Escolar Documentos
Profissional Documentos
Cultura Documentos
14 Nematodes Filarial Worms
Enviado por
Shivam PatelDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
14 Nematodes Filarial Worms
Enviado por
Shivam PatelDireitos autorais:
Formatos disponíveis
Filarial Worms
7 November 2011
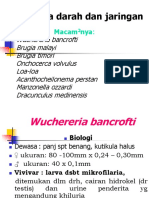
I. Filarial diseases A. Introduction 1. Superfamily Filaroidea a. Wuchereria bancrofti b. Brugia malayi c. Onchocerca volvulus d. Loa loa e. Mansonella perstans f. M. ozzardi g. M. streptocerca 2. blood and tissue habitats-live in blood of tissues 3. vector transmission 4. ovoviviparous- adult females. Eggs hatch in uterus, microfilariae(mf) released 5. microfilaria a. advanced embryos- not as developed as L1 in other species, they are instead called advanced embryo b. sheath- maybe sheathed- flexible egg shell- covering membrane-blood dwelling spp. c. long-lived- survive in blood for many years d. vector blood meal- ingested with blood meal by suitable vector e. identification nuclei- stain mf, location of nuclei f. periodicity- mf in peripheral blood only at certain times of day. Ex. W. bancrofti-maximum # of mf in peripheral blood during 10 PM to 2 AM. Vector=night-feeding mosquito. Day-mf in blood vessels of deep tissue- primary in lungs. Causes-physiology of host while sleeping. Decreases body time and H2O excretion by kidneys and increases body acidity. II. Wuchereria bancrofti. Elephantiasis, lymphatic filariasis A. Life cycle- adult worms live in major lymphatic ducts of humans- females- 8-10 cm, males-40mm.sheathed mf. 1. Periodicity 2. mosquito- Mf in lymphbloodingested by mosquito. Inside mosquitomoltL1L2L3-infective stage. L3 into proboscis, mosquito injected- lubricant, anticoagulant. L3 injected into host. L3 in skin of phlymphaticmolt to L4 molt to adult B. Pathology 1. incubation-asymptomatic, no detectable microfilaremia(mf in blood). ELISAdetect antigen. 2. acute(=inflammatory) response to antigen released from degenerating adults. a. episodic adenolymphangitis- (ADL)- inflammation of lymph nodes, inguinal, attacks of fever, chills + edema 3. chronic(=obstructive) 10-20 years after 1st exposure. Lymph tissue blockedworms, granulomas, fibrous connective tissue a. Grade I lymphedema- transient+soft, pressure- pit forms in skin. Treatment- rest and elevation of limb.
b. Grade II lymphedema-hard + permanent-does not pit on pressure. c. Grade III lymphedema-subcutaneous thickening outer skin layer. Hypertrophy-increase cell sizehyperkeratosis- nodules and fissures. d. Elephantiasis-repeated acute and chronic attaches legs, arms, scrotum. Chromic Lymph blockagefat fibrous tissue, psycholigcal+social impact. Rarely in people younger than 25 years old and mostly in people older than 40 yrs old. C. Diagnosis- mf in blood at times of peak periodicity 1. circulating filarial antigen test- (CFA)- any times and only blood droplets 2. ultrasonography- visualize worms in ducts. filarial dance D. Treatment 1. hygiene- wash-soap and water. Shoes and antibiotic creams. Raise limbs and exercise. 2. drugs a. diethylcarbamazine-(DEC)- may increase hosts immune responseaffects worm cuticle release of antigenic compounds b. albendazole- disrupts metabolic function c. ivermectin-increase GABA E. Costs associated with W. bancrofti infection 1. Costs of disease- permanent long-term disability, decrease in economic productivity and social loss 2. Costs of treatment- DEC- single annual dose- cost $0.02/person/year. DEC fortified salt- tasteless, survives cooking- cost- about $0.30/person/year. Albendazole- single annual dose- donated by smith-kline beecham- $0. Ivermectin- single annual dose- donated by Merck- $0. 3. Costs of diagnosis- CFA test- $1/test. Duagbisus +treatment=$1.32/person/yr. Ex. India- losses- $800 million-1 billion per year. F. Control of lymphatic filariasis- one of the 7 diseases targeted by WHO 1. elimination- reduction to 0 in a particular area 2. eradication- reduction to 0 worldwide. Bracunculus, T. solum, measles, mumps, rubella, polio. 3. characteristics-no amplification in vectors, no animal reservoirs, simple and accurate diagnostic tests, treatment- effective and inexpensive, variety of drugs, collateral health benefits, plans of actions, drug companies. III. Brugia malayi A. Adults- female- 55mm. males-25mm B. Mf- sheathed, do undergo periodicity-inperipheral blood at night, vector=mosquito C. South and southeast asia D. Same as w. bancrofti for life cycle, pathology, diagnosis, and treatment. IV. Onchocerca volvulus River blindness- Africa, central, South America by Slave trade.
