Escolar Documentos
Profissional Documentos
Cultura Documentos
8 Heart Failure - Notes-DONE - Printed
Enviado por
Kristin SmithDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
8 Heart Failure - Notes-DONE - Printed
Enviado por
Kristin SmithDireitos autorais:
Formatos disponíveis
Kristin Hinkle
NSC 386
Heart Failure
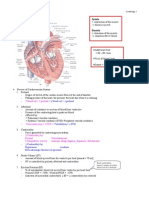
Heart Failure NSC 386 What is Heart Failure? Heart cannot pump blood to the body. Not a disease- lifelong process that must be manages; lifestyle changes etc. Pts. can be diagnosed chronic heart failure with acute exasperations (attacks) Inability of the heart to pump and/or fill Leads to: CO Inadequate tissue perfusion Impaired organ function Associated with: CAD and HTN After a MI- from muscle damage Valvular disease A lot go into renal & hepatic failure Atrial fibrillation- lose kick=stasis- working harder but not as effectively so it can lead to heart failure. (A fib can cause or be caused by HF) Heart Failure- Major Health Problem Most common reason for hospital admission in adults >65 y/o- rates of re-admission to hospital is . @ are re-admitted within 6 months! Economic burden In-hospital mean LOS= 6.5 days spend in hospital HF has a poor prognosis- @ 1/3 of diagnosed HF pts. will die within 1 year of diagnosis! Etiology of Heart Failure Risk Factors: CAD (#1 most common cause), advanced age, HTN, DM, cigarette smoking, obesity Heart Failure is caused by an interference with CO CO depends on: 1. Preload (volume) 2. Afterload (pressure/resistance) 3. Stroke volume 4. Heart rate Pathophysiology of Heart Failure 1. Systolic Failure: more common PUMP problem Caused by impaired contractility or increased afterload Hallmark of systolic failure= low ejection fraction (EF) Normal EF = 55-65% EF with heart failure < 40% EF is % of blood is ejected from heart with each cardiac contraction Ejection Fraction-(photo)- can be determined from echocardiogram; Heart failure is a structural problem with the heart so it cant pump as well= its EF Ejection Fraction Video
Formatted: Font: Not Bold
Formatted
Formatted: Numbered + Level: 1 + Numbering Style: 1, 2, 3, + Start at: 1 + Alignment: Left + Aligned at: 0.75" + Indent at: 1"
Formatted: Font: Bold
Formatted
Kristin Hinkle
NSC 386
Heart Failure
Pathophysiology of Heart Failure cont 2. Diastolic Failure- less common FILLING problem-ventricles cannot relax enough to fill Caused by chronic HTN (left ventricular hypertrophy) or cardiomyopathy Results in: SV and CO Will see a backup of blood in the pulmonary and systemic systems 3. Mixed Systolic and Diastolic Failure- very poor quality of life A PUMPING and FILLING problem Will see biventricular failure- both right and left are effected- cant pump or fill properly EF will be very low and BP will be low usually < 35% Often seen with cardiomyopathy Heart Failure- Compensatory Mechanisms In order to compensate for the decrease in CO associated with heart failure, we will see 1. Ventricular dilation 2. Ventricular hypertrophy 3. Activation of the SNS 4. Neurohormonal responses Heart Failure- Compensatory Mechanisms 1. Ventricular Dilation usually in left ventricle Result of high pressures in the heart over time Muscle fibers stretch to increase contractile force Over time, muscle fibers become overstretched = Poor contractility (think Starlings lawonce its overstretched, overtime it looses its stretch Heart Failure- Compensatory Mechanisms (cont.) 2. Ventricular Hypertrophy - increase in cardiac wall thickness- muscle gets bigger from working so hard then its not as effective - usually follows chronic dilation - initially, will see, improved CO but over time, CO will decrease Heart Failure- Compensatory Mechanisms (cont.) 3. Activation of the SNS 1st mechanism activated, but least effective - Epinephrine and Norepinephrine released = - see, vasoconstriction which increases the SVR (systemic vascular resistance)(afterload) - leads to an increased workload on the heart Heart Failure- Compensatory Mechanisms (cont.) 4. Neurohormal Response -kidneys Renin- Angiotensin- Aldosterone System (RAAS) CO to kidneys = kidneys release renin = conversion of angiotensin I to angiotensin II (a potent vasoconstrictor) ( afterload) = release of aldosterone = Na++ and H2O retention ( preload) = fluid overload less blood to kidneys- they try to compensate by fluid volume to BP Heart Failure- Compensatory Mechanisms (cont.) 2
Formatted: No bullets or numbering Formatted: Font: Bold
Formatted: Font: Bold
Formatted: Font: Bold Formatted: Font: Bold
Formatted: Font: Bold
Formatted: Font: Bold Formatted: Superscript
Formatted: Font: Bold
Kristin Hinkle
NSC 386
Heart Failure
4. Neurohormonal Response (cont.) Release of ADH (due to decrease in cerebral perfusion pressure)-body holds on to fluids Leads to an increase in H2O reabsorption = Preload Compensatory responses are more damaging overtime, making an already damaged heart work even harder Ventricular Remodeling result of compensatory mechanisms Because of: Hypertrophy of ventricles = EF Large, spherical chambers Often seen in the left ventricle- enlarged- starts to look like a football! Less effective pump! Ventricular remodeling is a risk factor for ventricular dysrhythmias & sudden cardiac death Heart Failure- Counter Regulatory Mechanisms Brain Natriuretic Pepide (BNP) Produced by the heart Secreted in response to increased pressure in the ventricles Leads to: 1. vasodilation- to combat afterload 2. diuresis & naturesis excreting extra sodium(helps with preload ) 3. Blockage of the RAAS- Renin-Angiotensin Aldosterone System- blockage that preload and afterload Types of Heart Failure Left-sided Heart Failure will see respiratory problems; more common than right pressure means heart has to work harder Caused by: Left ventricular dysfunction Backup of blood into the L atrium-then backs up into the lungs S/S: pulmonary edema and congestion- fluid moves into alveolar spaces; symptoms become more severe with more fluid accumulation SOA Wheezing Crackles Moist cough Cyanosis Chest Congestion-photo white in the xray, is fluid in the lungs
Formatted: Font: Not Bold
Formatted: Font: Bold
Formatted: Font: Bold
Formatted: List Paragraph, Bulleted + Level: 1 + Aligned at: 1.5" + Indent at: 1.75"
Normal Chest X-ray:
Pulmonary Congestion:
Types of Heart Failure (cont.) 3
Kristin Hinkle
NSC 386
Heart Failure
Formatted: Font: Bold
Right-sided Heart Failure- common in COPD pts. Caused by: Right ventricular dysfunction Backup of blood into R atrium Often a result of left- sided HF or cor pulmonale (result of pulmonary disease) S/S: systemic edema 1. JVD 2. Peripheral edema 3. Vascular congestion of GI tract (ascites) 4. Hepatomegaly enlarged liver ( liver enzymes)
Jugular Venous Distention-photo
Peripheral Edema- photo
pitting edema
