Escolar Documentos
Profissional Documentos
Cultura Documentos
Diabetes Mellitus Type 2, Formerly Known As Non-Insulin-Dependent Diabetes
Enviado por
donlynDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Diabetes Mellitus Type 2, Formerly Known As Non-Insulin-Dependent Diabetes
Enviado por
donlynDireitos autorais:
Formatos disponíveis
DISCUSSION OF THE PATHOPHYSIOLOGY FOR TYPE 2 DIABETES MELLITUS Diabetes mellitus type 2, formerly known as non-insulin-dependent diabetes mellitus
(NIDDM) or adult-onset diabetes, is a metabolic disorder that is characterized by high blood glucose in the context of insulin resistance and relative insulin deficiency. Type 2 diabetes mellitus is a disorder that disrupts the way your body uses glucose (sugar). Normally, a certain amount of glucose circulates in the blood. The major sources of this glucose are absorption of ingested food in the gastrointestinal tract and formation of glucose by the liver from food substances. All the cells in your body need sugar to keep them in normal function. The two main problems related to insulin in type 2 diabetes mellitus are insulin resistance and impaired insulin secretion by the beta cells in the islets of Langerhans of the pancreas. Insulin resistance refers to decreased tissue sensitivity to insulin. Normally, insulin binds to special receptors on cell surfaces and initiates a series of reactions involved in glucose metabolism. In type 2 diabetes, these intracellular reactions are diminished, making insulin less effective at stimulating glucose uptake by the tissues and at regulating glucose release by the liver. To overcome insulin resistance and to prevent the build up of glucose in the blood, increased amounts of insulin must be secreted to maintain the glucose level at a normal or slightly elevated level. This is called metabolic syndrome, which includes hypertension, hypercholesterolemia, and abdominal obesity. However, if the beta cells cannot keep up with the increased demand for insulin, the glucose level rises and type 2 diabetes mellitus develops. Despite the
impaired insulin secretion that is characteristic of type 2 diabetes, there is enough insulin present to prevent the breakdown of fat and the accompanying production of ketone bodies. Therefore, diabetic ketoacidosis does not typically occur in type 2 diabetes. However, uncontrolled type 2 diabetes may lead to another acute problem called hyperglycemic hyperosmolar nonketotic syndrome. This is a serious condition in which hyperosmolarity and hyperglycemia predominate, with alterations of the sensorium (sense of awareness). The basic biochemical defect is lack of effective insulin. Persistent hyperglycemia causes osmotic diuresis, which results in losses of water and electrolytes. Because type 2 diabetes is associated with a slow, progressive glucose intolerance, its onset may go undetected for many years. If patient experiences symptoms, they are frequently mild. Clinical manifestations depend on the patients level of hyperglycemia. Classic manifestations of all types of diabetes include the three Ps: polyuria (excessive urination), polydipsia (excessive thirst) and polyphagia (excessive hunger). In polyuria, when there is an increase in amount of blood glucose, the amount of glucose reabsorbed by the glomeruli of the kidney exceeds the amount that can be reabsorbed by the renal tubules. By the time the kidneys filter the blood high in glucose level, not all of them may be reabsorbed and the excess will be excreted together with the urine resulting to glycosuria, accompanied with large losses of water in the urine. Polydipsia happens as a result from intracellular dehydration where in when glucose is not able to enter the cell; they tend to pull out the water within the body cell, including those in the thirst center, making the cell dehydrated. Polyphagia causes cellular starvation
since the glucose cannot be transported and metabolized for energy. Symptoms that would prompt a person to seek include fatigue, and weakness, sudden vision changes, tingling or numbness in the hands or feet (paresthesia), dry mouth and dry skin, skin lesions or wounds that are slow to heal, and recurrent infections. Long term complications of diabetes include diabetic retinopathy, which is the leading cause of blindness, diabetic nephropathy or renal disease secondary to diabetic macrovascular changes in the kidney and diabetic neuropathy which refers to a group of disease that affect all types of nerves, including peripheral (sensimotor), autonomic and spinal nerves. Foot and Leg problems are also one complication of diabetes which may require lower extremity amputations to prevent the spread of infection, particularly if it involves the bone (osteomyelitis). Treatment includes lifestyle changes, diet modification, self care measures and medications. If all the signs and symptoms are left untreated and if there is no proper management of the disease, this may result to severe infection and death.
