Escolar Documentos
Profissional Documentos
Cultura Documentos
Sudden Death and Angelman Syndrome
Enviado por
Helsa Eldatarina JDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Sudden Death and Angelman Syndrome
Enviado por
Helsa Eldatarina JDireitos autorais:
Formatos disponíveis
CASE REPORT PATHOLOGY BIOLOGY
Jonathon Herbst,1,* M.D. and Roger W. Byard,2 M.B.B.S., M.D.
J Forensic Sci, January 2012, Vol. 57, No. 1 doi: 10.1111/j.1556-4029.2011.01901.x Available online at: onlinelibrary.wiley.com
Sudden Death and Angelman Syndrome
ABSTRACT: Angelman syndrome is a condition characterized by developmental delay due to abnormalities in the maternally derived chromosome 15q11-q13. Typical features include impaired expressive language, an ataxic gait, and seizures. Hyperactivity may result in accidental bruises and abrasions, raising issues of possible inflicted injury. A fascination with water may predispose to drowning. A 5-year-old boy with an established diagnosis of Angelman syndrome is reported who died of upper airway obstruction due to massively enlarged tonsils complicating infectious mononucleosis. Assessment of the severity of underlying illness in developmentally delayed children may be difficult due to failure to vocalize worsening symptoms and distress. In addition, signs of upper airway narrowing due to infection in Angelman syndrome may be masked by the sucking and swallowing difficulties that affected individuals may have with drooling and excessive chewing and mouthing behavior. KEYWORDS: forensic science, forensic pathology, Angelman syndrome, EpsteinBarr virus, airway obstruction, asphyxia, infectious
mononucleosis
Angelman syndrome is a condition characterized by developmental delay that results from abnormalities in the maternal contribution of the chromosome 15q11-q13 genomic region (1). Mutations affecting this area of the chromosome involve the ubiquitin-protein ligase E3A (UBE3A) gene (2). Clinical symptoms include motor impairment, impaired or absent expressive language and speech, ataxia, and seizures. Characteristically those affected are also noted to have a happy demeanor (2). Cases may come to forensic attention due to medical complications associated with immobility, severe scoliosis, dysphagia, aspiration, and severe epilepsy. There is also believed to be an increased risk of drowning due to a fascination with water. Another problem arises in the assessment of the severity of coincidental medical conditions due to difficulties in communication and examination. The case of a 5-year-old boy with Angelman syndrome is presented to demonstrate an unusual cause of acute upper airway obstruction due to EpsteinBarr infection. Case Report A 5-year-old boy with an established diagnosis of Angelman syndrome, with hyperactivity, recurrent respiratory infections, and sleep disturbance, was presented to a physician with fever, cervical adenopathy, and tonsillar enlargement. Additionally, he was noted by his mother to have cyanotic extremities. The clinical diagnosis was tonsillitis and he was begun on oral amoxicillin. Clinical improvement did not occur and he suffered a cardiorespiratory arrest at home several days later. Attempts at resuscitation were not successful.
Forensic Science South AustraliaPathology, 21 Divett Place, Adelaide, South Australia 5000, Australia. 2 Discipline of Pathology, University of Adelaide, Frome Rd., Adelaide, South Australia 5005, Australia. *Current address: University of Michigan, Department of Pathology, 1500 E. Medical Center Dr., Ann Arbor, MI 48109-5054. Received 17 Aug. 2010; and in revised form 15 Nov. 2010; accepted 20 Nov. 2010.
