Escolar Documentos
Profissional Documentos
Cultura Documentos
Angina
Enviado por
Sarah RepinDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Angina
Enviado por
Sarah RepinDireitos autorais:
Formatos disponíveis
Angina
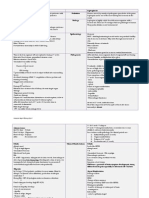
What are the common conditions that can present with chest pain? The answer Cardiovascular: o Angina o Acute myocardial infraction o Pericarditis o Aortic dissection Gastrointestinal: o Reflux esophagitis Pulmonary: o Pneumothroax o Pleuritis/pneumonia o Pulmonary embolus/infarction Musculoskeletal: o Traumatic injury o Costochondritis o Herpes zoster Somatization: o Anxiety
What are the characteristics of pain due to Angina? The answer Clinical Syndrome Myocardial ischemia Precordial discomfort, mostly felt beneath sternum Vague ache to crushing sensation Radiates to left shoulder, inside left arm, into throat, jaws, epigastrium Usually persists no more than few minutes (5-10 minutes) Triggered by physical activity, cold air Relieved by rest or sublingual Nitroglycerin
What are the characteristics of pain due to Acute myocardial infarction? How does it differ from angina? The answer Crushing chest pain with or without radiation. Lasts longer >20 minutes Not relieved by rest or Nitroglycerine Diaphoresis, nausea or vomiting ECG changes
Cardiac enzymes changes
What are the characteristics of pain due to reflux esophagitis ? The answer esophageal spasm may be severe and centered in the chest although it may also bore to the back. could also be relieved by nitroglycerin worse in supine position worse following meals relieved by antacids or acid blockers
What are the characteristics of pain due to Pericarditis ? The answer Precardiac, sharp, persistent. Worse in recumbent position Relieved by sitting.
What are the characteristics of pain due to Dissecting aorta ? The answer Sharp "tearing" pain radiating to back
What are the characteristics of pain due to Chest wall Lesions ? The answer Muscular skeletal pain often is o localized o with point tenderness o it mimics pleuritic pain during inspiration.
What are the characteristics of pain due to Pneumothorax ? The answer pain is sudden in onset localized sharp worse on deep breathing and coughing
associated with shortness of breath
Pleuritic pain of pneumonia has the same characteristics.
Describe Coronary arterial system. The answer Right and Left main coronary arteries. o Arising from aorta directly There is some collateral circulation but they mostly behave like end arteries.
How is flow of blood to myocardium is regulated? The answer Coronary blood flow during diastole Increased myocardial activity increases blood flow ( exercise, LV hypertrophy) Direct from ventricular chamber to myocardium. (small contribution)
Describe the pathogenesis of myocardial ischemia. The answer Decreased blood flow o Critical coronary artery obstruction (>70%) Atherosclerosis Spasm (Idiopathic, Cocaine) Increased demand o Increased cardiac work Calcific Aortic stenosis Hypertrophic subaortic stenosis
Describe the patho-physiology of myocardial ischemia The answer Myocardial O2 demand exceeds the ability of the coronary arteries to supply oxygenated blood. Coronary sinus blood pH falls/Cellular K loss occurs/EKG abnormalities appear Ventricular performance deteriorates/LV diastolic pressure rises Hypoxic metabolites/Discomfort
What are the risk factors for coronary atherosclerosis? The answer Hypertension Diabetes Mellitus Hypercholesterolemia Cigarette smoking Family history of ischemic heart disease
What do you understand by the terms nocturnal angina, crescedndo angina, angina decubitus, unstable angina, Syndrome X The answer Nocturnal angina: Angina may occur at night (nocturnal angina) preceded by a dream Crescendo angina: Attacks of angina increase in frequency to a fatal outcome Angina decubitus: Angina occuring spontaneously at rest Unstable angina: o increased intensity o decreased threshold of stimulus o longer duration o occurrence when the patient is sedentary or waking from sleep Syndrome X: o typical symptoms of angina relieved by rest or nitroglycerin o the exercise test is abnormal o yet the coronary arteriogram is normal. Prinzmetal angina:
