Escolar Documentos
Profissional Documentos
Cultura Documentos
Y3b3 Ong Groupd B - 13
Enviado por
Akmal ZaimDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Y3b3 Ong Groupd B - 13
Enviado por
Akmal ZaimDireitos autorais:
Formatos disponíveis
O n G GROUP D MCQ 1) true regarding antenatal care a) fetal heart sound is audible from 12w POA by using daptone
b) blood screening test done in Msia includes HIV, Hep B, VDRL, Rubella, Toxoplasma c) routine antenatal visit for diabetic patient is 4-weekly from 20week POA up to 32week POA d) rubella vaccine is contraindicated e) uterus is palpable on abdominal examination from 10 week POA 2) following condition requires vaginal assessment antenatally: a) extensive offensive foul smelling pv discharge b) transverse lie c) leaking liquor d) contraction pain e) pv bleeding of unknown cause 3) regarding menorrhagia a) blood loss more than 80 ml during menses b) coagulation effect is the common cause c) indication for endometrial sampling is increase endometrial thickness d) Mirena is the rx of choice 4) Ovarian CA a) Serous cystadenocarcinoma cancer b) Typically increase CEA c) Presented at late stage d) Effective screening alvailable 5) Regarding fetal assessment a) CRL measurement exclude limb measurement b) Lecithin sphingomyelin ratio is used to measure lung maturity c) Fetal movement perceived by mother included in the biophysical profile d) BPD is reliable for dating #rd trimester 6) Polyhydramnios: a) Postmaturity b) Polycystic kidney disease c) Increase frequency of leg edema d) Secondary PPH 7) Menopause: a) Loss of libido b) Increase vaginal acidity c) Increase osteoblast activity 8) regarding twin pregnancy
9)
10)
11)
12)
13)
14)
15)
a) monozygotic twin always have 1 placenta b) recognized complication are APH,preeclamsia,pretermlabour c) twin to twin transfusion syndrome occur usually in dichorionic d) mortality of 1st twin is higher than 2nd twin signs and symptoms of uterine rupture during labour a) continuous abdominal pain b) heavy vaginal bleeding c) strong uterine contraction d) fetal death Predisposing factor of abnormal lie: a) Uterine didelphys b) Primigravida c) Short stature d) Hydrocephalus e) Fetal neuromuscular condition Statement true regarding breech a) Planned vaginal delivery should be attended by experienced obstetrician b) Elective c-sec is safer than vaginal delivery for breech presentation at term c) ECV can be done at 35 w and above d) One of factors that favour the likelihood of successful breech vaginal delivery is primigravida PPROM a) CRP- reliable to diagnose chorioamnities b) Corticosterion is contraindication c) Vaginal exam in contraindicated d) Congenital pneumonia prevented with abintrapartum e) Litmus test blue to red indicate leaking pCOS a) acanthosisnigricans b) recurrent miscarriage c) pearl on string in US d) anovolutary cycle e) LH:FSH ratio is 1:2 Threathened miscarriage a) Vaginal blledingsi the symptoms b) Uterus is smaller than POG c) Weekly US is assessed as clinical evaluation d) Risk of having abnormal baby if pregnancy is cont e) Progesterone support is beneficial in luteal phase HCG a) Release by snycytiotrophoblast b) Double every 48 hours
c) B subunit HCG is share similar structure with B subunit of TSH d) In normal pregnancy, b HCG suppress FSH and LH OBA 1) 30/M/G6P5 admitted in active phase of labour. EFW: 3.5kg. she is obese with BMI=30. She is not hypertensive or diabetic. VE done at 3pm; cervical effacement 1cm, os 4cm, station 0. ARM done, liquor clear, CTG reactive. Review at 7pm reveals os 8cm. review at 9pm; os still 8cm, moulding 2+, CTG still reactive. What should you do? a. advise patient for C-Sec b. prepare patients GXM c. augmentlabour with oxytocin. d. prepare patient for ventouse delivery e. review patient again after 2 hours
2) 25 y/o, G1P0 at 30 week POA, c/o PV bleeding of one day duration. Previously told to have breech presentation 1 week prior. Went to see traditional midwife to massage in order to correct the presentation. Clinically, bruises were noted at left lumbar region, uterus size is 32 week. Head is 3/5th palpable. 3) Most likely diagnosis? a. abruption placenta. b. placenta previa c. bleeding disorder d. vasa previa e. show (sign of labour) 4) 26 sexually active. 4 months of white discharge foul smelling. Came with 2 days history of abdominal pain. a. Trachomonasvaginalis b. Chlamydia trachomonitis c. M. tuberculosis d. Israeli e. M. genitalis
5) 35/P4/LCB 5 years ago. Presented with history of menorrhagia and abdominal mass of 14 weeks equivalent. Most likely diagnosis a. Adenomyosis b. Uterine fibroid c. Estrogen secreting tumor d. endometriosis e. Tuboovarianabcess
6) 30/M/G6P5 admitted in active phase of labour. EFW: 3.5kg. she is obese with BMI=30. She is not hypertensive or diabetic. VE done at 3pm; cervical effacement 1cm, os 4cm, station 0. ARM done, liquor clear, CTG reactive. Review at 7pm reveals os 8cm. review at 9pm; os still 8cm, moulding 2+, CTG still reactive. Contraction 3 : 10 : 15 sec What should you do? a. advise patient for C-Sec b. prepare patients GXM c. augmentlabour with oxytocin. d. prepare patient for ventouse delivery e. review patient again after 2 hours
7) 28/G1P0 came for booking at 18 weeks POG. Urine analysis revealed glycosuria 3+. She gives no previous history of DM. What is the most appropriate thing to do at this point of time a. Repeat dipstick b. MOGTT c. d. Do blood sugar profile e. Do fasting blood sugar 8) 25 yo, G3P2@37/52 c/o abdominal pain and fresh PV bleeding. Pale and tachycardic. Uterine correspond to date &tander uterus. Dx a. Degenerative fibroid b. Uterine rupture c. Placenta abruption d. PP e. Twisted ovarian cyst 9) Primigravida came with antepartum haemorrhage< the bst to do a. Vaginal examination b. HVS c. ESR 10) Primigravida came with glucose 3+ during booking. What to do a. MOGTT b. RBS c. Start insulin d. Start diet rx e. Start metformin PMP 1) 22 years old secondary school teacher, G1P0 referred from KK Jaya Gading for blood pressure 170/110mmHg and proteinuria 4+.
