Escolar Documentos
Profissional Documentos
Cultura Documentos
1674 Full
Enviado por
Nadya PurwantyDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
1674 Full
Enviado por
Nadya PurwantyDireitos autorais:
Formatos disponíveis
Updated recommendations for managing the care of patients receiving oral bisphosphonate therapy : An advisory statement from the
American Dental Association Council on Scientific Affairs Beatrice J. Edwards, John W. Hellstein, Peter L. Jacobsen, Steven Kaltman, Angelo Mariotti and Cesar A. Migliorati JADA 2008;139(12):1674-1677
Downloaded from jada.ada.org on February 19, 2013
The following resources related to this article are available online at jada.ada.org ( this information is current as of February 19, 2013):
Updated information and services including high-resolution figures, can be found in the online version of this article at:
http://jada.ada.org/content/139/12/1674
This article cites 16 articles, 4 of which can be accessed free: http://jada.ada.org/content/139/12/1674/#BIBL This article appears in the following subject collections: Pharmacology http://jada.ada.org/cgi/collection/pharmacology Information about obtaining reprints of this article or about permission to reproduce this article in whole or in part can be found at: http://www.ada.org/990.aspx
Copyright 2013 American Dental Association. All rights reserved. Reproduction or republication strictly prohibited without prior written permission of the American Dental Association. The sponsor and its products are not endorsed by the ADA.
A S S O C I A T I O N
R E P O R T
Updated recommendations for managing the care of patients receiving oral bisphosphonate therapy
An advisory statement from the American Dental Association Council on Scientific Affairs
Beatrice J. Edwards, MD, FACP; John W. Hellstein, DDS, MS; Peter L. Jacobsen, PhD, DDS; Steven Kaltman, DMD, MD; Angelo Mariotti, DDS, PhD; Cesar A. Migliorati, DDS, MS, PhD; for the American Dental Association Council on Scientific Affairs Expert Panel on BisphosphonateAssociated Osteonecrosis of the Jaw Authors note: This advisory statement was developed as an educational tool on the basis of our opinion after a review of the literature. Because of a paucity of clinical data regarding the management of the dental care of patients receiving oral bisphosphonate therapy, these recommendations are based primarily on expert opinion and are not a product of a systematic review. These recommendations are intended as a resource for dentists to complement their own professional judgment, data obtained from the dental and medical literature and information from the patients treating physician, and they should be balanced with the practitioners professional judgment and the individual patients preferences and needs.
Downloaded from jada.ada.org on February 19, 2013
he incidence of bisphosphonateassociated osteonecrosis (BON) of the jaw and its concomitant risk factors are not wellknown. As a result, dentists understandably are concerned about how to appropriately manage the care of patients receiving oral bisphosphonate therapy. The information presented here is a summary of the panels new report, which updates the 2006 recommendations.1 (The full report can be accessed at www.ada.org/prof/ resources/topics/topics_ osteonecrosis_bisphosphonate_ report.pdf.2) On the basis of a review of the current literature, the panel members reiterate their conclusion from the 2006 report: that the risk of developing this condition is low for patients who are receiving oral bisphosphonate therapy. The panel newly concludes that screening tests used for the purpose of determining a patients risk of developing BON are unreliable.
ABSTRACT
Background and Overview. In 2005, the American Dental Association (ADA) Council on Scientific Affairs convened an expert panel to develop clinical recommendations for dentists treating patients who are receiving oral bisphosphonate therapy. The Journal of the American Dental Association published the resulting report in 2006. This 2008 advisory statement is the first of projected periodic updates of the 2006 clinical recommendations. Conclusion. This 2008 advisory statement concludes, on the basis of a review of the current literature, that for patients receiving bisphosphonate therapy, the risk of developing bisphosphonate-associated osteonecrosis (BON) of the jaw apparently remains low. It also newly concludes that current screening and diagnostic tests are unreliable for predicting a patients risk of developing the condition. This statement updates the 2006 recommendations regarding general dentistry, management of periodontal diseases, implant placement and maintenance, oral and maxillofacial surgery, endodontics, restorative dentistry and prosthodontics, and orthodontics. Key Words. Bisphosphonate-associated osteonecrosis; osteoporosis; osteonecrosis. JADA 2008;139(12):1674-1677.
