Escolar Documentos
Profissional Documentos
Cultura Documentos
Anatomy and Physiology of The Brain
Enviado por
Fildehl Janice Bomediano CatipayDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Anatomy and Physiology of The Brain
Enviado por
Fildehl Janice Bomediano CatipayDireitos autorais:
Formatos disponíveis
I.
Anatomy and Physiology of the CNS A. Parts of the brain 1. Cerebrum a) Cerebral hemispheres a1) Gyri Convolutions or many folded layers that results on the wrinkled appearance of the outside surface of the hemispheres. Responsible for the increase surface area of the brain, accounting for high level activity carried out by such a small-appearing organ. a2) Sulcus/fissure The anatomic division between each gyrus. The longitudinal fissure as an example separates the left and right cerebral hemisphere. Cerebral cortex The outer portion and contains billions of neuron cell bodies made up of gray matter, giving it a gray appearance. However, the inside part is composed of myelinated nerve fibers and neuroglial cells made up of white matter. These forms pathways or tracts that connect various brain parts to one another as well as the cortex to the lower portions of the brain and spinal cord. Corpus callosum A thick collection of nerve fibers that joins the left and right hemispheres at the lower portion of the fissure. Lobes Frontal The largest lobe located in front of the brain. Major functions include concentration, abstract thought, information storage or memory, and motor function. It contains Brocas area which is critical for motor control of speech. It is also responsible in large part for a persons affect, judgment, personality and inhibitions. Parietal A predominantly sensory lobe posterior to the frontal lobe. Analyzes sensory information and relays the interpretation of this information to other cortical areas and is essential to a persons awareness of body position in
a3)
a4)
a5)
space, size and shape discrimination, and right-left orientation. Temporal Located inferior to the frontal and parietal lobes and contains the auditory receptive areas and plays a role in memory of sound and understanding of language and music. Occipital Located posterior to the parietal lobe and is responsible for visual interpretation and memory. b) Thalamus Lies on either side of the third ventricle and acts primarily as a relay station for all sensation except smell. Hypothalamus Located anterior and inferior to the thalamus, and beneath and lateral top the third ventricle. Its infundibulum is connected to the posterior pituitary gland and thus plays an important role in endocrine system that influence metabolism, reproduction, stress response and urine production. It works with the pituitary in maintaining fluid balance and temperature regulation. The hunger center and centers regulating sleep-wake cycle, BP, aggressive and sexual behavior, and emotional responses are also found in here. Controls and regulates the ANS and contains the optic chiasm and mamillary bodies. Basal ganglia Masses of nuclei located deep in the cerebral hemispheres that are responsible for control of fine motor movements.
c)
d)
2. Brain Stem a) Midbrain Connects the pons and the cerebellum with the cerebral hemispheres and contains sensory and motor pathways and serves as the center for auditory and visual reflexes. b) Pons Situated in front of the cerebellum between the midbrain and the medulla and is bridge between the two halves of the cerebellum, and between the medulla and the midbrain. CN V and VIII originate here. It contains motor and sensory pathways. It also helps to regulate respiration. c) Medulla oblongata Motor fibers from the brain to the spinal cord and sensory fibers from the spinal cord to the brain are located here. CN IX and XII originate here. Reflex centers for respiration, BP, HR, coughing,
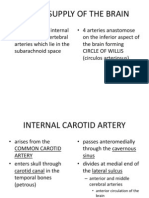
vomiting, swallowing, and sneezing are also found in here. The reticular formation, responsible for arousal and sleep-wake cycle begins in here. 3. Cerebellum Posterior to the midbrain and pons, and below the occipital lobe. This integrates sensory information to provide smooth coordinated movement. It controls fine movement, balance and position sense. B. Cerebral Circulation The brain receives approximately 15% of CO or 750 mL of blood/min. Brain circulation is unique in several aspects. First, arterial and venous circulation is not parallel as in other organs in the body due to its role in CSF absorption. Second, the brain has collateral circulations through the circle of willis , allowing blood flow to be redirected on demand. Third, blood vessels in the brain have 2 rather than 3 layers making it more prone to rupture when weakened or under high pressure. 1) Arteries Arterial blood supply originates from the common carotid artery, a bifurcation of the aorta, which then branches the internal carotid arteries comprising the anterior and middle cerebral arteries. Along these arteries is the anterior and posterior communicating arteries and together they form the circle of willis. The vertebral arteries branching from the subclavian artery then join to form the basilar artery which divides into 2 posterior cerebral arteries to supply most of the posterior circulation. Functionally, the two arterial circulations usually remain separated; however, in cases of vessel occlusion, the circle of willis can provide collateral circulation. 2) Veins The veins reach the brains surface, join larger veins, and then cross the subarachnoid space and empty into dural sinuses which are vascular channels laying within the dura. The venous blood in the sinus is then emptied through the internal jugular vein. 3) Blood-brain barrier The CNS is inaccessible to many substances that circulate in the plasma primarily due to the endothelial cells of the brain capillaries which creates barriers to macromolecules and many compounds. II. Causes of CNS Alterations
A. Head Injuries 4. Mechanism of Injury
