Escolar Documentos
Profissional Documentos
Cultura Documentos
Urinary Incontinence From Harrison's IM
Enviado por
nashey08Descrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Urinary Incontinence From Harrison's IM
Enviado por
nashey08Direitos autorais:
Formatos disponíveis
Urinary Incontinence Urinary incontinence (UI), the involuntary leakage of urine, is highly prevalent in older persons, especially in older
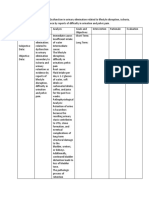
women, and has a profound negative impact on quality of life. Approximately 50% of American women will suffer from some form of UI over a lifetime. Increasing age, white race, childbirth, obesity, and medical comorbidity are all risk factors for UI. The three main clinical forms of UI are as follows: (1) Stress incontinence is the failure of the sphincteric mechanism to remain closed when there is a sudden increase in intraabdominal pressure, such as a cough or sneeze. In women, this condition is due to insufficient strength of the pelvic floor muscles, while in men it is almost exclusively secondary to prostate surgery. (2) Urge incontinence is the loss of urine accompanied by a sudden sensation of need to urinate and is due to detrusor muscle overactivity (lack of inhibition) due to loss of neurologic control or local irritation. (3) Overflow incontinence is characterized by urinary dribbling, either constantly or for some period after urination. This condition is due to impaired detrusor contractility (due usually to denervation, for example, in diabetes) or bladder outlet obstruction (prostate hypertrophy in men and cystocele in women). Thus, not surprisingly, the pathogenesis of urinary incontinence is connected to the disrupted aging systems that contribute to frailty, body composition changes (atrophy of the bladder and pelvic floor muscle), and neurodegeneration (both central and peripheral nervous systems). Frailty is a strong risk factor for urinary incontinence. Indeed, older women are more likely to have mixed (urge+stress) incontinence than any pure form (Fig. 72-18). In analogy with the other geriatric syndromes, UI derives from a predisposing condition superimposed on a stressful, precipitating factor. Accordingly, treatment of UI should address both. The first line of treatment is bladder training associated with pelvic muscle exercise (Kegel exercises) that sometimes should be associated with electrical stimulation. Those with possible vaginal or uterine prolapse should be referred to a specialist. Urinary infections should be investigated and eventually treated. A long list of medications can precipitate urinary incontinence, including diuretics, antidepressants, sedative hypnotics, adrenergic agonists or blockers, anticholinergic, and calcium channel blockers. Whenever possible, these medications
should be discontinued. Until recently, it was believed that estrogen oral or local treatments improved the UI symptoms in postmenopausal women, but this notion is now controversial. Antimuscarinic drugs such as tolterodine, darifenacin, and fesoterodine are modestly effective for mixed incontinence, but they all can affect cognition and so must be used with caution and careful follow-up monitoring of cognitive status. In some cases, surgical treatment should be considered. Chronic catheterization has many adverse effects and should be limited to chronic urinary retention that cannot be managed in any other way. Bacteriuria always occurs and should be treated only if symptomatic.
Você também pode gostar
- Urinary IncontinenceDocumento7 páginasUrinary IncontinenceasuratosAinda não há avaliações
- Urinary Incontinence in The Older Adult: by Kristen Cook, Pharm.D., BCPS and Linda M. Sobeski, Pharm.D., BCPSDocumento18 páginasUrinary Incontinence in The Older Adult: by Kristen Cook, Pharm.D., BCPS and Linda M. Sobeski, Pharm.D., BCPSNurul HafizaAinda não há avaliações
