Escolar Documentos
Profissional Documentos
Cultura Documentos
Impaired Physical Mobility
Enviado por
Hanya Bint PotawanDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Impaired Physical Mobility
Enviado por
Hanya Bint PotawanDireitos autorais:
Formatos disponíveis
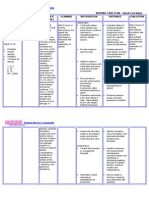
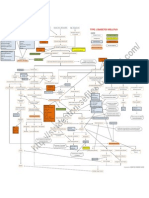
Nursing Diagnosis: Impaired physical Mobility May be related to: Neuromuscular involvement: weakness, paresthesia; flaccid, hypotonic paralysis
(initially); spastic paralysis, Perceptual or cognitive impairment Cause Analysis: A stroke is an upper motor neuron lesion and results in loss of voluntary control over motor movements. Because the upper motor neurons decussate (cross), a disturbance of voluntary motor control on one side of the body may reflect damage to the upper motor neurons on the opposite side of the brain. (Smeltzer et. al. [2010]. Brunner and Suddarths Medical Surgical Nursing, 12th edition, p.1897) Cues Objective Cues Inability to purposefully move within the physical environment Impaired coordination Limited range of motion (ROM), Decreased muscle strength and control Objectives Short-term Objective Within 8 hours of providing nursing interventions, the client will: Maintain or increase strength and function of affected or compensatory body part. Maintain optimal position of function as evidenced by absence of contractures and footdrop. Long-term Objective Within 3 days of providing nursing interventions, the client will: Demonstrate techniques and behaviors that enable resumption of activities. Maintain skin integrity. Independent Positioning Assess functional ability and extent of impairment initially and on a regular basis. Classify according to a 0 to 4 scale. (Refer to CP: Craniocerebral TraumaAcute Rehabilitative Phase, ND: impaired physical Mobility.) Change positions at least every 2 hours (supine, side lying) and possibly more often if placed on affected side. Nursing Interventions Rationale
Identifies strengths and deficiencies and may provide information regarding recovery. Assists in choice of interventions because different techniques are used for flaccid and spastic types of paralysis.
Reduces risk of tissue ischemia and injury. Affected side has poorer circulation and reduced sensation and is more predisposed to skin breakdown and pressure ulcers. Helps maintain functional hip extension; however, may increase anxiety, especially about ability to breathe.
Position in prone position once or twice a day if client can tolerate.
Prop extremities in functional position; use footboard during the period of flaccid paralysis. Maintain neutral position of head.
Prevents contractures and footdrop and facilitates use when or if function returns. Flaccid paralysis may interfere with ability to support head, whereas spastic paralysis may lead to deviation of head to one side. During flaccid paralysis, use of sling may reduce risk of shoulder subluxation and shoulder-hand syndrome.
Use arm sling when client is in upright position, as indicated.
Evaluate use of and need for positional aids and splints during spastic paralysis: Place pillow under axilla to abduct arm. Elevate arm and hand. Place hard hand-rolls in the palm with fingers and thumb opposed.
Flexion contractures occur because flexor muscles are stronger than extensors. Prevents adduction of shoulder and flexion of elbow. Promotes venous return and helps prevent edema formation. Hard cones decrease the stimulation of finger flexion, maintaining finger and thumb in a functional position. Maintains functional position. Prevents external hip rotation. Continued use after change from flaccid to spastic paralysis can cause excessive pressure on the ball of the foot, enhance spasticity, and actually increase plantar flexion. Edematous tissue is more easily traumatized and heals more slowly.
Place knee and hip in extended position. Maintain leg in neutral position with a trochanter roll. Discontinue use of footboard, when appropriate.
Observe affected side for color, edema, or other signs of compromised circulation. Inspect skin regularly, particularly over bony prominences.
Pressure points over bony prominences are most at risk for decreased perfusion and ischemia. Circulatory stimulation and padding help prevent skin breakdown and decubitus ulcer development.
Gently massage any reddened areas and provide aids such as sheepskin pads, as necessary.
