Escolar Documentos
Profissional Documentos
Cultura Documentos
DF
Enviado por
Vendi Cahyadi RiandikaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
DF
Enviado por
Vendi Cahyadi RiandikaDireitos autorais:
Formatos disponíveis
Pediatr Clin N Am 49 (2002) 1339 1368
Emerging cancer-targeted therapies
Robert J. Arceci, MD, PhDa,*, Timothy P. Cripe, MD, PhDb
Departments of Oncology and Pediatrics, Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins, 1650 Orleans Street, Room 2M51, Baltimore, Maryland, USA b Division of Hematology/Oncology, Cincinnati Childrens Hospital Medical Center, University of Cincinnati, 3333 Burnet Avenue, Cincinnati, Ohio, USA
a
In a perfect world there would be no cancer. Fantasy? Definitely, at least in the foreseeable future. The next best thing to no cancer would be cancer therapy that is so effective and specific that normal tissues are not harmed, yielding cures without side effects. Science fiction? Perhaps. Yet there is reason to believe that the unfolding revolution in molecular biology and translational research will allow selective targeting of tumor cells and radically change the way general practitioners and pediatric oncologists treat and follow children with cancer. This article highlights some of the most promising approaches being tested in the field. By learning about the underlying biology, the remaining hurdles, the projected timeline, and the possible impact of new therapies on the practice of pediatric oncology, health care professionals and patients should be better prepared for the future of pediatric oncology. Advances in targeted cancer therapy can be broadly categorized as (1) biologic retooling and (2) molecular intervention. Biologic retooling refers to strategies seeking to harness biologic systems that have already evolved specifically to destroy cells by redirecting these processes to cancer cells. Examples include immunotherapy and cancer vaccines, which seek to aim immunologic defense mechanisms at cancer cells rather than at microorganisms. Some microbes themselves have developed sophisticated and efficient methods to commandeer and destroy eukaryotic cells as part of their life cycle, processes that can now be specifically aimed at cancer cells. Molecular intervention encompasses a vast array of agents designed to interfere at the molecular level with cellular processes required for growth and division. Such agents run the gamut from small molecules to sequence-specific nucleic acids, whole genes, and proteins. The
* Corresponding author. Johns Hopkins Oncology Center, Bunting-Blaustein Cancer Research Building, 1650 Orleans Street, Room 2M51, Baltimore, Maryland 21231. E-mail address: arcecro@jhmi.edu (R.J. Arceci). 0031-3955/02/$ see front matter D 2002, Elsevier Science (USA). All rights reserved. PII: S 0 0 3 1 - 3 9 5 5 ( 0 2 ) 0 0 0 9 6 - 2
1340
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
adage know your enemy is apt; as each critical molecular process selective for a cancer cell is elucidated, so follows intentional means of intervention.
Biologic retooling Immunotargeting and monoclonal antibody therapy Over 25 years ago Kohler and Milstein [1] first developed the methods to generate antibodies from single clones by fusing murine B cells with nonsecreting myeloma tumor cells. The result was a hybrid cell, termed a hybridoma, that secreted a single antibody, termed a monoclonal antibody (Mab), with unique specificity. The enormous potential of this discovery was rapidly recognized and created hope that such antibodies would fulfill Erhlichs dream of targeted magic bullets to treat cancer. Unfortunately, reality dictated that many obstacles would need to be overcome in order to make such a hope a reality. One of the first challenges was to identify antibodies with sufficient tumor specificity and binding affinity. Doing so has been quite difficult, in part because of the large number of antigens shared by tumor cells and normal tissues. One way around this problem has been the realization that the potential toxicity from such cross-reactivity might be minimized if the normal cell population could be repopulated from progenitor cells or if the cross-reactive tissues were not essential for vital functions. In other situations, a differential level of antigen may be expressed so that tumor cells show a much higher level of a particular antigen than normal cells, thus resulting in a differential binding profile. Nevertheless, extensive testing of antigen expression in human tissues is important when evaluating any monoclonal antibody for in vivo testing. This importance was particularly well demonstrated in the early clinical development of Mabs with the use of anti-CD10, an antibody directed against the common acute lymphoblastic leukemia (ALL) antigen (CALLA) expressed on ALL blasts but also on renal tubular cells [2,3]. Another critical requirement for the successful use of Mabs is that their recognized antigen should be expressed on the surface of the cells of interest. Internalization of the antibody after binding the antigen is also usually an advantage, allowing the delivery of a toxin to the targeted cell. Antigens that do not internalize upon binding of the Mab may also be useful for delivering targeted radioactivity; in addition, such stable antigens may serve as excellent targets for antibody-dependent cellular cytotoxicity (ADCC) through Fc region binding of receptors present on effector cells. Another use of stable antigens is with Mabs coupled with effector cytokines, such as interleukin 2 (IL-2) or granulocyte-macrophage colony-stimulating factor (GM-CSF) [4,5]. On binding to the target cells, the chimeric antibody-cytokine conjugates then recruit and activate other effector cells. Antigens that are rapidly shed from the surface of cells are less likely to be useful therapeutic targets. Following the initial uses of murine Mabs in patients, it became clear that patients were able to develop human antimouse antibodies (HAMA) that can
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1341
cause severe allergic reactions and, in some cases, can neutralize the Mabs activity. Although some patients being treated for cancer may not be able to make HAMA, a significant number are able to generate these immune responses [6,7]. To minimize and possibly avoid this generation of HAMA, several different approaches have been used more recently to generate humanized antibodies. For example, using genetic engineering approaches, one can generate chimeric Mabs that retain the murine variable region with framework regions derived from human amino acid sequence. The degree of humanization can vary a great deal when constructing such molecules, ranging from antibodies that utilize human constant regions combined with entire murine variable regions to antibodies that contain only the hypervariable murine sequences. Such humanized Mabs are usually significantly less immunogenic and can often be used repeatedly to treat patients [8]. More recently, transgenic mice have been generated which have had their murine immunoglobulin genes replaced by human counterparts, allowing them to generate only human antibodies [9,10]. This approach could substantially enhance the ability to make humanized Mabs. Another approach to generating Mabs to specific tumor antigens has used the technique of screening recombinatorial phage libraries generated from B-cell cDNAs. These libraries consist of billions of phages, each of which expresses a filament protein that has been engineered to encode a variable region of a human antibody sequence that can bind to specific antigenic epitopes. Such libraries can be screened using tumor cells versus normal cell counterparts to isolate phages that selectively bind to the tumor cells. Once isolated, the phage can be used to infect bacteria, in which the phages are allowed to multiply to large numbers. The phages are subsequently purified, and the gene encoding the filamentous protein is sequenced, along with the variable region. These phages can thus be used to develop single-chain or chimeric antibodies for clinical use. An interesting alternative approach to isolating such tumor-selective or -specific antibodies involves the infusion of an entire phage library into an animal or patient harboring a tumor, then surgically removing the tumor and isolating the phage from the specimen. Several phase I trials have been performed to begin to test the utility of such phage-derived antibodies in patients with cancer [11 17]. An unexpected potential benefit from Mab therapy has been the development of anti-idiotype antibodies and anti-anti-idiotype networks that result in antitumor responses [6,7]. There are two basic approaches for using Mabs as immunogens. First, an antibody made by a tumor cell is used as an immunizing antigen. For example, B-cell lymphomas express a unique surface immunoglobulin that can be used to immunize patients against their own tumors [18,19,20]. The feasibility of this approach was demonstrated when specific malignant B-cell immunoglobulin variable regions (idiotypes) were cloned from individual patient tumors. After several courses of chemotherapy and with time allowed for immune recovery, patients were vaccinated with their own tumor idiotype and given the immunostimulatory cytokine, GM-CSF. Most immunized patients developed significant cytotoxic T-cell and antibody-mediated antitumor responses. Some anti-idiotype immune responses resulted in the elimination of minimal residual disease [21].
1342
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
Another approach to the development of anti-idiotypic responses has been based on Jernes original hypothesis of immune networking. This hypothesis is based on the findings that an immune response to a foreign antigen will elicit a specific antibody response. The binding site of the antitumor antigen antibody, however, can also serve as an antigen (ie, an idiotype antigen), which, in turn, can generate a secondary antibody response. The idiotype is really an internal image of the original tumor antigen; thus, the anti-idiotype antibody, when it further serves as an immunogen, can generate a third or anti-anti-idiotype response. This antianti-idiotype response, because it is directed toward the internal antigen image of the anti-idiotype antibody, can also recognize the original tumor antigen. This sequence of events has been demonstrated in a variety of experimental systems as well as in patients. In particular, the use of anti-GD2 antibodies in patients with melanoma and neuroblastoma has been relatively well studied, and anti-idiotype vaccine approaches are being tested in patients [6,7,19,22 25]. Although it has taken over 2 decades to understand better how to generate and use Mabs, recent studies have demonstrated that these antibodies can provide effective and relatively nontoxic anticancer therapy. For example, clinical efficacy has been demonstrated in lymphoid malignancies with antibodies to CD19 and CD20 as well as with T-cell selective antigens such as CD7 [26 29]. Myeloid malignancies have been successfully targeted with toxin-conjugated or radiolabeled anti-CD33 Mabs [30,31]. Several solid tumors have also been treated with antibodies, such as gastrointestinal tumors with anti-CEA Mabs [32], breast cancer with anti HER-2/neu Mabs [33,34], and other epithelial-derived tumors with anti epithelial growth factor (EGF) receptor Mabs. [35,36]. Of particular interest is the observation that some antibodies, such as those to HER-2/neu, also sensitize tumor cells to cisplatin. Chemosensitization has also been observed with the use of chemotherapy and anti CD20-ricin conjugates as well as with Mabs with the ability to inhibit multiple drug resistance-1 (MDR1) P-glycoprotein drug efflux transporter [37]. In terms of the inhibition of MDR1 or related drug efflux pumps, small molecule inhibitors have also been extensively tested, including a recently completed Pediatric Oncology Group trial (POG 9421) in children with acute myelogenous leukemia (AML) [38 42]. A challenge for the future will be how to optimize antibody-directed therapies to improve overall patient outcomes. Some antibodies have shown efficacy as single agents, either as a native antibody (such as anti-CD20 in lymphoid malignancies) or as an antibody-toxin conjugate (such as anti CD33-calicheamicin in AML) [30,31,43]. Anti-GD2 antibodies have been shown to clear chemotherapy-refractory neuroblastoma in the bone marrow of patients [4,25,44]. A critical issue, however, is whether antibodies directed against such differentiation antigens will effectively target the malignant stem cell or whether they will serve as only cytoreductive agents. In the case of AML, it is highly likely that the target antigen, CD33, is not present on the leukemic stem cell in many subtypes of AML. In other subtypes, such as acute promyelocytic leukemia (APL), CD33 may be an excellent target by which the leukemic stem cell might be eradicated. Thus, a pilot study in
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1343
adults with APL has attempted to eliminate conventional chemotherapy from the treatment regimen by using all transretinoic acid (ATRA) combined with anti CD33-calicheamicin, leading to prolonged remissions in a small number of adult patients [45]. Although eliminating conventional chemotherapy is a bold step and thus far is appropriate only for a subset of patients with APL, the possibility of cure without conventional chemotherapy for a subtype of AML is something that could only be dreamed about 20 years ago. Tumor-targeted antibodies will most likely be tested in combination with chemotherapy or as postremission therapy in an attempt to eliminate minimal residual disease. The efficacy of combining Mabs as native or conjugated molecules with chemotherapy is in the early stages of clinical investigation. The utility of Mabs following conventional cytotoxic therapy will depend on the capacity of the antibody to react to antigens present on the malignant stem cell and not on their partially differentiated progeny. Using the approach of postremission antibody therapy makes little sense if this requirement cannot be met. In addition, the degree to which antibody-mediated treatments spare normal tissues will depend on their specificity for unique tumor antigens. Antitumor immunostimulatory therapies The potential for stimulating immune responses to tumors in patients had important beginnings with the work of Dr. William Coley as early as the late 1800s [46,47]. His work was based on the observation that in some patients with cancer, tumor regression was associated with bacterial infections. He subsequently developed crude bacterial extracts, termed Coleys toxins, which were used to immunize patients. This type of immune stimulation was difficult to control and, thus, unpredictable in terms of expected responses or side effects. Some objective responses were observed, however. It is likely that such approaches, including the subsequent trials with Bacillus of Calmette and Guerin (BCG) immunostimulation, resulted in the enhancement of innate immune responses, primarily dependent on macrophage and dendritic cell activation followed by cytokine stimulation of lymphocytes and eosinophils. Another related approach has arisen from the observation that the lipophilic agent, muramyl tripeptide phosphatidylethanolamine (MTP-PE), can produce substantial activation of mononuclear phagocytes. This activation then leads to increased expression of a number of immunostimulatory cytokines such as IL-1, IL-2, IL-7, IL-8 IL-12, interferon gamma, and tumor necrosis factor [48 50]. Observations using a dog model of osteosarcoma demonstrated the clinical utility of exposure to MTP-PE following resection of primary tumors. These observations then led to clinical trials culminating in a randomized, phase III trial in patients with osteosarcoma. Results from this trial have been inconclusive in terms of any benefit resulting from MTP-PE alone; the only significant benefit was observed in patients who received MTP-PE plus ifosfamide. Pathologic findings of metastatic lesions demonstrated significant infiltration with inflammatory cells in patients who received MTP-PE [51].
