Escolar Documentos
Profissional Documentos
Cultura Documentos
Nutrition & Dietetics: Supplement
Enviado por
firdakusumaputriTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Nutrition & Dietetics: Supplement
Enviado por
firdakusumaputriDireitos autorais:
Formatos disponíveis
Nutrition & Dietetics
Journal of the Dietitians Association of Australia, including the Journal of the New Zealand Dietetic Association
Supplement
Evidence Based Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
Editor Linda Tapsell, PhD, MHPEd, Dip Nutr Diet, BSc, MAIFST, FDAA Wollongong, New South Wales Acting Supplement Editor Ingrid Hickman, PhD, BHSc, APD Brisbane, Queensland Editorial Assistant Kristy Parsons Canberra, Australian Capital Territory Prepared by the DAA Malnutrition Guideline Steering Committee Cheryl Watterson, Grad Dip Nutr Diet, BSc, APD Director, Nutrition and Dietetics John Hunter Hospital Newcastle, New South Wales Allison Fraser, BHSc, APD Research and Development Dietitian John Hunter Hospital Newcastle, New South Wales Merrilyn Banks, PhD, MHltSc, Grad Dip Nutr Diet, Grad Dip Ed, BSc, APD Director, Nutrition and Dietetics Royal Brisbane and Womens Hospital Brisbane, Queensland Elisabeth Isenring, PhD, BHSc, AdvAPD NHMRC Australian Clinical Training Fellow Queensland University of Technology Brisbane, Queensland Michelle Miller, PhD, MNutDiet, BSc, APD Senior Lecturer Flinders University Adelaide, South Australia Caitlin Silvester, PGrad Dip Diet, Grad Dip HlthSc, BSc, APD Dietitian Beechworth Health Services Beechworth, Victoria Roy Hoevenaars, PhD, BSc(Hons), Grad Dip Nutr Diet, BSc, APD Manager, Nutrition and Dietetics Barwon Health Geelong, Victoria Judy Bauer, PhD, MHSc, GDipNutrDiet, BSc, AdvAPD Director, Nutrition and Dietetics The Wesley Hospital Brisbane, Queensland Angela Vivanti, DHSc, MAppl Sc, Grad Dip Nutr Diet, BSc, AdvAPD Research & Development Dietitian Princess Alexandra Hospital Brisbane, Queensland Maree Ferguson, PhD, MBA, Grad Dip Nutr Diet, BAppSc, AdvAPD Director, Nutrition and Dietitics Princess Alexandra Hospital Brisbane, Queensland Journal and Scientic Publications Management Committee Margaret Allman-Farinelli (Director Responsible) Anthea Magarey (Chairperson) Linda Tapsell Judy Bauer Marina Reeves Giordana Cross Clare Collins Maree Ferguson Andrea Braakhuis Jane Elmslie Claire Hewat Kristy Parsons Aims and Scope: Nutrition & Dietetics is Australia and New Zealands leading peer-reviewed Journal in its eld. Covering all aspects of food, nutrition and dietetics, the Journal provides a basic forum for the reporting, discussion and development of scientically credible knowledge related to human nutrition and dietetics. Widely respected in Australia and around the world, Nutrition & Dietetics publishes original research, review papers, viewpoint articles, insights short papers on ndings from demonstrating practice, letters, book reviews, conference reports and continuing education quizzes. Abstracting and Indexing Services: The Journal is indexed by Abstracts on Hygiene and Communicable Diseases; Agricola C R I S; Animal Bredding Abstracts; Aquatic Sciences & Fisheries Abstracts; Australasian Medical Index; Australian Family and Society Abstracts; Cumulative Index to Nursing & Allied Health Literature; Dairy Science Abstracts; EBSCO Contentville; Food Science and Technology Abstracts; Horticultural Science Abstracts; Infotrac; Infotrieve; Leisure, Recreation and Tourism Abstracts; Nutrition Abstracts and Reviews; Postharvest News and Information; Potato Abstracts; Poultry Abstracts; Review of Aromative and Medicinal Plants; Rural Development Abstracts; SAGE; Soybean Abstracts; Sugar Industry Abstracts; Tropical Diseases Bulletin; World Agricultural Economics and Rural Sociology Abstracts; World Banking Abstracts; World Magazine Bank. Address for Editorial Correspondence: Editor, Nutrition & Dietetics 1/8 Phipps Close Deakin ACT 2600 Australia Email: journal@daa.asn.au Disclaimer: The Publisher, the Dietitians Association of Australia, the New Zealand Dietetic Association, and Editors cannot be held responsible for errors or any consequences arising from the use of information contained in this journal; the views and opinions expressed do not necessarily reect those of the Publisher, the Dietitians Association of Australia, the New Zealand Dietetic Association and Editors, neither does the publication of advertisements constitute any endorsement by the Publisher, the Dietitians Association of Australia, the New Zealand Dietetic Association and Editors of the products advertised. Journal compilation 2009 (Dietitians Association of Australia). For submission instructions, subscription and all other information visit www.blackwellpublishing.com/nd This journal is available online at Wiley Interscience. Visit www. interscience.wiley.com to search the articles and register for table of contents and email alerts. Access to this journal is available free online within institutions in the devoloping world through the AGORA initiative with the FAO and the HINARI initiative with the WHO. For information, visit www.aginternetwork.org, www.healthinternetwork.org. ISSN 1446-6368 (Print) ISSN 1747-0080 (Online)
NDI.JEB.Dec09
Nutrition & Dietetics
Journal of the Dietitians Association of Australia, including the Journal of the New Zealand Dietetic Association
Volume 66 Supplement 3 December 2009 Evidence based practice guidelines for the nutritional management of malnutrition in adult patients across the continuum of care Executive summary Summary of evidence-based recommendations Introduction Evidence based statements Acknowledgement References Appendices
ISSN 1446-6368
S1 S2S3 S4S10 S11S20 S21 S22S27 S28S34
The Dietitians Association of Australia (DAA) supported the printing of these DAA-endorsed Best Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care.
Nutrition & Dietetics 2009; 66 (Suppl. 3): S1
Evidence based practice guidelines for the nutritional management of malnutrition in adult patients across the continuum of care
EXECUTIVE SUMMARY
Malnutrition is a major international and Australian health problem, which continues to be unrecognised and therefore, untreated. It is both a cause and a consequence of ill health across many patient groups and healthcare settings. Malnutrition interferes with patients ability to benet from health treatments and affects every domain of their well-being. Additionally, it increases societys healthcare costs. This paper, Evidence based practice guidelines for nutritional management of malnutrition in adult patients across the continuum of care, has been developed to gather the best available evidence for detecting malnutrition and managing it with nutritional interventions. The Guideline Steering Committee hopes to inuence health care providers and especially dietitians to increase capacity within Australia to implement affordable detection systems, such as routine malnutrition screening. It is expected that the guidelines will provide a framework for evidence-based nutritional assessments and increase access to appropriate patient-focussed treatments for affected adults that are timely and occur both within and across hospital and primary care sectors. These guidelines are based on an agreed and rigorous process undertaken by the Steering Committee, and in accordance with the Dietitians Association of Australia (DAA) performance standards. They have resulted from the voluntary contribution of a collaboration of dietitians with clinical and research expertise across a range of practice settings. The process involved a systematic search of the literature, an assessment of the strength of the evidence, consultation with key stakeholders and the development of evidencebased statements and practice tips that may help to guide clinical practice and improve patient experience and health outcomes in Australian healthcare sectors for malnourished adults. The dissemination and implementation of the recommendations of the guidelines will be supported by the DAA.
2009 The Author. Journal compilation 2009 Dietitians Association of Australia
S1
Nutrition & Dietetics 2009; 66 (Suppl. 3): S2S3
SUMMARY OF EVIDENCE-BASED RECOMMENDATIONS
The guideline recommendations have been graded using the National Health and Medical Research Council (NHMRC) classications for grades of recommendation1, which are as follows: Level A Body of evidence can be trusted to guide practice. Level B Body of evidence can be trusted to guide practice in most situations. Level C Body of evidence provides some support for recommendation(s) but care should be taken in its application. Level D Body of evidence is weak and recommendation(s) must be applied with caution.
1. Nutrition screening
Clinical question
1a. What is the prevalence of malnutrition and is it a problem?
Evidence-based recommendations
The prevalence of malnutrition is high worldwide (including in Australia) in all healthcare settings, yet is largely underrecognised and under-diagnosed resulting in a decline in nutritional status. Therefore, it is recommended that healthcare professionals are informed that malnutrition is associated with adverse clinical outcomes and costs. NHMRC Grade of recommendation: A Malnutrition should be identied, treated and action taken to reduce the prevalence in Australian healthcare settings and in community-dwelling adults. NHMRC Grade of recommendation: B
Clinical question
1b. Should there be routine screening for malnutrition and if so where and when should malnutrition screening occur?
Evidence-based recommendations
Routine screening for malnutrition should occur in the acute setting to improve the identication of malnutrition risk and to allow for nutritional care planning. NHMRC Grade of recommendation: B Routine screening for malnutrition should occur in the rehabilitation, residential aged care and community settings to improve the identication of malnutrition risk and enable nutritional care planning. NHMRC Grade of recommendation: D
Clinical question
1c. What screening process can be used to identify adults at risk of malnutrition?
Evidence-based recommendations
Use a valid malnutrition screening tool appropriate to the population in which it is to be applied. NHMRC Grade of recommendation: B
S2
2009 The Author. Journal compilation 2009 Dietitians Association of Australia
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
2. Nutrition assessment
Clinical question
What nutrition assessment processes can be used to diagnose malnutrition in adults?
Evidence-based recommendations
Use a valid nutrition assessment tool appropriate to the population in which it is to be applied. NHMRC Grade of recommendation: B
3. Nutrition goals, interventions and monitoring
Clinical question
3a. In adults with malnutrition or at risk of malnutrition, what are the appropriate nutrition goals, for optimal client, clinical and cost outcomes?
Evidence-based recommendations
Aim to prevent decline/improve nutritional status and associated outcomes in adults with malnutrition or at risk of malnutrition. NHMRC Grade of recommendation: A
Clinical question
3b. What are the appropriate interventions for prevention and treatment of malnutrition in adults?
Evidence-based recommendations
Nutrition interventions can improve outcomes. Consideration should be given to the healthcare setting, resources, patient/client goals, requirements and preferences. NHMRC Grade of recommendation: BC
Clinical question
3c. What are appropriate monitoring and outcome measures to demonstrate improved patient, clinical and cost outcomes?
Evidence-based recommendations
Choose standardised measures which change in a clinically meaningful way to demonstrate the outcomes of nutrition interventions. NHMRC Grade of recommendation: not applicable
2009 The Author. Journal compilation 2009 Dietitians Association of Australia
S3
Nutrition & Dietetics 2009; 66 (Suppl. 3): S4S10
1 INTRODUCTION 1.1 Purpose and scope
The purpose of these guidelines is to provide health care professionals, especially dietitians with evidence based recommendations supporting the identication and nutritional management of malnourished adults. The Evidence Based Practice Guidelines for Nutritional Management of Malnutrition in Adult Patients across the Continuum of Care focus on the identication and treatment of malnutrition in the acute, rehabilitation, residential aged care, and community settings. Although there are other international guidelines which address malnutrition,2,3 it was determined that gaps existed in these guidelines which warranted addressing and it was perceived that there would be a benet in exploring the evidence base with respect to the Australian context. Malnutrition is dened as a state of nutrition in which a deciency or excess (or imbalance) of energy, protein, and other nutrients causes measurable adverse effects on tissue/ body form (body shape, size and composition) and function and clinical outcome.4 For the purpose of these guidelines malnutrition refers solely to protein-energy under-nutrition despite the denition given above which encompasses both under- and over-nutrition. In developed countries the increasing prevalence of obesity and its resultant health consequences has contributed to the lack of recognition of under-nutrition. For nutritional treatment of obesity the reader is referred to the Best Practice Guidelines for the Treatment of Overweight and Obesity in Adults endorsed by the Dietitians Association of Australia.5 The outcomes of the implementation of these evidence based guidelines will achieve the following anticipated benets for adults with malnutrition or at risk of malnutrition: Improved access to ethical, effective and efcient patient care by developing and implementing relevant patientcentred protocols and pathways appropriate to the healthcare setting. Correct diagnosis of malnourished patients increasing recognition of the impact of this disease/ condition on patients and health service. Improved patient experience and health outcomes for identied adults. A skilled Dietitian workforce playing a key role in addressing adult malnutrition across healthcare settings by continuing advocacy of the Dietitians Association of Australia. Advocacy for appropriate and adequate food services; eating environments; staff resources and policy. Capacity building in Australian health and human services for preventing, recognising and treating malnutrition by the entire health workforce and health policy makers.
1.2 Methods
1.2.1 Guideline framework
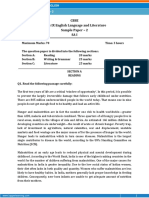
In developing these Guidelines the American Dietetic Associations Nutrition Care Process (NCP)6 has been used to dene the clinical questions for the systematic review. The NCP framework incorporates a standardised process and language as part of a conceptual model to guide and document nutrition care and patient outcomes.6 The framework includes nutrition assessment, nutrition diagnosis, nutrition intervention and nutrition monitoring and evaluation.6 This NCP framework has recently been adopted by the DAA. A trigger event initiates where and how the patient is identied for nutrition care.7 This trigger event may include nutrition screening. Since malnourished adults are often not recognised and thus fail to have access to the Nutrition Care Process, the trigger event has been added to the Guideline framework. This NCP including the trigger event is illustrated in Figure 1.7 Nutrition screening describes the process of identifying clients with characteristics commonly associated with nutrition problems who may require comprehensive nutrition assessment and may benet from nutrition intervention. These Guidelines refer to malnutrition screening which is used to identify those who may be malnourished or at risk of malnutrition. Nutrition assessment is a comprehensive approach to gathering pertinent data in order to dene nutritional status and identify nutrition-related problems. The assessment often includes patient history, medical diagnosis and treatment plan; nutrition and medication histories, nutrition related physical examination including anthropometry, nutritional biochemistry, psychological, social, and environmental aspects. Nutrition diagnosis is a clinical judgement based on data collected during the assessment phase. The set of nutrition diagnoses derived from the assessment data will give direction to prioritising treatment goals and intervention strategies. The nutrition diagnosis uses standardised terminology which identies and labels the actual occurrence, or risk of developing nutrition problems that dietitians treat independently. A nutrition diagnosis is written in PES format that states the problem (P) or nutrition diagnosis, the aetiology (E) or risk factors/ causes and the signs and symptoms (S) or measurable adverse nutrition status.8 Nutrition intervention is designed to address a nutrition problem or aetiology of the nutrition diagnosis. Nutrition interventions aim to change nutrition-related behaviour, risk factors, environmental aspects or characteristics of health status. Nutrition monitoring is the review and assessment of a patients status at a scheduled follow-up point with regard to the nutrition diagnosis, intervention plans/ goals, and outcomes. 2009 The Author Journal compilation 2009 Dietitians Association of Australia
S4
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
The Nutrition Care Process
Screening & Referral System Identify risk factors Use appropriate tools and methods Involve interdisciplinary collaboration
Practice Settings
Co d
e of
Ethics
Diet e
tics
Kn ow l ed ge
Pr ac t
Nutrition Assessment & Re-assessment
Obtain/collect timely & appropriate data Analyze/interpret with evidence-based standards Document
ice
Nutrition Diagnosis
Identify & label problem Determine cause/contributing risk factors Cluster signs & symptoms/defining characteristics Document
Evidenc e-b ase d
lth Hea
Competencies Skills &
Economics
Care System s
Relationship Between Patient/Client/Group & Dietetics Professional
Nutrition Monitoring & Evaluation
Monitor progress Measure outcome indicators Evaluate outcomes Document
Nutrition Intervention
Plan nutrition intervention Formulate goals & determine a plan of action Implement nutrition intervention Care is delivered & actions are carried out Document
Outcomes Management System Monitor the success of the Nutrition Care Process Implementation Evaluate the impact with aggregate date Identify and analyze causes of less than optimal performance and outcomes Refine the use of the Nutrition Care Process
Figure 1 American Dietetic Association Nutrition Care Process and Model7. Reproduced with the permission of Elsevier.