A. Life cycle- female-50cm male-40cm. in nodules under skin- oncnocercoma- some subcutaneous. Others- deep tissue. 9-10 yras . remain in skin, no periodcity, positively phototactic ingested by blackfly. 1. microfilaria2. Simulian fly- ingested by this black fly-blood meal. Scarifies skin, blood of blood, fly laps up blood + mf. Insdie black fly-mfhemocoelL1L2L3migrates to mouth parts. L3 infect next host into skin. In skin, L4adult B. Pathology 1. adults onchocercoma 2. onchocerciasis-by mf, skin+eyes a. microfilaria alive-little pathology b. microfilaria dead/degenerating-response to bacterium present in mf c. Wolbachia intracellular, inherited, found in many insects + crystaceans. Found in many filarial worm i. endosymbiont ii. LPS- molbachia cell wall- lipopolysaccharide. Endotoxin, stimulates host inflammatory response. Antibiotics-tertracycline-effective. Penicillin and liprofloxiacin-ineffective. d. acute skin lesions- mf in skin, persistent, itchy rash.scratch open skinsecondary bacterial infection, skin thickens, enlargemtn of lymph node in area. e. chronic lesions of skin and enlarged lymph nodes- skin-thickens and discolored, loss of skin elasticity. Femeral+inguinal lymph nodes enlarged + hanging loose skin hanging groins. f. ocular lesions- mf enter eyes + die, inflammation blindness. C. Simulian 1. female blood meal- females lay eggs in water of fast flowing rivers. 2. fast-flowing rivers D. Diagnosis 1. skin snip-small bits of skin raised, sliced with razer, in saline on slide, look for mf in microscope, should be no blood in sample. E. Treatment 1. Ivermectin 2. Mectizan 3. surgery- remove nodules 4. antibiotics F. Control programs 1. drugs, insecticides, antibiotics 2. Onchocerciasis Program of West Africa- 1974- 11 west African countries. 20*10^6 cases. Ended in Dec 2002.
3. Carter Center River Blindness Program- 1996- 11 countires in Africa + Americas. MDP- Mectizan distribution Program. 1988- Merch. Elimination- in colombia- 2007. In Ecuador- 2010, V. Loa loa- eye worm- in Africa. A. Life cycle- females- 50mm and females- 30 mm. subcultaneous tissue- migrate freely. Mf-sheathed. 1. periodicity-peripheral- day. Lungs- night 2. Chrysops- vectors- deerfly- mfL1L2L3. L3 enters skin with next meal. B. Pathology- mold- adults migrate stimulates inflammatory reaction 1. Calabar swelling- if adult remains in one location host reaction- localized, painful, swelling. Adults can migrate through conjectiva and cornea. C. Diagnosis- mf in blood D. Treatment and control- ivermectin+ DEC- kill mf, surgery. Control- deerfliesswampy areas of forests. VI. Mansonella spp.-minor A. Adult worms in body cavites+tissues B. Mf-unsheathed, no periodicity C. Vector- midges D. Pathology- localized tissue reaction VII. Dirofilaria immitis- heartworm A. Life cycle- similar to human filarial spp. Adults live in heart + pulmonary ateries. Mfin blood. Vector- mosquito B. Pathology- heart function impaired, fatigued, gernal loss of condition, cough+ respiratory problems C. Diagnosis- mf in blood. D. Treatment 1. Immiticide- arsenic- containing compound kill adult worms. Problemsa.arsenic toxicity- low margin of safety. B. dead worms- blockage. 2. Surgery- caval syndrome- heavy infection of heart worm in venae cava + right atrium. Immiticide contraindicated potential of obstruction. Surgery- risky and expensive. 3. Heartgard- ivermectin+pyrantel. Targets L3s.
