Escolar Documentos
Profissional Documentos
Cultura Documentos
Mabes Fluid and Electrolyte Imbalances
Enviado por
MabesDireitos autorais
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Mabes Fluid and Electrolyte Imbalances
Enviado por
MabesDireitos autorais:
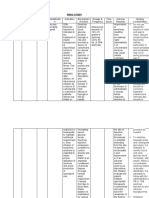
Major Serum Electrolytes Normal Values
Major Serum Electrolytes Sodium Potassium Calcium Magnesium Chloride Phosphate Approximate Serum Concentration mEq/L 142 5 5 2 103 2 Normal Value mEq/L 135 145 3.5 5.0 4.5 5.5 Ionized 1.5 2.5 97 107 Normal Value mg/dl Normal Value mmol/L 135 145 3.5 5.0 2.2 2.6 0.62 0.95 97 107 0.8 1.45
8.6 10.2 1.3 2.3 2.5 4.5
Laborato ry Tests
Laboratory Values Serum Osmolality Plasma Osmolality
Urine Osmolality
Blood Urea Nitrogen (BUN)
for evaluating Fluid Status Range Interpretation 280 300 Serum Osmolality measures sodium concentration mosm/kg Plasma Osmolality regulates ADH release for h20 resorption BUN and Glucose has a role in osmolality Increasing Osmolality (Serum Electrolytes > Water) FVD Severe dehydration Free water loss Diabetes insipidus Hyperglycemia Hypernatremia Stroke or head injury Decreasing Osmolality (Water > Serum Electrolytes) FVE Over hydration SIADH Adrenal Insufficiency Hyponatremia 200 300 Determined by urea, creatinine, and uric acid mosm/kg Most reliable indicator of urine concentration Increasing Osmolality (Concentrated Urine) FVD SIADH Congestive heart failure Acidosis Decreasing Osmolality (Diluted Urine) FVE Diabetes Insipidus Hyponatremia Aldosteronism Pyelonephritis 10 20 mg/dl Made up of urea (end product of protein metabolism by liver) Amino Acid breakdown Ammonia molecules absorbed in blood 3.6 -7.2 mmol/L Ammonia converted to urea Urea excreted thru urine Indicates renal function Increases when renal perfusion decreases Determines serum osmolality Affects protein and metabolism state Factors that Increases BUN Decreased Renal Function Dehydration Fever Increase protein intake
Serum Creatinine
0.7 1.4mg/dl 62 124 mmol/L 1.010 1.025
Urine Specific Gravity
Hematocrit
M: 42 52% F: 35 47% 75 200 mEq/24 Or mmol/L
Urine Sodium
GI bleeding Sepsis Factors that Decreases BUN Conditions that expand fluid volume Hyponatremia Overhydration SIADH ADH Low Protein Diet Starvation End product of muscle metabolism Better indicator of renal function than BUN b/c it doesnt vary with protein intake & metabolic state Increases when renal function decreases Measures ability of kidneys to conserve or excrete water. If Low = urine volume (hemodilution) If Elevated = urine volume (hemoconcentration) High glucose and protein falsely elevates result. Can be measured by Calibrated Hydrometer or Urinometer in a cylinder of approx 20mL of urine Measures the volume percentage of RBCs in the whole blood Hct = rbc, plasma volume; dehydration, polycythemia Hct = rbc, plasma volume; overyhydration, anemia Changes with sodium intake & status of fluid volume If sodium intake increases, excretion is increased Assess volume status, dx of hyponatremia, acute renal failure
TYPES OF FLUID IMBALANCES 1. Osmolar Imbalances loss or gain of water only in ECF; altered serum osmolality a. Hyperosmolar Imbalance (Dehydration) Loss of water only but increased serum electrolytes particularly sodium Causes Hyperosmolality and Hemoconcentration Cells shrink as water is pulled out from cell and drawn into ECF causing cellular dehydration Etiology: Insensible water losses, diabetes insipidus, elderly, enteral feedings w/o sufficient water b. Hypo-osmolar imbalance (Overhydration) Gain of water only but decreased serum electrolytes particularly sodium Causes Hemodilution Cells swell as water is drawn into cells causing cellular edema & impaired neurologic function Etiologic Factors: water intoxication, SIADH 2. Isotonic Imbalances loss or gain of water & electrolytes in equal proportions in ECF; serum osmolality remains the same. a. Hypovolemia or Fluid Volume Deficit Isotonic loss of water and electrolytes b. Hypervolemia or Fluid Volume Excess Isotonic gain of water and electrolytes
HYPOVOLEMIA / FLUID VOLUME DEFICIT / ISOTONIC DEHYDRATION
ECF volume deficit Loss of ECF volume exceeds water intake Isotonic loss of water & electrolytes in equal proportions in ECF resulting to decreased circulating blood volume & inadequate tissue perfusion
May occur alone or in combination with other imbalances
Nursing Diagnosis Fluid Volume Deficit Decreased Cardiac Output Potential Complication: Hypovolemic Shock Etiologic Factors 1. Decreased fluid intake (lack of access to gain fluids, anorexia, nausea, impaired swallowing, confusion, depression, infants, elderly, physically & mentally debilitated) 2. GI Losses (vomiting, diarrhea, fistula, prolonged GIT suctioning, bowel ostomies such as colostomy, cecostomy, ileostomy) 3. Profuse sweating /diaphoresis (sensible loss) 4. Fever (insensible loss) 5. Osmotic Diuresis (uo; excretion of glucose, mannitol) 6. Diabetes Insipidus (kidneys are unable to conserve water and inhibits ADH release causing urine production & excretion of large amts of diluted urine) 7. Uncontrolled DM (causes polyuria via osmotic diuresis, d/t blood sugar leaking into urine & taking excess water along with it) 8. Adrenal Insufficiency ( aldosterone release) 9. Coma 10. Third Space Fluid Shift (fluid shifts from vascular space to another area where its not accessible as an ECF; fluid remains in the body but unavailable for use) Ascites (fluid accumulation in peritoneal cavity) Massive bleeding Burns Peritonitis Clinical Manifestations (S/S) BP and CVP HR, PR (bounding), RR, Temp Postural or Orthostatic Hypotension Acute or rapid weight loss Fluid intake < output Oliguria ( uo; kidney attempts to conserve water) Concentrated urine Poor skin turgor (dry) Poor tongue turgor (several furrows, smaller tongue) Decreased capillary refill time Cold, clammy, pale skin d/t peripheral vasoconstriction Flat jugular veins Dry mouth & mucous membranes Sunken eyeballs Thirst Muscle weakness and cramps Lassitude (Fatigue)
Laboratory Data BUN and Creatinine (decreased renal perfusion) Serum and urine osmolality Urine specific gravity (hemoconcentration) Urine specific gravity (uo in Diabetes Insipidus) Hct & Hgb (RBC, plasma volume) Urine Sodium Medical Management 1. Fluid Replacement Oral fluids for mild or moderate losses IV Fluids Therapy for acute or severe losses Isotonic Solutions (Plasma Expanders) 0.9% NaCl, Lactated Ringers for hypotensives Hypotonic Solution (0.45% NaCl) for normotensives 2. Fluid Challenge Test To distinguish presence of renal damage Administer 100 200 ml of NSS x 15 mins for renal perfusion Normal Result: increased UO, BP, and CVP Pharmacologic Therapy Antidiarrheals for Diarrhea Anti-emetics for vomiting Anti-pyretics for fever
3.