IX. MEDICAL MANAGEMENT A. CLINICAL MANAGEMENT 1. TREATMENT AND PROCEDURES These are interventions done to ensure the safety of patient. 1. Interviewing This is done by the physician or a nurse to gather patients significant health history and to assess the patient.
2. Procedures 1. Vital signs taking closely monitored, any changes are reported because this serves as a baseline data of the patient and will indicate whether the patients condition is progressing or reclining. It is a routine taking of the patients temperature, pulse rate, respiration rate and blood pressure. 2. Intravenous fluid monitoring this is important to prevent overloading and under loading on the patients body. It is also prescribed or given to replace the patients loss fluid and electrolytes and also to replace the excessive loss of blood in the womans body from giving birth or during delivery and to those who have just undergone surgery. 3. Administering oral medication oral medicines are administered or given to the patient as ordered by their physician such as multivitamins with iron this is to replenish the loss blood of the woman from giving birth, antibiotics this is to prevent infection related to the perineal incision and analgesicto relieve pain. 4. Bedside care this is to monitor the patient closely, to help her or assist her in ambulating or if she needs something when her accompanying is not with her. This is also to make the patients bed clean and free from dust. 5. Health teaching this is to provide information to the patient about her condition and the need for her to take her medication and so that she will also take it positively.
6. Intake and Output measurement this is done to monitor patients hydration status. 7. Bed making and environmental sanitation this is done to provide comfort to patient and prevent infection caused by soiled linens and dusty environment. 2. MEDICATIONS 1. piperacillin + tazobactam 4.5 gm IV infusion every 8 hours ANST left arm Date ordered: August 22, 2011 2. catapres 75 mcg SL 1 tab q 6 prn for BP 160/100 Date ordered: August 22, 2011 3. Lifezar 100 mg tab, 1 tab OD Date ordered: August 22, 2011 4. Humulin R 4 U SQ now Date ordered: August 23, 2011 5. Atorvastatin (Avamax) 20 mg, 1 tab once a day q HS Date ordered: August 23, 2011 6. amlodipine 10 mg / tab OD 1st dose now
Date ordered: August 23, 2011 7. Actos 30 mg / tab, 1 tab after lunch Date ordered: August 24, 2011 8. Glucophage 1x XR 750 g / tab,1 tab OD presupper Date ordered: August 24, 2011 9. 0.9% Sodium Chloride (Plain Normal Saline Solution) to run at 20 gtts/min Date ordered: August 22-25,2011 3. DIET The patient was advised to have a strict compliance to her low salt, low fat, and low cholesterol diet. Patient was instructed to increase her fluid intake and increase her in take of foods high in fiber. B. ACTUAL NURSING MANAGEMENT B.1 ACTUAL CARE GIVEN As early as 7:30 in the morning, just a few minutes after the endorsement, the researcher took the vital signs of the patient and plotted it in the chart. She also measured her Intake and Output and recorded it. She checked patient's intravenous fluid whether it needs to be replaced or not or if it still follows its
ordered rate of flow. She asked her patient few questions for her additional data needed for the completion of patients history taking and when patient verbalized some of her concerns, she listened. She stayed for a while in the patients room to attend to her patients needs. She gave her health teachings about
management of her constipation, teachings on infection control and management of her diabetes. She evaluated her patient as to how she responded to her teaching. She also performed bed making on her patient and assured that her patients room would be organized. She was also able to perform sponge bath on her patient and change patients clothes. She was able to perform hand hygiene before and after she entered her patient's room to reduce transmission of microorganisms. She made an FDAR for her patient where in it emphasizes on the management of patients constipation. B.2 PROBLEMS ENCOUNTERED DURING THE IMPLEMENTATION OF NURSING CARE One of the problems encountered by the researcher during the implementation of her nursing care was the inconsistency of patients mood to cooperate on her plan of care. Patient is greatly affected regarding her misunderstanding with her eldest son. Patients emotions often get in her way resulting to her depression. The patient is often seen lying on bed with less