Exercise Therapy: Muscle Control Begin active or passive ROM to all extremities (including splinted) on Minimizes muscle atrophy, promotes circulation, and helps prevent contractures.
admission. Encourage exercises, such as quadriceps or gluteal exercise, squeezing rubber ball, and extension of fingers and legs and feet.
Reduces risk of hypercalciuria and osteoporosis if underlying problem is hemorrhage. Note: Excessive and imprudent stimulation can predispose to recurrence of bleeding.
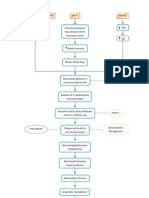
Assist client to develop sitting balance (such as raise head of bed; assist to sit on edge of bed, having client use the strong arm to support body weight and strong leg to move affected leg; increase sitting time) and standing balance put flat walking shoes on client, support clients lower back with hands while positioning own knees outside clients knees, and assist in using parallel bars and walker. Get client up in chair as soon as vital signs are stable except following cerebral hemorrhage.
Aids in retraining neuronal pathways, enhancing proprioception and motor response.
Helps stabilize BP, restoring vasomotor tone, and promotes maintenance of extremities in a functional position and emptying of bladder and kidneys, reducing risk of urinary stones and infections from stasis. Note: If stroke is not completed, activity increases risk of additional bleeding and infarction. Reduces pressure on the coccyx and prevents skin breakdown.
Pad chair seat with foam or water-filled cushion, and assist client to shift weight at frequent intervals. Set goals with client/significant other (SO) for increasing participation in activities, exercise, and position changes. Encourage client to assist with movement and exercises using unaffected extremity to support and move weaker side.
Promotes sense of expectation of progress and improvement, and provides some sense of control and independence. May respond as if affected side is no longer part of body and need encouragement and active training to reincorporate it as a part of own body.
Collaborative Positioning Provide egg-crate mattress, water bed, flotation device, or specialized bed, such as kinetic, as indicated. Promotes even weight distribution, decreasing pressure on bony points and helping to prevent skin breakdown and pressure ulcer formation. Specialized beds help with positioning, enhance circulation, and reduce venous stasis to decrease risk of tissue injury and complications such as orthostatic pneumonia. Individualized program can be developed to meet particular needs and deal with deficits in balance, coordination, and strength. May assist with muscle strengthening and increase voluntary muscle control, as well as pain control. May be required to relieve spasticity in affected extremities. Administer muscle relaxants and antispasmodics as indicated, such as baclofen (Lioresal) and dantrolene (Dantrium). References: Doenges et. al. (2008) Nursing Care Plans: Guidelines for Individualizing Client Care Across the Life Span, 8th edition, p244-245
Exercise Therapy: Muscle Control Consult with physical therapist regarding active, resistive exercises and client ambulation. Assist with electrical stimulationtranscutaneous electrical nerve stimulator (TENS) unit, as indicated.
