Escolar Documentos
Profissional Documentos
Cultura Documentos
Anestesia
Enviado por
ocoxodoTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Anestesia
Enviado por
ocoxodoDireitos autorais:
Formatos disponíveis
British Journal of Anaesthesia 100 (1): 7881 (2008)
doi:10.1093/bja/aem306
Advance Access publication October 24, 2007
OBSTETRICS Transcutaneous electrical nerve stimulation at the PC-5 and PC-6 acupoints reduced the severity of hypotension after spinal anaesthesia in patients undergoing Caesarean section
Y. C. P. Arai1*, N. Kato2, M. Matsura2, H. Ito2, N. Kandatsu2, S. Kurokawa2, M. Mizutani2, Y. Shibata2 and T. Komatsu2
1
Multidisciplinary Pain Centre and 2Department of Anaesthesiology, Aichi Medical University School of Medicine, 21 Karimata, Nagakutecho, Aichigun, Aichi 480-1195, Japan
*Corresponding author. E-mail: arainon@aichi-med-u.ac.jp
Background. Despite prophylactic measures, hypotension remains a common side-effect of spinal anaesthesia for parturients. Electroacupuncture at the Neiguan (PC-6) and Jianshi (PC-5) points inuences haemodynamics. We thus hypothesized that transcutaneous electrical nerve stimulation (TENS) at traditionally used acupuncture points would reduce the severity of hypotension after spinal anaesthesia in patients undergoing Caesarean section. Methods. After obtaining approval from the local ethics committee and written informed patient consent, 36 singleton parturients undergoing Caesarean section under spinal anaesthesia were randomized into three groups. The control group received no treatment, and the acupoint and non-acupoint groups received TENS at the PC-5 and PC-6 points of both arms and non-acupoints of both shoulders, respectively. Results. The median (range) of the lowest recorded systolic blood pressure was signicantly higher in the acupoint group compared with the other groups and that of the non-acupoint group was higher than that of the control group [control, 70 (68 82) mm Hg; acupoint, 94 (84 109) mm Hg; non-acupoint, 81 (70 92) mm Hg: P,0.001]. Signicantly more parturients in the control and non-acupoint groups experienced hypotension [control, 10 (83%); acupoint, 4 (33%); non-acupoint, 10 (83%): P0.013]. More ephedrine was required to maintain arterial blood pressure in the control and non-acupoint groups. Conclusions. TENS on the traditional acupuncture points reduced the severity and incidence of hypotension after spinal anaesthesia in parturients. Br J Anaesth 2008; 100: 7881 Keywords: acupuncture; anaesthesia, obstetric; anaesthetic techniques, subarachnoid; complications, hypotension; surgery, LSCS; TENS Accepted for publication: August 17, 2007
Downloaded from http://bja.oxfordjournals.org/ by guest on February 11, 2012
Hypotension after spinal anaesthesia for Caesarean section occurs commonly.1 3 Prophylactic measures include uid preload, lateral tilt, and the use of vasopressors.1 3 4 Despite these prophylactic measures, hypotension has an incidence of up to 3060% after spinal anaesthesia for parturients.1 6 Chinese acupuncture-based techniques have been used for perioperative management of anxiety,7 postoperative nausea and vomiting,8 and postoperative analgesia.9 In animal studies, electroacupuncture at the Neiguan (PC-6) and Jianshi (PC-5) points inuences vascular pressure responses and the cardiovascular sympathetic system,10 11
and especially electroacupuncture at the PC-6 point increases cardiovascular variables such as stroke volume and cardiac output and alleviates haemorrhagic hypotension.12 13 We hypothesized that transcutaneous electrical nerve stimulation (TENS) at traditionally used acupuncture points would reduce the severity of hypotension after spinal anaesthesia in patients undergoing Caesarean section. Thus, the purpose of the present preliminary study was to test the effect of TENS at the PC-6 and PC-5 points on haemodynamics after spinal anaesthesia in patients undergoing Caesarean section.