Can angina disappear spontaneously? The answer: Yes if adequate collateral coronary circulation develops if the ischemic area becomes infarcted if heart failure or intermittent claudication supervenes and limits activity
What do you know about HDL and LDL cholesterol? The answer HDL:
Good cholesterol. helps clear the body of cholesterol o by facilitating "reverse cholesterol transport"
LDL: Bad cholesterol when it exceeds normal levels. Most atherogenic lipoprotein Delivers cholesterol to peripheral tissues cells Triggers cascade of events leading to the development of foam cells o by clearance of a low-affinity "scavenger" pathway
What is the diagnostic strategy for evaluation of angina? The answer Diagnosis based primarily on history of characteristic pain Reversible ischemic ECG changes Characteristic relief of discomfort with sub-lingual Nitroglycerin Additional evaluation when the diagnosis is in doubt or interventional therapy is required
What are the ECG changes of angina? The answer Reversible ischemic ECG changes are seen during a spontaneous attack. o ST segment depression (typically) ST segment depression >= 0.1 millivolts (1 mm on the ECG when properly calibrated) lasting >= 0.08 sec. o ST segment elevation o decreased R-wave height o intraventricular or bundle branch conduction disturbances o arrhythmia (usually ventricular extrasystoles). Between attacks, the ECG at rest could be normal
How is Exercise stress ECG testing useful in the evaluation of angina? Exercise stress ECG testing: o Response of ECG to graded exercise o Ischemic response supports Angina o With chest pain specificity 70%: sensitivity 90% in men o Negative test is a reliable indicator of no disease.
What is the role of coronary angiogram in evaluation of angina? The answer Coronary angiography o Documents the extent of anatomic coronary artery occlusion o Obstruction is physiologically significant when the luminal diameter is reduced >70%
When will you consider exercise test and coronary angiogram in the evaluation of a patient with angina? The answer Exercise test: Diagnosis is not certain and Patient is stable Prior to coronary angiogram
Coronary angiogram: In unstable angina Diagnosis not certain Interventional therapy is planned It would be reasonable to obtain an exercise test and depending on the result of that test, proceed with a cardiac catheterization. If there is a high prior probability of coronary artery disease, then a negative exercise test may well be considered a false negative and one would go ahead with a Coronary Angiogram .
What is the immediate treatment of angina? How can you increase coronary blood flow immediately? The answer Rest (decrease demand for oxygen) Sublingual nitroglycerine o Organic nitrates are excellent drugs for the treatment of stable angina. o Nitroglycerin is a potent smooth-muscle relaxer and vasodilator.
How soon can you expect relief of pain with use of sublingual nitroglycerine? What are the usual instructions to apatient on the use of the drug? The answer Dramatic relief within 1.5 to 3 minutes Dose may be repeated after 5 minutes three times if there is no relief Patient should carry the tablets always
Drug looses potency/ refill small amounts frequently
What is the mechanism of action of nitroglycerine? The answer Decrease oxygen demand o The organic nitrates decrease ventricular wall stress (oxygen demand) by reducing both preload and after load {wall stress = (P x r)/ (2 x wall thickness)} This results from a primary action on venous capacitance vessels with a more minor effect on arterioles. Increase coronary blood flow and exert favorable effects on oxygen supply. o The reduced ventricular pressure during both diastole and systole will decrease extra vascular coronary resistance (compressive forces). o Dilate collateral vessels and produce a small dilatation of stenotic coronary arteries, when the stenosis is eccentric. The organic nitrates (R-O-NO2) combine with cysteine (R-SH) in the vessel wall to form a nitrosothiol that releases nitric oxide (NO).