Você também pode gostar
- Normal & Abnormal GaitDocumento29 páginasNormal & Abnormal GaitVidhya anand MAinda não há avaliações
- Christian Thibaudeau - Training The Three Types of ContractionsDocumento12 páginasChristian Thibaudeau - Training The Three Types of ContractionsPeter Walid100% (4)
- CVA Impaired Physical MobilityDocumento3 páginasCVA Impaired Physical MobilityJasmineAinda não há avaliações
- Lack of Knowledge On Diabetes Management or Blood Glucose ManagementDocumento2 páginasLack of Knowledge On Diabetes Management or Blood Glucose ManagementDanica Kate GalleonAinda não há avaliações
- Bobath Approach NotesDocumento5 páginasBobath Approach NotesJuling Perales100% (3)
- CHAPTER 10 Cerebral PalsyDocumento26 páginasCHAPTER 10 Cerebral PalsyMing MingAinda não há avaliações
- Nursing Care Plan for Patient with Impaired Physical MobilityDocumento4 páginasNursing Care Plan for Patient with Impaired Physical Mobilityssairej06100% (3)
- Handouts Parkinson DiseaseDocumento7 páginasHandouts Parkinson DiseaseSereneOneAinda não há avaliações
- PTH 725 - Multiple-Sclerosis-Case StudyDocumento19 páginasPTH 725 - Multiple-Sclerosis-Case StudyEnrique Guillen InfanteAinda não há avaliações
- Herbal MedicinesDocumento6 páginasHerbal MedicinesHanya Bint PotawanAinda não há avaliações
- Herbal MedicinesDocumento6 páginasHerbal MedicinesHanya Bint PotawanAinda não há avaliações
- 10.1007@978 3 319 74558 9Documento3.073 páginas10.1007@978 3 319 74558 9chindy layAinda não há avaliações
- Psychotropic DrugsDocumento49 páginasPsychotropic DrugsHanya Bint PotawanAinda não há avaliações
- Tues 10-20 Peripheral Nerve Disorders - A Practical OverviewDocumento36 páginasTues 10-20 Peripheral Nerve Disorders - A Practical OverviewGery FirmansyahAinda não há avaliações
- Assessment, diagnosis, planning, intervention, and evaluation for Parkinson's patientDocumento2 páginasAssessment, diagnosis, planning, intervention, and evaluation for Parkinson's patientBenjie DimayacyacAinda não há avaliações
- Muscle Re-Education by Venkata RamaiahDocumento8 páginasMuscle Re-Education by Venkata Ramaiahvenkata ramakrishnaiahAinda não há avaliações
- Hip Displacement in Cerebral PalsyDocumento9 páginasHip Displacement in Cerebral PalsyJohannesSchoppmannAinda não há avaliações
- Mobility Nursing Diagnosis GuideDocumento3 páginasMobility Nursing Diagnosis GuideYan ReyesAinda não há avaliações
- Assessment and Treatment of Spasticity: Cori Ponter, PT, MPT, NCS Barrow Neurological Institute 3/23/19Documento76 páginasAssessment and Treatment of Spasticity: Cori Ponter, PT, MPT, NCS Barrow Neurological Institute 3/23/19Praneetha100% (2)
- Neurology Approach For MRCPDocumento150 páginasNeurology Approach For MRCPdavidc198673% (11)
- Schizophrenia UndifferentiatedDocumento88 páginasSchizophrenia UndifferentiatedHanya Bint Potawan75% (4)
- Valdez Reflective-Questions PDFDocumento3 páginasValdez Reflective-Questions PDFDexel Lorren ValdezAinda não há avaliações
- Multiple SclerosisDocumento35 páginasMultiple SclerosisJc SeguiAinda não há avaliações
- Impaired Gas ExchangeDocumento2 páginasImpaired Gas ExchangeHanya Bint PotawanAinda não há avaliações
- CP DVTDocumento3 páginasCP DVTBrian O'NeillAinda não há avaliações
- Ischemic Stroke NCPDocumento11 páginasIschemic Stroke NCPJohannah DaroAinda não há avaliações
- Impaired Skin IntegrityDocumento1 páginaImpaired Skin IntegrityHanya Bint PotawanAinda não há avaliações
- Ineffective Cerebral Tissue PerfusionDocumento3 páginasIneffective Cerebral Tissue PerfusionHanya Bint Potawan88% (25)
