Escolar Documentos
Profissional Documentos
Cultura Documentos
A Randomized Controlled Study of Peritoneal Closure at Caesarean Section
Enviado por
Izzatun NisaDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
A Randomized Controlled Study of Peritoneal Closure at Caesarean Section
Enviado por
Izzatun NisaDireitos autorais:
Formatos disponíveis
A randomized controlled study of peritoneal closure at cesarean section
Khadra A. Galaal, MBChB, MPH, Andrzej Krolikowski, MD, PhD.
ABSTRACT
Objective: To assess the benefits or problems that may be associated with peritoneal closure at cesarean section. Methods: A randomized-controlled study of women undergoing cesarean section in Sultan Qaboos University Hospital Maternity Unit. After the decision is taken for cesarean section, women were randomized to either repair of peritoneum using standard technique or non-repair of peritoneum. Duration of operation, maternal morbidity, blood loss assessed by post-operative hemoglobin change and requirement of transfusion, post operative infection, thromboembolic disease, and length of hospital stay were analyzed in 2 groups of patients. Sixty women were randomized into the study, 30 group A, had peritoneal closure and 30, group B, and had non-closure. Results: The average duration of operation for group A was 61.9+/-12.734, and for group B was 53.56 +/-11.209 (p<0.01 statistically significant). There was no statistically significant difference in the length of stay, estimated blood loss, the mean drop in hemoglobin, postoperative pyrexia, and wound infection rate between the 2 groups. Conclusions: Our study has confirmed the previous study findings, and has shown that there are no advantages in suturing of the peritoneum in terms of blood loss, blood transfusion, operation duration, postoperative pyrexia and wound infection. In fact non-suturing of the peritoneum was associated with shorter operation duration (p<0.01 significant), and reduced cost.
Keywords: Cesarean section, peritoneal closure.
Saudi Medical Journal 2000; Vol. 21 (8): 759-761
parietal and T raditionally isboth theduring cesarean visceral peritoneum closed section. The reasons are to restore the anatomy, to approximate tissue for healing, and to reduce the risk of herniation or dehiscence of abdominal wound.1 It was also thought that it helped reduce adhesion formation.1,2 Few studies have shown that nonclosure of the peritoneum was associated with more rapid healing. The absence of suture material and the reduced tissue handling is thought to contribute to less adhesion formation.2,3 The physiological explanations for the better tissue healing and less adhesions are, the deperitonelized surfaces which are not traumatized heal without permanent adhesions because they retain their ability to lyse fibrinous adhesions before organization can occur.2-4 Tight
sutures may cause the peritoneum to become ischemic and therefore it losses the ability to lyse fibrin.3,4 There is evidence that if left unsutured, peritoneal defects will have mesothelial integrity within 48 hours, and there will be no fibrosis or scar formation in 5 days.3,5-8 Closure of the peritoneum was addressed at 4 randomized-controlled trials; all these trials were included in the Cochrane Systematic Review. The review concludes that currently available evidence questions the routine use of peritoneal closure as conventional practice in routine cesarean section. 5 Methods. The patients consent was taken once the clinical decision has been made for cesarean section. Sixty women were recruited from the labor
From the Department of Obstetrics and Gynecology, Sultan Qaboos University Hospital, Muscat, Sultanate of Oman. Received 12th February 2000. Accepted for publication in final form 14th May 2000. Address correspondence and reprint request to: Dr. K. A. Galaal, PO Box 38, Al-Khod 123, Muscat, Sultanate of Oman. Fax. +968 513418.
759
Peritoneal non-closure at cesarean section ... Galaal & Krolikowski
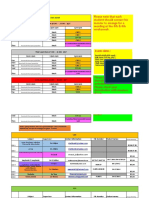
Table 1 - The clinical characteristics of women in the study.
procedure. The collected data was entered into a database for analysis. Results. All women who were asked to take part in the study accepted. The mean age of the patients in the group with peritoneal closure was 28 years, and 26 years in the group with peritoneal non-closure. There were no significant differences in the 2 examined groups as far as parity, weight and gestational age (Table 1). No case of deep venous thrombosis or pulmonary embolism occurred in either group. The duration of cesarean section performed using non-closure was much shorter than these performed by the standard technique. The difference was statistically significant. There were no differences in the length of stay, post operative infection rate, and no significant difference between the estimated blood loss, blood transfusion, and operative duration between the 2 groups (Table 2). Discussion. Closure of peritoneum was addressed at 4 randomized-controlled trials; all these trials were included in the Cochrane Systematic Review. The review concludes that currently available evidence questions the routine use of peritoneal closure as conventional practice in routine cesarean section. 5 Recommendation from the Royal College of Obstetricians and Gynecologists guideline No 15 states the closure of peritoneal defects even with minimally reactive suture materials, results in increased tissue reaction and may result in adhesion formation. Non-closure appears to have few risks and may be recommended in many obstetric and gynecology operations. Surgeons abandoning closure should be no less meticulous in other aspects of their craft.