What is/are the option to prevent further attacks of angina? The answer Long-acting nitrates o nitroglycerine patch o isosorbide dinitrate. Beta-blockers block sympathetic stimulation of the heart (reduce Systolic pressure, heart rate, contractility, cardiac output) and reduce myocardial O2 demand. Calcium channel blockers are vasodilators and are useful when angina is due to spasm or associated with Hypertension.
Long-acting nitrates alone or with beta-blockers or with calcium channel blockers or all three can be used based on clinical need.
How can you alter risk factors? The answer Smoking: Start smoking cessation programs Hypertension: Anti-hypertensive medication to lower blood pressure Hypercholesterolemia: An HMG-CoA reductase inhibitor to lower cholesterol
How does HMG-CoA reductase inhibitor lowers cholesterol? The answer
Synthesis o HMG-CoA reductase inhibitors block the rate limiting enzyme for the synthesis of cholesterol. Catabolism o Serum cholesterol levels fall not only from a reduced synthetic rate but from an upregulation of LDL receptors in hepatocytes and an increased rate of LDL catabolism from the circulating pool.
What is the goal of theapy with HMG-CoA reductase inhibitors? What is the effect on existing atherosclerotic changes? The goal of this therapy (combined with dietary restrictions) is o to reduce serum cholesterol to <190 mg/dL. o to reduce LDL cholesterol to <100mg/DL They do reduce the rate of progression of coronary artherosclerotic lesion and increase the frequency of regression. They do reduce the risk of death due to coronary artery disease and risk of nonfatal myocardial infarction.
What options do we have to prevent development of thrombosis in a coronary artery with atheromatous changes? The answer Aspirin reduces the risk of coronary thrombosis ( heart attack ) in patients with coronary artery disease' There is a strong indication for daily aspirin (81 mg/day) as prophylactic therapy. Aspirin causes decreased platelet aggregation. o by irreversible inhibition of platelet cyclooxygenase and decreased thromboxane A2 production
What are the options we have to relieve mechanical obstruction of Coronary arteries ? The answer Angioplasty: Involves insertion of a balloon tipped catheter into an artery at the site of partial obstruction Inflation of the balloon can rupture the intima and media and dramatically dilate the obstruction In a patient with suitable anatomic lesions Stents can be placed can be placed to reduce reocclusion
Coronary Artery Bypass Surgery Venous graft Internal mammary artery graft
Você também pode gostar
- AKI Guideline KDIGODocumento141 páginasAKI Guideline KDIGOSarah RepinAinda não há avaliações
- Wound BallisticsDocumento47 páginasWound BallisticsSarah RepinAinda não há avaliações
- Cardiac Arrhythmias: A. Supraventricular TachyarrhythmiaDocumento10 páginasCardiac Arrhythmias: A. Supraventricular TachyarrhythmiaSarah RepinAinda não há avaliações
- Acute GastritisDocumento28 páginasAcute GastritisSarah Repin50% (2)
- HFRS Vs LeptospirosisDocumento5 páginasHFRS Vs LeptospirosisSarah RepinAinda não há avaliações
- Trauma - Secondary SurveyDocumento39 páginasTrauma - Secondary SurveySarah RepinAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Reading Unit 9 CardiologyDocumento4 páginasReading Unit 9 CardiologyChristian SilvaAinda não há avaliações
- p56 - p110Documento6 páginasp56 - p110Bhushan D ThombareAinda não há avaliações
- ECG in Emergency MedicineDocumento228 páginasECG in Emergency MedicineM.FADLIAinda não há avaliações
