Escolar Documentos
Profissional Documentos
Cultura Documentos
Salem Hospital Financial Performance Update (Nov. 13, 2012)
Enviado por
Statesman JournalTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Salem Hospital Financial Performance Update (Nov. 13, 2012)
Enviado por
Statesman JournalDireitos autorais:
Formatos disponíveis
To:
All employees, medical staff and volunteers From: Aaron Crane, Chief Finance and Strategy Officer Date: November 13, 2012 RE: Financial update: Better documentation, surgery scheduling boost revenue As discussed in prior communications, in February management developed a financial improvement plan in response to sharp volume declines experienced over the last year. Thirty- one projects have resulted in year-to-date savings of more than $8 million. Our last financial performance update discussed variation-in-care initiatives. This update highlights two major projects involving staff and providers from across our health system. In addition to improving how we do our work, these teams have successfully increased the amount we are reimbursed for the care we give by $321,000.
ICD-10 and clinical documentation
This project addresses two major steps we must take. First, we are not capturing all of our patients co-morbidities and second, our clinical documentation would not meet the upcoming ICD-10 standards which require much more specificity than the current ICD-9 version does. Coding for co-morbidities. Co-morbidities are other conditions a patient has in addition to the reason the patient is being seen. For example, a patient may be here for heart surgery but also has diabetes. For the coding needed for billing and reporting to be accurate, the documentation about the patient, including his or her co-morbidities, must be specific and complete. When done correctly, the codes will reflect the care we provided and how sick the patient actually was. Coding with ICD-10. ICD (International Classification of Diseases and Procedures) is used to classify diseases and other health problems, and plays a role in how much we are reimbursed for the care we provide. In the U.S., ICD also classifies inpatient procedures. We are required to implement ICD-10 on October 1, 2014. The transition from ICD-9 to ICD-10 will be complex, in large part because the new system has nine times the number of potential codes. Accurately and completely documenting, and then coding, all of our patients co-morbidities and procedures is vital to a successful transition to ICD-10 in less than two years. Connection to quality reporting. Ratings companies, such as Consumer Reports and HealthGrades, rely on hospital coding to develop their quality rankings. Organizations ranking low on these lists will often say there was a problem with the documentation. To the public, that just sounds like an excuse. We have two ways we can ensure we rank highly: make sure we are providing great care and make sure we are accurately and thoroughly documenting it, including all co-morbidities. The team. Seven teams of Salem Health professionals are working on this project: IS analysts, physicians, outpatient clinics, payer contracting, finance, health information management,
patient financial services, lab, imaging, cath lab, professional billing, and access services, just to name a few. Making changes. The team worked with a consultant to identify the gap between what we are doing and what we need to do, including identifying specific medical and surgical specialties needing help. We hired Dr. Claire Norton, a former hospitalist, as the Medical Director for Continuum of Care. Additionally, five Clinical Documentation Specialists have been hired and trained. We are also recruiting for a Coding CDI Knowledge Expert, which is a coding subject-matter expert. Dr. Norton and the CDSs help providers completely and accurately document patients co- morbidities during the hospital stay. Post-discharge, they work closely with the inpatient coders, who must review the documentation and apply coding rules and principles to the final assigned codes. Dr. Norton has been meeting with physicians to show them the opportunities and to help them set up templates in Epic to support them. Results. Our first results came in September. We had expected an increase in reimbursement to the tune of $50,000. We achieved $121,000! Projecting growth with this level of success suggests as much as $3 million in increased reimbursement over the next year. Just as important, we will be accurately documenting our patients conditions so their healthcare records reflect the severity of their illness and the complexity of their treatments and outcomes.
Surgery scheduling
The
surgery
scheduling
project
was
created
to
ensure
we
have
all
the
correct
information
relating
to
a
patients
case
prior
to
surgery.
Historically,
weve
gotten
most
information,
but
in
a
fragmented
manner
with
some
information
missing
or
inaccurate.
This
resulted
in
an
annual
net
revenue
loss
of
$1.1
million.
The
team.