- كوزرملا حاضو .د .م.أ لباب ةعماج/ بطلا ةيلك 2019 Urinary Incontinence. Involuntary loss of urine in sufficient amount or frequency to constituteDocumento8 páginasكوزرملا حاضو .د .م.أ لباب ةعماج/ بطلا ةيلك 2019 Urinary Incontinence. Involuntary loss of urine in sufficient amount or frequency to constitutewzeer mohammedAinda não há avaliações
- Menopause - StatPearls - NCBI BookshelfDocumento8 páginasMenopause - StatPearls - NCBI BookshelfMichael HusainAinda não há avaliações
- Pharma-URO-U IncontinenceDocumento27 páginasPharma-URO-U IncontinenceHussein AlhaddadAinda não há avaliações
- Presentation 3Documento34 páginasPresentation 3Chidube UkachukwuAinda não há avaliações
- Pathomechanisms - Doc Bali 2010.doc RevisiDocumento14 páginasPathomechanisms - Doc Bali 2010.doc RevisiApriliaAinda não há avaliações
- Geriatric Urologic Disorder: Assignment 1 Name:moubark Saad Alsubaie Id:201713512 To Dr:kashifDocumento7 páginasGeriatric Urologic Disorder: Assignment 1 Name:moubark Saad Alsubaie Id:201713512 To Dr:kashifmoubarkAinda não há avaliações
- Urinary IncontienceDocumento102 páginasUrinary IncontienceHussein AlhaddadAinda não há avaliações
- Urinary Incontinence in Men - UpToDateDocumento31 páginasUrinary Incontinence in Men - UpToDatehochanh199xAinda não há avaliações
- Diagnosis & Management of Urinary Incontinence: G. M. Punarbawa RSUD Prov NTB/FK UNRAMDocumento39 páginasDiagnosis & Management of Urinary Incontinence: G. M. Punarbawa RSUD Prov NTB/FK UNRAMfarlamayanti100% (1)
- Urinary Incontinence in Individuals With Diabetes MellitusDocumento1 páginaUrinary Incontinence in Individuals With Diabetes MellitusBulan GhafirahAinda não há avaliações
- Fecal IncontinenceDocumento5 páginasFecal IncontinenceDaniel Galindo SotomayorAinda não há avaliações
- MenopauseDocumento14 páginasMenopauseMizna SabillaAinda não há avaliações
- Acute Urinary Retention....Documento27 páginasAcute Urinary Retention....Dr. ShireenAinda não há avaliações
- Incontinentia Urine: HasnawatyDocumento12 páginasIncontinentia Urine: HasnawatyafatspAinda não há avaliações
- Developing Geriatric Services For Incontinence in The ElderlyDocumento5 páginasDeveloping Geriatric Services For Incontinence in The ElderlyrnrmmanphdAinda não há avaliações
- Management of Urinary Incontinence in Frail Elderly Women: PrevalenceDocumento7 páginasManagement of Urinary Incontinence in Frail Elderly Women: PrevalenceKaren MoctezumaAinda não há avaliações
- UntitledDocumento22 páginasUntitledAnurag DwivediAinda não há avaliações
- EtiologyDocumento15 páginasEtiologyrendyjiwonoAinda não há avaliações
- Managing Urinary Tract Problem: FOCUS On The FollowingDocumento11 páginasManaging Urinary Tract Problem: FOCUS On The FollowingLovely DaroleAinda não há avaliações
- Female Urinary Retention - StatPearls - NCBI BookshelfDocumento26 páginasFemale Urinary Retention - StatPearls - NCBI BookshelfjqgjwgnnwkAinda não há avaliações
- Urinary Incontinence: Diagnostic Evaluation and First-Line TreatmentDocumento11 páginasUrinary Incontinence: Diagnostic Evaluation and First-Line Treatmentstalker2222Ainda não há avaliações
- Sci Bladder ProtocolDocumento45 páginasSci Bladder ProtocolAbbas JafarzadehabbasAinda não há avaliações
- Climacterium - Sundhed - DKDocumento9 páginasClimacterium - Sundhed - DKPavel BerlinschiAinda não há avaliações
- Lec. 3 - Urogynaecology and Urinary ProlapseDocumento9 páginasLec. 3 - Urogynaecology and Urinary ProlapseDr-Saja O. DmourAinda não há avaliações
- Pathophysiology of Female LUTS: 1 Storage DysfunctionDocumento10 páginasPathophysiology of Female LUTS: 1 Storage DysfunctionJaneva SihombingAinda não há avaliações
- 3028 Manuscript 19093 1 10 20210629Documento13 páginas3028 Manuscript 19093 1 10 20210629stella.gillesania.chenAinda não há avaliações
- Overview On The Management of Adult Urinary IncontinenceDocumento7 páginasOverview On The Management of Adult Urinary IncontinenceMUHAMMMAD FAKHRIAinda não há avaliações
