Escolar Documentos
Profissional Documentos
Cultura Documentos
Case Study 2016 Rcowger
Enviado por
api-307867274Descrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Case Study 2016 Rcowger
Enviado por
api-307867274Direitos autorais:
Formatos disponíveis
Case Study 2016
Rachel Cowger, DH2
Patient Selection Rationale
This patient qualified for the case study project because they were Periodontal Case Type
II/III and had a subgingival calculus deposit of a 3
I explained that both NSPT and Continuing Care would be included as part of this project,
and the patient agreed to be my case study
NSPT Dates
Began treatment: February 22nd, 2016
Completed treatment: March 7th, 2016
Pretreatment Assessment: Health History
Summary
I: none
S: Type II Diabetes
M: Metformin may cause taste disorder
E: none
A: none
D: patient brushes once daily with fluoride paste
Pretreatment Assessment: Vital Signs
Patient vital signs were within normal limits
ASA Class II
Pretreatment Assessment: I/O Findings
No significant findings
Pretreatment Assessment: Dental Charting
Following our dental exam, these findings were recorded in the dental chart as proposed restorations:
#1 O
#2 DO
#3 DO
#4 DO
#18 DO
#19 DO
#19 BV
#30 O
#31 O
#32 O
Pretreatment Assessment: Dental Charting
Following our dental exam, these findings were recorded in the dental chart as watch
surfaces:
#8 M
#9 M
#25 BV
Pretreatment Assessment: Perio
Assessment
Pretreatment Assessment: Perio
Assessment
Pretreatment Assessment: Microscope
Evaluation
Patient falls into Risk Factor C category
High Risk
High counts of spinning and gliding rods
High counts of spirochetes
Pretreatment Assessment: Radiographic
Findings
Bone loss: Generalized slight horizontal with localized moderate
Decay as previously listed (10 surfaces decay, 3 watch surfaces)
Molar Projections
Premolar Projections
Maxillary Anterior Projections
Mandibular Anterior Projections
Pretreatment Assessment: Study Models
Pretreatment Assessment: Study Models
I did my best, but the impressions did not include the entire crown of the third molars
present
The pour up had air bubbles in the base and in a couple anterior teeth on the mandible
The buzz trim went well, but the models ended up being off center
These models were made with the intent to be used in patient education, but
unfortunately my patient never returned after I had completed them, so they were never
used.
Dental Hygiene Diagnosis: Periodontal
Case Type
I diagnosed this patient as being a generalized periodontal case type II with localized
periodontal case type III
Generalized slight periodontitis with localized moderate periodontitis
Dental Hygiene Diagnosis: Calculus
Deposit
This patient originally was evaluated as a 2/2.5
Upon completion of assessments and a calculus chart, the deposit was changed to 2/3
Dental Hygiene Diagnosis: Gingival
Description
Color: Generalized slight-moderate hyperemic
Contour: Generalized slight-moderate enlarged with generalized slight recession
Consistency/Texture: Generalized slight-moderate edematous
Statement of Inflammation: Generalized slight-moderate papillary/marginal inflammation
Dental Hygiene Diagnosis: Radiographic
Support
The radiographs support the diagnosis by showing generalized slight horizontal bone loss;
this represents the slight periodontal involvement
There is localized moderate horizontal bone loss which shows more involved areas of
moderate periodontitis
Intraoral Photos
Intraoral Photos
Intraoral Photos
Intraoral Photos
Intraoral Photos
Risk Assessment: Periodontal Risk Factors
Dental Biofilm: Moderate risk; generalized moderate cervical and interproximal plaque
Calculus: Moderate risk; 2 supragingival and 3 subgingival
Bleeding on Probing: Low risk; localized slight BOP
Contributing Factors: Low risk; slight crowding in lower anteriors
Loss of Attachment: Moderate risk; generalized 1-2mm and localized 3-4mm CAL
Risk Assessment: Caries Risk Factors
Visible caries of white spot lesions: High risk; 10 surfaces of decay
Recently restored caries: N/A
Deep occlusal pits and fissures: High risk
Root exposure: Low risk; generalized slight recession
Visible dental biofilm: Moderate risk; generalized plaque along gumline and interproximal
Diet/frequent sugar exposure: Low risk; once or twice weekly
Xerostomia or saliva reducing factors: Low risk; patient has noticed dry mouth before, but
not often
Appliances: N/A
Risk Assessment: Patient Goals
This patient expressed a desire to work towards having a healthy mouth. After the
microscope assessment, they were very concerned about bacteria.
