Escolar Documentos
Profissional Documentos
Cultura Documentos
Gestational Diabetes Mellitus
Enviado por
john jumborockDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Gestational Diabetes Mellitus
Enviado por
john jumborockDireitos autorais:
Formatos disponíveis
Gestational Diabetes Mellitus
Submitted by: Airan katriel Manalo
Gestational diabetes mellitus (GDM)
Is defined as any degree of glucose intolerance with onset or first recognition during pregnancy. The definition applies whether insulin or only diet modification is used for treatment and whether or not the condition persists after pregnancy. It does not exclude the possibility that unrecognized glucose intolerance may have antedated or begun concomitantly with the pregnancy.
Approximately 7% of all pregnancies are complicated by GDM, resulting in more than 200,000 cases annually. The prevalence may range from 1 to 14% of all pregnancies, depending on the population studied and the diagnostic tests employed.
Gestational diabetes usually has no symptoms. That's why almost all pregnant women have a glucose-screening test between 24 and 28 weeks.
Consider these facts about GDM: It affects 7% of all pregnant women in the United States. More than 200,000 cases are diagnosed annually according to ADA (American Diabetes Association). Women with GDM have an evidence of islet cell autoimmunity. 67% reduction in their beta- cell compensation compared with normal pregnant women.
Gestational diabetes is usually diagnosed between the 24th and 28th week of pregnancy when the results of insulin resistance are clinically present.
Subtypes: Type A1abnormal oral glucose tolerance test but normal glucose level during fasting 2 hrs after meals; diet modification is sufficient to control
Type A2 abnormal (OGTT) compounded by normal glucose level during fasting 2 hrs after meals, additional therapy with insulin or other medication regularly
Any type of diabetes mellitus during first in pregnancy type A,B,C,D,E,F,R,RH,H,T
Greater risk for gestational diabetes:
Are older than 25 when you are pregnant Have a family history of diabetes Gave birth to a baby that weighed more than 9 -pounds or had a birth defect Have high blood pressure Have too much amniotic fluid
Symptoms
Usually there are no symptoms, or the symptoms are mild and not life threatening to the pregnant woman. The blood sugar (glucose) level usually returns to normal after delivery.
Symptoms may include: -Blurred vision -Fatigue -Frequent infections, including those of the bladder, vagina, and skin -Increased thirst -Increased urination
-Nausea and vomiting -Weight loss despite increased appetite
DIAGNOSIS
Women with the following clinical characteristics consistent with a high risk for GDM should receive testing with first prenatal visit: Marked obesity Personal history of GDM Glycosuria Strong family history
Low-risk status requires no glucose testing, but this category is limited to those women meeting all of the following characteristics: Age <25 years Weight normal before pregnancy Member of an ethnic group with a low prevalence of GDM No known diabetes in first-degree relatives No history of abnormal glucose tolerance No history of poor obstetric outcome (2005, Setji, Brown, & Feinglos, p. 23)
Diagnostic Criteria for GDM using the 50-g glucose Challenge Test Blood glucose levels less than 139 mg/dl requires no further testing. Blood glucose levels 140 mg/dl to 184 mg/dl indicate a positive result and additional testing with a 3-hour 100 g oral glucose tolerance test is needed. Blood glucose levels 185 mg/dl or greater indicates a diagnosis of gestational diabetes and no further testing is needed.