- Urinary IncontinenceDocumento17 páginasUrinary IncontinenceMohamed Na3eemAinda não há avaliações
- 1 s2.0 S183695532100014X MainDocumento8 páginas1 s2.0 S183695532100014X MainMetin HakkanAinda não há avaliações
- Pathophysiology of Urinary Incontinence: Basic ScienceDocumento6 páginasPathophysiology of Urinary Incontinence: Basic ScienceLauris TrujilloAinda não há avaliações
- Overaktifitas Kandung KemihDocumento4 páginasOveraktifitas Kandung KemihSarah PerezAinda não há avaliações
- Aging Changes in The Female Reproductive SystemDocumento6 páginasAging Changes in The Female Reproductive SystemMin JEeAinda não há avaliações
- Urinary Incontinence Has Sesven TypesDocumento55 páginasUrinary Incontinence Has Sesven TypesDhonat Flash100% (1)
- Male Urinary Retention - StatPearls - NCBI BookshelfDocumento9 páginasMale Urinary Retention - StatPearls - NCBI BookshelfMuh Ikhlasul AmalAinda não há avaliações
- Geriatric Urinary Incontinence & UTI CaseDocumento9 páginasGeriatric Urinary Incontinence & UTI CaseStarr NewmanAinda não há avaliações
- Menopause NotesDocumento5 páginasMenopause NotesJU WSD100% (1)
- A Written Output Gerontology: Submitted byDocumento15 páginasA Written Output Gerontology: Submitted bypetite15Ainda não há avaliações
- Urogynecology and Pelvic ReconstructionDocumento28 páginasUrogynecology and Pelvic ReconstructionIKM FKUNSOEDAinda não há avaliações
- Overview of Urinary Incontinence (UI) in The Long Term Care FacilityDocumento81 páginasOverview of Urinary Incontinence (UI) in The Long Term Care Facilityالغزال الذهبيAinda não há avaliações
- Urinary IncontinenceDocumento18 páginasUrinary IncontinenceShatha QudahAinda não há avaliações
- Urinary Incontinence in Elderly: DefinitionDocumento13 páginasUrinary Incontinence in Elderly: DefinitionTarek AhmedAinda não há avaliações
- About Urinary IncontinenceDocumento6 páginasAbout Urinary IncontinenceRitesh SinghAinda não há avaliações
- Lower Urinary Tract Symptoms (LUTS) in Middle-Aged and Elderly MenDocumento6 páginasLower Urinary Tract Symptoms (LUTS) in Middle-Aged and Elderly MenIrfanArifZulfikarAinda não há avaliações
- MedSurg Chapter 66 OutlineDocumento7 páginasMedSurg Chapter 66 OutlineJosephine NavarroAinda não há avaliações
- Original Article: Effects of Kegel Exercises Applied To Urinary Incontinence On Sexual SatisfactionDocumento10 páginasOriginal Article: Effects of Kegel Exercises Applied To Urinary Incontinence On Sexual SatisfactionAnonymous XxK0PcDEsAinda não há avaliações
- GBHLN5 PR QHNP 5 Sy 5 CJDJ DFSDocumento8 páginasGBHLN5 PR QHNP 5 Sy 5 CJDJ DFSyasmim16catarinaAinda não há avaliações
- Ariel Pemicu 5Documento37 páginasAriel Pemicu 5yuliAinda não há avaliações
- Postpartum Physical TherapyDocumento10 páginasPostpartum Physical TherapyMaya VilAinda não há avaliações
- Pathophysiology 1. Urinary Incontinence PathophysiologyDocumento6 páginasPathophysiology 1. Urinary Incontinence PathophysiologyDenny BunAinda não há avaliações
- Bab IiDocumento32 páginasBab Iiayamin musri suryaminAinda não há avaliações
- Urinary IncontinenceDocumento16 páginasUrinary IncontinenceOana BalintAinda não há avaliações
- Inkontinensia UrinDocumento36 páginasInkontinensia UrinWhydia Wedha SutedjaAinda não há avaliações
- Types of Urinary Incontinence - Harvard HealthDocumento11 páginasTypes of Urinary Incontinence - Harvard HealthJimmy GillAinda não há avaliações
- Postmenopausal Syndrome: Pronob K. Dalal, Manu AgarwalDocumento11 páginasPostmenopausal Syndrome: Pronob K. Dalal, Manu Agarwalwidya astutyloloAinda não há avaliações
- Women With Cronic Pelvic Pain. An Osteopathic Approach PDFDocumento3 páginasWomen With Cronic Pelvic Pain. An Osteopathic Approach PDFHapplo82Ainda não há avaliações
- CDN JU28 I4S2 10 DrDenisenkoSDocumento6 páginasCDN JU28 I4S2 10 DrDenisenkoSCATHERIN JULIANA LIZANA BERRUAinda não há avaliações