a. Blunt trauma Blunt (closed) brain trauma occurs when the head accelerates and then rapidly decelerates or collides with another object (e.g. A wall, the dashboard of a car) and brain tissue is damaged but there is no opening through the skull and dura. b. Coup and contrecoup In this kind of injury, the brain bounces back and forth inside of the head, causing damage to the brain where it hits the skull. The brain is injured at the point of direct impact, and because it bounces back into the opposite side of the skull, the opposite side of the brain is injured as well. c. Penetrating trauma Penetrating (open) brain trauma occurs when an object penetrates the skull, enters the brain, and damages the soft brain tissue in its path, or when blunt trauma to the head is so severe that it opens the scalp, skull, and dura to expose the brain. 5. Primary/secondary Injury - Primary injury: It is the initial damage to the brain that results from the traumatic event. This may include contusion, laceration, and torn blood vessels due to impact, acceleration, deceleration, or foreign object penetration. - Secondary injury: Evolves over the ensuing hours and days after the initial injury and results from inadequate delivery of nutrients and oxygen to the cells a. Skull fracture A skull fracture is a break in the continuity of the cranium. The most common types are the following: Simple: Linear crack without any displacement of the pieces Depressed: Broken bone pushed inward the brain Comminuted: Bone splintered into fragments Because basilar skull fractures tend to tear the dura, rhinorrhea, leaking of CSF from the nose, or otorrhea, leakage of CSF from the ear, may occur. In some cases periorbital ecchymosis, referred to as raccoon eyes, or bruising of the mastoid process behind the ear, called Battles sign, can be present. b. Brain trauma
injury to the brain, including that caused by migrating worm larvae, will have diffuse effects including the development of edema, and local effects due to pressure by displaced bone or to hemorrhage. Initial shock, manifested as unconsciousness, is likely to be followed by residual localizing signs, e.g. facial paralysis, head rotation. c. Contusion In cerebral contusion, a moderate to severe head injury, the brain is bruised and damaged in a specific area because of severe acceleration-deceleration force or blunt trauma. The impact of the brain against the skull leads to a contusion. Most contusions are located in the anterior portions of the frontal and temporal lobes. Contusions are characterized by loss of consciousness associated with stupor and confusion. Other characteristics may include tissue alteration and neurologic deficit without hematoma formation. d. Concussion A concussion after head injury is a temporary loss of neurologic function with no apparent structural damage. A concussion may or may not produce a brief loss of consciousness. If brain tissue in the frontal lobe is affected, the patient may exhibit bizarre irrational behavior, whereas involvement of the temporal lobe can produce temporary amnesia or disorientation. Two types of concussion: Mild: o May lead to a period of observed or self-reported transient confusion, disorientation, or impaired consciousness o Commonly, with a memory lapse of at the time of injury and a loss of consciousness of less than 30 minutes. Classic: o It is an injury that results in a loss of consciousness that lasts less than 6 hours. o This loss of consciousness is always accompanied with some degree of posttraumatic amnesia. o Diagnostic studies may show no apparent structural signs of injury. e. Diffuse axonal injury DAI results from widespread shearing and rotation forces that produce damage throughout the brain to axons in the cerebral hemispheres, corpus callosum , and brain stem. The injury area may be diffuse, with no identifiable focal lesion. DAI is associated with prolonged traumatic coma. Has poor prognosis. f. Intracranial hemorrhage
Hematomas are collections of blood in the brain that may be in three different kinds. Major symptoms are frequently delayed until the hematoma is large enough to cause distortion of the brain and increased Intracranial Pressure (ICP). The three types of hematomas are the following: 1. Epidural Hematoma Blood may be collected in the epidural -above the dura- (extradural) space between the skull and the dura mater. This can result from a skull fracture that causes a rupture or laceration of the middle meningeal artery, the artery that runs between the dura and the skull inferior to a thin portion of temporal bone. Hemorrhage from this artery causes rapid pressure on the brain. 2. Subdural Hematoma It is a collection of blood between the dura and the brain, a space normally occupied by a thin cushion of fluid. A subdural hemorrhage is more frequently venous in origin and is caused by the rupture of small vessels that bridge the subdural space. The hematoma may be acute, subacute, or chronic, depending on the blood vessels involved. 3. Intracerebral Hematoma It is bleeding into the substance of the brain. It is commonly seen in head injuries when the force is exerted to the head over a small area. The onset might be insidious, beginning with the development of neurologic defects followed by headache. 6. Increased ICP The skull is a hard, bony vault field with brain tissue, blood and cerebrospinal fluid (CSF). Because the bony skull cannot expand, when one of the three compartments expands the other two must compensate by decreasing in volume for the total brain volume and Intracranial Pressure (ICP) to remain constant. The following compensatory mechanisms are used during increased ICP: 1.displacement of the CSF into the spinal cord 2. Reduction of blood volume in the brain (autoregulation) 3. displacement of brain tissue (herniation) The last mechanism can lead to brain stem compression which may precipitate in death. 7. Others a. Meningitis:
Meningitis is characterized by inflammation of the meningitis, the membrane lining the brain and spinal cord. Bacterial Meningitis An inflammation in the meninges caused by bacteria that enters in the body. The most common bacteria are: o Meningococci o Pneumococci o Haemophilus influenza Factors predisposing: Circumstance where the dura has been compromised, such an open injury or brain surgery, systemic infection, anatomic defects of the skull, immunocompromise and other systemic illness Clinical manifestation: o Nuchal rigidity (rigidity of the neck) o Brudzinski sign ( the client is in supine lift the head rapidly up from the bed. Meningeal irritation occurs, forward neck flexion produces flexion on both thighs at the hips and flexure movements of the ankles n knees) o Kernigs sign (the client is in recumbent and the thigh flexed at a right angle to the abdomen, with the knee flexed at the 90-degree angle to the thigh. Then extend the clients lower leg. Meningeal irritation occurs, Upon extending the leg upward it causes pain, spasm of the hamstring muscles, and the resistance to further leg extension at the knee.) o Photophobia o Moderately elevated CSF pressures o Elevate d CSF protein level ( normal 15 to 45 mg/dl) o Decreased CSF glucose level ( normal 60 to 80 mg/dl or two thirds of the serum level) o Elevated white blood cells count , usually increased (100 to 10,000/ cm3) with predominantly polymorphonuclear leukocytes
Viral Meningitis An inflammation caused by a virus Most common viral meningitis is: o Mumps virus clinical manifestation: drowsiness, headache, weakness, photophobia management: symptomatic management to reduce headache, control fever, and increase general comfort b. Brain abscess
is a collection of infectious material/ pus within brain tissue may occur after a penetrating traumatic brain injuries or intracranial surgery frontal lobe is the common for brain abscess relatively rare they vary in size multiple abscess are microscopic in its early stage, the abscess produces inflammation, necrotic tissue and surrounding edema. Within several days, the center of abscess is purulent and a wall of granulation tissue forms, encapsulating the abscess. Infection may spread through thin places in the wall of the capsule, resulting in the development of additional abscess clinical manifestation: o same with those seen in space-occupying brain lesion o headache o lethargy o drowsiness o confusion o depressed mental status o increased ICP o transient focal neurologic disorder ( occur when abscess is located in a specific area such as motor or speech area Medical diagnosis is made by CT or MRI. However the appearance is same like a brain tumor
III.
Neurologic Assessment 1. Glasgow Comma Test is a tool for assessing a patients response to stimuli. Scores range from 3 (deep coma) to 15 (normal)
Eye opening response Spontaneous To voice To pain none Oriented Confused Inappropriate words Incomprehensible sounds none 4 3 2 1 5 4 3 2 1
Best verbal response
Best motor response
Obeys command Localizes pain Withdraws Flexion Extension none
6 5 4 3 2 1 3 to 15
total
2. Motor Activity Assessment Motor function is assessed frequently by observing spontaneous movements, asking the patients to raise and lower extremities, and comparing the strength and equality of the upper and lower extremities at periodic intervals. To assessed the upper extremities strength, the nurse instruct the patient to squeeze the examiners fingers tightly To assessed the lower extremities, by placing the hands on the soles of the patients feet and asking the patient to push down against the examiners hands If the patient does not demonstrate spontaneous movement, response to painful is assessed. Motor response to pain is assessed by applying a central stimulus to determine the patients best response. Abnormal response are associated with poor prognosis 3. PERRLA Unilaterally dilated and poorly responding pupils may indicate a developing hematoma, with subsequent pressure on the third cranial nerve due to shifting of the brain. If both pupils become fixed and dilated, this indicates overwhelming injury and intrinsic damage to the upper brain stem and is poor prognostic sign Deficits: o anosmia (lack of sense of smell); o eye movement abnormalities o aphasia o memory deficits o posttraumatic seizures or epilepsy IV. Management 1. Surgical Management a. Craniotomy Involves opening the skull surgically to gain access to intracranial structures This procedure is performed to remove a tumor, relieve elevated ICP, evacuate a blood clot or control hemorrhage The surgeon cuts the skull to create a bony flap, which can be repositioned after the surgery and held in place by periosteal or wire suture Approaches used:
o Above the tentorium ( supratentorial craniotomy) into the supratentorial compartment o Below the tentorium into the infratentorial (posterior fossa) compartment o Transsphenoidal approach is often used to gain access the pituitary gland Burr holes which are circular openings made in the skull by either a hand drill or an automatic craniotome b. Craniectomy Excision of the portion of the skull c. VP Shunts Ventriculoperitoneal shunting is surgery to relieve increased pressure inside the skull due to excess cerebrospinal fluid (CSF) on the brain. The VP shunt is small tubing that is placed inside the brains ventricle and tunneled underneath the skin to the peritoneum. A shunt helps to drain the excess fluid and relieve the pressure in the brain. 2. Pharmacological Management a. Mannitol Diagnostic agent; osmotic diuretic; urinary irrigant Indicated for the reduction of intracranial pressure and treatment of cerebral edema; of elevated IOP when the pressure cannot be lowered by other means Check BP before admission b. Corticosteroids May include bronchodilators that can facilitate breathing and gas exchange in clients with respiratory deficits or difficulties. Ex. Predisone c. Furosemide Loop diuretic Indication: o IV, Oral: edema, associated with heart failure, cirrhosis, renal disease o IV: acute pulmonary edema o Oral: hypertension d. Cefuroxime Axetil An antibiotic; 2nd generation of cephalosporin Inhibits synthesis of bactericidal cell wall causing cell death
Oral Indicated e. IV fluids Intravenous fluids are often used as a supportive measure for postoperative clients as either or both parenteral nutrition and/or fluid and electrolyte replacement. The kinds of the fluids vary depending on the need of the patient.