This
cross-functional
team
includes
surgery
scheduling
and
administration,
pre- surgical
screening,
access
services
insurance
verification,
care
management,
Kaizen
promotion
office,
and
continuous
improvement.
Also
participating
are
the
office
management
staffs
for
Dr.
Maurice
Collada
and
Willamette
Urology.
The
work.
The
groups
first
test
of
change
includes
new
tools
and
workflow
for
receiving
and
processing
the
information
needed
to
schedule
a
surgery.
The
new
process
involves
several
quality
checks
and
ensures
the
accuracy
of
information
that
is
received.
Information
is
consistently
shared
with
all
of
the
teams
prior
to
surgery
and
the
number
of
contacts
to
our
patients
and
physician
partners
is
minimized.
The
team
also
created
tools
to
ensure
that
patients
are
appropriately
screened
for
care
management
concerns
and
ensuring
that
patients
do
not
have
medically
unnecessary
days
in
the
hospital.
Results. The biggest impact so far has been to bring together a team that was historically operating as individual silos. Each team was doing a great job individually, but opportunities were missed because they were not working together. Since they have begun to work together they have developed standard work and shared understanding of one anothers work. This collaboration has led to changes in our workflows regarding medical necessity denials and payer-required consent forms, resulting in a revenue increase of approximately $200,000 since May. Future work. The current test of change will run for about two months, with the team checking and adjusting the process as needed. Then the team will begin to partner with other physicians to create a plan for roll out to all physician offices by the end of September 2013. The work of these two teams has brought in an additional $321,000 so far. They also brought together individuals from many areas of Salem Health, including the medical staff. In the future, you may be called on to participate in groups like these. When you are asked, please jump in with both feet. These collaborations make things better for our patients and for one another; and they help improve our financial position, making us more successful now and in the new world of healthcare reform. Questions? Remember to submit questions under the Financial Challenges link in the new Tools and Resources module on the intranet, so they can be answered for everyone to see. If you are reading this email at work, you can follow this link to the financial Q&A page: http://home/news/fin.html
Você também pode gostar
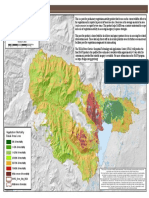
- Cedar Creek Vegitation Burn SeverityDocumento1 páginaCedar Creek Vegitation Burn SeverityStatesman JournalAinda não há avaliações
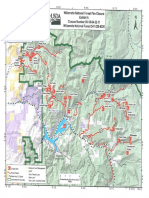
- Roads and Trails of Cascade HeadDocumento1 páginaRoads and Trails of Cascade HeadStatesman JournalAinda não há avaliações
- Letter To Judge Hernandez From Rural Oregon LawmakersDocumento4 páginasLetter To Judge Hernandez From Rural Oregon LawmakersStatesman JournalAinda não há avaliações
- Matthieu Lake Map and CampsitesDocumento1 páginaMatthieu Lake Map and CampsitesStatesman JournalAinda não há avaliações
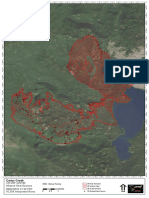
- Cedar Creek Fire Sept. 3Documento1 páginaCedar Creek Fire Sept. 3Statesman JournalAinda não há avaliações
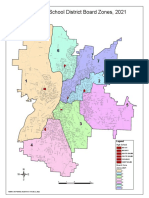
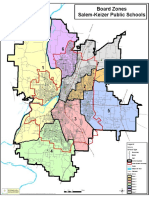
- School Board Zones Map 2021Documento1 páginaSchool Board Zones Map 2021Statesman JournalAinda não há avaliações