physical activity. Patient often talks about her son and her deceased husband. Patient experiences self pity and depression which led her to her verbalization of
kahibaw ko pait ug luoy akong kahimtang pero okay ra man pud kung mamatay nako kay wa naman sad koy rason mabuhi which now supports patients less interest to listen to the researcher and less interest to the improve the state of her condition. She views researchers entry to her room as a very soothing one because she knows very well that with the researcher around, she can vent out her feelings. Handling someones feelings is a very crucial responsibility because it requires a pure heart to listen and sincere soul understand. Now this becomes a challenge to gain the trust of the patient. Hence, researchers basic knowledge, skills and positive attitude are now made use in the clinical setting as to how she would create a smooth relationship between her and her patient. B.3 PATIENT TEACHING The researcher conducted a one on one discussion between her and her patient regarding the plan of care. The researcher encouraged the patient to become an active participant to the implementation of her care. She emphasized few instructions that are needed to be followed such as strict compliance to her prescribed diet. The patient should understand that she needs to avoid eating foods high in sodium, fat and cholesterol to prevent the occurrence of further complications. In addition, the patient needs to increase her fluid intake and eat foods high in fiber such as wheat grains, oatmeal, decaffeinated coffee, tea, pineapple and watermelon to manage constipation which is one of the side effects of some of her medications. She also included in her teaching that the patient
needs to comply on her medication regimen that was ordered by her physician. The researcher also encouraged the patient to exercise within limits of individual ability. Compliance to dietary restriction and exercise plays an important role in the improvement of patients condition. The researcher promoted infection control to her patient. She then encouraged her patient to practice hand hygiene at all times. She instructed patient to do frequent self-perineal care every after voiding and do proper personal hygiene such as taking a bath to prevent infection. X. CONCLUSION AND RECOMMENDATION After having experienced taking care of a patient with type 2 diabetes, the researcher was able to develop sympathy for all patients with this kind of condition. As a future health care provider handling this kind of case, the primary concern is to impart knowledge to the patient/s so that they will know what are the dos and donts with regards to their condition, and to their significant others so that there will be a continuation of care in and out of the hospital or the absence of health care provider/s. Rendering care is not also an easy task but having the right attitude and sincere purpose of doing such, everything would just be light.
The study was accomplished under an encouraging ambiance that facilitated for an undisturbed atmosphere both for the patient and the student nurse. The patient in spite of the discomforts of condition and the distress she felt
was still very accommodating which enabled the researcher to obtain pertinent information and data.
The researcher would like to recommend to all the future researchers to give a holistic care to their patients. This will truly help the patient, for what they are going through lies between life and death. She also recommends them to gather as much data as possible, and a very detailed one. The researchers should be geared towards realizing and restoring the patient's biopsychospiritual well being and assisting the client to live a dignified and normal life where in the patient would feel loved, cared for, trusted and understood.