Diagnostic Criteria for 100-g glucose Challenge Test Two or more of the following indicates diagnosis of gestational diabetes mellitus: 95 mg/dl or higher fasting blood glucose 180 mg/dl or higher at 1-hour postprandial blood glucose 155 mg/dl or higher at 2-hour postprandial blood glucose 140 mg/dl or higher at 3-hour postprandial blood glucose (Setji, Brown, & Feinglos, 2005)
MATERNAL AND FETAL COMPLICATIONS OF GDM Negative Maternal Health Outcomes: Greater increase in cesarean delivery rates - 22 to 30% for mothers with GDM and 17% for those without GDM Higher risk of third or fourth-degree laceration in women with GDM Polyhydramnios (an excess of amniotic fluid) Pregnancy induced hypertension Increased risk of gestational diabetes in subsequent pregnancies Possible increased risk for pre-eclampsia Higher risk for development of type 2 diabetes
Negative Neonatal Health Outcomes: Macrosomia (birth weight greater than 8 lbs) Brachial plexus injury Clavicular factures Hypoglycemia Increased possibility of a preterm birth Hypocalcemia Polycythemia Hyperbilirubinemia
Possible Complications Delivery-related complications due to the infant's large size Development of diabetes later in life Increased risk of newborn death and stillbirth Low blood sugar (glucose) or illness in the newborn
Routine screening for gestational diabetes Initial glucose challenge test. You'll begin the glucose challenge test by drinking a syrupy glucose solution. One hour later, you'll have a blood test to measure your blood sugar level. A blood sugar level below 130 to 140 milligrams per deciliter (mg/dL), or 7.2 to 7.8 mill moles per liter (mmol/L), is usually considered normal on a glucose challenge test, although this may vary at specific clinics or labs. If your blood sugar level is higher than normal, it only means you have a higher risk of gestational diabetes. Your doctor will diagnose you after giving you a follow-up test. Follow-up glucose tolerance testing. For the follow-up test, you'll be asked to fast overnight and then have your fasting blood sugar level measured. Then you'll drink another sweet solution this one containing a higher concentration of glucose and your blood sugar level will be checked every hour for a period of three hours. If at least two of the blood sugar readings are higher than normal, you'll be diagnosed with gestational diabetes.
DIAGNOSTIC TEST:
Several blood tests are used to measure blood glucose levels, the primary test for diagnosing diabetes. Additional tests can determine the type of diabetes and its severity. Random blood glucose test for a random blood glucose test, blood can be drawn at any time throughout the day, regardless of when the person last ate. A random blood glucose level of 200 mg/dL (11.1 mmol/L) or higher in persons who have symptoms of high blood glucose (see Symptoms above) suggests a diagnosis of diabetes.
Fasting blood glucose test fasting blood glucose testing involves measuring blood glucose after not eating or drinking for 8 to 12 hours (usually overnight). A normal fasting blood glucose
level is less than 100 mg/dL. A fasting blood glucose of 126 mg/dL (7.0 mmol/L) or higher indicates diabetes. The test is done by taking a small sample of blood from a vein or fingertip. It must be repeated on another day to confirm that it remains abnormally high (see Criteria for diagnosis below). Hemoglobin A1C test (A1C) The A1C blood test measures the average blood glucose level during the past two to three months. It is used to monitor blood glucose control in people with known diabetes, but is not normally used to diagnose diabetes. Normal values for A1C are 4 to 6 percent (show figure 3). The test is done by taking a small sample of blood from a vein or fingertip. Oral glucose tolerance test Oral glucose tolerance testing (OGTT) is the most sensitive test for diagnosing diabetes and pre-diabetes. However, the OGTT is not routinely recommended because it is inconvenient compared to a fasting blood glucose test. The standard OGTT includes a fasting blood glucose test. The person then drinks a 75 gram liquid glucose solution (which tastes very sweet, and is usually cola or orange-flavored). Two hours later, a second blood glucose level is measured.
ANATOMY AND PHYSIOLOGY:
Every cell in the human body needs energy in order to function. The bodys primary energy source is glucose, a simple sugar resulting from the digestion of foods containing carbohydrates (sugars and starches). Glucose from the digested food circulates in the blood as a ready energy source for any cells that need it. Insulin is a hormone or chemical produced by cells in the pancreas, an organ located behind the stomach. Insulin bonds to a receptor site on the outside of cell and acts like a key to open a doorway into the cell through which glucose can enter. Some of the glucose can be converted to concentrated energy sources like glycogen or fatty acids and saved for later use. When there is not enough insulin produced or when the doorway no longer recognizes the insulin key, glucose stays in the blood rather entering the cells.