Outcome evaluation is the systematic comparison of current ndings with previous status, intervention goals, or reference standards. Outcomes which can be used to show the effectiveness of nutrition interventions can be grouped into direct nutrition outcomes, clinical and health status outcomes, patient-centred outcomes, and health care utilisation and cost outcomes.9
1.2.2 Literature appraisal and collation
Developing the literature search strategy and clinical questions Relevant clinical questions were developed for components of the Nutrition Care Process (Figure 1). A systematic literature review of studies was designed to address the clinical questions using appropriate search terms and methodologies. Three searches were written for the Medline Database using the OVID search engine and then modied to suit Embase and CINAHL databases. The Cochrane Database of Systematic Reviews was searched for all papers relating to malnutrition. The searches were limited to the English language and studies involving humans. Limits were added which excluded tutorials, editorials, news, letters and comments. Articles not reported in full (abstract only) were also excluded. Preliminary inclusion and exclusion criteria were dened by agreement of the Steering Committee and included in the search methodology where applicable. Please refer to Appendix 1 for the detailed search strategy. The clinical questions were as follows: 2009 The Author Journal compilation 2009 Dietitians Association of Australia
1. Criteria for screening and referral systems (Figure 1): What is the best method for identication of adults with malnutrition or at risk of malnutrition for improved patient, clinical and cost outcomes? 2. Nutrition assessment (and Nutrition Diagnosis) (Figure 1): Which specic measures best reect nutritional status or change in nutritional status in adults with malnutrition or at risk of malnutrition, for the diagnosis of malnutrition, can be altered by nutritional intervention, and are associated with improved patient, clinical and cost outcomes? 3. Nutrition intervention; Nutrition monitoring and evaluation (Figure 1): a) What are the nutrition goals for adults with malnutrition or at risk of malnutrition for improved patient, clinical and cost outcomes? b) In adults with malnutrition or at risk of malnutrition, what are the appropriate nutrition interventions, to optimise nutritional status for improved patient, clinical and cost outcomes? c) In adults with malnutrition or at risk of malnutrition, how will nutrition interventions be monitored for improved patient, clinical and cost outcomes? All searches were conducted to August 2006. For the rst two clinical questions databases were searched from inception of the databases whereas the nal question (Q3) was from 1996. The searches returned a total of 3987 titles and abstracts for review. In response to the large number of S5
a itic Cr
lT
g kin hin
Social Systems
Collaboratio n
Co m m u
ca ni
n t io
Nutrition & Dietetics 2009; 66 (Suppl. 3): S4S10
Table 1 Final Guideline clinical questions Nutrition Care Process Nutrition Screening Clinical questions which informed the systematic search Q1a) What is the prevalence of malnutrition and is it a problem? 1b) Should there be routine screening for malnutrition and if so where and when should malnutrition risk screening occur? 1c) What screening process can be used to identify adults at risk of malnutrition? Q2. What nutrition assessment processes can be used to identify malnutrition in adults? Q3a) In adults with malnutrition or at risk of malnutrition, what are the appropriate nutrition goals, for optimal client, clinical and cost outcomes? Q3b) What are the appropriate nutrition interventions for prevention and treatment of malnutrition in adults? Q3c) What are appropriate monitoring and outcome measures to demonstrate improved patient, clinical and cost outcomes?
Table 2 Inclusion and Exclusion Criteria Inclusion criteria Protein-energy malnutrition Undernutrition Energy deciency Protein deciency Adults Medical Nutrition Therapy Measurements of Nutrition Status (eg biochemistry, anthropometry) Screening for Protein-Energy Malnutrition Assessments of Nutrition status (e.g. Assessment tools) Nutrient intakes Exclusion criteria Non-English language Children/ Paediatrics Specic Vitamin Deciencies (e.g. Vitamin D) Specic Mineral Deciencies (e.g. Magnesium) Eating Disorders (anorexia or bulimia) Cystic Fibrosis Coeliac Disease
Nutrition Assessment and Nutrition diagnosis Nutrition goals (a)
Obesity surgery (Gastric bypass/ bands) Liver Disease
Nutrition interventions (b)
Nutrition monitoring and evaluation (c)
abstracts retrieved, the Steering Committee made some modications to manage the literature appraisal as follows: The search for the nutrition screening tool section was modied to focus on the main recommendations from the Jones review in 200610 of 44 nutrition screening and assessment tools describing literature until the year 2000 and also any identied relevant articles of screening tools with level III-2 evidence or higher to support their use published after 2000. Ninety-six articles were identied published between January 2000 and November 2008. Since August 2006 modications have been made to the clinical questions. A newly devised question has been added to determine whether malnutrition is a problem in Australia (prevalence) and question 1 has been split into parts to enhance the focus of the evidence based statements. Diagnosis was removed from the clinical questions when the International Statistical Classication of Diseases and Related Health Problems 10th Revision Australian Modication (ICD-10-AM) criteria for diagnosing malnutrition was released.11 Consequently the new ICD-10-AM diagnostic criteria for malnutrition has been included in the document as a Nutrition Assessment practice tip. Please refer to Table 1 for the nal clinical questions. For question 1a evidence was extracted from Strattons comprehensive review of studies until 2003 investigating the S6
Renal disease and Chronic Kidney Disease Dialysis and Haemodialysis Nutrition interventions(a) Nutrition monitoring Hereditary protein deciency disorders Complications, mortality Non-Systematic reviews/ and morbidity relating to opinions/viewpoints malnutrition Unspecied nutritional Non-Western Countries deciency Critical care Crohns Disease Alcoholism Alcoholism if malnutrition is vitamin related Prevalence data only Cancer Screening tools with 2 HIV parameters for the screening section only
Note: if nutrition interventions included an exercise component, these studies were included in the guidelines, however pharmaceutical interventions are not specically addressed in these Guidelines. HIV, Human Immunodeciency Virus.
(a)
prevalence and consequences of malnutrition.12 A literature search was then conducted to identify international reviews between 2003 and 2008 as well as all published papers which investigated malnutrition prevalence in an Australian or New Zealand population. The literature identied in the searches for the initial clinical questions along with the literature attained from the additional clinical question (question 1a) was then appraised for the guidelines. Seventy-eight papers (including the Stratton review) met the inclusion criteria (refer to Table 2) for question 1a and b.12 In addition to the Jones 2006 review,10 41 papers published between January 2000 and November 2008 met the inclusion criteria for the screening tool part of the question (question 1c). For question 2, twenty-ve 2009 The Author Journal compilation 2009 Dietitians Association of Australia
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
papers were assessed as meeting the inclusion criteria and included an assessment tool measured against a means of conrming validity. One hundred and four papers were assessed as meeting the inclusion criteria for question 3 and retrieved for full appraisal. Thus, a total of 249 papers were reviewed for the guidelines. A minimum of two Steering Committee members independently assessed the titles and abstracts using the inclusion and exclusion criteria (Table 2) before retrieving the full article. Criteria were added when the reviewers commenced assessing the literature and determined further criteria were needed to ensure the scope of the guidelines remained focussed. Additional criteria exclude conditions and diseases which were already the subject of other DAA evidence based guidelines or were alternate, potentially co-existing mechanisms for protein-energy malnutrition such as sarcopenia or cachexia (please refer to existing DAA endorsed evidence based practice guidelines: Evidence Based Practice Guidelines for Nutritional Management of Patients Receiving Radiation Therapy,13 Cancer Cachexia,14 Chronic Kidney Disease,15 and Australasian Clinical Practice Guideline for Nutrition in Cystic Fibrosis.16) Tables were developed to collate the evidence for screening, assessment, intervention, monitoring and evaluation. Evidence was categorised by health care setting and patient characteristics as described in Table 3.
Table 3 Denitions used for collating evidence based statements Setting/ Demographic Acute Care Denition for the purpose of collating the evidence based statements Acute Care is dened as services occurring within an acute care hospital Rehabilitation is dened as services by a multidisciplinary team with the goal of reducing disability by improving task-oriented behaviour.17 Rehabilitation settings include both inpatient and ambulatory settings. Residential Aged Care is dened as services for aged people who can no longer be assisted to stay in their home.18 Residential aged care settings involve both low (hostel) and high care (nursing home). Community is dened as free living adults with or without assistance from community services. Across settings is used to describe evidence which involved participants or analysis in two or more of the above settings. Groups of study participants had a mean age over 60 years.
Rehabilitation
Residential Aged Care
Community
Across settings
1.2.3 Rating the evidence
The strength of the evidence was assessed using the level of evidence rating system recommended by the National Health and Medical Research Council (NHMRC) additional levels of evidence and grades of recommendations for developers of guidelines-Pilot Program (Appendix 2).1 NHMRC level of evidence of rating scheme is provided for various types of studies including: intervention; diagnosis; prognosis; aetiology; and screening (Appendix 2). Aetiology study criteria were used for clinical questions 1a and 1b Diagnostic studies were used for clinical questions 1c and 2 Intervention studies were used for clinical questions 3 a), b) &c) In all cases the evidence was ranked by two independent reviewers. Any disagreements between reviewers were handled by a third independent reviewer. This evidence then informed the evidence based statements. Only articles assessed as providing the highest level of evidence were included in the evidence based statements. However, with respect to the evidence base in the Australian and New Zealand populations, this evidence is also presented, where available, in addition to the higher level evidence from international studies. Unfortunately no New Zealand studies were located. This approach was supported by Dietitian stakeholder consultation in May 2008. Articles identied to be the same level of evidence but reporting inconclusive ndings have been noted. Articles were excluded if they reported inconclusive ndings and were reviewed as being of a lower level of evidence than articles 2009 The Author Journal compilation 2009 Dietitians Association of Australia
Older adult
Note: Literature describing the setting as sub-acute was reviewed closely and reported according to the setting for which the participants were most aligned. In most cases these were the acute and rehabilitation settings.
supporting the evidence based statement. Some articles were assigned two levels of evidence. This was to demonstrate the difference between ndings generated from analyses performed within (Level IV) and between group (Level II-III-3). If no evidence was returned during the search this was identied as no evidence located in the evidence based statements. The grades of recommendations were then formulated from the evidence based statements. The ve components that are considered in judging the body of evidence to apply a grade of recommendation according to the NHMRC classication are the volume of evidence, consistency of the results, potential clinical impact of the proposed recommendation, and the generalisability of the body of evidence to the Australian health care context (Appendix 2).1 The grades of recommendation are: Level A Body of evidence can be trusted to guide practice. Level B Body of evidence can be trusted to guide practice in most situations. Level C Body of evidence provides some support for recommendation(s) but care should be taken in its application. S7
Nutrition & Dietetics 2009; 66 (Suppl. 3): S4S10
Level D
Body of evidence is weak and recommendation(s) must be applied with caution. A process of decision making to deal with any conict arising between members of the Steering Committee was agreed upon. If one or more Steering Committee members were in disagreement with the majority then these Committee members were requested to seek additional information to support their position. If the conict was unable to be resolved at this point then the process was for the Steering Committee to seek advice from an independent expert.
1.2.4 Development of the practice tips
Whilst evidence based statements are objective interpretations of available evidence, practice tips were developed by the Committee where there was insufcient high level evidence from the literature to support an evidence based statement, but enough low level evidence and/or expert opinion to provide a statement of support for a practice approach. The practice tips contained within these Guidelines acknowledge the diversity of settings and age related target groups and are often an extension to relevant evidence based statements in order to provide further detail or clarication. In all cases, the practice tips have required consensus by all members of the Committee and external reviewers. The Committee also recommends that evidence based recommendations and practice tips contained in this document are read in conjunction with relevant complementary guidelines. Some examples include the National Institute for Health and Clinical Excellence (NICE) Nutrition support in adults,3 European Society of Parenteral and Enteral Nutrition (ESPEN) guidelines on adult enteral nutrition19 and the stroke guidelines.20,21 The development process for these other Guidelines allowed recommendations based on both formal and informal consensus methods using expert opinion when there was an absence of scientic literature.
1.3 Consultation process
At the DAA 26th National Conference in 2008, a formative consultation with dietitians was sought on: relevant content, ease of use, clarity of recommendations, organisational barriers and whether or not these guidelines would be used in practice. The feedback provided by the ninety ve participants indicated that the majority of dietitians understood the Guideline development process; found that the Guideline format and structure were easy to follow; that the overall objectives were clear and that the evidence based recommendations were specic and unambiguous. Participants strongly agreed that they would use the Guidelines as part of their everyday practice. Most agreed that the Guidelines would help to bridge the gap between research and practice and that the Guidelines would result in the anticipated benets claimed. Specic feedback on improvements to the document were considered by the Committee and incorporated as appropriate. For example, a range of DAA endorsed evidence based S8
practice guidelines, were reviewed and cross referenced with the current document where relevant. These included; Evidence based practice guidelines for nutritional management of radiation therapy,13 cancer cachexia,14 chronic kidney disease15 and cystic brosis.16 The Committee decided that it was also important to include information on disease states such as cancer, renal disease and (Human Immunodeciency Virus/ Acquired Immune Deciency Syndrome ) HIV/ AIDS in order to answer question 1a. What is the prevalence of malnutrition and is it a problem?. However, these diseases are not referred to in later questions; instead reference is made to the above guidelines. Further, where participants identied gaps in the literature in the intervention section, additional studies were located including studies published after the nal date of the systematic search. A list of barriers to the implementation of the Guidelines in workplaces across the continuum of care were identied by workshop participants in 2008. Another workshop was held at the DAA 27th National Conference in 2009 which focussed on addressing the barriers to implementation previously identied. This body of work is discussed under Applicability. As part of the DAA guideline development process, these Guidelines have been independently reviewed by experts and assessed using the Appraisal of Guidelines for Research and Evaluation (AGREE) instrument.22 Modications to these Guidelines have been undertaken in response to this review. Since the Steering Committee acknowledge that dietitians do not act alone in either the detection or treatment of malnourished patients, it was considered important to consult with a wide range of health professionals and consumers of health services. The March 2008 version was circulated by DAA on behalf of the Steering Committee for multidisciplinary feedback to a range of organisations including: Aged Care Association Australia (ACAA) Australasian Podiatry Council Australian Association for Exercise and Sports Science Australian Association of Gerontology Australian Association for Quality in Health Care (AAQHC) Australian Association of Occupational Therapists Australian Association of Social Workers Australian General Practice Network Australian Physiotherapy Association Australian Psychology Society Australian College of Health Service Executives (ACHSE) Australian Meals On Wheels Australian New Zealand Society for Geriatric Medicine Institute of Hospitality in Healthcare Royal College of Nursing Australia Services for Australian Rural and Remote Allied Health (SARRAH) Services for Australian Rural and Remote Allied Health Society of Hospital Pharmacists of Australia Speech Pathology Australia The Royal Australasian College of Physicians 2009 The Author Journal compilation 2009 Dietitians Association of Australia
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
The Steering Committee sought comments from the above organisations regarding identication of relevant outcomes, target audiences, format for different users, obstacles to implementation, and formulation of implementation strategies. Unfortunately, despite the request for feedback from some twenty organisations, including two patient advocacy groups, feedback was received from only three organisations: Speech Pathology Australia; Royal College of Nursing Australia; and the Australian New Zealand Society for Geriatric Medicine. All feedback was discussed by the Steering Committee and incorporated into this nal version of the guidelines where appropriate. Further engagement with stakeholders will be undertaken as part of the launch by DAA of these guidelines and a formal stakeholder consultation will be incorporated into the strategic review plan.
1.4 Review process
The Guideline review process will be undertaken by the establishment of an implementation committee. The role of this committee will be to regularly review the evidence base and recommendations for practice. The implementation committee will establish an implementation and evaluation strategic plan in association with DAA. One focus will be to evaluate the contribution of the Guidelines towards achieving the anticipated benets listed at the front of the document. Another will be increasing awareness of this health issue and participation amongst stakeholders including patients in implementing sustainable practice change. This will be accomplished by converting these guidelines to a living document by using the Wiki format (refer to http://wiki.org for further information). This will allow ongoing comment by the target audience and timely revision of the document based on new evidence by the implementation committee. It is anticipated that at least bi-annual review will occur. The workshops conducted in 2008 and 2009 have also begun the evaluative phase of the guidelines and will continue as a result of the national guideline dissemination process.
1.5 Applicability
Although, these Guidelines provide the best available evidence and a framework to aid clinical decision making, they do not replace health professionals responsibility to make decisions appropriate to the circumstances of the individual patient. Malnutrition identication and treatment processes must conform with ethical and legal requirements. The best interests of the patient should be paramount; this includes a consideration of the risks and benets of identifying and treating malnutrition for the individual patient. Treatment must be undertaken with the informed consent of the patient or carer.3 Nutrition support management should be individualised and include the patients preferences and allow for commu 2009 The Author Journal compilation 2009 Dietitians Association of Australia
nication difculties or cognitive impairments. In addition, it needs to be culturally appropriate, comprehensive, and coordinated across all relevant disciplines and settings. The goals and outcomes of nutrition intervention will be dependent on the diagnosis and prognosis of the person. Patients need to be managed in the context of their co-morbidities. The benets and risks including potential adverse effects of any nutrition treatment such as risk of swallowing impairment need to be assessed and explained to the individual patient.3 For persons with end-stage disease the desired outcome of nutritional management is to maximise patient comfort and quality of life. The publication, Guidelines for a Palliative Approach in Residential Aged Care23 may help inform health professional decision making around physical symptom assessment and management for patients with end-stage disease. Putting evidence into practice is difcult.24 For these Guidelines to have an effect on reducing the burden of malnutrition on the Australian population there needs to an effective dissemination and implementation strategy. Innovations require one or more health professionals to lead, support and drive them through. Dietitians are ideally placed to act as clinical lead in applying this Guideline across Australian healthcare settings. Clinical coordinators are recognised as amongst the most effective implementation strategies.25 Practice change strategies coordinated by dietitian co investigators have been shown to lead to successful implementation of an evidence based guideline in a complex Australian healthcare setting.26 Also the DAA Board is committed to an active role in disseminating the Guideline by publication and to holding continuing professional development activities (road shows) around Australia to which all stakeholders will be invited. The DAA website, www.daa.asn.au will provide a link to the Guideline in both the members section (DINER) and a webpage available to non-members. National dissemination will support Dietitians to develop skills in organising screening pathways and using valid assessment tools. The DAA website will also link members with relevant implementation resources.27,28 The new National Competency Standards for Entry Level Dietitians in Australia29 now include performance criteria which support knowledge and skills in nutrition screening and assessment tools. National workshops conducted in 2008 and 2009 have resulted in participants identifying barriers and discussing solutions to overcoming these barriers (enablers) using the National Institute of Clinical Studies (NICS) barrier tool.30 Barriers typically included time, skills, knowledge and organisational agenda. Recognition of the importance of addressing malnutrition in a health setting together with staff/colleague willingness to prioritise management of malnutrition is a necessity for successful implementation.
