Escolar Documentos
Profissional Documentos
Cultura Documentos
Seksual Desire Disorder
Enviado por
Larassati UthamiDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Seksual Desire Disorder
Enviado por
Larassati UthamiDireitos autorais:
Formatos disponíveis
50-55_Montgomery.
qxp
6/16/08
3:15 PM
Page 50
[REVIEW]
Sexual Desire Disorders
by KEITH A. MONTGOMERY, MD
AUTHOR AFFILIATIONS: Dr. Montgomery is a fourth year resident at Wright State University School of Medicine, Department of Psychiatry,
Dayton, Ohio.
ABSTRACT
Hypoactive sexual desire disorder
(HSDD) and sexual aversion disorder
(SAD) are an under-diagnosed group
of disorders that affect men and
women. Despite their prevalence,
these two disorders are often not
addressed by healthcare providers
and patients due their private and
awkward nature. As physicians, we
need to move beyond our own
unease in order to adequately
address our patients sexual
problems and implement appropriate
treatment. Using the Sexual
Response Cycle as the model of the
physiological changes of humans
during sexual stimulation and the
Diagnostic and Statistical Manual
of Mental Disorders, Fourth
Edition this article will review the
current literature on the desire
disorders focusing on prevalence,
etiology, and treatment.
ADDRESS CORRESPONDENCE TO: Dr. Keith Montgomery, Wright State University School of Medicine, Department of Psychiatry, 627 S. Edwin
C. Moses Blvd., Dayton, Ohio 45408-1461; E-mail: montgoka@hotmail.com
KEY WORDS: sexual desire disorders, sexuality, sexual dysfunction, sexual disorders, sexual response cycle, desire disorder, sexual arousal
disorder, hypoactive sexual disorder
INTRODUCTION
Hypoactive sexual desire disorder
(HSDD) and sexual aversion disorder
(SAD) affect both men and women.
Despite their prevalence, these
disorders are often not addressed by
healthcare providers or patients due
to their private and awkward nature.
Using the Sexual Response Cycle as
the model of the physiological
changes of humans during sexual
stimulation and the Diagnostic and
Statistical Manual of Mental
50
Psychiatry 2008 [ J U N E ]
Disorders, Fourth Edition (DSMIV-TR), this article will review the
current literature on the two desire
disorders, focusing on prevalence,
etiology, and treatment. With this
knowledge, hopefully, physicians will
move beyond their unease with the
topic in order to adequately address
patients sexual problems and to
implement appropriate treatment.
Sexuality defined. Sexuality is a
complex interplay of multiple facets,
including anatomical, physiological,
psychological, developmental,
cultural, and relational factors.1 All of
these contribute to an individuals
sexuality in varying degrees at any
point in time as well as developing
and changing throughout the life
cycle. Sexuality in adults consists of
seven components:
Gender identity
Orientation
Intention
50-55_Montgomery.qxp
6/16/08
3:15 PM
Page 51
Desire
Arousal
Orgasm
Emotional satisfaction
Gender identity, orientation, and
intention form sexual identity,
whereas desire, arousal, and orgasm
are components of sexual function.
The interplay of the first six
components contributes to the
emotional satisfaction of the
experience. In addition to the
multiple factors involved in sexuality,
there is the added complexity of the
corresponding sexuality of the
partner. The expression of a persons
sexuality is intimately related to his
or her partners sexuality.2,3
Sexual response cycle. The
sexual response cycle consists of
four phases: desire, arousal, orgasm,
and resolution. Phase 1 of the sexual
response cycle, desire, consists of
three components: sexual drive,
sexual motivation, and sexual wish.
These reflect the biological,
psychological, and social aspects of
desire, respectively. Sexual drive is
produced through
psychoneuroendocrine mechanisms.
The limbic system and the preoptic
area of the anterior-medial
hypothalamus are believed to play a
role in sexual drive. Drive is also
highly influenced by hormones,
medications (e.g., decreased by
antihypertensive drugs, increased by
dopaminergic compounds to treat
Parkinsons disease), and legal and
illegal substances (e.g., alcohol,
cocaine).4
Phase 2, arousal, is brought on by
psychological and/or physiological
stimulation. Multiple physiologic
changes occur in men and women
that prepare them for orgasm,
mainly perpetuated by
vasocongestion. In men, increased
blood flow causes erection, penile
color changes, and testicular
elevation. Vasocongestion in women
leads to vaginal lubrication, clitoral
tumescence, and labial color
changes. In general, heart rate, blood
pressure, and respiratory rate as well
as myotonia of many muscle groups
increase during this phase.5
Phase 3, orgasm, has continued
51
elevation of respiratory rate, heart
rate, and blood pressure and the
voluntary and involuntary
contraction of many muscle groups.
In men, ejaculation is perpetuated by
the contraction of the urethra, vas,
seminal vesicles, and prostate. In
women, the uterus and lower third of
the vagina contract involuntarily.
The duration of the final phase,
resolution, is highly dependent on
whether orgasm was achieved. If
orgasm is not achieved, irritability
and discomfort can result, potentially
lasting for several hours. If orgasm is
achieved, resolution may last 10 to
15 minutes with a sense of calm and
relaxation. Respiratory rate, heart
rate, and blood pressure return to
baseline and vasocongestion
diminishes. Women can have
factors.7 In order for a patient to be
diagnosed with a sexual dysfunction
disorder, a psychophysiologic
problem must exist, the problem
must cause marked distress or
interpersonal difficulty, and the
problem cannot be better accounted
for by another Axis I diagnoses. Also,
two sexual disorders must be ruled
out before one can diagnosis HSDD
or SAD. These are substanceinduced sexual dysfunction and a
sexual disorder due to general
medical condition.