3. Nursing Management a. Independent Monitoring Neurologic Function o Level of consciousness The GCS is used to assess the LOC at regular intervals, because the change in LOC precedes all the changes in vital and neurologic signs. o Vital signs Vital signs are monitored to assess the intracranial status. Signs of increasing ICP include slowing heart rate, increasing systolic blood pressure widening pulse (cushings reflex) Rapid increase of body temperature is regarded as unfavorable because hyperthermia increases the metabolic demands of the brain and may indicate brain stem damage. Temperature should be maintained at less than 380C (100.40F). Tachycardia and arterial hypotension may indicate that bleeding is occurring o Motor functions Motor function is assessed frequently by observing spontaneous movements, asking the patient to raise and lower the extremities and comparing the strength and equality of the upper and lower extremities at periodic intervals o Other neurologic signs This is assessed through observing the spontaneous eye opening, evaluated with the GCS, the size and equality of the pupils and their reaction to light. Maintaining the airway o Establishing and maintaining adequate airway is one of important degrees nursing goal in caring a patient with head injury o Brain is extremely sensitive to hypoxia, hence, maintaining optimal oxygenation is directed to preserved cerebral function o Obstruction of the airway causes the carbon dioxide to retention and hypoventilation, which can produce cerebral vessel dilatation and increased ICP
o Interventions: Maintaining the unconscious patient in a position that facilitates drainage of oral secretions, with head is elevated about 30 degrees to decrease intracranial venous pressure Establishing effective suctioning procedures ( pulmonary secretions produce coughing and straining which increase ICP) Guarding against aspiration and respiratory insufficiency Closely monitoring the arterial blood gas values to assess the adequacy of ventilation, to ensure there is adequate cerebral blood flow Monitoring the patient who is receiving mechanical ventilator for pulmonary complications such as acute respiratory distress syndrome (ARDS) and pneumonia Monitoring fluid and electrolyte balance o Serial studies of blood and urine electrolytes and osmolality are carried out because head injuries may be accompanied by disorders of sodium regulation. o Hyponatremia is common after head injury due to shifts in extracellular fluid, electrolytes, and volume. May also occur as a result of sodium retention that may last for a several days, followed by a sodium diuresis. o Increasing lethargy, confusion, and seizures may be the result of electrolyte imbalance o Endocrine function is evaluated by monitoring the serum electrolytes, blood glucose values, and intake and output. o Urine is tested regularly for acetone Promoting adequate nutrition o Head injuries results in metabolic changes that increase calorie consumption and nitrogen excretion o Parenteral nutrition via a central line or enteral feeding administered via a nasogastric or nasojejunal feeding tube should be considered. o If CSF rhinorrhea occurs, an oral feeding tube should be inserted instead of a nasal tube o Laboratory should be monitored closely o Elevating the head of the bed and aspirating the enteral tube for evidence of residual feeding before administering additional feeding can help to prevent distension, regurgitation and aspiration o A continuous drip infusion or pump may be used to regulate the feeding o Enteral or parenteral feeding is usually continued until the swallowing reflex returns and the patient can meet caloric requirements orally. Preventing injury
o The patient is assessed to ensure the oxygenation is adequate and the bladder is not distended. Dressing and casts are checked for constriction o Padded side rails are used or the patients hands are wrapped in mitts to protect the patient from self injury and dislodging the tube. Restraints are avoided because straining against them can increase ICP or cause other injury. Enclosed or floor-level specialty beds may be indicated o Opioids are avoided as a means of controlling restlessness because they depress respiration, constrict the pupils and alter responsiveness o Environmental stimuli are reduced by keeping the room quite, limiting visitors, speaking calmly, and providing frequent orientation information o Adequate lighting is provided to prevent visual hallucination o Efforts are made to minimize disruption of the patients sleep-wake cycles o The patients skin is lubricated with oil or emollient lotion to prevent irritation due to rubbing against the sheet o If continence occurs, an external sheath catheter may be used on male patient. Because prolonged use of an indwelling catheter inevitably produces an intermittent catheterization schedule Maintain body temperature o The nurse monitors the patient temperature every 2 to 4 hours. If the temperature increases, efforts are made to identify the cause and to control in using acetaminophen and cooling blankets to maintains normothermia. Cooling blankets should be used with caution so as not to induce shivering, which increases ICP o Use of mild hypothermia to 340C to 350C ( 940F to 960F) has been tested in small randomized controlled trials for at least 12 hours versus normothermia (control) in patients with closed head injury. Maintaining skin integrity o Assessing all body surfaces in documenting skin integrity every 8 hours o Turning and repositioning the patient every 2 hours o Providing skin care every 4 hours o Assisting the patient to get out of the bed to a chair three times a day Preventing sleep pattern disturbance o Patients are usually disturbed in their sleep due to assessment of LOC. To allow the patient longer times of uninterrupted sleep and rest, the nurse can group nursing care activities so that the patient is disturbed less frequently.