Risk Assessment: Planned Interventions
Ultrasonic
Hand scaling
Use of dental floss or other interproximal aid
Risk Assessment: Expected Outcomes
Reduced inflammation
Better plaque control
Risk Assessment: Greatest Disease Risk
The greatest disease risk at this time is caries
Treatment Plan and Rationale: Treatment
Plan
Appointment #1:
D0120 Periodic Oral Evaluation
D4341 Periodontal Scaling and Root Planing UR
D1330 Oral Hygiene Instructions
Appointment #2:
D4341 Periodontal Scaling and Root Planing LR
D1330 Oral Hygiene Instructions
Appointment #3:
D4341 Periodontal Scaling and Root Planing UL
D4341 Periodontal Scaling and Root Planing LL
D1330 Oral Hygiene Instructions
D1206 Topical Application of Fluoride Varnish
Appointment #4:
D4910 Periodontal Maintenance Procedures
D1330 Oral Hygiene Instructions
D1206 Topical Application of Fluoride Varnish
Treatment Plan and Rationale: Clinical
Knowledge
Based off of the findings from assessment procedures, this patient needed NSPT
The deposit level and level of sensitivity the patient had during probing/exploring
confirmed the use of local anesthesia
Treatment Plan and Rationale: Cultural
Knowledge
This patient was Hispanic and spoke very little English, so I had a hard time communicating
all of the necessary information
I was very fortunate to have a fellow student and instructor who were willing to be
available to help me translate
Treatment Plan and Rationale: Behavior
Modification Strategies
This patient was concerned about how the appearance of their teeth
There has been extractions done a couple weeks prior to NSPT and they were upset that you
could see teeth missing when they smiled
I tried to use appearance as a motivational tool in homecare. I had my instructor talk to the
patient about the gingival inflammation and plaque being visible, and that it can be controlled
with proper brushing technique
I also tried to motivate behavior change by discussing the amount of restorative work needing
to be done. We talked about the teeth needing priority, and then how to prevent future decay
Another way I tried to motivate behavior change was talking about injections. The patient did
not want any injections for anything, but knew they were necessary. I talked to them about
taking better care of their teeth so that they wouldnt need more restorations or NSPT and
wouldnt be needing injections
Treatment Progress Notes
2/19/16 Patient was in for NPI appointment
2/22/16 Patient was in for NSPT in UL
2/24/16 Patient was in for FMX in DH1 lab
2/29/16 Patient was in for NSPT in LR
3/7/16 Patient was in to complete NSPT in LL and UR
Patient did not return for continuing care
Oral Hygiene Instruction: Initial
Recommendations
Initially the patient said they were not doing anything to clean interproximally
We went over sulcular brushing technique, recommended twice daily
Demonstrate c-curve flossing and recommended this once daily, or as often as they could
Oral Hygiene Instruction: Patient
Compliance
At the second appointment the patient said they were brushing twice a day, but still were
not flossing
Oral Hygiene Instruction: Modifications
The only modification was to try and incorporate flossing
I talked to the patient to see if they would be willing to try another interproximal aid, but
they said that they would floss they had just forgotten the c-curve technique, so we
demonstrated that again
Oral Hygiene Instruction: Patient
Compliance with Modifications
At the final scaling appointment, the patient reported that they were brushing twice and
flossing once daily
Motivation Strategies: Patient Intrinsic
Motivation
This patient was self-conscious of their teeth and appearance, so that was the intrinsic
motivation for them
Motivation Strategies: Patient Extrinsic
Motivation
I tried to get the patient to think of taking care of their teeth as a reward system. If they
kept up on homecare and hygiene treatment, they would be rewarded with less painful
cleanings and a beautiful smile
Motivation Strategies
Ive already mentioned my motivation strategies for this patient during OHI and they
didnt change over the course of treatment
I used appearance, fear of injections, and their overall dental pain to motivate and push
them toward better homecare and dental care
Continuing Care Appointment
This patient did not return for the continuing care
When contacted to plan and schedule the appointment, the patient said that they were
no longer able to come in because they had gotten a job
I tried to get them to come in the evening or anytime that would work for them, and I
reminded them that it was a no cost appointment, but they still decided not to return
Comparison: NSPT and Continuing Care
I have not seen the patient since completing NSPT, and they have not been in to
complete any restorative work
It is unfortunate, but I have nothing to compare!