LMP: 11/5/2009 Booking: 11w POA
Questions: a. Calculate EDD and POA b. 5 relevant questions in history? c. What other assessment would you obtain during dating scan? d. What findings you would like to elicit in this patient? (6m) e. List investigations you would like to order and give reasons. f. What are the complications that this patient may have? (4m) 2) 54 yomalay housewife presented to gynae clinic with hx of per vaginal bleeding for 3 months. She is para 5, children between 19 to 5yo. She has the hx taking OCP for 10 years in between her pregnancy. She has know known medical illnesses. Her husband has 3 other younger wives. One of them is being treated for HPV. Ix revealed that the mass is confined to the cervix and upper third of vagina. No invasion surrounding tissue. No LN invovlment a. Give 3 DDx b. Further hx c. List all risk factor of the patient d. Expected findings inpelvic examination e. What stage of the disease f. What is final dx g. What rx cam be offered 3) 36 yo, G4P3, referred from KK with complain of gushing of fluid per vagina and mild intermittent abd pain. LNMP was on 20/2/2012. Booking done at 12 weeks POA, US done to comform date. Her 3rd pregnancy was complicated with premature labour at 35 weeks POA a. Calculate EDD b. Stete 2 possible obs diagnoses c. Further info regarding presentation d. Expectation in PE e. List 5 ix n reason f. Outline management in this patient
LONG CASE (DR AYU)
SHORT CASE (DR RAJA ARIF) patient 22 years old g1p0, orang asli (namenye
Bed 2 (acute bed) 26y/o, G1P0 @ 33 weeks POA admitted 2 days ago for management of high blood pressure. LMP 21/9/2011 EDD 28/6/2012 Diagnosed during routine antenatal checkup. Bp high taken on 2 separate readings four hours apart. proteinuria, denied any impending eclampsia symptoms (nausea & vomiting, Headache etc). referred for stabilising of her bp. been given meds to control her bp. U/s done, no iugr all parameters normal. urine monitored as well for proteinuria. Ant hx: GDM on d/c glycosuria but not proteinuria during booking. Had to do MOGTT on next follow up. Indication: her weight, family hx of DM (father) and glycosuria during booking. result was abnormal. referred to dietician for diet ctrl. BSP done once in 2 weeks, all results normal. other ant hx uneventful. other hx macam biasa but unsignificant. Examination: oedema up to knee. hyperreflexia (maybe, ku ketuk2, laju je kaki beliau naik). Questions: 1) signs of eclampsia (show me). 2)investigation 3)drugs for PIH *banyak soalan medical, sebab signs of eclampsia
chomel). redd 26th june, calculate the maturity of her pregnancy. Instruction: examine her general apprearance and abdomen
now present. small build women. why u highlight? short stature (common in orang asli) uterus correspond to date- tell me the measurement abdomen exam findings (tak tau la betul ke x)oblique lie. why? appears distended more on the right hypochondrium. palpate, head at RHC, breech LIF. why? head hard, rounded, ballotable. est weight 1.8- 2.0 kg, liquor adequate. Question: this patient came for prem contraction. how do u manage in low risk? (investigation) speculum, HVS, assess the cervix. Then? admit to HDU. then? tocolyse, dexa complete. if still progress? beranak je la bro. 34 weeks (after complete dexa) okeh. tenkiu. habes.