1.6 Editorial Independence
The Guidelines were developed without the assistance of commercial sponsorship. As highlighted in the S9
Nutrition & Dietetics 2009; 66 (Suppl. 3): S4S10
Acknowledgements section of these guidelines, some funding was provided by both Hunter New England Population Health (Steering Committee Research Ofcer to devise and conduct a systematic review of the literature) and DAA (funded one face to face Steering Committee Meeting). In
kind support was provided by the employers of the Steering Group. To ensure integrity of the recommendations in these guidelines, Steering Committee members who were also authors of an article being reviewed were removed from the process of evaluating the article for levels of evidence.
S10
2009 The Author Journal compilation 2009 Dietitians Association of Australia
Nutrition & Dietetics 2009; 66 (Suppl. 3): S11S20
EVIDENCE BASED STATEMENTS 1. Nutrition Screening
Clinical question
1a: What is the prevalence of malnutrition and is it a problem?
Evidence Statement There is a high prevalence of malnutrition in the: Acute care setting (in the order of 2050%) Level of Evidence (using Aetiology criteriaAppendix 1) Level l12,31 Level ll3234 [Aus] Level IV3537 [Aus] Level l12 Level II32,3840 [Aus] Level l12 Level IV35,41 Level l12 Level IV42,43 [Aus]
Rehabilitation setting (in the order of 3050%) Residential aged care setting (in the order of 4070%) Community setting (in the order of 1030%)
The prevalence of malnutrition is higher in certain groups of individuals eg. in older adults; and in certain disease states: Older adults Level l12 Level IV35 [Aus] Cancer Level l12 Level IV35 [Aus] Critical illness Level l12 Level IV35 [Aus] Neurological disease Level l12 Orthopaedic injury Level l12 Level IV44 [Aus] Respiratory disease Level l12 Level IV45 [Aus] Gastrointestinal and liver disease Level l12 Renal disease Level l12 HIV and AIDS Level l12 Malnutrition is associated with adverse clinical outcomes and costs in the: Acute care setting Rehabilitation setting Residential aged care setting Community setting Malnutrition is under-recognised and under-diagnosed in the: Acute care setting Rehabilitation setting Residential aged care setting Community setting Level l12 Level II3840 [Aus] 46,47 Level II48 Level l12 Level II43 [Aus] Level I12,49 Level IV36,37 [Aus] Level l12 Level II39 [Aus] Level l12,49 Level lV50 [Aus] Level I12,49
Identication, documentation and coding of malnutrition results in a favourable reimbursement under casemix funding in the: Acute care setting Level II33 [Aus], 5153 Other settings Not applicable
2009 The Author Journal compilation 2009 Dietitians Association of Australia
S11
Nutrition & Dietetics 2009; 66 (Suppl. 3): S11S20
Nutritional status deteriorates in a signicant proportion of individuals over the course of admission in the: Acute care setting Level II5458 Rehabilitation setting Level II59 [Aus] Residential aged care setting No evidence located Community setting No evidence located Recommendations The prevalence of malnutrition is high worldwide (including in Australia) in all healthcare settings, yet is largely under-recognised and under-diagnosed resulting in a decline in nutritional status. Therefore, it is recommended that healthcare professionals are informed that malnutrition is associated with adverse clinical outcomes and costs. NHMRC Grade of recommendation: A Malnutrition should be identied, treated, and action taken to reduce the prevalence in Australian healthcare settings, and in community dwelling adults. NHMRC Grade of recommendation: B Clinical question
1b: Should there be routine screening for malnutrition and if so where and when should malnutrition screening occur?
Evidence Statement Level of Evidence (using Aetiology criteriaAppendix 1)
Implementation of malnutrition risk screening programs improves the identication of individuals at risk of malnutrition. Acute care setting Level II52,60 Rehabilitation setting No evidence located Residential aged care setting No evidence located Community setting Level lV61 Implementation of routine malnutrition risk screening facilitates timely and appropriate referral for nutrition care in settings. Acute setting Level II60,62,63 Rehabilitation setting No evidence located Residential aged care setting No evidence located Community setting Level lV61 There is no available evidence to determine the required frequency of routine malnutrition screening across settings. Across all settings No evidence located Recommendations Routine screening for malnutrition should occur in the acute setting to improve the identication of malnutrition risk and to allow for nutritional care planning. NHMRC Grade of recommendation: B Routine screening for malnutrition should occur in the rehabilitation, residential aged care and community setting to improve the identication of malnutrition risk and enable nutritional care planning. NHMRC Grade of recommendation: D Clinical question
1c: What screening process can be used to identify adults at risk of malnutrition?
Evidence Based Statement In the acute care setting, valid malnutrition screening tools include: Malnutrition Screening Tool (MST)64 [Aus] Malnutrition Universal Screening Tool (MUST)66 Mini Nutritional Assessment-Short Form (MNA-SF)71 older adults only Nutritional Risk Screening (NRS-2002)73 Simplied Nutritional Assessment Questionnaire (SNAQ(c))62 Level of Evidence (using Diagnostic criteriaAppendix 1) Level Level Level Level Level Level II65 III-264 [Aus] III-26670 III-172 III-268,69,73 II65
S12
2009 The Author Journal compilation 2009 Dietitians Association of Australia
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
In the rehabilitation setting, valid malnutrition screening tools include: MNA-SF71 Rapid Screen40 [Aus] In the residential aged care setting, valid malnutrition screening tools include: MNA-SF71 older adults only MUST66 Simplied Nutritional Appetite Questionnairec (SNAQ)78 Simple Nutrition Screening Tool79,80 In the community setting, valid malnutrition screening tools include: MNA-SF71 older adults only MUST66 Seniors in the Community: Risk Evaluation for Eating and Nutrition (SCREEN II)81 older adults only SNAQ78 (a) SNAQ(c)62
Level III-274 [Aus], 71 Level II40 [Aus] Level Level Level Level III-271,75,76 III-277 III-278 III-279,80
Level III-271,75 Level III-266 Level III-181 Level III-278 Level II82
Recommendation Use a valid malnutrition screening tool appropriate to the population in which it is to be applied. NHMRC Grade of recommendation: B
a
NB: there are two different screening tools called SNAQ; one developed in the USA78 and one developed in the Netherlands.62
Malnutrition Screening Practice Tips:
1a.i. Determination of malnutrition prevalence conduct a single day survey of the nutritional status of a majority of patients, residents or clients in your setting using a validated nutrition assessment tool (refer to Question 2). Prevalence of malnutrition = number of malnourished patients/total number of patients assessed. 1a.ii. In the acute setting, consider determination of potential reimbursement of coding for malnutrition under casemix funding.33 Refer to Nutrition Assessment practice tip 2.iii. 1a.iii. Reasons to exclude certain patient groups from malnutrition screening include: groups with low risk of malnutrition e.g. obstetric patients, who are unlikely to benet from intervention; or very high risk of malnutrition e.g. head and neck cancer patients requiring mandatory referral for nutritional intervention.13,49 1b.i. Malnutrition screening could be performed by people who come into contact with all individuals at risk of malnutrition such as nursing staff, assistants, administrative staff, doctors or directly by patients/ carers themselves. Who performs malnutrition screening may be dependent on the setting or specic facility e.g. dietetic assistants may conduct screening in rural facilities, whereas nursing staff may do this in tertiary hospitals.64 1b.ii. The malnutrition screen should be incorporated into standard processes e.g. admission forms, patient information sheets or residential aged care forms.49 1b.iii. Repeat malnutrition screening for those initially screened as at low risk. Due to lack of studies, there are no evidence-based statements regarding the frequency of nutrition screening, but examples of recommended screening frequency include: ideally rescreening weekly in hospital or rehabilitation 3 monthly in residential aged care settings,83 and annually in the community setting (perhaps by GP, practice nurse, MOW, HACC), or more frequently where there is clinical concern.42,84 1c.i. Select a valid malnutrition screening tool for your setting. Most of the valid malnutrition screening tools contain similar parameters. Some tools are very similar e.g. Rapid Screen40 and Simple Nutrition Screening tool79,80 both consist of Body Mass Index (BMI) and percentage weight loss. Key considerations for choice of a screening tool include: who will be undertaking the screening e.g. skill level, time to undertake; and burden of completion e.g. number of questions, measurements, equipment and calculations that may be required (refer to Appendix 3). For example; to determine BMI requires equipment for measurements, a certain level of skill to undertake the measurements and calculation of the actual BMI, which may result in the tool not being completed correctly.85 For calculation of BMI in older adults, an appropriate alternative method for estimating standing height is to measure knee height according to standard protocol and using purpose specic equipment.86 1c.ii. A scored malnutrition screening tool can help with workload management issues by prioritising those patients with the greatest need for nutrition support.64 1c.iii. Single parameters, such as Corrected Arm Muscle Area (CAMA), BMI and albumin, have some evidence of predictive validity8790 however, screening tools with at least two parameters are recommended because there is evidence that they have higher sensitivity and specicity at predicting nutritional status. 2009 The Author Journal compilation 2009 Dietitians Association of Australia S13
Nutrition & Dietetics 2009; 66 (Suppl. 3): S11S20
1c.iv. For patients identied as at risk of malnutrition, a process for assessment, intervention and monitoring needs to be put in place appropriate to the setting. It is important to regularly audit compliance with nutrition screening processes and address identied barriers. 1c.v. If the client has been referred to a dietitian by direct methods e.g. medical referral, nutrition screening is unnecessaryproceed directly to nutrition assessment and intervention. For details of screening tools validated in cancer and chronic kidney disease refer to the DAA endorsed guidelines by Isenring et al. 2008,13 Bauer et al. 200614 and Australia and New Zealand Renal Guidelines Taskforce.15
2. Nutrition Assessment
Clinical question
What nutrition assessment processes can be used to diagnose malnutrition in adults?
Evidence Based Statement In the acute care setting valid nutrition assessment tools include: Subjective global assessment (SGA)91 all adults Mini-nutritional assessment (MNA)97 (a) undertaken in older adults only Patient generated subjective global assessment (PG-SGA)102 all adults In the rehabilitation setting valid nutrition assessment tools include: Subjective global assessment (SGA) undertaken in older adults only Mini-nutritional assessment (MNA) undertaken in older adults only In the residential aged care setting valid nutrition assessment tools include: Subjective global assessment (SGA) undertaken in older adults only Mini-nutritional assessment (MNA) undertaken in older adults only In the community setting valid nutrition assessment tools include: Subjective global assessment (SGA) undertaken in older adults only Mini-nutritional assessment (MNA) undertaken in older adults only Level of Evidence (using Diagnostic criteriaAppendix 1) Level III-192,93 Level III-29496 Level III-275,95,98101 Level III-2103 (b) [Aus]
Level II104 Level III-239,47,105
(b)
Level III-248
(b)
Level III-275,98,105,106
Level III-2107 Level III-243 [Aus], 108 (b), 107,75,101 (b)
Recommendation Use a valid nutrition assessment tool appropriate to the population in which it is to be applied. NHMRC Grade of recommendation: B
Any modied versions of the MNA, SGA and PG-SGA (including cutoffs) cannot be assumed as validated until evaluated across a range of settings, against recognised nutrition assessment parameters, with adequate power. (b) Level of Evidence assessed using predictive (but not clinical) validity.
(a)
Nutrition Assessment Practice Tips:
2. Select a valid nutrition assessment tool for diagnosing protein-energy malnutrition which meets the needs of your setting, ideally across all patient/ client groups. 2.i. Training is required for the correct application of nutrition assessment tools. 2.ii. Nutrition assessment may not always be able to be completed immediately and more information may need to be sought, for example; from families of patients with communication or cognition difculties, or from interpreters for non-English speaking patients, or by direct observation of food intake, before a diagnosis of malnutrition can be made. However this should not preclude commencing a nutrition intervention. S14 2009 The Author Journal compilation 2009 Dietitians Association of Australia
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
2.iii. To diagnose malnutrition, use the ICD-10-AM Sixth Edition11 criteria (see Appendix 3): E43 Unspecied severe protein energy malnutrition In adults, BMI < 18.5 kg/m2 or unintentional loss of weight ( 10%) with evidence of suboptimal intake resulting in severe loss of subcutaneous fat and/or severe muscle wasting. E44 Protein-energy malnutrition of moderate and mild degree In adults, BMI < 18.5 kg/m2 or unintentional loss of weight (59%) with evidence of suboptimal intake resulting in moderate loss of subcutaneous fat and /or moderate muscle wasting. In adults, BMI < 18.5 kg/m2 or unintentional loss of weight (59%) with evidence of suboptimal intake resulting in mild loss of subcutaneous fat and/or mild muscle wasting. Amendments were made to the criteria for diagnosis of malnutrition in ICD-10-AM Sixth Edition (July 2008). In the acute care setting, clinical coders will now assign the appropriate code for malnutrition if there is adequate documentation by a dietitian. Consequently, dietitians need to ensure that nutrition documentation meets the diagnostic criteria. It is important to liaise with clinical coders in the acute care setting to discuss how the organisations documentation meets the diagnostic criteria. A malnutrition sticker may be useful to help identify patients to coders and standardise dietetic practice. In several Australian states in acute care facilities, assignment of the correct malnutrition code in some cases may increase the complexity and comorbidity level and thus, alter the Diagnosis Related Group and increase the casemix funding to the facility. 2.iv. The inclusion of BMI < 18.5 kg/m2 is based on World Health Organisation (WHO) criteria. However, in all settings clients with a higher BMI may be malnourished. There is evidence to suggest that weight loss of 5% annually is predictive of poor outcomes in older adults in acute and community settings.88,109,110 The mini nutritional assessment (MNA) acknowledges a higher BMI cut off for older adults.97 Unintentional weight loss is a better predictor of malnutrition than a weight or BMI at a single time point. For weight loss, a timeframe of 3 to 6 months is the consensus opinion,3 however clinical professional judgement should be used. 2.v. Single parameters have some evidence of predictive validity for nutrition assessment, however the same limitations apply here as for malnutrition screening (see practice point 1c.iii.). Valid assessment tools are recommended because they have higher sensitivity and specicity at predicting nutritional status. 2.vi. Subjective Global Assessment (SGA) and PG-SGA have previously been identied as valid methods of assessing nutritional status in patients as determined by levels of evidence in DAA Evidence Based Practice Guidelines for Nutrition Management Cancer Cachexia (SGA and PGSGA), Patients Receiving Radiation Therapy (SGA and PGSGA) and Chronic Kidney Disease (SGA).1315 2.vii. During nutritional assessment, as well as collecting pertinent data for diagnosing malnutrition, make sure to collect data on the aetiology or contributing causes of the low BMI, unintentional weight loss, and/or poor intake. These may include physiological causes such as altered nutrient need, malabsorption, Dysphagia, socio-economic causes such as lack of access to food, poor nutrition related knowledge, and psychological causes such as depression, dementia, and/or eating disorder. These causes of malnutrition are identied to inform the nutrition care process.8,9
3. Nutrition Goals, Interventions and Monitoring
Clinical question
3a: In adults with malnutrition or at risk of malnutrition, what are the appropriate nutrition goals, for optimal client, clinical and cost outcomes?
Evidence Statement Level of Evidence (using Intervention criteriaAppendix level 1)
In all settings improved outcomes may be achieved by establishing nutrition goals which focus on: Prevention of decline in nutritional status and associated adverse Level I3,111114 outcomes such as increased complications, including infections; incidence of pressure ulcer formation and mortality. Optimising nutritional status and other health outcomes by Level I3,112,115,116 improving total nutrient intake and body anthropometry in collaboration with the multidisciplinary team by timely interventions which are appropriate to the patients needs. Recommendation Aim to prevent decline/ improve nutritional status and associated outcomes in adults with malnutrition or at risk of malnutrition. NHMRC Grade of recommendation: A 2009 The Author Journal compilation 2009 Dietitians Association of Australia S15
Nutrition & Dietetics 2009; 66 (Suppl. 3): S11S20
Clinical question
3b: What are the appropriate interventions for prevention and treatment of malnutrition in adults?