1344
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
Although these general approaches to stimulating innate immunity to generate antitumor responses have not been exceptionally successful, they have led to the belief that more potent and specific forms of immunostimulation might result in more consistent responses. The next phase in this approach was the use of immunostimulatory cytokines. For example, the administration of IL-2 has been shown to achieve significant responses in patients with renal cell carcinoma, melanoma, and less often in AML [28,52 54]. A randomized trial of IL-2 in the postremission period of therapy for pediatric patients with AML is currently being carried out with the Childrens Cancer Group 2961 trial. Whether other cytokines, used alone or in combination, can be more effective remains uncertain. Unfortunately, systemic exposure of patients to some immunostimulatory cytokines (eg, IL-2) has also resulted in significant adverse side effects, such as pulmonary capillary leak syndrome, renal insufficiency, and neutrophil dysfunction [54]. Clearly, the use of these approaches is not particularly targeted and could be considered similar to approaches with conventional chemotherapy, although directed at antitumor immunostimulation. Thus, from the point of view of selective antitumor therapy, these strategies may be most important in identifying more specific pathways of antitumor immune responses. Cancer vaccines Although a means for directing patients immune system to fight off their own cancers has been sought for many years, only relatively recently have several important discoveries pointed the way to formally and definitively testing this possibility. Critical to this effort has been the development of inbred strains of mice. Such mouse strains allowed definitive experiments to be done that proved the fundamental importance of the major histocompatibility (MHC) locus in both tissue graft rejection and immunogenicity. The work of Gross and Foley [55,56] demonstrated that active immunization with a variety of methylcholanthrene (MC)-induced tumors in inbred strains of mice could generate clearly effective antitumor responses. During the 1960s and 1970s, immunostimulatory antigens on murine leukemias, derived from infection with leukemogenic viruses, were identified [57]. Subsequently, both molecular and biochemical methods were developed to identify immunostimulatory tumor antigens, first in murine and then in human tumors [58 60]. These antigens usually include (1) normal differentiation antigens, (2) genes expressed during early embryonic development whose expression reappears following malignant transformation, (3) mutated protooncogenes or fusion proteins generated by gene and chromosomal abnormalities, and (4) viral-derived proteins [61,62]. In addition to these advances, a more fundamental understanding of the biologic requirements for specific T-lymphocyte activation has been salient to cancer vaccine development. The process by which T lymphocytes become activated is now recognized to depend on mechanisms regulating cell-cell
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1345
adhesion, antigen presentation (usually by either MHC class I or class II molecules), T-cell receptor recognition of the antigen, and, lastly, costimulatory signals involving specific cell surface receptors on antigen representing cells (eg, dendritic cells) or on tumor cells [63,64]. The incorporation of these discoveries into strategies for tumor vaccine development has resulted in several different approaches that have been shown to be effective in murine models and are now being tested in patients [61,65]. These approaches have been developed for ex vivo immunostimulation of tumorreactive T cells as well as with active in vivo vaccination [66 69]. The responses observed to the infusion of donor lymphocytes for relapses following bone marrow transplantation in patients with chronic myelogenous leukemia (CML) and, to a less extent, in patients with AML and ALL have shown that effective antitumor responses can be generated from the passive infusion of allogeneic T cells. Of course, these T-cell populations are not tumorspecific and are, therefore, often associated with the development of significant degrees of graft-versus-host disease [70,71]. The incubation of autologous or allogeneic T cells with whole tumor cells, specific peptide-pulsed dendritic cells, or dendritic cells transduced with tumor-cell RNA or with cDNA encoding specific tumor antigens can generate relatively large numbers of T cells with antitumor reactivity. The infusion of these T cells into patients would then be expected to result in an effective antitumor response. This approach has been successful particularly in the setting of posttransplantation Epstein Barr virus (EBV) induced lymphoproliferative disease and malignant lymphoma [72 74]. Such lymphomas express reasonably strong, immunostimulatory, EBV-derived antigens, however. Most other tumors do not express tumor-specific antigens with that level of immunogenicity. In addition, it is unclear what the optimal in vitro conditions are for generating large numbers of tumor-specific lymphocytes that represent appropriately balanced proportions of helper and cytolytic lymphocyte subtypes. To this end, several approaches have been developed directed at in vivo active immunization or vaccination. An essential question of all these approaches is what the optimal antigen is and how best to present it immunologically to T cells. Thus, a variety of vaccine approaches have been tested, including whole tumor cells, tumor cells modified with immunostimulatory cytokines, tumor cells transduced to express costimulatory receptors, dendritic cells transduced with tumor RNAs or specific cDNAs, dendritic cells allowed to react and process tumor-specific proteins or peptides, and peptides or DNAs encoding tumor antigens in combination with immune adjuvants [75 78]. Although the approaches that use specific tumor antigens would seem to have the best chance for specifically targeting antitumor T-cell responses, it has not been possible to optimize many of these antigens to generate significant in vivo antitumor responses. Many clinical trials have thus involved the use of wholecell vaccines with tumor cells or bystander cells transduced with immunostimulatory cytokines or receptors. Although in most of these trials it is still too early to determine whether they afford an advantage in disease-free survival,
1346
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
they should provide evidence for feasibility and the generation of surrogate antitumor responses. A potential problem with all cancer vaccines that do not use tumor-specific antigens is cross-reactivity of T-cell responses to normal tissues expressing the same antigen. This cross-reactivity has been observed in some of the melanoma vaccine trials in which patients developed vitiligo caused by cross-reactivity with normal melanocytes. Although this adverse effect may be essentially cosmetic, cross-reactivity with a vital organ or with a hematopoietic stem cell could prove fatal [79]. In addition to optimizing the type of vaccine, several other problems will need to be overcome to demonstrate the usefulness for vaccination-based therapies. For vaccines that include the genetic modification of tumor cells, there are problems in isolating sufficient numbers of tumor cells and effectively transducing and expressing the genes of interest in them. Sufficient cells are likely to be obtainable from bone marrow aspiration or pheresis for patients with hematologic malignancies, but the isolation of such numbers from solid tumors is more problematic. Furthermore, many tumors cannot be effectively propagated in vitro; and even were in vitro propagation possible, the in vitro culture conditions have the potential of significantly altering their antigenic characteristics. Traditional approaches to gene transfer, such as retroviruses, are quite inefficient in many tumor types, especially in hematopoietic malignances, although lentiviruses may offer an improvement [80]. Other viral vectors, such as adenoviruses, are being used, but many such viruses are quite immunogenic by themselves. To develop carefully controlled clinical trials, one would have to randomize to a viral vector alone versus a viral vector plus the immunostimulatory gene product, a process that has not been done [62,81,82]. A further consideration for all vaccination-based approaches to therapy is the timing of immunization with respect to other therapy. In nearly all animal models, the optimal setting in which to use tumor vaccines is that of minimal residual disease. Unfortunately, most currently used cytotoxic treatments are quite immunosuppressive, abrogating the efficacy of vaccines to stimulate antitumor responses. There is some evidence from preclinical animal models, however, that effective immunostimulation with whole-cell tumor vaccines can occur shortly after autologous bone marrow transplantation [83,84]. This setting would potentially be ideal for testing vaccine-based immunostimulation in patients. Alternatively, the development of nonimmunosuppressive therapies that are targeted to tumor cells would be ideal cytoreductive therapy that might precede vaccination-based therapies. Because vaccine-based therapies may work best when there is minimal residual disease, a state that may be difficult to measure in some tumor types, the development of immune surrogate markers that are predictive of clinical effectiveness should provide additional trial endpoints. At the current time, there are very few such markers of response. Most in vitro cytolytic, antitumor T-cell activity assays are not often very predictive of response. The measurement of T cells with anti tumor-specific antigen reactivity through the use of soluble
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1347
T-cell antigen receptor tetrameric proteins has, however, proven to be useful in this regard [85]. In addition, the measurement of T-cell stimulation by their ability to secrete cytokines using enzyme-linked immunospot (ELISPOT) methods has become an accepted means of measuring surrogate immune responses [86]. Nevertheless, the efficacy of cancer vaccines will only be proven using controlled, randomized trials that demonstrate improved survival of patients. At the current time, immunostimulatory vaccines are an important approach that should be rigorously tested in patients with cancer. Although the potential for specific tumor targeting is great, this hope has not yet been realized. In addition, relatively little is known about resistance mechanisms to immunemediated killing that tumor cells can develop. Although antitumor T lymphocytes may exist at a very low frequency in some patients, a patient with cancer rarely generates a clinically detectable immune-mediated antitumor response. Mechanisms by which tumor cells can avoid immune-mediated killing are clearly varied and complex. They include decreased antigen presentation through decreased expression of MHC class I and class II proteins, decreased expression of costimulatory receptors resulting in anergy, decreased surface adhesion molecules, the development of antigenic variants (antigenic drift), secretion of immunosuppression factors, and altered expression of MHC class I molecules that can alter natural killer cell mediated cytotoxicity [87]. The large number of effective mechanisms by which tumor cells can evade immune-mediated killing is reminiscent of the wide variety of mechanisms of resistance to chemotherapy that tumor cells acquire. Much work thus remains in developing cancer vaccines that are both specific and clinically effective. Oncolytic microbes The idea of using infectious agents such as viruses to treat cancer dates back at least a century, but only in the last decade has the understanding of the molecular biology of viruses and of cancer converged to enable the rational targeting of these agents to cancer cells [88]. Tumor-selective, conditionally replicative viruses (CRVs) have long been sought for their ability to kill tumor cells (oncolysis) [88,89]. Cell death results from replication of viral particles rather than from the more common gene therapy approach of expressing a toxic gene product. The distinct advantage of replicating viruses is their natural ability to spread, obviating the need to reach all cells with the initial infection. Tumor targeting results either from missing viral genes that are complemented by tumor cells but not by normal cells (type I CRV) or by the placement of critical viral genes under the control of tumor-specific promoter or enhancers (type II CRV). Tumor regression after direct intratumoral injection has been demonstrated repeatedly using a variety of viruses and tumor models. In some cases, viral oncolysis elicited an antitumor immune response, suggesting that viral infection served as an in situ cancer vaccine [90 92]. Viral replication could also be controlled by antiviral agents or by engineering viral gene expression to be drug-
1348
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