cth: if uncontrolled bp-CVA, how u assess? APO- what is the sound heard in the lungs? fundoscopy etc..tapi dr banyak tlg jawab la. tq dr! (DR Muna) 38 y.o,G2P1 at EDD+2d complaint of decrease fetal movemnet 1 day PTA -Mx of pt - c-sec or not? -how to asses fetal ok or not -detail about CTG n U/S (DR MUNA) prem cntrction. Pt ade underlying gastritis, n u/s shows breech n p. Previa Dr muna tnye pasal effect of prem to baby.. Resp distress syndrom, acute necrotizing colitis n intracranial hemorhage.. doc ayu 28/G4P1+2/ @36W6D presented with contraction pain and reduced fetal movement Ddx - prem secondary to assymptomatic uti What other causes of uti Why she had mogtt. Excessive weight gain is not indication. Recurrent miscarriage What so significant bout bacteriuria Ix- urine test- how many bacteria in urine we said it is assymptomatic bacteriurea Mx- labour progress chart What her causes of miscarriage I'm lack ddx (Dr. Raja) 30 y/o, G1P0 at 10w POA admitted yesterday due (prof. Zalina) 27 y/o, G1P0, at 39w.....but SFH 34... DR RAJA reduce fetal movmen. Dr raja tanye ix to order n ape managmen utk pts... (DR Azam) middle age lady at 36w POA -examine pt abdomen. -ix -how to asses fetal well being -detail about fx of U/S
dr raja Uterus smaller than date Ddx ( dx fetus tu renal agenesis) Ix Complication of nil liquor - hypoplastic lung
to excessive vomiting 2days PTA. HOPI n booking sume ikut cm bese...cmer letih kne denied symptoms of other ddx (thyroid, liver, appendicitis, PUD, food poisoning, GTD) SYSTEMIC REVIEW kne pegi satu2 since kne exclude yg ats ddx...dr. raja xmau....systemic rview was unremarkable others history not really significant.... PE....bwat smua especially abdomen, CVS, thyroid.... IX....cm bese FBC, BUSE, UFEME n etc( jgn lpe TFT ngan LFT) ......what important of U/s in pregnant women especially in early pregnancy like this (10w)? (viable/single/multiple/etc)....kalo mcm problem in early pregnt plak....(molar/ectopic/miscarriage/etc....what expected finding?) doc; awk bwat urine dipstick td? R: errr....x doc: haisshhh...so what ur expected finding?.......ketone....why ketone? other than ketone ap lg ader dlm dehydrate ptt? Princpel MX.....(dlm clerking note ader....) final diagnosis? compilation?....have u ever heard about wernicke's encephalopathy?...blk bace....huhu threatened miscrriage.. (prof murad) - what ur ddx ( pv bleed, os closed? - bout planng family. Wut u advce -provsional diagnosis smaller thn date (dr ayu) -present! -show me how to check head prsntation? - ddx.. - investgation.. cause of uterus smaller than date? cause of oligo?.....wrong date, IUGR n IUD....no, i want other from mother........err...zzz....LL kot? huhu..... Investigation?...... Management?.....since 39w, IOL.... ok, before that... bishop score?......so her score is 9/10... dkat labour room nk wat pe?.....
- wut obimin? Wat its content? - y u worry of folic acid? Disease if folic acid def? - how u check da anemia? Show me 4 ways? - investgation? - in us wut u want to check? - if patient excessive hyperem, wut u expect? - if the patient palpitation, hypotensive? Wut u expect? - do u want to do upt? Y? - y u want to do fbc? - different between 5 miscariage? - in threatened, wut u want to confirm by clinical examination.. - if this patient, how u want to do/manage? - blablaballaaa bnyak lagi.. dr.azam Summary: mdm m, 26y/o, g1p0 @ 40 w admitted d/t gdm for IOL with no sign symptomps of labour. Quest: What is the complication of gdm to the fetus? What is the investigation for gdm? What is common assymptomatic infection in gdm? What is the normal level for bsp?how long we can know the patient diet from bsp? Fructosamine?for how long? How you would manage this pt? Before iol what do you like to do? ( Dr Azam) 29 y/o, G4P2+1 at 12 week POA c/o: PV bleeding for 1 hour duration pta - bright red in color, flooding, soaked her panties - no passing out product of conception, no blood clots, no vesicles, no foul smelling d/c - complained of dizziness, no SOB, no palpitation, no fainitng attack
Cnfirm?
prof murad Pt smaller than date. Edd is 18 mei 2012,what is her poa? What else do you want to do? If fetal heart rate cannot be heard using pinard what do you want to do? What is the cause of smaller than date? How do you estimate fetal weight? How do you assess pt liquor? What is clinical sign for iugr? Can iugr be found in edequate liquor pt? What is the common cause of smaller than date apart from wrong date? (Dr Muna) She gave me the LMP, and asked me to calculate the POA. Patient's POA is 34 week but the SFH was 30 cm. Uterus smaller than date. Questions: 1- Causes of uterus smaller than date. 2- Causes of oligohydramnios.
- no abdominal pain, no sx of UTI, no fever - no fall/trauma, no SI - history of miscarriage, D+C done - no history of molar, ectopic pregnancy, fobroids, PID - denied blood disorder in family, hyperthyroidism - no DM, no HPT Questions: 1- Ddx? 2- What other examinations would you like to do? 3- How do you differentiate between incomplete and complete miscarriage? 4- How do you differentiate between threatened and missed miscarriage? 5- Investigations? 6- Management? (Dr. Raja) 27 y/o, Malay, primigravida @29 weeks POA. LNMP = (xigt, but tpt 29 weeks) CC : Per vaginal bleeding 1 day prior to admission 1 episode, bright red in color, soaked part of her panties - no passing out product of conception, no blood clots, no vesicles, no foul smelling d/c - no dizziness, no SOB, no palpitation, no fainitng attack - no abdominal pain, no sx of UTI, no fever - no fall/trauma, SI (3 days prior to bleeding,
3- How to differentiate SGA and IUGR? 4- How do you check the fetal well being?
(Prof Zalina) 30 years old, Malay, G2 P0+1 @ 30 weeks POA history of miscarriage Presented with the complain of reduced Fetal movement
Examine the patient's abdomen
Due to poor technique the following questions were asked - How to attain SFH properly?
insignificant) - denied blood disorder in family, hyperthyroidism - no DM, no HPT Questions : What other examination would like to do? (Speculum) What would you expect to see? (with regards to your differential diagnosis?) What did she say about her past ultrascan results (there were 2, and 1 more at screening room) What investigation would you like to do? - So what did she say regarding her last USS at screening room? (said normal) - What did you ask specifically in regards to your differential diagnosis? - Where does the normal placenta lie? - What other investigation? Indeterminate APH - How you going to manage this patient? - So what advise are you going to give? (prof zalina): 31/m/G4P3 history of still birth baby(29month), risk factor of aneamia during (P) n thyroid disorder on medication C/c: per vaginal bleed 1/7 PTA.. -bleeding scanty, no ass abd pain,no fever, lupa tnya psal SI -3x admitted d/t hyperem during this (P) -moral of the story, kene detail pasal medical disorder klu ade n how its ass w the complain.. (DR MUNA)
- What are the features of the fetal head?