Study Questions Nematodes Filarial worms
1. What are the seven species in the superfamily Filaroidea which are of significant human health importance? Where do filarial worms live in the definitive host? How are filarial worms transmitted to the definitive host? 2. What are microfilaria? What is the sheath? Do all species have a sheath? How long do mf survive in the host? How can they be identified? What is periodicity? Give an example of periodicity using Wuchereria bancrofti. 3. What disease is caused by Wuchereria bancrofti? Trace its life cycle. How big are the adult worms and where do they live? Are the mf sheathed? What is the vector? 4. What are the 3 phases of pathology? Describe the incubation phase. What is microfilaremia? 5. What is episodic adenolymphangitis and in which phase of pathology does it occur? 6. When does chronic pathology develop? What is lymphoedema? Compare the three grades of lymphoedema. What is elephantiasis? 7. What are the advantages of the CFA test for diagnosis of W. bancrofti infection? What can be observed using ultrasonography? 8. How is infection treated? What drugs are effective? Why is hygiene important? 9. What are the costs of infection with lymphatic filariasis? Compare the costs of disease and treatment. How do these costs and other factors contribute to the control of lymphatic filariasis? 10. What is the size of Brugia malayi adults? Is there periodicity in this species? Are the mf sheathed? This species is very similar to which other species?
11. Trace the life cycle of Onchocerca volvulus. What are onchocercomas and where are they found? How long do the adults live? What is the vector in the life cycle? What stage is infective to the vector? How does the vector become infected? What is the development of the parasite inside the vector? 12. What is Wolbachia? What is lipopolysaccharide and how is it related to pathology in Onchocerca infections? Compare acute, chronic, and ocular lesions in onchocerciasis. 13. Why do Simulian flies live near rivers? How is onchocerciasis diagnosed? Why is it important not to draw blood during the skin snip? 14. What is the treatment? How do Ivermectin and Mectizan function? Briefly describe the Onchocerciasis Program of West Africa and the Carter Center River Blindness Program. 15. In what part of body do Loa loa adults live? What is the vector? What is the pathology? How is infected diagnosed? How can infection be treated? 16. Where do Mansonella spp. adults live in the DH? What is the vector? Is pathology usually severe in these infections? 17. What is the common name of Dirofilaria immitis? What is the vector? What pathology results? How is infection diagnosed? How is infection treated? What stage is killed by Immiticide? Why should a drug such as Heartgard be used? 18. Figure Assignment Fig. 17-1. Life cycle of filarial worms (p. 364)
Sample questions 1. Which of the following is a characteristic of Grade II lymphoedema? A. Transient and soft B. Pressure causes pit to form in skin C. Skin does not pit on pressure D. Thickening of subcutaneous tissue E. Fissures, nodules, and warty appearance 2. Periodicity in Wuchereria bancrofti is triggered by changes that occur in the host during A. puberty B. eating C. sleeping D. exercise E. sickness 3. One characteristic of Onchocerca volvulus is that A. it is transmitted by blackflies B. the vector can survive only in slow-moving streams C. onchocercomas form primarily in the lungs and brain D. the microfilariae are the infective stage to humans E. the infective stage is transmitted to humans by copepods
1. C; 2. C; 3. A