Closure Age Parity Weight in kg Gestation (weeks) 28 4 65 39
Non-closure 26 5 63 39
ward at Sultan Qaboos University Hospital. They were randomized to one of 2 groups by numbered envelope technique. Thirty to peritoneal closure and 30 to non-closure of peritoneum. Group A. After closure of the uterus in the usual manner, the parietal and visceral peritoneum was closed using 2.0 vicryl sutures. Hemostasis is checked as normally practiced. Abdominal wall is closed in layers as standard practice. Group B. The procedure is as for group A except that both the parietal and visceral peritoneum is left without closure. Again hemostasis is checked before continuing to close the abdominal wall. All women had primary cesarean section, and no previous laparotomy. The Pfanennsteil incision was used for all patients, and general anesthesia was used in both groups. No patient received corticosteriods, pre operative antibiotics or antihistamines. All women under going cesarean section have a sample of blood taken for hemoglobin estimation. Post-operative hemoglobin specimens were taken 48 hours after the cesarean section. The hematocrit was noted in each specimen, to allow accurate estimation of the drop in Hb concentration, which reflects blood loss. The doctors completed a questionnaire after the
Table 2 - Study parameters in both groups.
Group A n = 30 Duration of op in minutes Drop in Hb Blood transfusion Estimate of blood loss (ml) Hospital stay (days) Post-op Pyrexia Ileus Wound infection op = operation Hb = hemoglobin 61.9 +/- 12.734 0.633
Group B n = 30 53.56 +/- 11.209 0.657 +/2.0 0.557
z 2.69 1.41
p <0.01 ns 1.00
0.874 +/3.0 483.3 6.0 9.0 0.0 7.0
+/- 187.696 +/0.913
400.0 5.5 7.0 0.0 4.0
+/- 177.628 +/1.137
1.76 1.88
ns ns 0.771
0.506
z = Fishers exact test
p = p value (single tailed distribution, p < 0.05 (significant))
760
Saudi Medical Journal 2000; Vol. 21 (8)
Peritoneal non-closure at cesarean section ... Galaal & Krolikowski
Our study has confirmed the previous studies findings and has shown that there are no advantages in suturing of the peritoneum in terms of blood loss, blood transfusion, operation duration, post-operative pyrexia and wound infection. In fact non-suturing of the peritoneum was associated with shorter operation duration (p<0.01 significant), reduced rate of postoperative pyrexia and wound infections (nonsignificant). Non-closure of the peritoneum would be associated with reduced operative time and therefore reduce the exposure to anesthesia and rate of thromb-embolic complications. The shorter operative time leads to more efficient use of the theater time and therefore reduces cost. Another aspect we have addressed in this study was the cost of the suture materials. The suture used for closure of the peritoneum is vicryl 0.0, and on average 2 of these suture materials are used during cesarean delivery. In the non-closure group R.O 1.013 was saved for each procedure, i.e. in total = 30.39. This study shows that non-closure of the peritoneum at cesarean section is associated with reduced operation time which in-turn reduces the anesthetic exposure and complications. It has further proven that non-closure of the peritoneum is not associated with increased morbidity.
References
1. Duffy DM, di Zerega GS. Is peritoneal closure necessary? Obstet Gynecol Surv 1994; 49: 817-822. 2. di Zerega GS, Duffy DM. Is peritoneal closure necessary? The Royal College of Obstetricians and gynecologists. PACE Review 1996: 96/02. 3. Nygaard IE, Squatrito RC. Abdominal incisions from creation to closure. Obstet Gynecol Surv 1996; 51: 429-436. 4. Rayburn WF, Schwartz WJ 3rd. Refinement in performing a cesarean delivery. Obstet Gynecol Surv 1996; 51: 445-451. 5. Hankins GDV, Clarks SL, Cunningham G, Gilstrap LC. Cesarean section. In: Operative Obstetrics. Connecticut: Appleton and Langer; 1995. p. 301-332. 6. Tulandi T, Hum HS, Gelfand MM. Closure of laparotomy incisions with or without peritoneal suturing and second look laparoscopy. Am J Obstet Gynecol 1988; 158: 536-537. 7. Wilkinson CS, Enkin MW. Peritoneal non-closure at cesarean section. In: Neilson JP, Crowther CA, Hodnett ED, Hofmeyr GJ, editors. Pregnancy and Childbirth Module of the Cochrane Database of Systemic Reviews. The Cochrane Collaboration, Issue 1. Oxford: Update Software; 1997. 8. Hull DV, Vaner MW. A randomized study of closure of the peritoneum at cesarean delivery. Obstet Gynecol 1991; 77: 818-821.