Nursing Management 1. Assess and monitor patients with FVD manifestations 2. Monitor I & O 3. Monitor v/s 4. Assist and teach clients how to change positions slowly to avoid postural hypotension and falls 5. Monitor daily weights same time & same amount of clothing of patient approximate the weight loss: * 1 kg (2.2 lbs) = 1L of fluids are lost * 0.5kg = 500ml of fluids are lost 6. Minimize fluid losses Provide oral fluids as tolerated If patient is reluctant to drink, provide mouth care and offer ORS in small amounts in frequent intervals (ex. pedialyte) IV administration of fluids 7. Monitor skin and tongue turgor Skin turgor press inner aspects of thighs, abdomen; forehead and sternum for elderly Tongue turgor not affected by age; normal is 1 longitudinal furrow; several furrows & smaller tongue in FVD 8. Monitor Mental Status and LOC may be affected due to cerebral perfusion
HYPERVOLEMIA / FLUID VOLUME EXCESS / ISOTONIC OVERHYDRATION
Isotonic expansion of ECF Isotonic gain of water and electrolytes in equal proportions in ECF due to sodium & water retention resulting to increased circulating blood volume & fluid overload. Always related to increased total body sodium resulting to increased total body water
Nursing Diagnosis Fluid volume excess Risk for inadequate airway clearance Risk for impaired skin integrity Disturbed body image Potential complications a. Pulmonary Edema b. Ascites form of edema wherein fluid is accumulated in peritoneal cavity; etiologic factors such as nephrotic syndrome, some malignant tumors, liver cirrhosis; shortness of breath and dyspnea due to pressure on the diaphragm Etiologic Factors 1. Excessive intake of dietary sodium 2. Excessive or prolonged administration of sodium containing IV fluids (Hypertonic IV Solutions) 3. Compromised regulatory mechanisms in heart failure, renal failure, and liver cirrhosis 4. SIADH (ADH release causes water retention) 5. Hyperaldosteronism ( aldosterone release causes water and sodium retention) 6. Prolonged corticosteroid therapy, OTC drugs, sodium bicarbonate Clinical Manifestations (S/S) BP, CVP, HR, RR, PR Shortness of breath and dyspnea Wheezes and moist crackles (rales) upon auscultation Acute or rapid weight gain Fluid Intake > Output Polyuria / Increased UO (kidney compensates to excrete excess fluids; diluted urine) Distended jugular veins Pitting edema on dependent parts such as ankles, legs, and feet if patient is ambulatory; sacral if patient is confined to bed. Generalized edema or anasarca if theres presence of heart, liver, and renal failure.
Serum and urine osmolality Urine specific gravity (UO; kidney compensates by excretion of excess fluids) Hematocrit (rbc, plasma volume) Urine Sodium (kidneys excrete excess volume)
Medical Management 1. Discontinue IVF if related to sodium containing IVF 2. Dietary sodium and water restriction Avoid foods high in sodium Depends on water source (distilled water can be used; bottled water contains sodium; avoid water supplements and water softeners) 3. Increase Protein Intake for malnourished or with low protein levels to increase oncotic pressure for excretion 4. Diuretics Thiazide mild to moderate FVE; blocks sodium reabsorption in distant tubule Loop severe FVE; blocks sodium reabsorption in loop of henle (ex. Furosemide lasix) 5. Dialysis (Hemodialysis or Peritoneal) for severely impaired renal function removes nitrogenous wastes, sodium and water for acid base balance 6. Continuous renal replacement in cases of renal failure Nursing Management 1. Assess clients with FVE manifestations 2. Monitor I & O, daily weights, vital signs 3. Monitor breath sounds (especially if with IV fluids) 4. Monitor IV infusion rates 5. Monitor responses to diuretics Electrolyte imbalances may occur such as hyponatremia, hypokalemia (administer potassium supplements), hypermagnesemia, and azotemia (increased nitrogen levels & urea & creatinine is not excreted) 6. Monitor pitting edema note pitting degree & measure circumference in millimetres (mm) 7. Dietary sodium and fluid restriction 8. Restriction of OTC drugs 9. Promote rest periods for blood circulation and renal perfusion to avoid venous pooling 10. Assist in Semi Fowler Position for lung expansion 11. Turn and reposition every 1 2 hours to prevent skin breakdown; provide skin care to avoid pressure sores 12. Elevate legs and use of antiembolic stockings 13. Teach clients about edema, ascites, and necessities of paracentesis
Laboratory Data (Hemodilution) BUN and Creatinine
SODIUM IMBALANCES
Sodium
Normal value: 135 145 mEq/L Most prevalent cation in ECF Loss or gain is accompanied by loss or gain of water Imbalances are associated with parallel changes in osmolality
Regulated by thirst, ADH, and Renin Angiotensin Aldosterone System Aldosterone increases sodium and water retention Its concentration is the major determinant of ECF volume Sodium increases calcium loss
Functions of Sodium
1. 2. 3. 4. 5. Primary regulator of ECF volume and concentration Major determinant of ECF osmolality Transmission of nerve impulses Assists in muscle contraction Regulates acid - base balance
Common Food Sources
Table salt, seasonings, ketchup, mustard, butter, cheese, processed &canned foods, shellfish, meat, eggs
SODIUM DEFICIT: HYPONATREMIA
Serum sodium level <135 mEq/L associated with loss of sodium containing fluids or excess of water Cells swell as water is pulled from ECF and drawn into cells resulting to cellular edema
Poor skin turgor (dry) Decreased mucosa and saliva GI changes anorexia nausea & vomiting abdominal cramps Neurological changes Cerebral edema (acute loss) Status Epilepticus (chronic loss; state of persistent seizure) Signs of increased ICP when <115 mEq/L Muscle twitching Lethargy Hemiparesis (weakness on one side of the body; patient can move impaired side but with reduced muscular strength) Papilledema (optic disc swelling) Seizure Coma
Nursing Diagnosis: Risk for Injury Etiologic Factors 1. Loss of Sodium GI losses Profuse sweating Diuretics Adrenal Insufficiency 2. Gain of Water Water intoxication resulting to diluted serum sodium or dilutional hyponatremia Excessive Isotonic D5W Excessive Hypotonic IV solutions & tube feedings Excessive water supplements Hyperglycemia (DM) Heart failure SIADH ADH release causes water retention Head trauma, AIDS, malignant tumors, oat cell lung cancer Medications associated with water retention Certain tranquilizers OTC drugs Oxytocin
Laboratory Data - HEMODILUTION Serum sodium level <135 mEq/L Serum and urine osmolality Urine specific gravity (UO; kidney compensates to excrete excess water) Urine sodium (diluted urine) Medical Management: 1. Sodium Replacement Increase dietary sodium intake Administration of sodium containing IV fluids a. Isotonic Solutions (0.9%NaCl, LR) not > 12 mEq/L in 24 to avoid neurological damage b. Hypertonic Solution (3% NaCl) if neurological manifestations (seizure) occurs; not >125 mEq/L 2. Water Restriction 3. Administration of Lithium prescribed for SIADH Nursing Management 1. Identify & monitor at risk patients for early treatment 2. Monitor I & O, VS, daily weights, abnormal losses of sodium & gains of water, GI and neurologic changes 3. Encourage dietary sodium if cause is sodium loss 4. Fluid restriction if cause is water gain 5. Assess signs of circulatory overload for patients with cardiovascular disease (cough, dyspnea, weight gain in 24, crackles upon auscultation) 6. Seizure precaution 7. Observe signs of Lithium toxicity
3.