Dr. Edwards is an associate professor, Department of Medicine and Orthopaedic Surgery, Feinberg School of Medicine, Northwestern University, Chicago. Dr. Hellstein is a clinical professor, Department of Oral Pathology, Radiology and Medicine, University of Iowa, Iowa City. Dr. Jacobsen is an adjunct professor, Department of Pathology and Medicine, Arthur A. Dugoni School of Dentistry, University of the Pacific, San Francisco. Dr. Kaltman is the chairman, Department of Oral Surgery, College of Dental Medicine, Nova Southeastern University, Fort Lauderdale, Fla. Dr. Mariotti is a professor and the chair, Division of Periodontology, College of Dentistry, The Ohio State University, Columbus. Dr. Migliorati is a professor, Department of Diagnostic SciencesOral Medicine, College of Dental Medicine, Nova Southeastern University, Fort Lauderdale, Fla. Address reprint requests to the American Dental Association Council on Scientific Affairs, 211 E. Chicago Ave., Chicago, Ill. 60611.
1674
JADA, Vol. 139
http://jada.ada.org
December 2008
Copyright 2008 American Dental Association. All rights reserved. Reprinted by permission.
A S S O C I A T I O N
R E P O R T
On the basis of the current literature and of the cases reported so far, the panel concludes that a patients risk of developing BON of the jaws as a result of oral bisphosphonate therapy is minute as compared with the risk associated with intravenous bisphosphonate therapy in patients with cancer. Accordingly, the majority of reported cases of BON of the jaws have occurred in patients receiving the drugs intravenously for cancer therapy. There are no studies that adequately address the incidence of BON. Studies have estimated that BON occurs in about 20 percent of patients receiving bisphosphonates intravenously for cancer therapy (after extended use of zoledronate) and in between zero and 0.04 percent of patients taking these drugs orally.3-10 Although total U.S. prescriptions for oral bisphosphonates in 2006 exceeded 30 million,11 fewer than 10 percent of BON cases are associated with patients taking orally administered bisphosphonate drugs.3,12 The small risk of developing BON as a result of receiving oral bisphosphonate therapy must be weighed against the significant health benefits associated with the use of these drugs. Osteoporosis is a major cause of morbidity, functional dependence and institutionalization in older Americans. In 2004, the U.S. surgeon general published a report titled Bone Health and Osteoporosis that highlighted the public health imperative to address osteoporosis and prevent its health-related consequences.13 Each year, this bone disease accounts for 1.5 million new fractures. Of these fractures, 250,000 are hip fractures that result in mortality rates exceeding 20 percent in women and 30 percent in men, recurrent hospitalizations, increased office visits and, often, the need for care at extended-treatment facilities.13 In people who sustain hip fractures, less than 25 percent of them regain full function.14 All decisions with respect to use of drugs prescribed for medical conditions should be discussed with the prescribing physician. Given the risks associated with osteoporosis and the proven benefits of oral bisphosphonate therapy in treating it, the physician and patient should discuss fully any decision to alter the use of these medications.
RECOMMENDATIONS FOR MANAGEMENT OF DENTAL CARE OF PATIENTS RECEIVING ORAL BISPHOSPHONATE THERAPY
care of patients receiving oral bisphosphonate therapy: dRoutine dental treatment generally should not be modified solely because of the patients use of oral bisphosphonates. dAll patients should receive routine dental examinations. Patients who are prescribed oral bisphosphonates and are not receiving regular dental care likely would benefit from a comprehensive oral examination before or during the early portion of their bisphosphonate therapeutic regimen. dAll patients taking the drug should be informed that oral bisphosphonate use places them at very low risk of developing BON of the jaws (the actual incidence is unknown, with estimates ranging from zero to one in 2,260 cases3,6-10); the low risk of developing BON may be minimized but not eliminated; an oral health program consisting of sound oral hygiene practices and regular dental care may be the optimal approach for lowering the risk of developing BON; there is no validated diagnostic technique available to determine if patients are at increased risk of developing BON; discontinuing bisphosphonate therapy may not eliminate or reduce the risk of developing BON; if any problem develops in the oral cavity during oral bisphosphonate therapy, the patient should contact a dentist. A major goal in the prevention of BON is to limit the possibility of extensive or multifocal involvement. Although there is no evidence to support a conservative clinical approach, it may be prudent to proceed conservatively in some cases, potentially allowing the practitioner to gain some insight into how a patient will heal before putting multiple quadrants at risk. On the other hand, periapical pathoses, sinus tracts, purulent periodontal pockets, severe periodontitis and active abscesses that already involve the medullary bone all may exacerbate osteonecrosis, and these areas should be treated immediately even if multiple quadrants are involved.