This study aims every nurse, and student nurse alike, to widen and share this knowledge and skills with regards to the care given to anyone family, friends, or even strangers. This study will offer information in the minds of those non-medically oriented and affix superfluous details to health care provider, and so as to every human being. Thus, student nurses must think wholly in bestowing worth to their patient/s, especially the diabetic ones as individuals that dont just need care but also support and encouragement. XI. IMPLICATION OF THE STUDY TO A. NURSING EDUCATION
Education primarily is the highlight of this case study. This serves as a momentous tool for every health care provider. It stresses out all the information on the concept of type 2 diabetes mellitus. This serves as a magnifier to dissect and observe all the information and gives extensive grasp on the said concept. The study is one tool in giving way to a more holistic and effective care in patients who have diabetes. Having a good outlook and positive attitude is another thing we could get out of this case study. Being a positive and confident in dealing with these patients will make the patients feel at ease and trust their nurses more which aids in giving effective and better care. B. NURSING PRACTICE It is when you know that this study is geared towards the optimal care for clients who have this particular case. Doing a case study contributes much to nursing education as it widens our knowledge base and apply them to appropriate situations, which is in turn contributes to our efficacy. The study focuses on the skill that is essential to provide best possible care. Knowledge should be supported with skills and practice. Skills that is refined with constant practice and an open mind for improvements, and the appropriate stance, to understand patients situation. And as time progresses, it also needs revision to cope with the changing need and demands. C. NURSING RESEARCH
Research is the heart of more scientific based care. It is a vital part to every theory, formula and newly concepts rendered to the society. To do research, benefits not only students who are taking up nursing but for those nurses who practice their profession. Also, it is in research that we update ourselves to the very fast paced track and trends in nursing. Nursing is an ever-changing field. What may not be applicable today may be applicable tomorrow.
This study can be a good basis for the future researchers and professionals so that better interventions and knowledge will soon be made and imparted to all patients, their significant others and professionals dealing with this condition. It serves as reference and it provides valuable data on how to care for individuals with type 2 diabetes mellitus. Through this, they can attain information and the appropriate measures in giving nursing care.
Você também pode gostar
- The Obesity Fix - James DiNicolantonioDocumento811 páginasThe Obesity Fix - James DiNicolantoniokirin91% (11)
- Shear and Moment DiagramsDocumento38 páginasShear and Moment DiagramsdonlynAinda não há avaliações
- Calculating Insulin DoseDocumento5 páginasCalculating Insulin DoseMąhmóúd SąmíAinda não há avaliações
- ABC of DiabetesDocumento111 páginasABC of DiabetesCandy E Ri ViAinda não há avaliações
- Power Supply RepairDocumento4 páginasPower Supply RepairterezkiAinda não há avaliações
- + +Over+40+Ab+Solution+PDF eBook,+Shaun+HadsallDocumento65 páginas+ +Over+40+Ab+Solution+PDF eBook,+Shaun+HadsallSherif Abdel Hamid Fakhry100% (2)