PREVALENCE
The prevalence of desire disorders
is often underappreciated. The
National Health and Social Life
Survey found that 32 percent of
women and 15 percent of men
Despite their prevalence, these disorders are often not
addressed by healthcare providers or patients due to their
private and awkward nature. Physicians must move beyond
their unease in order to adequately address patients sexual
problems and implement appropriate treatment.
multiple successive orgasms
secondary to a lack of a refractory
period.1 The vast majority of men
have a refractory period following
orgasm in which subsequent orgasm
is not possible.6
CRITERIA
As previously stated, there are
two sexual desire disorders. HSDD in
the DSM-IV-TR7 is defined as
persistently or recurrently deficient
(or absent) sexual fantasies and
desire for sexual activity. The
judgment of deficiency or absence is
made by the clinician, taking into
account factors that affect sexual
functioning, such as age and the
context of the persons life. SAD is
defined as persistent or recurrent
extreme aversion to, and avoidance
of, all (or almost all) genital sexual
contact with a sexual partner. The
DSM-IV-TR lists six subtypes:
lifelong, acquired, generalized,
situational, due to psychological
factors, and due to combined
lacked sexual interest for several
months within the last year. The
study population was
noninstitutionalized US English
speaking men and women between
the ages of 18 and 59 years.8 There
are no large study prevalence figures
on SAD, but it is thought to be a rare
disorder. Both HSDD and SAD have
a higher female to male prevalence
ratio, although this discrepancy is
greater in SAD. The desire disorders
can be considered on a continuum of
severity with HSDD being the less
severe of the two disorders.1
ETIOLOGY
The proposed etiology of HSDD
influences how it is subtyped (i.e.,
generalized or situational, lifelong or
acquired). For example, lifelong
HSDD can be due to sexual identity
issues (gender identity, orientation,
or paraphilia) or stagnation in sexual
growth (overly conservative
background, developmental
abnormalities, or abuse). Conversely,
[JUNE]
Psychiatry 2008
51
50-55_Montgomery.qxp
6/11/08
2:40 PM
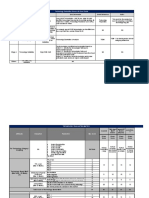
TABLE 1. Common psychotropic classes causing sexual
dysfunction
TRICYCLIC ANTIDEPRESSANTS
Mechanism of action (general)
Inhibits the re-uptake of norepinephrine and serotonin (5-HT)
Modulates norephinephrine and 5-HT activity at
the neural synapse
Mechanism of action (sexual)
Positive
Increased adrenergic 1 activity
Decreased cortisol
Negative
Decreased adrenergic activity
Decreased cholinergic activity
Decreased histamine
Decreased oxytocin
Increased prolactin
Increased serotonin
Direct sexual side effects*
Desire disorders
Dyspareunia
Erection difficulties
Orgasm disorders
Orgasmic inhibition
Anorgasmia
Spontaneous orgasm
Ejaculation disorders
Retarded ejaculation
Ejaculation without orgasm
Anesthetic ejaculation
* Despiramine appears to have the least amount of
sexual side effects of the TCAs
MONOAMINE OXIDASE INHIBITORS
Mechanism of action (general)
Decreases the neural monoamine oxidase enzymatic metabolic breakdown of norepinephrine and
serotonin I
Increases norepinephrine and serotonin activity at
the neural synapse
Mechanism of action (sexual)
Positive
Increased adrenergic 1 activity
Decreased monoamine oxidase
Negative
Decreased -adrenergic activity
Decreased cholinergic activity
Increased prolactin
Increased serotonin
Decreased testosterone
Direct sexual side effects*
Desire disorders
Erection difficulties
Orgasm disorders
Orgasmic inhibition
Decreased number
Ejaculation disorders
Retarded, inhibited
premature ejaculation
diminished
Adapted from Crenshaw TL, Goldberg JP. Sexual
Pharmacology: Drugs That Affect Sexual Functioning.
New York, NY: W. W. Norton & Company, 1996.
52
Psychiatry 2008 [ J U N E ]
Page 52
difficulty in a new sexual
relationship may lead to an acquired
or situational subtype of HSDD.
Although it is theoretically possible
to have no etiology, all appropriate
avenues should be explored,
including whether the patient was
truthful in responses to questions
regarding sexuality and if the patient
is consciously aware that he or she
has a sexual disorder.2,3
Diagnosis and treatment of desire
disorders is often difficult due to
confounding factors, such as high
rates of comorbid disorders and
combined subtype sexual disorders
involving medical and substanceinduced contributors.13 For example,
in a patient being treated for
recurrent major depressive disorder
and obstructive sleep apnea (OSA),
it would be difficult to separate out
whether the cause of his or her
decreased sexual desire was due to
the depressive episode,
antidepressant treatment, OSA,15
multiple potential interpersonal
problems, or a combination of
factors.
Even with a detailed and accurate
longitudinal history, honing in on the
main factor can be difficult.
Decreased sexual desire has been
seen in multiple psychiatric
disorders. For example, individuals
with schizophrenia and major
depression experienced decreased
sexual desire. Before treatment
commences for HSDD and SAD, a
thorough work-up must be done to
first rule out a general medical
condition or a substance that caused
decreased desire or aversion. This
would include a thorough physical
exam and laboratory work-up. An
important physiological maker for
which to test is a thyroid profile,
which would be abnormal in
hypothyroidism and could cause
decreased sexual desire.16 Also, low
testosterone has been shown affect
to desire. Normal physiological
testosterone concentrations range
from 3 to 12ng/mL. The apparent
critical level for sexual function in
males is 3ng/mL.14
A variety of medical conditions
can also decrease sexual desire (e.g.,
diabetes mellitus, hypothyroidism,
Addisons disease, Cushings disease,
temporal lobe lesions, menopause,16
coronary artery disease, heart
failure, renal failure, stroke, and
HIV). Also, as we naturally age,
desire can lessen.14 Many psychiatric
medications can lead to decreased
desire for sex including multiple
classes of antidepressants (selective
serotonin reuptake inhibitors,
norepinephrine serotonin reuptake
inhibitors, tricyclic antidepressants,
monoamine oxidase inhibitors, and
antipsychotics (Table 1).22
Two important biological
mediators of sexual desire are
dopamine and prolactin. Dopamine
acting through the mesolimbic
dopaminergic reward pathway is
hypothesized to increase desire,
whereas prolactin is thought to
decrease libido, although the
mechanisms are poorly understood.