Setting
(b)
Outcome(a)
Level of evidence
Modications to food provision methods may improve outcomes including: Level II Acute care Energy intake and weight status117 Level III-3 Global nutritional status118 Level II Rehabilitation Energy intake119 Level III-2 Protein intake119 Level II Residential aged care Fluid intake120 Level III-1 Energy and protein intake;121,122 weight status;123 physical function;123 quality of life; 123 and global nutritional status121 Level III-2 Community Weight status124 Level IV Global nutritional status125 NHMRC Grade of recommendation: B Feeding support provided by health care assistants may improve outcomes including: Level II Acute care Energy intake;126 body composition;126 use of antibiotics127 and life expectancy126 Rehabilitation No evidence located Residential aged care No evidence located Community No evidence located NHMRC Grade of recommendation: C A nutrition support team(c) may improve outcomes including: Level II Acute care Energy and protein intake128 Level IIl-1 Complications and costs129 Rehabilitation No evidence located Level IV Residential aged care Weight status130 Community No evidence located NHMRC Grade of recommendation: C Nutrition education provided on malnutrition to health professionals may improve outcomes: Acute care No evidence located Rehabilitation No evidence located Residential aged care No evidence located Level IIl-2 Community Global nutritional status131 NHMRC Grade of recommendation: D Multi-nutrient oral nutritional supplements (high energy and/or protein) may improve outcomes including: Level I Across settings Body composition,132,133 complications3 and life expectancy3,132,133 Level l Weight statusevidence of effect112 Level l Weight statusinconclusive3 Level ll Global nutritional status134 Level ll Energy intakeevidence of effect134 Level ll Energy intakeinconclusive135 Level III-2 Health care expenditure136 Level I Acute care Weight status;3,112,116 body composition;112,116 complications3,112 and pressure ulcers114 Level l Life expectancyevidence of an effect112,132,133 Level l Life expectancyinconclusive3 Level II Energy intake;137141 protein intake;139,141,142 global nutritional status143 and mood144 Level I Rehabilitation Complications and length of stay145 Level II Weight status;146 body composition146 and physical function147 Level IV Nutritional biochemistry; self-rated health and well-being148 Level I Residential aged care Weight status112 Level IV Energy intake149 Level I Community Weight status3,112 Level II Energy intake;150,151 body composition152 and physical function150,153 Level IV Cognition and quality of life154 [Aus] NHMRC Grade of recommendation: A S16 2009 The Author Journal compilation 2009 Dietitians Association of Australia
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
Dietary counselling(d) (with multi-nutrient oral nutritional supplements if deemed necessary) by a dietitian may improve outcomes including: Across settings No evidence located Level II Acute care Weight status and physical function155 Level IV Weight status and body composition156 Rehabilitation No evidence located Residential aged care No evidence located Community No evidence located NHMRC Grade of recommendation: C Enteral tube feeding(d) may improve outcomes including: Level I Across settings Complications111 Level l Acute care Weight status157 and length of stay158 Level I Risk of infectionevidence of effect158,159 Level l Risk of infectioninconclusive3 Level II Energy intake160 Level IV Body composition;161 nutritional biochemistry;161 and global nutritional status161,162 Rehabilitation No evidence located Residential aged care No evidence located Community No evidence located NHMRC Grade of recommendation: B Multi-nutrient oral nutritional supplements or enteral tube feeding in addition to exercise may improve outcomes including: Level II Acute care Weight status and nutritional biochemistry163 Level IV Physical function164,165 Level II Rehabilitation Weight status59 [Aus] Level II Residential aged care Energy intake and weight status166 Community No evidence located NHMRC Grade of recommendation: B Parenteral nutrition may improve outcomes including: Level I Acute care Risk of infection and life expectancy compared to no nutrition intervention159 Level I Life expectancy compared to EN, particularly delayed EN167 Level II Nutritional biochemistry168,169 Level IV Weight status170,171 and body composition170 Rehabilitation No evidence located Residential aged care No evidence located Community No evidence located NHMRC Grade of recommendation: B Individually prescribed nutritional support using mixed approaches (high energy diets +/- ONS; ETF; PN) may improve outcomes including: Level I Across settings Complications; risk of infection and length of stay111 Level II Acute care Energy intake172 and wound healing173 Level IV Weight status174 and nutritional biochemistry174 Rehabilitation No evidence located Level IV Residential aged care Weight status; body composition; nutritional biochemistry and physical function175 Community No evidence located NHMRC Grade of recommendation: C
2009 The Author Journal compilation 2009 Dietitians Association of Australia
S17
Nutrition & Dietetics 2009; 66 (Suppl. 3): S11S20
Recommendation Nutrition interventions can improve outcomes. Consideration should be given to the health care setting, resources, patient/client goals, requirements and preferences. NHMRC Grade of recommendation: BC
(a) Age, measures of body composition, nutritional biochemistry, global nutritional status (scores generated from two or more indicators of nutritional status), and other outcomes including physical function, vary across individual studies and readers are referred to study tables to determine measures used. (b) Studies evaluating food provision methods included strategies such as nutrient density, small portion sizes and improvements to the dining experience (eg. buffet style meals rather than pre-plated). (c) Nutrition support team interventions ranged from teams including a nurse and a dietitian to teams including nurses, a dietitian, speech and language therapists, caterers and occupational therapists. (d) Further evidence exists for certain patient groups [refer to Evidence Based Guidelines for the Nutritional Management of Patients Receiving Radiation Therapy].13 NB. Where NICE guidelines are referred to, only ndings from meta-analyses are included.3 ETF Enteral Tube Feed; ONS, High energy and protein multi-nutrient oral supplements; PN, Parenteral Nutrition. ,
Clinical question
3c: What are appropriate monitoring and outcome measures to demonstrate improved patient, clinical and cost outcomes?
Outcome measures Direct nutrition outcomes: Improving nutrition knowledge Suggested frequency of review of measure being monitored Inpatient: Daily initially for patient and team reducing to twice weekly as knowledge is gained3 Ambulatory: at least fortnightly13 Inpatient: Daily initially reducing to twice weekly when the patient/ resident is stable3 Ambulatory: minimum fortnightly dietitian contact13 Rationale or clarication Measure knowledge gained; behaviour change; adherence to plan.
Improved nutrient intake Energy Protein Fluid Improved nutrition anthropometry: Body weight
Monitor using direct observation and quantitative dietary intake methods especially of energy and protein.14 Monitor uid balance.176 Review progress towards nutrient goals; set criteria for commencing interventions such as high energy diets; ONS; ETF; PN.59 [Aus] Use calibrated equipment and standardised techniques and calculations where required. Ideally measure MAMC to take into account both body fat and muscle.175,177
MAMC Tricep skinfold thickness Improved score on validated global nutrition assessment tool Baseline and monthly MNA score134,143 PG-SGA score178
Inpatient: daily if concerns about uid status, otherwise weekly reducing to monthly3 Ambulatory: minimum fortnightly reducing to monthly; biannually as patient stabilises15 Baseline and monthly3
Global nutrition assessment tools can provide pre and post intervention comparisons so long as there is consistency in the application of the tool Many measures of nutritional biochemistry exist. Caution should be exercised in the interpretations of biochemistry particularly in the acute care setting; consideration should be given to the cost of testing and burden of testing to the patient.
Clinical and Health Status Outcomes Improved nutritional biochemistry Baseline then weekly3
S18
2009 The Author Journal compilation 2009 Dietitians Association of Australia
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
Prevention of pressure ulcers114
Patients at risk of developing pressure ulcers only: baseline/ admission and then weekly
Improved wound healing
Daily
Reduced infections and use of antibiotics Increased peak expiratory ow156 Decreased nausea, vomiting and/or diarrhea (from ONS and/or ETF) Patient-Centered Outcomes Improved quality of life, self rated health & well being
May be a suitable outcome measure for quality audits of the effectiveness of nutrition interventions Daily until problem resolves Daily until problem resolves
Consider a preventative nutrition intervention where there is a risk of pressure ulcers based on pressure ulcer risk tool e.g. Waterlow Pressure ulcer tool.114 Many tools are available; needs to be performed by an appropriately skilled health professional.154,173 Outcome needs to be monitored at the population level. To be performed by appropriate health professional. Intervene with early feeding where necessary. Review tolerance to formula/ feeding regimen to ensure achievement of goals.3,158 Use a culturally appropriate tool, e.g. Medical Outcomes Study 36-item Short-Form General Health Survey (SF-36) is commonly used.156 Culturally appropriate depression scales.144,179 Many measures of physical function exist, which may be used to monitor nutrition interventions. Tools require training, standardised techniques and calibrated equipment. Often, the measures may be undertaken in association with an appropriate health professional. For example, use the results of the Mini Mental State Examination (MMSE) tool.154 Outcome needs to be monitored at the population level.
Baseline and at the appropriate interval as per tool protocol
Improved mood Improved physical function Activities of Daily Living (eg; Katz index)147,155 Hand-grip strength
Baseline and at the appropriate interval as per tool protocol Baseline and monthly
Improved cognition
Baseline and at the appropriate interval as per tool protocol Hospital discharge, quarterly and yearly- audit health information datasets Yearly- survey of patients180
Improved life expectancy
Outcome needs to be monitored at the Patient satisfaction with nutrition population level. services provided by dietitians Healthcare utilisation and cost outcomes Reduced prevalence of Yearly-cross-sectional audit of Outcome needs to be monitored at malnutrition malnutrition prevalence the population level. Increased referrals of patients at Yearly-audit activity statistics risk of malnutrition to a dietitian Yearly-audit health information Reduced length of stay111 datasets Yearly-audit health information Reduced readmissions156 datasets Requires assistance from a Health Reduced costs11,136,176 Economist. Recommendation Choose standardised measures which change in a clinically meaningful way to demonstrate the outcomes of nutrition interventions. NHMRC Grade of recommendation: N/A
Note: The suggested frequency of review of the measures represents consensus opinion. MAMC, mid arm muscle circumference; MNA, mini nutritional assessment; High energy and protein multi-nutrient oral supplements; PG-SGA, Patient Generated- Subjective Global Assessment; PN, Parenteral Nutrition.
2009 The Author Journal compilation 2009 Dietitians Association of Australia
S19
Nutrition & Dietetics 2009; 66 (Suppl. 3): S11S20
Nutrition goals; intervention; monitoring practice tips:
3. The NICE Guideline Development Group recommend do not let your patients starve and when you offer them nutrition support, do so by the safest, most simplest, effective route.3 Consider nutrition support methods available in your setting, and assess any clinical risks. Ensure nutrition intervention will benet the patient and ethical and legal issues have been considered as well as clinical outcomes and quality of life.2 3a.i. Nutrition treatment goals and outcomes are based on each patients individual nutritional requirements and preferences. The goals address the multifactorial causes of malnutrition identied and prioritised during the assessment phase and are planned in partnership with the patient and health care team. 3b.i. Nutrition interventions include advocacy for food provision systems which support nutritional adequacy, for example; increased nutrient density (fortication of normal foods),119,163 more frequent meals and uids,120 improving the eating environment through socialisation,121 help with eating,126,127 and protected mealtimes.181 Ensure staff nutrition education programmes support these interventions.131 3b.ii. Consider liberalisation of previously prescribed or self imposed diets in older adults.182 3b.iii. Certain disease processes or conditions should mean automatic referral to a dietitian. For example; patients with eating and swallowing disturbances are often malnourished or at risk of malnutrition if the disturbance continues. Dysphagia is reported to affect 10% of acute patients, 3060% residents in Residential Aged Care facilities and 10% of the general population over the age of 50.182 Speech Pathologists are the appropriate health professionals to assess swallowing difculties, including aspiration.182 Consultation with a dietitian is also essential to ensure adequate hydration and nutrition can be obtained within the texture and uid modications that may be recommended.3,182 3b.iv. Start nutrition intervention prophylactically: for example; in the pre-operative phase provide nutrition interventions to surgical patients screened as at malnutrition risk and where appropriate continue nutrition support post surgery.113 3b.v. When providing multinutrient oral nutritional supplements, consider the following: base individual prescription on gap between oral intake and estimated requirements not met through oral intake alone.149,150 continuing the nutrition support for an adequate timeframe, since this is correlated with improved weight change.59 avoid administering high energy and protein multi-nutrient oral supplements (ONS) with meal times.183 delivering the ONS via the medication round to facilitate adherence.184 encouraging a supportive environment to facilitate adherence.184 using dietetic assistants to improve adherence to meal plans and ONS.126 3b.vi. Consider adjunctive therapies which support nutrition status maintenance or improvement. For example; referral to a regular exercise program for malnourished patients to improve function and oral intake.163,165,166 A comprehensive review of the literature on pharmaceutical interventions (orexigenic agents such as megestrol acetate and some anabolic steroids), was beyond the scope of these Guidelines. Please note, however, that these agents may improve outcomes relating to energy intake,185 weight status,186188 body composition,147,187,188 physical function147,187 and quality of life.147,187 3b.vii. It is outside the scope of these Guidelines to address the planning and administration of enteral or parenteral nutrition. Refer to DAA Enteral Feeding Manual for Adults in Health Care Facilities, DAA Parenteral Nutrition Manual for Adults in Health Care Facilities, ESPEN; American Society of Parenteral and Enteral Nutrition (ASPEN) and NICE Guidelines.3,189192 Home enteral and parenteral nutrition guidelines also exist via the NSW Greater Metropolitan Clinical Taskforce (GMCT) Guidelines190 and Australasian Society of Parenteral and Enteral Nutrition (AuSPEN) Guidelines.191 3b.viii. Treatment is timely and incorporates discharge planning and seamless transitions within and across sectors.193 The treatment outcomes are specic, measurable, achievable with the allocated resources, realistic to the patients circumstances and expectations, and the timeframe available.176 3c.i. Audits of malnutrition prevalence and/or dietitian referrals may be useful outcome indicators to evaluate quality improvement programmes. For example, OFlynn et al. 2005, demonstrated a decrease in malnutrition prevalence following the implementation of malnutrition screening; changes in food service delivery and nurse nutrition education.118 3c.ii. Root cause analysis of adverse events can be undertaken to improve future nutrition intervention practice. The occurrence of events such as refeeding syndrome, aspiration, lack of help with eating, inappropriate restraint of patients, inadequate access to appropriate & adequate normal food (example restricted dietary regimes such as clear uids), should be monitored and reported.
S20
2009 The Author Journal compilation 2009 Dietitians Association of Australia
Nutrition & Dietetics 2009; 66 (Suppl. 3): S21
ACKNOWLEDGEMENT
The Steering Committee would like to acknowledge the following people and organisations for their valuable contributions to the development of these guidelines. Catherine Roe (formerly Hunter New England Population Health NSW), Elizabeth Scott (Orange Base Hospital NSW) and Marian Barr (formerly Prince of Wales Hospital NSW) helped facilitate the workshop Looking beyond the screening tool: establishing best practice processes for malnutrition across the continuum of care at the DAA 24th National Conference 2006. Acknowledgement is also extended to all participants present at this workshop. Karen Abbey (formerly Queensland Health) and Elizabeth Scott were founding members of the Steering Committee formed to drive the guideline development, and assisted with the development of the clinical questions. Rachel Sutherland (Hunter New England Population Health NSW) organised funding for the Steering Committee Research Ofcer to devise and conduct a systematic review of the literature. Stephen Mears, Medical Librarian (John Hunter Hospital NSW), assisted the Research Ofcer with the literature search.
Fiona Barr (Flinders University), Jennifer Bengtson (Queensland University of Technology), Katrina Campbell (formerly Queensland University of Technology), Karen Fry (John Hunter Hospital NSW) and Jacinda Wilson (Queensland University of Technology) helped the committee members with sourcing identied articles and data extraction. Participants at the DAA 26th National Conference workshop: Crunch time: Evidence Based Guidelines for the Nutritional Management of Malnutrition across the Continuum of Care as well as the participants at the DAA 27th National Conference workshop: Implementing evidence based guidelines for nutritional management of adult malnutrition in your workplace for their valuable feedback. Dietitians Association of Australia funded interstate Steering Committee members to attend a face-to-face workshop in Brisbane in October 2008 to nalise the guidelines. Finally, appreciation is extended to respective employers for allowing committee members time to contribute to the development of these guidelines.