o Environmental noise is decreased, and the room lights are dimmed. Back rubs and other measure to increase comfort may sleep and rest. Monitoring and managing potential complications o Decreased cerebral perfusion pressure Maintenance of the CPP is important to prevent serious complications, adequate CPP is greater than 60 mm Hg. o Cerebral Edema and herniation Administer osmotic diuretics as prescribed ( monitor serum osmolality) to promotes venous return Maintain head of bed elevated 30 degrees to prevent impairment of venous return through the jugular veins o Impaired oxygenation and ventilation Administer endotracheal intubation, mechanical ventilation and positive end-expiratory pressure o Impaired fluid, electrolyte and nutritional balance Insulin administration may be prescribed to treat hyperglycemia Decision about early tube feeding should be individualized; options include IV hyperalimenation or placement of a feeding tube (jejunal or gastric) Caloric expenditure can increase up to 120% to 140% with TBI, requiring close monitoring of nutritional status Feeding tubes should be placed 3 to 7 days after neurologic injury to replace energy and nitrogen losses, prevent increased mortality and improve outcomes. o Post-traumatic seizures Post-traumatic seizures are classified as immediate (within 24 hours after injury), early (within 1 to 7 days after injury), or late (more than 7 days after injury) Seizure prophylaxis is the practice of administering anti-seizure medications to patients with head injury to prevent seizure.
b. Dependent Improving cognitive function o These problems require collaboration among many disciplines. o Neuropsychologist (specialist in evaluating and treating cognitive problems) plans a programs and initiates therapy or counseling to help the patient reach maximal potential. o Rancho Los Amigos Level of Cognitive Function scale is frequently used to assess cognitive function and evaluate ongoing recovery from head injury.
Computed tomography (CT) scan uses a high speed of x-ray scanning to detect less apparent abnormalities Referrals for Magnetic Resonance Imagining (MRI)
Você também pode gostar
- Lung Development Biological and Clinical Perspectives: Biochemistry and PhysiologyNo EverandLung Development Biological and Clinical Perspectives: Biochemistry and PhysiologyPhilip FarrellAinda não há avaliações
- 0001 5866aDocumento830 páginas0001 5866aZllison Mae Teodoro MangabatAinda não há avaliações
- Chapter 54 - Drugs Acting On The Upper Respiratory TractDocumento13 páginasChapter 54 - Drugs Acting On The Upper Respiratory TractJonathonAinda não há avaliações
- Sample Research ProposalDocumento43 páginasSample Research ProposalLuis LazaroAinda não há avaliações
- Chapter 48 - Drugs Affecting Blood CoagulationDocumento12 páginasChapter 48 - Drugs Affecting Blood CoagulationJonathon100% (1)
- Patterns of RespirationDocumento67 páginasPatterns of Respirationsteven hkAinda não há avaliações
- Chapter 47 - Lipid-Lowering AgentsDocumento13 páginasChapter 47 - Lipid-Lowering AgentsJonathonAinda não há avaliações
- Anatomy and Physiology of Blood VesselDocumento3 páginasAnatomy and Physiology of Blood Vesselneleh grayAinda não há avaliações
- Chapter 1 The Foundations of BiochemistryDocumento5 páginasChapter 1 The Foundations of BiochemistryghurapAinda não há avaliações
- CVS HistologyDocumento43 páginasCVS Histologyبراءة أحمد السلامات100% (1)
- Chapter 59 - Antiemetic AgentsDocumento11 páginasChapter 59 - Antiemetic AgentsJonathonAinda não há avaliações
- Chapter 55 - Drugs Acting On The Lower Respiratory TractDocumento13 páginasChapter 55 - Drugs Acting On The Lower Respiratory TractJonathonAinda não há avaliações
- Anatomy and Physiology of The BRAINDocumento5 páginasAnatomy and Physiology of The BRAING FernandezAinda não há avaliações
- Chapter 52 - Drugs Affecting The Urinary Tract and The BladderDocumento12 páginasChapter 52 - Drugs Affecting The Urinary Tract and The BladderJonathonAinda não há avaliações