- DM Care PlanDocumento9 páginasDM Care PlanHarish Kumar KumawatAinda não há avaliações
- Ignition TimingDocumento7 páginasIgnition TimingdonlynAinda não há avaliações
- How EXERCISE Helps Control DiabetesDocumento23 páginasHow EXERCISE Helps Control DiabetesApurba MukherjeeAinda não há avaliações
- Insulin and Insulin ResistanceDocumento21 páginasInsulin and Insulin ResistanceFisiologiaUFCG100% (1)
- Final DM IIDocumento90 páginasFinal DM IITine Mendoza100% (1)
- Fan RepairDocumento22 páginasFan RepairdonlynAinda não há avaliações
- FINAL CASE STUDY of Diabetes MellitusDocumento40 páginasFINAL CASE STUDY of Diabetes MellitusRomeo Avecilla Cabral100% (3)
- Pathophysiology of Diabetes MellitusDocumento2 páginasPathophysiology of Diabetes MellitusShelly_Ann_Del_9959Ainda não há avaliações
- 70th BATCH - First Session of Intensive Reversal ProgramDocumento78 páginas70th BATCH - First Session of Intensive Reversal ProgramChandrika veerareddyAinda não há avaliações
- Gastroparesis in Type 1 Diabetes Final Working PaperDocumento12 páginasGastroparesis in Type 1 Diabetes Final Working Paperapi-384481487Ainda não há avaliações
- Accident Reporting PolicyDocumento2 páginasAccident Reporting PolicybmkallarackalAinda não há avaliações
- Diabetis MelitusDocumento25 páginasDiabetis MelitusIrma0% (1)
- Engine OilDocumento14 páginasEngine OildonlynAinda não há avaliações
- Diabetes Chapter 1 IntroductionDocumento23 páginasDiabetes Chapter 1 IntroductionHannah CaldinoAinda não há avaliações
- Diabetes Mellitus NCPDocumento7 páginasDiabetes Mellitus NCPjfgnzls182892% (12)
- AIR II TR I AB C of X Glycation Carbamylation Carbonylation Spring MMXVIIDocumento121 páginasAIR II TR I AB C of X Glycation Carbamylation Carbonylation Spring MMXVIIalan50% (2)
- How To Treat Candida InfectionDocumento14 páginasHow To Treat Candida InfectiondonlynAinda não há avaliações
- Naturopathy and Yoga for Diabetes ManagementDocumento68 páginasNaturopathy and Yoga for Diabetes Managementjohn009Ainda não há avaliações
- Diabetes Mellitus Type 2 NotesDocumento5 páginasDiabetes Mellitus Type 2 NotesAimee Kaye DetablanAinda não há avaliações
- Managing Diabetes Through Proper Treatment and MonitoringDocumento10 páginasManaging Diabetes Through Proper Treatment and Monitoringjoeln_9Ainda não há avaliações
- Personal Security Essentials for Safety at Home, While Traveling and MoreDocumento11 páginasPersonal Security Essentials for Safety at Home, While Traveling and MoredonlynAinda não há avaliações
- LaPaz Batchoy RecipeDocumento10 páginasLaPaz Batchoy RecipedonlynAinda não há avaliações
- Diabetes Perspectives and TreatmentsDocumento32 páginasDiabetes Perspectives and TreatmentsyellahfellahAinda não há avaliações
- R2Documento24 páginasR2Nomer SenadorAinda não há avaliações
- Sleep DebtDocumento15 páginasSleep DebtDarla Carroll100% (2)
- Nursing Care Plans For Diabetes MellitusDocumento12 páginasNursing Care Plans For Diabetes MellitusRaveen mayi85% (59)
- FINAL CASE STUDY of Diabetes MellitusDocumento52 páginasFINAL CASE STUDY of Diabetes MellitusTuTit100% (1)
- Diabetes Mellitus Type 2, Formerly Known As Non-Insulin-Dependent DiabetesDocumento12 páginasDiabetes Mellitus Type 2, Formerly Known As Non-Insulin-Dependent DiabetesdonlynAinda não há avaliações
- A Project Proposal On Case Study and Management of A Type 1 Diabetes Mellitus ClientDocumento6 páginasA Project Proposal On Case Study and Management of A Type 1 Diabetes Mellitus ClientMichael Kivumbi100% (3)
- By: Chiara Azra C.P./ J520160042/ Group EDocumento2 páginasBy: Chiara Azra C.P./ J520160042/ Group EChiara Azra CendaniAinda não há avaliações
