Report - Madyson ObrienDocumento7 páginasFinal Research Report - Madyson Obrienapi-548979710Ainda não há avaliações
- Hydrotherapy in OTDocumento4 páginasHydrotherapy in OTPauleen SenoAinda não há avaliações
- E-Portfolio Writing Sample - Iwa Research ProjectDocumento9 páginasE-Portfolio Writing Sample - Iwa Research Projectapi-590697968Ainda não há avaliações
- CH 8 Childhood Mental and Developmental DisordersDocumento43 páginasCH 8 Childhood Mental and Developmental DisordersayuvindaAinda não há avaliações
- Addressing The Characteristics of Autism Spectrum Disorder PaperDocumento11 páginasAddressing The Characteristics of Autism Spectrum Disorder Paperapi-635957960Ainda não há avaliações
- Lagasse 2014Documento26 páginasLagasse 2014dimasAinda não há avaliações
- Autism A Key Piece of The Global Mental Health PuzzleDocumento3 páginasAutism A Key Piece of The Global Mental Health Puzzlepatriciafernandes.toAinda não há avaliações
- Parenting Neurodiverse Children: A Comprehensive Guide to Supporting Children with ADHD, Autism, and DyslexiaNo EverandParenting Neurodiverse Children: A Comprehensive Guide to Supporting Children with ADHD, Autism, and DyslexiaAinda não há avaliações
- Medical Aspects of Autism Spectrum DisorderDocumento12 páginasMedical Aspects of Autism Spectrum DisorderTimquannaAinda não há avaliações
- Psych EEDocumento6 páginasPsych EESindhuja RamanAinda não há avaliações
- Overcoming Autism Spectrum Disorder in children: Empowering Young Minds: A Holistic Approach to Navigating Autism Spectrum Disorder in ChildrenNo EverandOvercoming Autism Spectrum Disorder in children: Empowering Young Minds: A Holistic Approach to Navigating Autism Spectrum Disorder in ChildrenAinda não há avaliações
- Developmental DisabilityDocumento8 páginasDevelopmental DisabilityAryan KhannaAinda não há avaliações
- Music As A Therapeutic Intervention With Autism: A Systematic Review of The LiteratureDocumento18 páginasMusic As A Therapeutic Intervention With Autism: A Systematic Review of The LiteratureDaphne XanthopoulouAinda não há avaliações
- Evidence-Based Treatments For Autism Spectrum DisoDocumento20 páginasEvidence-Based Treatments For Autism Spectrum DisoNadia AzmieraAinda não há avaliações
- A Qualitative Exploration of Primary School Students Experience & Utilization of Mindfullness-2017Documento14 páginasA Qualitative Exploration of Primary School Students Experience & Utilization of Mindfullness-2017K. KhanAinda não há avaliações
- Mental Health AwarenessDocumento22 páginasMental Health AwarenessShiela P. ZumarragaAinda não há avaliações
- (2017) Empowering Preschool Teachers To Identify Mental Health Problems A Task-Sharing Intervention in EthiopiaDocumento11 páginas(2017) Empowering Preschool Teachers To Identify Mental Health Problems A Task-Sharing Intervention in EthiopiaJulián A. RamírezAinda não há avaliações
- Interoception Based Interventon For Children ASD Pilot Study 2020Documento15 páginasInteroception Based Interventon For Children ASD Pilot Study 2020hannahAinda não há avaliações
- Lesson 2B Implementation of Nursing Care of The Older Adult Psychosocial Care of Older AdultDocumento6 páginasLesson 2B Implementation of Nursing Care of The Older Adult Psychosocial Care of Older Adultczeremar chanAinda não há avaliações
- Signature Assignment: Final Draft !1Documento17 páginasSignature Assignment: Final Draft !1Allison Van KirkAinda não há avaliações