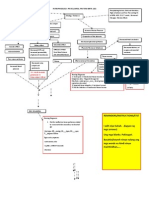
PATHOPHYSILOGY
The precise mechanisms underlying gestational diabetes remain unknown. The hallmark of GDM is increased insulin resistance. Pregnancy hormones and other factors are thought to interfere with the action of insulin as it binds to the insulin receptor. The interference probably occurs at the level of the cell signaling pathway behind the insulin receptor. Since insulin promotes the entry of glucose into most cells, insulin resistance prevents glucose from entering the cells properly. As a result, glucose remains in the bloodstream, where glucose levels rise. More insulin is needed to overcome this resistance; about 1.5-2.5 times more insulin is produced than in a normal pregnancy.
Because glucose travels across the placenta (through diffusion facilitated by GLUT3 carriers), the fetus is exposed to higher glucose levels. This leads to increased fetal levels of insulin (insulin itself cannot cross the placenta). The growth-stimulating effects of insulin can lead to excessive growth and a large body (macrosomia). After birth, the high glucose environment disappears, leaving these newborns with ongoing high insulin production and susceptibility to low blood glucose levels (hypoglycemia).
Management:
The goal is to prevent adverse pregnancy outcomes. o o o A multidisciplinary approach is used. Patient is seen every 1-2 wks until 36 wks gestation and then weekly. Patient is asked to keep an accurate diary of their blood glucose concentration.
Intrapartum: The goal is to maintain normoglycemia in order to prevent neonatal hypoglycemia. Check patients glucose q1-2 hours. Start insulin drip to maintain a glucose level of between 80 - 110 mg/dL. Observe infant closely for hypoglycemia, hypocalcemia, and hyperbilirubinemia after birth.
Postpartum Care: After delivery: Measure blood glucose.
-fasting blood glucose concentrations should be <105 mg/dL and one hour postprandial concentrations should be < 140 mg/dL.
Administer one half of the pre-delivery dose before starting regular food intake.
Follow up: Per American Diabetes Association, a 75 g two hours oral GTT should be performed 6-8 wks after delivery.
Follow up: If the pts postpartum GTT is normal, she should be re-evaluated at a minimum of 3 years interval with a fasting glucose. All pts should be encouraged to exercise and lose wt. All pts should be evaluated for glucose intolerance or DM before a subsequent pregnancy.
NURSING INTERVENTIONS:
Advice patient about the importance of an individualized meal plan in meeting weekly weight loss goals and assist with compliance. Assess patients for cognitive or sensory impairments, which may interfere with the ability to accurately administer insulin.
Demonstrate and explain thoroughly the procedure for insulin self-injection. Help patient to achieve mastery of technique by taking step by step approach. Review dosage and time of injections in relation to meals, activity, and bedtime based on patients individualized insulin regimen. Instruct patient in the importance of accuracy of insulin preparation and meal timing to avoid hypoglycemia. Explain the importance of exercise in maintaining or reducing weight. Advise patient to assess blood glucose level before strenuous activity and to eat carbohydrate snack before exercising to avoid hypoglycemia. Assess feet and legs for skin temperature, sensation, soft tissues injuries, corns, calluses, dryness, hair distribution, pulses and deep tendon reflexes. Maintain skin integrity by protecting feet from breakdown. Advice patient who smokes to stop smoking or reduce if possible, to reduce vasoconstriction and enhance peripheral flow.