4.
Clinical Manifestations (S/S) Hypotension Headache
SODIUM EXCESS: HYPERNATREMIA
Elevated serum sodium >145 mEq/L associated with sodium gain or water loss Causes Hyperosmolality (increased serum sodium concentration in ECF) which pulls fluid out of cells cells shrink and may result to cellular dehydration
Nursing Diagnosis: Risk for Injury
2. 3. 4. 5. 6.
Etiologic Factors a. Sodium Gain Excessive dietary sodium intake Excessive hypertonic IV fluids & enteral feedings Excessive corticosteroid, sodium bicarbonate, sodium chloride, OTC drugs Near drowning in sea water b. Water Loss Inadequate water intake Water deprivation (patients who cant perceive, respond, or communicate thirst such as elderly, infants, cognitively impaired) Insensible water losses (hyperventilation, fever) Heat stroke Watery diarrhea Diabetes insipidus
7.
Obtain medical & diet history to check sodium content of food & medications. Provide teaching to avoid OTC drugs. Monitor abnormal gains of sodium & loss of water, thirst, elevated temperature, behavioural changes Promote dietary sodium restriction Provide fluids regularly. If oral route is not possible, plan with Physician the alternative route. If Enteral Feedings, provide sufficient water to keep serum sodium within normal limits. Administer Hypotonic IV Solutions SLOWLY monitor response, check serum sodium levels, & observe neurologic changes.
Clinical Manifestations Temp, BP, HR, PR Thirst may be impaired in elderly and ill patients Dry, red, swollen tongue Dry, sticky mucosa Dry, flushed skin Restlessness and weakness Neurological changes in severe cases Laboratory Data - Hemoconcentration serum sodium levels >145 mEq/L serum and urine osmolality urine specific gravity urine osmolality in Diabetes Insipidus Medical Management 1. Dietary Sodium Restriction 2. Restriction of medications that contains sodium 3. Gradual lowering of serum sodium by IV admin a. Isotonic D5W water replacement w/o sodium b. Hypotonic Saline Solution (0.3% NaCl) 4. Diuretics to excrete excess sodium 5. Desmopressin Acetate (DDAVP) for Diabetis Insipidus Nursing Management 1. Assess and monitor at risk patients
POTASSIUM IMBALANCES
Potassium Normal Values: 3.5 5.0 mEq/L Most prevalent cation in ICF Moves in and out of cells by the NaK+ pump Normal renal function is essential for 80% of K+ is excreted thru kidneys & 20% is lost thru bowel & sweat. Kidneys regulate potassium levels by adjusting the amount of excreted urine Aldosterone increases potassium excretion
As serum K+, so does its level in renal tubule cell Insulin helps K+ move into ICF Tissue damage & acidosis shifts potassium out of cells.
Functions of Potassium 1. Maintains ICF Osmolality 2. Transmission and conduction of nerve impulses 3. Maintains normal cardiac rhythm 4. Skeletal muscle contraction 5. Regulates acid base balance Potassium Rich Foods ** Must be ingested daily b/c body cannot conserve it ** Fruits (banana, oranges, apricot, cantaloupe, raisins) Vegetables (avocado, raw tomato, raw carrot, spinach, baked potato, legumes) Whole grains, meat, fish Milk, coffee, orange juice
ventricular arrhythmias, impaired repolarization, impaired arterial blood flow Fatigue, paresthesias, muscle weakness, leg cramps, depressed DTRS, paralysis Glucose Intolerance
Laboratory Data 1. ECG Changes Flat or inverted T waves or both suggesting ischemia ST depression Elevated U Wave 2. ABG: Metabolic Alkalosis (high pH) Medical Management 1. Oral Potassium Replacement Increase dietary potassium intake Oral potassium supplements if dietary intake is inadequate; for mild & moderate losses. Administer w/ food or fluids to prevent gastric irritation. 2. IV Potassium Replacement Mandatory if severe losses 2mEq/L Adult without abnormal losses 40 80 mEq/L Nursing Management 1. Assess and monitor patients at risk b/c severe hypokalemia is life threatening and can lead to cardiac or respiratory arrest and death. 2. Encourage foods high in potassium 3. Monitor ECG changes 4. Monitor ABG for increased HcO3 and Ph levels 5. Monitor renal function thru BUN and Creatinine 6. Careful selection of pre mixed solution of IV Potassium Chloride as concentration ranges from I0 40 mEq/100mL 7. Monitor UO. Administer potassium after adequate UO has been established. Stop infusion if UO is <20ml/hr. Serum K+ levels can rise dangerously in oliguria 8. Administer potassium using IV Infusion Pump. DO NOT administer by IV PUSH or IM to avoid replacement of potassium quickly a. Peripheral IV Line 20 mEq/100ml; no faster than 10 20 mEq/hr; painful in peripheral veins b. Central IV Catheter - >20 mEq/100ml 9. Care in elderly who have low potassium requirements 10. Monitor digitalis toxicity
HYPOKALEMIA OR POTASSIUM DEFICIT
Serum potassium <3.5 mEq/L Deficit in total potassium stores Potential Complication: Arrythmias
Etiologic Factors 1. GI Losses (K+ is high in intestinal fluids) vomiting, diarrhea, prolonged GIT suctioning, enema, misuse of laxatives, ileostomy that divert and drain liquid fecal material villous adenoma (tumor of intestinal tract; excretes potassium rich mucous) 2. Poor Dietary Potassium Intake 3. Metabolic Alkalosis (K+ shifts from ECF to ICF) 4. Hyperaldosteronism 5. Insulin Hypersecretion 6. Potassium wasting diuretics, digitalis, sodium penicillin, carbenicillin, corticosteroids
Clinical Manifestations Nausea, vomiting, anorexia, decreased bowel motility Hypotension, bradypnea, altered airway responsiveness, dysrhythmias, potentially lethal
HYPERKALEMIA OR POTASSIUM EXCESS Serum potassium >5mEq/L Potential complication: Arrhythmias, Cardiac Arrest Nursing Diagnosis: Risk for Injury
Etiologic Factors 1. Usually Iatrogenic or treatment related 2. Rapid IV admin of Potassium 3. Improper use of Potassium supplements 4. Impaired renal function
5. 6. 7. 8. 9.
Hypoaldosteronism Addisons Disease Metabolic Acidosis (movement of K+ from ICF to ECF) Severe tissue trauma, injury, & infections Pseudohyperkalemia (tight tourniquet while drawing blood sample, marked leukocytosis, thrombocytosis, drawing blood above the site while K+ is infusing) 10. Transfusion of aged or stored blood to patients with impaired renal function 11. Potassium sparing diuretics, potassium chloride, ACE inhibitors, NSAIDS, beta blockers, heparin Clinical Manifestations (S/S) 1. Cardiac changes: effect on myocardium Dysrhythmia (irregular heartbeat) Ventricular fibrillation or cardiac standstill Impaired cardiac depolarization Repolarization occurs frequently Tachycardia Bradycardia Arrhythmias Cardiac arrest 2. GI Manifestations Hyperactive bowel sounds; increased motility Abdominal cramping Intestinal colic Diarrhea 3. Skeletal muscle weakness leading to paralysis (flaccid quadriplegia) Laboratory Data 1. ECG Changes (Moderate) Tall Peaked, narrow T waves Depressed ST segment Shortened QT interval Wide, flat P Wide QRS 2. ECG Changes (Extreme) cardiac arrest may occur Prolonged PR Interval Absence of P waves Wider QRS complex 3. ABG : Metabolic or Respiratory Acidosis
2.