- DM Dan No. 1 Urine Incontinence - Id.enDocumento2 páginasDM Dan No. 1 Urine Incontinence - Id.enAndi Widya Nirwana NingsihAinda não há avaliações
- Long Term Care ServicesDocumento8 páginasLong Term Care ServicesCole GoAinda não há avaliações
- NCP-impaired Urinary Elimination-TAHBSODocumento3 páginasNCP-impaired Urinary Elimination-TAHBSOtinatin9890% (1)
- Fistula Genital Pasca Persalinan UrDATE 2018Documento35 páginasFistula Genital Pasca Persalinan UrDATE 2018Apidha KartinasariAinda não há avaliações
- UroflowmetryDocumento4 páginasUroflowmetryGolam MasudAinda não há avaliações
- Urinary Incontinence As A Possible Signal of Neuromuscular Toxicity During Immune Checkpoint Inhibitor Treatment - Case Report and Retrospective Pharmacovigilance StudyDocumento10 páginasUrinary Incontinence As A Possible Signal of Neuromuscular Toxicity During Immune Checkpoint Inhibitor Treatment - Case Report and Retrospective Pharmacovigilance StudyRA Tri Retno WulanAinda não há avaliações
- CystoceleDocumento4 páginasCystocelesandeepv08Ainda não há avaliações
- Care of ElderlyDocumento37 páginasCare of Elderlymerin sunil100% (2)
- Sindromes GeriatricosDocumento7 páginasSindromes Geriatricoseduardo lopezAinda não há avaliações
- ACE MRCOG Part II and III Syllabus Checklist 2018 AUADocumento13 páginasACE MRCOG Part II and III Syllabus Checklist 2018 AUABharat GAinda não há avaliações
- Benigna Hiperplasia ProstatDocumento23 páginasBenigna Hiperplasia ProstatShanti ArianiAinda não há avaliações
- Bladder Training (For Resident With A Catheter)Documento2 páginasBladder Training (For Resident With A Catheter)Charley Degamo100% (1)
- Female Genital Mutilation (FGM) Frequently Asked QuestionsDocumento47 páginasFemale Genital Mutilation (FGM) Frequently Asked QuestionsfdskndAinda não há avaliações
- PenisEnlargementBible PDFDocumento19 páginasPenisEnlargementBible PDFQhomeke Hlabathe67% (3)
- Impaired Urinary EliminatonDocumento5 páginasImpaired Urinary EliminatonLoriejae Marie DesulocAinda não há avaliações
- Abram Study NotesDocumento6 páginasAbram Study Notesteeman2Ainda não há avaliações
- Moms Into Fitness Prenatal Postnatal Exercise GuideDocumento19 páginasMoms Into Fitness Prenatal Postnatal Exercise GuideSanket YamgawaliAinda não há avaliações
- Physiologic Changes in ElderlyDocumento6 páginasPhysiologic Changes in ElderlyAngelie PantajoAinda não há avaliações
- Applying The Three Levels of Prevention in Elderly CareDocumento17 páginasApplying The Three Levels of Prevention in Elderly CareSalma AbdullahAinda não há avaliações
- A Critical Review of The Waterlow ToolDocumento6 páginasA Critical Review of The Waterlow ToolHardeep Singh BaliAinda não há avaliações
- A Case of Prolonged Postpartum Urinary Retention: An Obstetrician's Dilemmas'Documento3 páginasA Case of Prolonged Postpartum Urinary Retention: An Obstetrician's Dilemmas'noony 98Ainda não há avaliações
- Gerontological Nursing LectureDocumento18 páginasGerontological Nursing Lecturenonalynne8056150% (2)
- Nursing SciencesDocumento23 páginasNursing SciencesHermann CHEMEUHIAinda não há avaliações
- Concept of EliminationDocumento42 páginasConcept of EliminationOpen UserAinda não há avaliações
- Nle June 2007Documento59 páginasNle June 2007ocampotutorialsAinda não há avaliações
- The Gynecologic History and Pelvic Examination Up To Date 2016Documento14 páginasThe Gynecologic History and Pelvic Examination Up To Date 2016Mateo GlAinda não há avaliações
- Urological Complications of Uterine Leiomyoma: A Review of LiteratureDocumento9 páginasUrological Complications of Uterine Leiomyoma: A Review of LiteratureAmalia Tata NirwanaAinda não há avaliações
- Gero Nurse ExamDocumento33 páginasGero Nurse ExamEghosa Osagie100% (9)
- Doctorwriting7 1531890392220Documento3 páginasDoctorwriting7 1531890392220Haris Kalim YousafzaiAinda não há avaliações
- Benign Prostate HypertrophyDocumento22 páginasBenign Prostate Hypertrophyjyoti kunduAinda não há avaliações