- Diabetes AssignmentDocumento8 páginasDiabetes AssignmentMildred Obeng AgyeiwaaAinda não há avaliações
- Diabetes R&DDocumento132 páginasDiabetes R&Dlali62Ainda não há avaliações
- Health Safety and EMSDocumento9 páginasHealth Safety and EMSAreeba MazharAinda não há avaliações
- DM Grand Case PresDocumento24 páginasDM Grand Case PresBing Howell de GuzmanAinda não há avaliações
- Nursing Report on Diabetes Mellitus at University of Muthanna CollegeDocumento12 páginasNursing Report on Diabetes Mellitus at University of Muthanna CollegeAbbas AwfiAinda não há avaliações
- Indian Medicinal Plants in DiabetesDocumento6 páginasIndian Medicinal Plants in DiabetesDr Dushyant Kamal DhariAinda não há avaliações
- A. Patient's InformationDocumento8 páginasA. Patient's InformationCamille Quilao PantoniAinda não há avaliações
- Matheson FinalresearchDocumento11 páginasMatheson Finalresearchapi-198635366Ainda não há avaliações
- Diabete Mellitus HandoutsDocumento7 páginasDiabete Mellitus HandoutsSittie Nashieva A. UsmanAinda não há avaliações
- Pathophysiology ScribdDocumento8 páginasPathophysiology ScribdTamil VillardoAinda não há avaliações
- Diabetes ProjectDocumento8 páginasDiabetes ProjectBhupesh KumarAinda não há avaliações
- Safari - 26 Jul. 2019 01:14Documento1 páginaSafari - 26 Jul. 2019 01:14Jonathan ZapataAinda não há avaliações
- Assignmetn Stem CellDocumento13 páginasAssignmetn Stem CellPeeyushAinda não há avaliações
- Aims and ObjectivesDocumento13 páginasAims and Objectivesmamun183Ainda não há avaliações
- Chapter 50 51 Prelec Quizzes Case Studies Discussion Topis and Critical Thinking Exercises Work To Be Done..Documento8 páginasChapter 50 51 Prelec Quizzes Case Studies Discussion Topis and Critical Thinking Exercises Work To Be Done..Besael BaccolAinda não há avaliações
- Case Study B.EDocumento14 páginasCase Study B.EKOBE TOMAGANAinda não há avaliações
- Diabetes and HerbsDocumento132 páginasDiabetes and HerbsAjmal KhanAinda não há avaliações
- Types & Causes of DiabetesDocumento4 páginasTypes & Causes of DiabetesNor Ashikin IsmailAinda não há avaliações
- Chapter-5_DMDocumento8 páginasChapter-5_DMFitri YaniAinda não há avaliações
- Diabetes Mellitus: Causes, Symptoms and TreatmentDocumento34 páginasDiabetes Mellitus: Causes, Symptoms and TreatmentAru VermaAinda não há avaliações
- Managing Diabetes and RisksDocumento8 páginasManaging Diabetes and RisksChristopher LontocAinda não há avaliações
- Diabetes Mellitus, Often Simply Referred To As Diabetes, Is A Group of Metabolic Diseases inDocumento28 páginasDiabetes Mellitus, Often Simply Referred To As Diabetes, Is A Group of Metabolic Diseases inKrissy GaluraAinda não há avaliações
- Nursing Interventions for DiabetesDocumento2 páginasNursing Interventions for DiabetesYayan BeltranAinda não há avaliações
- Antidiabetic Effects of D. Philippinensis - Midterm OutputDocumento12 páginasAntidiabetic Effects of D. Philippinensis - Midterm Outputrebecca martillanaAinda não há avaliações
- Final Manuscript TorresDocumento22 páginasFinal Manuscript Torrescharibel torresAinda não há avaliações
- Diabetes Mellitus 2Documento28 páginasDiabetes Mellitus 2ryanAinda não há avaliações
- DM FinaDocumento3 páginasDM FinaChared LumbaAinda não há avaliações
- Diabetes MelitusDocumento14 páginasDiabetes MelitusDewa Ayu Pradnya DewiAinda não há avaliações
- Diabetes NCLEX QuestionsDocumento22 páginasDiabetes NCLEX QuestionsGesta, Van Gerard T.Ainda não há avaliações
- Diabetes Case Study Fall 2016 1Documento7 páginasDiabetes Case Study Fall 2016 1api-284823421Ainda não há avaliações