1
At autopsy, no overt dysmorphic features were seen. There was no evidence of scoliosis. The most significant findings were in the oropharynx and neck where there was marked bilateral tonsillar enlargement (Fig. 1) associated with prominent cervical lymphadenopathy (Fig. 2). The tonsils were coated with a copious tan-white exudate and were so enlarged that no upper airway inlet was visible. The spleen was enlarged and weighed 247 g (normal = 47 grams) (3). Other findings at autopsy included congested, edematous lungs and focal neuronal dysplasia of the brain. There were no other underlying conditions present that could have caused or contributed to death and there was no evidence of trauma. Given the findings of lymphadenopathy, tonsillomegaly with significant airway narrowing, and splenomegaly, serum was taken postmortem and sent for EpsteinBarr virus (EBV) serology. This showed IgM antibodies to EBV, with no detection of IgG antibodies to EBV, in keeping with current or recent infection. Microscopic examination of the tonsils and lymph nodes showed benign paracortical expansion with scattered atypical immunoblasts and immunohistochemistry for EBV latent membrane protein (EBVLMP) showed strong staining in an interfollicular distribution (Fig. 3). There were no oropharyngeal malformations that would have contributed to the upper airway obstruction. Toxicology revealed therapeutic concentrations of codeine, paracetamol, and morphine in keeping with over-the-counter medication. There was also a therapeutic level of clobazam. Death was attributed to upper airway obstruction complicating infectious mononucleosis. Discussion Angelman syndrome is a condition associated with neurodevelopmental delay due to a deletion involving the maternally inherited chromosome 15q11-13 (in approximately 70% of cases) (4). Loss of the paternal genetic material at this area results in PraderWilli syndrome. Other significant genetic findings include 3% of affected individuals with uniparental disomy of chromosome 15, 1% with a mutation in the imprinting center, and 6% with mutations of the
257
2011 American Academy of Forensic Sciences
258
JOURNAL OF FORENSIC SCIENCES
FIG. 3Immunostain for EpsteinBarr virus latent membrane protein (EBV-LMP). Section of tonsil demonstrated positive staining in an interfollicular location.
FIG. 1The tonsils were markedly enlarged with no visible upper respiratory inlet.
FIG. 2There was prominent cervical lymphadenopathy. Note enlarged nodes at both sides of the neck.
UBE3A gene. Additionally, it is possible to have no detectable genetic abnormality. Most of the genetic abnormalities affect UBE3A gene expression. Recently, studies have shown interaction between the underlying defects responsible for Angelman syndrome
and Rett syndrome (5). These syndromes can have significant overlap of clinical findings. The underlying genetic defect for Rett syndrome is on Xq28 (6). Typical clinical features of Angelman syndrome may be seen at approximately 612 months of age, with the major findings including impaired expressive language, an ataxic gait, and seizures. Typical behavioral patterns include a happy demeanor and a reduced attention span (4). Another frequent behavioral manifestation is hyperactivity, and it has been noted that in extreme cases that constant movement may result in accidental bruises and abrasions, raising issues of possible inflicted injury. Older children also grab, pinch, and bite (4). Ishmael et al. (7) have reported a fascination with water in individuals with Angelman syndrome with a possible increased risk of accidental drowning. Factors, which may lead to difficulties with water and swimming in particular, include poor coordination, ataxia, reduced muscle tone, and poor cognition (7). The authors emphasize the need for carers to exercise particular vigilance around water or during water-based activities. Other features that have been reported in 2080% of cases include a protruding tongue, tongue thrusting, sucking and swallowing difficulties, feeding problems during infancy, prognathia, frequent drooling, and excessive chewing mouthing behaviors (8). Over 90% of patients have epilepsy, and many different types of seizures occur including refractory epilepsy, atypical absences, myoclonic seizures, and convulsive or nonconvulsive status epilepticus (2,4). The seizure activity may improve during the teenage years (9). Although it has been reported that individuals with Angelman syndrome have a normal life span, the high incidence of epilepsy, with immobility, severe scoliosis, dysphagia, and aspiration (factors that all predispose to respiratory problems), would suggest otherwise (9). The current case demonstrates an additional problem that occurs with mentally and developmentally delayed children and that is with the assessment of the severity of underlying illness. In the reported case, significant airway narrowing had resulted from tonsillar enlargement due to underlying infectious mononucleosis. In a child with normal mental and physical development, enlargement of the tonsils to the degree demonstrated would result in readily apparent swallowing difficulties. Unfortunately, this may be masked in a child who already has sucking and swallowing difficulties, with drooling and excessive chewing and mouthing behaviors. It is also possible that the speech difficulties associated with Angelman syndrome may also prevent vocalization of worsening symptoms and distress.