3. 4. 5. 6. 7. 8.
Oral or Retention Enema of cation exchange resins (ie. Kayexelate) for severe cases; contraindicated to paralytic ileus (may cause intestinal perforation), heart failure (may cause sodium retention) IV Calcium Gluconate antagonizes cardiac conduction abnormalities IV Sodium Bicarbonate alkalinize plasma & move +K into cells IV Insulin & Hypertonic Dextrose shift K+ into cells Beta 2 Antagonists (Albuterol) decrease serum K+ but may cause tachycardia & chest discomfort Diuretics Dialysis
Nursing Management 1. Monitor patients at risk (ex. patients with renal failure) 2. Monitor ECG to check cardiac status 3. Monitor ABG for acidosis 4. Promote adherence to dietary potassium restriction 5. Observe the ff when withdrawing blood: Avoid prolonged use of tourniquet Warn patient not to exercise extremity before blood is drawn Dont take blood sample at the extremity where potassium is administered Deliver blood sample asap to prevent hemolysis
Medical Management 1. Dietary potassium restriction & removal of K+ containing medications for mild or non acute cases
CALCIUM IMBALANCES
Calcium Normal values: 8.6 10.2 mg/dl or 2.2 2.6 mmol/L More than 99% of bodys calcium is combined with phosphorous & concentrated in skeletal system Has inverse or opposite relationship with phosphorous (High phosphate = low calcium) 2 Types: Ionized Calcium & Bound to plasma proteins Ionized form is biologically active w/c is essential for neuromuscular activity & blood coagulation (clotting) Obtained from ingested foods and absorbed in the presence of gastric acidity and vitamin D Excreted primarily in feces and the remainder in urine
Functions 1. Major structural component of bones & teeth -Formation of bones and teeth 2. Transmission of nerve impulses 3. Regulates muscle contraction & relaxation (ie. myocardial contraction for regular heart beat) 4. Blood coagulation (clotting) 5. Decreases neuromuscular irritability 6. For Vitamin B12 absorption and use Regulations 1. GIT calcium is absorbed in intestine vitamin D helps increase calcium absorption 2. Renal regulation calcium is filtered in glomerulus and reabsorbed in kidney tubules 3. Endocrine regulation Parathyroid Hormone (PTH) from Parathyroid Glands is released when calcium level is LOW. Results to the release of calcium from bones, increased absorption from GIT, increased retention by kidneys but phosphate is excreted Calcitonin from Thyroid Gland is released when calcium level is high which causes excretion of both calcium & phosphate by the kidney and promotes deposition of calcium in bones. HYPOCALCEMIA OR CALCIUM DEFICIT Serum calcium <8.6 mg/dl must be considered in conjunction with low serum albumin level (protein) Etiologic Factors 1. Osteoperosis total body calcium loss but may have normal serum calcium levels 2. Low Serum Albumin 3. Hyperphosphatemia 4. Hypoparathyroidism (PTH; idiopathic /post surgery) 5. Inadequate Dietary Calcium 6. Calcium Malabsorption 7. Vitamin D deficiency 8. Massive transfusion of citrated blood (Citrate combined with ionized calcium) 9. Alkalosis calcium combined to albumin 10. Pancreatitis 11. Renal Failure 12. Alcoholism Clinical Manifestations (S/S) 1. TETANY Induced by neuromuscular excitability Tingling sensations of fingertips & toes (carpopedal spasms) & facial muscle spasms. Pain may develop as a result. Hyperactive deep tendon reflexes 2. Positive TROUSSEAUSS SIGN Can be elicited by inflating BP cuff on upper arm 20 mmHg above systole within 2 5 minutes (approximately 3 mins) Ischemia induced carpal spasms (ischemia of ulnar nerve develops; contraction of fingers and hand; adducted thumb, flexed wrist &
metacarphophalangeal joints, extended interphalangeal joints with fingers together)
3.
Positive CHVOSTEKS SIGN Twitching of the lip at the corner of mouth to spasms of all facial muscles. Can be elicited by tapping the facial nerve 2cm anterior to earlobe, just below zygomaticus arch
4.
Respiratory: Dyspnea, laryngeal stridor, laryngspasms, bronchospasms 5. Mental changes impaired memory, depression, confusion, delirium, hallucinations 6. Seizures 7. Chronic Hypocalcemia Can retard growth & IQ in children Hyperactive bowel sounds, dry and brittle hair & nails, abnormal clotting, hypotension Laboratory Results Decreased serum calcium <8.6mg/dl Elevated phosphate level Decreased Prothrombin Time (PT) Torsades de Pointes ECG: Prolonged QT interval, Lengthened ST segment
Medical Management 1. Administer IV Calcium Salt by SLOW IV BOLUS or IV INFUSION using volumetric infusion pump or diluted with D5W a. Calcium Gluconate yields 4.5 mEq/L b. Calcium Gluceptate c. Calcium Chloride yields 13. 6 mEq/L; more ionized but not commonly used - may cause irritation & sloughing of tissues if it infiltrates
2. Dont add calcium with the ff: 0.9% NaCl which increases renal calcium loss Parenteral solutions that contains bicarbonate or phosphates which causes precipitation Vitamin D Therapy to increase absorption in GIT Aluminum hydroxide, calcium acetate, or calcium carbonate antacids to decrease phosphorous levels
2. 3.
4. 5.