- Dental Management of Patients With Diabetes MellitusDocumento8 páginasDental Management of Patients With Diabetes Mellitusاحمد سلامAinda não há avaliações
- Pathophysiology of Type II Diabetes MellitusDocumento7 páginasPathophysiology of Type II Diabetes Mellituschinthaka18389021Ainda não há avaliações
- Types of Childhood Diabetes and Treatment UpdatesDocumento51 páginasTypes of Childhood Diabetes and Treatment UpdatesJulie Carnetion DAinda não há avaliações
- Drug Study - Regular InsulinDocumento8 páginasDrug Study - Regular InsulinRaijenne VersolaAinda não há avaliações
- Experiences of Insulin-Dependent PatientsDocumento4 páginasExperiences of Insulin-Dependent PatientsWilbert Antonino CabanbanAinda não há avaliações
- What Is Diabetes? What Causes Diabetes?Documento8 páginasWhat Is Diabetes? What Causes Diabetes?Khaleda FatmawatiAinda não há avaliações
- Diabetes Mellitus Diabetes Mellitus, Often Simply Diabetes, Is A Syndrome Characterized by DisorderedDocumento8 páginasDiabetes Mellitus Diabetes Mellitus, Often Simply Diabetes, Is A Syndrome Characterized by DisorderedRachel Ann BatayolaAinda não há avaliações
- DiabetesDocumento10 páginasDiabetesFatima El HassouniAinda não há avaliações
- Diabetes: Causes, Symptoms and TreatmentsDocumento4 páginasDiabetes: Causes, Symptoms and TreatmentsAbdullah BazryAinda não há avaliações
- DR ZegeyeDocumento1.254 páginasDR ZegeyesirawAinda não há avaliações
- Breaking the Chains of Diabetes. A Comprehensive Guide to Understanding and Managing Diabetes NaturallyNo EverandBreaking the Chains of Diabetes. A Comprehensive Guide to Understanding and Managing Diabetes NaturallyAinda não há avaliações
- Perations Anual: Project or System NameDocumento13 páginasPerations Anual: Project or System NameViren SehgalAinda não há avaliações
- Materials For Septic Tank Using BarrelsDocumento2 páginasMaterials For Septic Tank Using BarrelsdonlynAinda não há avaliações
- Obd CodesDocumento2 páginasObd CodesdonlynAinda não há avaliações
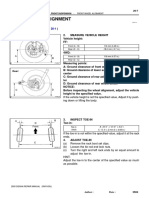
- Wheel AlignmentDocumento4 páginasWheel AlignmentdonlynAinda não há avaliações
- Grammar 1Documento1 páginaGrammar 1donlynAinda não há avaliações
- Steering (Manual)Documento6 páginasSteering (Manual)donlynAinda não há avaliações
- Materials For Septic Tank Using BarrelsDocumento2 páginasMaterials For Septic Tank Using BarrelsdonlynAinda não há avaliações
- Understanding Perfect Tenses - Present, Past, FutureDocumento1 páginaUnderstanding Perfect Tenses - Present, Past, FuturedonlynAinda não há avaliações
- 2015 Maintenance Section - Non-Turbo - PDF Montero PDFDocumento17 páginas2015 Maintenance Section - Non-Turbo - PDF Montero PDFdonlynAinda não há avaliações
- How to rebuild an alternator in under 40 stepsDocumento29 páginasHow to rebuild an alternator in under 40 stepsdonlynAinda não há avaliações
- Bring Dead Lead Acid Battery To Live AgainDocumento14 páginasBring Dead Lead Acid Battery To Live AgaindonlynAinda não há avaliações
- Security TemplateDocumento89 páginasSecurity TemplatedonlynAinda não há avaliações
- PhilosophyDocumento3 páginasPhilosophydonlynAinda não há avaliações
- Richard WagnerDocumento2 páginasRichard Wagnerdonlyn100% (1)
- Running CostDocumento6 páginasRunning CostdonlynAinda não há avaliações
- Accident Investigation Report Reviews: Health & Safety Committee (Worker Members)Documento1 páginaAccident Investigation Report Reviews: Health & Safety Committee (Worker Members)donlynAinda não há avaliações
- Witness Statement FormDocumento1 páginaWitness Statement FormdonlynAinda não há avaliações