What investigation would you like to do?
(dr azam).. Uterus smaller than date:) dgr2 fetal heart, gaya je lebih, tp x dgr pun..hahaha
(PROF HAMIZAH) - breech + uterus smaller than
24/OA/G3P2@ 36wk5d P/W prem contraction + bacteruia for 1 days -claimed has frequency but no hematuria, dysuria or urgency antibiotic was given and frequency was rsolved but contraction still persisit -past obs- preterm delivery at 6 months due to UTI and baby was admitted to NICU for 9 months and died -was referred to htaa from rompin -currently has contraction pain 2:10 in 10 sec (time contraction jgn lpe!) -otherwise, no leaking liqour or show, fetal movement was good, cervical os still closed Q: why u dont time the contraction pain? (sy x wt, sdeyyyy T_T - doakan sy lulus) -it is to support ur dx, whether it is prem or resolved by antibiotic -what is ur ix? -in urinalysis what do u expect? -what is ur management? in this case what do u want to do =since dh 36wk5d kn allow je labour, no dexa or toco
date EDD: 29/5/12 (TODAY: 11/5/12) Q: POA? -do the exmnation to this pt (sy present cephalic, sdeyyy T_T slh lg) then doc tnjk ajar, cmne nk cri head-ballotable, in buttock presentation-firm (doc btw kt pt baby tgh duduk meniarap) doc siap tny pt nk pass kn x student ni (T_T sdey2) -what ix u want to do to rule out the cause = USS -what r the causes of breech -in breech case what is ur management= do ECV if less than 37wk or do ELSCS -why in this pt the ECV was not successful = inadequate liqour *kwn2, doakan dimurahkan rezeki sy :)
(dr dalia) mdm M, 31 y.o, Malay g4 p2+1, 29 weeks c/0 albuminuria and glucosuria, electively admitted to investigate for 24 hr proteinuria -during booking, urine and blood was normal, not raised of BP, no GDM -did not remember since when started to have albuminuria and glucosuria -denied of any symptoms of pre eclampsia, UTI -has previous history of PIH during 1st pregnancy, albuminuria in second pregnancy
(prof hamizah) patient Atrial Septal Defect, EDD- 1/7/12 -terus nervous bila dpt patient ni ingat kne buat CVS exm, last2 abdomen exm -POA? -33w -one previous scar -singleton fetus -cephalic presentation -longitudinal lie -not engage -liquor adequate -efw 2.4-2.5kg
Q: -what do u want to exclude the causes of persistence proteinuria? -what do u think the causes of proteinuria despite of during pregnancy? -can u tell me how MOGTT done? -what the risk factor of this patient to do MOGTT? -what do u want to investigate this patient? byk lg soalan, tp x ingat dah (Dr Raja) 37/OA/G3P2@33w admitted for further mx of ASD fever n cough during follow up @28w on PE murmur was heard in cvs examination referred to HTAA...no UTI sx, no palpitation, no dyspnea, no chest pain, no syncopal attack 2 prev scar, poor spacing, short stature, ejection systolic murmur on pulmonary area best heard during inspiration Q;define short stature.. what ix you want to do? what do you want to look for in us? when can we detect congenital anomalies by us? do you surprise by looking at this pt?no cyanosis bec left to right shunt how do you want to deliver the baby? antepartum, intrapartum n postpartum mx for this pt? Drmuna C/O IOL due to evidence of IUGR in twin 24 yr G2P1 at 38 Question What is the complication of twin pregnancy by first and second trimester Complication intrapartum Complication during post natal Investigation needed Management Detail about ctg Prof mokhtar 29 weeks poa On inspection, hyperpigmentation n rashes on abdomen skin Uterus correspond to date Question Question to confirm the skill The patient admitted for elevated bp 170/100. Whats ur investgx?? Whats history u want to ask. Any sign to elicit in pih (Dr Dahlia) Unstable lie@37w2d Q;1st thing u worry in unstable lie? Mx for unstable lie? Lie chart?
Epiigatric pain? What cause the pain? What do u think the rash n hyperpigmentation come from?(candida) Long case: Prof Hamizah Case: 32yo, G2P1, at EDD. She is subfertile for the last 13years and now presented because of management of Gestational Diabetes Mellitus. Questions: -Present the case -Type of subfertility and possible disease for this patient (PCOS). -Do Physical examination in front of Prof Hamizah -Management *ada lagi soalan tp lupe da :) LONG CASE (our beloved DR Dalia) mdm S, 21 y.o, Malay g2p1 (h/o stillbirth at 29 weeks) @24w POA c/o : headache, blurring of vision and nausea 1d PTA (1st episode) -upon booking, normotensive, x anemic, urinalysis revealed proteinuria, no glycosuria -denied of other symptoms of IE -no fever (ask about symp2 infx cm meningitis or encep) -no h/o seizure, no trauma -has similar hx during 1st pregnancy(still birth) last year she remained normotensive with proteinuria..then at 29w tu suddenly dpt seizure..then admitted to hospital in view of eclampsia, no fetal heart..huhu..) *Present takat hopi n past ob hx ja..p.e pon doc x suh present..agak risau...dan... 5% bersyukur.. Short case: Dr. Raja Case: 36 weeks of POA Questions: -Examine this patient -What investigation you want to do -Management
SHORT CASE (Yang Berbahagia DR Ziana) Pt mcm OA, 33w POA, case:SGA
DR : general comment of pt X : short statue DR : Do general exm n proceed with abdominal exm..Comment about pulse rate..rhythm, volume..what else? (x sempat abes general. Doc suh wat abdo trus) Palpate tapi x leh appreciate the lie n presentation..fundus pon mcm susah nk cari, SFH 30cm) *agak cuak tp yg bestnya doc x suh present pon..wee DR : It it difficult to appreciate? Y?? X: err, polyhydramnion, IUGR or SGA.. DR : is it normal to be admitted at 32w? Why do u think the pt prob? X : might be due to severe IUGR kot..