Ascites- photo Right vs. Left Sided Heart Failure Right Sided HF R ventricle pump failure = back-up congestion in peripheral tissue & organs Increased venous pressure = JVD, peripheral edema, ascites, hepatomegaly Left Sided HF L ventricle pump failure = back-up congestion in lungs Increased pulmonary pressure = fluid forced from pulmonary capillaries into pulmonary tissues and alveoli = pulmonary edema Acute Decompensated Heart Failure probably have a Dx of HF; may have eaten a salty meal Due to acute L ventricular failure Manifests as: pulmonary edema- alveoli become flooded in bases of lungs Acute Decompensated Heart Failure requires immediate action! Signs and Symptoms: Anxious & restless Pale- may have cyanotic nail beds Cool, clammy skin from CNS vasoconstriction Severe dyspnea RR > 30 breaths/min Wheezing, crackles, or rhonchi Cough with frothy, pink sputum- BAD sign! ABGs: low PaO2 and high PaCO2- bad gas exchange- alveoli cant exchange so they cant get rid of CO2 or get in O2= respiratory acidosis Chronic Heart Failure 4
Formatted: Font: Not Bold
Formatted: Font: Not Bold
Kristin Hinkle
NSC 386
Heart Failure
Formatted: Underline
Progressive worsening of ventricular function Often see symptoms of biventricular failure (left & right failure) Acronym FACES Fatigue Limitation of Activities Chest Congestion Edema Shortness of breath Chronic Heart Failure Symptoms 1. Fatigue- due to a decrease in oxygen to the tissues, tired all the time; dont sleep well; one of the earliest signs of heart failure 2. Dyspnea- seen with mild exertion, but as it progresses, it can be seen while lying in bed Orthropnea- SOA when pt. lies down; a lot will sleep with many pillows Paroxysmal Nocturnal Dyspnea (PND)- result of reabsorption of fluid when the pt. is lying down; wake up with a panicky drowning feeling Pre-load goes at night because they are lying down 3. Tachycardia- early onset symptom of HF; from reduced cardiac output 4. EdemaR-sided = peripheral edema, hepatomegaly, ascites L-sided = pulmonary edema 5. Nocturia- when pt. lies down Fluid reabsorption when pt. lies down = renal blood flow= diuresis 6. Skin Changes- r/t poor oxygenation in tissues; dusky appearance, cool & damp lower extremities: shiny & swollen, brownish pigment 7. Behavioral Changes- restless, confused, anxiety 8. Chest Pain- typically relieved by Nitroglycerin 9. Weight changes- initial weight gain from fluid; later, may see a loss- from not eating well-may still look big from the edema Complications of Heart Failure Renal Failure Decrease in renal perfusion BUN & Creatinine, Urine output Left Ventricular Thrombus- stasis of blood in Lt. ventricle Enlarged LV and decreased CO= higher risk for thrombus formations Pleural Effusion (collection of fluid) Fluid accumulation in pleural space- drain them or diuresis them Complications of Heart Failure (cont.) Dysrhythmias Result of stretching of the heart chambers
Formatted
Formatted
Often see- Atrial fibrillation- seen in 1/3 of pts. with heart failure Hepatomegaly- seen with RV failure; leads to impaired liver function- see changes in liver enzymes American Heart Association Stages of Heart Failure 5
Kristin Hinkle
NSC 386
Heart Failure
Stage A Pt. at high risk for HF, but no symptoms or structural changes of the heart -Treatment: lifestyle changes Stage B Pt. has structural heart disease, but has not shown symptoms Treatment: lifestyle changes, possible meds Stage C Pt. has prior or current symptoms of HF along with underlying structural heart disease Treatment: lifestyle changes, possible meds, possible ICD Stage D Pt. has refractory (treatment doesnt work) HF and needs specialized interventions (Treatment: same measures as above, plus end of life care, heart transplant, experimental drugs) Diagnostic Studies Goal= determine the underlying cause- lung disease? CAD? History and Physical- do they have HTN, CAP, Rt or Lt. side failure? Chest X-ray- look for white out; pulmonary congestion; cardiomyopathy Echocardiogram Will see a low ejection