- AutismDocumento6 páginasAutismnehaAinda não há avaliações
- Duplooy 2018Documento18 páginasDuplooy 2018AxelAinda não há avaliações
- Autism Brief Nov 06Documento13 páginasAutism Brief Nov 06Izhaan AkmalAinda não há avaliações
- Mental Health, Intellectual and Developmental Disabilities and the Ageing ProcessNo EverandMental Health, Intellectual and Developmental Disabilities and the Ageing ProcessAinda não há avaliações
- Can Children With Autism Recover? If So, How?: Neuropsychology Review January 2009Documento29 páginasCan Children With Autism Recover? If So, How?: Neuropsychology Review January 2009Faiber RojasAinda não há avaliações
- Globalna Perspektiva AutizmaDocumento7 páginasGlobalna Perspektiva AutizmaJohn SmithAinda não há avaliações
- Visual attention to social and non-social objects across the autism spectrumNo EverandVisual attention to social and non-social objects across the autism spectrumAinda não há avaliações
- Project Diagnostic - AutismDocumento3 páginasProject Diagnostic - Autismapi-706711480Ainda não há avaliações
- Educating Adults With Autism Spectrum Condition As An International IssueDocumento14 páginasEducating Adults With Autism Spectrum Condition As An International IssueHanan AlmasoudAinda não há avaliações
- Psychopathology in Adolescents and Adults with Autism Spectrum DisordersNo EverandPsychopathology in Adolescents and Adults with Autism Spectrum DisordersRoberto KellerAinda não há avaliações
- Standard 7Documento7 páginasStandard 7api-671863522Ainda não há avaliações
- Steele and Van Der Hart Attachment and Dissociation Chapter 2013Documento17 páginasSteele and Van Der Hart Attachment and Dissociation Chapter 2013Rosita Blanco Prieto100% (1)
- Sensory Integration TherapyDocumento17 páginasSensory Integration Therapyapi-427151706Ainda não há avaliações
- 2015edf2028 Assignment 1 Tanya NguyenDocumento8 páginas2015edf2028 Assignment 1 Tanya Nguyenapi-320409861Ainda não há avaliações
- Best Ch1 Understanding Individuals With Physical Health and Multiple DisabilitiesDocumento25 páginasBest Ch1 Understanding Individuals With Physical Health and Multiple DisabilitiesMarkoAinda não há avaliações
- Understanding Autism Spectrum Disorder: A Book That Every Parent and Teacher Should HaveNo EverandUnderstanding Autism Spectrum Disorder: A Book That Every Parent and Teacher Should HaveAinda não há avaliações
- CC - Health Care Assess To Children in Psychiatric FacilitiesDocumento10 páginasCC - Health Care Assess To Children in Psychiatric Facilitiesapi-570349057Ainda não há avaliações
- Nur 420 - Policy Action Plan PaperDocumento9 páginasNur 420 - Policy Action Plan Paperapi-375928224Ainda não há avaliações
- Cerebral PalsyDocumento7 páginasCerebral Palsyapi-315294234Ainda não há avaliações
- Dekker 2014Documento9 páginasDekker 2014PIR oTECNIAAinda não há avaliações
- Adjustment and Academic Achievement in AdolescentsNo EverandAdjustment and Academic Achievement in AdolescentsAinda não há avaliações
- Hunger: Mentalization-based Treatments for Eating DisordersNo EverandHunger: Mentalization-based Treatments for Eating DisordersNota: 1 de 5 estrelas1/5 (1)
- Free Research Papers On Mental IllnessDocumento5 páginasFree Research Papers On Mental Illnesssvfziasif100% (1)
- Group intervention reduces adolescent depression and anxiety in KenyaDocumento33 páginasGroup intervention reduces adolescent depression and anxiety in KenyaTom OsbornAinda não há avaliações