HERBST AND BYARD SUDDEN DEATH AND ANGELMAN SYNDROME
259
EBV is a DNA gamma-herpes virus that infects over 90% of the human population worldwide (10). It is the etiologic agent in infectious mononucleosis and is generally spread between young children by salivary contact (11). Clinical signs of infectious mononucleosis include cervical adenopathy (12), splenomegaly, hepatitis, and pharyngitis. Rarely massive tonsillar enlargement with pharyngeal edema may occur resulting in airway obstruction and death (13). On occasion, upper airway obstruction may be exacerbated by narcotic analgesia (14,15) and so toxicology testing may be a useful adjunct in these cases. The significance of the therapeutic levels of codeine and morphine in the current case is uncertain although it is possible that these may have contributed to airway relaxation. Other causes of sudden death in infectious mononucleosis that were not found in the reported case include splenic rupture, neurological complications, and myocarditis (14). In conclusion, this case shows that sudden death in children with significant genetic conditions may not be directly related to the defining morphological features of the syndromes. Assessment of the medical status, however, may be complicated by other factors such as reduced cognition, impaired vocalization and features such as difficulties with sucking and swallowing. Acknowledgement We would like to thank the South Australian State Coroner, Mr. M. Johns, for permission to publish selected details of this case. References
1. Gurrieri F, Accadia M. Genetic imprinting: the paradigm of Prader-Willi and Angelman syndromes. Endocr Dev 2009;14:208. 2. Pelc K, Boyd SG, Cheron G, Dan B. Epilepsy in Angelman syndrome. Seizure 2008;17:2117.
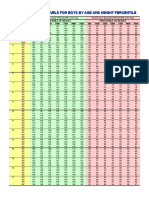
3. Coppelletta JM, Wolbach SB. Body length and organ weights of infants and children: a study of the body length and normal weights of the more important vital organs of the body between birth and twelve years of age. Am J Pathol 1933;9:5570. 4. Guerrini R, Carrozzo R, Rinaldi R, Bonanni P. Angelman syndrome: etiology, clinical features, diagnosis, and management of symptoms. Paediatr Drugs 2003;5:64761. 5. Jedele KB. The overlapping spectrum of Rett and Angelman syndromes: a clinical review. Semin Pediatr Neurol 2007;14:10817. 6. Byard RW. Forensic issues and possible mechanisms of sudden death in Rett syndrome. J Clin Forensic Med 2006;13:969. 7. Ishmael HA, Begleiter ML, Butler MG. Drowning as a cause of death in Angelman syndrome. Am J Ment Retard 2002;107:6970. 8. Williams CA, Beaudet Al, Clayton-Smith J, Knoll JH, Kyllerman M, Laan LA, et al. Angelman syndrome 2005: updated consensus for diagnostic criteria. Am J Med Genet A 2006;140:4138. 9. Dan B, Pelc K. Natural history of Angelman syndrome. Dev Med Child Neurol 2008;50:3925. 10. Vetsika EK, Callan M. Infectious mononucleosis and EpsteinBarr virus. Expert Rev Mol Med 2004;6:116. 11. Macsween KF, Crawford DH. EpsteinBarr virus recent advances. Lancet Infect Dis 2003;3:13140. 12. Ebell MH. EpsteinBarr virus infectious mononucleosis. Am Fam Physician 2004;70:127987. 13. Bogiolli LR, Taff ML. Sudden asphyxial death complicationg infectious mononucleosis. Am J Forensic Med Pathol 1998;19:1747. 