- Heart Failure Mcqs ExplainedDocumento2 páginasHeart Failure Mcqs ExplainedHawi BefekaduAinda não há avaliações
- Drug Study-DobutamineDocumento2 páginasDrug Study-DobutamineCyril Joy N. FernandoAinda não há avaliações
- Eng - OUT SOURCE & Recognised PVT Hosp - To EDPDocumento8 páginasEng - OUT SOURCE & Recognised PVT Hosp - To EDPMinerva Medical Treatment Pvt LtdAinda não há avaliações
- Dilated CardiomyopathyDocumento16 páginasDilated CardiomyopathyRosemarie Manatad TerioAinda não há avaliações
- Myocardial Infarction: Seminar OnDocumento17 páginasMyocardial Infarction: Seminar OnSuhas IngaleAinda não há avaliações
- Resume For ApplicationDocumento3 páginasResume For Applicationapi-157341650Ainda não há avaliações
- 319-Article Text-1439-1-10-20221110Documento5 páginas319-Article Text-1439-1-10-20221110Arfina YusufAinda não há avaliações
- MRCPCH Part 1 Questions With Individual Subject Summaries 4eDocumento52 páginasMRCPCH Part 1 Questions With Individual Subject Summaries 4ePasTestBooks88% (25)
- BLS ExamDocumento4 páginasBLS ExammanalgalmutairiAinda não há avaliações
- Percutaneous Interventional Cardiovascular Medicine - The PCR-EAPCI TextbookDocumento15 páginasPercutaneous Interventional Cardiovascular Medicine - The PCR-EAPCI TextbookRanda TabbahAinda não há avaliações
- 2018 Book PrimaryAngioplastyDocumento339 páginas2018 Book PrimaryAngioplastyRami El-Mokdad100% (2)
- Sgarbossa CrtiteriaDocumento4 páginasSgarbossa Crtiteriaanisah astiraniAinda não há avaliações
- Rigel Uni Sim Lite DatasheetDocumento5 páginasRigel Uni Sim Lite Datasheetmailalexmd.vrn.ruAinda não há avaliações
- Modified Valsalva Manoeuvre For Supraventricular TachycardiaDocumento3 páginasModified Valsalva Manoeuvre For Supraventricular TachycardiaJyotirmayeeAinda não há avaliações
- 2021 Meng Arendt Obstetric Anesthesia and Heart DiseaseDocumento20 páginas2021 Meng Arendt Obstetric Anesthesia and Heart DiseaseRocio Ayaque AguirreAinda não há avaliações
- Mekanisme Fetal TakikardiDocumento2 páginasMekanisme Fetal TakikardifinandaAinda não há avaliações
- Anti Arrhythmic Drugs - FINALDocumento25 páginasAnti Arrhythmic Drugs - FINALThanyun Yun100% (1)
- Stemi Vs NstemiDocumento31 páginasStemi Vs NstemiFadhilAfifAinda não há avaliações
- CVS & Hypolipidemic Drugs-NursingDocumento71 páginasCVS & Hypolipidemic Drugs-NursingManikanta Guptha100% (1)
- Internal Medicine Residency BrochureDocumento23 páginasInternal Medicine Residency Brochuredanskip1025Ainda não há avaliações
- ECG Interpretation For ACLSDocumento27 páginasECG Interpretation For ACLSZH. omg sarAinda não há avaliações
- CV DR Pedro Brugada I TerradellasDocumento244 páginasCV DR Pedro Brugada I TerradellasbirbiloAinda não há avaliações
- Angina: Angina:chest Pain Caused by Reduced Blood Flow To The Heart MuscleDocumento11 páginasAngina: Angina:chest Pain Caused by Reduced Blood Flow To The Heart MuscleMohammed Falih HassanAinda não há avaliações
- Find Biomime Morph - A Drug Eluting Stent Designed by Meril LifeDocumento2 páginasFind Biomime Morph - A Drug Eluting Stent Designed by Meril LifeAnkit ShirkeAinda não há avaliações
- (KEL 1) Jurnal IMA (Pak Arif)Documento8 páginas(KEL 1) Jurnal IMA (Pak Arif)Nurul HendrianiAinda não há avaliações
- Insuficienţa Renală Acută (IRA) Acute Kidney Injury (AKI) : Dr. Cristina StoicaDocumento58 páginasInsuficienţa Renală Acută (IRA) Acute Kidney Injury (AKI) : Dr. Cristina StoicaDafina DanielAinda não há avaliações
- HFDocumento162 páginasHFOmar AyashAinda não há avaliações