before treating hypocalcemia in patients with chronic renal failure. Administer cautiously to patients receiving digitalis as it potentiates the action of digitalis Thiazide diuretics to decrease excretion of calcium
confusion, disorientation, impaired memory, slurred speech, lethargic, acute psychotic behaviour, coma
Nursing Management 1. Observe patient for hypocalcaemia manifestations 2. Encourage dietary intake of calcium rich foods 3. Encourage oral calcium supplements 4. Restrict alcohol, caffeine, laxatives & antacids that contain phosphorous w/c calcium absorption 5. Restrict smoking which increases calcium loss 6. Encourage regular exercise to decrease bone loss 7. Monitor IV rate; rapid admin can cause cardiac arrest 8. Keep patient in bed during infusion & monitor BP b/c calcium replacement can cause postural hypotension 9. Maintain Patent Airway - Laryngeal Stridor may occur 10. Seizure precaution 11. Observe digitalis toxicity CALCIUM EXCESS: HYPERCALCEMIA Serum calcium >10.2 mg/dl Potential complication: Arrythmias Etiologic Factors 1. Hyperparathyroidism (PTH release) 2. Malignant tumors 3. Prolonged immobilization (causes demineralization or loss of bone minerals) 4. Acidosis 5. Excessive calcium supplements 6. Vitamin A & D intoxication 7. Lithium and Theophylline toxicity 8. Digitalis Toxicity 9. Thiazide diuretics potentiates PTH action on kidneys reducing urinary calcium excretion 10. Milk Alkali Syndrome too much milk or antacids
Laboratory Results Serum calcium >10.2 mg/dl ECG changes: shortened ST segment and QT interval bradycardia heart blocks Double Antibody PTH test differentiates primary hyperparathyroidism and malignancy as a cause of hypercalcemia; xrays may reveal bone changes secondary to malignancy, bone cavity, and urinary calculi Sulkowitch Urine Test analyzes calcium in urine; dense precipitation is observed Medical Management 1. Treat underlying cause chemotherapy if malignancy parathyroidectomy if parathyroidism 2. IV admin of 0.9% NaCl to dilute & and excrete calcium 3. IV admin of Phosphate 4. Calcitonin Administer IM; for patients with heart disease or renal failure who cant tolerate large amounts of sodium; reduces bone resorption; increases deposit of calcium and phosphorous in bones and increases urinary excretion of calcium & phosphorous 5. Loop Diuretics 6. Mobilization Nursing Management 1. Monitor and assess at risk patients 2. Monitor ECG changes 3. Perform skin allergy testing prior administration of calcitonin. 4. Encourage mobilization 5. Encourage increase fluid intake (fluids with sodium unless contraindicated b/c sodium excretes calcium) 6. Encourage dietary fiber in case of constipation 7. Safety precautions during mental changes
Clinical Manifestations Hypertension Flank Abdominal pain and bone pain Polyuria and Polydypsia Decreased muscle tone fatigue, muscle weakness, nausea, vomiting, constipation, hypoactive DTRS Mental changes
MAGNESIUM IMBALANCES
Magnesium NV: 1.3 2.3 mg/dl (0.62 0.95 mmol/L) 50 60% contained in bone Second most abundant electrolyte in ICF Factors that regulate calcium balance influence magnesium balance Major Functions
1. Coenzyme in carbohydrate and protein metabolism 2. Acts directly in myoneural junction Mg = neuromuscular irritability & contractility Mg = neuromuscular excitability Produces sedative effect by inhibiting release of acetylcholine (neurotransmitter) Increases stimulus threshold in nerve fibers 3. Important for normal cardiac function MAGNESIUM DEFICIT: HYPOMAGNESEMIA Serum Level <1.3 mg dl (< 0.62 mmol/L) Associated with hypokalemia and hypocalcemia Etiologic Factors GI Losses (i.e. prolonged nasogastric suctioning, intestinal fistulas, diarrhea) Disruption in small bowel function because its the major site of magnesium absorption (i.e. intestinal resection, inflammatory bowel disease) Alcohol withdrawal; chronic alcoholism Enteral / parenteral feeding deficient in magnesium Rapid administration of citrated blood Medications: aminoglycosides, cyclosporine, cisplatin, digitalis, amphotericin Occurs in Diabetic Ketoacidosis, insulin therapy Pregnancy, lactation, burns, hypothermia
neuromuscular hyperexcitability with muscle weakness, tremors, & athetoid movements (slow, involuntary twisting) Tremors, vertigo, nystagmus, generalized or focal seizures, laryngeal stridor, (+) chvosteks and (+) trousseauss sign 2. Mental Changes Mood alterations: depression, confusion, apprehension Delusions, hallucinations, psychoses 3. Hypotension, Vasodilation 4. Dysrrythmias Laboratory Data Serum magnesium <1.3 mg/dl Coexisting low serum potassium & calcium levels Medical Management 1. Dietary Intake of magnesium rich foods for mild losses Green leafy vegetables Nuts, seeds, legumes, whole grains seafood Peanut butter and cocoa Oral Magnesium salts IV Magnesium Sulfate NOT > 150mg/min OR 67 mEq/8hrs Nursing Management 1. Assess and monitor at risk patients 2. Monitor VS to identify changes in cardiac rhythm, hypotension, and respiratory distress 3. Monitor DYSPHAGIA; assess ability to swallow with water prior admin of foods and medication 4. Encourage dietary magnesium rich foods 5. Monitor UO before, during, & after administration ; notify physician if UO is <100ml / 4hrs 6. Monitor IV magnesium rate Ready Calcium Gluconate to treat Mg toxicity Seizure precaution For Alcoholics, provide teaching, counselling, and possible referral to alcohol abstinence programs. Monitor and treat potential hypocalcemia
Clinical Manifestations 1. Neuromuscular changes
MAGNESIUM EXCESS: HYPERMAGNESEMIA Serum level > 2.3 mg/dl (> 0.95 mmol/L) Associated with hyperkalemia and hypercalcemia Etiologic Factors Renal failure
Excessive administration of Magnesium Excessive use of magnesium antacids and laxatives (ie. Maalox, milk of magnesia) Diabetic Ketoacidosis Adrenal insufficiency Addisons disease Medications that decrease GI motility (i.e. Opioids, Anti-cholinergics)
Clinical Manifestations Hypotension, Bradycardia, Respiratory Distress (Respiratory depression) Soft tissue calcification Facial flushing Hypoactive or diminished reflexes, muscle weakness, paralysis Lethargy, Difficulty in speaking (DYSARTHIA) Platelet clumping and delayed thrombin formation Laboratory Data Serum calcium >2.3 mg/dl Coexisting Hypokalemia and Hypocalcemia Medical Management 1. Avoid administration to patients with renal failure 2. Restriction of dietary magnesium intake and oral magnesium salts 3. In EMERGENCIES such as RESPIRATORY DISTRESS: VENTILATORY SUPPORT & IV CALCIUM GLUCONATE 4. IV 0.9%NaCl, Lactated Ringers, Loop Diuretics for patients with normal renal function Nursing Management 1. Asses and monitor at risk patients 2. Avoid dietary magnesium intake & administration of medications that contains magnesium 3. Monitor: Hypotension Decreased Respirations <12 bpm and shallow respirations Decreased patellar reflexes Decreased urine output <30ml/h Diminished LOC
PHOSPHOROUS IMBALANCES