14. Byard RW. Unexpected death due to infectious mononucleosis. J Forensic Sci 2002;47:2024. 15. Byard RW, Gilbert JD. Narcotic administration and stenosing lesions of the upper airwaya potentially lethal combination. J Clin Forensic Med 2005;12:2931. Additional information and reprint request: Jonathon Herbst, M.D. University of Michigan Department of Pathology 1500 E. Medical Center Dr. 2G309 UH SPC 5054 Ann Arbor, MI 48109-5054 E-mail: jherbst@med.umich.edu
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Introduction To Public Health... 1stDocumento37 páginasIntroduction To Public Health... 1stNELSONJD20195100% (3)
- DK50 Developer Parts ABDocumento15 páginasDK50 Developer Parts ABedu3ipbAinda não há avaliações
- Mindvalley - Superbrain Quest - SummaryDocumento17 páginasMindvalley - Superbrain Quest - SummaryMagdy El ID100% (3)
- TestingDocumento1 páginaTestingHelsa Eldatarina JAinda não há avaliações
- Lampiran CMLDocumento3 páginasLampiran CMLHelsa Eldatarina JAinda não há avaliações
- XXXXXXXXXXXXXXXXXXXXXXXXXXXXXDocumento5 páginasXXXXXXXXXXXXXXXXXXXXXXXXXXXXXHelsa Eldatarina JAinda não há avaliações
- Surgical Complication of Typhoid FeverDocumento10 páginasSurgical Complication of Typhoid FeverHelsa Eldatarina JAinda não há avaliações
- A AaaaaaaaaaaaaaaDocumento2 páginasA AaaaaaaaaaaaaaaHelsa Eldatarina JAinda não há avaliações
- Case StudyDocumento6 páginasCase StudyHelsa Eldatarina JAinda não há avaliações
- Daftar PustakaDocumento2 páginasDaftar PustakaHelsa Eldatarina JAinda não há avaliações
- Intestinal MalrotationDocumento10 páginasIntestinal MalrotationHelsa Eldatarina JAinda não há avaliações
- Blood PressureDocumento3 páginasBlood PressurephandinhvinhsanAinda não há avaliações
- Congestive Heart Failure FC III Et Causa Coronary Artery Disease + Hypertensive Falciparum Malaria Complicated With Acute Pancreatitis: A Report of Case SeriesDocumento1 páginaCongestive Heart Failure FC III Et Causa Coronary Artery Disease + Hypertensive Falciparum Malaria Complicated With Acute Pancreatitis: A Report of Case SeriesHelsa Eldatarina JAinda não há avaliações
- A AaaaaaaaaaaaaaaDocumento2 páginasA AaaaaaaaaaaaaaaHelsa Eldatarina JAinda não há avaliações
- Suju - No Other LyricsDocumento2 páginasSuju - No Other LyricsHelsa Eldatarina JAinda não há avaliações
- MalariaDocumento9 páginasMalariaHelsa Eldatarina JAinda não há avaliações
- GbsDocumento4 páginasGbsHelsa Eldatarina JAinda não há avaliações
- Higher Algebra - Hall & KnightDocumento593 páginasHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Curing Stage 4 Cancer and Terminal Liver Disease with Alpha Lipoic AcidDocumento14 páginasCuring Stage 4 Cancer and Terminal Liver Disease with Alpha Lipoic Acidguy777Ainda não há avaliações
- MDR Guideline Medical Devices LabelingDocumento7 páginasMDR Guideline Medical Devices Labelingarade43100% (1)
- KPI - Foruth EditionDocumento30 páginasKPI - Foruth EditionAnonymous qUra8Vr0SAinda não há avaliações
- Abbott Rabeprazole PM e PDFDocumento45 páginasAbbott Rabeprazole PM e PDFdonobacaAinda não há avaliações
- Risk Assessment For Balustrade Glass InstallationDocumento3 páginasRisk Assessment For Balustrade Glass InstallationNicos PapadopoulosAinda não há avaliações