- Imaging Findings and Clinical Correlation: Cerebral Herniation SyndromesDocumento64 páginasImaging Findings and Clinical Correlation: Cerebral Herniation SyndromessridharAinda não há avaliações
- Myasthenia Gravis: An Autoimmune Neurologic DisorderDocumento16 páginasMyasthenia Gravis: An Autoimmune Neurologic DisorderHibba NasserAinda não há avaliações
- Review of Cardiovascular SystemDocumento20 páginasReview of Cardiovascular SystemVăn ĐứcAinda não há avaliações
- 24 Cerebral Blood FlowDocumento31 páginas24 Cerebral Blood FlowZuhaib Ahmed100% (1)
- Blood Supply of The BrainDocumento11 páginasBlood Supply of The Brainneleh grayAinda não há avaliações
- Renal 2 MTC PDFDocumento55 páginasRenal 2 MTC PDFDrbee10Ainda não há avaliações
- Components of The Cardiovascular SystemDocumento23 páginasComponents of The Cardiovascular SystemMr. DummyAinda não há avaliações
- Hydrocephalus PDFDocumento17 páginasHydrocephalus PDFEdna López100% (1)
- Lec - 1H - Special Senses System ReviewerDocumento18 páginasLec - 1H - Special Senses System ReviewerProfessor GhoulAinda não há avaliações
- Physiology of VomitingDocumento24 páginasPhysiology of VomitingKingWayne Tagatac BajoAinda não há avaliações
- Physiology Chap10 (Rhythmical Excitation of The Heart)Documento3 páginasPhysiology Chap10 (Rhythmical Excitation of The Heart)Man Dejelo100% (1)
- Nutri WopsDocumento4 páginasNutri WopsRizzy Ugay100% (1)
- Molecular Diagnosis of Cystic FibrosisDocumento25 páginasMolecular Diagnosis of Cystic Fibrosisyugen31Ainda não há avaliações
- CopdDocumento4 páginasCopdapi-3739910100% (2)
- Bilaminar and Trilaminar Germ DiscDocumento40 páginasBilaminar and Trilaminar Germ DiscjabirAinda não há avaliações
- 06 - 07 - Anatomy of The Chest Wall and BreastDocumento16 páginas06 - 07 - Anatomy of The Chest Wall and Breastbo gum parkAinda não há avaliações
- Angina PectorisDocumento8 páginasAngina PectorisJoanne LagusadAinda não há avaliações
- Neurology Lectures 1 5 DR - Rabo 2Documento20 páginasNeurology Lectures 1 5 DR - Rabo 2Miguel Cuevas DolotAinda não há avaliações
- Gross Anats Presem ReviewDocumento14 páginasGross Anats Presem ReviewCarlos NiñoAinda não há avaliações
- Blood Supply of The CNS: Mrs A.A.NwakanmaDocumento25 páginasBlood Supply of The CNS: Mrs A.A.NwakanmaJames AchuAinda não há avaliações
- Case Analysis HydrocephalusDocumento11 páginasCase Analysis HydrocephalusRaiAinda não há avaliações
- Exercise 10Documento4 páginasExercise 10aker39Ainda não há avaliações
- Cerebrovascular AccidentDocumento6 páginasCerebrovascular AccidentRodel CamposoAinda não há avaliações
- Brain HerniationDocumento40 páginasBrain HerniationAnusha VergheseAinda não há avaliações
- Physiology 8 Nervous SystemDocumento7 páginasPhysiology 8 Nervous SystemFahim Khan100% (18)
- Hemorrhoid MedscapeDocumento10 páginasHemorrhoid MedscapeRastho Mahotama100% (1)
- Embryology-Development of Central Nervous SystemDocumento28 páginasEmbryology-Development of Central Nervous Systemtenshi315Ainda não há avaliações
- The Physiology of VisionDocumento24 páginasThe Physiology of VisionSana MohsinAinda não há avaliações
- Intro Head and NeckDocumento74 páginasIntro Head and NeckAuza Moses Ibrahim100% (2)
- Physiology of RespirationDocumento2 páginasPhysiology of RespirationIOSRjournalAinda não há avaliações
- Breasts and AxillaeDocumento10 páginasBreasts and Axillaedlneisha61100% (1)
- Pulmonary Tuberculosis: Presented By: Mis.M.K.Kaku Nursing TutorDocumento16 páginasPulmonary Tuberculosis: Presented By: Mis.M.K.Kaku Nursing TutorKaku ManishaAinda não há avaliações
- Lecture - 3 Properties of Cardiac MuscleDocumento35 páginasLecture - 3 Properties of Cardiac MuscleMRM7MDAinda não há avaliações
- Hepatitis BDocumento12 páginasHepatitis BTeti AndriAinda não há avaliações
- U Michigan Written Practice Quiz Brain and MeningesDocumento3 páginasU Michigan Written Practice Quiz Brain and MeningesJublant JimmiyahAinda não há avaliações
- 3.0 Grand Physiology Finals Compilation - Batch 2017Documento89 páginas3.0 Grand Physiology Finals Compilation - Batch 2017Sheryl Layne Lao-SebrioAinda não há avaliações