dependent [93]. One of the issues yet to be adequately addressed is systemic delivery of virus to sites of distant metastatic disease. Herpes simplex viruses Herpes simplex viruses (HSVs) deleted of critical metabolic genes such as thymidine kinase (tk), DNA polymerase, and ribonucleotide reductase are attenuated in nondividing cells but are capable of lytic replication in dividing cells that transcomplement the missing viral functions [94]. In addition, a gene responsible for neurovirulence in HSV (ICP34.5) is dispensable for viral replication. Thus, viruses deleted for ICP34.5 have minimal risk for causing encephalitis. Such viruses have passed preclinical safety evaluations [95 98] and have been successfully administered to humans in phase I studies [99,100]. Even systemic administration has been shown in animal models to cause tumor regression at distant sites [101 104]. An ongoing clinical trial is evaluating the potential of such agents to treat colon cancer metastatic to the liver using intraportal vein injections. Although primary HSV infection usually occurs in mucosal epithelium, HSV is capable of infecting a wide variety of cell types. In addition to gliomas, most published studies have focused on adult carcinomas including those of liver, breast, pancreas, prostate, squamous cell, ovary, and bladder [90,101 106]. Cells derived from a retinoblastoma [107] as well as rhabdomyosarcomas and osteosarcomas [108] have also been shown to be susceptible to HSV-mediated oncolysis. Cell lines derived from Ewings sarcomas were resistant [108], possibly because of the deletion of the neurovirulence gene in these viruses because Ewings sarcoma cells are neuroectodermal in origin. Targeting of HSV replication to sarcoma cells that express the calponin gene (synovial cell sarcoma, leiomyosarcoma, and osteosarcoma) has been achieved by placing the viral ICP4 gene under control of the calponin promoter [109]. Clearly, the range of tumor types that may be amenable to HSV-mediated oncolysis has not been adequately investigated. Adenovirus The use of adenovirus for clinical gene transfer has been questioned because of the fatal immune response in a patient given a high intraportal dose of virus to the liver [110]. Although there are possibly serious concerns about the use of this system in humans, the potential utility of adenovirus warrants further development and exploration [111]. Indeed, one conditionally replicative adenovirus (CRAd) has already undergone extensive clinical testing by intratumoral, intraportal, and intravenous routes in humans and has been shown to be safe up to systemic doses of at least 21013 virus particles [112]. In addition, an antiviral immune response to infected cells is predicted to be advantageous as an anticancer mechanism if the viral infection can be limited to cancer cells. Therefore, adenovirus may have an important role in future cancer therapy. The type I CRAd best studied is an E1B-mutant adenovirus termed DI-1520 (previously called dl1520 and ONYX-015) that is markedly attenuated in normal cells and selectively replicates in many cells [113 115]. DI-1520 has shown a safe clinical profile in multiple human trials when administered by intratumoral,
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1349
intraarterial, and intravenous routes [112]. Although DI-1520 has shown synergy with coadministered chemotherapy [116], its use as a single agent for treating solid tumors seems limited. The limited efficacy of DI-1520 is thought to result in part from the missing E1B function, which results in less effective viral replication. Poor expression of the major adenovirus receptor may also limit its utility [117 119]. Clearly, further understanding and engineering of CRAds will be required to maximize their anticancer effectiveness. Modifications of the virus coat protein may be useful in this regard; the cell-tropism of ONYX-015 was expanded by addition of a lysine tail to the fiber knob, resulting in higher oncolytic potency for glioma cells [120]. Binding to other cell surface molecules such as integrins by the incorporation of peptide motifs in the virus coat proteins has also been shown to increase oncolysis [117,120]. Other type I CRAds have been created containing a mutated E1A protein that is defective for binding to cell-cycle checkpoint retinoblastoma protein (Rb); therefore these CRAds replicate only in dividing cells [121,122]. For reasons that are not understood, the potency of some E1A mutants may be greater than wild-type adenovirus [122]. Examples of type II CRAds include those whose virus genes are controlled by promoters active in prostate cancer cells by virtue of the prostatespecific antigen promoter [123,124] or hepatoma cells using the a-fetoprotein promoter [125]. The latter could potentially be useful for other pediatric embryonal tumors, such as hepatoblastoma, which overexpress a-fetoprotein. An adenovirus whose replication is dependent on increased expression of the b-catenin/T-cell factor pathway such as occurs in colon cancer has also been described [126]. This adenovirus could potentially be useful for treatment of patients with hereditary polyposis coli, desmoid tumors, and possibly other childhood cancers that may be found to harbor similar genetic defects. A type II CRAd has also been described with replication controlled by the midkine promoter, active in a variety of tumors including Wilms tumor, neuroblastoma, and Ewings sarcoma [127]. Although these agents are directed to selected tumors based on promoter expression, many of them do show some nonspecific replication in other cells as the result of viral regulatory sequences that cause promiscuous, low-level promoter activity. Therefore, further iterations of many of these viruses will be necessary to achieve tighter (and thus safer) control of viral replication. Numerous studies have shown that almost all adenovirus given intravenously is found in the liver. Although the biodistribution of intravenous adenovirus may be a potential problem for reaching micrometastatic disease, CRAds given systemically in animal models have been shown to be capable of inhibiting tumor growth at distant sites [124,128]. Modifications of virion capsid proteins may further facilitate delivery to extrahepatic sites [129], so there is hope that better delivery to distant tumor sites will eventually be achieved. Reovirus Reovirus is a double-stranded RNA virus that is frequently cultured from the human respiratory and gastrointestinal tracts but has not been associated with any human disease. The subclinical nature of infection probably results from natural
1350
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
cellular defense mechanisms: in response to reovirus infection, normal human cells activate a protein kinase that inhibits translation of viral proteins [130]. Curiously, some cancers are targets of efficient reovirus replication because such inhibition does not occur in cells with an activated Ras pathway, permitting a lytic viral infection [131]. Because there is not a 100% correlation of virus infection with activated Ras, however, a complete understanding of the cell selectivity of virus infection remains elusive. Therefore, it is not yet possible to predict completely whether a given cancer will be sensitive to reovirus-mediated oncolysis. In this context, gliomas have been the most extensively studied, and a single injection of reovirus was shown to cure subcutaneous and orthotopic intracerebral gliomas in mouse xenograft models [132]. All nine primary glioma cultures tested were sensitive to reovirus oncolysis. Whether pediatric brain tumors will be susceptible to reovirus remains unclear, particularly because Ras mutations seem to be rare events in these patients [133]. Reovirus therapy might be useful, however, in the treatment of other pediatric cancers that are associated with activated Ras including myelodysplastic syndrome [134], AML [135], T-cell ALL [136], retinoblastoma (one third of cases) [137], and all tumors in patients with neurofibromatosis. Ras has been found to be activated in normal blood and marrow mononuclear cells, although the implications of this finding for systemic reovirus administration are not known [136]. Other safety concerns are yet to be addressed, such as the mechanism of the widespread lethal infection seen in immunocompromised animals. Nevertheless, human phase I clinical trials using direct intratumoral injections of wildtype reovirus are currently underway. As the mechanisms of cell sensitivity become clearer, it may be possible to engineer mutants that are more specifically targeted to tumor cells. Poliovirus Poliovirus neurotropism primarily results from the expression of its cellular receptor, CD155, on motor neurons. One of the major determinants of the efficiency of poliovirus replication, however, resides in the internal ribosomal entry site (IRES) found in the 50 untranslated region of its RNA genome [138]. Thus, substitution of the poliovirus IRES with IRES elements derived from other RNA viruses, such as rhinovirus, renders the virus essentially replicationdefective in neuronal cells. Because the new IRES elements function in other cell types, however, such recombinant polioviruses are capable of causing a lytic infection in other cells expressing CD155. Although its normal physiologic function is unknown, CD155 is thought to play a role in cell adhesion, and its expression may be increased in a variety of cancers [139 141]. Despite their neuronal origin, CD155-positive glioma cells also support robust replication of IRES-substituted poliovirus. Complete dissolution of subcutaneous xenograft gliomas was observed after either direct intratumoral or intravenous virus injections [139]. Only intratumoral and not intravenous injections cured mice with orthotopic (brain) gliomas, however, suggesting unknown barriers to systemic viral delivery to central nervous system tumors. Seventy-six percent
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1351
of primary gliomas examined expressed CD155 (including 8 of 13 cases of glioblastoma multiforme), so poliovirus-based therapy might be feasible for a majority of these intractable tumors. Whether other childhood cancers of neuroectodermal origin, such as neuroblastoma and Ewings sarcoma family of tumors, express CD155 and support recombinant poliovirus replication has yet to be reported. Newcastle disease virus Newcastle disease virus (NDV) is an avian paramyxovirus, closely related to parainfluenza and mumps viruses, that is oncolytic for certain human tumors. Early clinical trials in humans in the mid twenty-first century were abandoned because of tumor regrowth, thought to be caused by the robust humoral and cellular antiviral immune response [142]. These failures may have resulted in part from weak oncolytic viral potency, which varies widely among NDV strains [143]. Newcastle disease virus strains can be selected for increased oncolytic potency, however, and direct intratumoral injections of strain 73T induced remissions in mouse models of neuroblastoma and fibrosarcoma [144,145]. Intravenous administration of strain PV701 has been shown to be safe in humans, and delivery of virus to tumor tissue was documented [146]. Patients were found to tolerate higher doses of virus after the initial dose, suggesting that traditional phase I strategies to identify the maximum tolerable dose need to be modified for testing such biologic agents. The robust immune response has also prompted trials of NDV-infected cancer oncolysates as cancer vaccines [147]. Although the concept of using NDV as a cancer therapy is far from new, modern molecular tools are now available to study the complex virus-host interactions to gain insight that will be required to employ NDV effectively as a cancer therapy. Measles virus The live-attenuated Edmonston-B strain of measles virus used as a vaccine has been shown to infect myeloma cells selectively compared with stimulated peripheral blood lymphocytes and to cause tumor regression and, in some cases, remission in xenograft models [148]. Whether the high doses of virus required will be tolerable is unclear. Whether other leukemias might also be susceptible to measles-mediated oncolysis has not been reported, so the use of this agent for treatment of childhood malignancies is unknown. Bacteria Other types of replicating microbes have long been sought as antitumor agents. Certain bacteria such as Salmonella have been shown to be capable of selective replication in tumors such as mouse melanoma, even at sites distant from inoculation, causing an antitumor effect [104]. Recent studies have also demonstrated promising results in animal models using Clostridium novyi, which has been genetically manipulated to lack its lethal toxin but still be capable of growing in anaerobic regions such as tumors. These studies have shown significant tumor cytotoxicity [149]. Much of the work in this area is currently
1352
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
proprietary, so it is not clear how close to human trials such agents may be and which tumors are susceptible. Again, however, any active biologic agent has the potential to be understood in its mechanisms and therefore manipulated to focus targeting more effectively to tumor cells. Impact of microbial therapy The precise roles of conditionally replicative viruses and bacteria in future cancer therapy are not yet clear. They may be useful as a biologic surgery through direct intratumoral injection. They could offer an alternative for local control when surgery is contraindicated or radiation risks are high. It is even conceivable that viral or bacterial oncolysis could someday supplant surgery and radiation as the primary means of removing some tumors, avoiding the attendant risks of those procedures. In some cases, the microbial infection may have the additional benefit of eliciting a cell-mediated antitumor immune response and thereby may result in either the shrinkage of metastatic disease or protection from recurrence in patients with minimal residual disease. The future role of oncolytic microbes in the treatment of metastatic disease is less clear. Although animal models have demonstrated feasibility for this type of nonimmunosuppressive therapy, coaxing large amounts of the administered virus to reach sites of disease remains a hurdle. Because of microbe amplification through replication at disease sites, however, small improvements in viral delivery may be significant. Further refinements of all CRVs include the addition of other therapeutic genes (armed virus) and redirecting cell binding by ablating the binding to the native receptor or retargeting to other cell surface receptors using peptide motifs or antibody conjugates. Systemic delivery is the remaining major challenge for the use of replicative microbes to have a significant impact as therapy for cancer. More efficient systemic delivery of these agents to tumor beds will probably be necessary before these agents significantly affect the outcome of patients with metastatic disease. Oncolytic microbial therapy is at the crossroads of two complex biologic systems microbe replication and cancer cell survival. Better understanding of these systems will allow modification of these agents to maximize their interactions. As Fig. 1 indicates, little has been done in terms of modifications for many of these agents, so the field of oncolytic microbes is really still in its infancy. Once these agents are more refined and the systemic delivery hurdle is overcome, targeted replicative viruses could represent a treatment modality lacking most or all of the side effects of chemotherapy, surgery, and radiation. Certainly, turning one set of human scourges against another would be poetic justice.