- Ineffective Airway ClearanceDocumento2 páginasIneffective Airway ClearanceHanya Bint PotawanAinda não há avaliações
- SP CSDocumento4 páginasSP CSKhan HansAinda não há avaliações
- Nursing Priorities: 8 Fracture Nursing Care Plan (NCP)Documento10 páginasNursing Priorities: 8 Fracture Nursing Care Plan (NCP)PagodAinda não há avaliações
- Fistula NCPDocumento1 páginaFistula NCPHasna LisnaAinda não há avaliações
- BSN - 4C: PresentorsDocumento52 páginasBSN - 4C: PresentorsHanya Bint Potawan100% (1)
- Nursing Care Plans For Activity IntoleranceDocumento4 páginasNursing Care Plans For Activity IntolerancethebigtwirpAinda não há avaliações
- NCP For StokeDocumento5 páginasNCP For StokeMemedAinda não há avaliações
- Nursing Care Plan for Spinal Cord InjuryDocumento3 páginasNursing Care Plan for Spinal Cord InjuryDan Leo UnicoAinda não há avaliações
- NCP PainDocumento1 páginaNCP Painsitz04Ainda não há avaliações
- Managing Fatigue Through Activity Pacing and RestDocumento2 páginasManaging Fatigue Through Activity Pacing and ResthaniehaehaeAinda não há avaliações
- FractureDocumento1 páginaFractureReechie TeasoonAinda não há avaliações
- Constipation NCPDocumento2 páginasConstipation NCPKaren Pili100% (1)
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocumento4 páginasAssessment Diagnosis Planning Intervention Rationale EvaluationJhoizel VenusAinda não há avaliações
- 5ncp AnemiaDocumento8 páginas5ncp Anemiabeverly_domingoAinda não há avaliações
- Cues Objectives Interventions Rationale Evaluation: Nursing Care PlanDocumento1 páginaCues Objectives Interventions Rationale Evaluation: Nursing Care Planaprilrosehibaya100% (1)
- Bowel incontinence diagnosis and interventionsDocumento9 páginasBowel incontinence diagnosis and interventionsners_gun100% (1)
- Post-Appendectomy Care AssessmentDocumento9 páginasPost-Appendectomy Care AssessmentChristina Espiña EjercitoAinda não há avaliações
- NCP Self Care DeficitDocumento3 páginasNCP Self Care DeficitLeizel ApolonioAinda não há avaliações
- Case Study RespiDocumento3 páginasCase Study RespiMark Jheran AlvarezAinda não há avaliações
- NCP Sicu!Documento6 páginasNCP Sicu!joanne190Ainda não há avaliações
- Nursing Care Plan PrioritizationDocumento1 páginaNursing Care Plan PrioritizationKASIA SyAinda não há avaliações
- Burns - Skin Integrity, ImpairedDocumento2 páginasBurns - Skin Integrity, Impairedmakyofrancis20Ainda não há avaliações
- Impaired Physical MobilityDocumento2 páginasImpaired Physical MobilityAbdelhafiz SusmiranAinda não há avaliações
- NCP Total Hip ReplacementDocumento11 páginasNCP Total Hip ReplacementDoneva Lyn MedinaAinda não há avaliações
- Ineffective Breathing PatternDocumento185 páginasIneffective Breathing PatternSusi LambiyantiAinda não há avaliações
- Ineffective Tissue PerfusionDocumento5 páginasIneffective Tissue PerfusionKryza Dale Bunado BaticanAinda não há avaliações
- NCPDocumento2 páginasNCPjoyce_albertoAinda não há avaliações
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationDocumento1 páginaNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyAinda não há avaliações
- NCP Self CaRE DeficitDocumento1 páginaNCP Self CaRE Deficitnicole pageAinda não há avaliações
- Examples of Therapeutic and Non Therapeutic Communication TechniquesDocumento6 páginasExamples of Therapeutic and Non Therapeutic Communication TechniquesReya Mae OrcajadaAinda não há avaliações
- Impaired Physical Mobility...Documento3 páginasImpaired Physical Mobility...Christy BerryAinda não há avaliações