ABBREVIATION KEY. ADA: American Dental Association. BON: Bisphosphonate-associated osteonecrosis. CTX: C-terminal cross-linking telopeptide of Type I collagen. NTX: N-telopeptide of Type I collagen.
JADA, Vol. 139 http://jada.ada.org December 2008 1675
Downloaded from jada.ada.org on February 19, 2013
General dentistry. The expert panel makes the following recommendations for the general dental
Copyright 2008 American Dental Association. All rights reserved. Reprinted by permission.
A S S O C I A T I O N
R E P O R T
be informed of the risk of developing BON, To the extent possible, the dentist should answer all of the patients questions regarding although that risk is small. The clinician should bisphosphonate use and the patients oral health. discuss with the patient alternative treatment The dentist should consider documenting the displans, which include endodontics (endodontic cussion of risks, benefits and treatment options treatment followed by removal of the clinical with the patient and obtaining the patients crown), allowing the roots to exfoliate (instead of written acknowledgment of that discussion and extraction) and provision of bridges and partial consent for the chosen course of treatment. dentures (instead of implant placement). Management of periodontal diseases. If extractions or bone surgery are necessary, Appropriate forms of nonsurgical therapy should the clinician should consider conservative surbe combined with the commonly recommended gical technique with primary tissue closure, when reevaluation at four to six weeks. If the disease feasible. In addition, immediately before and after fails to resolve and surgery becomes necessary, any surgical procedures involving bone, the the goal of surgical treatment should be to obtain patient should rinse gently with a chlorhexidineaccess to root surfaces. When necessary, the clinicontaining rinse until the site has healed. The cian should use modest bone-recontouring techregimen may be extended on the basis of the niques. At this time, there is no evidence that patients healing progress. Use of prophylactic periodontal procedures such as antibiotics after a surgical proguided tissue regeneration or bonecedure should be based on the risk replacement grafts increase or of an infection and not on the There is no evidence decrease the risk of BON developpatients bisphosphonate therapy. that malocclusion ment or the success of implant There is no evidence that the use of or masticatory forces treatment. The clinician should antibiotics is effective in preventing increase the risk consider the use of such techniques BON. of developing judiciously on the basis of patient Endodontics. Endodontic treatbisphosphonateneed. Primary soft-tissue closure ment is preferable to surgical after periodontal surgical promanipulation if a tooth is salvageassociated cedures is desirable, when feasible. able. Routine endodontic technique osteonecrosis. Implant placement and mainshould be used. Manipulation beyond the apex is not recomtenance. There is a paucity of data mended. In some situations, depending on risk, regarding the effects of implant placement in the clinician may consider the endodontic treatpatients receiving oral bisphosphonate ment of nonrestored teeth after removal of the therapy.15,16 clinical crown, which allows passive exfoliation of Because implant placement requires the prepathe root tip. Endodontic surgical procedures ration of the osteotomy site, the dentist should should be guided by the same recommendation as consider treatment options. The patient may be at increased risk of developing BON when extensive is used for any oral and maxillofacial surgical proimplant placement is necessary or when guided cedure described above. bone regeneration is required to augment a defiRestorative dentistry and prosthodontics. cient alveolar ridge before implant placement. There is no evidence that malocclusion or mastiMaintenance of implants should follow catory forces increase the risk of developing BON. accepted mechanical and pharmaceutical All routine restorative procedures may be conmethods to prevent peri-implantitis, including ducted in a patient receiving oral bisphosphonate regular monitoring of the patient. The clinician therapy. Prosthodontic appliances in patients should be adjusted for fit promptly to prevent should consider appropriate forms of nonsurgical ulceration and possible bone exposure. therapy combined with a prolonged phase of iniOrthodontics. We found no published studies tial therapy for patients with peri-implantitis. If examining the effect of bisphosphonates on orthothe disease does not resolve, surgical revision of dontic treatment. Case reports have recounted soft tissues around the implant(s) may be approinhibited tooth movement in patients receiving priate; when necessary, the clinician also may bisphosphonates.17,18 Patients should be advised of consider modest bone recontouring. Oral and maxillofacial surgery. Patients this potential complication. undergoing invasive surgical procedures should Collagen breakdown product testing and
1676 JADA, Vol. 139 http://jada.ada.org December 2008
Downloaded from jada.ada.org on February 19, 2013
Copyright 2008 American Dental Association. All rights reserved. Reprinted by permission.