# The Board of Management and Trustees of the British Journal of Anaesthesia 2007. All rights reserved. For Permissions, please e-mail: journals.permissions@oxfordjournals.org
TENS for spinal hypotension
Methods
After obtaining approval from the local ethics committee and written informed patient consent, 36 ASA I multigravida parturients carrying a singleton pregnancy at fullterm gestation (38 39 weeks) and presenting for elective Caesarean section were enrolled in this randomized study. Parturients suffering from preeclampsia, hypertension, diabetes, or obesity (BMI.30 kg m22) were excluded. Patients were randomized to three groups, using computer-generated sealed envelopes. The control group received no treatment, the acupoint group received TENS bilaterally at the PC-5 and PC-6 points (on the palmar side of both arms, between the tendon of the long palmar muscle and radial exor muscle of the wrist)14 (Fig. 1) using a TENS stimulator (NeuroTraxTM TENS & AcuStim; Verity Medical Ltd, Hampshire, UK), and the non-acupoint group received TENS at non-acupoints of both shoulders8 (Fig. 1) using the TENS stimulator. All parturients fasted for a minimum of 6 h before operation. On arrival in the operation room, all parturients had standard monitoring in place (non-invasive blood pressure, ECG, and pulse oximetry) and 5 min later, the baseline values were recorded in the supine position. In the acupoint and non-acupoint groups, small-sized (1.5 cm) cutaneous electrode pads were placed bilaterally at the PC-6 and PC-5 points and non-acupoints of the shoulders, respectively. The intensity of the electrical stimulation was adjusted to produce the most intense tolerable electrical sensation without muscle contractions or uncomfortable feelings at a frequency of 50 Hz. The electrical stimulation was administered until delivery. Large-bore i.v. access was secured and acetated Ringers solution (10 ml kg21) was administered before the induction of anaesthesia. With the parturients in the right lateral position, a 20-gauge epidural catheter was placed after identication of the epidural space at the L1 L2 interspace using a 17-gauge Tuohy needle. Then, dural puncture was performed at the L3 L4
interspace using a median approach and a 25-gauge Quincke needle. After free ow of cerebrospinal uid had been obtained, 2.4 ml of isobaric bupivacaine 0.5% and 0.4 ml of fentanyl (20 mg) was injected intrathecally over approximately 15 s. Then, the parturients were positioned supine. Oxygen at 2 3 litre min21 was delivered via a face mask. The sensory block level was assessed by pinprick at the left mid-clavicular line every 2 min. Surgery was allowed to start when at least the T6 dermatome was blocked. The extent of sensory block obtained at incision was considered to be the maximal blocked level, as further follow-up might be inappropriate once surgery started. In the case of insufcient cephalad spread of anaesthesia, incremental epidural supplements of lidocaine 1% were injected, starting with 5 ml. When necessary, additional 3 ml boluses were given no earlier than 5 min after the preceding top-up. Haemodynamics were recorded every minute until delivery. Ephedrine i.v. in increments of 4 mg was given every 2 min to treat hypotension, dened in the present study as a decrease in systolic blood pressure (SBP) 30% below baseline values or to ,90 mm Hg. SBP, diastolic blood pressure (DBP), and heart rate (HR) were recorded every minute until delivery. The parturient and provider were not blinded; however, the individual collecting data were blinded to group allocation. A pilot study using 15 patients showed the mean (SD) of the lowest SBP to be 74 (9), 99 (13), and 83 (8) in the control, acupoint, and non-acupoint groups, respectively. Thus, a group size of at least 10 patients was needed to show a difference of 15 (SD 10) mm Hg in the lowest SBP with a signicant level of 0.05 (a0.05) and a power of 80% (b0.20). Data are expressed as median (range). Statistical analysis was performed using the Kruskal Wallis test followed by Student Newman Keuls method for multiple comparisons. P,0.05 was considered to be signicant.
Downloaded from http://bja.oxfordjournals.org/ by guest on February 11, 2012
Results
Patient characteristics, baseline measurements to delivery interval, and maximal block height were comparable among the three groups (Table 1). Baseline SBP, DBP, and HR were similar among these groups (Table 2). The intensity of TENS was the same between the acupoint and the non-acupoint groups. The number and amount of epidural supplementation were similar among the three groups. The lowest recorded SBP and DBP were signicantly higher in the acupoint group compared with the other groups and the SBP of the non-acupoint group was higher than that of the control group (Table 2). Signicantly more parturients in the control and non-acupoint groups experienced hypotension. The HR after spinal anaesthesia was not different among these groups. More ephedrine was
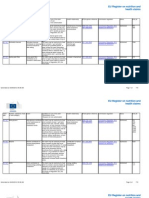
Fig 1 The locations of small-sized cutaneous electrode pads for TENS.
79
Arai et al.