PHOSPHATE Normal value: 2.5 4.5 mg/dl (0.8 1.45 mmol/L) Maintenance requires adequate renal function Primary anion of ICF 85% is located in the bones and teeth, 14% in soft tissues, and less than 1% in ECF
Functions 1. Structural support for bones and teeth 2. Maintains function of muscles, RBCS, & nervous system 3. ATP formation and 2,3 Diphosphoglycerate (facilitates release of oxygen in Hgb) 4. Maintains acid base buffering system 5. Metabolism of carbohydrates, proteins, and fats
Food Sources 1. milk and milk products (ie. hard cheese, creams) 2. organ meats (i.e. liver) 3. nuts and whole grains 4. fish and poultry 5. dried vegetables 6. sardines PHOSPHOROUS DEFICIT: HYPOPHOSPHATEMIA Serum phosphorous level <2.5mg/dl Can be caused by intracellular shift of K+ from serum into cells, increased urinary excretion of K+, or decreased intestinal absorption of K+ Etiologic Factors 1. Poor dietary intake of phosphorous 2. Admin of calories to patients w/ severe protein calorie malnutrition (ie. anorexia or alcoholism) 3. Excessive intake or admin of simple carbohydrates 4. Chronic Alcoholism & Alcohol withdrawal 5. Heat Stroke 6. Prolonged hyperventilation 7. Diabetic Ketoacidosis 8. Respiratory Alkalosis (intracellular shift of PO4) 9. Hepatic Encepalopathy 10. Major Thermal Burns 11. Low Mg, Low K+, & Hyperparathyroidism 12. Excess phosphorous binds to antacids 13. Chronic diarrhea or severe potassium restriction 14. Vitamin D deficiency (may lead to OSTEOMALACIA softened brittled bones) Clinical Manifestations 1. Neurologic manifestations 2. Tissue hypoxia (leads to RR & Respiratory Alkalosis) 3. Muscle damage (muscle weakness & pain; weak respiratory muscles impairs ventilation) 4. Insulin resistance and thus hyperglycemia 5. Bruising & bleeding from platelet dysfunction (chronic) Laboratory Data 1. Serum level <1.3 mg/dl 2. Glucose or insulin may cause slight decrease in serum phosphorous level 3. PTH level increased in Hyperparathyroidism 4. X-ray - skeletal changes of osteomalacia or rickets Medical Management 1. Oral Phosphate replacement Increase dietary intake Oral phosphate supplements (Neutro phos capsule, fleets phosphorous soda) 2. IV Phosphorous replacement
IV phosphorous available as sodium or potassium phosphate. Rate of admin should not > 10 mEq/h
Nursing Management 1. Identify & monitor patients at risk b/c malnourished patients receiving parenteral nutrition are at risk when calories are administered rapidly. Gradually introduce calories to avoid rapid shift of phosphorous into cells. 2. Monitor IV site for sloughing & necrosis may occur with infiltration 3. Encourage foods high in phosphate for mild losses 4. Oral Phosphate supplements for moderate losses 5. Prevent Infection b/c granulocytes may be altered PHOSPHOROUS EXCESS: HYPERPHOSPHATEMIA Serum level > 4.5 mg/dlc (>1.45 mmol/L) Etiologic Factors 1. RENAL FAILURE 2. Increase intake, decreased output, or shift from ICF to ECF and increased absorption 3. Excessive Vitamin D intake 4. Administration of TPN 5. Chemotherapy for neoplastic disease 6. Hypoparathyroidism 7. Metabolic or respiratory acidosis 8. Diabetic Ketoacidosis 9. Acute Hemolysis 10. Muscle necrosis Primary Complication: Metastatic Calcification (soft tissues, joints, arteries) Clinical Manifestations 1. Tetany (short term consequence) 2. Soft tissue calcifications (long term consequence occurs with patients with low GFR) 3. Decreased UO, impaired vision, and palpitations Medical Management 1. Treat underlying cause 2. Restrict dietary phosphate 3. Oral or Parenteral Vitamin D (CALCITRIOL) Oral (Rocaltrol) Parenteral (Calcijex) 3. Calcium binding antacids (calcium carbonate/ citrate) 4. Admin of Amphojel with meals but can cause bone & CNS toxicity with long term use. 5. Loop Diuretics, IV Saline, Dialysis 6. Surgery - removal of large ca & phosphate deposits Nursing Management 1. Assess and monitor at risk patients for manifestations 2. Advise to avoid phosphorous-rich foods 3. Advise to avoid phosphate containing substances such as laxatives and enemas Serum level of chloride reflects a change in dilution and concentration of the ECF and does so in direct proportion to the sodium concentration. Clinical manifestations Muscle Diagnostic test results Serum
CHLORIDE
Contained in gastric & pancreatic juices, sweat, bile, and saliva. Sodium and chloride in water make up the composition of the ECF and assist in determining osmotic pressure.
Electrolyte Imbalance
hypertonicity and tetany HYPOCHLOREMIA Chlorine deficit Shallow, depressed breathing Usually associated with hyponatremia and its characteristic symptoms, such as muscle weakness, and twitching
chloride <98mEq/L Serum pH >7.45 (supportive value) Serum CO2 >32 mEq/L (supportive value)
HYPERCHLOREMIA Chlorine excess
>108mEq/L Weakness Diminished cognitive ability, possibly leading to coma Serum pH <7.35, Serum CO2 < 22 mEq/L (supportive values)
Contributing Factors Addisons disease Reduced chloride intake or malabsorption Untreated diabetic ketoacidosis, metabolic alkalosis, overuse of bicarbonate Excessive sweating, diarrhea Vomiting, gastric suctioning Sodium and potassium deficiency Loop, osmotic, thiazide diuretic Rapid removal of ascitic fluid with high sodium content IV fluids that lack chloride (dextrose and water) Draining fistulas and ileostomies Heart failure, cystic fibrosis Medical Management 1. Administration of IV Normal saline (0.9%) and half strength (0.45%) solution to replace chloride. 2. Re-evaluate whether patient receiving diuretic should be discontinued or changed 3. Ammonium chloride to treat metabolic alkalosis depending on patients weight and serum chloride level. caution w/ patients with impaired liver or renal function Nursing Management 1. Encourage dietary intake of foods high in chloride: tomato juice, eggs, cheese, milk, salty broth, canned veggies, processed meats 2. Avoid water w/o electrolytes b/c it excretes large amount of chloride 3. Monitor I&O, V/S, ABG, LOC, muscle strength Electrolyte Imbalance Clinical manifestations Deep, rapid breathing Diagnostic test results Serum chloride
Contributing Factors Excessive sodium chloride infusions with water loss; hypernatremia Head injury Renal failure Corticosteroid use Dehydration; severe diarrhea (loss of bicarbonate) Respiratory alkalosis Administration of diuretics, overdose of salicylates Kayexalate, acetazolamide, phenylbutazone Ammonium chloride use Hyperparathyroidism, metabolic acidosis Medical Management 1. Hypotonic IV solutions to restore balance. 2. Lactated Ringers solution to convert lactate to bicarbonate in liver increasing bicarbonate & corrects acidosis. 3. IV sodium bicarbonate to increase bicarbonate levels. 4. Diuretics 5. Sodium, chloride, and fluids are restricted. Nursing Management 1. Monitoring of I & O, vital signs and ABGS 2. Assessment findings related to respiratory, neurologic, and cardiac systems are documented and observed for any changes that should be communicated with the physician. 3. Teach patient the diet that should be followed to manage hyperchloremia & maintain adequate hydration.