A S S O C I A T I O N
R E P O R T
drug holidays. Recently, the use of serum levels of the collagen breakdown product C-terminal cross-linking telopeptide of Type I collagen (CTX) has been advocated as a risk predictor for development of BON.19 Serum CTX and urinary Ntelopeptide of Type I collagen (NTX) are considered markers for bone resorption. Reports suggest that dental treatment decisions should be based on the results of serum CTX/NTX level tests.19 These recommendations are derived from clinical observations at one institution that have not been validated. It remains to be seen if these recommendations will be corroborated by wellcontrolled, randomized clinical trials. Therefore, while this expert panel recognizes the value of predicting and mitigating the risk of developing BON in individual patients, until objective research studies document and correlate the specificity, predictive value and reliability of such tests, we can make no recommendations.
CONCLUSION
On the basis of a review of the current literature, the expert panel concludes that the risk of developing BON of the jaw apparently remains low for patients receiving bisphosphonate therapy. Therefore, routine dental treatment generally should not be modified solely because the patient is taking oral bisphosphonates. Furthermore, given the morbidity and mortality associated with osteoporosis and the proven benefits of oral bisphosphonate therapy, patients should not alter their use of these medications without first consulting with their physicians. More research is needed to identify risk factors for developing BON, as well as screening tools to predict patients risk.
Disclosure. None of the authors reported any disclosures. 1. American Dental Association Council on Scientific Affairs. Dental
management of patients receiving oral bisphosphonate therapy: expert panel recommendations. JADA 2006;137(8):1144-1150. 2. American Dental Association Council on Scientific Affairs. Dental management of patients receiving oral bisphosphonate therapy: expert panel recommendationsreport of the Council on Scientific Affairs. www.ada.org/prof/resources/topics/topics_osteonecrosis_ bisphosphonate_report.pdf. Accessed Oct. 22, 2008. 3. Grbic JT, Landesberg R, Lin SQ, et al. Incidence of osteonecrosis of the jaw in women with postmenopausal osteoporosis in the Health Outcomes and Reduced Incidence With Zoledronic Acid Once Yearly Pivotal Fracture Trial. JADA 2008;139(1):32-40. 4. Bilezikian JP. Osteonecrosis of the jaw: do bisphosphonates pose a risk? N Engl J Med 2006;355(22):2278-2281. 5. Boonyapakorn T, Schirmer I, Reichart PA, Sturm I, Massenkeil G. Bisphosphonate-induced osteonecrosis of the jaws: prospective study of 80 patients with multiple myeloma and other malignancies. Oral Oncol 2008;44(9):857-869. 6. Felsenberg D, Hoffmeister B, Amling M. Bisphosphonattherapie assoziierte. Kiefernekrosen Deutsches Arzteblatt 2006;46: A3078-A3080. 7. Mavrokokki T, Cheng A, Stein B, Goss A. Nature and frequency of bisphosphonate-associated osteonecrosis of the jaws in Australia. J Oral Maxillofac Surg 2007;65(3):415-423. 8. Black DM, Delmas PD, Eastell R, et al.; HORIZON Pivotal Fracture Trial. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 2007;356(18):1809-1822. 