Você também pode gostar
- EFT GuideDocumento11 páginasEFT Guidenokaion19% (26)
- n320 GDM Teaching BrochureDocumento2 páginasn320 GDM Teaching Brochureapi-302336744Ainda não há avaliações
- Postpartum Care Plan New BornDocumento10 páginasPostpartum Care Plan New BornUche Edwards-ShahidAinda não há avaliações
- Introduction RevisionDocumento50 páginasIntroduction RevisionGracie S. VergaraAinda não há avaliações
- Dengue Case StudyDocumento20 páginasDengue Case Studyjohn jumborockAinda não há avaliações
- Dengue Case StudyDocumento20 páginasDengue Case Studyjohn jumborockAinda não há avaliações
- IGCSE Biology (O610) Workbook: Balanced DietDocumento5 páginasIGCSE Biology (O610) Workbook: Balanced DietPatrick Abidra100% (1)
- FEDIAF Nutritional Guidelines 2020 20200917Documento96 páginasFEDIAF Nutritional Guidelines 2020 20200917luciana ribeiroAinda não há avaliações
- Gestational Diabetes MellitusDocumento21 páginasGestational Diabetes MellitusGlen Jacobs SumadihardjaAinda não há avaliações
- Gestational Diabetes MellitusDocumento14 páginasGestational Diabetes MellitusCzarina PorciunculaAinda não há avaliações
- Gestational Diabetes MellitusDocumento11 páginasGestational Diabetes Mellitusjohn jumborock100% (1)
- Case Study of DMDocumento6 páginasCase Study of DMbuzz Q0% (1)
- Gestational Diabetes MellitusDocumento25 páginasGestational Diabetes MellitusMazlina MaidinAinda não há avaliações
- Case Study - GDMDocumento5 páginasCase Study - GDMRomeo ReyesAinda não há avaliações
- Gestational Diabetes MellitusDocumento7 páginasGestational Diabetes MellitusYujen0% (1)
- Gestational DMDocumento50 páginasGestational DMKevin MarquezAinda não há avaliações
- Case Study On Pregnancy Induced Hypertension (PIH) : University of Northern Philippines College of NursingDocumento42 páginasCase Study On Pregnancy Induced Hypertension (PIH) : University of Northern Philippines College of Nursing3B NOVIDA, ALEYA G.Ainda não há avaliações
- PREECLAMPSIADocumento93 páginasPREECLAMPSIADaly L. Nacional100% (1)
- Fetal Distress Case DiscussionDocumento55 páginasFetal Distress Case DiscussionHafsah G.Ainda não há avaliações
- Activity Intolerance R/T Increased Energy Demands Due To Disease Condition and Increased Fetal Nutrient UptakeDocumento8 páginasActivity Intolerance R/T Increased Energy Demands Due To Disease Condition and Increased Fetal Nutrient UptakeAbdelmar SusulanAinda não há avaliações
- Gestational Diabetes MellitusDocumento16 páginasGestational Diabetes Mellitusarjunr19910% (1)
- Gestational Diabetes Screening Case StudiesDocumento50 páginasGestational Diabetes Screening Case Studiesdiabetes asia100% (1)
- Placenta PreviaDocumento11 páginasPlacenta PreviaHomerAinda não há avaliações
- Gestational Diabetes MellitusDocumento31 páginasGestational Diabetes MellitusJasmine PraveenAinda não há avaliações
- Case-Study FinalDocumento39 páginasCase-Study Finalcoosa liquorsAinda não há avaliações
- PIHDocumento18 páginasPIHArtyom GranovskiyAinda não há avaliações
- Case3 Case StudyDocumento6 páginasCase3 Case StudyKrizzia Angela BacotocAinda não há avaliações
- Neonatal HypoglycemiaDocumento22 páginasNeonatal HypoglycemiaRonak Sheth100% (3)
- Gestational Diabetes Mellitus PDFDocumento7 páginasGestational Diabetes Mellitus PDFMaxenia FaboresAinda não há avaliações
- NCPGDMDocumento8 páginasNCPGDMChristopher LontocAinda não há avaliações
- Postpartum Physical AssessmentDocumento60 páginasPostpartum Physical AssessmentJhgrace Mary Pacaña Gallo100% (1)