Tonicity of IV Fluids
Isotonic 0.09%NaCl (PNSS) D5W D5NSS Lactated Ringers Cell volume remains the same Fluid moves equally between compartments Hypotonic Fluid 0.45% NaCl
moves into RBC causing cell rupture (hemolysis) Fluid moves from vascular space (plasma) and enter the cells Hypertonic D5LR 5% Dextrose in 0.45Saline 5% Dextrose in 0.9 Saline D10W
Fluid moves out of the cell causing crenation (shrinking) of RBC
Fluid is pulled out of the cells and into the vascular system, so intravascular volume
Você também pode gostar
- Gender Dysphoria & ADHDDocumento21 páginasGender Dysphoria & ADHDAndrew StewartAinda não há avaliações
- Cardiovascular FunctionDocumento157 páginasCardiovascular FunctionJonnabelle PadillaAinda não há avaliações
- Subject: Leukemia Professor: Ia Marashkhia Researcher: Alireza Farhadiyeh (1701940)Documento14 páginasSubject: Leukemia Professor: Ia Marashkhia Researcher: Alireza Farhadiyeh (1701940)alirezaAinda não há avaliações
- Handout Medical-Surgical Nursing Fluid and ElectrolyteDocumento13 páginasHandout Medical-Surgical Nursing Fluid and ElectrolytePaul Christian P. Santos, RN100% (10)
- Fluid Electrolyte Balances and ImbalanceDocumento157 páginasFluid Electrolyte Balances and ImbalanceManisha Shakya0% (1)
- Med Surg CardsDocumento54 páginasMed Surg CardsIanne Merh100% (3)
- Anti Psychotic DrugsDocumento2 páginasAnti Psychotic DrugscalfornianursingacadAinda não há avaliações
- Nervous SystemDocumento11 páginasNervous SystemMabesAinda não há avaliações
- GI DrugsDocumento79 páginasGI DrugsreecoleAinda não há avaliações
- Small Bowel Obstruction System - DisorderDocumento1 páginaSmall Bowel Obstruction System - DisorderMarina Wasem Netzlaff0% (1)
- Chapter61 Management of Patients With Neurologic DysfunctionDocumento49 páginasChapter61 Management of Patients With Neurologic DysfunctionAhmed 123Ainda não há avaliações
- Emergency Approaches To Neurosurgical ConditionsDocumento217 páginasEmergency Approaches To Neurosurgical Conditionsashwini sharmaAinda não há avaliações
- Alteration in Fluid and Electrolyte ImbalanceDocumento118 páginasAlteration in Fluid and Electrolyte ImbalanceRenuga SureshAinda não há avaliações
- Medication Work Sheet For MedSurgDocumento5 páginasMedication Work Sheet For MedSurgRyanMitchell100% (2)
- Urosepsis-Sepsis - (KeithRN-Unfolding THIGPEN PDFDocumento11 páginasUrosepsis-Sepsis - (KeithRN-Unfolding THIGPEN PDFOLga A. Thigpen100% (4)
- Nursing Concept MapDocumento2 páginasNursing Concept MapMary Mann100% (1)
- Blood Transfusion Purpose: 9. Check Blood For Presence of BubblesDocumento2 páginasBlood Transfusion Purpose: 9. Check Blood For Presence of BubblesMabes100% (1)
- Pharmocology Drug Cards: InnovarDocumento33 páginasPharmocology Drug Cards: InnovarnamitaAinda não há avaliações
- X-Ray Interpretation Skills: Dr. Hisham AlsanawiDocumento68 páginasX-Ray Interpretation Skills: Dr. Hisham AlsanawiVika DamayAinda não há avaliações
- Pharmacology Drug ClassificationDocumento4 páginasPharmacology Drug ClassificationjetdoctrzAinda não há avaliações
- Basic Nursing NotesDocumento4 páginasBasic Nursing Notesbonggoi100% (1)
- Concept Map 1Documento5 páginasConcept Map 1api-396919069Ainda não há avaliações
- Basic or InstrumentsDocumento21 páginasBasic or InstrumentsMabes100% (1)
- Clinical Log Term II PDFDocumento9 páginasClinical Log Term II PDFPriscilla S100% (1)
- Prof Ad BON and NursesDocumento7 páginasProf Ad BON and NursesMabesAinda não há avaliações
- NCP HyperthermiaDocumento2 páginasNCP HyperthermiaMeljonesDaanAinda não há avaliações
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Documento9 páginasNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Gayu Patel0% (1)
- Parenteral Therapy:: Intravenous Therapy (IVT) or VenipunctureDocumento3 páginasParenteral Therapy:: Intravenous Therapy (IVT) or VenipunctureMabes100% (1)
- Digoxin Drug CardDocumento1 páginaDigoxin Drug CardMahsa Ahmadzadeh100% (2)
- Dalidig - Drug StudyDocumento28 páginasDalidig - Drug StudyRaf DalidigAinda não há avaliações
- Simple Study Notes For Nursing - StrokeDocumento5 páginasSimple Study Notes For Nursing - StrokeAshleigh Johnstone100% (1)
- VasopressinDocumento2 páginasVasopressinKim LompotAinda não há avaliações
- Taste and SmellDocumento1 páginaTaste and SmellMabesAinda não há avaliações
- NandaDocumento28 páginasNandaAmit MartinAinda não há avaliações
- Risk For Falls Aeb Loss of BalanceDocumento4 páginasRisk For Falls Aeb Loss of BalanceAlexandrea MayAinda não há avaliações
- Infective EndocarditisDocumento68 páginasInfective EndocarditisDr. Rajesh PadhiAinda não há avaliações
- Cardiovascular DrugsDocumento12 páginasCardiovascular DrugshannahcoAinda não há avaliações
- Drug Card Motrin 800mgDocumento2 páginasDrug Card Motrin 800mgAdrianne BazoAinda não há avaliações
- Hematologic DiseasesDocumento11 páginasHematologic DiseasesPerrilyn Perey100% (2)
- NCC-SickleCellAnemiaManagement ConceptMap InteractivePDFDocumento2 páginasNCC-SickleCellAnemiaManagement ConceptMap InteractivePDFLoggerz Arck100% (1)
- CHN GapuzDocumento23 páginasCHN GapuzMabes100% (1)
- Therapeutic Diet NutritionistDocumento3 páginasTherapeutic Diet NutritionistMabesAinda não há avaliações
- Suture and NeedlesDocumento5 páginasSuture and NeedlesMabesAinda não há avaliações
- Fluids Concept MappingDocumento1 páginaFluids Concept Mappingmariagarcia415100% (1)
- CHF Cardiomegaly Volume OverloadDocumento1 páginaCHF Cardiomegaly Volume Overloadnursing concept mapsAinda não há avaliações
- PositioningDocumento3 páginasPositioningMabesAinda não há avaliações
- PainDocumento3 páginasPainMabesAinda não há avaliações
- NURSING Review Session (Nur 220) Part 1Documento8 páginasNURSING Review Session (Nur 220) Part 1Mariel EstoniloAinda não há avaliações
- Ampicillin Med InfoDocumento1 páginaAmpicillin Med InfoJan McgovernAinda não há avaliações
- Asepsis and InfectionDocumento6 páginasAsepsis and InfectionMabes100% (1)
- Drugs Acting On Cardiovascular SystemDocumento18 páginasDrugs Acting On Cardiovascular SystemIbrahem AlAinda não há avaliações
- LasixDocumento1 páginaLasixKatie McPeek100% (2)
- CHF Concept MapDocumento1 páginaCHF Concept MapChristy Wegner Cooper100% (4)
- Zaroxolyn MetolazoneDocumento1 páginaZaroxolyn MetolazoneCassieAinda não há avaliações
- Fluids and Electrolytes ConceptDocumento31 páginasFluids and Electrolytes ConceptDarwin AndalAinda não há avaliações