Q: -regarding ultrasound, when is d most accurate. -CRL up to bpa mggu, then proceed with parameter pa (HC, AC, BPD, FL) -prob of this patient? -Upon admission what hv been done? (lupa tanya la weii!!, doc agk keciwa) if this patient come to u msa kat emergency, what u want to do? -Is it possible to have proteinuria with normal BP..at how many week we diagnosed pt as having pre-elampsia? Protenuria bpe? If from urine dipstick bpe? -Ask details bout mg sulphate..(most of them x leh jwb pon, doc frust lagi..rupa2nya budak2 ni ckp doc yg ajaq psai menda alah ni.hue) -Toxicity of mg sulphate -In this pt, do u think it is PIH or other underlying medical illness? List the med illness.. -what d importance kita detect proteinuria early of pregnancy? -investigate? Management-very superficial.. byk lg soalan, tp x ingat dah
DR : amboi, severe ja?? IUGR biasa2 x yah ke? X : bkn2, suma IUGR kna msok.. DR : do u notice this scar?? (suprapubic scar) what are the cause for pt to hv this type of scar?? X : LSCS DR : kalo this type of scar mmg LSCS ja ka?? X : nope..bley ja classical pong..pastu myomectomy, hysterectomy.. DR : hah, hysterectomy? X : bg contoh je..kalo da hysterectomy,cmna gaya pt leh ngandung..hee DR : what else?? X : hhhmmmmmmm..ape lg ye..appendicectomy..??! hmm (cacat pegi sebot) DR : appendicectomy?? X : eh, bukan2..appendicectomy yg grid iron scar tu.. DR : nasib baek agi..kalo x, mmg dah ketok hang.. (bkpe doc ckp utagha ni) X : haha..sori doc..tq
Você também pode gostar
- Octaseeds Rise Review Posttest Compilation 120qDocumento19 páginasOctaseeds Rise Review Posttest Compilation 120qAngela Saldajeno100% (3)
- Obstetric ExamDocumento35 páginasObstetric ExamRafi MahandaruAinda não há avaliações
- Medical School Companion Obstetrics and Gynecology Practice Question BookNo EverandMedical School Companion Obstetrics and Gynecology Practice Question BookAinda não há avaliações
- Obs UM Paper 2Documento16 páginasObs UM Paper 2Muhammad Abbas AliAinda não há avaliações
- Ats Menjawab Super Brankas Soal Unas 2020-2015Documento424 páginasAts Menjawab Super Brankas Soal Unas 2020-2015anton suponoAinda não há avaliações
- Juli 2022Documento28 páginasJuli 2022Chynthea ParamithaAinda não há avaliações
- ObstetricsDocumento92 páginasObstetricsMARK ARTHUR MARTINEZ100% (1)
- SURAT CINTA ULM 2022 + JawabanDocumento25 páginasSURAT CINTA ULM 2022 + JawabanBerry BancinAinda não há avaliações
- UNAS Nov 2019Documento25 páginasUNAS Nov 2019paramitastellaAinda não há avaliações
- DR Nadine Rev All (Samra's Edition)Documento313 páginasDR Nadine Rev All (Samra's Edition)Cyril I.Makar100% (1)
- Obstetrics MukundaDocumento48 páginasObstetrics Mukundadocivirus100% (1)
- ATS Menjawab Soal UKN Maret 2021 HQQDocumento18 páginasATS Menjawab Soal UKN Maret 2021 HQQanton suponoAinda não há avaliações
- Juli 2021Documento39 páginasJuli 2021Chynthea ParamithaAinda não há avaliações
- Soal Regarding Menoupause ConditionDocumento6 páginasSoal Regarding Menoupause ConditionfeliaAinda não há avaliações
- OBG Question DiscussionDocumento19 páginasOBG Question DiscussionNesreden Jemal KedirAinda não há avaliações
- MCQ Remake Group A 2022Documento16 páginasMCQ Remake Group A 2022V Sugrim100% (1)
- MCQ 21Documento8 páginasMCQ 21irynAinda não há avaliações
- D. Central Venous PressureDocumento9 páginasD. Central Venous Pressuredaniel_alexander_susenoAinda não há avaliações
- UNAS 59th (NOV 2020) FIXDocumento23 páginasUNAS 59th (NOV 2020) FIXmhariskurniawanAinda não há avaliações
- Mid Eval JCDocumento8 páginasMid Eval JCiglesiasowenAinda não há avaliações
- OB-GYNE Final Exam Aug-Sept 2019Documento21 páginasOB-GYNE Final Exam Aug-Sept 2019Alfonso Martin Plantilla100% (1)
- Soal SoalDocumento3 páginasSoal SoalfirmianisaAinda não há avaliações
- Unas November 2019Documento21 páginasUnas November 2019Muhammad FaisalAinda não há avaliações
- CDocumento31 páginasCHambrian Wijaya100% (1)
- Y3b1 Ong Groupb B - 13Documento5 páginasY3b1 Ong Groupb B - 13Akmal ZaimAinda não há avaliações
- Obs-UM - Paper - 1Documento16 páginasObs-UM - Paper - 1Muhammad Abbas AliAinda não há avaliações
- Contoh Soal FetomaternalDocumento10 páginasContoh Soal FetomaternalBella AgustinAinda não há avaliações
- Ectopic PregnancyDocumento54 páginasEctopic Pregnancypatriciaatan1497Ainda não há avaliações