- Physio Reviewer Renal To Acid BaseDocumento11 páginasPhysio Reviewer Renal To Acid BaseNicole ChanAinda não há avaliações
- Fetal CirculationDocumento20 páginasFetal CirculationMuhyeeSalaIdjadAinda não há avaliações
- #4 Nervous-SystemDocumento19 páginas#4 Nervous-SystemLapitan Jared Anne S.Ainda não há avaliações
- The Thoracic CavityDocumento43 páginasThe Thoracic Cavitybayenn100% (2)
- The Gut Tube and Body CavitiesDocumento31 páginasThe Gut Tube and Body CavitiesGeoffreyAinda não há avaliações
- Guyton and Hall Textbook of Medical Physiology 13th Ed (2015) - 974-1006Documento33 páginasGuyton and Hall Textbook of Medical Physiology 13th Ed (2015) - 974-1006siñthiAinda não há avaliações
- Causes Obstruction Causes CSF To Build Up in The Brain. If The Cause Is Congenital, Symptoms Such As AnDocumento22 páginasCauses Obstruction Causes CSF To Build Up in The Brain. If The Cause Is Congenital, Symptoms Such As Anmhelandie100% (1)
- ANA 6.01 General Somatic Afferents Dr. EsguerraDocumento22 páginasANA 6.01 General Somatic Afferents Dr. EsguerraNinna Ricci San JuanAinda não há avaliações
- Nervous System - Anatomy of The BrainDocumento3 páginasNervous System - Anatomy of The BrainKhate Cassey ParalejasAinda não há avaliações
- LP Trauma Kapitis PDFDocumento29 páginasLP Trauma Kapitis PDFPajoAinda não há avaliações
- Adults and Children 15 Y Pediatric 6 - 14 YDocumento2 páginasAdults and Children 15 Y Pediatric 6 - 14 YFildehl Janice Bomediano Catipay100% (1)
- Bad Effects of E-Gadgets On Health and Safety UseDocumento19 páginasBad Effects of E-Gadgets On Health and Safety UseFildehl Janice Bomediano CatipayAinda não há avaliações
- Classification (S) Therapeutic: Anti-Infectives Pharmacologic: FluoroquinolonesDocumento9 páginasClassification (S) Therapeutic: Anti-Infectives Pharmacologic: FluoroquinolonesFildehl Janice Bomediano CatipayAinda não há avaliações
- SalbutamolDocumento5 páginasSalbutamolFildehl Janice Bomediano CatipayAinda não há avaliações
- Zinc SulfateDocumento2 páginasZinc SulfateFildehl Janice Bomediano CatipayAinda não há avaliações
- Martin Buber: BiographyDocumento4 páginasMartin Buber: BiographyFildehl Janice Bomediano CatipayAinda não há avaliações
- Prelims: - Intro To Calvarium and Head/brain Imaging Modalities - Craniofacial TraumaDocumento97 páginasPrelims: - Intro To Calvarium and Head/brain Imaging Modalities - Craniofacial TraumaRica AriasAinda não há avaliações
- 3 - Head Injured PatientDocumento94 páginas3 - Head Injured PatientAmmarAinda não há avaliações
- Cranial Base Dan Emergency CaseDocumento34 páginasCranial Base Dan Emergency Caserahmad wahyuAinda não há avaliações
- Head Injury OkeDocumento42 páginasHead Injury OkeAnonymous p9msXAEwAinda não há avaliações
- 39 MCQ's in NeurosurgeryDocumento26 páginas39 MCQ's in NeurosurgeryAhmed Hamid Ibrahim100% (4)
- Emergency and Disaster NursingDocumento19 páginasEmergency and Disaster NursingNina OaipAinda não há avaliações
- First Aid 2Documento20 páginasFirst Aid 2Casper ScholesAinda não há avaliações
- Harris - Harris - The Radiology of Emergency Medicine, 5th EditionDocumento1.050 páginasHarris - Harris - The Radiology of Emergency Medicine, 5th EditionMadalina Talpau100% (1)
- Rad. Positioning 2Documento553 páginasRad. Positioning 2Lalaine De JesusAinda não há avaliações
- Final-Exam Neurosurgery - 3-VersionDocumento6 páginasFinal-Exam Neurosurgery - 3-VersionMAMA LALAAinda não há avaliações
- Ear Trauma PDFDocumento14 páginasEar Trauma PDFAnggi CalapiAinda não há avaliações
- RADIOLOGY 2.1e Skull FracturesDocumento1 páginaRADIOLOGY 2.1e Skull FracturesZazaAinda não há avaliações
- Skull Fracture Vs SuturesDocumento6 páginasSkull Fracture Vs Suturesmohit372Ainda não há avaliações
- Cranioplasty With Custom-Made Titanium Plates-14 Years ExperienceDocumento10 páginasCranioplasty With Custom-Made Titanium Plates-14 Years Experiencethanhnhat5521Ainda não há avaliações
- Medical Radiology - Diagnostic ImagingDocumento412 páginasMedical Radiology - Diagnostic ImagingBiancaRalucaAinda não há avaliações