Table 1 Patient characteristics and anaesthetic data of parturients undergoing Caesarean section. Data are mean (range), mean (SD) or number (percentage). Base del interval, baseline measurements to delivery interval Control (n512) Age (yr) Height (cm) Weight (kg) Maximal block height (dermatome) Epidural supplementation (n) Amount of epidural lidocaine 1% (ml) Base del interval (min) 33 (31 35) 158 (5) 61 (6) T5 (T3 T6) 3 (25%) 0 (0 2.5) 43 (35 49) Acupoint (n512) 31 (29 35) 161 (3) 59 (6) T5 (T4 T6) 3 (25%) 0 (0 2.5) 39 (37 50) Non-acupoint (n512) 29 (26 32) 158 (7) 64 (9) T5 (T4 T6) 3 (25%) 0 (0 2.5) 40 (30 50) P-value 0.114 0.441 0.448 0.763 1.00 1.00 0.893
Table 2 Haemodynamic variables of parturients undergoing Caesarean section. Data are median (range) or number (percentage). SBP, systolic blood pressure; DBP, diastolic blood pressure. *Using Mann Whitney test. Signicantly different from the other groups. }Signicantly different from the control group Control (n512) Acupoint (n512) Non-acupoint (n512) P-value
Intensity of 12 (9 15) 13 (9 18) 0.237* TENS (mA) Baseline SBP 119 (115 127) 126 (113 135) 118 (110 123) 0.355 (mm Hg) Lowest SBP 70 (68 82) 94 (84 109) 81 (70 92)} ,0.001 (mm Hg) Baseline DBP 60 (50 76) 66 (58 88) 62 (46 86) 0.069 (mm Hg) 36 (26 44) ,0.001 Lowest DBP 27 (20 50) 44 (30 68) (mm Hg) 76 (65 92) 82 (64 120) 83 (70 105) 0.154 Baseline HR (beats min21) HR at lowest 68 (48 110) 81 (64 110) 84 (60 120) ,0.05 SBP (beats 21 min ) 10 (83%) 0.013 Incidence of 10 (83%) 4 (33%) hypotension (n) Ephedrine (mg) 8 (8 16) 0 (0 12) 14 (8 18) 0.025
required to maintain arterial blood pressure in the control and non-acupoint groups compared with the acupoint group (Table 2).
Discussion
The present study showed that TENS itself reduced the severity of hypotension of parturients after spinal anaesthesia, and that TENS at specic acupoints further reduced the severity and incidence of hypotension. Electroacupuncture at an acupuncture point is known to inuence haemodynamics and cardiovascular sympathoexcitatory responses.14 16 Electroacupuncture at the PC-6 point is known to increase stroke volume and cardiac output, and alleviate haemorrhagic hypotension.12 13 In the present study, TENS was delivered at the most intense tolerable electrical sensation, and it would not be surprising if TENS itself had some sympathomimetic effect,17 as shown in the non-acupoint group. When giving the same level of electrical stimulation, however, TENS at the specic acupoints signicantly reduced the severity of
hypotension compared with TENS at the non-specic points. An electrical stimulation of somatic afferents from muscle at 40 Hz causes a pressor response.18 Electroacupuncture at the PC-6 point also augments sympathetic tone and improves the inhibited cardiovascular function.12 13 We thus postulate that TENS applied on the PC-6 and PC-5 points might have augmented sympathetic tone, thereby increasing cardiac function and vascular tone and alleviating hypotension after spinal anaesthesia in parturients undergoing Caesarean section. A limitation in the present study is the failure to clarify the optimal frequency of electrical stimulation of TENS. In fact, some studies showed that electoacupuncture at 2 4 Hz can inhibit cardiovascular sympathoexcitatory responses.10 11 In contrast, electroacupuncture stimulation frequency to 5 Hz did not lead to any effect on the cardiovascular system and increasing the frequency to 30 70 Hz induced recognizable pressor responses.12 13 Thus, we chose the frequency of 50 Hz in the present study. However, we need further studies in order to nd the optimal frequency of TENS. Another limitation is that the incidence of epidural supplementation was relatively high in each group in the present study (25%). We speculated that the spinal dose of bupivacaine would have been insufcient for the spinal anaesthesia of Caesarean section in the present study. We also consider that the use of isobaric bupivacaine might have led to the present results and that repeating spinal anaesthesia with hyperbaric bupivacaine would decrease the need for epidural supplementation and alter the results. In conclusion, TENS on the traditional acupuncture points reduced the severity and incidence of hypotension after spinal anaesthesia in parturients.