- Choose The Most Accurate Single Answer: (1 Mark Each)Documento9 páginasChoose The Most Accurate Single Answer: (1 Mark Each)Salmonella TyphiAinda não há avaliações
- AttachmentDocumento10 páginasAttachmentdheasuyuthiAinda não há avaliações
- USULDocumento6 páginasUSULdika putrayudaAinda não há avaliações
- Ospe Bank PDFDocumento318 páginasOspe Bank PDFMed StudentAinda não há avaliações
- A 18-Year-Old G1 at 30 4/7 Weeks Presents For Her Scheduled Obstet Ric (OB) Appointment. A 28-Week Ultrasound Showed The Fetus To BDocumento13 páginasA 18-Year-Old G1 at 30 4/7 Weeks Presents For Her Scheduled Obstet Ric (OB) Appointment. A 28-Week Ultrasound Showed The Fetus To BHambrian WijayaAinda não há avaliações
- Obs 1 Bleeding in Early Pregnancy QuestionsDocumento9 páginasObs 1 Bleeding in Early Pregnancy QuestionsSalmonella TyphiAinda não há avaliações
- Tes PanoramaDocumento57 páginasTes Panoramamuttaqin95Ainda não há avaliações
- Ats Menjawab Soal Unas November 2021 EditedDocumento26 páginasAts Menjawab Soal Unas November 2021 Editedanton suponoAinda não há avaliações
- 10-OBGYN-Glory GroupDocumento46 páginas10-OBGYN-Glory Groupanmar alkhudhriAinda não há avaliações
- Obgyn Questions 1-100Documento26 páginasObgyn Questions 1-100Fika AmaliaAinda não há avaliações
- Jan 12 - SarahDocumento16 páginasJan 12 - Sarahrayyan212121Ainda não há avaliações
- Jointly Team: SMLE GroupDocumento11 páginasJointly Team: SMLE GroupAkpevwe EmefeAinda não há avaliações
- Practice Test: Order Your Manuals NowDocumento31 páginasPractice Test: Order Your Manuals NowTadele DerbewAinda não há avaliações
- Exam MohemDocumento7 páginasExam Mohemnada elfarraAinda não há avaliações
- Unas Agustus 2017Documento18 páginasUnas Agustus 2017Dewi Arianti BudiantoAinda não há avaliações
- OBS Oral Sheet Not AnsweredDocumento5 páginasOBS Oral Sheet Not AnsweredMuhammed MostafaAinda não há avaliações
- Gynae and ObsDocumento71 páginasGynae and ObsmarviAinda não há avaliações
- 11 16Documento27 páginas11 16Iful SaifullahAinda não há avaliações
- PLAB Obs Gyne MCQsDocumento33 páginasPLAB Obs Gyne MCQsHenrypat Uche Ogbudu100% (3)
- Obstetric and Gynecology: A. ColpotomyDocumento44 páginasObstetric and Gynecology: A. ColpotomyAloah122346100% (1)
- Mcqs - Obstetrics and Gynaecology (For Post Graduate Preparing For FNB and Professionals) Obstetrics and GynaecologyDocumento27 páginasMcqs - Obstetrics and Gynaecology (For Post Graduate Preparing For FNB and Professionals) Obstetrics and GynaecologyAnonymous kQCQ30Rq5OAinda não há avaliações
- Juli 2019Documento21 páginasJuli 2019Chynthea ParamithaAinda não há avaliações
- T and DDocumento24 páginasT and DBakana6Ainda não há avaliações
- MCCQE - 1 - November 2003 1. For Nocturnal Enuresis How Long You ...Documento71 páginasMCCQE - 1 - November 2003 1. For Nocturnal Enuresis How Long You ...Vinil SaratchandranAinda não há avaliações
- Final SCS 2023 - ObsGyne Child BlockDocumento8 páginasFinal SCS 2023 - ObsGyne Child Blocks129682Ainda não há avaliações
- Unas UnsriDocumento29 páginasUnas UnsriMuhammad DasawarsaAinda não há avaliações
- Jointly Team: SMLE GroupDocumento22 páginasJointly Team: SMLE GroupAkpevwe EmefeAinda não há avaliações
- UNAS Ob Surabaya 2017Documento31 páginasUNAS Ob Surabaya 2017Zurya UdayanaAinda não há avaliações
- Obst 8 - All Obstetrics 4 2021Documento28 páginasObst 8 - All Obstetrics 4 2021Menna KamalAinda não há avaliações
- Parts of The Body and Health ProblemDocumento13 páginasParts of The Body and Health ProblemSonia Tri AgustinaAinda não há avaliações
- Guru AppointmentDocumento2 páginasGuru AppointmentKirankumar MutnaliAinda não há avaliações
- Fey Lougawou (Wonder of The World Plant)Documento7 páginasFey Lougawou (Wonder of The World Plant)Salomon YvesAinda não há avaliações
- Seema Jain CV 2013Documento3 páginasSeema Jain CV 2013api-152953067Ainda não há avaliações
- The Enigma of Facial Beauty: Esthetics, Proportions, Deformity, and ControversyDocumento6 páginasThe Enigma of Facial Beauty: Esthetics, Proportions, Deformity, and ControversyIsmaelLouGomezAinda não há avaliações
- Dorset County Hospital NHS Foundation TrustDocumento1 páginaDorset County Hospital NHS Foundation TrustRika FitriaAinda não há avaliações
- Journal Reading Radiologi EllaDocumento44 páginasJournal Reading Radiologi EllaElla Putri SaptariAinda não há avaliações