- Types of Brain HemorrhageDocumento2 páginasTypes of Brain HemorrhageRichie Marie BajaAinda não há avaliações
- Traumatic Brain Injury and Cerebral ResuscitationDocumento56 páginasTraumatic Brain Injury and Cerebral ResuscitationsyahirAinda não há avaliações
- Traumatic Brain Injury (TBI)Documento48 páginasTraumatic Brain Injury (TBI)Alaa OmarAinda não há avaliações
- Finished Head Injury Ppt-1Documento76 páginasFinished Head Injury Ppt-1Chalie MequanentAinda não há avaliações
- Basilar Skull Fractures & DAIDocumento17 páginasBasilar Skull Fractures & DAIIsabela OlgaAinda não há avaliações
- Head Injury SymptomsDocumento3 páginasHead Injury SymptomsMay NitayakulAinda não há avaliações
- Guillain - Barre SyndromeDocumento63 páginasGuillain - Barre SyndrometheamaciasAinda não há avaliações
- Unusually Delayed Posttraumatic CSF Rhinorrhoea: Case ReportDocumento2 páginasUnusually Delayed Posttraumatic CSF Rhinorrhoea: Case ReportPcrAinda não há avaliações
- Head Injury 5Documento68 páginasHead Injury 5drvishal bhattAinda não há avaliações
- Traumatic Brain Injury (TBI) - Definition and Pathophysiology - Overview, Epidemiology, Primary InjuryDocumento15 páginasTraumatic Brain Injury (TBI) - Definition and Pathophysiology - Overview, Epidemiology, Primary InjuryUtari Septiana DewiAinda não há avaliações
- Types of Skull FractureDocumento5 páginasTypes of Skull FractureKhor Hui DiAinda não há avaliações
- Soal Ujian Bedah SarafDocumento7 páginasSoal Ujian Bedah SarafdrghempikAinda não há avaliações
- Emergency traumaEMQ34Documento34 páginasEmergency traumaEMQ34assssadfAinda não há avaliações
- Head Injury PathologyDocumento12 páginasHead Injury Pathologyimilosavljev@gmail.comAinda não há avaliações
- Head Trauma Brain InjuryDocumento54 páginasHead Trauma Brain Injurymirzabb1Ainda não há avaliações
- The Storyteller: Expanded: ...Because There's More to the StoryNo EverandThe Storyteller: Expanded: ...Because There's More to the StoryNota: 5 de 5 estrelas5/5 (13)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsNo EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsNota: 4.5 de 5 estrelas4.5/5 (39)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDNo EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDNota: 4.5 de 5 estrelas4.5/5 (167)
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesNo EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesNota: 5 de 5 estrelas5/5 (70)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisNo EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisNota: 4 de 5 estrelas4/5 (9)
- The Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItNo EverandThe Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItNota: 4.5 de 5 estrelas4.5/5 (107)
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeNo EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeNota: 4.5 de 5 estrelas4.5/5 (141)
- Feel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveNo EverandFeel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveNota: 4 de 5 estrelas4/5 (250)
- Summary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisNo EverandSummary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisNota: 5 de 5 estrelas5/5 (5)
- Bare Bones: I'm Not Lonely If You're Reading This BookNo EverandBare Bones: I'm Not Lonely If You're Reading This BookNota: 4 de 5 estrelas4/5 (11)
- Binaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationNo EverandBinaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationNota: 5 de 5 estrelas5/5 (9)
- The 27 Club: Curse or Coincidence?: The True Stories Behind Entertainment's Most Enduring Urban LegendNo EverandThe 27 Club: Curse or Coincidence?: The True Stories Behind Entertainment's Most Enduring Urban LegendNota: 4 de 5 estrelas4/5 (10)
- Summary: Greenlights: by Matthew McConaughey: Key Takeaways, Summary & AnalysisNo EverandSummary: Greenlights: by Matthew McConaughey: Key Takeaways, Summary & AnalysisNota: 4 de 5 estrelas4/5 (6)
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeNo EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeNota: 4.5 de 5 estrelas4.5/5 (49)