Saudi Medical Journal 2000; Vol. 21 (8) 761
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5782)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Life-members-Indian Medico-Legal & Ethics Association (Imlea) - Mix State & Mix DepartmentDocumento64 páginasLife-members-Indian Medico-Legal & Ethics Association (Imlea) - Mix State & Mix DepartmentKriti Kumari100% (1)
- ComprehensiveUnifiedPolicy TBDocumento159 páginasComprehensiveUnifiedPolicy TBallan14_reyesAinda não há avaliações
- Handout Fundamentals of Dermatology PDFDocumento4 páginasHandout Fundamentals of Dermatology PDFKoushik Mazumder ShuvoAinda não há avaliações
- Suvendu Hota Cowin CertificateDocumento1 páginaSuvendu Hota Cowin CertificateHemalika SharmaAinda não há avaliações
- Effect of Transcutaneous Electrical Nerve Stimulation On Spasticity in Adults With Stroke A Syst Review and Metaanalysis PDFDocumento18 páginasEffect of Transcutaneous Electrical Nerve Stimulation On Spasticity in Adults With Stroke A Syst Review and Metaanalysis PDFjaunasvyras69 Jaunasvyras69Ainda não há avaliações
- Calculations Practice TestDocumento13 páginasCalculations Practice TestFrancis VillanuevaAinda não há avaliações
- Acute Kidney InjuryDocumento64 páginasAcute Kidney InjuryBIAN ALKHAZMARIAinda não há avaliações
- Basics of Chest X-RayDocumento44 páginasBasics of Chest X-RayMelissa Aina Mohd YusofAinda não há avaliações
- Nursing Education Department: Informed Consent Informed ConsentDocumento13 páginasNursing Education Department: Informed Consent Informed ConsentSitti Mardiya SariolAinda não há avaliações
- Sample CollectionDocumento18 páginasSample Collectioncawsey mohamedAinda não há avaliações
- Instant Download Ebook PDF Administrative Medical Assisting 8th Edition PDF ScribdDocumento41 páginasInstant Download Ebook PDF Administrative Medical Assisting 8th Edition PDF Scribdwilliam.smith656100% (41)
- Scrotal Swelling Causes and TreatmentsDocumento63 páginasScrotal Swelling Causes and TreatmentsTommysAinda não há avaliações
- Reservoir Bag Physics J PhilipDocumento44 páginasReservoir Bag Physics J PhilipJashim JumliAinda não há avaliações
- Adult Tachycardia With A Pulse Algorithm: Doses/DetailsDocumento1 páginaAdult Tachycardia With A Pulse Algorithm: Doses/DetailsZakiyahulfahdwAinda não há avaliações
- Answ1 PDFDocumento184 páginasAnsw1 PDFAbdirahiim Ahmed100% (1)
- Book1new Table B6Documento12 páginasBook1new Table B6Maryam BajAinda não há avaliações
- Dosages and Flow Rates and Pediatric Drug Administration AssignmentDocumento6 páginasDosages and Flow Rates and Pediatric Drug Administration AssignmentNavin Barnwal0% (1)
- Step Test Aerobic Fitness MeasureDocumento1 páginaStep Test Aerobic Fitness MeasureJerico Villa MaglasangAinda não há avaliações
- Acupuncture (Reseach IonDocumento17 páginasAcupuncture (Reseach IonRalph NicolasAinda não há avaliações
- Infection - Nursing Test QuestionsDocumento58 páginasInfection - Nursing Test QuestionsRNStudent1100% (3)
- BrochureDocumento3 páginasBrochureapi-400730798Ainda não há avaliações
- The "S" in W.I.S.E.: Unit VDocumento31 páginasThe "S" in W.I.S.E.: Unit VCamille AnibAinda não há avaliações
- FRCPath Chemical Pathology CurriculumDocumento109 páginasFRCPath Chemical Pathology Curriculummonday125Ainda não há avaliações
- Formulation and Characterization of Nanoparticles for Antidiabetic DrugsDocumento12 páginasFormulation and Characterization of Nanoparticles for Antidiabetic DrugsPradeep NimaseAinda não há avaliações
- Resume - Taraneh Sadeghian HaghighiDocumento3 páginasResume - Taraneh Sadeghian Haghighiarian tejaratAinda não há avaliações
- Basal Implants in The Mandibular Esthetic Zone A Case SeriesDocumento6 páginasBasal Implants in The Mandibular Esthetic Zone A Case SeriesInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- MAST TestDocumento5 páginasMAST TestEnkelBulicaAinda não há avaliações
- JCQWORKHEET No.2Documento3 páginasJCQWORKHEET No.2Jan Cleo Cerdiña QuijanoAinda não há avaliações
- Dalteparin Medication CardDocumento2 páginasDalteparin Medication CardAnja de VriesAinda não há avaliações
- Nursing Care Plan for Medical Dx/SurgeryDocumento5 páginasNursing Care Plan for Medical Dx/SurgeryBob SandersAinda não há avaliações