Molecular targeting of tumor cells: is this really noncytotoxic therapy? Recent advances in the definition of molecular events leading to malignant transformation of normal cells as well as understanding of the growth and survival
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1353
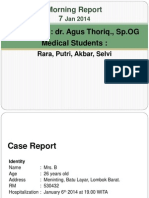
Fig. 1. Retooling conditionally replicative viruses (CRVs) to target cancer cells selectively. Although a number of virus strains show natural selectivity for certain cancer types, early experience with adenovirus suggests that all viruses could be further modified to improve targeting. Type I CRVs exhibit cell selectivity based on missing functions complemented by cancer cells, and type II CRVs exhibit cell selectivity based on cell-specific promoter activity. Either type can be further modified to express therapeutic genes (armed viruses). Viral binding to cells can also be modified by ablating binding to native receptors or by redirecting binding to other cell surface molecules.
mechanisms of tumor cells has provided a foundation on which potentially tumorspecific and, thus, nontoxic cancer treatment can be designed. Many recent reviews deal with the many aspects of these approaches [150 152]. Rather than going into extensive detail, this article instead attempts to highlight concepts and some of the primary biologic opportunities for tumor-specific targeting. There are two fundamental strategies for targeting molecular pathways that allow tumor cells rather than normal cells to be selectively killed. The first strategy involves specific molecular defects in mechanisms on which tumor cells depend for their growth and survival and, thus are unique pathways that can be targeted. This class of targets might be called the Achilles heel group and represents the potential for truly specific targeting of tumor cells. The second strategy is to target pathways that are common to neoplastic and normal cells but on which cancer cells are preferentially dependent for survival. This latter approach, although not truly specific targeting, might be considered somewhat similar to conventional chemotherapy. Nevertheless, this latter approach may prove both effective and somewhat less toxic than traditional chemotherapy as new agents are developed that selectively inhibit biologic pathways rather than causing more global genotoxic damage [153]. The essence of therapeutic molecular targeting of cancer cells is based on the observations that tumor cells are characterized by dysregulated proliferation and abnormal apoptotic responses. Mutations in genes that regulate cell proliferation produce downstream alterations in signal transduction pathways that in turn result in further changes in gene expression. These molecular alternations lead to changes in the ability of tumor cells to respond normally to environmental growth inhibitory or stimulatory signals and often to concomitant changes in pathways regulating cell survival (Fig. 2) [154]. These alterations also often result in the activation of
1354
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
Fig. 2. Mutant receptors and potential signaling pathways leading to altered proliferation, survival mechanisms, and drug resistance. These receptors and downstream pathways can also be targeted therapeutically. The figure depicts a wild-type receptor on the left and an activating mutant receptor on the right that dimerizes even in the absence of ligand. Activation can be caused by a variety of mutations, as described in the text. The larger arrows depict the potential for preferential signaling by the mutant receptor.
cellular pathways that regulate resistance to chemotherapeutic agents and radiation therapy. They therefore represent potentially superb therapeutic targets. Examples of genetic mutations that can lead to these profound cellular changes include molecules belonging to the class III tyrosine kinase receptors, such as FLT3, c-FMS, platelet-derived growth factor (PDGF), and c-KIT. These receptors are critical in the response of cells to growth- and survival-signaling pathways. Mutations have been described that lead to the constitutive activation of these receptors resulting in continuous signaling of proliferation and survival pathways [155,156]. In addition, these mutations, which often involved the kinase domain or adjacent regions of the molecule, may result in downstream signaling that is distinct for the mere activation of the receptor by its physiologic ligand. For example, activating point mutations in the FLT3 and c-KIT kinase domain result in cytokine-independent growth, increased proliferative rate, and resistance to various chemotherapeutic agents [155 160]. These cellular consequences resulting from a mutated c-KIT receptor, for example, do not occur with maximal stimulation of the wildtype receptor with its cognate ligand [157,158,161,162]. Mutations in the juxtamembrane region of the FLT3 receptor, characterized by internal tandem duplications (ITD), can also lead to a constitutively activated receptor [155,156]. The
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1355
presence of only the FLT-ITD receptor in myeloid leukemia cells has been shown to result in an extremely poor prognosis for such patients [155,156,163 167]. Activating mutations of such growth-regulatory molecules is both an active and promising area of current investigation. In particular, such receptor mutations could provide true targeted therapy if an inhibitor was specifically directed toward the unique structural motif resulting from the mutation. This result has in part been realized with reports that the selective inhibition of the FLT3-ITD receptor in chemoresistant myeloid leukemia cells results in the induction of apoptosis [159,160]. These inhibitors of FLT3-ITD receptors do not seem to block wildtype or FLT3 receptors harboring activating point mutations efficiently. Similarly, these inhibitors are not effective against wild-type or constitutively active c-KIT receptors because of point mutations in their kinase domain [168,169]. This type of selectivity has tremendous potential for reducing the cytotoxicity toward normal tissues. Another important example of selective targeting is the development of inhibitors to the cytoplasmic bcr-abl fusion tyrosine kinase that characterizes chronic myelogenous leukemia [152,170,171]. The development of STI-571 (Gleevac, Imatinib Novartis Pharmaceuticals Corporation, East Hanover, NJ) as an important therapeutic agent in patients with CML has clearly provided an important therapeutic advance. Critical to the effectiveness of STI-571 is the profound dependence CML cells have on its expression and function. Although it remains unclear whether bcr-abl inhibition can cure patients with CML, 70% to 80% of patients with chronic phase CML achieve cytogenetic remissions with relatively few side effects [172]. A new trial testing the use of STI-571 in children with CML is currently being opened through the cooperative group mechanism. The development of STI-571 raises other important issues and a word of caution about biologic targeting. Subsequent to the work on the bcr-abl fusion protein, it was shown that STI-571 had significant activity against the activating mutations of c-Kit that involve the juxtamembrane region of the receptor. These mutations are characteristically associated with gastrointestinal stromal cell tumors (GIST) that are essentially resistant to conventional chemotherapeutic agents [169,173,174]. Several clinical trials have now demonstrated that STI-571 has excellent activity in patients with GIST, leading to significant numbers of objective responses and some complete remissions [169,173,174]. STI-571, however, does not inhibit activating mutations of c-Kit that are a result of changes in the kinase domain. Thus, the precise nature and location of an activating mutation has profound effects on whether a particular small molecule will be inhibitory. This type of selectivity (one could say specificity) leads to the conclusion that an important aspect of molecular targeting will be the careful analysis and testing of specific mutations on the assumed targets. Another important lesson that is being learned from STI-571 is the development of resistance in CML cells from patients chronically exposed to the drug. The emergence of resistance has been documented to result, at least in some cases, from point mutations in the region of the bcr-abl fusion protein that affect binding of STI-571. There is also growing evidence that increased expression of alternative survival pathways can result in resistance to STI-571 [175 178].
1356
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
Thus, although it is not completely fair to generalize to all molecular inhibitors from these data, the excitement of molecular targeting must be tempered by recognition of the ability of tumor cells to develop alternative means of survival. To this end, the most effective use of targeted inhibitors may be in combination with other antitumor agents directed toward alternative pathways. A third lesson from STI-571 has been the realization that this drug can inhibit even some wild-type tyrosine kinase receptors, such as c-KIT and PDGF. Although this type of activity may prove useful in the treatment of tumors expressing these receptors, it is likely that normal tissues that depend on the function of these receptors will also be affected. This type of approach may be less selective than targeting specific mutations but might nevertheless be efficacious as antitumor therapy if the malignant cells are more dependent on these pathways for survival than normal cells. For example, farnesyl transferase inhibitors (FTI) have been developed with the hope that they would be selective inhibitors of the potent growth-promoting protooncogene, RAS, whose activity in part depends on posttranslational farnesylation [179,180]. Significant numbers of other proteins, however, require farnesylation for their activity. Thus, the mechanism by which FTIs result in tumor cell killing is unclear but may reflect their activity against multiple cellular pathways. Additional consequences of inhibiting specific receptor or enzyme mutations as well as their downstream signaling pathways include the ability of tumor cells to stimulate angiogensis [150]. Although the precise pathways through which tumor cells regulate local angiogenesis have not been ascertained, it is clear that certain oncogenic proteins, such as Ras and Myc, can be angiogenic. Thus, inhibiting specific tumor-specific pathways or the tumor bed vasculature may result in decreased angiogenesis and resultant tumor regression. The concept of antiangiogenic therapy for cancer was proposed more than 30 years ago [181]. Now there are many clinical studies using antiangiogenesis-directed therapies targeted to tumor vasculature [182 185]. An interesting possibility to consider for the future is that tumor cell specific approaches may also have profound effects on local blood vessel growth and integrity, truly killing two birds with one stone. Another downstream pathway involved in cell survival and chemotherapeutic resistance is the antiapoptotic protein Bcl-2. The increased expression of Bcl-2 plays an essential role in the regulation of apoptosis through the release of mitochondrial cytochrome c and caspase activation [186]. By playing such an important role in protecting cells from apoptosis, molecules such as Bcl-2 become important potential therapeutic targets. Disruption of Bcl-2 function has been achieved through the use of antisense oligonucleotides. For example, exposure of AML cells to cytarabine and Bcl-2 antisense oligonucleotides results in decreased Bcl-2 levels and increased apoptosis [187 189]. The use of antisense oligonucleotides directed toward Bcl-2 is currently in clinical trials in adults and children with AML, both alone and in combination with chemotherapy. Initial results suggest that the antisense oligonucleotides are well tolerated. Although they are specific in their sequence to Bcl-2, because of their relatively short sequence length, their absolute specificity will be difficult to definitively prove.
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1357
Mutations in p53, a critical regulator of cell cycle checkpoints and DNA repair, have been observed in a variety of both solid tumors and hematologic malignancies [190]. In addition, the critical function of p53 in drug resistance has been well demonstrated using p53-deficient (p53 / ) mouse embryonic fibroblasts transformed by adenovirus E1A protein. Fibroblasts of the p53 / genotype were shown to be resistant to both ionizing radiation and several chemotherapeutic agents, whereas wild-type or heterozygotic mutant p53- expressing fibroblastderived tumors demonstrated increased sensitivity and apoptosis to such agents [191,192]. Because of such data and the central role of p53 in tumorigenesis and resistance to therapy, this pathway has been enthusiastically pursued as a therapeutic target. For example, some groups have introduced wild-type p53 into p53 / tumor cell lines using adenovirus, demonstrating that increased apoptosis and growth inhibition results, as discussed earlier in this article [193,194]. A more pharmacologic type of approach has been the development of adapter drugs or molecules that are able to restore the normal p53 structural configuration and function of mutant p53 [195]. An alternative approach that is being considered is the modulation of regulators of p53-mediated pathways, such as MDM2 expression [196,197]. In addition to targeting mutated regulators of tumor cell proliferation and survival, there is increasing evidence that the chromosomal translocations that characterize many different solid tumors and leukemia may function by recruiting transcriptional repressor complexes that result in blocked differentiation [198,199]. The recruitment of transcriptional repressor complexes includes methyl transferases and histone deacetylases leading to the hypermethylation of promoters and the deacetylation of histones, respectively [200 202]. Both changes result in transcriptional repression of chromatin. Thus, part of the phenotype of many tumors is a block in their ability to differentiate fully. The extraordinary clinical results achieved with the use of ATRA in acute promyelocytic leukemia are a direct result the destabilizing effect of ATRA on the recruitment repressor complexes by the PML/RAF fusion protein [203]. The AML/ ETO fusion protein that characterizes t(8;21) AML has also been shown to recruit transcriptional repressor complexes, resulting in a block in differentiation [204]. Although ATRA does not have significant activity for the AML/ETO fusion product, there is hope that other types of inhibitors can be identified [205]. An alternative, albeit more global approach, is to bypass the binding event of the fusion protein and attack the downstream effects of repressor complex activity, such as DNA methylation and histone deacetylations [200 202,206]. Several active, demethylating drugs, such as azacytidine and decitabine, are being used alone and in combination with inhibitors of histone deacetylases, such as phenylbutyrate, to treat patients with a variety of hematologic and solid tumors [207 213]. Another potentially useful consequence of this type of derepression therapy is the induction of expression of genes which have been repressed by promoter hypermethylation but would otherwise be expressed and function in controlling cell cycle kinetics or drug sensitivity. Such examples have included p16, Rb, cyclins, and caspase 8 [214 216]. One can thus hypothesize that combinations of
1358
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
Fig. 3. Schematic representation of some potential therapeutic targets in cancer, as discussed in the text.
derepression approaches in combination with cytotoxic drugs or differentiation factors would potentially be able to overcome chemotherapeutic resistance resulting from the reduced expression of such genes. Clinical trials employing these strategies are currently being performed for a variety of tumor types. As these examples demonstrate, molecularly targeted therapy can be directed against tumor-specific mutations in proteins that regulate growth regulation and survival or against pathways on which tumor cells may have a preferential dependence for proliferation or survival (Fig. 3). The former approach represents truly specific molecular targeting and has the likely advantage of being relatively nontoxic to normal tissues. The latter approach, depending on the cytotoxic dose response of tumor cells versus normal cells, is likely to be less specific and therefore to have more adverse effects on normal tissues. Such therapies also have the potential for being more cytostatic rather than cytotoxic. This effect will depend in part on how these inhibitors affect the gene expression pattern of tumor cells and, in turn, how those changes influence normal tissues surrounding the tumor. For instance, altered tumor cell gene expression may influence the angiogenic capacity of the tumors, thereby altering the delivery of inhibitor to the tumor cells. Finally, the clearly demonstrated ability of tumor cells to develop additional mutations that block the action of inhibitors will be a difficult problem to overcome, just as drug resistance to conventional chemotherapy has been difficult to circumvent.
References
[1] Kohler G, Milstein C. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 1975;256:495 7.