Você também pode gostar
- SolutionsManual NewDocumento123 páginasSolutionsManual NewManoj SinghAinda não há avaliações
- Oxford Math AA SL Exam Practise Additional ResourcesDocumento172 páginasOxford Math AA SL Exam Practise Additional ResourcesSıla DenizAinda não há avaliações
- Jean-Louis Cohen - Exhibitionist Revisionism - Exposing Architectural History (September 1999)Documento10 páginasJean-Louis Cohen - Exhibitionist Revisionism - Exposing Architectural History (September 1999)Javier PerezAinda não há avaliações
- Parasitology Lec 3.01b Blood and Tissue NematodesDocumento15 páginasParasitology Lec 3.01b Blood and Tissue NematodesEnaWahahaAinda não há avaliações
- FILARIASIS PPT FINALDocumento39 páginasFILARIASIS PPT FINALBinita Shakya100% (1)
- Protozoa Usus 2Documento15 páginasProtozoa Usus 2Yoga NuswantoroAinda não há avaliações
- Proceedings of the First International Congress of Parasitology: Roma, 21-26 September 1964No EverandProceedings of the First International Congress of Parasitology: Roma, 21-26 September 1964Augusto CorradettiAinda não há avaliações
- Cyber Frauds, Scams and Their Victims - Mark Button, Cassandra CrossDocumento253 páginasCyber Frauds, Scams and Their Victims - Mark Button, Cassandra CrossMitesh MehtaAinda não há avaliações
- Chapter - 1 - Digital - Systems - and - Binary - Numbers EE228 15-16Documento81 páginasChapter - 1 - Digital - Systems - and - Binary - Numbers EE228 15-16mohamed hemdanAinda não há avaliações
- The Secret of Forgiveness of Sin and Being Born Again by Pastor Ock Soo Park 8985422367Documento5 páginasThe Secret of Forgiveness of Sin and Being Born Again by Pastor Ock Soo Park 8985422367Justinn AbrahamAinda não há avaliações
- Revision: Types of Life Cycle in Trematoda and CestodaDocumento54 páginasRevision: Types of Life Cycle in Trematoda and CestodaMicroscopeGeekAinda não há avaliações
- Blood and Tissue Nematodes BiologiDocumento47 páginasBlood and Tissue Nematodes BiologiAxzchiuu :vAinda não há avaliações
- Blood Tissue NematodesDocumento27 páginasBlood Tissue NematodesAfif Mamen100% (1)
- Brugia MalayiDocumento4 páginasBrugia MalayiJericha IsidroAinda não há avaliações
- Yousif AlaaDocumento7 páginasYousif AlaaYousif AlaaAinda não há avaliações
- Epidemiology and Control of Filariasis: Reshma Ann MathewDocumento59 páginasEpidemiology and Control of Filariasis: Reshma Ann MathewHanna HonorisAinda não há avaliações
- BIOLOGY PROJECTS CLASS 12 CBSE INVESTIGTORY Elephantiasis Causes Cures Prevention, Treatment, Causes and Case Studies..Documento28 páginasBIOLOGY PROJECTS CLASS 12 CBSE INVESTIGTORY Elephantiasis Causes Cures Prevention, Treatment, Causes and Case Studies..Gaurav Kumar63% (19)
- FILARIAL Worms - Y2S2 RumalaDocumento36 páginasFILARIAL Worms - Y2S2 Rumalamicroperadeniya100% (1)
- Helemnth ReportDocumento15 páginasHelemnth ReportHawre NajmaddinAinda não há avaliações
- 28 Sept 2016 Kuliah Filariasis BaruDocumento31 páginas28 Sept 2016 Kuliah Filariasis BaruRafif AmirAinda não há avaliações
- FilariasisDocumento40 páginasFilariasisAarzoo SainiAinda não há avaliações
- LeishmaniaFilaria Part 1Documento45 páginasLeishmaniaFilaria Part 1YS Nate100% (1)
- To Medical ParasitologyDocumento55 páginasTo Medical ParasitologyLibanos FekaduAinda não há avaliações
- 4.3. Blood and Tissue NematodesDocumento89 páginas4.3. Blood and Tissue NematodesRediat GossayeAinda não há avaliações
- Segi College Kuala Lumpur: Group Member Khamini IzaidahDocumento17 páginasSegi College Kuala Lumpur: Group Member Khamini Izaidahshally918Ainda não há avaliações
- EPIDIMIOLOGYDocumento4 páginasEPIDIMIOLOGYMaxamed Ali AadenAinda não há avaliações