Downloaded from http://bja.oxfordjournals.org/ by guest on February 11, 2012
References
1 Saravanan S, Kocarev M, Wilson RC, Watkins E, Columb MO, Lyons G. Equivalent dose of ephedrine and phenylephrine in the prevention of post-spinal hypotension in Caesarean section. Br J Anaesth 2006; 96: 95 9 2 Hall PA, Bennett A, Wilkes MP, Lewis M. Spinal anaesthesia for Caesarean section: comparison of infusions of phenylephrine and ephedrine. Br J Anaesth 1994; 73: 471 4 3 Kang YG, Abouleish E, Caritis S. Prophylactic intravenous ephedrine infusion during spinal anesthesia for cesarean section. Anesth Analg 1982; 61: 839 42
80
TENS for spinal hypotension
4 Morgan P. The role of vasopressors in the management of hypotension induced by spinal and epidural anaesthesia. Can J Anaesth 1994; 41: 404 13 5 Dahlgren G, Granath F, Pregner K, Rosblad PG, Wessel H, Irestedt L. Colloid vs. crystalloid preloading to prevent maternal hypotension during spinal anaesthesia for elective cesarean section. Acta Anaesthesiol Scand 2005; 49: 1200 6 6 Kee WD, Khaw KS, Lee BB, Lau TK, Gin T. A dose response study of prophylactic intravenous ephedrine for the prevention of hypotension during spinal anesthesia for cesarean delivery. Anesth Analg 2000; 90: 1390 5 7 Agarwal A, Ranjan R, Dhiraaj S, Lakra A, Kumar M, Singh U. Acupressure for prevention of pre-operative anxiety: a prospective, randomised, placebo controlled study. Anaesthesia 2005; 60: 978 81 8 Zarate E, Mingus M, White PF, et al. The use of transcutaneous acupoint electrical stimulation for preventing nausea and vomiting after laparoscopic surgery. Anesth Analg 2001; 92: 629 35 9 Chen L, Tang J, White PF, et al. The effect of location of transcutaneous electrical nerve stimulation on postoperative opioid analgesic requirement: acupoint versus nonacupoint stimulation. Anesth Analg 1998; 87: 1129 34 10 Tjen-A-Looi SC, Li P, Longhurst JC. Midbrain vlPAG inhibits rVLM cardiovascular sympathoexcitatory responses during electroacupuncture. Am J Physiol Heart Circ Physiol 2006; 290: H2543 53
11 Li P, Tjen-A-Looi SC, Longhurst JC. Excitatory projections from arcuate nucleus to ventrolateral periaqueductal gray in electroacupuncture inhibition of cardiovascular reexes. Am J Physiol Heart Circ Physiol 2006; 290: H2535 42 12 Syuu Y, Matsubara H, Kiyooka T, et al. Cardiovascular benecial effects of electroacupuncture at Neiguan (PC-6) acupoint in anesthetized open-chest dog. Jpn J Physiol 2001; 51: 231 8 13 Syuu Y, Matsubara H, Hosogi S, Suga H. Pressor effect of electroacupuncture on hemorrhagic hypotension. Am J Physiol Regul Integr Comp Physiol 2003; 285: R1446 52 14 Li P, Ayannusi O, Reid C, Longhurst JC. Inhibitory effect of electroacupuncture (EA) on the pressor response induced by exercise stress. Clin Auton Res 2004; 14: 182 8 15 Haker E, Egekvist H, Bjerring P. Effect of sensory stimulation (acupuncture) on sympathetic and parasympathetic activities in healthy subjects. J Auton Nerv Syst 2000; 79: 52 9 16 Li Z, Wang C, Mak AF, Chow DH. Effects of acupuncture on heart rate variability in normal subjects under fatigue and nonfatigue state. Eur J Appl Physiol 2005; 94: 633 40 17 Buonocore M, Mortara A, La Rovere MT, Casale R. Cardiovascular effects of TENS: heart rate variability and plethysmographic wave evaluation in a group of normal subjects. Funct Neurol 1992; 7: 391 4 18 Clement DL, Pelletier CL, Shepherd JT. Role of muscular contraction in the reex vascular responses to stimulation of muscle afferents in the dog. Circ Res 1973; 33: 386 92
Downloaded from http://bja.oxfordjournals.org/ by guest on February 11, 2012
81
Você também pode gostar
- Tens Po Toracolomia - SEZENDocumento5 páginasTens Po Toracolomia - SEZENKamylla Caroline SantosAinda não há avaliações
- 1 s2.0 S0007091217366175 MainDocumento5 páginas1 s2.0 S0007091217366175 MainMeutia LaksaniAinda não há avaliações
- Annex 8a Translation Le Tohic-Venous Insufficiency 2008 (Pasien Hamil)Documento7 páginasAnnex 8a Translation Le Tohic-Venous Insufficiency 2008 (Pasien Hamil)KHAIRULAinda não há avaliações
- Onia Uerghi Ohamed Ougacha Abil Rikha Aher Estiri Ohamed en Mmar and Hamed EbazaaDocumento6 páginasOnia Uerghi Ohamed Ougacha Abil Rikha Aher Estiri Ohamed en Mmar and Hamed EbazaaHuda FauziAinda não há avaliações