9. Etminan M, Aminzadeh K, Matthew IR, Brophy JM. Use of oral bisphosphonates and the risk of aseptic osteonecrosis: a nested casecontrol study. J Rheumatol 2008;35(4):691-695. 10. Cartsos VM, Zhu S, Zavras AI. Bisphosphonate use and the risk of adverse jaw outcomes. JADA 2008;139(1):23-30. 11. Drug Topics. Top 200 brand-name drugs by units in 2006. www.drugtopics.com/drugtopics/Pharmacy+Facts+And+Figures/ Top-200-brand-name-drugs-by-units-in-2006/ArticleStandard/Article/ detail/407649?contextCategoryId=7604. Accessed Sept. 12, 2007. 12. Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg 2004;62(5):527-534. 13. U.S. Department of Health & Human Services. Bone health and osteoporosis: a report of the surgeon general (2004). www. surgeongeneral.gov/library/bonehealth/content.html. Accessed Oct. 2, 2008. 14. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet 2002;359(9319):1761-1767. 15. Jeffcoat MK. Safety of oral bisphosphonates: controlled studies on alveolar bone. Int J Oral Maxillofac Implants 2006;21(3):349-353. 16. Wang HL, Weber D, McCauley LK. Effect of long-term oral bisphosphonates on implant wound healing: literature review and a case report. J Periodontol 2007;78(3):584-594. 17. Schwartz JE. Ask us: some drugs affect tooth movement. Am J Orthod Dentofacial Orthop 2005;127(6):644. 18. Rinchuse DJ, Rinchuse DJ, Sosovicka MF, Robison JM, Pendleton R. Orthodontic treatment of patients using bisphosphonates: a report of 2 cases. Am J Orthod Dentofacial Orthop 2007;131(3):321-326. 19. Marx RE, Cillo JE, Ulloa JJ. Oral bisphosphonate-induced osteonecrosis: risk factors, prediction of risk using serum CTX testing, prevention, and treatment. J Oral Maxillofac Surg 2007;65(12): 2397-2410.
Downloaded from jada.ada.org on February 19, 2013
JADA, Vol. 139
http://jada.ada.org
December 2008
1677
Copyright 2008 American Dental Association. All rights reserved. Reprinted by permission.
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- KDIGO 2023 CKD Guideline Public Review Draft 5 July 2023Documento339 páginasKDIGO 2023 CKD Guideline Public Review Draft 5 July 2023oscar coreaAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Quick Guide To Cardiopulmonary Care 4th EditionDocumento185 páginasQuick Guide To Cardiopulmonary Care 4th EditionLorenzo Romero AlbarranAinda não há avaliações
- User Manual: Samsung Medison Diagnostic Ultrasound SystemDocumento686 páginasUser Manual: Samsung Medison Diagnostic Ultrasound SystemHuế Trần100% (1)
- Doxycycline Inhibition of Interleukin-1 in The Corneal EpitheliumDocumento14 páginasDoxycycline Inhibition of Interleukin-1 in The Corneal EpitheliumNadya PurwantyAinda não há avaliações
- Dental Research Journal: Microflora and Periodontal DiseaseDocumento5 páginasDental Research Journal: Microflora and Periodontal DiseaseNadya PurwantyAinda não há avaliações
- Microrna-146 Inhibits Pro-Inflammatory Cytokine Secretion Through Il-1 Receptor-Associated Kinase 1 in Human Gingival FibroblastsDocumento9 páginasMicrorna-146 Inhibits Pro-Inflammatory Cytokine Secretion Through Il-1 Receptor-Associated Kinase 1 in Human Gingival FibroblastsNadya PurwantyAinda não há avaliações
- Periodontal Infectogenomics: ReviewDocumento6 páginasPeriodontal Infectogenomics: ReviewNadya PurwantyAinda não há avaliações