- Jurnal Ria Suak 091511195Documento6 páginasJurnal Ria Suak 091511195resyaAinda não há avaliações
- Upper Respiratory Tract InfectionDocumento3 páginasUpper Respiratory Tract Infectionmcvirgo014100% (1)
- At The PharmacyDocumento6 páginasAt The PharmacyCristian González GonzálezAinda não há avaliações
- Fact Sheet: StutteringDocumento2 páginasFact Sheet: StutteringHaley TutwilerAinda não há avaliações
- Metatron Resonance Brochure WebsiteDocumento3 páginasMetatron Resonance Brochure WebsiteShaun DennisAinda não há avaliações
- Acute and Chronic CholecystitisDocumento10 páginasAcute and Chronic Cholecystitisissam_1994Ainda não há avaliações
- Nabh Entry LevelDocumento64 páginasNabh Entry LevelRenuka MuruganAinda não há avaliações
- DAFTAR PUSTAKA Rachel ParasianDocumento3 páginasDAFTAR PUSTAKA Rachel ParasianAnto TomodachiRent SusiloAinda não há avaliações
- Marinedrugs 17 00636 PDFDocumento24 páginasMarinedrugs 17 00636 PDFNindah IkaAinda não há avaliações
- Radial Head FractureDocumento40 páginasRadial Head FractureammarAinda não há avaliações
- Introductory Lecture Series: The Anesthesia MachineDocumento37 páginasIntroductory Lecture Series: The Anesthesia MachineDenny RamdhanAinda não há avaliações
- Dilip K. Ghosh, R. B. Smarta-Pharmaceuticals To Nutraceuticals - A Shift in Disease Prevention-Taylor & Francis - CRC Press (2017)Documento274 páginasDilip K. Ghosh, R. B. Smarta-Pharmaceuticals To Nutraceuticals - A Shift in Disease Prevention-Taylor & Francis - CRC Press (2017)davidAinda não há avaliações
- WhoDocumento64 páginasWhoIga AfifahAinda não há avaliações
- AKUH Kampala Hospital-Press Release - Final - 17 December 2015Documento3 páginasAKUH Kampala Hospital-Press Release - Final - 17 December 2015Robert OkandaAinda não há avaliações
- Evaluation of Anti-Inflammatory Effect of Ashwagandha: A Preliminary Study in VitroDocumento3 páginasEvaluation of Anti-Inflammatory Effect of Ashwagandha: A Preliminary Study in VitroAmmar Ali KhanAinda não há avaliações
- Critical Care Medicine An Algorithmic Approach 2023Documento335 páginasCritical Care Medicine An Algorithmic Approach 2023Ahmed AbusalabAinda não há avaliações
- Buffer Systems in The Body: Protein Buffers in Blood Plasma and CellsDocumento11 páginasBuffer Systems in The Body: Protein Buffers in Blood Plasma and CellsK Jayakumar KandasamyAinda não há avaliações
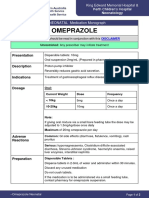
- OmeprazoleDocumento2 páginasOmeprazolephawphawphawAinda não há avaliações
- Community Pharmacy Organization: Pharmaceutical Management.Documento12 páginasCommunity Pharmacy Organization: Pharmaceutical Management.pawannnnAinda não há avaliações
- Infochap10 12Documento18 páginasInfochap10 12Nareeza AbdullaAinda não há avaliações
- Biology Investigatory Project: TopicDocumento13 páginasBiology Investigatory Project: TopicRaj SahuAinda não há avaliações
- Case Study - DR EldaDocumento3 páginasCase Study - DR EldaShashi KumarAinda não há avaliações
- Arthritis Protocol 1Documento11 páginasArthritis Protocol 1Co Bay-AgiAinda não há avaliações
- Healing PCOS: A 21-Day Plan for Reclaiming Your Health and Life with Polycystic Ovary SyndromeNo EverandHealing PCOS: A 21-Day Plan for Reclaiming Your Health and Life with Polycystic Ovary SyndromeAinda não há avaliações
- The Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouNo EverandThe Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouAinda não há avaliações
- The Longevity Book: The Science of Aging, the Biology of Strength, and the Privilege of TimeNo EverandThe Longevity Book: The Science of Aging, the Biology of Strength, and the Privilege of TimeNota: 3.5 de 5 estrelas3.5/5 (13)
- What to Expect When You’re Expecting (5th Edition)No EverandWhat to Expect When You’re Expecting (5th Edition)Nota: 5 de 5 estrelas5/5 (1)
- Awakening Fertility: The Essential Art of Preparing for PregnancyNo EverandAwakening Fertility: The Essential Art of Preparing for PregnancyNota: 4.5 de 5 estrelas4.5/5 (36)
- All in Her Head: The Truth and Lies Early Medicine Taught Us About Women’s Bodies and Why It Matters TodayNo EverandAll in Her Head: The Truth and Lies Early Medicine Taught Us About Women’s Bodies and Why It Matters TodayNota: 4.5 de 5 estrelas4.5/5 (3)
- Crones Don't Whine: Concentrated Wisdom for Juicy WomenNo EverandCrones Don't Whine: Concentrated Wisdom for Juicy WomenNota: 2.5 de 5 estrelas2.5/5 (3)