- The Effects of Age On Neural Blockade and Hemodynamic Changes After Epidural Anesthesia With RopivacaineDocumento6 páginasThe Effects of Age On Neural Blockade and Hemodynamic Changes After Epidural Anesthesia With RopivacaineAnonymous K9tmd7T0PzAinda não há avaliações
- Endovascular Therapy For Acute Stroke With A Large Ischemic Region NEJMDocumento21 páginasEndovascular Therapy For Acute Stroke With A Large Ischemic Region NEJMSubhashini KAinda não há avaliações
- Ondan Hipo 3Documento5 páginasOndan Hipo 3putri maharani andesAinda não há avaliações
- Carpal Tunnel Syndrome - A ReviewDocumento10 páginasCarpal Tunnel Syndrome - A ReviewkenthepaAinda não há avaliações
- Acupuntura para La RodillaDocumento9 páginasAcupuntura para La Rodillaoscarin123456789Ainda não há avaliações
- The Effects of Dexmedetomidine Added To Spinal Bupivacaine For Lower Limb SurgeryDocumento4 páginasThe Effects of Dexmedetomidine Added To Spinal Bupivacaine For Lower Limb SurgeryInternational Organization of Scientific Research (IOSR)Ainda não há avaliações
- JCM 08 00051 v2Documento7 páginasJCM 08 00051 v2joelruizmaAinda não há avaliações
- A Comparative Study of Phenylephrine, Ephedrine and Mephentermine For Maintainance of Arterial Pressure During Spinal Anaesthesia in Caesarean SectionDocumento6 páginasA Comparative Study of Phenylephrine, Ephedrine and Mephentermine For Maintainance of Arterial Pressure During Spinal Anaesthesia in Caesarean SectionInternational Organization of Scientific Research (IOSR)Ainda não há avaliações
- Ondan Hipo 2Documento6 páginasOndan Hipo 2putri maharani andesAinda não há avaliações
- Lumbar PunctureDocumento4 páginasLumbar PunctureJeann sumbillaAinda não há avaliações
- Mecanismos 2Documento8 páginasMecanismos 2Arellano M VictorAinda não há avaliações
- Hemodynamic Effects of Chest-Knee Position: Comparison of Perioperative Propofol and Sevoflurane AnesthesiaDocumento6 páginasHemodynamic Effects of Chest-Knee Position: Comparison of Perioperative Propofol and Sevoflurane AnesthesiaAprilico Fadhil PangestuAinda não há avaliações
- Cardiac Rehabilitation: Interventions and Outcomes 631: ROC Curve For The Cut-Off Value of 6MWDDocumento1 páginaCardiac Rehabilitation: Interventions and Outcomes 631: ROC Curve For The Cut-Off Value of 6MWDKings AndrewAinda não há avaliações
- The Effects of Taping Neuromuscular Compare To Physical Therapies Modalities in Patients With Adhesive Capsulitis of The ShoulderDocumento8 páginasThe Effects of Taping Neuromuscular Compare To Physical Therapies Modalities in Patients With Adhesive Capsulitis of The ShouldersilviaAinda não há avaliações
- Jurnal Cts 2Documento10 páginasJurnal Cts 2Muhammad Hanafi QAinda não há avaliações
- Final PPRDocumento24 páginasFinal PPRAman hussainAinda não há avaliações
- Cervical Epidural Anesthesia For Sub-Total Thyroidectomy in A Patient With Aortic IncompetenceDocumento3 páginasCervical Epidural Anesthesia For Sub-Total Thyroidectomy in A Patient With Aortic Incompetenceaparna_losariAinda não há avaliações
- Stimulation With High-Frequency TENS - Effects On Lower Limb Spasticity After StrokeDocumento6 páginasStimulation With High-Frequency TENS - Effects On Lower Limb Spasticity After StrokeequalbenAinda não há avaliações
- Acupuncture For CTSDocumento7 páginasAcupuncture For CTSspiderAinda não há avaliações
- Articulo 1 ObesidadDocumento4 páginasArticulo 1 ObesidadOsiris AleitaAinda não há avaliações
- Nej M 199905203402002Documento6 páginasNej M 199905203402002Ridwan Hadinata SalimAinda não há avaliações
- Carotid Endarterectomy: Experience in 8743 Cases.Documento13 páginasCarotid Endarterectomy: Experience in 8743 Cases.Alexandre Campos Moraes AmatoAinda não há avaliações
- FRIDMAN - Achilles - Tendinopathies PDFDocumento3 páginasFRIDMAN - Achilles - Tendinopathies PDFadalberto torrealbaAinda não há avaliações
- Open Fixation in Flail Chest: Review of 64 Patients: Riginal OntributionDocumento6 páginasOpen Fixation in Flail Chest: Review of 64 Patients: Riginal OntributionDian PermatasariAinda não há avaliações
- New England Journal Medicine: The ofDocumento10 páginasNew England Journal Medicine: The ofsyafahalimAinda não há avaliações