2009 The Author. Journal compilation 2009 Dietitians Association of Australia
S21
Nutrition & Dietetics 2009; 66 (Suppl. 3): S22S27
REFERENCES
1 National Health and Medical Research Council. N.H.M.R.C. additional levels of evidence and grades of recommendations for developers of guidelines-Pilot Program 2005; www.nhmrc. gov.au/consult/add_levels_grades_dev_guidelines2.htm. 2 Council of Europe. Resolution ResAP(2003)3E on food and nutritional care in hospitals. www.coe.int, 2003. Accessed 4 February 2005. 3 National Institute for Health and Clinical Excellence (NICE). Nutrition support in adults: oral nutrition support, enteral tube feeding and parenteral nutrition (clinical guideline 32). London National Institute for Health and Clinical Excellence (NICE), 2006. 4 Elia M, editor Guidelines for detection and management of malnutrition. Malnutrition Advisory Group. Maidenhead: BAPEN, 2000. 5 Dietitians Association of Australia. Acting on Obesity Working Party. Best practice guideline for the treatment of overweight and obesity in adults. Canberra: Dietitians Association of Australia, 2005; http://www.daa.asn.au/les/DINER/Obesity %20Guidelines%20(Final).pdf. 6 Hakel-Smith N, Lewis N. A standardised nutrition care process and language are essential components of a conceptual model to guide and document nutrition care and patient outcomes. J Am Diet Assoc 2004; 104: 187884. 7 Lacey K, Pritchett E. Nutrition Care Process and Model: ADA adopts road map to quality care and outcomes management. J Am Diet Assoc 2003; 103: 106172. 8 American Dietetic Association. Nutrition Diagnosis: A critical step in the nutrition care process. Chicago: American Dietetic Association, 2006. 9 Kieselhorst K, Skates J, Pritchett E. American Dietetic Association: Standards of practice in nutrition care and updated standards of professional performance. J Am Diet Assoc 2005; 105: 6415. 10 Jones JM. Nutritional screening and assessment tools. New York: Nova Science Publishers Inc, 2006. 11 National Centre for Classication in Health. Australian coding standards for I.C.D.-10-AM. Sydney: National Centre for Classication in Health, 2008. 12 Stratton RJ, Green CJ, Elia M. Disease-related malnutrition: an evidence-based approach to treatment. Wallingford: CABI Publishing, 2003. 13 Isenring L, Hill J, Davidson W, et al. Evidence Based Practice Guidelines for the Nutritional Management of Patients Receiving Radiation Therapy. Nutr Diet 2008; 65: S120. 14 Bauer J, Ash S, Davidson W, et al. Evidence based practice guidelines for the nutritional management of cancer cachexia. Nutr Diet 2006; 63: S332. 15 Australia and New Zealand Renal Guidelines Taskforce. Evidence Based Practice Guidelines for Nutritional Management of Chronic Kidney Disease. Canberra: Dietitians Association of Australia, 2005; http://www.daa.asn.au/les/DINER/CKD%20 Guidelines%202005.pdf. 16 National Cystic Fibrosis Interest Group. Australasian Clinical Practice Guidelines for Nutrition in Cystic Fibrosis. Dietitians Association of Australia 2006; http://www.daa.asn.au/les/ DINER/Aust%20Clin_Pract_Guide_CF_nal.pdf. 17 Cameron I, Handoll H, Finnegen T, Langhorne P. Multidisciplinary rehabilitation for older people with hip fractures [pro18
19 20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
tocol]. The Cochrane database of systematic review. 2008: art.no.:CD007125. DOI:10.1002/14651858.CD007125. Department of Health and Ageing. Part 5: Residential Care Services. 2008; http://www.health.gov.au/internet/main/ publishing.nsf/Content/ageing-publicat-aged-careaustralia.htm~ageing-publicat-aged-care-australia-p1. Lochs H, Valentini L, Schtz T, et al. ESPEN Guidelines on adult enteral nutrition. Clin Nutr 2006; 25: 177360. National Stroke Foundation. Clinical Guidelines for Acute stroke Management. 2007; http://www.strokefoundation. com.au/news/welcome/clinical-guidelines-for-acute-strokemanagement. Accessed 8 November 2008. National Stroke Foundation. Clinical Guidelines for stroke rehabilitation and recovery. 2005; http://www. strokefoundation.com.au. Accessed 8 August 2007. The AGREE Collaboration. Appraisal of Guidelines for Research and Evaluation (AGREE) Instrument. London: St Georges Hospital Medical School, 2001. Accessed 4 February 2005. National Health and Medical Research Council. Guidelines for a Palliative Approach in Residential Aged Care. In: Prepared by Edith Cowan University, editor: Canberra: Commonwealth of Australia, 2006; http://www.nhmrc.gov.au/PUBLICATIONS/ synopses/ac12to14syn.htm. Accessed 3 September 2008. National Health and Medical Research Council. How to put the evidence into practice: implementation and dissemination strategies. Canberra: Commonwealth of Australia 2000; http:// www.nhmrc.gov.au/publications/synopses/_les/cp71.pdf. Livesay EA, Noon JM. Implementing guidelines: what works. Archives of disease in Childhood Education and Practice Edition 2007; 92: 12934. Doig G, Simpson F, Finfer S, et al. Effect of Evidence-based Feeding Guidelines on Mortality of Critically Ill Adults. J Am Med Assoc 2008; 300: 273141. National Institute for Health and Clinical Excellence (NICE). Suggested actions for implementing the NICE clinical guideline on nutrition support in adults National Institute for Health and Clinical Excellence (NICE), 2006; http:// www.nice.org.uk/CG032. Accessed 8 November 2008. Splett PL. Developing and Validating Evidence-Based Guides for Practice: A Tool Kit for Dietetics Professionals. Chicago: American Dietetic Association, 1999. Dietitians Association of Australia. National Competency Standards, 2009; http://www.daa.asn.au/index.asp?PageID= 2145872322. National Institute of Clinical Studies (NICS). Identifying Barriers to evidence uptake. Melbourne: National Institute of Clinical Studies, 2006; http://www.nhmrc.gov.au/nics/ material_resources/resources/identifying_barriers.htm. Accessed 4 February 2009. Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr 2008; 27: 515. Beck E, Patch C, Milosavljevic M, et al. Implementation of malnutrition screening and assessment by dietitians: malnutrition exists in acute and rehabilitation settings. Aust J Nutr Diet 2001; 58: 927. Ferguson M, Capra S, Bauer J, Banks M. Coding for malnutrition enhances reimbursement under casemix-based funding. Aust J Nutr Diet 1997; 54: 1028. Thomas JM, Isenring E, Kellett E. Nutritional status and length of stay in patients admitted to an acute assessment unit. J Hum Nutr Dietet 2007; 20: 3208.
S22
2009 The Author Journal compilation 2009 Dietitians Association of Australia
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
35 Banks M, Ash S, Bauer J, Gaskill D. Prevalence of malnutrition in adults in Queensland public hospitals and residential aged care facilities. Nutr Diet 2007; 64: 1728. 36 Lazarus C, Hamlyn J. Prevalence and documentation of malnutrition in hospitals: A case study in a large private hospital setting. Nutr Diet 2005; 62: 417. 37 Middleton MH, Nazarenko G, Nivison-Smith I, Smerdely P. Prevalence of malnutrition and 12-month incidence of mortality in two Sydney teaching hospitals. Intern Med J 2001; 31: 45561. 38 Kaur S, Miller M, Giles L, Halbert J, Crotty M. Nutritional status and clinical outcomes of older adults participating in ambulatory rehabilitation. Asia Pac J Clin Nutr 2008; 17: 199 207. 39 Neumann S, Miller M, Daniels L, Crotty M. Nutritional status and clinical outcomes of older patients in rehabilitation. J Hum Nutr Dietet 2005; 18: 12936. 40 Visvanathan R, Penhall R, Chapman I. Nutritional screening of older people in a sub-acute care facility in Australia and its relation to discharge outcomes. Age Ageing 2004; 33: 2605. 41 Miller M, Loh W, Watterson C, Fraser A, Nowson C. Nutrition screening in long term care facilities: an evaluation of the methodological quality of available instruments. CAB Reviews: Perspectives in Agriculture, Veterinary Science, Nutrition and Natural Resources 2008; 3: 17. 42 Leggo M, Banks M, Isenring E, Stewart L, Tweedale M. A quality improvement nutrition screening and intervention program available to Home and Community Care eligible clients. Nutr Diet 2008; 65: 1616. 43 Visvanathan R, Macintosh C, Callary M, Penhall R, Horowitz M, Chapman I. The nutritional status of 250 older Australian recipients of domicillary care services and its association with outcomes at 12 months. J Am Geriatr Soc 2003; 51: 100711. 44 Miller M, Crotty M, Whitehead C, Daniels L, Finucane P. Nutritional assessment and intervention in patients admitted with a femoral neck fracture: a chronicle of missed opportunities. Nutr Diet 2001; 58: 8691. 45 Humphreys K, Cross G, Frith P, Cafarella P. Nutritional status and dietary intake of outpatients with chronic obstructive pulmonary disease. Nutr Diet 2008; 65: 16874. 46 Brantervik AM, Jacobsson IE, Grimby A, Wallen TCE, Bosaeus IG. Older hospitalised patients at risk of malnutrition: correlation with quality of life, aid from the social welfare system and length of stay? Age Ageing 2005; 34: 4449. 47 Thomas DR. Malnutrition in subacute care. Am J Clin Nutr 2002; 75: 30813. 48 Sacks GS, Dearman K, Replogle WH, Cora VL, Meeks M, Canada T. Use of subjective global assessment to identify nutrition associated complications and death in geriatric long term care facility residents. J Am Coll Nutr 2000; 19: 5707. 49 Elia M, Zellipour L, Stratton R. To screen or not to screen for adult malnutrition? Clin Nutr 2005; 24: 86784. 50 Gaskill D, Black LJ, Isenring E, Hassell S, Sanders F, Bauer JD. Malnutrition prevalence and nutrition issues in residential aged care facilities. Australasian Journal on Ageing 2008; 27: 18994. 51 Amaral TF, Matos LC, Tavares MM, et al. The economic impact of disease-related malnutrition at hospital admission. Clin Nutr 2007; 26: 77884. 52 Ockenga J, Freudenreich M, Zakonsky R, Norman K, Pirlich M, Lochs H. Nutritional assessment and management in hospitalised patients: Implication for DRG-based reimbursement and health care quality. Clin Nutr 2005; 24: 91319.
53 Raja R, Lim AV, Lim YP, Lim G, Chan SP, Vu CKF. Malnutrition screening in hospitalised patients and its implication on reimbursement. Intern Med J 2004; 34: 17681. 54 Braunschweig C, Gomez S, Sheean PM. Impact of declines in nutritional status on outcomes in adult patients hospitalized for more than 7 days. J Am Diet Assoc 2000; 100: 131622. 55 Bruun LI, Bosaeus I, Bergstad I, Nygaard K. Prevalence of malnutrition in surgical patients: evaluation of nutritional support and documentation. Clin Nutr 1999; 18: 1417. 56 Dzieniszewski J, Jarosz M, Szczygiel B, et al. Nutritional status of patients hospitalised in Poland. Eur J Clin Nutr 2005; 59: 55260. 57 Gariballa S. Malnutrition in hospitalized elderly patients: when does it matter? Clin Nutr 2001; 20: 48791. 58 Kondrup J, Johansen N, Plum LM, et al. Incidence of nutritional risk and causes of inadequate nutritional care in hospitals. Clin Nutr 2002; 21: 4618. 59 Miller M, Crotty M, Whitehead C, Bannerman E, Daniels L. Nutritional supplementation and resistance training in nutritionally at risk older adults following lower limb fracture: a randomized controlled trial. Clin Rehabil 2006; 20: 31123. 60 Roubenoff R, Roubenoff RA, Preto J, Balke W. Malnutrition among Hospitalized Patients. Arch Intern Med 1987; 147: 146265. 61 Coombs J. The Role of Nutrition Screening and Intervention Programs in Managed Care. Manag Care Q 1998; 6: 4350. 62 Kruizenga HM, Seidell JC, De Vet HCW, Wierdsma NJ, van Bokhurst-de Van der Schueren MAE. Development and validation of a hospital screening tool for malnutrition: the short nutritional assessment questionnaire (SNAQ). Clin Nutr 2005; 24: 7582. 63 Rypkema G, Adang E, Dicke H, et al. Cost-effectiveness of an interdisciplinary intervention in geriatric inpatents to prevent malnutrition. J Nutr Health Aging 2003; 2: 1227. 64 Ferguson M, Capra S, Bauer J, Banks M. Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition 1999; 15: 45864. 65 van Venrooij LMW, de Vos R, Borgmeijer-Hoelen AMMJ, Kruizenga HM, Jonkers-Schuitema CF, deMol BAMJ. Quickand-easy nutritional screening tools to detect disease-related undernutrition in hospital in-and out-patient settings: A systematic review of sensitivity and specicity. e-SPEN 2007; 2: 2137. 66 Elia M. Screening for malnutrition: a multidisciplinary responsibility. Development and use of the malnutrition universal screening tool (MUST) for Adults. Redditch: BAPEN, 2003. 67 Malnutrition Advisory Group (MAG): A Standing Committee of the British Association for Parenteral and Enteral Nutrition (BAPEN). The MUST Explanatory Booklet. A Guide to the Malnutrition Universal Screening Tool (MUST) for Adults: BAPEN, 2003. Accessed 17 October 2005. 68 Stratton RJ, Hackston A, Longmore D, et al. Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the mlanutrition universal screening tool (MUST) for adults. Br J Nutr 2004; 92: 799808. 69 Kyle UG, Kossovsky MP, Karsegard VL, Pichard C. Comparison of tools for nutritional assessment and screening at hospital admission: a population study. Clin Nutr 2006; 25: 40917. 70 Stratton RJ, King CL, Stroud MA, Jackson AA, Elia M. Malnutrition Universal Screening Tool predicts mortality and length of hospital stay in acutely ill elderly. Br J Nutr 2006; 95: 32530.
2009 The Author Journal compilation 2009 Dietitians Association of Australia
S23
Nutrition & Dietetics 2009; 66 (Suppl. 3): S22S27
71 Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form Mini-Nutritional Assessment (MNA-SF). Journal of Gerontology A Biol Sci Med Sci 2001; 56: M36672. 72 Ranhoff AH, Gjoen AU, Mowe M. Screening for malnutrition in elderly acute medical patients: the usefulness of MNA-SF. J Nutr Health Aging 2005; 9: 2215. 73 Kondrup J, Rasmussen HH, Hamberg O, Stanga Z. Nutritional Risk Screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 2003; 22: 32136. 74 Neumann SA, Miller MD, Daniels LA, Ahern M, Crotty M. Inter-rater reliability and validity of the mini nutritional assessment in older Australians undergoing rehabilitation. Nutr Diet 2007; 64: 17985. 75 Kuzuya M, Kanda S, Koike T, Suzuki Y, Statke S, Iguchi A. Evaluation of the Mini-Nutritional Assessment for Japanese frail elderly. Nutrition 2005; 21: 498503. 76 Langkamp-Henken B, Hudgens J, Stechmiller JK, HerrlingerGarcia KA. Mini Nutritional Assessment and screening scores are associated with nutritional indicators in elderly people with pressure ulcers. Journal of the America Dietetic Association 2005; 105: 15906. 77 Harris DG, Davies C, Ward H, Haboubi NY. An observational study of screening for malnutrition in elderly people living in sheltered accommodation. J Hum Nutr Dietet 2008; 21: 39. 78 Wilson M-MG, Thomas DR, Rubenstein LZ, et al. Appetite assessment: simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am J Clin Nutr 2005; 82: 107481. 79 Laporte M, Villalon L, Payette H. Simple nutrition screening tools for healthcare facilities: development and validity assessment. Can J Diet Pract Res 2001; 62: 2634. 80 Laporte M, Villalon L, Thibodeau J, Payette H. Validity and reliability of simple nutrition screening tools adapted to the elderly population in healthcare facilities. J Nutr Health Aging 2001; 5: 2924. 81 Keller HH, Goy R, Kane SL. Validity and reliability of SCREEN II (Seniors in the Community: Risk evaluation for eating and nutrition, Version II). Eur J Clin Nutr 2005; 59: 114957. 82 Neelemaat F, Kruizenga HM, de Vet HC, Seidell JC, Butterman M, van Bokhorst-de Van der Schueren MA. Screening malnutrition in hospital outpatients. Can the SNAQ malnutrition screening tool also be applied to this population? Clin Nutr 2008; 27: 43946. Epub 2008 Apr 18. 83 Victorian Government Department of Human Services. Resource Manual Quality Indicators in Public Sector Aged Care Services-Resource Manual 2007200 version 1. http:// www.health.vic.gov.au/agedcare/downloads/ psracs_resource_manualpdf. Melbourne: Published by Rural and Regional Health and Aged Care Services Division, Victorian Government Department of Human Services, 2007; http://www.health.vic.gov.au/agedcare/downloads/ psracs_resource_manual.pdf. 84 Vellas B, Villars H, Abellan G, et al. Overview of the MNAIts history and challenges. Journal of Nutrition, Health & Aging 2006; 10: 45663; discussion 635. 85 Cook S, Kirk S, Lawrenson S, Sandford S. Use of BMI in the assessment of malnutrition in older subjects: reecting on practice. Proc Nutr Soc 2005; 64: 31317. 86 Hickson M, Frost G. A comparison of three methods for estimating height in acutely ill elderly population. J Hum Nutr Dietet 2003; 16: 1320.