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1359
[2] Ritz J, Pesando JM, Sallan SE, et al. Serotherapy of acute lymphoblastic leukemia with monoclonal antibody. Blood 1981;58:141 52. [3] Metzgar RS, Borowitz MJ, Jones NH, et al. Distribution of common acute lymphoblastic leukemia antigen in nonhematopoietic tissues. J Exp Med 1981;154:1249 54. [4] Yu AL, Uttenreuther-Fischer MM, Huang CS, Tsui CC, Gillies SD, Reisfeld RA, et al. Phase 1 trial of a human-mouse chimeric anti-disialoganglioside monoclonal antibody ch14.18 in patients with refractory neuroblastoma and osteosarcoma. J Clin Oncol 1998;16:2169 80. [5] Kendra K, Gan J, Ricci M, et al. Pharmacokinetics and stability of the ch14.18-interleukin-2 fusion protein in mice. Cancer Immunol Immunother 1999;48:219 29. [6] Cheung NK, Guo HF, Cheung IY. Correlation of anti-idiotype network with survival following anti-G(D2) monoclonal antibody 3F8 therapy of stage 4 neuroblastoma. Med Pediatr Oncol 2000;35:635 7. [7] Cheung NK, Guo HF, Heller G, et al. Induction of Ab3 and Ab30 antibody was associated with long-term survival after anti-G(D2) antibody therapy of stage 4 neuroblastoma. Clin Cancer Res 2000;6:2653 60. [8] Reichert JM. Therapeutic monoclonal antibodies: trends in development and approval in the US. Current Opinions in Molecular Therapeutics 2002;4:110 8. [9] Green LL. Antibody engineering via genetic engineering of the mouse: XenoMouse strains are a vehicle for the facile generation of therapeutic human monoclonal antibodies. J Immunol Methods 1999;231:11 23. [10] Davis CG, Gallo ML, Corvalan JR. Transgenic mice as a source of fully human antibodies for the treatment of cancer. Cancer Metastasis Rev 1999;18:421 5. [11] Baca M, Presta LG, OConnor SJ, et al. Antibody humanization using monovalent phage display. J Biol Chem 1997;272:10678 84. [12] Hayden MS, Gilliland LK, Ledbetter JA. Antibody engineering. Curr Opin Immunol 1997; 9:201 12. [13] Berger M, Shankar V, Vafai A. Therapeutic applications of monoclonal antibodies. Am J Med Sci 2002;324:14 30. [14] Hemminki A. From molecular changes to customised therapy. Eur J Cancer 2002;38:333 8. [15] Tur MK, Sasse S, Stocker M, et al. An anti-GD2 single chain Fv selected by phage display and fused to Pseudomonas exotoxin A develops specific cytotoxic activity against neuroblastoma derived cell lines. Int J Mol Med 2001;8:579 84. [16] Goel A, Augustine S, Baranowska-Kortylewicz J, et al. Single-dose versus fractionated radioimmunotherapy of human colon carcinoma xenografts using 131I-labeled multivalent CC49 single-chain Fvs. Clin Cancer Res 2001;7:175 84. [17] Kreitman RJ, Wilson WH, White JD, et al. Phase I trial of recombinant immunotoxin antiTac(Fv)-PE38 (LMB-2) in patients with hematologic malignancies. J Clin Oncol 2000;18: 1622 36. [18] Timmerman JM. Vaccine therapies for non-Hodgkins lymphoma. Current Treatment Options in Oncology 2002;3:307 15. [19] Bendandi M. Role of anti-idiotype vaccines in the modern treatment of human follicular lymphoma. Expert Rev Anticancer Ther 2001;1:65 72. [20] Press OW, Leonard JP, Coiffier B, et al. Immunotherapy of non-Hodgkins lymphomas. Hematology 2001:221 40. [21] Bendandi M, Gocke CD, Kobrin CB, et al. Complete molecular remissions induced by patientspecific vaccination plus granulocyte-monocyte colony-stimulating factor against lymphoma. Nat Med 1999;5:1171 7. [22] Bhattacharya-Chatterjee M, Chatterjee SK, Foon KA. The anti-idiotype vaccines for immunotherapy. Curr Opin Mol Ther 2001;3:63 9. [23] Alfonso M, Diaz A, Hernandez AM, et al. An anti-idiotype vaccine elicits a specific response to N-glycolyl sialic acid residues of glycoconjugates in melanoma patients. J Immunol 2002;168: 2523 9. [24] Davis TA, Maloney DG, Czerwinski DK, et al. Anti-idiotype antibodies can induce long-term
1360
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368 complete remissions in non-Hodgkins lymphoma without eradicating the malignant clone. Blood 1998;92:1184 90. Cheung NK. Monoclonal antibody-based therapy for neuroblastoma. Curr Oncol Rep 2000;2: 547 53. Uckun FM, Messinger Y, Chen CL, et al. Treatment of therapy-refractory B-lineage acute lymphoblastic leukemia with an apoptosis-inducing CD19-directed tyrosine kinase inhibitor. Clin Cancer Res 1999;5:3906 13. Uckun FM, Chelstrom LM, Finnegan D, et al. Effective immunochemotherapy of CALLA + C mu+ human pre-B acute lymphoblastic leukemia in mice with severe combined immunodeficiency using B43 (anti-CD19) pokeweed antiviral protein immunotoxin plus cyclophosphamide. Blood 1992;79:3116 29. Maloney DG. Advances in immunotherapy of hematologic malignancies. Curr Opin Hematol 1998;5:237 43. Flavell DJ, Boehm DA, Noss A, et al. Therapy of human T-cell acute lymphoblastic leukaemia with a combination of anti-CD7 and anti-CD38-SAPORIN immunotoxins is significantly better than therapy with each individual immunotoxin. Br J Cancer 2001;84:571 8. Stadtmauer EA. Gemtuzumab ozogamicin in the treatment of acute myeloid leukemia. Curr Oncol Rep 2002;4:375 80. Sievers EL, Linenberger M. Mylotarg: antibody-targeted chemotherapy comes of age. Curr Opin Oncol 2001;13:522 7. Behr TM, Salib AL, Liersch T, et al. Radioimmunotherapy of small volume disease of colorectal cancer metastatic to the liver: preclinical evaluation in comparison to standard chemotherapy and initial results of a phase I clinical study. Clin Cancer Res 1999;5: 3232s 42s. Kumar R, Mandal M, Vadlamudi R. New insights into anti-HER-2 receptor monoclonal antibody research. Semin Oncol 2000;27:84 91. Ligibel JA, Winer EP. Trastuzumab/chemotherapy combinations in metastatic breast cancer. Semin Oncol 2002;29:38 43. Herbst RS, Shin DM. Monoclonal antibodies to target epidermal growth factor receptor-positive tumors: a new paradigm for cancer therapy. Cancer 2002;94:1593 611. Lynch DH, Yang XD. Therapeutic potential of ABX-EGF: a fully human anti-epidermal growth factor receptor monoclonal antibody for cancer treatment. Semin Oncol 2002;29:47 50. Martin M. Platinum compounds in the treatment of advanced breast cancer. Clin Breast Cancer 2001;2:190 208; discussion 209. Advani R, Saba HI, Tallman MS, et al. Treatment of refractory and relapsed acute myelogenous leukemia with combination chemotherapy plus the multidrug resistance modulator PSC 833 (Valspodar). Blood 1999;93:787 95. Arceci RJ. Can multidrug resistance mechanisms be modified? Br J Haematol 2000;110: 285 91. Bradshaw DM, Arceci RJ. Clinical relevance of transmembrane drug efflux as a mechanism of multidrug resistance. J Clin Oncol 1998;16:3674 90. Dantzig AH, Law KL, Cao J, et al. Reversal of multidrug resistance by the P-glycoprotein modulator, LY335979, from the bench to the clinic. Curr Med Chem 2001;8:39 50. Sonneveld P. Multidrug resistance in haematological malignancies. J Intern Med 2000;247: 521 34. Jandula BM, Nomdedeu J, Marin P, et al. Rituximab can be useful as treatment for minimal residual disease in bcr-abl-positive acute lymphoblastic leukemia. Bone Marrow Transplant 2001;27:225 7. Cheung IY, Barber D, Cheung NK. Detection of microscopic neuroblastoma in marrow by histology, immunocytology, and reverse transcription-PCR of multiple molecular markers. Clin Cancer Res 1998;4:2801 5. Estey EH, Giles FJ, Beran M, et al. Experience with gemtuzumab ozogamycin (mylotarg) and all-trans retinoic acid in untreated acute promyelocytic leukemia. Blood 2002;99:4222 4.
[25] [26]
[27]
[28] [29]
[30] [31] [32]
[33] [34] [35] [36] [37] [38]
[39] [40] [41] [42] [43]
[44]
[45]
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1361
[46] Coley W. The treatment of malignant tumors by repeated inoculations of erysipelas: with a report of ten original cases. Am J Med Sci 1893;105:487 511. [47] Nauts SHC, Swift WE. The treatment of malignant tumors by bacterial toxins as developed by the late William B. Coley, M.D. Cancer Res 1946;6:205 16. [48] Kleinerman ES, Erickson KL, Schroit AJ, et al. Activation of tumoricidal properties in human blood monocytes by liposomes containing lipophilic muramyl tripeptide. Cancer Res 1983;43: 2010 4. [49] Kleinerman ES. Biologic therapy for osteosarcoma using liposome-encapsulated muramyl tripeptide. Hematol Oncol Clin N Am 1995;9:927 38. [50] Worth LL, Jeha SS, Kleinerman ES. Biologic response modifiers in pediatric cancer. Hematol Oncol Clin N Am 2001;15:723 40 [ix.]. [51] Meyers P, Schwartz C, Bernstein M, et al. Addition of ifosfamide and muramyl tripeptide to cisplatin, doxorubicin and high-dose methotrexate improves event free survival (efs) in localized osteosarcoma (OS). In: Proceedings of the American Society of Clinical Oncology. San Francisco: American Society of Clinical Oncology; 2001. p. 367a. [52] Skog AL, Wersall P, Ragnhammar P, et al. Treatment with GM-CSF and IL-2 in patients with metastatic colorectal carcinoma induced high serum levels of neopterin and sIL-2R, an indicator of immune suppression. Cancer Immunol Immunother 2002;51:255 62. [53] Glaspy JA. Therapeutic options in the management of renal cell carcinoma. Semin Oncol 2002;29:41 6. [54] Atkins MB. Interleukin-2: clinical applications. Semin Oncol 2002;29:12 7. [55] Gross L. Intradermal immunization of C3H mice against a sarcoma that originated in an animal of the same line. Cancer Res 1943;3:326 33. [56] Foley EJ. Antigenic properties of methylcholanthrene-induced tumors in mice of the strain of origin. Cancer Res 1953;13:835 7. [57] Currie GA. Eighty years of immunotherapy: a review of immunological methods used for the treatment of human cancer. Br J Cancer 1972;26:141 53. [58] Kawakami Y, Eliyahu S, Delgado CH, et al. Cloning of the gene coding for a shared human melanoma antigen recognized by autologous T cells infiltrating into tumor. Proc Natl Acad Sci U S A 1994;91:3515 9. [59] Kawakami Y, Rosenberg SA. Immunobiology of human melanoma antigens MART-1 and gp100 and their use for immuno-gene therapy. International Reviews in Immunology 1997; 14:173 92. [60] Boon T, Cerottini JC, Van den Eynde B, et al. Tumor antigens recognized by T lymphocytes. Annu Rev Immunol 1994;12:337 65. [61] Pardoll DM. Inducing autoimmune disease to treat cancer. Proc Natl Acad Sci U S A 1999; 96:5340 2. [62] Arceci RJ. The potential for antitumor vaccination in acute myelogenous leukemia. J Mol Med 1998;76:80 93. [63] Guinan EC, Gribben JG, Boussiotis VA, et al. Pivotal role of the B7:CD28 pathway in transplantation tolerance and tumor immunity. Blood 1994;84:3261 82. [64] Foss FM. Immunologic mechanisms of antitumor activity. Semin Oncol 2002;29:5 11. [65] Herlyn D, Birebent B. Advances in cancer vaccine development. Ann Med 1999;31:66 78. [66] Wolchok JD, Chapman PB. Phase I trial of adoptive immunotherapy with cytolytic T lymphocytes immunized against a tyrosinase epitope. J Clin Oncol 2002;20:3176; discussion 3176 77. [67] Oka Y, Tsuboi A, Elisseeva OA, et al. WT1 as a novel target antigen for cancer immunotherapy. Curr Cancer Drug Targets 2002;2:45 54. [68] Meijer SL, Dols A, Urba WJ, et al. Adoptive cellular therapy with tumor vaccine draining lymph node lymphocytes after vaccination with HLA-B7/beta2-microglobulin gene- modified autologous tumor cells. J Immunother 2002;25:359 72. [69] Slavin S, Morecki S, Weiss L, et al. Donor lymphocyte infusion: the use of alloreactive and tumorreactive lymphocytes for immunotherapy of malignant and nonmalignant diseases in conjunction with allogeneic stem cell transplantation. J Hematother Stem Cell Res 2002;11:265 76.