- Informed Consent and Release, Waiver, and Quitclaim: Know All Men by These PresentsDocumento2 páginasInformed Consent and Release, Waiver, and Quitclaim: Know All Men by These PresentsRobee Camille Desabelle-SumatraAinda não há avaliações
- Eo No. 013 - 2018 Reorganization of BhertDocumento2 páginasEo No. 013 - 2018 Reorganization of BhertAnne Kimberly Peñalba BabaanAinda não há avaliações
- Effect of Ointment Base Type on Percutaneous Drug AbsorptionDocumento4 páginasEffect of Ointment Base Type on Percutaneous Drug AbsorptionINDAHAinda não há avaliações
- Idiopathic Thrombocytopenic PurpuraDocumento3 páginasIdiopathic Thrombocytopenic Purpuraproxytia64Ainda não há avaliações
- Nursing DX: Acute Pain Related To Surgical Manipulation (Laminectomy) As Manifested by Reports of Pain On The Lumbar Area Rated As 7/10Documento1 páginaNursing DX: Acute Pain Related To Surgical Manipulation (Laminectomy) As Manifested by Reports of Pain On The Lumbar Area Rated As 7/10YESSAMIN GUADIZ100% (2)
- Personality Disorders Cluster CDocumento19 páginasPersonality Disorders Cluster CPahw BaluisAinda não há avaliações
- NUST Hostel Admission Form New PDFDocumento2 páginasNUST Hostel Admission Form New PDFMuhammad Waqas0% (1)
- Vol3issue12018 PDFDocumento58 páginasVol3issue12018 PDFpyrockerAinda não há avaliações
- Full Plate Diet BookDocumento164 páginasFull Plate Diet BookScarlettNyx100% (4)
- Complete VaccinationDocumento2 páginasComplete VaccinationNgoo NwosuAinda não há avaliações
- Legal Medicine 2020 2021Documento4 páginasLegal Medicine 2020 2021Zie DammiAinda não há avaliações
- Hahnemann Advance MethodDocumento2 páginasHahnemann Advance MethodRehan AnisAinda não há avaliações
- API SM Part 1Documento7 páginasAPI SM Part 1Ronaldo JanglinAinda não há avaliações
- Table : Number of Population, Hospitals and Beds in All Over JordanDocumento8 páginasTable : Number of Population, Hospitals and Beds in All Over JordanjAinda não há avaliações
- The Precious Little Black Book DownloadDocumento226 páginasThe Precious Little Black Book DownloadAsanda YekiAinda não há avaliações
- How To Make An ELearning ModuleDocumento22 páginasHow To Make An ELearning ModulePradeep RawatAinda não há avaliações
- Journal On The Impact of Nursing Informatics To Clinical PracticeDocumento2 páginasJournal On The Impact of Nursing Informatics To Clinical PracticeLhara Vhaneza CuetoAinda não há avaliações
- Sysman Safety-Integrated-5ed en PDFDocumento345 páginasSysman Safety-Integrated-5ed en PDFErdincAinda não há avaliações
- Success Manual and Cheat Sheet Notes To Pass Your Basic Life Support (BLS) CourseDocumento11 páginasSuccess Manual and Cheat Sheet Notes To Pass Your Basic Life Support (BLS) CourseanthonyAinda não há avaliações
- GoalSettingWorkbookFinal PDFDocumento21 páginasGoalSettingWorkbookFinal PDFDato KhutsishviliAinda não há avaliações
- KT Instructions AC Joint PDFDocumento1 páginaKT Instructions AC Joint PDFariel JaldinAinda não há avaliações
- Kidde Fire Systems Nitrogen Engineered Systems: Design, Installation, Operation and Maintenance ManualDocumento110 páginasKidde Fire Systems Nitrogen Engineered Systems: Design, Installation, Operation and Maintenance ManualYoyon HaryonoAinda não há avaliações