fraction (EF) <40% Normal EF = 55-65% BNP (nml = 0-100 pg/mL) BNP 100-500 pg/mL= HF probable BNP >500 pg/mL= HF highly probable Chronic BNP levels = around 550 pg/ml Acute BNP levels = 1500+ pg/ml Nursing Care in Acute Decompensated Heart Failure (ADHF) Case Study - Mr. Miller, age 74, presents to the ED today with acute onset of dyspnea. Crackles are audible throughout both lung fields and his O2 sat is 88% on RA. Hi wife mentioned that he has been c/o increasing SOB over the past few days, inability to sleep at night (he uses 2 pillows), getting up numerous times a night to urinate, his socks are too tight and he can only wear his house shoes. Symptoms: peripheral edema (rt side), crackles (lt. side), Biventricular HF?, urinating frequently at night, sleeping with 2 pillows, O2 -88% Priority: get O2 up! What is his position? Is he lying down? Sit him Up! Give oxygen, get labs- BNP, ABG, Creatinine- get before diuresing, get fluid off. Medical Hx- previous Dx? Compliant with meds? Lifestyle compliance? What has he been eating or drinking? Nursing Care in Acute Decompensated Heart Failure (ADHF) This is Mr. Millers 3rd admission in the past 6 months. He lives with his wife who has beginning stages of dementia. He states he often forgets to take his medicine. He and his wife eat lots of frozen dinners. He c/o fatigue during the day and has difficulty walking to his driveway to get his daily newspaper. He has gained 12 pounds since his last admission 2 months ago. Acute Heart Failure- Collaborative and Nursing Care (cont.) 6
Formatted: Underline
Formatted: Underline
Formatted: Underline
Formatted: Underline
Formatted: Underline Formatted: Underline Formatted: Underline Formatted: Underline Formatted: Underline Formatted: Underline
Kristin Hinkle
NSC 386
Heart Failure
Formatted: Underline Formatted
Improve Gas Exchange and Oxygenation- TOP PRIORITY 1. High fowlers position- 90* 2. Supplemental oxygen- start with NC, 2-4L 3. Morphone0 decrease anxiety= decreased O2 demand, so RR, overall workload of heart and lungs Acute Heart Failure- Collaborative and Nursing Care (cont.) Decrease Intravascular Volume/ Reduce Preload fluid volume 1. High Fowlers position with legs dangling or horizontal in bed 2. Loop Diuretics (Lasix) given IV- rapid acting nsg: watch K+ levels, monitor I&O, auscultate breath sounds, check pt. weight 3. Vasodilators (Nitroglycerin- NTG) Nsg: watch for hypotension- check every 15 minutes Acute Heart Failure- Collaborative and Nursing Care (cont.) Decrease Afterload NTG Nipride (STRONG vasodilator) given in ICU Improved cardiac contraction= CO and pulmonary congestion Nsg: watch for hypotension, thiocynate toxicity Nesiritide (Natercor)- synthetic BNP Arterial and venous vasodilator Provides diuresis and sodium excretion Nsg: must be on an IV pump, watch for hypotension ACE Inhibitors: -pril blocks RAAS- Renin-Angiotensin Aldosterone System (keeps this from retaining fluids) Acute Heart Failure- Collaborative and Nursing Care (cont.) Improve Cardiac Function Inotropic Therapy- if pt. has NOT responded to vasiodialators or diuretics For SHORT TERM management of acute HF Increases myocardial contractility Digoxin- PO, IV push Dobutamine continuous IV infusion Nursing Care in Chronic Heart Failure Mr. Miller loses 18 pounds while in the hospital. He states he can breathe much easier now, his regular shoes fit comfortably, and he is ready for DC home. Educate: meds, diet, lifestyle changes Core/Performance (minimum standards) Measures for Heart Failure These measures must be documented with every admission: 1. Left Ventricular Function Assessment Ejection Fraction-from echocardiogram 2. ACE Inhibitor or ARB (Angiotensin Receptor Blocker) for EF <40% 3. Discharge Instructions: 1. Activity level 2. Diet / fluid intake 3. Actions when symptoms worsen 7