1362
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
[70] Kolb HJ, Holler E. Adoptive immunotherapy with donor lymphocyte transfusions. Curr Opin Oncol 1997;9:139 45. [71] Slavin S, Ackerstein A, Morecki S, et al. Immunotherapy of relapsed resistant chronic myelogenous leukemia post allogeneic bone marrow transplantation with alloantigen pulsed donor lymphocytes. Bone Marrow Transplant 2001;28:795 8. [72] Haque T, Taylor C, Wilkie GM, et al. Complete regression of posttransplant lymphoproliferative disease using partially HLA-matched Epstein Barr virus-specific cytotoxic T cells. Transplantation 2001;72:1399 402. [73] Gottschalk S, Heslop HE, Roon CM. Treatment of Epstein-Barr virus-associated malignancies with specific T cells. Adv Cancer Res 2002;84:175 201. [74] Heslop HE, Rooney CM. Adoptive cellular immunotherapy for EBV lymphoproliferative disease. Immunol Rev 1997;157:217 22. [75] Dermime S, Armstrong A, Hawkins RE, et al. Cancer vaccines and immunotherapy. Br Med Bull 2002;62:149 62. [76] Alving CR. Design and selection of vaccine adjuvants: animal models and human trials. Vaccine 2002;20(Suppl 3):S56 64. [77] Klade CS. Proteomics approaches towards antigen discovery and vaccine development. Curr Opin Mol Ther 2002;4:216 23. [78] Fay JW. Hematopoietic growth factors, dendritic cell biology, and vaccine therapy of cancer. Curr Opin Hematol 2002;9:202 6. [79] Yu Z, Restifo NP. Cancer vaccines: progress reveals new complexities. J Clin Invest 2002; 110:289 94. [80] Stripecke R, Cardoso AA, Pepper KA, et al. Lentiviral vectors for efficient delivery of CD80 and granulocyte-macrophage-colony-stimulating factor in human acute lymphoblastic leukemia and acute myeloid leukemia cells to induce antileukemic immune responses. Blood 2000;96: 1317 26. [81] Mitchell MS. Cancer vaccines, a critical review part I. Curr Opin Investig Drugs 2002;3: 140 9. [82] Mitchell MS. Cancer vaccines, a critical review part II. Curr Opin Investig Drugs 2002;3: 150 8. [83] Borrello I, Sotomayor EM, Rattis FM, et al. Sustaining the graft-versus-tumor effect through posttransplant immunization with granulocyte-macrophage colony-stimulating factor (GMCSF)-producing tumor vaccines. Blood 2000;95:3011 9. [84] Borrello I, Sotomayor EM, Cooke S, et al. A universal granulocyte-macrophage colony-stimulating factor-producing bystander cell line for use in the formulation of autologous tumor cellbased vaccines. Hum Gene Ther 1999;10:1983 91. [85] Cerundolo V. Use of major histocompatibility complex class I tetramers to monitor tumorspecific cytotoxic T lymphocyte response in melanoma patients. Cancer Chemother Pharmacol 2000;46:S83 5. [86] Whiteside TL. Immunologic monitoring of clinical trials in patients with cancer: technology versus common sense. Immunol Invest 2000;29:149 62. [87] Wang E, Phan GQ, Marincola FM. T-cell-directed cancer vaccines: the melanoma model. Expert Opin Biol Ther 2001;1:277 90. [88] Kirn D. Replication-selective microbiological agents: fighting cancer with targeted germ warfare. J Clin Invest 2000;105:837 9. [89] Kenney S, Pagano J. Viruses as oncolytic agents: a new age for therapeutic viruses? J Natl Cancer Inst 1994;86:1185 6. [90] Toda M, Rabkin SD, Martuza RL. Treatment of human breast cancer in a brain metastatic model by G207, a replication-competent multimutated herpes simplex virus 1. Hum Gene Ther 1998;9:2177 85. [91] Toda M, Rabkin SD, Kojima H, et al. Herpes simplex virus as an in situ cancer vaccine for the induction of specific anti-tumor immunity. Hum Gene Ther 1999;10:385 93. [92] Todo T, Rabkin SD, Sundaresan P, et al. Systemic antitumor immunity in experimental brain
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1363
[93] [94] [95]
[96]
[97]
[98] [99]
[100]
[101]
[102]
[103] [104]
[105]
[106]
[107] [108]
[109]
[110] [111] [112]
tumor therapy using a multimutated, replication-competent herpes simplex virus. Hum Gene Ther 1999;10:2741 55. Yao F, Eriksson E. A novel tetracycline-inducible viral replication switch. Hum Gene Ther 1999;10:419 27. Martuza R. Conditionally replicating herpes vectors for cancer therapy. J Clin Invest 2000;105: 841 6. Meignier B, Longnecker R, Roizman B. In vivo behavior of genetically engineered herpes simplex viruses R7017 and R7020: construction and evaluation in rodents. J Infect Dis 1988;158:602 14. Meignier B, Martin B, Whitley R, et al. In vivo behavior of genetically engineered herpes simplex viruses R7017 and R7020. II. Studies in immunocompetent and immunosuppressed owl monkeys (aotus trivirgatus). J Infect Dis 1990;162:313 21. Hunter WD, Martuza RL, Feigenbaum F, et al. Attenuated, replication-competent herpes simplex virus type 1 mutant G207: safety evaluation of intracerebral injection in nonhuman primates. J Virol 1999;73:6319 26. Sundaresan P, Hunter WD, Martuza RL, et al. Attenuated, replication-competent herpes simplex virus type 1 mutant G207: safety evaluation in mice. J Virol 2000;74:3832 41. Markert JM, Medlock MD, Rabkin SD, et al. Conditionally replicating herpes simplex virus mutant, G207 for the treatment of malignant glioma: results of a phase I trial. Gene Ther 2000;7:867 74. Rampling R, Cruickshank G, Papanastassiou V, et al. Toxicity evaluation of replication-competent herpes simplex virus (ICP 34.5 null mutant 1716) in patients with recurrent malignant glioma. Gene Ther 2000;7:859 66. Carew JF, Kooby DA, Halterman MW, et al. Selective infection and cytolysis of human head and neck squamous cell carcinoma with sparing of normal mucosa by a cytotoxic herpes simplex virus type 1 (G207). Hum Gene Ther 1999;10:1599 606. Walker JR, McGeagh KG, Sundaresan P, et al. Local and systemic therapy of human prostate adenocarcinoma with the conditionally replicating herpes simplex virus vector G207. Hum Gene Ther 1999;10:2237 43. Oyama M, Ohigashi T, Hoshi M, et al. Intravesical and intravenous therapy of human bladder cancer by the herpes vector G207. Hum Gene Ther 2000;11:1683 93. Pawlik TM, Nakamura H, Yoon SS, et al. Oncolysis of diffuse hepatocellular carcinoma by intravascular administration of a replication-competent, genetically engineered herpesvirus. Cancer Res 2000;60:2790 5. Kasuya H, Nishiyama Y, Nomoto S, et al. Intraperitoneal delivery of hrR3 and ganciclovir prolongs survival in mice with disseminated pancreatic cancer. J Surg Oncol 1999;72: 136 41. Coukos G, Makrigiannakis A, Montas S, et al. Multi-attenuated herpes simplex virus-1 mutant G207 exerts cytotoxicity against epithelial ovarian cancer but not normal mesothelium and is suitable for intraperitoneal oncolytic therapy. Cancer Gene Ther 2000;7:275 83. Nicolo M, Chiocca EA. Marker gene transfer and oncolysis of human Y79 retinoblastoma cells mediated by herpes simplex virus mutants. Ophthalmic Res 1998;30:30 6. Bharatan N, Currier M, Cripe T. Differential susceptibility of pediatric sarcoma cells to oncolysis by conditionally replication-competent herpes simplex viruses. J Pediatr Hematol Oncol 2002;24:447 53. Yamamura H, Hashio M, Noguchi M, et al. Identification of the transcriptional regulatory sequences of human calponin promoter and their use in targeting a conditionally replicating herpes vector to malignant human soft tissue and bone tumors. Cancer Res 2001;61: 3969 77. Marshall E. Gene therapy death prompts review of adenovirus vector. Science 1999;286:2244 5. Brenner M. Reports of adenovector death are greatly exaggerated. Mol Ther 2000;1:205. Kirn D. Clinical research results with dl1520 (Onyx-015), a replication-selective adenovirus for the treatment of cancer: what have we learned? Gene Ther 2001;8:89 98.