- NCPDocumento6 páginasNCPNik Rose ElAinda não há avaliações
- Healthcare - Nursing Care Plan - Excess Fluid VolumeDocumento4 páginasHealthcare - Nursing Care Plan - Excess Fluid VolumeBenjamin CañalitaAinda não há avaliações
- Child - Major Burn PDFDocumento3 páginasChild - Major Burn PDFAldith GrahamAinda não há avaliações
- Potts DiseaseDocumento8 páginasPotts Diseaseaimeeros0% (2)
- LortabDocumento1 páginaLortabSheri490Ainda não há avaliações
- Nursing Care Plan: Risk For Disuse SyndromeDocumento2 páginasNursing Care Plan: Risk For Disuse SyndromeRozsy FakhrurAinda não há avaliações
- NursingCribcom Nursing Care Plan KyphosisDocumento2 páginasNursingCribcom Nursing Care Plan KyphosisKrissa Pearl CalleraAinda não há avaliações
- Nursing Care Plan: Determine Cause of Activity - Determining The Cause of A Disease CanDocumento2 páginasNursing Care Plan: Determine Cause of Activity - Determining The Cause of A Disease Canrix07Ainda não há avaliações
- WHOQOL 100 InglesDocumento30 páginasWHOQOL 100 Inglescristhianibo777Ainda não há avaliações
- Complications of Plaster Cast PATIENT LEAFLETDocumento6 páginasComplications of Plaster Cast PATIENT LEAFLETRadiyan MeidhiyantoAinda não há avaliações
- Problem Nursing Diagnosis Outcome Plan Intervention Evaluation Subjective Data: "Masakit Po Yung Sa Short Term: IndependentDocumento2 páginasProblem Nursing Diagnosis Outcome Plan Intervention Evaluation Subjective Data: "Masakit Po Yung Sa Short Term: IndependentkyawAinda não há avaliações
- Nursing Care PlanDocumento4 páginasNursing Care PlanDewi PurnamasariAinda não há avaliações
- Renal Failure NCPDocumento3 páginasRenal Failure NCPjsksAinda não há avaliações
- Urinary Incontinence Guide for Care and ManagementDocumento5 páginasUrinary Incontinence Guide for Care and ManagementfakrulnersmudaAinda não há avaliações
- NCPDocumento10 páginasNCPNefre Dayap DarrocaAinda não há avaliações
- Impaired Tissue Integrity - CellulitisDocumento3 páginasImpaired Tissue Integrity - CellulitisKelvin Kurt B. AgwilangAinda não há avaliações
- NCP Knowledge Deficit PDFDocumento2 páginasNCP Knowledge Deficit PDFskylertAinda não há avaliações
- Nursing Diagnosis: Urinary Retention: NOC Outcomes (Nursing Outcomes Classification)Documento4 páginasNursing Diagnosis: Urinary Retention: NOC Outcomes (Nursing Outcomes Classification)rem_Ainda não há avaliações
- Small Bowel Obstruction Concept MapDocumento1 páginaSmall Bowel Obstruction Concept MapTessa Claire JaranowskiAinda não há avaliações
- ImmobilityDocumento1 páginaImmobilitymicopoliAinda não há avaliações
- Nursing Care Plan for Improving HygieneDocumento2 páginasNursing Care Plan for Improving HygieneMartin Lєtmaku EspinaAinda não há avaliações
- Impaired Physical MobilityDocumento3 páginasImpaired Physical MobilityCalimlim Kim100% (1)
- Fracture Canada BasedDocumento26 páginasFracture Canada BasedVane UcatAinda não há avaliações
- Impaired Verbal and or Written CommunicationDocumento2 páginasImpaired Verbal and or Written CommunicationHanya Bint Potawan100% (1)
- Rhu Day 1 RequirementsDocumento4 páginasRhu Day 1 RequirementsHanya Bint PotawanAinda não há avaliações
- Rhu Day 1 RequirementsDocumento4 páginasRhu Day 1 RequirementsHanya Bint PotawanAinda não há avaliações
- Rhu Day 1 RequirementsDocumento4 páginasRhu Day 1 RequirementsHanya Bint PotawanAinda não há avaliações
- Impaired Breathing PatternDocumento1 páginaImpaired Breathing PatternHanya Bint PotawanAinda não há avaliações