87 Kulminski AM, Arbeev KG, Kulminskaya IV, et al. Body mass index and nine-year mortality in disabled and nondisabled older U.S. individuals. J Am Geriatr Soc 2008; 56: 10510. 88 Beck AM, Ovesen L. At which body mass index and degree of weight loss should hospitalised elderly patients be considered at nutritional risk? Clin Nutr 1998; 17: 1958. 89 Miller M, Crotty M, Giles L, et al. Corrected arm muscle area: an independent predictor of long term mortality in communitydwelling older adults. J Am Geriatr Soc 2002; 50: 12727. 90 Ranieri P, Bianchetti A, Margiotta A, Virgillo A, Clini E, Trabucchi M. Predictors of 6-Month Mortality in Elderly Patients with Mild Chronic Obstructive Pulmonary Disease Discharged from a Medical Ward After Acute Nonacidotic Exacerbation. J Am Geriatr Soc 2008; 56: 90913. 91 Detsky AS, McLaughlin JR, Baker JP, et al. What is Subjective Global Assessment of Nutritional Status? Journal of Parenteral and Enteral Nutrition 1987; 11: 813. 92 Baker JP, Detsky AS, Wesson DE, et al. Nutritional assessment: a comparison of clinical judgement and objective measurements. N Engl J Med 1982; 306: 96972. 93 Baker JP, Detsky AS, Whitwell J, Langer B, Jeejeebhoy KN. A comparison of the predictive value of nutritional assessment techniques. Hum Nutr Clin Nutr 1982; 36: 23341. 94 Kyle UG, Unger P, Mensi N, Genton L, Pichard C. Nutrition Status in Patients Younger and Older Than 60 y at Hospital Admission: A Controlled Population Study in 995 Subjects. Nutrition 2002; 18: 46369. 95 Persson MD, Brismar KE, Katzarski KS, Nordenstrom J, Cederholm TE. Nutritional status using mini nutritional assessment and subjective global assessment predict mortality in geriatric patients. J Am Geriatr Soc 2002; 50: 19962002. 96 Pirlich M, Schutza T, Normana K, et al. The German hospital malnutrition study. Clin Nutr 2006; 25: 56372. 97 Guigoz Y, Vellas B, Garry PJ. Assessing the Nutritional Status of the Elderly: The Mini Nutritional Assessment as Part of the Geriatric Evaluation. Nutr Rev 1996; 54: S5965. 98 Compan B, Di Castri A, Plaze JM, Arnaud-Battandier F. Epidemiological study of malnutrition in elderly patients in acute, sub-acute and long-term care using the MNA. Journal of Nutrition, Health & Aging 1999; 3: 14651. 99 Gazzotti C, Albert A, Pepinster A, Petermans J. Clinical usefulness of the mini nutritional assessment (MNA) scale in geriatric medicine. Journal of Nutrition, Health & Aging 2000; 4: 17681. 100 Van Nes MC, Herrmann FR, Gold G, Michel JP, Rizzoli R. Does the Mini Nutritional Assessment predict hospitalization outcomes in older people? Age Ageing 2001; 30: 2216. 101 Vellas B, Guigoz Y, Garry PJ, et al. The Mini Nutritional Assessment (MNA) and Its Use in Grading the Nutritional State of Elderly Patients. Nutrition 1999; 15: 11622. 102 Ottery F. Denition of standardized nutritional assessment and interventional pathways in oncology. Nutrition 1996; 12 (supp 1): S159. 103 Martineau J, Bauer JD, Isenring E, Cohen S. Malnutrition determined by the patient-generated subjective global assessment is associated with poor outcomes in acute stroke patients. Clin Nutr 2005; 24: 10737. 104 Duerksen DR, Yeo TA, Siemens JL, OConnor MP. The validity and Reproducibility of clinical assessment of nutritional status in the elderly. Nutrition 2000; 16: 7404. 105 Donini LM, Rosano A, De Felice MR, et al. MNA predictive value in the follow up of geriatric patients. Journal of Nutrition, Health & Aging 2003; 75: 28293.
S24
2009 The Author Journal compilation 2009 Dietitians Association of Australia
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
106 Saletti A, Lindgren EY, Johansson L, Cederholm TE. Nutritional status according to mini nutritional assessment in an institutionalised elderly population in Sweden. Gerontology 2000; 46: 13945. 107 Christensson L, Unosson M, Ek A. Evaluation of nutritional assessment techniques in elderly people newly admitted to municipal care. Eur J Clin Nutr 2002; 56: 81018. 108 Beck AM, Ovesen L, Schroll M. A six months prospective follow up of 65+ year old patients from general practice classied according to nutritional risk by the Mini Nutritional Assessment. Eur J Clin Nutr 2001; 55: 102833. 109 Bannerman E, Miller MD, Daniels L, et al. Anthropometric indices predict physical function and mobility in older Australians: the Australian Longitudinal Study of Ageing. Public Health Nutrition 2002; 5: 65562. 110 Newman AB, Yanez D, Harris T, Duxbury A, Enright PT, Fried LP. Weight change in old age and its association with mortality. Journal of American Geriatrics Society 2001; 49: 130918. 111 Koretz R, Avenell A, Lipman T, Braunschweig C, Milne A. Does Enteral Nutrition affect clinical outcome? A systematic review of the randomized trials. Am J Gastroenterol 2007; 102: 412 29. 112 Milne A, Avenell A, Potter J. Meta-Analysis: Protein and energy supplementation in older people. Ann Intern Med 2006; 144: 3748. 113 Weimann A, Braga M, Harsanyi L, Laviano A, Ljunqvist O, Soeters P. E.S.P.E.N Guidelines on Enteral Nutrition: Surgery including Organ Transplantation. Clin Nutr 2006; 25: 22444. 114 Stratton RJ, Ek AC, Engfer M, et al. Enteral nutritional support in prevention and treatment of pressure ulcers: a systematic review and meta-analysis. Ageing Res Rev 2005; 4: 42250. 115 Baldwin C, Parsons T, Logan S. Dietary advice for illnessrelated malnutrition in adults (Review). Cochrane Database of Systematic Reviews. 2007: Art. No.:CD002008. DOI: 10.1002/14651858.CD002008.pub2. 116 Vanderkroft D, Collins C, FitzGerald M, Lewis S, Neve M, Capra S. Minimising undernutrition in the older inpatient. International Journal of Evidence-based Healthcare 2007; 5: 110 81. 117 Forli L, Pedersen J, Bjortuft O, Vatn M, Boe J. Dietary support to underweight patients with end-stage pulmonary disease assessed for lung transplantation. Respiration 2001; 68: 517. 118 OFlynn J, Peake H, Hickson M, Foster D, Frost G. The prevalence of malnutrition in hospitals can be reduced: results from three consecutive cross-sectional studies. Clin Nutr 2005; 24: 107888. 119 Barton A, Beigg C, Macdonald I, Allison S. A recipe for improving food intakes in elderly hospitalized patients. Clin Nutr 2000; 19: 4514. 120 Taylor K, Barr S. Provision of small, frequent meals does not improve energy intake of elderly residents with dysphagia who live in an extended-care facility. J Am Diet Assoc 2006; 106: 111518. 121 Nijs K, de Graaf C, Siebelink E, et al. Effect of family-style meals on energy intake and risk of malnutrition in Dutch nursing home residents: a randomized controlled trial. J Gerontol 2006; 61A: 93542. 122 Young KW, Greenwood CE, van Reekum R, Binns MA. A randomised, crossover trial of high-carbohydrate foods in nursing home residents with Alzheimers disease: associations among intervention response, body mass index, and behavioural and cognitive function. Journals of Gerontology Series ABiological Sciences & Medical Sciences 2005; 60: 103945.
123 Nijs KA, de Graaf C, Kok FJ, van Staveren WA. Effect of family style mealtimes on quality of life, physical performance and body weight of nursing home residents: cluster randomised controlled trial. BMJ 2006; 332: 11804. 124 Krester A, Voss T, Kerr W, Cavadini C, Friedmann J. Effects of two models of nutritional intervention on homebound older adults at nutritional risk. Journal of the American Dietetic Association 2003; 103: 32936. 125 Keller HH. The SCREEN I (Seniors in the Community: Risk Evaluation for Eating and Nutrition) index adequately represents nutritional risk. J Clin Epidemiol 2006; 59: 83641. 126 Duncan D, Beck S, Hood K, Johansen A. Using dietetic assistants to improve the outcome of hip fracture: a randomised controlled trial of nutritional support in an acute trauma ward. Age Ageing 2006; 35: 14853. 127 Hickson M, Bulpitt C, Nunes M, et al. Does additional feeding support provided by health care assistants improve nutritional status and outcome in acutely ill older in-patients?a randomised control trial. Clin Nutr 2004; 23: 6977. 128 Johansen N, Kondrup J, Plum L, et al. Effect of nutritional support on clinical outcome in patients at nutritional risk. Clin Nutr 2004; 23: 53950. 129 Hassell JT, Games AD, Shaffer B, Harkins LE. Nutrition support team management of enterally fed patients in a community hospital is cost-benecial. J Am Diet Assoc 1994; 94: 9938. 130 Biernacki C, Barratt J. Improving the nutritional status of people with dementia. Br J Nurs 2001; 10: 110414. 131 Faxen-Irving G, Andren-Olsson B, Geijerstam A, Basun H, Cederholm T. Nutrition education for care staff and possible effects on nutritional status in residents of sheltered accommodation. Eur J Clin Nutr 2005; 59: 94754. 132 Milne A, Avenell A, Potter J. Oral protein and energy supplementation in older people: a systematic review of randomized trials. Nestle Nutrition Workshop Series Clinical & Performance Program 2005; 10: 10325. 133 Milne A, Potter J, Avenell A. Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database of Systematic Reviews. 2005: Art. No.: CD003288. 134 Lauque S, Arnaud-Battandier F, Gillette S, et al. Improvement of weight and fat free mass with oral nutritional supplementation in patients with Alzheimers disease at risk of malnutrition: a prospective randomized study. J Am Geriatr Soc 2004; 52: 17027. 135 MacFie J, Woodcock N, Palmer M, Walker A, Townsend S, Mitchell C. Oral dietary supplements in pre- and postoperative surgical patients: a prospective and randomized clinical trial. Nutrition 2000; 16: 7238. 136 Arnaud-Battandier F, Malvy D, Jeandel C, et al. Use of oral supplements in malnourished elderly patients living in the community: a pharmaco-economic study. Clin Nutr 2004; 23: 1096103. 137 Ryan M, Salle A, Favreau A-M, et al. Oral supplements differing in fat and carbohydrate content: effect on the appetite and food intake of undernourished elderly patients. Clin Nutr 2004; 23: 6839. 138 Potter J, Roberts M, McColl J, Reilly J. Protein energy supplements in unwell elderly patientsa randomized controlled trial. Journal of Parenteral and Enteral Nutrition 2001; 25: 323 29. 139 Vermeeren M, Wouters E, Geraerts-Keeris A, Schols A. Nutritional support in patients with chronic obstructive pulmonary disease during hospitalization for an acute exacerbation;
2009 The Author Journal compilation 2009 Dietitians Association of Australia
S25
Nutrition & Dietetics 2009; 66 (Suppl. 3): S22S27
140
141 142
143
144
145
146
147
148
149
150
151
152
153
154
155
156
157
a randomized controlled feasibility trial. Clin Nutr 2004; 23: 118492. Irvine P, Mouzet J, Marteau C, et al. Short-term effect of a protein load on appetite and food intake in diseased mildly undernourished elderly people. Clin Nutr 2004; 23: 114652. Saluja S, Kaur N, Shrivastava U. Enteral nutrition in surgical patients. Surg Today 2002; 32: 6728. Bourdel-Marchasson I, Barateau M, Rondeau V, et al. A Multicenter trial of the effects of oral nutritional supplementation in critically ill older inpatients. Nutrition 2000; 16: 15. Gazzotti C, Arnaud-Battandier F, Parello M, et al. Prevention of malnutrition in older people during and after hospitalisation: results from a randomised controlled clinical trial. Age Ageing 2003; 32: 3215. Gariballa S, Forster S. Effects of dietary supplements on depressive symptoms in older patients: A randomised doubleblind placebo-controlled trial. Clin Nutr 2007; 26: 54551. Avenell A, Handoll H. Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database of Systematic Reviews. 2006: Art No.: CD001880. Steiner M, Barton R, Singh S, Morgan M. Nutritional enhancement of exercise performance in chronic obstructive pulmonary disease: a randomised controlled trial. Thorax 2003; 58: 74551. Tidermark J, Ponzer S, Carlsson P, et al. Effects of protein-rich supplementation and nandrolone in lean elderly women with femoral neck fractures. Clin Nutr 2004; 23: 58796. Creutzberg E, Wouters E, Mostert R, Weling-Scheepers C, Schols A. Efcacy of nutritional supplementation therapy in depleted patients with chronic obstructive pulmonary disease. Nutrition 2003; 19: 1207. Lauque S, Arnaud-Battandier F, Mansourian R, et al. Proteinenergy oral supplementation in malnourished nursing home residents. A controlled trial. Age Ageing 2000; 29: 516. Edington J, Barnes R, Bryan F, et al. A prospective randomised controlled trial of nutritional supplementation in malnourished elderly in the community: clinical and health economic outcomes. Clin Nutr 2004; 23: 195204. Knowles J, Fairbarn M, Wiggs B, Chan-Yan C, Pardy R. Dietary supplementation and respiratory muscle performance in patients with COPD. Chest 1988; 93: 97783. Otte K, Anhlburg P, DAmore F, Stellfeld M. Nutritional repletion in malnourished patients with emphysema. Journal of Parenteral and Enteral Nutrition 1989; 13: 1526. Price R, Daly F, Pennington C, McMurdo M. Nutritional supplementation of very old people at hospital discharge increases muscle strength: A randomised controlled trial. Gerontology 2005; 51: 17985. Collins C, Kershaw J, Brockington S. Effect of nutritional supplements on wound healing in home-nursed elderly: A randomized trial. Nutrition 2005; 21: 14755. Persson M, Hytter-Landahl A, Brismar K, Cederholm T. Nutritional supplementation and dietary advice in geriatric patients at risk of malnutrition. Clin Nutr 2007; 26: 21624. Norman K, Kirchner H, Freudenreich M, Ockenga J, Lochs H, Pirlich M. Three month intervention with protein and energy rich supplements improve muscle function and quality of life in malnourished patients with non-neoplastic gastrointestinal diseaseA randomized controlled trial. Clin Nutr 2008; 27: 4856. Potter J, Langhorne P, Roberts M. Routine protein energy supplementation in adults: systematic review. BMJ 1998; 317: 495501.
158 Lewis SJ, Egger M, Sylvester PA, Thomas S. Early enteral feeding versus nil by mouth after gastrointestinal surgery: a systematic review and meta-analysis of controlled trials. BMJ 2001; 323: 77376. 159 Braunschweig C, Levy P, Sheean P, Wang X. Enteral compared with parenteral nutrition: a meta-analysis. Am J Clin Nutr 2001; 74: 53442. 160 Sullivan D, Nelson C, Klimberg S, Bopp M. Nightly enteral nutrition support of elderly hip fracture patients: a pilot study. J Am Coll Nutr 2004; 23: 68391. 161 Hebuterne X, Vaillon F, Peroux J-L, Rampal P. Correction of malnutrition following gastrectomy with cyclic enteral nutrition. Dig Dis Sci 1999; 44: 187582. 162 Hebuterne X, Schneider S, Peroux J-L, Rampal P. Effects of refeeding by cyclic enteral nutrition on body composition: comparative study of elderly and younger patients. Clin Nutr 1997; 16: 2839. 163 Bermon S, Hebuterne X, Peroux J-L, Marconnet P, Rampal P. Correction of protein-energy malnutrition in older adults: effects of a short-term aerobic training program. Clin Nutr 1997; 16: 2918. 164 Bourdel-Marchasson I, Joseph P-A, Dehail P, et al. Functional and metabolic early changes in calf muscle occurring during nutritional repletion in malnourished elderly patients. Am J Clin Nutr 2001; 73: 8328. 165 Dehail P, Joseph P-A, Faux P, et al. Early changes in isokinetic lower limb muscle strength in recovering geriatric subjects on the basis of nutritional status. Journal of Nutrition, Health & Aging 2005; 9: 35663. 166 Fiatarone M, ONeill E, Ryan N, et al. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med 1994; 330: 176975. 167 Simpson F, Doig GS. Parenteral vs enteral nutrition in the critically ill patient: a meta-analysis of trials using the intention to treat principle. Intensive Care Med 2005; 31: 1223. 168 Hu S, Fontaine F, Kelly B, Bradford D. Nutritional depletion in staged spinal recontructive surgery: the effect of total parenteral nutrition. Spine 1998; 23: 14015. 169 Lapp M, Bridwell K, Lenke L, Baldus C, Blanke K, Iffrig T. Prospective randomization of parenteral hyperalimentation for long fusions with spinal deformity: it effect on complication and recovery from postoperative malnutrition. Spine 2001; 26: 80917. 170 Carbonnel F, Messing B, Rimbert A, Rongier M, Koziet J, Darmaun D. Energy and protein metabolism during recovery from malnutrition due to nonneoplastic gastrointestinal disease. Am J Clin Nutr 1997; 65: 151723. 171 Georgiannos S, Renaut A, Goode A. Short-term restorative nutrition in malnourished patients: pros and cons of intravenous and enteral alimentation using compositionally matched nutrients. Int Surg 1997; 82: 3016. 172 Eneroth M, Olsson U-B, Thorngren K-G. Insufcient uid and energy intake in hospitalised patients with hip fracture. A prospective randomised study of 80 patients. Clin Nutr 2005; 24: 297303. 173 Eneroth M, Apelqvist J, Larsson J, Persson B. Improved wound healing in transtibial amputees receiving supplementary nutrition. Int Orthop 1997; 21: 1048. 174 Fuenzalida C, Petty T, Jones M, et al. The immune response to short-term nutritional intervention in advanced chronic obstructive pulmonary disease. Am Rev Respir Dis 1990; 42: 4956.