- Ij2023 14Documento7 páginasIj2023 14Julenda CintarinovaAinda não há avaliações
- Effect of Early Physiotherapy On Intracranial PressureDocumento6 páginasEffect of Early Physiotherapy On Intracranial Pressurebendot29Ainda não há avaliações
- Immediate Effects of 2 Types of Braces On Pain and Grip Strength in People With Lateral Epicondylalgia: A Randomized Controlled TrialDocumento9 páginasImmediate Effects of 2 Types of Braces On Pain and Grip Strength in People With Lateral Epicondylalgia: A Randomized Controlled TrialRodrigo HamadaAinda não há avaliações
- Low Dose Levobupivacaıne 0.5% With Fentanyl in Spinal Anaesthesia For Transurethral Resection of Prostate SurgeryDocumento6 páginasLow Dose Levobupivacaıne 0.5% With Fentanyl in Spinal Anaesthesia For Transurethral Resection of Prostate Surgeryblabarry1109Ainda não há avaliações
- Low Dose Hyperbaric Bupivicaine Injected at T12-L1 Provides Adequate Anesthesia With Stable Hemodynamics For Elderly Patients Undergoing TURPDocumento6 páginasLow Dose Hyperbaric Bupivicaine Injected at T12-L1 Provides Adequate Anesthesia With Stable Hemodynamics For Elderly Patients Undergoing TURPblabarry1109Ainda não há avaliações
- 6Documento8 páginas6Mihai PopescuAinda não há avaliações
- Cervical Epidural Anaesthesia For Shoulder Arthroscopy and Effective Postoperative Physiotherapy For A Frozen Shoulder: A Case StudyDocumento4 páginasCervical Epidural Anaesthesia For Shoulder Arthroscopy and Effective Postoperative Physiotherapy For A Frozen Shoulder: A Case StudySutiyono TyoAinda não há avaliações
- Independent Risk Factor ShiveringDocumento9 páginasIndependent Risk Factor ShiveringAnonymous r2nNdvvweAinda não há avaliações
- Abat 2016Documento8 páginasAbat 2016toaldoAinda não há avaliações
- BMC Neurology: Autonomic Nervous System Dysfunction Predicts Poor Prognosis in Patients With Mild To Moderate TetanusDocumento4 páginasBMC Neurology: Autonomic Nervous System Dysfunction Predicts Poor Prognosis in Patients With Mild To Moderate TetanusYeli AstiAinda não há avaliações
- Eledjam1991 Article BrachialPlexusBlockWithBupivac PDFDocumento6 páginasEledjam1991 Article BrachialPlexusBlockWithBupivac PDFKalpanaAinda não há avaliações
- 24 G Sprotte and 27 G Quincke NeedleDocumento5 páginas24 G Sprotte and 27 G Quincke NeedleburhansmAinda não há avaliações
- Echo 6Documento10 páginasEcho 6Indera VyasAinda não há avaliações
- Mendigutiagmez 2016Documento11 páginasMendigutiagmez 2016Shinta Falah SariAinda não há avaliações
- 00003Documento8 páginas00003Anonymous zPwXqwAinda não há avaliações
- Artigo - Auricular AcupunctureDocumento2 páginasArtigo - Auricular AcupunctureAry NogueiraAinda não há avaliações
- International Journal of CardiologyDocumento5 páginasInternational Journal of CardiologyDiah Kris AyuAinda não há avaliações
- 7 Cochrane - UltrasoundGuided Percutaneous Electrolysis andDocumento10 páginas7 Cochrane - UltrasoundGuided Percutaneous Electrolysis andFranco Suazo MoralesAinda não há avaliações
- Content ServerDocumento8 páginasContent ServerKennie RamirezAinda não há avaliações
- Tens Us Ic Neck PainDocumento5 páginasTens Us Ic Neck PainMahnoor AqeelAinda não há avaliações
- Mitral Valve Annular Downsizing Forces: Implications For Annuloplasty Device DevelopmentDocumento8 páginasMitral Valve Annular Downsizing Forces: Implications For Annuloplasty Device Developmentdiana25Ainda não há avaliações
- Epidural Spinal Cord Stimulation Facilitates Immediate RestorationDocumento11 páginasEpidural Spinal Cord Stimulation Facilitates Immediate RestorationnorazmiAinda não há avaliações
- Incidence Severity and Detection of Blood Pressure and Heart Rate Perturbations in Postoperative Ward Patients After Noncardiac Surgery ScienceDirectDocumento6 páginasIncidence Severity and Detection of Blood Pressure and Heart Rate Perturbations in Postoperative Ward Patients After Noncardiac Surgery ScienceDirectChristian OpinaldoAinda não há avaliações
- Effectiveness of Tens Versus Intermittent CervicalDocumento6 páginasEffectiveness of Tens Versus Intermittent CervicalshindyAinda não há avaliações