Formatted: Underline
Formatted
Formatted Formatted: Underline Formatted: Font: Bold
Formatted: Font: Bold Formatted: Font: Bold
Formatted: Font: Bold Formatted: Indent: First line: 0.5", No bullets or numbering Formatted: Indent: Left: 0", Hanging: 1", No bullets or numbering Formatted: Underline Formatted
Formatted Formatted: Underline
Kristin Hinkle
NSC 386
Heart Failure
4. Daily weights 5. Follow up appointments 6. Medications Chronic Heart Failure- Collaborative and Nursing Care Goals for treatment of Chronic HF: 1. Treat the underlying cause 2. Maximize CO 3. Symptom management 4. Improve quality of life and decrease mortality rates 5. Preserve target organ function Chronic Heart Failure- Collaborative and Nursing Care (cont.) Oxygen Therapy Activity Balance of rest and activity For stable chronic HF- Stage A & B pts.- start slowly, then increase a few minutes each day (like 5 min/day of walking) Teach pts. how to check their HR and RR Chronic Heart Failure- Collaborative and Nursing Care (cont.) Drug Therapy Diuretics Thiazide diuretics preferred for chronic HF Lasix for acute ACE Inhibitors Block the RAAS system Vasodilators- nitrates For patients who can not tolerate ACE Inhibitors Chronic Heart Failure- Collaborative and Nursing Care (cont.) Nutritional Therapy 2-4g is normal recommendation (healthy) Sodium restriction- Americans average @ 7-15g/day Should be limited to < 2g per day Avoid canned or processed foods Encourage fresh fruits and vegetables No table salt! Fluid Restriction For patients with Class C & D Heart Failure Should be < 2 liters per day Give ice, gum, lemon flavored things, hard candy to help with thirst Chronic Heart Failure- Collaborative and Nursing Care (cont.) Daily Weights/Monitor Fluid Balance How do we teach our patients to weigh themselves? Same time, same clothing, same scale, morning is best before breakfast Weight gain of 3 lbs over 2 days or 3-5 lbs over a week = contact MD in weight is an earlier indication of fluid retention than edema How do we assess fluid balance? 1. Ankle swelling 2. Abdominal swelling 3. Orthopnea- SOA when lying flat 8
Formatted: Underline
Formatted: Font: Bold
Formatted: Numbered + Level: 1 + Numbering Style: 1, 2, 3, + Start at: 1 + Alignment: Left + Aligned at: 1.25" + Indent at: 1.5"
Kristin Hinkle
NSC 386
Heart Failure
4. Paroxysmal Nocturnal Dyspnea 5. Weight Gain Chronic Heart Failure- Collaborative and Nursing Care (cont.) Limit Alcohol/ Smoking Cessation Avoid Herbal Therapy and NSAIDS (ibuprofen, Alieve, Motrin) can lead to sodium and water retension Education about s/s of Acute Decompensation- SOA, swelling Chronic Heart Failure- Collaborative and Nursing Care (cont.) Address Psychosocial Issues Depression- high rates Stress/Anxiety Sexual Dysfunction Class A & B can use Viagra (as long as not on nitrates), Class C & D cannot Nursing Diagnoses for Chronic Heart Failure Activity intolerance r/t fatigue Excess fluid volume r/t cardiac dysfunction Impaired gas exchange e/t alveolar-capillary membrane changes Anxiety r/t dyspnea & fear of death Decreased cardiac output r/t altered contractility & stroke volume Knowledge deficit r/t . Advanced/End Stage Heart Failure- Class D Biventricular Pacing Coordinates R and L ventricular contractility, which improves LV function and CO Implantable Cardioverter Defibrillator- for ventricular dysrhythmias Cardiac Transplantation