Dopamine directly inhibits prolactin
release from the pituitary gland.
Medications that increase prolactin
release or inhibit dopamine release
can decrease sexual desire along
with other sexual side effects.19
If a patient has no history of
sexual desire problems and has
started a new sexual relationship,
other possibilities for low sexual
desire must be excluded. It is
possible that neither individual has a
desire disorder but rather there is a
marked difference between each
individuals level of desire, creating a
discrepancy. Separate interviews
with each partner are important to
obtain a more accurate picture of the
relationship.13
Important to remember that
HSDD in men is often misdiagnosed
as erectile dysfunction because of
the common misconception that all
men desire sex. This myth has
caused men to not seek treatment
and has also led to misdiagnosis by
health professionals. This may partly
explain the failure rate of adequately
treating erectile dysfunction. As part
of an initial history and physical
examination, a sexual history is
necessary because most patients will
not divulge any sexual problems
unless explicitly asked. There are
50-55_Montgomery.qxp
6/11/08
2:40 PM
Page 53
tests that deal entirely with sexual
desire (Sexual Desire Inventory) and
others have subscales for sexual
desire (International Index of
Erectile Function).14
TREATMENT
Psychotherapy. Although there
are many proposed treatments for
desire disorders, there are virtually
no controlled studies evaluating
them.20 Psychotherapy is a common
treatment for desire disorders. From
a psychodynamic perspective, sexual
dysfunction is caused by unresolved
unconscious conflicts of early
development. Treatment focuses on
bringing awareness to these
unresolved conflicts and how they
impact the patients life. While
improvement may occur, the sexual
dysfunction often becomes
autonomous and persists, requiring
additional techniques to be
employed.
An approach that has shown some
success in the treatment of desire
disorders as well as other sexual
dysfunctions, pioneered by Masters
and Johnson, is dual sex therapy.5 In
this therapy, the couple along with
one male and one female therapist
(gay and lesbian couples may opt for
same-sex therapists) meet together.
The relationship is treated as a
whole, with sexual dysfunction being
one aspect of the relationship.
Another important underlying
premise of this form of therapy is
that only one partner in the
relationship is suffering from sexual
dysfunction and absence of other
major psychopathology. The aim is to
reestablish open communication in
the relationship. Homework
assignments are given to the couple,
the results of which are discussed at
the following session. The couple is
not allowed to engage in any sexual
behavior together other than what is
assigned by the therapists.
Assignments start with foreplay,
which encourages the couple to pay
closer attention to the entire process
of the sexual response cycle as well
as the emotions involved and not
solely on achieving orgasm.
Eventually the couple progresses to
intercourse with encouragement to
try various positions without
completing the act.1
Cognitive behavioral therapy has
been shown to be efficacious in the
treatment of anxiety, depression, and
other psychiatric disorders. Its core
premise is that activating events lead
to negative automatic thoughts.
These negative thoughts in turn
result in disturbed negative feelings
and dysfunctional behaviors. The
goal is to reframe these irrational
beliefs through structured sessions.21
CBT has been also used to treat
sexual desire disorders by focusing
on dysfunctional thoughts,
unrealistic expectations, partner
behavior that decreases desire in
intercourse, and insufficient physical
stimulation. These sessions often
include both partners.20 Specific
exercises may be used. For example,
men with sexual desire disorder or
male erectile disorder may be
instructed to masturbate to address
performance anxiety related to
achieving a full erection and
ejaculation.
Finally, analytically oriented sex
therapy combines sex therapy with
psychodynamic and psychoanalytic
therapy and has shown good results.1
Specifically, for desire disorders due
to developmental and identity issues,
long-term psychodynamic
psychotherapy could be helpful.9 In
general, lifelong and generalized
desire disorders are more difficult to
treat.13
SAD is often progressive and
rarely reverses spontaneously. It is
also treatment-resistant.2 Poor
prognostic indicators are global,
lifelong, comorbid depression, or
associated with anorgasmia.24 Despite
difficulty in treatment, behavioral
therapy has been shown to be
effective for managing SAD.25,26
Pharmacotherapy. Multiple
hormones have been studied for
treatment of sexual desire disorders.
For example, androgen replacement
has been studied as a possible
treatment for HSDD. In patients
with induced or spontaneous
hypogonadism, either pathological
withdrawal and re-introduction or
TABLE 1. Common psychotropic classes causing sexual
dysfunction, continued
SELECTIVE SEROTONIN REUPTAKE INHIBITORS
Mechanism of action (general)
Work through selective serotonin-uptake
inhibition
Mechanism of action (sexual)
Negative
Increased cortisol
Increased opioids
Increased prolactin
Increased serotonin (5-HT)
Direct sexual side effects
Desire disorders
Hyposexuality
Hypersexuality
Orgasm disorders
Orgasmic inhibition
Anorgasmia
Spontaneous orgasm
Ejaculation disorders
Retarded ejaculation
Ejaculatory inhibition
Erection disorders
Inability/difficulty obtaining erection
Decreased quality of erection
Decreased or absent nocturnal/morning erections
ANTIPSYCHOTICS
Mechanism of action (general)
Block dopamine activity
Block sigma receptors and/or 5-HT2 serotonin
receptors
Mechanism of action (sexual)
Negative
Decreased adrenergic 1 activity
Decreased cholinergic activity
Decreased dopamine
Increased prolactin
Decreased testosterone
Decreased LHRH pulsatile activity
Direct sexual side effects
Desire disorders
Hyposexuality
Hypersexuality (rare)
Orgasm disorders
Orgasmic inhibition
Anorgasmia
Diminished number of orgasms
Ejaculation disorders
Retarded ejaculation
Ejaculatory inhibition
Decreased ejaculatory volume
Anesthetic ejaculation
Orgasm without ejaculation
Dyspareunia
Erection disorders
Inability/difficulty obtaining erection
Decreased quality of erection
Priapism
Adapted from Crenshaw TL, Goldberg JP. Sexual
Pharmacology: Drugs That Affect Sexual Functioning.