- Pregnancy Induced Hypertension (Pih)Documento56 páginasPregnancy Induced Hypertension (Pih)shandi23100% (5)
- Shoulder DystociaDocumento20 páginasShoulder DystociaDanielle Francis Hirang0% (1)
- GDMDocumento11 páginasGDMNikki GarlejoAinda não há avaliações
- PPH Introduction 1Documento95 páginasPPH Introduction 1regine maeAinda não há avaliações
- Case StudyDocumento19 páginasCase Studywella goAinda não há avaliações
- Neonatal SepsisDocumento44 páginasNeonatal SepsisIsabel Barredo Del MundoAinda não há avaliações
- Hypertension in Pregnancy CompiledDocumento67 páginasHypertension in Pregnancy CompiledRaiza Love Caparas-PablicoAinda não há avaliações
- Ectopic Pregnancy - OMDocumento9 páginasEctopic Pregnancy - OMrheindAinda não há avaliações
- Fetal Macrosomia UptodateDocumento22 páginasFetal Macrosomia UptodateWinny Roman AybarAinda não há avaliações
- Gestational Diabetes Mellitus Case StudiesDocumento21 páginasGestational Diabetes Mellitus Case Studiesdiabetes asia100% (3)
- Diabetes Mellitus & Pregnancy: G.M PunarbawaDocumento27 páginasDiabetes Mellitus & Pregnancy: G.M PunarbawaMartina RizkiAinda não há avaliações
- Psychological Perspective of Abnormal LaborDocumento25 páginasPsychological Perspective of Abnormal LaborPriscilla Sarah PayneAinda não há avaliações
- Neonatal Hypoglycemia APNECDocumento26 páginasNeonatal Hypoglycemia APNECyumicheongAinda não há avaliações
- Infant of Diabetic MotherDocumento14 páginasInfant of Diabetic MothersreekalaAinda não há avaliações
- Pre EclampsiaDocumento8 páginasPre EclampsiaJamie Agbannawag100% (1)
- Clinical Guideline For The Management of A Woman With Eclampsia And/Or Severe Pre Eclampsia 1. Aim/Purpose of This GuidelineDocumento15 páginasClinical Guideline For The Management of A Woman With Eclampsia And/Or Severe Pre Eclampsia 1. Aim/Purpose of This GuidelineMegane YuliAinda não há avaliações
- Finished Case Study GDMDocumento9 páginasFinished Case Study GDMapi-242547654100% (1)
- Diabetes Mellitus and PregnancyDocumento45 páginasDiabetes Mellitus and Pregnancyilham muntari100% (1)
- OB CH20 NotesDocumento16 páginasOB CH20 NotesVeronica EscalanteAinda não há avaliações
- Severe PreeclampsiaDocumento84 páginasSevere PreeclampsiaJm Bernardo50% (2)
- SIM - Anemias of PregnancyDocumento17 páginasSIM - Anemias of PregnancyGabrielle EvangelistaAinda não há avaliações
- Gestational Diabetes Mellitus Gestational Diabetes Mellitus (GDM) Is One of TheDocumento10 páginasGestational Diabetes Mellitus Gestational Diabetes Mellitus (GDM) Is One of TheJobelle AcenaAinda não há avaliações
- 16 Amniotic Fluid EmbolismDocumento46 páginas16 Amniotic Fluid EmbolismAhmed TarigAinda não há avaliações
- CP Ovarian Cyst Chap5Documento11 páginasCP Ovarian Cyst Chap5Katherine 'Chingboo' Leonico LaudAinda não há avaliações
- Abruptio PlacentaDocumento5 páginasAbruptio PlacentaJuan Carlo Z. SolidumAinda não há avaliações
- Pregnancy Induced Hypertension: Mariano Marcos State UniversityDocumento37 páginasPregnancy Induced Hypertension: Mariano Marcos State UniversityLyca Mae AurelioAinda não há avaliações
- IUFDDocumento2 páginasIUFDnurseon0% (1)
- Claudio Case Study of Pregnancy Induced HypertensionDocumento78 páginasClaudio Case Study of Pregnancy Induced HypertensionTanya Victoria Lean ClaudioAinda não há avaliações
- NCM - Pregancy Induced HypertensionDocumento5 páginasNCM - Pregancy Induced HypertensionZam PamateAinda não há avaliações
- Pathophysiology of PihDocumento3 páginasPathophysiology of PihMargueretti Delos ReyesAinda não há avaliações
- Postpartal Diabetes MellitusDocumento7 páginasPostpartal Diabetes Mellitusnursereview100% (3)