Formatted: Underline
Formatted: List Paragraph, Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
Formatted: Font: Not Bold
Você também pode gostar
- Cardiology NotesDocumento13 páginasCardiology NotesFreeNursingNotes78% (9)
- Cardiac Meds ChartDocumento1 páginaCardiac Meds ChartCharlotte Louise75% (4)
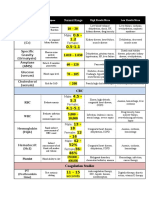
- Lab ValuesDocumento3 páginasLab Valuessurviving nursing school100% (1)
- Dysrhythmias Cheat SheetDocumento2 páginasDysrhythmias Cheat SheetKatie Coughlan100% (2)
- Cardiac DrugsDocumento35 páginasCardiac DrugsCristina Centurion100% (3)
- Hyperkalemia and HypokalemiaDocumento37 páginasHyperkalemia and HypokalemiaDiena AshlihatiAinda não há avaliações
- Physical Exam SheetDocumento6 páginasPhysical Exam SheetDidi SaputraAinda não há avaliações
- Cardiology Study Guide Handout PDFDocumento86 páginasCardiology Study Guide Handout PDFStarr Newman100% (1)
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsNo EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsAinda não há avaliações
- Pathophysiology of Heart Failure With Reduced Ejection Fraction - Hemodynamic Alterations and Remodeling - UpToDateDocumento29 páginasPathophysiology of Heart Failure With Reduced Ejection Fraction - Hemodynamic Alterations and Remodeling - UpToDatesamAinda não há avaliações
- Heart FailureDocumento108 páginasHeart FailureDeasy Rizka Rahmawati100% (1)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsAinda não há avaliações
- EKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!No EverandEKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!Ainda não há avaliações
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsAinda não há avaliações
- A Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisNo EverandA Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisNota: 5 de 5 estrelas5/5 (1)
- Abnormal Slow Heart Beats, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandAbnormal Slow Heart Beats, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Fluid and Electrolytes for Nursing StudentsNo EverandFluid and Electrolytes for Nursing StudentsNota: 5 de 5 estrelas5/5 (12)
- Heart Arrhythmias, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandHeart Arrhythmias, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Heart Valve Diseases, A Simple Guide to These ConditionsNo EverandHeart Valve Diseases, A Simple Guide to These ConditionsAinda não há avaliações
- ECG & EKG Interpretation: How to interpret ECG & EKG, including rhythms, arrhythmias, and more!No EverandECG & EKG Interpretation: How to interpret ECG & EKG, including rhythms, arrhythmias, and more!Ainda não há avaliações
- Congestive Heart Failure PDFDocumento9 páginasCongestive Heart Failure PDFSheryl Ann Mae BombalesAinda não há avaliações
- Stages of ShockDocumento13 páginasStages of ShockA. P.Ainda não há avaliações
- Cardiac II Study GuideDocumento6 páginasCardiac II Study GuiderunnermnAinda não há avaliações
- Arrythmia Review TableDocumento6 páginasArrythmia Review TablealobrienAinda não há avaliações
- Cardiac DisordersDocumento38 páginasCardiac Disordersprototypeallhell100% (1)
- Cardiovascular I: CAD: Coronary Artery Disease (Most Common in US) Risk FactorsDocumento4 páginasCardiovascular I: CAD: Coronary Artery Disease (Most Common in US) Risk FactorsJessica100% (1)
- Valvular Heart Disease 2Documento46 páginasValvular Heart Disease 2Topea BogdanAinda não há avaliações
- Heart FailureDocumento1 páginaHeart Failurehannahhwolf100% (3)
- Cardiac DisordersDocumento15 páginasCardiac Disordersgold_enriquez100% (3)
- Heart FailureDocumento3 páginasHeart FailureDr. Jennie Kim100% (3)