- Filariasis: Signs and SymptomsDocumento30 páginasFilariasis: Signs and SymptomsAnonymous VJjzqbAlAinda não há avaliações
- Dracunculus Medinensis Onchocerca Loa LoaDocumento45 páginasDracunculus Medinensis Onchocerca Loa LoaMeenachi Chidambaram100% (1)
- Reviewer For para (Blood and Tissue Nematode)Documento4 páginasReviewer For para (Blood and Tissue Nematode)K DAinda não há avaliações
- 490 12Documento8 páginas490 12shravanidasari248425Ainda não há avaliações
- FilariasisDocumento16 páginasFilariasisJohnAinda não há avaliações
- Filarial NematodeDocumento18 páginasFilarial NematodeHawre NajmaddinAinda não há avaliações
- Lecture 7 Nematodes Part 2 New 2023Documento19 páginasLecture 7 Nematodes Part 2 New 2023ayaessam392002Ainda não há avaliações
- MalariaDocumento5 páginasMalariasubhashreepal700Ainda não há avaliações
- FilariasisDocumento11 páginasFilariasiskartiz008Ainda não há avaliações
- Micropara 3-5Documento5 páginasMicropara 3-5flixiexpressAinda não há avaliações
- Scrofuloderma: A Common Type of Cutaneous Tuberculosis. A Case ReportDocumento5 páginasScrofuloderma: A Common Type of Cutaneous Tuberculosis. A Case ReportIndah IndrianiAinda não há avaliações
- FilariaDocumento85 páginasFilariaRajkishor YadavAinda não há avaliações
- Epidemiology of Lymphatic FilariasisDocumento26 páginasEpidemiology of Lymphatic FilariasisvaishnaviAinda não há avaliações
- FilariaDocumento16 páginasFilariaJessa MayAinda não há avaliações
- Loa LoaDocumento12 páginasLoa LoaRajesh Kumar AsunalaAinda não há avaliações
- Filariasis in NepalDocumento41 páginasFilariasis in NepalBinaya100% (1)
- ShimoseDocumento6 páginasShimoseIsabella Puspa DewiAinda não há avaliações
- BN Filarial WormDocumento137 páginasBN Filarial WormCherenet TomaAinda não há avaliações
- Cutaneous & Mucocutaneous LeishmaniasisDocumento27 páginasCutaneous & Mucocutaneous LeishmaniasisMarwan TahaAinda não há avaliações
- FILARIADocumento25 páginasFILARIAKristina DavidAinda não há avaliações
- Filariasis A. Readings: CD ReportDocumento6 páginasFilariasis A. Readings: CD ReportAisa ShaneAinda não há avaliações
- Worksheet in Bio 102: Microbiology and Parasitology (WEEK 17)Documento3 páginasWorksheet in Bio 102: Microbiology and Parasitology (WEEK 17)DELOS SANTOS JESSIECAHAinda não há avaliações
- The Filariae: Lymphatic System, Subcutaneous and Deep Connective TissueDocumento17 páginasThe Filariae: Lymphatic System, Subcutaneous and Deep Connective TissueKaranja GitauAinda não há avaliações
- Filariasis: Dr. Mejbah Uddin AhmedDocumento19 páginasFilariasis: Dr. Mejbah Uddin Ahmedapi-19969058Ainda não há avaliações
- Chapter 84Documento38 páginasChapter 84Naimon Kumon KumonAinda não há avaliações
- FilariasisDocumento8 páginasFilariasisTheeya QuigaoAinda não há avaliações
- Parasitology Questions and Answers by Emile Munyembaraga, BSNMDocumento6 páginasParasitology Questions and Answers by Emile Munyembaraga, BSNMNiyitegeka OlivierAinda não há avaliações
- Wuchereria Bancrofti: Aby Elijah L. BernardinoDocumento22 páginasWuchereria Bancrofti: Aby Elijah L. BernardinoAby Brr100% (1)
- Ecthyma Contagiosum (Human Orf)Documento2 páginasEcthyma Contagiosum (Human Orf)Deba P SarmaAinda não há avaliações
- Lymphatic Filariasis ClassDocumento68 páginasLymphatic Filariasis ClassthehexhealthAinda não há avaliações
- Filariasis: By: Barrantes, Patrick and Garcia, Charina JaneDocumento17 páginasFilariasis: By: Barrantes, Patrick and Garcia, Charina Janerhimineecat71Ainda não há avaliações
- Filariasis & Related Infections: Dr. Sartono SP PDDocumento21 páginasFilariasis & Related Infections: Dr. Sartono SP PDInthanAinda não há avaliações