- Cedar Creek Fire Soil Burn SeverityDocumento1 páginaCedar Creek Fire Soil Burn SeverityStatesman JournalAinda não há avaliações
- Proclamation Parent & Guardian Engagement in Education 1-11-22 Final, SignedDocumento1 páginaProclamation Parent & Guardian Engagement in Education 1-11-22 Final, SignedStatesman JournalAinda não há avaliações
- Complaint Summary Memo To Superintendent Re 8-9 BD Meeting - CB 9-14-22Documento4 páginasComplaint Summary Memo To Superintendent Re 8-9 BD Meeting - CB 9-14-22Statesman JournalAinda não há avaliações
- LGBTQ Proclaimation 2022Documento1 páginaLGBTQ Proclaimation 2022Statesman JournalAinda não há avaliações
- Salem-Keizer Parent and Guardian Engagement in Education Month ProclamationDocumento1 páginaSalem-Keizer Parent and Guardian Engagement in Education Month ProclamationStatesman JournalAinda não há avaliações
- Revised Closure of The Beachie/Lionshead FiresDocumento4 páginasRevised Closure of The Beachie/Lionshead FiresStatesman JournalAinda não há avaliações
- Mount Hood National Forest Map of Closed and Open RoadsDocumento1 páginaMount Hood National Forest Map of Closed and Open RoadsStatesman JournalAinda não há avaliações
- Windigo Fire ClosureDocumento1 páginaWindigo Fire ClosureStatesman JournalAinda não há avaliações
- Resource List For Trauma Responses: Grounding Breathing Exercises To Take You Out of "Fight/Flight" ModeDocumento3 páginasResource List For Trauma Responses: Grounding Breathing Exercises To Take You Out of "Fight/Flight" ModeStatesman JournalAinda não há avaliações
- SIA Report 2022 - 21Documento10 páginasSIA Report 2022 - 21Statesman JournalAinda não há avaliações
- Crib Midget Day Care Emergency Order of SuspensionDocumento6 páginasCrib Midget Day Care Emergency Order of SuspensionStatesman JournalAinda não há avaliações
- Salem-Keizer Discipline Data Dec. 2021Documento13 páginasSalem-Keizer Discipline Data Dec. 2021Statesman JournalAinda não há avaliações
- Statement From Marion County Medical Examiner's Office On Heat-Related DeathsDocumento1 páginaStatement From Marion County Medical Examiner's Office On Heat-Related DeathsStatesman JournalAinda não há avaliações
- Oregon Annual Report Card 2020-21Documento71 páginasOregon Annual Report Card 2020-21Statesman JournalAinda não há avaliações
- Schools, Safe Learners (RSSL) Guidance. We Have Established A Statewide Rapid Testing ProgramDocumento3 páginasSchools, Safe Learners (RSSL) Guidance. We Have Established A Statewide Rapid Testing ProgramStatesman Journal100% (1)
- Gcab - Personal Electronic Devices and Social Media - StaffDocumento2 páginasGcab - Personal Electronic Devices and Social Media - StaffStatesman JournalAinda não há avaliações
- School Board Zone MapDocumento1 páginaSchool Board Zone MapStatesman JournalAinda não há avaliações
- Op Ed - Anthony MedinaDocumento2 páginasOp Ed - Anthony MedinaStatesman JournalAinda não há avaliações
- City of Salem Photo Red Light Program 2021 Legislative ReportDocumento8 páginasCity of Salem Photo Red Light Program 2021 Legislative ReportStatesman JournalAinda não há avaliações
- SB Agenda 20210415 EnglishDocumento1 páginaSB Agenda 20210415 EnglishStatesman JournalAinda não há avaliações
- 2021 Ironman 70.3 Oregon Traffic ImpactDocumento2 páginas2021 Ironman 70.3 Oregon Traffic ImpactStatesman JournalAinda não há avaliações
- Zone Resolution PDFDocumento2 páginasZone Resolution PDFStatesman JournalAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Plant Report Template Class 81Documento2 páginasPlant Report Template Class 81Kamran KhanAinda não há avaliações