- Pulmonary Med Charts Part 2Documento2 páginasPulmonary Med Charts Part 2NursingSchoolNotes100% (3)
- ABG Interpretation - ATSDocumento5 páginasABG Interpretation - ATSHAMMYER ALROKHAMIAinda não há avaliações
- Cardiac Stuff That You Have To MemorizeDocumento1 páginaCardiac Stuff That You Have To MemorizeNursingSchoolNotes100% (1)
- ABG Poster A3Documento1 páginaABG Poster A3Araceli Ecot Calunod100% (2)
- Cardiovascular MneumonicsDocumento10 páginasCardiovascular MneumonicsKaly RieAinda não há avaliações
- PerfusionDocumento9 páginasPerfusionAmanda Brittain100% (2)
- CardioDocumento7 páginasCardioGerald AndrinAinda não há avaliações
- Cardiac DysrythmiasDocumento190 páginasCardiac DysrythmiasKoRnflakes100% (4)
- Congenital Heart DiseasesDocumento6 páginasCongenital Heart Diseasestheglobalnursing100% (2)
- Common Drugs ChartDocumento15 páginasCommon Drugs Chartforminsko100% (1)
- Cardiac NursingDocumento26 páginasCardiac Nursingjgcriste95% (20)
- Chapter - 036 Arrhythmias ClassDocumento129 páginasChapter - 036 Arrhythmias ClassWisdomIsMiseryAinda não há avaliações
- Cardiology MnemonicsDocumento12 páginasCardiology MnemonicsEliza SparkAinda não há avaliações
- Valvular Heart DiseaseDocumento10 páginasValvular Heart DiseaseEzyan SyaminAinda não há avaliações
- Cardiac Cath Lab Basis - Indications, Complications and Radiation ManagementDocumento62 páginasCardiac Cath Lab Basis - Indications, Complications and Radiation ManagementenzomontresolAinda não há avaliações
- Diabetes and Endocrine ChartsDocumento3 páginasDiabetes and Endocrine ChartsAja Blue86% (7)
- N53 ATI PHARM 207637583-Ati-PharmacologyDocumento26 páginasN53 ATI PHARM 207637583-Ati-PharmacologyWMWrian100% (3)
- Cardiovascular DrugsDocumento6 páginasCardiovascular Drugslhayes123488% (16)
- Cardiac SystemDocumento7 páginasCardiac Systemsccctutor100% (3)
- Congestive Heart Failure ReportDocumento6 páginasCongestive Heart Failure ReportSunshine_Bacla_4275100% (1)
- ABGs Respiratory/MetabolicDocumento3 páginasABGs Respiratory/MetabolicJoe B100% (1)
- Cardiac AssessmentDocumento7 páginasCardiac AssessmentBryan Mae H. Degorio75% (4)
- Adult III Cardiac Study GuideDocumento15 páginasAdult III Cardiac Study GuideNursingSchoolNotes100% (6)
- Cardionursing 110207023802 Phpapp01Documento18 páginasCardionursing 110207023802 Phpapp01LudwigJayBarayuga100% (5)
- My Cheat SheetDocumento3 páginasMy Cheat SheetTenzin KyizomAinda não há avaliações
- CHAPTER 27 - Heart Failure With A Preserved Ejection FractionDocumento15 páginasCHAPTER 27 - Heart Failure With A Preserved Ejection FractionReda SoAinda não há avaliações
- Medsurg Cardio Ana&PhysioDocumento6 páginasMedsurg Cardio Ana&Physiorabsibala80% (10)
- Cardiac MedsDocumento7 páginasCardiac MedsMary Fair DelcidAinda não há avaliações
- Chest Tube Explanation by AllnursesDocumento3 páginasChest Tube Explanation by AllnursesYemaya84Ainda não há avaliações
- Cardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandCardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Nice 2016Documento85 páginasNice 2016Diana ToroAinda não há avaliações
- Right Ventricular Function and Failure: Special ReportDocumento10 páginasRight Ventricular Function and Failure: Special ReportAny CórdovaAinda não há avaliações
- The Combined Impact of Surgical Team Education and Chlorhexidine 2% Alcohol On The Reduction of Surgical Site Infection Following Cardiac SurgeryDocumento7 páginasThe Combined Impact of Surgical Team Education and Chlorhexidine 2% Alcohol On The Reduction of Surgical Site Infection Following Cardiac SurgeryShandaPrimaDewiAinda não há avaliações