- Skinny Bitch: A No-Nonsense, Tough-Love Guide for Savvy Girls Who Want to Stop Eating Crap and Start Looking Fabulous!No EverandSkinny Bitch: A No-Nonsense, Tough-Love Guide for Savvy Girls Who Want to Stop Eating Crap and Start Looking Fabulous!Nota: 3.5 de 5 estrelas3.5/5 (489)
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisNo EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisNota: 3 de 5 estrelas3/5 (2)
- Breaking Free from Body Shame: Dare to Reclaim What God Has Named GoodNo EverandBreaking Free from Body Shame: Dare to Reclaim What God Has Named GoodNota: 5 de 5 estrelas5/5 (33)
- Natural Hospital Birth: The Best of Both WorldsNo EverandNatural Hospital Birth: The Best of Both WorldsNota: 5 de 5 estrelas5/5 (33)
- The Menopause Manifesto: Own Your Health With Facts and FeminismNo EverandThe Menopause Manifesto: Own Your Health With Facts and FeminismNota: 4 de 5 estrelas4/5 (18)
- Medical Bondage: Race, Gender, and the Origins of American GynecologyNo EverandMedical Bondage: Race, Gender, and the Origins of American GynecologyNota: 4.5 de 5 estrelas4.5/5 (75)
- Women, Food, And Hormones: A 4-Week Plan to Achieve Hormonal Balance, Lose Weight, and Feel Like Yourself AgainNo EverandWomen, Food, And Hormones: A 4-Week Plan to Achieve Hormonal Balance, Lose Weight, and Feel Like Yourself AgainNota: 4 de 5 estrelas4/5 (14)
- The Pain Gap: How Sexism and Racism in Healthcare Kill WomenNo EverandThe Pain Gap: How Sexism and Racism in Healthcare Kill WomenNota: 4 de 5 estrelas4/5 (154)
- Pregnancy Hacks: 350+ Easy Hacks for a Happy and Healthy Pregnancy!No EverandPregnancy Hacks: 350+ Easy Hacks for a Happy and Healthy Pregnancy!Nota: 5 de 5 estrelas5/5 (1)
- The Hormone Secret: Discover Effortless Weight Loss and Renewed Energy in Just 30 DaysNo EverandThe Hormone Secret: Discover Effortless Weight Loss and Renewed Energy in Just 30 DaysNota: 4.5 de 5 estrelas4.5/5 (5)
- Younger Next Year, 2nd Edition: Live Strong, Fit, Sexy, and Smart-Until You're 80 and BeyondNo EverandYounger Next Year, 2nd Edition: Live Strong, Fit, Sexy, and Smart-Until You're 80 and BeyondNota: 4 de 5 estrelas4/5 (111)
- A Radical Guide for Women with ADHD: Embrace Neurodiversity, Live Boldly, and Break Through BarriersNo EverandA Radical Guide for Women with ADHD: Embrace Neurodiversity, Live Boldly, and Break Through BarriersNota: 4.5 de 5 estrelas4.5/5 (72)
- Hormone Balance: A Woman's Guide to Restoring Health and VitalityNo EverandHormone Balance: A Woman's Guide to Restoring Health and VitalityNota: 5 de 5 estrelas5/5 (3)
- Not a Diet Book: Take Control. Gain Confidence. Change Your Life.No EverandNot a Diet Book: Take Control. Gain Confidence. Change Your Life.Nota: 4.5 de 5 estrelas4.5/5 (124)
- Bumpin': The Modern Guide to Pregnancy: Navigating the Wild, Weird, and Wonderful Journey From Conception Through Birth and BeyondNo EverandBumpin': The Modern Guide to Pregnancy: Navigating the Wild, Weird, and Wonderful Journey From Conception Through Birth and BeyondNota: 4.5 de 5 estrelas4.5/5 (3)
- Period Power: Harness Your Hormones and Get Your Cycle Working For YouNo EverandPeriod Power: Harness Your Hormones and Get Your Cycle Working For YouNota: 4 de 5 estrelas4/5 (25)
- Bumpin': The Modern Guide to Pregnancy: Navigating the Wild, Weird, and Wonderful Journey From Conception Through Birth and BeyondNo EverandBumpin': The Modern Guide to Pregnancy: Navigating the Wild, Weird, and Wonderful Journey From Conception Through Birth and BeyondNota: 4.5 de 5 estrelas4.5/5 (39)
- Period Repair Manual: Natural Treatment for Better Hormones and Better Periods, 2nd editionNo EverandPeriod Repair Manual: Natural Treatment for Better Hormones and Better Periods, 2nd editionNota: 4.5 de 5 estrelas4.5/5 (28)
- Hypnobirthing: Hypnotherapy for Happy, Healthy MindsNo EverandHypnobirthing: Hypnotherapy for Happy, Healthy MindsNota: 5 de 5 estrelas5/5 (8)
- Mindful Birthing: Training the Mind, Body, and Heart for Childbirth and BeyondNo EverandMindful Birthing: Training the Mind, Body, and Heart for Childbirth and BeyondNota: 4 de 5 estrelas4/5 (15)
- Intoxicating Lies: One Woman’s Journey to Freedom from Gray Area DrinkingNo EverandIntoxicating Lies: One Woman’s Journey to Freedom from Gray Area DrinkingNota: 5 de 5 estrelas5/5 (1)