New York, NY: W. W. Norton & Company, 1996.
[JUNE]
Psychiatry 2008
53
50-55_Montgomery.qxp
6/11/08
2:40 PM
Page 54
exogenous androgens affects the
frequency of sexual fantasies,
arousal, desire, spontaneous
erections during sleep and in the
morning, ejaculation, sexual
activities with and without a partner,
and orgasms through coitus and
masturbation.14 Unfortunately, the
evidence for the efficacy of
testosterone in eugonadal men is
conflicting. Some studies show no
benefit,27 whereas others studies do
show some benefit. For example, a
study by OCarroll and Bancroft
showed that testosterone injections
did have efficacy for sexual interest,
but unfortunately this did not
translate into an improvement in
their sexual relationships.34 One
theory for the lack of efficacy in
eugonadal men is that it is more
difficult to manipulate endogenous
androgen levels with administration
of exogenous androgens due to
efficient homeostatic hormone
mechanisms.14 Androgen
supplementation is available in many
forms, including oral, sublingual,
cream, and dermal patch. Side
effects of testosterone
supplementation in women include
weight gain, clitoral enlargement,
facial hair, hypercholesterolemia,32
changes in long-term breast cancer
risk, and cardiovascular factors.16
Side effects in men of androgen
supplementation include
hypertension and prostatic
enlargement.1 The benefit of
androgen therapy in women is also
not clear.28 Although studies using
supraphysiologic levels of androgens
have shown increased sex libido,
there is the risk of masculinization
from chronic use.18 Testosterone
therapy has shown to improve sexual
function in postmenopausal women
in multiple ways, including increased
desire, fantasy, sexual acts, orgasm,
pleasure, and satisfaction of sexual
acts.16 Roughly half of all
testosterone production in women is
from the ovaries. Thus, an
oophorectomy can cause a sudden
drop of testosterone levels.18 Shifren,
et al.,17 studied 31- to 56-year-old
women who had hysterectomies and
oophorectomies. They were given
54
Psychiatry 2008 [ J U N E ]
150 or 300g of testosterone daily
for 12 weeks. Both groups, with a
dose response relationship, showed
increased frequency of sexual
activities and pleasurable orgasms.
At the 300g dose, there was even
higher scores for frequency of
fantasy, masturbation, and engaging
in sexual intercourse at least once a
week.18 Feelings of general wellbeing
were also increased.17
Estrogen replacement in
postmenopausal women can improve
clitoral and vaginal sensitivity,
increase libido, and decrease vaginal
dryness and pain during intercourse.
Estrogen is available in several
forms, including oral tablets, dermal
patch, vaginal ring, and cream.
Testosterone supplementation has
demonstrated increased libido,
increased vaginal and clitoral
sensitivity, increased vaginal
lubrication, and heightened sexual
arousal.32
Dehydroepiandrosterone-sulfate
(DHEA-S), a testosterone precursor,
has also been studied for the
treatment of sexual desire disorders.
Low physiologic levels of DHEA-S
have been found in women
presenting with HSDD.30 Increased
libido was observed in women with
adrenal insufficiency who were given
DHEA-S.31 Women with breast cancer
reported increased libido while
receiving tamoxifen, which increases
gonadotropin-releasing hormone
levels and therefore testosterone
concentrations.1
Some medications can be used to
increase desire due to their receptor
profiles. For example, amphetamine
and methylphenidate can increase
sexual desire by increasing dopamine
release. Bupropion, a norepinephrine
and dopamine reuptake inhibitor, has
been shown to increase libido.19 A
study by Segraves, et al.,33 showed
that bupropion treatment in
premenopausal women increased
desire, but not to a statistically
significant level compared to
placebo. But, bupropion SR group
did show statistically significant
difference in other measures of
sexual function: increased pleasure
and arousal, and frequency of
orgasms. Multiple herbal remedies,
such as yohimbine and ginseng root,
are purported to increase desire, but
this has not been confirmed in
studies.1
CONCLUSION
Sexual desire disorders are underrecognized, under-treated disorders
leading to a great deal of morbidity
in relationships. A thorough history
and physical examination are critical
to properly diagnosis and determine
the causative agent(s). With
appropriate treatment, improvement
can be made but continued research
in sexual dysfunction is critical in the
sensitive yet ubiquitous area. By
becoming more familiar with
prevalence, etiology, and treatment
of sexual desire disorders, physicians
hopefully will become more
comfortable with the topic so that
they can adequately address
patients sexual problems and to
implement appropriate treatment.
REFERENCES
1.
2.
3.
4.
5.
6.
7.
Sadock BJ, Sadock VA. Kaplan
and Sadocks Synopsis of
Psychiatry: Behavioral Sciences
and Clinical Psychiatry, Ninth
Edition. Philadelphia: Lippincott
Williams & Wilkins, 2003.
Levine SB, Risen CB, Althof SE
(eds). Handbook of Clinical
Sexuality for Mental Health
Professionals. New York: BrunnerRoutledge, 2003.
Levine SB. Sexual disorders. In:
Tasman A, Kay J, Lieberman J
(eds). Psychiatry, Second
Edition. Hoboken, NJ: Wiley, 2003.
Levine SB. Reexploring the
concept of sexual desire. J Sex
Marital Ther 2002;28:3951.
Masters WH, Johnson VE. Human
Sexual Response. Boston: Little,
Brown & Co., 1966.