1364
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
[113] Bischoff J, Kirn D, Williams A, et al. An adenovirus mutant that replicates selectively in p53deficient human tumor cells. Science 1996;274:373 6. [114] Heise C, Sampson-Johannes A, Williams A, et al. ONYX-015, an E1B gene-attenuated adenovirus, causes tumor-specific cytolysis and antitumoral efficacy that can be augmented by standard chemotherapeutic agents. Nat Med 1997;3:639 45. [115] Ries S, Brandts C, Chung A, et al. Loss of p14ARF in tumor cells facilitates replication of the adenovirus mutant dl1520 (ONYX-015). Nat Med 2000;6:1128 33. [116] Heise C, Lemmon M, Kirn D. Efficacy with a replication-selective adenovirus plus cisplatinbased chemotherapy: dependence on sequencing but not p53 functional status or route of administration. Clin Cancer Res 2000;6:4908 14. [117] Cripe T, Dunphy E, Holub A, et al. Fiber knob modifications overcome low, heterogeneous expression of the coxsackievirus-adenovirus receptor which limits adenovirus gene transfer and oncolysis for human rhabdomyosarcoma cells. Cancer Res 2001;61:2953 60. [118] Dmitriev I, Krasnykh V, Miller C, et al. An adenovirus vector with genetically modified fibers demonstrates expanded tropism via utilization of a coxsackievirus and adenovirus receptorindependent cell entry mechanism. J Virol 1998;72:9706 13. [119] Okegawa T, Li Y, Pong R-C, et al. Mechanism of coxsackie and adenovirus receptor (CAR) and its impact on prostate cancer therapy. Proceedings of the American Association of Cancer Research 2000;41:351. [120] Shinoura N, Yoshida Y, Tsunoda R, et al. Highly augmented cytopathic effect of a fiber-mutant E1B-defective adenovirus for gene therapy of gliomas. Cancer Res 1999;59:3411 6. [121] Fueyo J, Gomez-Manzano C, Alemany R, et al. A mutant oncolytic adenovirus targeting the Rb pathway produces anti-glioma effect in vivo. Oncogene 2000;19:2 12. [122] Heise C, Hermiston T, Johnson L, et al. An adenovirus E1A mutant that demonstrates potent and selective systemic anti-tumoral efficacy. Nat Med 2000;10:1134 9. [123] Rodriguez R, Schuur E, Lim H, et al. Prostate attenuated replication competent adenovirus (ARCA) CN706: a selective cytotoxic for prostate-specific antigen-positive prostate cancer cells. Cancer Res 1997;57:2559 63. [124] Yu D-C, Chen Y, Seng M, et al. The addition of adenovirus type 5 region E3 enables Calydon virus 787 to eliminate distant prostate tumor xenografts. Cancer Res 1999;59:4200 3. [125] Hallenbeck P, Chang Y-N, Hay C, et al. A novel tumor-specific replication-restricted adenoviral vector for gene therapy of hepatocellular carcinoma. Hum Gene Ther 1999;10:1721 33. [126] Chen R-H, McCormick F. Selective targeting to the hyperactive b-catenin/T-cell factor pathway in colon cancer cells. Cancer Res 2001;61:4445 9. [127] Adachi Y, Reynolds P, Yamamoto M, et al. A midkine promoter-based conditionally replicative adenovirus for treatment of pediatric solid tumors and bone marrow tumor purging. Cancer Res 2001;61:7882 8. [128] Heise C, Williams A, Xue S, et al. Intravenous administration of ONYX-015, a selectively replicating adenovirus, induces antitumoral efficacy. Cancer Res 1999;59:2623 8. [129] Reynolds P, Dmitriev I, Curiel D. Insertion of an RGD motif into the HI loop of adenovirus fiber protein alters the distribution of transgene expression of the systemically administered vector. Gene Ther 1999;6:1336 9. [130] Strong J, Coffey M, Tang D, et al. The molecular basis of viral oncolysis: usurpation of the Ras signaling pathway by reovirus. EMBO J 1998;17:3351 62. [131] Coffey M, Strong J, Forsyth P, et al. Reovirus therapy of tumors with activated Ras pathway. Science 1998;282:1332 4. [132] Wilcox M, Yang W, Senger D, et al. Reovirus as an oncolytic agent against experimental human malignant gliomas. J Natl Cancer Inst 2001;93:903 12. [133] Maltzman T, Mueller B, Schroeder J, et al. Ras oncogene mutations in childhood brain tumors. Cancer Epidemiol Biomarkers Prev 1997;6:239 43. [134] Grawe G, Cripe T. Myelodysplastic syndrome. Emedicine Journal 2001;2 [serial online]. Available at http://www.emedicine.com/ped/topic1527.htm. Accessed November 14, 2001. [135] Kiyoi H, Naoe T, Yokota S, et al. Internal tandem duplication of FLT3 associated with leuko-
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1365
[136] [137] [138] [139] [140] [141] [142] [143] [144]
[145] [146] [147]
[148] [149] [150] [151] [152] [153] [154] [155] [156] [157] [158] [159] [160]
[161]
cytosis in acute promyelocytic leukemia. Leukemia Study Group of the Ministry of Health and Welfare (Kohseisho). Leukemia 1997;11:1447 52. von Lintig F, Huvar I, Law P, et al. Ras activation in normal white blood cells and childhood acute lymphoblastic leukemia. Clin Cancer Res 2000;6:1804 10. Bautista D, Emanuel J, Granville C, et al. Identification of mutations in the Ki-ras gene in human retinoblastoma. Invest Ophthalmol Vis Sci 1996;37:2313 7. Gromeier M, Bossert B, Arita M, et al. Dual stem loops within the poliovirus internal ribosomal entry site control neurovirulence. J Virol 1999;73:958 64. Gromeier M, Lachmann S, Rosenfeld M, et al. Intergeneric poliovirus recombinants for the treatment of malignant glioma. Proc Natl Acad Sci U S A 2000;97:6803 8. Lange R, Peng X, Wimmer E, et al. The poliovirus receptor CD155 mediates cell-to-matrix contacts by specifically binding to vitronectin. Virology 2001;285:218 27. Masson D, Jarry A, Baury B, et al. Overexpression of the CD155 gene in human colorectal carcinoma. Gut 2001;49:236 40. Sinkovics J, Horvath J. New developments in the virus therapy of cancer: a historical review. Intervirology 1993;36:193 214. Sinkovics J, Horvath J. Newcastle disease virus (NDV): brief history of its oncolytic strains. J Clin Virol 2000;16:1 15. Lorence R, Reichard K, Katubig B, et al. Complete regression of human neuroblastoma xenografts in athymic mice after local newcastle disease virus therapy. J Natl Cancer Inst 1994;86: 1228 33. Lorence R, Katubig B, Reichard K, et al. Complete regression of human fibrosarcoma xenografts after local Newcastle disease virus therapy. Cancer Res 1994;54:6017 21. Pecora AL, Rizvi N, Cohen GI, et al. Phase I trial of intravenous administration of PV701, an oncolytic virus, in patients with advanced solid cancers. J Clin Oncol 2002;20:2251 66. Schirrmacher V, Haas C, Bonifer R, et al. Human tumor cell modification by virus infection: an efficient and safe way to produce cancer vaccine with pleiotropic immune stimulatory properties when using Newcastle disease virus. Gene Ther 1999;6:63 73. Peng K-W, Ahmann G, Pham L, et al. Systemic therapy of myeloma xenografts by an attenuated measles virus. Blood 2001;98:2002 7. Dang LH, Bettegowda C, Huso DL, et al. Combination bacteriolytic therapy for the treatment of experimental tumors. Proc Natl Acad Sci U S A 2001;98:15155 60. Evan GI, Vousden KH. Proliferation, cell cycle and apoptosis in cancer. Nature 2001;411:342 8. Blume-Jensen P, Hunter T. Oncogenic kinase signalling. Nature 2001;411:355 65. Druker BJ. Perspectives on the development of a molecularly targeted agent. Cancer Cell 2002;1:31 6. Sausville EA, El-Sayed Y, Monga M, et al. Signal transduction directed cancer treatments. Annu Rev Pharmacol Toxicol 2002;19:19. Sherr CJ. Cell cycle control and cancer. Harvey Lect 2000;96:73 92. Gilliland DG, Griffin JD. The roles of FLT3 in hematopoiesis and leukemia. Blood 2002;100: 1532 42. Gilliland DG, Griffin JD. Role of FLT3 in leukemia. Curr Opin Hematol 2002;9:274 81. Ning ZQ, Li J, Arceci RJ. Activating mutations of c-kit at codon 816 confer drug resistance in human leukemia cells. Leuk Lymphoma 2001;41:513 22. Ning ZQ, Li J, McGuinness M, et al. STAT3 activation is required for Asp(816) mutant c-Kit induced tumorigenicity. Oncogene 2001;20:4528 36. Levis M, Allebach J, Tse KF, et al. A FLT3-targeted tyrosine kinase inhibitor is cytotoxic to leukemia cells in vitro and in vivo. Blood 2002;99:3885 91. Levis M, Tse KF, Smith BD, et al. A FLT3 tyrosine kinase inhibitor is selectively cytotoxic to acute myeloid leukemia blasts harboring FLT3 internal tandem duplication mutations. Blood 2001;98:885 7. Tsujimura T. Role of c-kit receptor tyrosine kinase in the development, survival and neoplastic transformation of mast cells. Pathol Int 1996;46:933 8.
1366
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
[162] Piao X, Paulson R, van der Geer P, et al. Oncogenic mutation in the Kit receptor tyrosine kinase alters substrate specificity and induces degradation of the protein tyrosine phosphatase SHP-1. Proc Natl Acad Sci U S A 1996;93:14665 9. [163] Boissel N, Cayuela JM, Preudhomme C, et al. Prognostic significance of FLT3 internal tandem repeat in patients with de novo acute myeloid leukemia treated with reinforced courses of chemotherapy. Leukemia 2002;16:1699 704. [164] Schnittger S, Schoch C, Dugas M, et al. Analysis of FLT3 length mutations in 1003 patients with acute myeloid leukemia: correlation to cytogenetics, FAB subtype, and prognosis in the AMLCG study and usefulness as a marker for the detection of minimal residual disease. Blood 2002;100:59 66. [165] Thiede C, Steudel C, Mohr B, et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood 2002;99:4326 35. [166] Meshinchi S, Woods WG, Stirewalt DL, et al. Prevalence and prognostic significance of Flt3 internal tandem duplication in pediatric acute myeloid leukemia. Blood 2001;97:89 94. [167] Kondo M, Horibe K, Takahashi Y, et al. Prognostic value of internal tandem duplication of the FLT3 gene in childhood acute myelogenous leukemia. Med Pediatr Oncol 1999; 33:525 9. [168] Ma Y, Zeng S, Metcalfe DD, et al. The c-KIT mutation causing human mastocytosis is resistant to STI571 and other KIT kinase inhibitors; kinases with enzymatic site mutations show different inhibitor sensitivity profiles than wild-type kinases and those with regulatory-type mutations. Blood 2002;99:1741 4. [169] Heinrich MC, Blanke CD, Druker BJ, et al. Inhibition of KIT tyrosine kinase activity: a novel molecular approach to the treatment of KIT-positive malignancies. J Clin Oncol 2002;20: 1692 703. [170] Capdeville R, Buchdunger E, Zimmermann J, et al. Glivec (STI571, imatinib), a rationally developed, targeted anticancer drug. Nature Reviews in Drug Discovery 2002;1:493 502. [171] Druker BJ. STI571 (Gleevec) as a paradigm for cancer therapy. Trends Mol Med 2002;8:S14 8. [172] Kantarjian H, Sawyers C, Hochhaus A, et al. Hematologic and cytogenetic responses to imatinib mesylate in chronic myelogenous leukemia. N Engl J Med 2002;346:645 52. [173] Dematteo RP, Heinrich MC, El-Rifai WM, et al. Clinical management of gastrointestinal stromal tumors: before and after STI-571. Hum Pathol 2002;33:466 77. [174] Demetri GD. Targeting c-kit mutations in solid tumors: scientific rationale and novel therapeutic options. Semin Oncol 2001;28:19 26. [175] Corbin AS, Buchdunger E, Pascal F, et al. Analysis of the structural basis of specificity of inhibition of the abl kinase by STI571. J Biol Chem 2002;277:32214 9. [176] Gorre ME, Sawyers CL. Molecular mechanisms of resistance to STI571 in chronic myeloid leukemia. Curr Opin Hematol 2002;9:303 7. [177] von Bubnoff N, Schneller F, Peschel C, et al. BCR-ABL gene mutations in relation to clinical resistance of Philadelphia-chromosome-positive leukaemia to STI571: a prospective study. Lancet 2002;359:487 91. [178] Barthe C, Cony-Makhoul P, Melo JV, et al. Roots of clinical resistance to STI-571 cancer therapy. Science 2001;293:2163. [179] Haluska P, Dy G, Adjei A. Farnesyl transferase inhibitors as anticancer agents. Eur J Cancer 2002;38:1685. [180] Hoover RR, Mahon FX, Melo JV, et al. Overcoming STI571 resistance with the farnesyl transferase inhibitor SCH66336. Blood 2002;100:1068 71. [181] Folkman J. Anti-angiogenesis: new concept for therapy of solid tumors. Ann Surg 1972;175:409 16. [182] Ribatti D, Vacca A, Nico B, et al. Angiogenesis and anti-angiogenesis in neuroblastoma. Eur J Cancer 2002;38:750 7. [183] Hunt S. Technology evaluation: IMC-1C11, ImClone Systems. Current Opinions in Molecular Therapeutics 2001;3:418 24.
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
1367
[184] Mross K. Anti-angiogenesis therapy: concepts and importance of dosing schedules in clinical trials. Drug Resistance Updates 2000;3:223 35. [185] Cherrington JM, Strawn LM, Shawver LK. New paradigms for the treatment of cancer: the role of anti-angiogenesis agents. Adv Cancer Res 2000;79:1 38. [186] Kroemer G. The proto-oncogene Bcl-2 and its role in regulating apoptosis. Nat Med 1997;3: 614 20. [187] Keith FJ, Bradbury DA, Zhu YM, et al. Inhibition of bcl-2 with antisense oligonucleotides induces apoptosis and increases the sensitivity of AML blasts to Ara-C. Leukemia 1995;9: 131 8. [188] Tamm I, Dorken B, Hartmann G. Antisense therapy in oncology: new hope for an old idea? Lancet 2001;358:489 97. [189] Banerjee D. Genasense (Genta Inc). Current Opinions in Investigational Drugs 2001;2:574 80. [190] Vogelstein B, Kinzler KW. Achilles heel of cancer? Nature 2001;412:865 6. [191] Lowe SW, Jacks T, Housman DE, Ruley HE. Abrogation of oncogene-associated apoptosis allows transformation of p53-deficient cells. Proc Natl Acad Sci U S A 1994;91:2026 30. [192] Lowe SW, Ruley HE, Jacks T, et al. p53-dependent apoptosis modulates the cytotoxicity of anticancer agents. Cell 1993;74:957 67. [193] Clayman GL, el-Naggar AK, Roth JA, et al. In vivo molecular therapy with p53 adenovirus for microscopic residual head and neck squamous carcinoma. Cancer Res 1995;55:1 6. [194] Fujiwara T, Grimm EA, Mukhopadhyay T, et al. A retroviral wild-type p53 expression vector penetrates human lung cancer spheroids and inhibits growth by inducing apoptosis. Cancer Res 1993;53:4129 33. [195] Foster BA, Coffey HA, Morin MJ, et al. Pharmacological rescue of mutant p53 conformation and function. Science 1999;286:2507 10. [196] Wang H, Prasad G, Buolamwini JK, et al. Antisense anticancer oligonucleotide therapeutics. Curr Cancer Drug Targets 2001;1:177 96. [197] Lane DP, Lain S. Therapeutic exploitation of the p53 pathway. Trends Mol Med 2002;8:S38 42. [198] Cairns BR. Emerging roles for chromatin remodeling in cancer biology. Trends Cell Biol 2001; 11:S15 21. [199] Rountree MR, Bachman KE, Herman JG, et al. DNA methylation, chromatin inheritance, and cancer. Oncogene 2001;20:3156 65. [200] Redner RL, Wang J, Liu JM. Chromatin remodeling and leukemia: new therapeutic paradigms. Blood 1999;94:417 28. [201] Melnick A, Licht JD. Histone deacetylases as therapeutic targets in hematologic malignancies. Curr Opin Hematol 2002;9:322 32. [202] Johnstone RW. Histone-deacetylase inhibitors: novel drugs for the treatment of cancer. Nature Reviews in Drug Discovery 2002;1:287 99. [203] Slack JL. Biology and treatment of acute progranulocytic leukemia. Curr Opin Hematol 1999;6:236 40. [204] Minucci S, Nervi C, Lo Coco F, et al. Histone deacetylases: a common molecular target for differentiation treatment of acute myeloid leukemias? Oncogene 2001;20:3110 5. [205] Waxman S. Differentiation therapy in acute myelogenous leukemia (non-APL). Leukemia 2000;14:491 6. [206] Ferrara FF, Fazi F, Bianchini A, et al. Histone deacetylase-targeted treatment restores retinoic acid signaling and differentiation in acute myeloid leukemia. Cancer Res 2001;61:2 7. [207] Warrell Jr RP, He LZ, Richon V, et al. Therapeutic targeting of transcription in acute promyelocytic leukemia by use of an inhibitor of histone deacetylase. J Natl Cancer Inst 1998;90:1621 5. [208] Fournel M, Trachy-Bourget MC, Yan PT, et al. Sulfonamide anilides, a novel class of histone deacetylase inhibitors, are antiproliferative against human tumors. Cancer Res 2002;62:4325 30. [209] He LZ, Tolentino T, Grayson P, et al. Histone deacetylase inhibitors induce remission in transgenic models of therapy-resistant acute promyelocytic leukemia. J Clin Invest 2001;108: 1321 30.