- Study On Pityriasis Versicolor in Patients Referred To Clinics in TabrizDocumento5 páginasStudy On Pityriasis Versicolor in Patients Referred To Clinics in TabrizMiranda Yudhi CyubidubiduuAinda não há avaliações
- BP802T Lymphatic FilariasisDocumento51 páginasBP802T Lymphatic FilariasisMisha ModiAinda não há avaliações
- Frequently Asked Quaestions (FAQs)Documento22 páginasFrequently Asked Quaestions (FAQs)Drop Ur.questionAinda não há avaliações
- ElephantiasisDocumento23 páginasElephantiasisNitin0% (1)
- Eukaryotic Diseases - 06Documento33 páginasEukaryotic Diseases - 06Vien WhitlockAinda não há avaliações
- The Intestinal Protozoa: A. IntroductionDocumento32 páginasThe Intestinal Protozoa: A. Introductionهاني عقيل حسين جوادAinda não há avaliações
- 6 Lecture PDFDocumento6 páginas6 Lecture PDFAhmad KayanAinda não há avaliações
- TOS 1st QuarterDocumento6 páginasTOS 1st QuarterQuerisa Ingrid MortelAinda não há avaliações
- Tescom Technical Training - Pressure Regulators Explained - Ver1.1Documento19 páginasTescom Technical Training - Pressure Regulators Explained - Ver1.1Amod DeshpandeAinda não há avaliações
- Imamsha Maharaj Na Parcha NewDocumento16 páginasImamsha Maharaj Na Parcha NewNARESH R.PATELAinda não há avaliações
- Mucic Acid Test: PrincipleDocumento3 páginasMucic Acid Test: PrincipleKrizzi Dizon GarciaAinda não há avaliações
- Booklet The 8th JAKINUDocumento20 páginasBooklet The 8th JAKINUsamuelionardiAinda não há avaliações
- RHEL 9.0 - Configuring Device Mapper MultipathDocumento59 páginasRHEL 9.0 - Configuring Device Mapper MultipathITTeamAinda não há avaliações
- Win Darab V7 DatasheetDocumento3 páginasWin Darab V7 DatasheetPatrick StivénAinda não há avaliações
- Dinengdeng RecipeDocumento1 páginaDinengdeng RecipeFuAinda não há avaliações
- SR Cheat Sheets PDFDocumento4 páginasSR Cheat Sheets PDFDevin ZhangAinda não há avaliações
- Parafusos PT SemblexDocumento10 páginasParafusos PT SemblexSBonderAinda não há avaliações
- Fabrication Techniques of A PN Junction DiodeDocumento5 páginasFabrication Techniques of A PN Junction DiodeNida Amber100% (3)
- 3.3 (B) Mole N MassDocumento20 páginas3.3 (B) Mole N MassFidree AzizAinda não há avaliações
- Fulltext PDFDocumento454 páginasFulltext PDFVirmantas JuoceviciusAinda não há avaliações
- Hitachi VSP Pricelist PeppmDocumento57 páginasHitachi VSP Pricelist PeppmBahman MirAinda não há avaliações
- Transcendental Meditaton ProgramDocumento3 páginasTranscendental Meditaton Programacharyaprakash0% (3)
- The Normal DistributionDocumento9 páginasThe Normal DistributionElfren BulongAinda não há avaliações
- BVP651 Led530-4s 830 Psu DX10 Alu SRG10 PDFDocumento3 páginasBVP651 Led530-4s 830 Psu DX10 Alu SRG10 PDFRiska Putri AmirAinda não há avaliações
- 7TH Maths F.a-1Documento1 página7TH Maths F.a-1Marrivada SuryanarayanaAinda não há avaliações
- Pit Viper 351Documento6 páginasPit Viper 351Sebastian Robles100% (2)
- Wincam TornoDocumento3 páginasWincam Tornocaballerillo100% (1)
- Internal Audit, Compliance& Ethics and Risk Management: Section 1) 1.1)Documento6 páginasInternal Audit, Compliance& Ethics and Risk Management: Section 1) 1.1)Noora Al ShehhiAinda não há avaliações
- V3 Tool Installation GuideDocumento13 páginasV3 Tool Installation GuideLeonardo Floresta NascimentoAinda não há avaliações
- 2022+ACCF+111+Class+test+2 Moderated+versionDocumento8 páginas2022+ACCF+111+Class+test+2 Moderated+versionLucas LuluAinda não há avaliações
- Semi Formal Asking To Borrow BooksDocumento75 páginasSemi Formal Asking To Borrow BooksPei Cheng WuAinda não há avaliações