Bechtel S. The practical
encyclopedia of sex and health:
From aphrodisiacs and hormones
to potency, stress, vasectomy, and
yeast infection. Emmaus (PA):
Rodale, 1993.
American Psychiatric Association.
Diagnostic and Statistical
Manual of Mental Disorders,
50-55_Montgomery.qxp
8.
9.
10.
11.
12.
13.
14.
15.
6/11/08
2:40 PM
Page 55
Fourth Edition, Text Revision.
Washington, DC: American
Psychiatric Press Inc., 2000.
Laumann EO, Paik A, Rosen RC.
Sexual dysfunction in the United
States: prevalence and predictors.
JAMA 1999;281:537544.
Kaplan HS. Sexual aversion, sexual
phobias, and panic disorder. New
York: Brunner: Mazel, 1987.
Coleman CC, King BR, BoldenWatson C et al. A placebocontrolled comparison of the
effects on sexual functioning of
bupropion sustained release and
fluoxetine. Clin Ther
2001;23:1040101058.
Hindermarch I. The behavioral
toxicity of antidepressants: effects
on cognition and sexual function.
Int Clin Psychopharmacol
1998;13 (Suppl. 6):S58.
Balercia G, Boscaro M, Lombardo
F, et al. Sexual symptoms in
endocrine diseases: psychosomatic
perspectives. Psychother
Psychosom 2007;76:134140.
Wincze JP, Carey MP. Sexual
Dysfunction: A Guide for
Assessment and Treatment,
Second Edition. New York:
Guilford Press, 2001.
Meuleman E, Van Lankveld J.
Hypoactive sexual desire disorder:
an underestimated condition in
men. Presented at University
Medical Centre St Radboud and
Pompekliniek, Nijmegen, the
Netherlands. 12 July 2004.
Douglas N. Sleep apnea. In: Fauci
AS, Braunwald E, Kasper DL
(eds). Harrisons Principles of
Internal Medicine, Seventeenth
Edition. New York: McGraw Hill,
16.
17.
18.
19.
20.
21.
22.
24.
25.
26.
2008.
Abdallah RT, Simon JA.
Testosterone therapy in women: its
role in the management of
hypoactive sexual desire disorder.
Int J Impotence Res
2007;19:458463.
Shifren JL, Braunstein GD, Simon
JA, et al. Transdermal testosterone
treatment in women with impaired
sexual function after
oophorectomy. N Engl J Med
2000;343:682688.
Basson R. Womens sexual
dysfunction: revised and expanded
sexual definitions. CMAJ
2005;172(10):13271333.
Stahl SM. Essential
Psychopharmacology:
Neuroscientific Basis and
Practical Applications, Second
Edition. New York: Cambridge
University Press, 2000.
Trudel G, Marchand A, Ravart M,
et al. The effect of a cognitivebehavioral group treatment
program on hypoactive sexual
desire in women. Sex Relat Ther
2001;16:145164.
Ellis A, Harper R. A New Guide to
Rational Living. Chatsworth, CA:
Wilshire Book Company, 1975
Crenshaw TL, Goldberg JP. Sexual
Pharmacology: Drugs That Affect
Sexual Functioning. New York,
W. W. Norton & Company, 1996.
Crenshaw TL. The sexual aversion
syndrome. J Sex Marital Ther
1985;11:285292.
Ponticas Y. Sexual aversion versus
hypoactive sexual desire: a
diagnostic challenge. Psychiatr
Med 1992;10:273281.
Crenshaw TL, Goldberg JP, Stern
27.
28.
29.
30.
31.
32.
33.
34.
WC. Pharmacologic modification of
psychosexual dysfunction. J Sex
Marital Ther 1987;13:239252.
Morales A, Heaton JP. Hormonal
erectile dysfunction. Evaluation
and management. Urol Clin North
Am 2001;28:279288.
Waxenberg SE, Drellich MG,
Sutherlamd AM. The role of
hormones in human behavior. I.
Changes in female sexuality after
adrenalectomy. J Clin Endocrinol
Metab 1959;19:193202.
Basson R. Androgen replacement
for women. Can Fam Physician
1999;45:21002107.
Guay AT, Jacobson J. Decreased
free testosterone and
dehydroepiandrosterone-sulfate
(DHEA-S) levels in women with
decreased libido. J Sex Marital
Ther 2002;28(Suppl 1):129142.
Arlt W, Callies F, van Vlijmen JC, et
al. Dehydroepiandrosterone
replacement in women with
adrenal insufficiency. N Engl J
Med 1999;341:10131020.
Walsh KE, Berman JR. Sexual
dysfunction in the older woman: an
overview of the current
understanding and management.
Drugs Aging 2004;21:655675.
Segraves R, Clayton A, Croft H, et
al. Bupropin sustained release for
the treatment of sexual desire
disorder in premenopausal women.
J Clin Psychopharmacol
2004;3:339342.
OCarroll R, Bancroft J.
Testosterone therapy for low
sexual interest and erectile
dysfunction in men: a controlled
study. Br J Psychiatry
1984;145:146151.