1368
R.J. Arceci, T.P. Cripe / Pediatr Clin N Am 49 (2002) 13391368
[210] Kramer OH, Gottlicher M, Heinzel T. Histone deacetylase as a therapeutic target. Trends Endocrinol Metab 2001;12:294 300. [211] Gilbert J, Baker SD, Bowling MK, et al. A phase I dose escalation and bioavailability study of oral sodium phenylbutyrate in patients with refractory solid tumor malignancies. Clin Cancer Res 2001;7:2292 300. [212] Saito A, Yamashita T, Mariko Y, et al. A synthetic inhibitor of histone deacetylase, MS-27 275, with marked in vivo antitumor activity against human tumors. Proc Natl Acad Sci U S A 1999;96:4592 7. [213] Miki K, Shimizu E, Yano S, et al. Demethylation by 5-aza-20-deoxycytidine (5-azadC) of p16INK4A gene results in downregulation of vascular endothelial growth factor expression in human lung cancer cell lines. Oncol Res 2000;12:335 42. [214] DiCroce L, Raker VA, Corsaro M, et al. Methyltransferase recruitment and DNA hypermethylation of target promoters by an oncogenic transcription factor. Science 2002;295:1079 82. [215] Robertson KD, Jones PA. DNA methylation: past, present and future directions. Carcinogenesis 2000;21:461 7. [216] Teitz T, Wei T, Valentine MB, et al. Caspase 8 is deleted or silenced preferentially in childhood neuroblastomas with amplification of MYCN. Nat Med 2000;6:529 35.
Você também pode gostar
- Antikoagulan Untuk VTEDocumento6 páginasAntikoagulan Untuk VTEVendi Cahyadi RiandikaAinda não há avaliações
- Morning Report May 30 2014: Supervisor: DM: Akbar, Amandha, Ryan, VendiDocumento6 páginasMorning Report May 30 2014: Supervisor: DM: Akbar, Amandha, Ryan, VendiVendi Cahyadi RiandikaAinda não há avaliações
- Jurnal Reading Diabetes InsipidusDocumento39 páginasJurnal Reading Diabetes InsipidusVendi Cahyadi RiandikaAinda não há avaliações
- 10.1177 17588359221110171Documento12 páginas10.1177 17588359221110171Vendi Cahyadi RiandikaAinda não há avaliações
- KetDocumento6 páginasKetVendi Cahyadi RiandikaAinda não há avaliações
- MR 11-02-2014 K-II LamaDocumento9 páginasMR 11-02-2014 K-II LamaVendi Cahyadi RiandikaAinda não há avaliações
- Differential Diagnosis: Ial TestsDocumento1 páginaDifferential Diagnosis: Ial TestsVendi Cahyadi RiandikaAinda não há avaliações
- HypochondriasisDocumento12 páginasHypochondriasisVendi Cahyadi RiandikaAinda não há avaliações
- Morning Report May 31 2014: Supervisor: Dr. Agus Thoriq SP, OG DM: Dandi, Ardi, Yos, Ryan, VendiDocumento10 páginasMorning Report May 31 2014: Supervisor: Dr. Agus Thoriq SP, OG DM: Dandi, Ardi, Yos, Ryan, VendiVendi Cahyadi RiandikaAinda não há avaliações
- MR 06-01-2014 GemelliDocumento6 páginasMR 06-01-2014 GemelliVendi Cahyadi RiandikaAinda não há avaliações
- Morning Report May 31 2014: Supervisor: Dr. Agus Thoriq SP, OG DM: Dandi, Ardi, Yos, Ryan, VendiDocumento10 páginasMorning Report May 31 2014: Supervisor: Dr. Agus Thoriq SP, OG DM: Dandi, Ardi, Yos, Ryan, VendiVendi Cahyadi RiandikaAinda não há avaliações
- MR 13Documento6 páginasMR 13Vendi Cahyadi RiandikaAinda não há avaliações
- Morning Report May 31 2014: Supervisor: Dr. Agus Thoriq SP, OG DM: Dandi, Ardi, Yos, Ryan, VendiDocumento10 páginasMorning Report May 31 2014: Supervisor: Dr. Agus Thoriq SP, OG DM: Dandi, Ardi, Yos, Ryan, VendiVendi Cahyadi RiandikaAinda não há avaliações
- Case Report: IdentityDocumento5 páginasCase Report: IdentityVendi Cahyadi RiandikaAinda não há avaliações
- KPD Drip Oxytocin-18.04.12Documento6 páginasKPD Drip Oxytocin-18.04.12Vendi Cahyadi RiandikaAinda não há avaliações
- 27 Mei PER+postermDocumento6 páginas27 Mei PER+postermVendi Cahyadi RiandikaAinda não há avaliações
- Ruang C Meja Pengawas SEATING LayoutDocumento1 páginaRuang C Meja Pengawas SEATING LayoutVendi Cahyadi RiandikaAinda não há avaliações
- Lampiran 6bDocumento1 páginaLampiran 6bVendi Cahyadi RiandikaAinda não há avaliações
- Ruang D (Done)Documento1 páginaRuang D (Done)Vendi Cahyadi RiandikaAinda não há avaliações
- Hiit JournalsDocumento1 páginaHiit JournalsVendi Cahyadi RiandikaAinda não há avaliações
- OligoDocumento9 páginasOligoVendi Cahyadi RiandikaAinda não há avaliações
- Lampiran 6. Hasil Analisis Data: Case Processing SummaryDocumento3 páginasLampiran 6. Hasil Analisis Data: Case Processing SummaryVendi Cahyadi RiandikaAinda não há avaliações
- Pengaruh Push Up Terhadap Tekanan Intraokular: Eko PoerwantoDocumento6 páginasPengaruh Push Up Terhadap Tekanan Intraokular: Eko PoerwantoKarman DjamaluddinAinda não há avaliações
- Hari SeninDocumento9 páginasHari SeninVendi Cahyadi RiandikaAinda não há avaliações
- Babyloss PreeclampsiaDocumento4 páginasBabyloss PreeclampsiaVendi Cahyadi RiandikaAinda não há avaliações
- Hiit Vs Moderate TrainingDocumento1 páginaHiit Vs Moderate TrainingVendi Cahyadi RiandikaAinda não há avaliações
- Hiit JournalsDocumento1 páginaHiit JournalsVendi Cahyadi RiandikaAinda não há avaliações
- PediatricDocumento2 páginasPediatricVendi Cahyadi RiandikaAinda não há avaliações
- Hiit Vs Moderate TrainingDocumento1 páginaHiit Vs Moderate TrainingVendi Cahyadi RiandikaAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Cardioversion and DefibrillationDocumento12 páginasCardioversion and DefibrillationNAGARAJ100% (1)
- Spinal Anesthesia - Technique - UpToDateDocumento37 páginasSpinal Anesthesia - Technique - UpToDateSamir Perez CasadiegoAinda não há avaliações
- Formulation and Evaluation of An Injectable Soluti PDFDocumento7 páginasFormulation and Evaluation of An Injectable Soluti PDFdhirazhrAinda não há avaliações
- 6.PIO TTG Seven Step Handling QueryDocumento29 páginas6.PIO TTG Seven Step Handling QueryNurinaAdaniSukiakusumahAinda não há avaliações
- Chapter 017Documento18 páginasChapter 017wn4tb100% (2)
- Self AttuneDocumento6 páginasSelf AttuneBodibodi100% (2)
- Vertigo Vertigoheel 2001Documento7 páginasVertigo Vertigoheel 2001Dr. Nancy Malik100% (1)
- PsychiaDocumento9 páginasPsychiaNoel RafaelAinda não há avaliações
- The Pathophysiology of Chemotherapy-Induced Nausea and VomitingDocumento13 páginasThe Pathophysiology of Chemotherapy-Induced Nausea and VomitingLeoberto Batista Pereira SobrinhoAinda não há avaliações
- Ampicillin PDFDocumento3 páginasAmpicillin PDFandriAinda não há avaliações
- Insomnia PowerpointDocumento16 páginasInsomnia Powerpointapi-255944865Ainda não há avaliações
- Dailymed - Nlm.nih - Gov METRONIDAZOLEDocumento16 páginasDailymed - Nlm.nih - Gov METRONIDAZOLELip StickAinda não há avaliações
- Clasic MindfullneseDocumento15 páginasClasic Mindfullneseayu yuliantiAinda não há avaliações
- MeconiumDocumento46 páginasMeconiumМаnal AlJobranAinda não há avaliações
- Relationship Between The Five Element Points and Some Major Physiological SystemsDocumento4 páginasRelationship Between The Five Element Points and Some Major Physiological SystemsNilton Benfatti100% (1)
- Lived Experience Leading The Way: Peer Support in Mental HealthDocumento4 páginasLived Experience Leading The Way: Peer Support in Mental HealthCarolyn AndersonAinda não há avaliações
- AripripazoleDocumento13 páginasAripripazoleOneng IfayaniAinda não há avaliações
- Respiratory Patient Pathway INT Issue 1 WebDocumento44 páginasRespiratory Patient Pathway INT Issue 1 Webmd edaAinda não há avaliações
- Ws Viii Dyspepsia - Dr. Ignatia Sinta Murti, SP - Pd-KgehDocumento79 páginasWs Viii Dyspepsia - Dr. Ignatia Sinta Murti, SP - Pd-KgehSriHandaryatiAinda não há avaliações
- Gerd NotesDocumento14 páginasGerd NotesNguyen Phuong100% (1)
- Senior Citizen Policy - 0Documento14 páginasSenior Citizen Policy - 0nywd806033Ainda não há avaliações
- Paracetamol Use Dec 2008Documento30 páginasParacetamol Use Dec 2008Nararto PrijogoAinda não há avaliações
- ZetamycinDocumento6 páginasZetamycinelcapitano vegetaAinda não há avaliações
- 2 - Ospina 2007 ArqDocumento472 páginas2 - Ospina 2007 ArqMarcia KoikeAinda não há avaliações
- Web BrochureDocumento12 páginasWeb BrochureZoe Brigden-SmallwoodAinda não há avaliações
- Ocular Drug DeliveryDocumento99 páginasOcular Drug DeliveryRishi ModyAinda não há avaliações
- TrismusDocumento9 páginasTrismusJoão de BarrosAinda não há avaliações
- Monkey Bite ProtocolDocumento2 páginasMonkey Bite ProtocolOngky AristianAinda não há avaliações
- DKA Protocol With Calculation SheetDocumento7 páginasDKA Protocol With Calculation SheetAmanda Marie Best OsbourneAinda não há avaliações