S26
2009 The Author Journal compilation 2009 Dietitians Association of Australia
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
175 Christensson L, Ek A-C, Unosson M. Individually adjusted meals for older people with protein-energy malnutrition: a single case study. J Clin Nurs 2001; 10: 491502. 176 Russell CA. The impact of malnutrition on healthcare costs and the economic considerations for the use of oral nutritional supplements. Clinical Nutrition Supplments 2007; 2: 2532. 177 Beattie A, Prach A, Baxter J, Pennington C. A randomised controlled trial evaluating the use of enteral nutritional supplements postoperatively in malnourished surgical patients. Gut 2000; 46: 81318. 178 Oncology Nutrition Dietetic Practice group. The clinical guide to oncology nutrition, p4850 second edn. Elliot L, Molseed LL, Davis McCallum P (eds). Chicago: American Dietetic Association, 2006. 179 Stanga Z, Field J, Iff S, Stucki A, Lobo D, Allison S. The effect of nutritional management on the mood of malnourished patients. Clin Nutr 2007; 26: 37982. 180 Vivanti A, Ash S, Hulcombe J. Validation of a satisfaction survey for rural and urban outpatient dietetic services. J Hum Nutr Diet 2007; 20: 419. 181 National Patient Safety Agency. National Patient Safety Agency Protected Mealtimes Review ndings and recommendations report http://www.npsa.nhs.uk/EasysiteWeb/getresource.axd? AssetID=2654&type=full&servicetype=Attachment. 182 Hudson HM, Daubert CR, Mills RH. The interdependency of protein energy malnutrition, aging and dyspagia. Dysphagia 2000; 15: 318. 183 Wilson MM, Purushothaman R, Morley JE. Effect of liquid dietary supplements on energy intake in the elderly. Am J Clin Nutr 2002; 75: 9447. 184 Roberts M, Potter J, McColl J, Reilly J. Can prescription of sip-feed supplements increase energy intake in hospitalised older people with medical problems? Br J Nutr 2003; 90: 4259. 185 Simmons S, Walker K, Osterweil D. The effect of megestrol acetate on oral food and uid intake in nursing home residents: a pilot study. J Am Med Dir Assoc 2005; 6: S511. 186 Weisberg J, Wanger J, Olson J, et al. Megestrol Acetate stimulates weight gain and ventilation in underweight COPD patients. Chest 2002; 121: 10708. 187 Chu L-W, Lam K, Tam S, et al. A randomized controlled trial of low-dose recombinant human growth hormone in the treatment of malnourished elderly medical patients. The Journal of Clinical Endocrinology & Metabolism 2001; 86: 191320. 188 Ferreira I, Verreschi I, Nery L, et al. The inuence of 6 months or oral anabolic steroids on body mass and respiratory muscles in undernourished COPD patients. Chest 1998; 114: 1928. 189 Volkert D, Berner Y, Berry E, et al. ESPEN Guidelines on Enteral Nutrition: Geriatrics. Clin Nutr 2006; 25: 33060. 190 Greater Metropolitan Clinical Taskforce. Guidelines for Home Enteral Nutrition (HEN) Services. 2007; http://
191
192
193
194
195
196
197
198
199
200
201
202
203
www.health.nsw.gov.au/resources/gmct/hen/ hen_guidelines_2007_05_28_pdf.asp. Australasian Society of Parenteral and Enteral Nutrition. Clinical Practice Guidelines Home Enteral Nutrition in Australia. 2006; http://www.auspen.org.au/upload/HEN-Guidelines.doc. Dietitians Association of Australia Nutrition Support Interest Group (NSW Chapter). Enteral Feeding Manual for Adults in Health Care Facilities 2007; http://www.daa.asn.au/ index.asp?pageID=2145845151. Accessed 5 March 2008. The Australian Council of Healthcare Standards. The ACHS EQuIP 4 Guide: Part 1Accreditation, standards, guidelines. Standard 1: Clinical. Australian Council of Healthcare Standards, 2006. Banks M. Economic analysis of malnutrition and pressure ulcers in Qld public hospitals and residential aged care facilities. School of Public Health Brisbane: Queensland University of Technology, 2008. Stratton R, Longmore D, Elia M. Concurrent validity of a newly developed malnutrition universal screening tool (MUST). Clin Nutr 2003; 22: S10. King CL, Elia M, Stroud MA, Stratton R. The predictive validity of the malnutrition screening tool (MUST) with regard to morality and length of stay in elderly patients. Clin Nutr 2003; 22: S4. Kondrup J, Rasmussen HH, Hamberg O, Stanga Z. Nutritional Risk Screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 2003; 22: 32136. Cooper BA, Bartlett LH, Aslani A, Allen BJ, Ibels LS, Pollock CA. Validity of Subjective Global Assessment as a nutritional marker in end-stage renal disease. Am J Kidney Dis 2001; 40: 12632. Thoresen L, Fjeldstad I, Krogstad K, Kaasa S, Falkmer U. Nutritional status of patients with advanced cancer: the value of using the Subjective Global Assessment of nutritional status as a screening tool. Palliat Med 2002; 16: 3342. Ottery F. Patient-generated subject global assessment. In: McCallum P, Polisena C (eds). The clinical guide to oncology nutrition. Chicago: American Dietetic Association, 2005. Bauer J, Capra S, Ferguson M. Use of the scored PatientGenerated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. Eur J Clin Nutr 2002; 56: 77985. Desbrow B, Bauer J, Blum C, Kandasamy A, McDonald A, Montgomery K. Assessment of nutritional status in hemodialysis patients using patient-generated subjective global assessment. J Ren Nutr 2005; 15: 21116. Guigoz Y, Vellas B, Garry PJ. Mini nutritional assessment: A practical assessment tool for grading the nutritional state of elderly patients. Facts, Res Gerontol. 1994; 4: 1559.
2009 The Author Journal compilation 2009 Dietitians Association of Australia
S27
Nutrition & Dietetics 2009; 66 (Suppl. 3): S28S34
APPENDIX 1: SEARCH STRATEGY
The following tables outline the search terms used for the search of the Medline database using the OVID search engine. Search terms were then modied for the other databases searched, Embase and CINAHL.
Question 1. Criteria for referral for screening and referral systems:
What is the best method for identication of adults with malnutrition or at risk of malnutrition for improved patient, clinical and cost outcomes? # 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Search historyMedline exp *Malnutrition/ or malnutrition.mp undernutrition.mp risk adj2 malnutrition 1 or 2 or 3 *Risk Assessment/ or *Risk/ or *Risk Factors/ 5 and (malnutrition.ti,ab.) 4 or 6 *Mass Screening/or *Multiphasic screening Malnutrition screening tool.mp Mini Nutrition$ assessment Malnutrition Universal Screening Tool Nutrition$ risk screen$ *Referral and Consultation identif$.tw. 8 or 9 or 10 or 11 or 12 or 13 or 14 15 and 7 Limit 13 to (all adult (19 plus years) and humans and English) 17 not (editorial or tutorial or news or letter or comment).pt.
Question 2. Nutrition assessment and nutrition diagnosis:
Which specic measures best reect nutritional status or change in nutritional status in adults with malnutrition or at risk of malnutrition, for the diagnosis of malnutrition, can be altered by nutritional intervention and are associated with improved patient, clinical and cost outcomes? # 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 Search historyMedline exp *Malnutrition/ or malnutrition.mp undernutrition.mp risk adj2 malnutrition 1 or 2 or 3 nutritional status.mp or exp *Nutritional Status measure.mp or exp *(Weights and Measures) 5 and 6 Nutrition assessment. mp or exp *Nutrition Assessment 7 or 8 9 and 4 malnutrition adj3 diagnosis.mp. Malnutrition/di,pc 10 or 11 or 12 Subjective Global Assessment Full Nutrition$ Assessment Mini Nutrition$ Assessment Nutrition Risk 14 or 15 or 16 or 17 13 or 18 Limit 19 to (human and English language and all adult (19 plus years)) 20 not (editorial or news or tutorial or letter or comment).pt.
Search of MEDLINE, EMBASE and CINAHL databases from inception until August 2006 returned 1627 titles or abstracts.
Search of MEDLINE, EMBASE and CINAHL databases from inception until August 2006 returned 2025 titles or abstracts.
S28
2009 The Author. Journal compilation 2009 Dietitians Association of Australia
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
Question 3. Nutrition intervention (includes goals), nutrition monitoring and evaluation:
(a) What are the nutrition goals for adults with malnutrition or at risk of malnutrition for improved patient, clinical and cost outcomes? (b) In adults with malnutrition or at risk of malnutrition, what are the appropriate nutrition interventions, to optimise nutritional status for improved patient, clinical and cost outcomes? (c) In adults with malnutrition or at risk of malnutrition, how will nutrition interventions be monitored for improved patient, clinical and cost outcomes? # 1 2 3 4 5 6 7 8 9 10 1a 2a 3a 4a 5a 6a 7a 8a 9a Search history *Malnutrition/nu, dh, dt, pc, rh, th [Nursing, Diet Therapy, Drug Therapy, Prevention & Control, Rehabilitation, Therapy] Exp *Protein-Energy Malnutrition/nu, dh, dt, pc, rh, th [Nursing, Diet Therapy, Drug Therapy, Prevention & Control, Rehabilitation, Therapy] 1 or 2 3 and exp adult/ Limit 4 to (humans and english language) *Nutrition Disorders/ nu, dh, dt, pc, rh, th [Nursing, Diet Therapy, Drug Therapy, Prevention & Control, Rehabilitation, Therapy] 6 and (malnutrition or malnourish$ or undernourish$).tw. 7 and exp adult/ Limit 8 to (humans and English language) 5 or 9 Exclusions then added to this search included: Exp ascorbic acid deciency/ or exp vitamin a deciency/ or exp vitamin b deciency/ or exp vitamin d deciency/ or exp vitamin e deciency/ or exp vitamin k deciency/ Magnesium deciency/ or potassium deciency/ Exp liver diseases or cystic brosis/ Celiac disease Exp Eating Disorders/ Exp Kidney Diseases Renal replacement therapy/ or exp renal dialysis/ Or/1-7 Exp *ascorbic acid deciency/ or exp *vitamin a deciency/ or exp *vitamin b deciency/ or exp *vitamin d deciency/ or exp *vitamin e deciency/ or exp vitamin k deciency/ or (magnesium deciency/ or *potassium deciency/) or exp *Eating Disorders/ or exp *Kidney Diseases/ or (*renal replacement therapy/ or exp *renal dialysis) 10 NOT 8a
Search of MEDLINE, EMBASE and CINAHL databases from 1996 until August 2006 returned 335 titles or abstracts. The Cochrane Database of Systematic Reviews was searched using the term malnutrition to identify all relevant Cochrane reviewsthree identied.
2009 The Author. Journal compilation 2009 Dietitians Association of Australia
S29
Nutrition & Dietetics 2009; 66 (Suppl. 3): S28S34
S30 Diagnosis Prognosis Aetiology* Screening A systematic review of level II studies A prospective cohort study A systematic review of level II studies A prospective cohort study All or none A retrospective cohort study Pseudorandomised controlled trial (i.e. alternate allocation or some other method) A systematic review of level II studies A study of test accuracy with: an independent, blinded comparison with a valid reference standard, among consecutive patients with a dened clinical presentation A study of test accuracy with: an independent, blinded comparison with a valid reference standard, among non-consecutive patients with a dened clinical presentation A comparison with reference standard that does not meet the criteria required for level II and III-1 evidence Analysis of prognostic factors among untreated control patients in a randomised controlled trial A retrospective cohort study A casecontrol study Diagnostic casecontrol study A casecontrol study Study of diagnostic yield (no reference standard) Case series or cohort study of patients at different stages of disease A cross-sectional study A comparative study with concurrent controls: non-randomised experimental trial, cohort study, casecontrol study A comparative study without concurrent controls: historical control study, two or more single-arm study Case series
APPENDIX 2: NHMRC ADDITIONAL LEVELS OF EVIDENCE AND GRADES OF RECOMMENDATIONS FOR DEVELOPERS OF GUIDELINES PILOT PROGRAM 20051
Table 4 Evidence hierarchy
Intervention
II
A systematic review of level II studies A randomised controlled trial
A systematic review of level II studies A randomised controlled trial
III-1
Pseudo-randomised controlled trial (i.e. alternate allocation or some other method)
III-2
A comparative study without concurrent controls: non-randomised, experimental trial, cohort study, casecontrol study, interrupted time series with a control group
III-3
IV
A comparative study without concurrent controls: historical control study, two or more single-arm study, interrupted time series without a parallel control group Case series with either post-test or pretest/post-test outcomes
2009 The Author. Journal compilation 2009 Dietitians Association of Australia
* If it is only possible and/or ethical to determine a causal relationship using observational evidence, then the aetiology hierarchy of evidence should be used.