[JUNE]
Psychiatry 2008
55
Você também pode gostar
- Overcoming Sexual Deficiency: A Comprehensive Guide to Restoring IntimacyNo EverandOvercoming Sexual Deficiency: A Comprehensive Guide to Restoring IntimacyAinda não há avaliações
- Sexuality and Sexual DisordersDocumento13 páginasSexuality and Sexual DisordersCharmaigne Aurdane PajeAinda não há avaliações
- Decoding Male Sexual Disorders: A Comprehensive Guide for Patients and PartnersNo EverandDecoding Male Sexual Disorders: A Comprehensive Guide for Patients and PartnersAinda não há avaliações
- Icu BookDocumento140 páginasIcu BookRaMy “MhMd” ElaRabyAinda não há avaliações
- Power BI AssignmentDocumento147 páginasPower BI AssignmentAditya SharmaAinda não há avaliações
- Medical Record StaffDocumento84 páginasMedical Record StaffTuan DzungAinda não há avaliações
- List of DisordersDocumento4 páginasList of DisordersRain Simonette GuanAinda não há avaliações
- Maternal Mortality Rates Report For 2022Documento5 páginasMaternal Mortality Rates Report For 2022ABC Action NewsAinda não há avaliações
- Nonoperating Room Anesthesia Anesthesia in The Gastrointestinal SuiteDocumento16 páginasNonoperating Room Anesthesia Anesthesia in The Gastrointestinal SuiteGustavo ParedesAinda não há avaliações
- Sexual DisordersDocumento18 páginasSexual DisordersKadek Fabrian KhamandanuAinda não há avaliações
- Poverty & Sex TraffickingDocumento11 páginasPoverty & Sex TraffickingBryan GraczykAinda não há avaliações
- 06 Addictive and Sexual DisordersDocumento58 páginas06 Addictive and Sexual DisordersSteven T.Ainda não há avaliações
- Social Work and Resouces Development in Malaysia PDFDocumento76 páginasSocial Work and Resouces Development in Malaysia PDFErmanita AnikAinda não há avaliações
- Social Work Practice With DisabilityDocumento34 páginasSocial Work Practice With DisabilityNamrata SinhaAinda não há avaliações
- Sex Trafficking EssayDocumento11 páginasSex Trafficking EssayInked LacunaAinda não há avaliações
- Anggota BadanDocumento1 páginaAnggota BadanAinurNazuraAinda não há avaliações
- Welcome To N.G Acharya and D.K. Maratha College: - Aditya NashteDocumento5 páginasWelcome To N.G Acharya and D.K. Maratha College: - Aditya NashteTHE ELECTRONIC SQUADAinda não há avaliações
- CATIE Trial Summary PaperDocumento14 páginasCATIE Trial Summary PaperNim RodAinda não há avaliações
- Diabetic Foot Ulcer ClinicalDocumento28 páginasDiabetic Foot Ulcer Clinicaladharia78Ainda não há avaliações
- Anesthesia and Sedation Outside ofDocumento9 páginasAnesthesia and Sedation Outside ofPutriRahayuMoidadyAinda não há avaliações
- Sexual DysfunctionDocumento14 páginasSexual DysfunctionMik Leigh CruzAinda não há avaliações
- Pharmacology of Sexually Compulsive BehaviorDocumento9 páginasPharmacology of Sexually Compulsive Behaviorsara_vonAinda não há avaliações
- SHypo Active Sexual Desire DisorderDocumento74 páginasSHypo Active Sexual Desire Disorderimdad MagfurAinda não há avaliações
- Psychiatric Medicine II The Sexual Disorders Meg Kaplan, PH.DDocumento10 páginasPsychiatric Medicine II The Sexual Disorders Meg Kaplan, PH.DPradeep100% (1)
- Nzomo Elijah MutuaDocumento6 páginasNzomo Elijah MutuaElijahAinda não há avaliações
- 3.-Func y Disf Sex FemeninaDocumento15 páginas3.-Func y Disf Sex FemeninaCristina Bravo100% (1)
- Factors of Sexual DysfunctionDocumento5 páginasFactors of Sexual Dysfunctionaftab khanAinda não há avaliações
- Female Sexual Dysfunction - Sexual Pain DisordersDocumento44 páginasFemale Sexual Dysfunction - Sexual Pain DisordersDian Wijayanti100% (1)
- Sexuality in Older AdultDocumento10 páginasSexuality in Older AdultNisa100% (1)
- ReportDocumento10 páginasReportCindy Mae CamohoyAinda não há avaliações
- Psychosexual DisordersDocumento12 páginasPsychosexual DisordersEJ07100% (1)
- Sexuality and Its Disorders - 1Documento21 páginasSexuality and Its Disorders - 1Adepeju Adedokun AjayiAinda não há avaliações
- How Does Premature Ejaculation Impact A Man S LifeDocumento11 páginasHow Does Premature Ejaculation Impact A Man S LifeSubham TalukdarAinda não há avaliações
- Female Sexual: Assessing & ManagingDocumento8 páginasFemale Sexual: Assessing & ManagingJazmin GarcèsAinda não há avaliações
- Psychiatry SeminarDocumento152 páginasPsychiatry SeminarMichael GebreamlakAinda não há avaliações
- Sexual and Gender Identity DisorderDocumento13 páginasSexual and Gender Identity DisorderWillington ShinyAinda não há avaliações
- Sexual Disorders or Sexual Dysfunction: Linda C. Shafer, M.DDocumento14 páginasSexual Disorders or Sexual Dysfunction: Linda C. Shafer, M.DNur AzizaAinda não há avaliações
- To TransgenderHealth 2015Documento4 páginasTo TransgenderHealth 2015kiki leungAinda não há avaliações
- HypersexualityDocumento7 páginasHypersexualitysuzyAinda não há avaliações
- Lecture 6 Part 2Documento35 páginasLecture 6 Part 2Natia Badridze100% (1)
- Psychosexual DisordersDocumento22 páginasPsychosexual DisordersMaria Zamantha GatchalianAinda não há avaliações
- Female Sexual DysfunctionDocumento18 páginasFemale Sexual DysfunctionRisky SetiawanAinda não há avaliações