- MSHC Ordr PRC FormatDocumento4 páginasMSHC Ordr PRC FormatHanya Bint PotawanAinda não há avaliações
- Hanieyah Guro OR DR PRC FormatDocumento4 páginasHanieyah Guro OR DR PRC FormatHanya Bint PotawanAinda não há avaliações
- Pa Tho Physiology - Type 1 Diabetes (Hanieyah Guro)Documento1 páginaPa Tho Physiology - Type 1 Diabetes (Hanieyah Guro)Hanya Bint PotawanAinda não há avaliações
- Jose Rizal: 'Those Who Cannot See Where They Came From Will Never Get To Where They Are Going.'Documento55 páginasJose Rizal: 'Those Who Cannot See Where They Came From Will Never Get To Where They Are Going.'Anne Ginez BilledoAinda não há avaliações
- Akiya - DiphtheriaDocumento52 páginasAkiya - DiphtheriaHanya Bint PotawanAinda não há avaliações
- DOH Officials Directory Execom MembersDocumento2 páginasDOH Officials Directory Execom MembersHanya Bint PotawanAinda não há avaliações
- Angina PectorisDocumento2 páginasAngina PectorisHanya Bint PotawanAinda não há avaliações
- Dopamine HydrochlorideDocumento1 páginaDopamine HydrochlorideJoannes SanchezAinda não há avaliações
- Mr. Bean's diagnostic blood test resultsDocumento2 páginasMr. Bean's diagnostic blood test resultsHanya Bint PotawanAinda não há avaliações
- SCI Assessment: 5 Key ComponentsDocumento24 páginasSCI Assessment: 5 Key ComponentsArslan AslamAinda não há avaliações
- Mojap 05 00232Documento9 páginasMojap 05 00232Fasha Since AndampuryAinda não há avaliações
- Impact of Cerebral Palsy Outline: A Research Review: Sharath Hullumani VDocumento5 páginasImpact of Cerebral Palsy Outline: A Research Review: Sharath Hullumani VSharath Hullumani VAinda não há avaliações
- Classification of Cerebral PalsyDocumento15 páginasClassification of Cerebral PalsypraveenAinda não há avaliações
- Cerebral Palsy Procedure Reduces SpasticityDocumento7 páginasCerebral Palsy Procedure Reduces SpasticityAlvaro Perez HenriquezAinda não há avaliações
- Intracerebral Hemorrhage TitleDocumento25 páginasIntracerebral Hemorrhage TitleJane StarkAinda não há avaliações
- Bobath ApproachesDocumento27 páginasBobath Approachesali imranAinda não há avaliações
- Bounders-How To ChooseDocumento1 páginaBounders-How To ChooseSummit GautamAinda não há avaliações
- 13 DeLisa - 039 - sESPASTICIDAD-1343-1361Documento19 páginas13 DeLisa - 039 - sESPASTICIDAD-1343-1361Alexandra SotoAinda não há avaliações
- 03 Rehabilitation 67-110Documento44 páginas03 Rehabilitation 67-110Ongky SajaAinda não há avaliações
- Paramedical Dissertations 2018, 2019 BatchDocumento69 páginasParamedical Dissertations 2018, 2019 Batchsana naazAinda não há avaliações
- Cerebral Palsy: An Overview of Epidemiology, Pathophysiology and InterventionsDocumento12 páginasCerebral Palsy: An Overview of Epidemiology, Pathophysiology and InterventionsMATERIAL24Ainda não há avaliações
- Review of Common Pathologies Requiring Ankle-Foot OrthosesDocumento32 páginasReview of Common Pathologies Requiring Ankle-Foot OrthosesnovitaAinda não há avaliações
- Lab Report 2Documento8 páginasLab Report 2api-350081950Ainda não há avaliações
- EPOS E-Learning Advanced Course: Treatment Principles in Cerebral PalsyDocumento2 páginasEPOS E-Learning Advanced Course: Treatment Principles in Cerebral PalsyCasa MironeAinda não há avaliações
- Gait Analysis GuideDocumento66 páginasGait Analysis GuidesenoAinda não há avaliações
- Effectiveness of Serial Casting in Patients With Severe Cerebral Spasticity: A Comparison StudyDocumento7 páginasEffectiveness of Serial Casting in Patients With Severe Cerebral Spasticity: A Comparison StudyDaniel MarvasoAinda não há avaliações