Reflection
I would give this patient the same treatment and treatment plan
I would consider trying a desensitizing pre-polish for this patient to see if that made any
difference for them. Although they did need local anesthesia, it was difficult to do the
reappoint procedures because they were so sensitive
My recommended recall interval for this patient is 3 months for periodontal maintenance. I
would want them in at 3 months for continuing care to see how everything was doing and
make sure the homecare was effective. After a few appointments of being on track I
would say that the patient could come in every 4 months, and if things were still stable
and their homecare was good, I would recommend 6 months
This patient would not benefit from seeing a periodontist unless they were considering
implants for their extracted teeth. This patient was only localized case type III, so they were
not too difficult to be seen at our clinic or at any general office
Reflection
This project was a challenge for me. In all honesty, my patient would have preferred to be
seen by someone who could communicate better in Spanish, and I believe that factor
and their extreme sensitivity kept them from wanting to come back. The language barrier
was difficult, but I did my best and felt that I was successful in keeping my patient
comfortable throughout treatment
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Perio Office Visit 2016 RcowgerDocumento4 páginasPerio Office Visit 2016 Rcowgerapi-307867274Ainda não há avaliações
- Special Care Client Rcowger 2016Documento4 páginasSpecial Care Client Rcowger 2016api-307867274Ainda não há avaliações
- Specialty Office Visit Fall 2015 RcowgerDocumento6 páginasSpecialty Office Visit Fall 2015 Rcowgerapi-307867274Ainda não há avaliações
- Microscope Narrative RcowgerDocumento4 páginasMicroscope Narrative Rcowgerapi-307867274Ainda não há avaliações
- RcowgerceDocumento1 páginaRcowgerceapi-307867274Ainda não há avaliações
- Oral Hygiene Instruction RcowgerDocumento17 páginasOral Hygiene Instruction Rcowgerapi-307867274Ainda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Barriers To The Evidence-Based Patient Choice (EBPC) Vs EBM. Paper Study. Evidence Based Medicine Interest.Documento7 páginasBarriers To The Evidence-Based Patient Choice (EBPC) Vs EBM. Paper Study. Evidence Based Medicine Interest.Lourdes Fernandez CabreraAinda não há avaliações
- Nurani Kaeda - Part 1Documento5 páginasNurani Kaeda - Part 1farah_nishuAinda não há avaliações
- Informative Speech OutlineDocumento2 páginasInformative Speech OutlinemaddieAinda não há avaliações
- Dental ChartDocumento1 páginaDental Chartkhalil carloas mendozaAinda não há avaliações
- CandidiasisDocumento27 páginasCandidiasisWr Newgate50% (2)
- MUHAMMAD NAJEEB KALLIDUKKIL LECTURER CVDocumento4 páginasMUHAMMAD NAJEEB KALLIDUKKIL LECTURER CVnajeeb500Ainda não há avaliações
- Orthopedics TraumatologyDocumento8 páginasOrthopedics TraumatologyCpopAinda não há avaliações
- DMSCO Log Book Vol.25 1947Documento49 páginasDMSCO Log Book Vol.25 1947Des Moines University Archives and Rare Book RoomAinda não há avaliações
- Ophthalmic Artery Doppler Predicts Preeclampsia RiskDocumento4 páginasOphthalmic Artery Doppler Predicts Preeclampsia RiskImagen Molecular Del Sureste Spect-ct ChiapasAinda não há avaliações
- Dental ClinicsDocumento109 páginasDental ClinicsMar Men AguiAinda não há avaliações
- Continuing Nursing Education: Importance of Lifelong LearningDocumento6 páginasContinuing Nursing Education: Importance of Lifelong LearningDebashrita MisraAinda não há avaliações
- FINALS ReviewerDocumento14 páginasFINALS ReviewerJustine Simeon lagunzadAinda não há avaliações
- The - Erlangen - Test - of - Activities - of - Daily - Living - in ADocumento3 páginasThe - Erlangen - Test - of - Activities - of - Daily - Living - in Akwstas79Ainda não há avaliações
- 2028 Ajcc Melanoma and BeyondDocumento6 páginas2028 Ajcc Melanoma and BeyondDaniel Atl Lopez FabilaAinda não há avaliações
- FREE NLE REVIEW Fundies and OthersDocumento40 páginasFREE NLE REVIEW Fundies and OthersAngel Lopez100% (1)
- Vacancies in The Department of Health: DirectorateDocumento3 páginasVacancies in The Department of Health: DirectorategxjjsjejduAinda não há avaliações
- 4.2 Endo - Nisha GargDocumento556 páginas4.2 Endo - Nisha GargSrishti SrivastavaAinda não há avaliações
- Placenta PreviaDocumento33 páginasPlacenta PreviamidoAinda não há avaliações
- مزاولة مهنة - طب أسنان نوفمبر 2020Documento5 páginasمزاولة مهنة - طب أسنان نوفمبر 2020وردة صبرAinda não há avaliações
- CV Serviceline WhitepaperDocumento12 páginasCV Serviceline WhitepaperAbidi HichemAinda não há avaliações
- Pulp Therapy For Primary and Immature Permanent Teeth: Latest RevisionDocumento9 páginasPulp Therapy For Primary and Immature Permanent Teeth: Latest RevisionGhufran KhalilAinda não há avaliações
- Kode DiagnosaDocumento1 páginaKode Diagnosapuskesmas sukahening100% (1)
- New QuestionnreDocumento3 páginasNew Questionnreawadesh44raiAinda não há avaliações
- Expanded Mobile Crisis Outreach Team (EMCOT)Documento3 páginasExpanded Mobile Crisis Outreach Team (EMCOT)Kyle A McCallAinda não há avaliações
- EPIDEMIOLOGY OF HEAD INJURY IN COIMBATOREDocumento6 páginasEPIDEMIOLOGY OF HEAD INJURY IN COIMBATOREArjun CVAinda não há avaliações
- Micormedex NeoFax-neonatologieDocumento869 páginasMicormedex NeoFax-neonatologiebaranclaudiaAinda não há avaliações
- 11 BPHDocumento59 páginas11 BPHبدرول هشام100% (1)
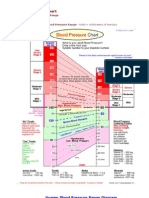
- Blood Pressure ChartDocumento5 páginasBlood Pressure Chartmahajan1963100% (1)
- Medical Cert - EENTDocumento1 páginaMedical Cert - EENTHydie Lumadeo50% (2)