- Comparison of Ultrasound-Guided Thoracic Paravertebral and Pectoralis Interfascial Plane Block For Modified Radical MastectomyDocumento7 páginasComparison of Ultrasound-Guided Thoracic Paravertebral and Pectoralis Interfascial Plane Block For Modified Radical MastectomyIJAR JOURNALAinda não há avaliações
- Extracorporeal Shock Wave Therapy VersusDocumento7 páginasExtracorporeal Shock Wave Therapy VersusGiannis SaramantosAinda não há avaliações
- 2020 Acupuncture Therapy For Poststroke Spastic HemiplegiaDocumento13 páginas2020 Acupuncture Therapy For Poststroke Spastic HemiplegiaHumberto Salas VelizAinda não há avaliações
- 03 Malone Spinal Cord InjuriesDocumento35 páginas03 Malone Spinal Cord InjuriesAnanta MiaAinda não há avaliações
- Clinical Handbook of Cardiac ElectrophysiologyNo EverandClinical Handbook of Cardiac ElectrophysiologyBenedict M. GloverAinda não há avaliações
- Current Techniques in Canine and Feline NeurosurgeryNo EverandCurrent Techniques in Canine and Feline NeurosurgeryAndy ShoresAinda não há avaliações
- Case-Based Device Therapy for Heart FailureNo EverandCase-Based Device Therapy for Heart FailureUlrika Birgersdotter-GreenAinda não há avaliações
- Chapt 01Documento12 páginasChapt 01ocoxodoAinda não há avaliações
- Clinical Application Meridian Diagnosis-FratkinDocumento20 páginasClinical Application Meridian Diagnosis-Fratkinocoxodo100% (3)
- A Grammar of The Arabic LanguageDocumento378 páginasA Grammar of The Arabic LanguagemanelaoAinda não há avaliações
- Analgesic Mechanism of Electroacupuncture in An Arthritic Pain Model of Rats: A Neurotransmitter StudyDocumento6 páginasAnalgesic Mechanism of Electroacupuncture in An Arthritic Pain Model of Rats: A Neurotransmitter Studyocoxodo0% (1)
- Research Article: Effects of Electroacupuncture at BL60 On Formalin-Induced Pain in RatsDocumento7 páginasResearch Article: Effects of Electroacupuncture at BL60 On Formalin-Induced Pain in RatsocoxodoAinda não há avaliações
- Treating Musculo-Skeletal Pain With Traditional Chinese MedicineDocumento2 páginasTreating Musculo-Skeletal Pain With Traditional Chinese MedicineocoxodoAinda não há avaliações
- Measures A: J. B. P. StephensonDocumento2 páginasMeasures A: J. B. P. StephensonocoxodoAinda não há avaliações
- Chronic PainDocumento13 páginasChronic PainocoxodoAinda não há avaliações
- Some Common A: Acupuncture For Evaluative ResearchDocumento5 páginasSome Common A: Acupuncture For Evaluative ResearchocoxodoAinda não há avaliações
- Effect of Acupuncture Depth On Muscle Pain: Research Open AccessDocumento5 páginasEffect of Acupuncture Depth On Muscle Pain: Research Open AccessocoxodoAinda não há avaliações
- Claims FoodDocumento68 páginasClaims FoodocoxodoAinda não há avaliações
- Health ClaimsDocumento719 páginasHealth ClaimsocoxodoAinda não há avaliações
- Post-Induction Hypotension and Intraoperative Hypotension As Potential Separate Risk Factors For The Adverse Outcome A Cohort StudyDocumento9 páginasPost-Induction Hypotension and Intraoperative Hypotension As Potential Separate Risk Factors For The Adverse Outcome A Cohort Studyfranco vidalAinda não há avaliações
- Intrathecal Morphine For Analgesia in Minimally Invasive Cardiac Surgery: A Randomized, Placebo-Controlled, Double-Blinded Clinical TrialDocumento13 páginasIntrathecal Morphine For Analgesia in Minimally Invasive Cardiac Surgery: A Randomized, Placebo-Controlled, Double-Blinded Clinical TrialLidwina ApyakaAinda não há avaliações
- P&T Chapter Wise 300 MCQDocumento13 páginasP&T Chapter Wise 300 MCQsudeep kulkarni100% (1)
- KAP Post Op Pain EthiopiaDocumento6 páginasKAP Post Op Pain EthiopiaJehan AliodenAinda não há avaliações
- BernaDocumento13 páginasBernaBernadette Collamar Dela CruzAinda não há avaliações
- Advancesinanesthesia Monitoring: Yi Deng,, Jovany Cruz Navarro,, Sandeep MarkanDocumento9 páginasAdvancesinanesthesia Monitoring: Yi Deng,, Jovany Cruz Navarro,, Sandeep MarkanUmer HussainAinda não há avaliações
- Somatics Brochure Thymatron PDFDocumento8 páginasSomatics Brochure Thymatron PDFCumhur TaşAinda não há avaliações
- Nonoperating Room Anesthesia Anesthesia in The Gastrointestinal SuiteDocumento16 páginasNonoperating Room Anesthesia Anesthesia in The Gastrointestinal SuiteGustavo ParedesAinda não há avaliações