- Write Up On Aphrodisiac by Sanusi OluwagbotemiDocumento41 páginasWrite Up On Aphrodisiac by Sanusi OluwagbotemiOLUWAGBOTEMI SANUSIAinda não há avaliações
- Psychosexual DisordersDocumento7 páginasPsychosexual Disordersvivek100% (1)
- By: DR Aini SimonDocumento54 páginasBy: DR Aini SimonRusman BustamanAinda não há avaliações
- Treatment of Sexual DysfunctionDocumento70 páginasTreatment of Sexual DysfunctionCeleste Velasco100% (4)
- Sexual Dysfunctions Self StudyDocumento6 páginasSexual Dysfunctions Self StudymelissagoldenAinda não há avaliações
- Abnormal Psychology IiDocumento3 páginasAbnormal Psychology Iipujitha7122Ainda não há avaliações
- SLP MM20705 Psychosexual Disorders 2019.3.17 PDFDocumento7 páginasSLP MM20705 Psychosexual Disorders 2019.3.17 PDFBrandonRyanF.MosidinAinda não há avaliações
- Antidepressants and Sexual DysfunctionDocumento15 páginasAntidepressants and Sexual DysfunctionGe NomAinda não há avaliações
- Sexual Dysfunctions, Paraphilic Disorders & Gender DysphoriaDocumento23 páginasSexual Dysfunctions, Paraphilic Disorders & Gender DysphoriaJosh Polo100% (3)
- Sexual & Gender Identity DisordersDocumento41 páginasSexual & Gender Identity Disordersrmconvidhya sri2015Ainda não há avaliações
- SexdysguidDocumento19 páginasSexdysguidhitchbashaAinda não há avaliações
- Factsheet: Low Libido (Sexual Desire)Documento1 páginaFactsheet: Low Libido (Sexual Desire)vdphbfiuAinda não há avaliações
- Phases of The Sexual Response CycleDocumento7 páginasPhases of The Sexual Response CyclesimonAinda não há avaliações
- Nejmcp1008161.Pdf - Care of Transsexual PersonsDocumento7 páginasNejmcp1008161.Pdf - Care of Transsexual PersonsCarol RochaAinda não há avaliações
- Sexual Problems EssayDocumento2 páginasSexual Problems EssayPAMELA CLAUDIA SORIAAinda não há avaliações
- Sexual & Gender Identity DisordersDocumento42 páginasSexual & Gender Identity DisordersVikas SamotaAinda não há avaliações
- Sexual Disorders FinalllllDocumento35 páginasSexual Disorders FinalllllYohanes Bosco Panji PradanaAinda não há avaliações
- Systemic Rituals in Sexual Therapy by Gary L. SandersDocumento17 páginasSystemic Rituals in Sexual Therapy by Gary L. SandersOlena BaevaAinda não há avaliações
- The Social SelfDocumento7 páginasThe Social SelfPatricia Ann PlatonAinda não há avaliações
- Mental Health Team by Delicia Ann SDocumento3 páginasMental Health Team by Delicia Ann SDelicia SohtunAinda não há avaliações
- An Overview of Sigmund Freud's TheoriesDocumento13 páginasAn Overview of Sigmund Freud's TheoriesChi NguyễnAinda não há avaliações
- Intro Abnormal PsychologyDocumento30 páginasIntro Abnormal Psychology1989920198950% (2)
- Introduction To Cognitive and Physiological Psychology Week1v2Documento33 páginasIntroduction To Cognitive and Physiological Psychology Week1v2Odaine BennettAinda não há avaliações
- Developing Professional CapacityDocumento6 páginasDeveloping Professional Capacityapi-476189522Ainda não há avaliações
- Istrazivanja Moralnog Razvoja I Moralnog PDFDocumento23 páginasIstrazivanja Moralnog Razvoja I Moralnog PDFlejla13Ainda não há avaliações
- 2 - Management of InstructionDocumento15 páginas2 - Management of InstructionMyla Ebillo100% (4)
- Specific Learning DisabilitiesDocumento44 páginasSpecific Learning DisabilitiesNeeti Moudgil100% (1)
- Linda Leonard - The Puella and The Perverted Old ManDocumento12 páginasLinda Leonard - The Puella and The Perverted Old ManIuliana IgnatAinda não há avaliações
- Types of Speech ContextDocumento2 páginasTypes of Speech ContextKatrina Jade Pajo79% (14)
- 01-People - Psychology - CXL Institute PDFDocumento1 página01-People - Psychology - CXL Institute PDFEarl CeeAinda não há avaliações
- Educ1 Module 1Documento10 páginasEduc1 Module 1Kristina Marie lagartoAinda não há avaliações
- AT2 Tivar VictorioDocumento2 páginasAT2 Tivar VictorioVic TivarAinda não há avaliações
- Ed. 421 Ed. PsychologyDocumento7 páginasEd. 421 Ed. PsychologyHari Prasad100% (1)
- Abridged Report Executive SummaryDocumento5 páginasAbridged Report Executive SummaryledermandAinda não há avaliações
- EMDR WorksheetDocumento2 páginasEMDR WorksheetEcaterina IacobAinda não há avaliações
- Empathy, Mimesis, Magic of AlterityDocumento31 páginasEmpathy, Mimesis, Magic of AlterityVinícius Pedreira100% (1)
- What Is Classroom Observation Guide For ReportingDocumento4 páginasWhat Is Classroom Observation Guide For ReportingMark Bryan CervantesAinda não há avaliações
- Running Head: DRIVING MISS DAISY 1Documento11 páginasRunning Head: DRIVING MISS DAISY 1api-216578352Ainda não há avaliações
- The Hearing Voices Movement: Sandra Escher and Marius RommeDocumento9 páginasThe Hearing Voices Movement: Sandra Escher and Marius RommeJavier Ladrón de Guevara MarzalAinda não há avaliações
- Report For Cynefin FrameworkDocumento3 páginasReport For Cynefin FrameworkAlfadzly AlliAinda não há avaliações
- Kormbip 2Documento300 páginasKormbip 2DerickAinda não há avaliações
- CAS 104-Human Relations and Group DynamicsDocumento46 páginasCAS 104-Human Relations and Group DynamicsERVY BALLERASAinda não há avaliações
- 2ND CotDocumento14 páginas2ND CotJessa MolinaAinda não há avaliações