- Can Children With Autism Recover Helt Fein Etal FINALDocumento28 páginasCan Children With Autism Recover Helt Fein Etal FINALkarthick vasudevanAinda não há avaliações
- Brain Sciences: Ffects of Social Isolation and Loneliness inDocumento31 páginasBrain Sciences: Ffects of Social Isolation and Loneliness inJoson AlyannaAinda não há avaliações
- Wilson2010AMH GeneraldistressandhelpavoidanceDocumento11 páginasWilson2010AMH GeneraldistressandhelpavoidanceAye Myat KyawAinda não há avaliações
- Education Research Paper Draft RevisionDocumento9 páginasEducation Research Paper Draft Revisionapi-508949220Ainda não há avaliações
- Nurse Education in Practice: Margaret Mcallister, RN, Ed D, Bruce Allen Knight, PHD, Cathie Withyman, Mbus. (Research)Documento6 páginasNurse Education in Practice: Margaret Mcallister, RN, Ed D, Bruce Allen Knight, PHD, Cathie Withyman, Mbus. (Research)Lushy Ayu DistaAinda não há avaliações
- Yogic Care For Neurodevelopmental Rehabilitation:: Arun Pratap SinghDocumento15 páginasYogic Care For Neurodevelopmental Rehabilitation:: Arun Pratap SinghGustavo SilvaAinda não há avaliações
- Hirvikoski, Et Al.j. (2015) - Cognitive Behavior Therapy-Based Psychoeducational Groups For Adults With ADHD and Their Significant OthersDocumento11 páginasHirvikoski, Et Al.j. (2015) - Cognitive Behavior Therapy-Based Psychoeducational Groups For Adults With ADHD and Their Significant OthersjuanAinda não há avaliações
- autism-fact-sheetDocumento5 páginasautism-fact-sheethopps75Ainda não há avaliações
- Autism Spectrum DisorderDocumento10 páginasAutism Spectrum Disordersobs sajadAinda não há avaliações
- Intensive Child Centered Play Therapy Fo-1Documento11 páginasIntensive Child Centered Play Therapy Fo-1Kainat MunirAinda não há avaliações
- Autastic Horizons: Navigating Life's Spectrum with Autism UnveiledNo EverandAutastic Horizons: Navigating Life's Spectrum with Autism UnveiledAinda não há avaliações
- Chronic Illness and People With Intellectual Disability: Prevalence, Prevention and ManagementDocumento42 páginasChronic Illness and People With Intellectual Disability: Prevalence, Prevention and ManagementErsya MusLih AnshoriAinda não há avaliações
- Sensory Processing Evaluation and Intervention in Mental Health - Mar10Documento6 páginasSensory Processing Evaluation and Intervention in Mental Health - Mar10Kimberly WoodlandAinda não há avaliações
- Disease ProjectDocumento18 páginasDisease Projectapi-293515530Ainda não há avaliações
- Lei 4711 Treatment ProgramDocumento5 páginasLei 4711 Treatment Programapi-293515530Ainda não há avaliações
- Accessibility AssignmentDocumento9 páginasAccessibility Assignmentapi-293515530Ainda não há avaliações
- Resume - InternshipDocumento1 páginaResume - Internshipapi-293515530Ainda não há avaliações
- MictobsDocumento7 páginasMictobsAnuja AnushaAinda não há avaliações
- ABO, RH, Minor Blood Grps AHG Test Pretransfusion Test Automation in BBDocumento32 páginasABO, RH, Minor Blood Grps AHG Test Pretransfusion Test Automation in BBJill Arciaga0% (1)
- Lab Manual GeneticsDocumento15 páginasLab Manual Geneticsapi-319985329100% (1)
- Antibiotic Sensitivity TestingDocumento3 páginasAntibiotic Sensitivity Testingbliss polleyAinda não há avaliações
- Borrador Writing 3Documento3 páginasBorrador Writing 3Carlos LazoAinda não há avaliações
- RBC AnomaliesDocumento10 páginasRBC AnomaliesSHUPATUSSAIAinda não há avaliações