- Accident Reporting Procedure2Documento1 páginaAccident Reporting Procedure2donlynAinda não há avaliações
- Work Accident Report FormDocumento1 páginaWork Accident Report FormdonlynAinda não há avaliações
- Corrective Action FormDocumento1 páginaCorrective Action FormdonlynAinda não há avaliações
- Accident/Incident Investigation: PurposeDocumento1 páginaAccident/Incident Investigation: PurposedonlynAinda não há avaliações
- Dasha Lavana Dravakam PDFDocumento9 páginasDasha Lavana Dravakam PDFDgbabu BabuAinda não há avaliações
- Banting Diet Review: Does Low-Carb Plan Aid Weight LossDocumento33 páginasBanting Diet Review: Does Low-Carb Plan Aid Weight Losstmendes00Ainda não há avaliações
- Reviews: Bariatric and Metabolic Surgery: A Shift in Eligibility and Success CriteriaDocumento13 páginasReviews: Bariatric and Metabolic Surgery: A Shift in Eligibility and Success CriteriaJulia SCAinda não há avaliações
- Sepsis from UTI due to uncontrolled diabetesDocumento1 páginaSepsis from UTI due to uncontrolled diabetesJobelle Rodriguez BernabeAinda não há avaliações
- Swimming Exercise: Impact of Aquatic Exercise On Cardiovascular HealthDocumento11 páginasSwimming Exercise: Impact of Aquatic Exercise On Cardiovascular HealthMihail RonnyAinda não há avaliações
- Nutrigenomics White PaperDocumento36 páginasNutrigenomics White PaperAna Raudhatul JannahAinda não há avaliações
- Choosing The Most Appropriate Biologic Therapy For Crohn's Disease According To Concomitant Extra-Intestinal Manifestations, Comorbidities, or Physiologic ConditionsDocumento44 páginasChoosing The Most Appropriate Biologic Therapy For Crohn's Disease According To Concomitant Extra-Intestinal Manifestations, Comorbidities, or Physiologic ConditionsBernadett FarkasAinda não há avaliações
- Pathophysiology of Gestational DMDocumento3 páginasPathophysiology of Gestational DMAnonymous GtR96jCAinda não há avaliações
- Metabolic Changes in Diabetes: R. D. G. Leslie LondonDocumento4 páginasMetabolic Changes in Diabetes: R. D. G. Leslie LondonManuAinda não há avaliações
- Nutrisi Pada DMDocumento48 páginasNutrisi Pada DMalwiAinda não há avaliações
- Taiwanese Journal of Obstetrics & Gynecology: Ching-Ju Shen, Shih-Han Wang, Chien-Hung Lee, Te-Fu ChanDocumento4 páginasTaiwanese Journal of Obstetrics & Gynecology: Ching-Ju Shen, Shih-Han Wang, Chien-Hung Lee, Te-Fu ChanIman Ru-ancaAinda não há avaliações
- Pcos StudiesDocumento34 páginasPcos StudiesDoctora SantanaAinda não há avaliações
- Diabetes Case StudyDocumento3 páginasDiabetes Case Studydsaitta108Ainda não há avaliações
- Etiopathogenesis of Diabetes MellitusDocumento35 páginasEtiopathogenesis of Diabetes MellitusironAinda não há avaliações
- Classification of Diabetes Mellitus - Endotext - NCBI BookshelfDocumento11 páginasClassification of Diabetes Mellitus - Endotext - NCBI BookshelfSwati ParijaAinda não há avaliações
- To Health, Nutrition, and Diabetes Indian Foods: AAPI's GuideDocumento96 páginasTo Health, Nutrition, and Diabetes Indian Foods: AAPI's GuideGyanaRaghavan-chamuAinda não há avaliações
- HomaDocumento12 páginasHomaArjuna NaturalAinda não há avaliações
- Diabeties NewDocumento54 páginasDiabeties NewDipti SharmaAinda não há avaliações
- Johnston Et Al. - 2008 - A Preliminary Evaluation of The Safety and ToleranDocumento5 páginasJohnston Et Al. - 2008 - A Preliminary Evaluation of The Safety and ToleranMiin ChanAinda não há avaliações
- Durruty, Et Al (2019) Pathogenesis of Type 2 DiabetesDocumento19 páginasDurruty, Et Al (2019) Pathogenesis of Type 2 Diabetestantry puspitasariAinda não há avaliações