- NURS 627 Case Study PaperDocumento11 páginasNURS 627 Case Study PaperJaclyn Strangie100% (4)
- Non-Invasive Cardiac ImagingDocumento9 páginasNon-Invasive Cardiac Imagingoddone_outAinda não há avaliações
- Late Complications Following Tetralogy of Fallot RepairDocumento7 páginasLate Complications Following Tetralogy of Fallot RepairSam_pilzyAinda não há avaliações
- Physiological Reports - 2022 - Mulder - Distinct Morphologies of Arterial Waveforms Reveal Preload Contractility andDocumento18 páginasPhysiological Reports - 2022 - Mulder - Distinct Morphologies of Arterial Waveforms Reveal Preload Contractility andMASIEL AMELIA BARRANTES ARCEAinda não há avaliações
- 2022 AHA/ACC/HFSA Guideline For The Management of Heart Failure: Executive SummaryDocumento24 páginas2022 AHA/ACC/HFSA Guideline For The Management of Heart Failure: Executive SummaryAna RuizAinda não há avaliações
- Heart Failure - A Clinical Nursing HandbookDocumento273 páginasHeart Failure - A Clinical Nursing Handbookjustbeingclever100% (2)
- Acupuncture Heart FailureDocumento11 páginasAcupuncture Heart Failureabraham rumayaraAinda não há avaliações
- Best Management in Isolated Right Ventricular Hypoplasia With Septal Defects in AdultsDocumento7 páginasBest Management in Isolated Right Ventricular Hypoplasia With Septal Defects in AdultsReinaldi octaAinda não há avaliações
- Low Ejection FractionDocumento6 páginasLow Ejection FractionSanjay kumarAinda não há avaliações
- Vivid S70N-English-brochure - JB80430XXDocumento18 páginasVivid S70N-English-brochure - JB80430XXArrief nurcahyo100% (1)
- Duchenne Dilated Cardiomyopathy: Cardiac Management From Prevention To Advanced Cardiovascular TherapiesDocumento18 páginasDuchenne Dilated Cardiomyopathy: Cardiac Management From Prevention To Advanced Cardiovascular TherapiesKelvin SupriamiAinda não há avaliações
- Openhrt 2021 001732Documento9 páginasOpenhrt 2021 001732benypermadiAinda não há avaliações
- Physiology in Health and Disease L Britt Wilson, Richard A HoppmannDocumento324 páginasPhysiology in Health and Disease L Britt Wilson, Richard A HoppmanncjijcAinda não há avaliações
- New DOCX DocumentDocumento2 páginasNew DOCX DocumentPunjabi FootballAinda não há avaliações
- Esc Guideline Gagal JantungDocumento55 páginasEsc Guideline Gagal JantungdwiAinda não há avaliações
- Echocardiography Function Guiline Image 추가Documento105 páginasEchocardiography Function Guiline Image 추가stoicea catalin100% (1)
- MySono U5 Reference Manual EDocumento196 páginasMySono U5 Reference Manual ERenatoMonteiroAinda não há avaliações
- SonoAce - R7 - Reference Manual - PDocumento230 páginasSonoAce - R7 - Reference Manual - PEcomedical PlussAinda não há avaliações
- YMJE 2022 ASE AbstractsDocumento103 páginasYMJE 2022 ASE AbstractsGuillermo CenturionAinda não há avaliações
- Diafragma en ICCDocumento13 páginasDiafragma en ICCMonserrat CruzAinda não há avaliações
- Presentation2 BREAST IMAGING - LatestDocumento53 páginasPresentation2 BREAST IMAGING - LatestLadipo Temitope AyodejiAinda não há avaliações
- Ecocardiografia NeonatalDocumento10 páginasEcocardiografia NeonatalRonald MHAinda não há avaliações
- Heart FailureDocumento20 páginasHeart Failurelancer 89100% (1)
- Quantum Resonance Magnetic Analyzer - Arnulfo Yu Laniba TestDocumento87 páginasQuantum Resonance Magnetic Analyzer - Arnulfo Yu Laniba TestArnulfo Yu Laniba100% (3)
- ESC/EACTS vs. ACC/AHA Guidelines For The Management of Severe Aortic StenosisDocumento17 páginasESC/EACTS vs. ACC/AHA Guidelines For The Management of Severe Aortic StenosisMiguel PugaAinda não há avaliações