- Bone Grafting: Classification by OriginDocumento4 páginasBone Grafting: Classification by OriginHerlangga Fadhillah AkbarAinda não há avaliações
- Ganong Physiology Self-Assessment QuestionsDocumento51 páginasGanong Physiology Self-Assessment QuestionsShasheendra JayawickramaAinda não há avaliações
- Bio All ModulesDocumento561 páginasBio All ModulesBlake M RhoadesAinda não há avaliações
- Handbook of Pediatric Hematology and Oncology 3rd Edition 2021Documento492 páginasHandbook of Pediatric Hematology and Oncology 3rd Edition 2021pgginecologiahospirioAinda não há avaliações
- Clinical Bioinformatics - A New Emerging ScienceDocumento3 páginasClinical Bioinformatics - A New Emerging ScienceSUMAN CHAUDHURIAinda não há avaliações
- Sistem Otot Dan Kerangka UnggasDocumento20 páginasSistem Otot Dan Kerangka UnggasWahyu Solhan MaghfurAinda não há avaliações
- Andrews - Chapter 1 - Skin Basic Structure and FunctionDocumento38 páginasAndrews - Chapter 1 - Skin Basic Structure and FunctionAngeli Ramos-EstrellaAinda não há avaliações
- tmp7092 TMPDocumento8 páginastmp7092 TMPFrontiersAinda não há avaliações
- Antigen Processing and Presentation 09Documento34 páginasAntigen Processing and Presentation 09Khairul Ikhwan100% (2)
- MDP10108 Student Guidebook 2023-24-3Documento8 páginasMDP10108 Student Guidebook 2023-24-3frinnnaaaaAinda não há avaliações
- Virus TableDocumento3 páginasVirus TableFrozenManAinda não há avaliações
- Yasser Al Kadri and Zaid Al AzemDocumento14 páginasYasser Al Kadri and Zaid Al Azemalsakar26Ainda não há avaliações
- CRL 9609Documento3 páginasCRL 9609naveenmi2Ainda não há avaliações
- Aphasia: Dr. Ika Marlia, M.SC, Sps Bagian/Smf Neurologi FK Unsyiah/Rsud DR Zainoel Abidin Banda AcehDocumento14 páginasAphasia: Dr. Ika Marlia, M.SC, Sps Bagian/Smf Neurologi FK Unsyiah/Rsud DR Zainoel Abidin Banda AcehRudy LusmiandaAinda não há avaliações
- Seminar On Cancer: Submitted To Submitted byDocumento13 páginasSeminar On Cancer: Submitted To Submitted byUdaya SreeAinda não há avaliações
- Biochemical and Molecular Characterization of The Venom From The Cuban Scorpion Rhopalurus JunceusDocumento10 páginasBiochemical and Molecular Characterization of The Venom From The Cuban Scorpion Rhopalurus JunceusCapitulina AmbrioletaAinda não há avaliações
- Survival in Long CaseDocumento7 páginasSurvival in Long CaseRapid MedicineAinda não há avaliações
- Blood Gas Analysis ExplainedDocumento28 páginasBlood Gas Analysis ExplainedanojAinda não há avaliações
- Preanalytical Variability Associated With The Procurement and Study of Small Biopsies - 091022dwDocumento19 páginasPreanalytical Variability Associated With The Procurement and Study of Small Biopsies - 091022dwkamulegeya RogersAinda não há avaliações
- Mercury Poisoning Symptoms and TreatmentsDocumento1 páginaMercury Poisoning Symptoms and TreatmentsRakheeb BashaAinda não há avaliações
- Dissociative Identity Disorder Research OverviewDocumento7 páginasDissociative Identity Disorder Research Overviewthom_evans_2Ainda não há avaliações
- Human Amyloid Imaging 2015 Book DraftDocumento151 páginasHuman Amyloid Imaging 2015 Book DraftWorldEventsForumAinda não há avaliações
- Basic Risk MeasurementDocumento18 páginasBasic Risk Measurementgoku krishnaAinda não há avaliações
- Big Data in Health Care Sector: Department of Computer ApplicationsDocumento9 páginasBig Data in Health Care Sector: Department of Computer ApplicationsReshma K.PAinda não há avaliações