- Diabetes in PregnancyDocumento88 páginasDiabetes in PregnancyKathleenZunigaAinda não há avaliações
- Gestational Diabetes MellitusDocumento31 páginasGestational Diabetes MellitusLidya BintangAinda não há avaliações
- Gestational DiabetesDocumento42 páginasGestational Diabetesjohn jumborock100% (1)
- STD and GITDocumento3 páginasSTD and GITjohn jumborockAinda não há avaliações
- ResumeDocumento4 páginasResumeAaRomalyn F. ValeraAinda não há avaliações
- The Impact of Longitudinal Studies On Understanding Development From Young Adulthood To Old AgeDocumento11 páginasThe Impact of Longitudinal Studies On Understanding Development From Young Adulthood To Old AgeLana PeharAinda não há avaliações
- Gear Oil 85W-140: Safety Data SheetDocumento7 páginasGear Oil 85W-140: Safety Data SheetsaadAinda não há avaliações
- Leptospirosis PDFDocumento48 páginasLeptospirosis PDFTuan HaikalAinda não há avaliações
- N4H InvitationLetter - FinalDocumento2 páginasN4H InvitationLetter - Finalluis DiazAinda não há avaliações
- Human and Health Rights in Relation To Sustainable2Documento17 páginasHuman and Health Rights in Relation To Sustainable2ptkabworldAinda não há avaliações
- Company Name: Aims Industries LTDDocumento40 páginasCompany Name: Aims Industries LTDkishoreAinda não há avaliações
- Acute HepatitisDocumento14 páginasAcute Hepatitisapi-379370435100% (1)
- PNA 2012 National Convention LectureDocumento60 páginasPNA 2012 National Convention LectureHarby Ongbay AbellanosaAinda não há avaliações
- Acl Reconstruction Without Meniscus RepairDocumento1 páginaAcl Reconstruction Without Meniscus Repairsathvik gowdaAinda não há avaliações
- Abstrak EnglishDocumento1 páginaAbstrak EnglishputrapaninjauanAinda não há avaliações
- Answer Key Ielts 2Documento16 páginasAnswer Key Ielts 2Sovannak OnAinda não há avaliações
- Providing Information Raising Awareness: June 2015Documento17 páginasProviding Information Raising Awareness: June 2015Aymanahmad AymanAinda não há avaliações
- NCPPDocumento11 páginasNCPPAngelo Miguel MuñozAinda não há avaliações
- Mr. Maroof Khan: Speech and Language Pathologist/TherapistDocumento15 páginasMr. Maroof Khan: Speech and Language Pathologist/TherapistshamsAinda não há avaliações
- NSTP Project Proposal 1Documento8 páginasNSTP Project Proposal 1Laila J. Ignacio100% (2)
- 20 MG 100 ML ConivaptanDocumento18 páginas20 MG 100 ML Conivaptanahmedradwan2005Ainda não há avaliações
- Nursing - Burn InjuryDocumento39 páginasNursing - Burn Injuryamaracha2003Ainda não há avaliações
- Lecture in Geriatrics Physical Therapy 1Documento27 páginasLecture in Geriatrics Physical Therapy 1S.AAinda não há avaliações
- For DissertationDocumento13 páginasFor DissertationRegi viniciyaAinda não há avaliações
- Safety Pocket Guide Web 061808Documento534 páginasSafety Pocket Guide Web 061808hombre911100% (1)
- Health Opportunities Through Physical EducationDocumento8 páginasHealth Opportunities Through Physical EducationAngel Erica TabigueAinda não há avaliações
- Lab Report 15438869 20231127064225Documento1 páginaLab Report 15438869 20231127064225carilloabhe21Ainda não há avaliações
- Bassam Osman ResumeDocumento4 páginasBassam Osman ResumeBassam OsmanAinda não há avaliações
- ESI ER CompleteDocumento45 páginasESI ER Completetammy2121Ainda não há avaliações
- Roma Therapy IN Yurveda: N.SrikanthDocumento89 páginasRoma Therapy IN Yurveda: N.SrikanthAkshay TandleAinda não há avaliações
- Drug Study 1Documento2 páginasDrug Study 1Hafza MacabatoAinda não há avaliações