- Inspection Report For Apartment Building at 1080 93rd St. in Bay Harbor IslandsDocumento13 páginasInspection Report For Apartment Building at 1080 93rd St. in Bay Harbor IslandsAmanda RojasAinda não há avaliações
- Advantages Renewable Energy Resources Environmental Sciences EssayDocumento3 páginasAdvantages Renewable Energy Resources Environmental Sciences EssayCemerlang StudiAinda não há avaliações
- Lab 2 - Permeability TestDocumento9 páginasLab 2 - Permeability TestAinur NasuhaAinda não há avaliações
- SAED90DR Rev1 2 21.01.2011Documento24 páginasSAED90DR Rev1 2 21.01.2011Cherry AbhiAinda não há avaliações
- Flowrox Valve Solutions Catalogue E-VersionDocumento16 páginasFlowrox Valve Solutions Catalogue E-Versionjavier alvarezAinda não há avaliações
- Malling DemallingDocumento25 páginasMalling DemallingVijay KumarAinda não há avaliações
- ATS2017 ProspectusDocumento13 páginasATS2017 ProspectusGiri WakshanAinda não há avaliações
- EmployWise JAVA ASSIGNMENTDocumento2 páginasEmployWise JAVA ASSIGNMENTPreet PatelAinda não há avaliações
- April 2021 BDA Case Study - GroupDocumento4 páginasApril 2021 BDA Case Study - GroupTinashe Chirume1Ainda não há avaliações
- Thermodynamic c106Documento120 páginasThermodynamic c106Драгослав БјелицаAinda não há avaliações
- Uts Cmo Module 5Documento31 páginasUts Cmo Module 5Ceelinah EsparazAinda não há avaliações
- Remedy MidTier Guide 7-5Documento170 páginasRemedy MidTier Guide 7-5martin_wiedmeyerAinda não há avaliações
- FHHR 013 Red Tag Procedure PDFDocumento5 páginasFHHR 013 Red Tag Procedure PDFN3N5YAinda não há avaliações
- SRS Document Battle Royale Origins - V2Documento36 páginasSRS Document Battle Royale Origins - V2Talha SajjadAinda não há avaliações
- Taxation Law 1Documento7 páginasTaxation Law 1jalefaye abapoAinda não há avaliações
- Design and Optimization of A Medium Altitude Long Endurance UAV Wingbox StructureDocumento8 páginasDesign and Optimization of A Medium Altitude Long Endurance UAV Wingbox StructureamirAinda não há avaliações
- STARCHETYPE REPORT ReLOADED AUGURDocumento5 páginasSTARCHETYPE REPORT ReLOADED AUGURBrittany-faye OyewumiAinda não há avaliações
- DLI Watchman®: Vibration Screening Tool BenefitsDocumento2 páginasDLI Watchman®: Vibration Screening Tool Benefitssinner86Ainda não há avaliações
- Assessing The Marks and Spencers Retail ChainDocumento10 páginasAssessing The Marks and Spencers Retail ChainHND Assignment Help100% (1)
- List of HTML TagsDocumento5 páginasList of HTML TagsdorinadidAinda não há avaliações
- Fear of God-3Documento50 páginasFear of God-3Duy LêAinda não há avaliações
- Angelo (Patrick) Complaint PDFDocumento2 páginasAngelo (Patrick) Complaint PDFPatLohmannAinda não há avaliações
- Course DescriptionDocumento54 páginasCourse DescriptionMesafint lisanuAinda não há avaliações
- Reference by John BatchelorDocumento1 páginaReference by John Batchelorapi-276994844Ainda não há avaliações
- VLT 6000 HVAC Introduction To HVAC: MG.60.C7.02 - VLT Is A Registered Danfoss TrademarkDocumento27 páginasVLT 6000 HVAC Introduction To HVAC: MG.60.C7.02 - VLT Is A Registered Danfoss TrademarkSamir SabicAinda não há avaliações
- ASHRAE Elearning Course List - Order FormDocumento4 páginasASHRAE Elearning Course List - Order Formsaquib715Ainda não há avaliações
- For ClosureDocumento18 páginasFor Closuremau_cajipeAinda não há avaliações
- Donnan Membrane EquilibriaDocumento37 páginasDonnan Membrane EquilibriamukeshAinda não há avaliações
- Agm 1602W-818Documento23 páginasAgm 1602W-818Daniel BauerAinda não há avaliações