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
Table 5 NHMRCAssessing the body of evidence form Key question: (circle appropriate grade for each component) Evidence table ref:
1. Volume of evidence (quantity, level, methodological quality and relevance to patients of the body of evidence for this question, based on critical appraisal of each individual study according to Minimum Requirements) A Excellent (several level I or II studies with low risk of bias) B Good (one or two level II studies with low risk of bias or SR/multiple level III studies with low risk of bias) C Satisfactory (level III studies with low risk of bias or level I or II studies with moderate risk of bias) D Poor (level IV studies or level I to III studies with high risk of bias) 2. Consistency (the degree of consistency demonstrated by the available evidence. Where there are conicting results indicate how the group formed a judgement as to the overall direction of the evidence) A Excellent (all studies consistent) B Good (most studies consistent and inconsistency can be explained) C Satisfactory (some inconsistency, reecting genuine uncertainty around question) D Poor (evidence is inconsistent) 3. Clinical impact (the potential impact of recommendation, i.e. size of patient population, relevance of outcomes to the question, balance of risks and benets, relative benet over other management options, resource and organisational implications) A Excellent (very large clinical impact) B Good (substantial clinical impact) C Satisfactory (moderate clinical impact) D Poor (slight or restricted clinical impact) 4. Generalisability (how reasonable is it to generalise from the results of the studies used as evidence to the target population for this guideline?) A Excellent (directly generalisable to target population) B Good (directly generalisable to target population with some caveats) C Satisfactory (not directly generalisable to the target population but could be sensibly applied) D Poor (not directly generalisable to target population and hard to judge whether it is sensible to apply) 5. Applicability (the extent to which the body of evidence is directly applicable to Australian healthcare context) A Excellent (directly applicable to Australian healthcare context) B Good (applicable to Australian healthcare context with few caveats) C Satisfactory (probably applicable to Australian healthcare context with some caveats) D Poor (not applicable to Australian healthcare context)
2009 The Author. Journal compilation 2009 Dietitians Association of Australia
S31
APPENDIX 3: COMMON SCREENING AND ASSESSMENT TOOLS
Nutrition screening parameters When By whom Within 24 hours of admission and weekly during admission Medical, nursing, dietetic, administrative staff; family, friends, patients themselves Agreement by two dietitians in 22/23 (96%) cases, Kappa = 0.88 Agreement by a dietitian and nutrition assistant in 27/29 (93%) of cases Kappa = 0.84; and 31/32 (97%) of cases, Kappa = 0.93 Not reported Reliability Established Recent weight loss Recent poor intake Scores 01 for recent intake Scores 04 for recent weight loss Score 2 or more = at risk of malnutrition Criteria for risk of malnutrition
Nutrition & Dietetics 2009; 66 (Suppl. 3): S28S34
S32
Validity Established Recent intake Recent weight loss Mobility Recent psychological stress or acute disease Neuropsychological problems BMI Scores 03 for each parameter 11 at risk, continue with MNA On admission and regularly Not stated BMI Weight loss (%) Acute disease effect score Scores of 03 for each parameter based on cut-off values and predetermined acute disease effect Low risk, score 0 Medium risk, score 1 High risk, score 2 Scores 03 for each parameter based on cut-off values and predetermined severity of disease score If total score 3: start nutritional support Initial assessment and repeat regularly All staff able to use Compared with MNA and clinical nutritional status. Sensitivity = 97.9% Specicity = 100% Diagnostic accuracy = 98.7% Quoted to be internally consistent and reliable Very good to excellent reproducibility, Kappa = 0.81.0 Recent weight loss (%) Recent poor intake (%) BMI Severity of disease Elderly At admission and regularly during admission Medical and nursing staff Good agreement between a nurse, dietitian and physician, Kappa = 0.67
Table 6 Summary of most commonly referenced nutrition screening tools. Table adapted from Banks 2008194
Author year Country (Name)
Patient population
Ferguson et al. 199964 Australia (MST)
Acute adults
Compared with Subjective Global Assessment (SGA) and objective measures of nutrition assessment Patients classied at high risk had longer length of stay Sensitivity = 93% Specicity = 93%
Rubenstein et al. 200171 USA (MNA-SF)
Elderly
Malnutrition Advisory Group, 200367 UK (MUST)
Adultsacute and community
Face validity, content validity, concurrent validity with other screening tools (MST and NRS)195 Predicts risk of mortality and increased length of stay and discharge destination in acute patients196 Retrospective analysis of 128 RCTs of nutrition support. Patients fullling the risk criteria had a higher likelihood of a positive outcome from nutrition support Prospective study that showed a decreased length of stay among patient selected at risk by the screening tool, provided nutrition support
2009 The Author. Journal compilation 2009 Dietitians Association of Australia
Kondrup et al. 2003197 Denmark (NRS 2002)
Acute adult
Practice Guidelines for the Nutritional Management of Malnutrition in Adult Patients Across the Continuum of Care
Table 7 Summary of the most commonly used nutrition assessment tools. Table adapted from Banks 2008194 Name Author, year SGA Subjective Global Assessment91 Setting and patient population Setting: Acute91,198,199 Rehab104 Community107 Residential aged care Patient group: Surgery91 Geriatric48,95,104,107 Oncology199 Renal198 Setting: Acute103,201,202 Patient group: Oncology201 Renal202 Stroke103 Nutrition assessment parameters Includes medical history (weight, intake, GI symptoms, functional capacity) and physical examination Categorises patients as: SGA A (well nourished) SGA B (mildmoderate malnutrition) or SGA C (severe malnutrition) Includes medical history (weight, intake, symptoms, functional capacity, metabolic demand) and physical examination Categorises patients into SGA categories (A, B or C) as well as providing a numerical score for triaging Includes: Screening: 6 questions Assessment: 18 questions Includes diet history, anthropometry, medical and functional status Assessed based on numerical score as: no nutritional risk at risk of malnutrition or malnourished Rationale/ Clarication Requires training Easy to administer Good intra- and interrater reliability
PG-SGA Patent Generated Subjective Global Assessment200
MNA Mini-Nutritional Assessment203
Setting: Acute Community Rehab Long-term care Patient group: Geriatric203
Numerical score assists in monitoring improvements in nutritional status Easy to administer Scoring can be confusing but this can be addressed through training Patients can complete the rst half of the tool Lengthy Low specicity for screening section of tool Can be difcult to obtain anthropometric data in this patient group MNA website: http:// www.mna-elderly.com MNA CD (available through Nestle)
2009 The Author. Journal compilation 2009 Dietitians Association of Australia
S33
Nutrition & Dietetics 2009; 66 (Suppl. 3): S28S34
APPENDIX 4: TABULAR LISTS OF DISEASES (ICD-10-AM SIXTH EDITION) Malnutrition (E40E46)
Note
The degree of malnutrition is usually measured in terms of weight, expressed in standard deviations from the mean of the relevant reference population. In children, when one or more previous measurements are available, lack of weight gain or evidence of weight loss is usually indicative of malnutrition. When only one measurement is available, the diagnosis is based on probabilities and is not denitive without other clinical or laboratory tests. In the exceptional circumstances that no measurement of weight is available, reliance should be placed on clinical evidence. In adults, malnutrition includes weight loss of at least 5%, with evidence of suboptimal intake resulting in subcutaneous fat loss and/or muscle wasting. If an observed weight is below the mean value of the reference population, there is a high probability of severe malnutrition if there is an observed value situated three or more standard deviations below the mean value of the reference population; a high probability of moderate malnutrition for an observed value located between two and less than three standard deviations below this mean; and a high probability of mild malnutrition for an observed value located between one and less than two standard deviations below this mean.
standard deviations below the mean value for the reference population (or a similar loss expressed through other statistical approaches). When only one measurement is available, there is a high probability of severe wasting when the observed weight is three or more standard deviations below the mean of the reference population. In adults, BMI < 18.5 kg/m2 or unintentional loss of weight ( 10%) with evidence of suboptimal intake resulting in severe loss of subcutaneous fat and/or severe muscle wasting. Starvation oedema
E44 Protein-energy malnutrition of moderate and mild degree
E44.0 Moderate protein-energy malnutrition
In children, weight loss or lack of weight gain leading to an observed weight that is two or more but less than three standard deviations below the mean value for the reference population (or a similar loss expressed through other statistical approaches). When only one measurement is available, there is a high probability of moderate protein-energy malnutrition when the observed weight is two or more but less than three standard deviations below the mean of the reference population. In adults, BMI < 18.5 kg/m2 or unintentional loss of weight (59%) with evidence of suboptimal intake resulting in moderate loss of subcutaneous fat and/or moderate muscle wasting.
Excludes
Intestinal malabsorption (K90.-) Nutritional anaemias (D50D53) Sequelae of protein-energy malnutrition (E64.0) Starvation (T73.0)
E44.1 Mild protein-energy malnutrition
In children, weight loss or lack of weight gain leading to an observed weight that is one or more but less than two standard deviations below the mean value for the reference population (or a similar loss expressed through other statistical approaches). When only one measurement is available, there is a high probability of mild protein-energy malnutrition when the observed weight is one or more but less than two standard deviations below the mean of the reference population. In adults, BMI < 18.5 kg/m2 or unintentional loss of weight (59%) with evidence of suboptimal intake resulting in mild loss of subcutaneous fat and/or mild muscle wasting.
E40 Kwashiorkor
Severe malnutrition with nutritional oedema with dyspigmentation of skin and hair Excludes: marasmic kwashiorkor (E42)
E41 Nutritional marasmus
Severe malnutrition with marasmus Excludes: marasmic kwashiorkor (E42)
E42 Marasmic kwashiorkor
Severe protein-energy malnutrition (as in E43): Intermediate form With signs of both kwashiorkor and marasmus
E45 Retarded development following protein-energy malnutrition
Nutritional: Short stature Stunting Physical retardation due to malnutrition.
E43 Unspecied severe protein-energy malnutrition
In children, severe loss of weight (wasting) or lack of weight gain leading to an observed weight that is at least three
S34
2009 The Author. Journal compilation 2009 Dietitians Association of Australia
Copyright of Nutrition & Dietetics is the property of Blackwell Publishing Limited and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
Você também pode gostar
- Out 6Documento9 páginasOut 6firdakusumaputriAinda não há avaliações
- Firdha Kusuma Putri - 220110110146Documento1 páginaFirdha Kusuma Putri - 220110110146firdakusumaputriAinda não há avaliações
- Ketentuan Group Study VisitDocumento5 páginasKetentuan Group Study VisitfirdakusumaputriAinda não há avaliações
- 1interventions To Reduce Postpartum Stress in First-Time Mothers A Randomized-Controlled TrialDocumento9 páginas1interventions To Reduce Postpartum Stress in First-Time Mothers A Randomized-Controlled TrialfirdakusumaputriAinda não há avaliações
- Hhka ChudecDocumento1 páginaHhka ChudecfirdakusumaputriAinda não há avaliações
- 59403223Documento5 páginas59403223firdakusumaputriAinda não há avaliações
- Ketentuan Group Study VisitDocumento5 páginasKetentuan Group Study VisitfirdakusumaputriAinda não há avaliações
- 66325997Documento5 páginas66325997firdakusumaputriAinda não há avaliações
- Medical ErrorDocumento9 páginasMedical ErrorfirdakusumaputriAinda não há avaliações
- Hospital Diagnosis of Malnutrition:: A Call For ActionDocumento6 páginasHospital Diagnosis of Malnutrition:: A Call For ActionfirdakusumaputriAinda não há avaliações
- 7 Information&Communication Technology For Supporting People With Serious Chronic DiseaseDocumento8 páginas7 Information&Communication Technology For Supporting People With Serious Chronic DiseasefirdakusumaputriAinda não há avaliações
- Suspected Appendicitis in Pregnant PatientsDocumento8 páginasSuspected Appendicitis in Pregnant PatientsfirdakusumaputriAinda não há avaliações
- 64720579Documento12 páginas64720579firdakusumaputriAinda não há avaliações
- Training Nurses To Save Lives of Malnourished Children: Research ArticleDocumento7 páginasTraining Nurses To Save Lives of Malnourished Children: Research ArticlefirdakusumaputriAinda não há avaliações
- Bagus Tapi 2005Documento9 páginasBagus Tapi 2005firdakusumaputriAinda não há avaliações
- 64720579Documento12 páginas64720579firdakusumaputriAinda não há avaliações
- Structural and Ultra-Structural Features of The First Mandibular Molars of Young Rats Submitted To Pre and Postnatal Protein DeficienciesDocumento8 páginasStructural and Ultra-Structural Features of The First Mandibular Molars of Young Rats Submitted To Pre and Postnatal Protein DeficienciesfirdakusumaputriAinda não há avaliações
- Diare Pada Kwashiorkor - NewDocumento8 páginasDiare Pada Kwashiorkor - NewfirdakusumaputriAinda não há avaliações
- Undernutrition in Older AdultsDocumento7 páginasUndernutrition in Older Adultsfirdakusumaputri100% (1)
- Protein-Calorie Malnutrition Legal RiskDocumento6 páginasProtein-Calorie Malnutrition Legal RiskfirdakusumaputriAinda não há avaliações
- Siblings With Hepatosplenomegaly and Lipoprotein Lipase DeficiencyDocumento2 páginasSiblings With Hepatosplenomegaly and Lipoprotein Lipase DeficiencyfirdakusumaputriAinda não há avaliações
- Diare Pada KwashiorkorDocumento5 páginasDiare Pada KwashiorkorfirdakusumaputriAinda não há avaliações
- UFD3UXDocumento7 páginasUFD3UXfirdakusumaputriAinda não há avaliações
- Rehab Therapy Services For Stroke PatientsDocumento6 páginasRehab Therapy Services For Stroke Patientsfirdakusumaputri100% (1)
- Rehabilitation StrokeDocumento3 páginasRehabilitation StrokefirdakusumaputriAinda não há avaliações
- AAV ID 2012 0437583 UFD3UX Nurina RachmantiDocumento1 páginaAAV ID 2012 0437583 UFD3UX Nurina RachmantifirdakusumaputriAinda não há avaliações
- AAV ID 2012 0437583 UFD3UX Billy NoviansyahDocumento1 páginaAAV ID 2012 0437583 UFD3UX Billy NoviansyahfirdakusumaputriAinda não há avaliações
- Jazzy Love Songs CollectionDocumento2 páginasJazzy Love Songs CollectionfirdakusumaputriAinda não há avaliações
- Sharing Nutrition StatusDocumento17 páginasSharing Nutrition StatusfirdakusumaputriAinda não há avaliações
- What is BMI for Children and TeensDocumento7 páginasWhat is BMI for Children and Teensprita_camellaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Detailed Lesson Plan in Technology and Livelihood Education IDocumento8 páginasDetailed Lesson Plan in Technology and Livelihood Education IJuana Arapan ArvesuAinda não há avaliações
- Community Based Nutrition CMNPDocumento38 páginasCommunity Based Nutrition CMNPHamid Wafa100% (4)
- GF670 Desertification Successful MGMT in The SahelDocumento4 páginasGF670 Desertification Successful MGMT in The SahelThaddeus NgAinda não há avaliações
- Research - BLT Feeding Program - FinalDocumento20 páginasResearch - BLT Feeding Program - FinalRed Senoc67% (3)
- 10 - Annual Report 2018-2019Documento9 páginas10 - Annual Report 2018-2019pubg xenziaAinda não há avaliações
- Thank you for the role play. I hope Mrs. Citra can improve her nutrition and getbetter soon. Have a nice day everyoneDocumento5 páginasThank you for the role play. I hope Mrs. Citra can improve her nutrition and getbetter soon. Have a nice day everyoneHafidhotul IlmillahAinda não há avaliações
- The Relationship Between Dietary Patterns and Nutritional Knowledge With The Nutritional Status of Bajo Tribe Pregnant Women in Duruka District, Muna RegencyDocumento5 páginasThe Relationship Between Dietary Patterns and Nutritional Knowledge With The Nutritional Status of Bajo Tribe Pregnant Women in Duruka District, Muna RegencytreesAinda não há avaliações
- Nutritional Practices HandoutDocumento2 páginasNutritional Practices Handoutapi-530144731Ainda não há avaliações
- Sydney M PRPDocumento23 páginasSydney M PRPapi-465406877Ainda não há avaliações
- Hospital Food Service (Rosario Walton 2019)Documento28 páginasHospital Food Service (Rosario Walton 2019)Gizi Kesehatan UGM 2017Ainda não há avaliações
- BNAP TemplateDocumento55 páginasBNAP TemplateLee Ecaldre100% (1)
- Cbse Class IX English Language and Literature Sample Paper - 2 SAIDocumento7 páginasCbse Class IX English Language and Literature Sample Paper - 2 SAIFufkAinda não há avaliações
- GE 3 Chapter 6 Lesson 2 Global Food SecurityDocumento20 páginasGE 3 Chapter 6 Lesson 2 Global Food Securityjuliet maeAinda não há avaliações
- Situational Analysis of Children in The Philippines PDFDocumento376 páginasSituational Analysis of Children in The Philippines PDFRheii EstandarteAinda não há avaliações
- New Microsoft Office Word DocumentDocumento7 páginasNew Microsoft Office Word DocumentSumati PanchalAinda não há avaliações
- 2015 UNSLCD - Plan of ActionDocumento19 páginas2015 UNSLCD - Plan of ActionRaponcel AbuegAinda não há avaliações
- Food For ThoughtDocumento12 páginasFood For ThoughtcomputeraidAinda não há avaliações
- Ending Hunger by 2030 - Policy Actions and CostsDocumento8 páginasEnding Hunger by 2030 - Policy Actions and CostsToyanath JoshiAinda não há avaliações
- J Americ Oil Chem Soc - 2018 - Di Stefano - Plant RuBisCo An Underutilized Protein For Food ApplicationsDocumento12 páginasJ Americ Oil Chem Soc - 2018 - Di Stefano - Plant RuBisCo An Underutilized Protein For Food ApplicationsYashaswini BalrajuAinda não há avaliações
- Acceptability and Use of Cereal-Based Foods in Refugee Camps: Case-Studies From Nepal, Ethiopia, and TanzaniaDocumento137 páginasAcceptability and Use of Cereal-Based Foods in Refugee Camps: Case-Studies From Nepal, Ethiopia, and TanzaniaOxfamAinda não há avaliações
- Nutrition Program EndorsementDocumento2 páginasNutrition Program EndorsementLouwella RamosAinda não há avaliações
- Wa0046Documento99 páginasWa0046john mwambuAinda não há avaliações
- Rangkuman Ujian Sempro Dalam Bahasa InggrisDocumento9 páginasRangkuman Ujian Sempro Dalam Bahasa InggrisdesyAinda não há avaliações
- Local Development Plan For Children SampleDocumento16 páginasLocal Development Plan For Children SampleArman Bentain100% (14)
- Invisible City MakersDocumento98 páginasInvisible City MakersBiswajit DarbarAinda não há avaliações
- Becoming Vegan by Brenda DavisDocumento283 páginasBecoming Vegan by Brenda DavisLora Diaconu70% (10)
- 019-2020 BF1KD-01Documento2 páginas019-2020 BF1KD-01barangaybingay100% (1)
- UNICEF Report: Children in Pakistan - Six Months After The FloodDocumento18 páginasUNICEF Report: Children in Pakistan - Six Months After The FloodUNICEF0% (1)
- Leaf Protein ManualDocumento362 páginasLeaf Protein ManualMatisAinda não há avaliações