- Caudal Anesthesia - NYSORADocumento27 páginasCaudal Anesthesia - NYSORApradeep daniel100% (1)
- Patient Safety in Dentistry: Dental Care Risk Management PlanDocumento16 páginasPatient Safety in Dentistry: Dental Care Risk Management PlanMiguel Jose LopezAinda não há avaliações
- Article On Difficult AirwayDocumento121 páginasArticle On Difficult AirwaySrilekha YarlagaddaAinda não há avaliações
- Anesthesia Machines - Orbis (Presentation)Documento52 páginasAnesthesia Machines - Orbis (Presentation)Zlatko JusupovicAinda não há avaliações
- Palestine Medical Council Certificate Examination: AnaesthesiaDocumento18 páginasPalestine Medical Council Certificate Examination: AnaesthesiaMysheb SSAinda não há avaliações
- Journal of Psychosomatic Research: Asish Subedi, Krishna Pokharel, Birendra Prasad Sah, Pashupati ChaudharyDocumento6 páginasJournal of Psychosomatic Research: Asish Subedi, Krishna Pokharel, Birendra Prasad Sah, Pashupati Chaudharynermal93Ainda não há avaliações
- Pharma Syllabus (Edited)Documento21 páginasPharma Syllabus (Edited)BSN CMUAinda não há avaliações
- Rguhs Oral SurgeryDocumento9 páginasRguhs Oral SurgerydrpnnreddyAinda não há avaliações
- Day 5 - APPEC 2021 PDFDocumento643 páginasDay 5 - APPEC 2021 PDFGaurieAinda não há avaliações
- Contact Details For Private Hospitals Day Procedure Centres and Mobile Health ServicesDocumento11 páginasContact Details For Private Hospitals Day Procedure Centres and Mobile Health Servicesshankey varmaAinda não há avaliações
- Solution To Mnm-Eng-Ix 2nd Term Pws Total Pages 72 PDFDocumento72 páginasSolution To Mnm-Eng-Ix 2nd Term Pws Total Pages 72 PDFpipraniaejaj1Ainda não há avaliações
- Management If Intra-Arterial Injection, ATOTW 2023Documento6 páginasManagement If Intra-Arterial Injection, ATOTW 2023Ali AftabAinda não há avaliações
- Complex Head and Neck Microvascular - SurgeryDocumento327 páginasComplex Head and Neck Microvascular - Surgerydoctorsoha.shAinda não há avaliações
- Moline-Roberts ArticleDocumento9 páginasMoline-Roberts Articleapi-244230664Ainda não há avaliações
- Standardized Color-Coding Solution Labeling in The Operating RoomDocumento3 páginasStandardized Color-Coding Solution Labeling in The Operating Roomcumar cabdicazizAinda não há avaliações
- Anesthprog00276-0033-Summary of The Scientific Literature For Pain and Anxiety Control in Dentistry-Journal Literature, January 1986-December 1987Documento19 páginasAnesthprog00276-0033-Summary of The Scientific Literature For Pain and Anxiety Control in Dentistry-Journal Literature, January 1986-December 1987skyclad_21Ainda não há avaliações
- Neuromuscular Disorders & Anaesthesia Anaesthesia Tutorial of The Week 126Documento9 páginasNeuromuscular Disorders & Anaesthesia Anaesthesia Tutorial of The Week 126friday ChitsongaAinda não há avaliações
- Remifentanil Pharmacology PDFDocumento41 páginasRemifentanil Pharmacology PDFamin138irAinda não há avaliações
- Anatomy Journal PDFDocumento9 páginasAnatomy Journal PDFHelda AudyaAinda não há avaliações
- [Journal of the American Veterinary Medical Association] Development of Enhanced Recovery After Surgery (ERAS) protocols in veterinary medicine through a one-health approach_ the role of anesthesia and locoregional techniquesDocumento9 páginas[Journal of the American Veterinary Medical Association] Development of Enhanced Recovery After Surgery (ERAS) protocols in veterinary medicine through a one-health approach_ the role of anesthesia and locoregional techniquesFrancisco Laecio Silva de AquinoAinda não há avaliações
- Coley 2019Documento8 páginasColey 2019KaniAinda não há avaliações
- Achieving Excellence in Cataract Surgery PDFDocumento150 páginasAchieving Excellence in Cataract Surgery PDFLiyanti RinceAinda não há avaliações


































































































![[Journal of the American Veterinary Medical Association] Development of Enhanced Recovery After Surgery (ERAS) protocols in veterinary medicine through a one-health approach_ the role of anesthesia and locoregional techniques](https://imgv2-1-f.scribdassets.com/img/document/597027379/149x198/4e86c3e723/1710567751?v=1)