- Student Clinical Report SheetDocumento2 páginasStudent Clinical Report SheetMike100% (4)
- FiberCon (Polycarbophil)Documento1 páginaFiberCon (Polycarbophil)EAinda não há avaliações
- This Study Resource Was: System DisorderDocumento1 páginaThis Study Resource Was: System DisorderDeo FactuarAinda não há avaliações
- Drug Class:: Prototype (Generic/Trade) : Eskalith, LithobidDocumento1 páginaDrug Class:: Prototype (Generic/Trade) : Eskalith, LithobidAaLona Robinson100% (2)
- NCP Blood Glucose Imbalance 4thDocumento2 páginasNCP Blood Glucose Imbalance 4thRainier IbarretaAinda não há avaliações
- ClindamycinDocumento3 páginasClindamycinShaira TanAinda não há avaliações
- Acute Renal Failure-Student-Rapid ReasoningDocumento4 páginasAcute Renal Failure-Student-Rapid Reasoningapi-268403950Ainda não há avaliações
- Generic Name: BudesonideDocumento8 páginasGeneric Name: BudesonidemeangelmeAinda não há avaliações
- Ati Medication Template CodeineDocumento1 páginaAti Medication Template CodeineSharee HaywoodAinda não há avaliações
- Drug CardDocumento2 páginasDrug CardHannahAinda não há avaliações
- Drug Card AmbienDocumento1 páginaDrug Card AmbienAdrianne Bazo100% (1)
- Drug StudyDocumento3 páginasDrug StudyKwin SaludaresAinda não há avaliações
- 16 ARDS - Nursing Care ManagementDocumento2 páginas16 ARDS - Nursing Care ManagementTisha CarretteAinda não há avaliações
- Ati Medication Template HydrocortisoneDocumento1 páginaAti Medication Template HydrocortisoneSharee HaywoodAinda não há avaliações
- STUDENT Sepsis Rapid ReasoningDocumento6 páginasSTUDENT Sepsis Rapid Reasoningghodghod123Ainda não há avaliações
- Special DietsDocumento52 páginasSpecial DietsMara Faye R. AvilesAinda não há avaliações
- Calcium AcetateDocumento3 páginasCalcium AcetateKIM NAMJOON'S PEACHES & CREAM100% (1)
- HypokalemiaDocumento3 páginasHypokalemiaSergeiAinda não há avaliações
- Augmenten (Amoxicillin Clavulan)Documento2 páginasAugmenten (Amoxicillin Clavulan)Adrianne BazoAinda não há avaliações
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideAinda não há avaliações
- Electrolytes Slide 21Documento111 páginasElectrolytes Slide 21Elaisha Mae C. CarsulaAinda não há avaliações
- Bowel Diversion: Parameter Colostomy IleostomyDocumento1 páginaBowel Diversion: Parameter Colostomy IleostomyMabesAinda não há avaliações
- Commonly Asked Emergency DrugsDocumento17 páginasCommonly Asked Emergency DrugsrianneAinda não há avaliações
- Pentagon CompilationDocumento20 páginasPentagon CompilationMabesAinda não há avaliações
- Triage PrinciplesDocumento2 páginasTriage PrinciplesMabesAinda não há avaliações
- Respiratory DiagnosticDocumento3 páginasRespiratory DiagnosticMabesAinda não há avaliações
- Route of ParenteralDocumento3 páginasRoute of ParenteralMabes100% (1)
- Enema Administration: Size of Rectal TubeDocumento3 páginasEnema Administration: Size of Rectal TubeMabesAinda não há avaliações
- Mabes Fluid and Electrolyte ImbalancesDocumento15 páginasMabes Fluid and Electrolyte ImbalancesMabesAinda não há avaliações
- Decubitus Ulcer / Pressure SoresDocumento1 páginaDecubitus Ulcer / Pressure SoresMabesAinda não há avaliações
- Bowel Elimination MabesDocumento2 páginasBowel Elimination MabesMabesAinda não há avaliações
- DocumentationDocumento3 páginasDocumentationMabesAinda não há avaliações
- All Nursing TheoriesDocumento26 páginasAll Nursing TheoriesMabesAinda não há avaliações
- Prof Ad JurisprudenceDocumento7 páginasProf Ad JurisprudenceMabesAinda não há avaliações
- Roses Are Red, Violets Are Blue, Without Your Lungs Your Blood Would Be, Too.Documento249 páginasRoses Are Red, Violets Are Blue, Without Your Lungs Your Blood Would Be, Too.MabesAinda não há avaliações
- Water Soluble VitaminsDocumento6 páginasWater Soluble VitaminsMabesAinda não há avaliações
- Lee Zu Ying Problem of The Spine 541-16-17Documento25 páginasLee Zu Ying Problem of The Spine 541-16-17Star CruiseAinda não há avaliações
- Epigastric Pain and Management of FeverDocumento41 páginasEpigastric Pain and Management of FeverAkhr RiAinda não há avaliações
- 1 Q PDFDocumento44 páginas1 Q PDFMysheb SSAinda não há avaliações
- Narrative ReportDocumento1 páginaNarrative ReportMelvin Aurelio100% (1)
- Salmonella Enterica: Trends in MicrobiologyDocumento2 páginasSalmonella Enterica: Trends in Microbiologyshaznay delacruzAinda não há avaliações
- CHN Lec FinalsDocumento14 páginasCHN Lec FinalsMay Chelle ErazoAinda não há avaliações
- CPG On Allergic Rhinitis 2Documento8 páginasCPG On Allergic Rhinitis 2mkct111Ainda não há avaliações
- Treatment of Bell's PalsyDocumento5 páginasTreatment of Bell's Palsymaryrose_jordanAinda não há avaliações
- Introduction To Low VisionDocumento15 páginasIntroduction To Low VisionHira AtifAinda não há avaliações
- Indice Diastolico de ChoqueDocumento11 páginasIndice Diastolico de ChoqueLUIS AYALAAinda não há avaliações
- Is Marijuana Good or BadDocumento3 páginasIs Marijuana Good or BadGenry TanAinda não há avaliações
- Trigger FingerDocumento2 páginasTrigger FingerTJPlayzAinda não há avaliações
- MCQ Cases Neoplasia 3rd YearDocumento9 páginasMCQ Cases Neoplasia 3rd YearG.KAinda não há avaliações
- Intravenous Pyelogram (IVP) PDFDocumento4 páginasIntravenous Pyelogram (IVP) PDFMarcelitaTaliaDuwiri100% (1)
- " Drop Foot": Arranged By: Nabiilah Aznesia NPM 71170891191Documento12 páginas" Drop Foot": Arranged By: Nabiilah Aznesia NPM 71170891191NaomiRimaClaudyaAinda não há avaliações
- Yellow Fever Vaccine:: What You Need To KnowDocumento2 páginasYellow Fever Vaccine:: What You Need To Knowamal aldhafeeriAinda não há avaliações
- Inserting IV Cannula LessonsDocumento3 páginasInserting IV Cannula LessonsAlkenedy KahalAinda não há avaliações
- Placenta Previa - Gynecology and Obstetrics - MSD Manual Professional EditionDocumento3 páginasPlacenta Previa - Gynecology and Obstetrics - MSD Manual Professional EditionAtinul KulsumAinda não há avaliações
- SHAHMEERDocumento29 páginasSHAHMEERMosa AbdullahAinda não há avaliações
- Mini-OSCE Internal PicturesDocumento108 páginasMini-OSCE Internal PicturesCheru TadesseAinda não há avaliações
- Drug Eruptions 2 Medical Students-1Documento24 páginasDrug Eruptions 2 Medical Students-1Abdelmouez AnwerAinda não há avaliações
- TB Child ExtrapulmonaryDocumento9 páginasTB Child Extrapulmonarygiant nitaAinda não há avaliações