- Exceptional MemoryDocumento9 páginasExceptional MemoryDoina MiruzarAinda não há avaliações
- Burnout in CounselingDocumento54 páginasBurnout in CounselingmokaAinda não há avaliações
- Barrett's TaxonomyDocumento19 páginasBarrett's TaxonomyAlice100% (5)
- PART 1 Health Assessment Lec Prelim TransesDocumento11 páginasPART 1 Health Assessment Lec Prelim TransesLoLiAinda não há avaliações
- Gender ContinuumDocumento3 páginasGender ContinuumTrisha MariehAinda não há avaliações
- Tears of the Silenced: An Amish True Crime Memoir of Childhood Sexual Abuse, Brutal Betrayal, and Ultimate SurvivalNo EverandTears of the Silenced: An Amish True Crime Memoir of Childhood Sexual Abuse, Brutal Betrayal, and Ultimate SurvivalNota: 4.5 de 5 estrelas4.5/5 (136)
- The Longest Race: Inside the Secret World of Abuse, Doping, and Deception on Nike's Elite Running TeamNo EverandThe Longest Race: Inside the Secret World of Abuse, Doping, and Deception on Nike's Elite Running TeamNota: 5 de 5 estrelas5/5 (59)
- You Can Thrive After Narcissistic Abuse: The #1 System for Recovering from Toxic RelationshipsNo EverandYou Can Thrive After Narcissistic Abuse: The #1 System for Recovering from Toxic RelationshipsNota: 5 de 5 estrelas5/5 (16)
- Unwanted Advances: Sexual Paranoia Comes to CampusNo EverandUnwanted Advances: Sexual Paranoia Comes to CampusNota: 4 de 5 estrelas4/5 (22)
- Emotional Abuse: Recovering and Healing from Toxic Relationships, Parents or Coworkers while Avoiding the Victim MentalityNo EverandEmotional Abuse: Recovering and Healing from Toxic Relationships, Parents or Coworkers while Avoiding the Victim MentalityNota: 5 de 5 estrelas5/5 (12)
- The Myth of Repressed Memory: False Memories and Allegations of Sexual AbuseNo EverandThe Myth of Repressed Memory: False Memories and Allegations of Sexual AbuseNota: 3 de 5 estrelas3/5 (6)
- What Is a Girl Worth?: My Story of Breaking the Silence and Exposing the Truth about Larry Nassar and USA GymnasticsNo EverandWhat Is a Girl Worth?: My Story of Breaking the Silence and Exposing the Truth about Larry Nassar and USA GymnasticsNota: 4.5 de 5 estrelas4.5/5 (40)
- Unbound: My Story of Liberation and the Birth of the Me Too MovementNo EverandUnbound: My Story of Liberation and the Birth of the Me Too MovementNota: 5 de 5 estrelas5/5 (147)
- The Courage to Heal: A Guide for Women Survivors of Child Sexual AbuseNo EverandThe Courage to Heal: A Guide for Women Survivors of Child Sexual AbuseAinda não há avaliações
- Body Language for Women: Learn to Read People Instantly and Increase Your InfluenceNo EverandBody Language for Women: Learn to Read People Instantly and Increase Your InfluenceNota: 5 de 5 estrelas5/5 (1)
- In the Body of the World: A Memoir of Cancer and ConnectionNo EverandIn the Body of the World: A Memoir of Cancer and ConnectionNota: 4.5 de 5 estrelas4.5/5 (68)
- Dear Professor: A Woman's Letter to Her StalkerNo EverandDear Professor: A Woman's Letter to Her StalkerNota: 4 de 5 estrelas4/5 (157)
- QAnon & the #Pizzagates of Hell: Unreal Tales of Occult Child Abuse by the CIANo EverandQAnon & the #Pizzagates of Hell: Unreal Tales of Occult Child Abuse by the CIANota: 3 de 5 estrelas3/5 (2)
- Girls Like Us: Fighting for a World Where Girls Are Not for Sale, an Activist Finds Her Calling and Heals HerselfNo EverandGirls Like Us: Fighting for a World Where Girls Are Not for Sale, an Activist Finds Her Calling and Heals HerselfNota: 4.5 de 5 estrelas4.5/5 (49)
- Unheard Screams: A True Childhood Horror Story of a CODA Survivor and How She Overcame Her Father's Sexual AbuseNo EverandUnheard Screams: A True Childhood Horror Story of a CODA Survivor and How She Overcame Her Father's Sexual AbuseAinda não há avaliações
- Breaking the Silence Habit: A Practical Guide to Uncomfortable Conversations in the #MeToo WorkplaceNo EverandBreaking the Silence Habit: A Practical Guide to Uncomfortable Conversations in the #MeToo WorkplaceAinda não há avaliações
- I Love You Baby Girl... A heartbreaking true story of child abuse and neglect.No EverandI Love You Baby Girl... A heartbreaking true story of child abuse and neglect.Nota: 3.5 de 5 estrelas3.5/5 (7)
- Invisible Abuse - Instantly Spot the Covert Deception and Manipulation Tactics of Narcissists, Effortlessly Defend From and Disarm Them, and Effectively Recover: Deep Relationship Healing and RecoveryNo EverandInvisible Abuse - Instantly Spot the Covert Deception and Manipulation Tactics of Narcissists, Effortlessly Defend From and Disarm Them, and Effectively Recover: Deep Relationship Healing and RecoveryNota: 5 de 5 estrelas5/5 (2)
- Somebody's Daughter: Inside an International Prostitution RingNo EverandSomebody's Daughter: Inside an International Prostitution RingNota: 5 de 5 estrelas5/5 (3)
- Damaged: The Heartbreaking True Story of a Forgotten ChildNo EverandDamaged: The Heartbreaking True Story of a Forgotten ChildNota: 4 de 5 estrelas4/5 (131)
- Understanding Sexual Abuse: A Guide for Ministry Leaders and SurvivorsNo EverandUnderstanding Sexual Abuse: A Guide for Ministry Leaders and SurvivorsNota: 3.5 de 5 estrelas3.5/5 (3)