- CRP and IL-1B Gene Polymorphisms and CRP in Blood in Periodontal DiseaseDocumento6 páginasCRP and IL-1B Gene Polymorphisms and CRP in Blood in Periodontal DiseaseNadya PurwantyAinda não há avaliações
- 55 233 1 PBDocumento7 páginas55 233 1 PBNadya PurwantyAinda não há avaliações
- 14 1 Association Interleukin BayoumiDocumento8 páginas14 1 Association Interleukin BayoumiNadya PurwantyAinda não há avaliações
- Effect of Rheumatoid Arthritis On Periodontitis: A Historical Cohort StudyDocumento6 páginasEffect of Rheumatoid Arthritis On Periodontitis: A Historical Cohort StudyNadya PurwantyAinda não há avaliações
- j1 SparloxacinDocumento11 páginasj1 SparloxacinNadya PurwantyAinda não há avaliações
- Asociacin Enfermedad Periodontal EnfermedadessistTmicasDocumento7 páginasAsociacin Enfermedad Periodontal EnfermedadessistTmicasNadya PurwantyAinda não há avaliações
- Journal 5Documento5 páginasJournal 5Nadya PurwantyAinda não há avaliações
- Mechanical Interview Questions and Answers - Fluid MechanicsDocumento2 páginasMechanical Interview Questions and Answers - Fluid MechanicsannukiitAinda não há avaliações
- G1 CurvedDocumento16 páginasG1 CurvedElbert Ryan OcampoAinda não há avaliações
- Reviewer Crim 3 FinalsDocumento6 páginasReviewer Crim 3 FinalsMaria Rafaella P. DadoAinda não há avaliações
- Ansi Asa S3.22 - 2014Documento54 páginasAnsi Asa S3.22 - 20147620383tlAinda não há avaliações
- EMI Course CatalogDocumento645 páginasEMI Course CatalogFarouk OthmaniAinda não há avaliações
- The Necessity of Using Neurophysiological Methods For Diagnosing Communication Disorders. by Akhsaful To Tawhida Jahan MamDocumento11 páginasThe Necessity of Using Neurophysiological Methods For Diagnosing Communication Disorders. by Akhsaful To Tawhida Jahan MamAkhsaful ImamAinda não há avaliações
- ENG 110-Task 4 (Unintended Messages)Documento2 páginasENG 110-Task 4 (Unintended Messages)Erika Noreen Dela RosaAinda não há avaliações
- 04 TitrimetryDocumento7 páginas04 TitrimetryDarwin Fetalbero ReyesAinda não há avaliações
- Pharmacy Incharge JDDocumento5 páginasPharmacy Incharge JDUsman JamilAinda não há avaliações
- Competency Competency Multiple Choice Multiple Choice ComputationDocumento4 páginasCompetency Competency Multiple Choice Multiple Choice ComputationAaron James LicoAinda não há avaliações
- A-Level: Psychology 7182/1Documento20 páginasA-Level: Psychology 7182/1Queen Bee (Tt)Ainda não há avaliações
- Energy Savings at DCL PDFDocumento83 páginasEnergy Savings at DCL PDFnsprasad88100% (1)
- Corrosion Short Courses - Environmental CrackingDocumento8 páginasCorrosion Short Courses - Environmental CrackingMario SalayaAinda não há avaliações
- Textile Chemical Brochure 8.6.22 - 031Documento1 páginaTextile Chemical Brochure 8.6.22 - 031NIKESH PRAKASHAinda não há avaliações
- Top AttorneysDocumento7 páginasTop AttorneysArlington MagazineAinda não há avaliações
- Lecture 5 - Elements of Plasticity TheoryDocumento13 páginasLecture 5 - Elements of Plasticity TheoryNeeraj KumarAinda não há avaliações
- Granulation Process Basic UnderstandingDocumento3 páginasGranulation Process Basic UnderstandingRainMan75Ainda não há avaliações
- Inverter ProjectDocumento19 páginasInverter ProjectRavi Sharma100% (1)
- 2018 Haar Wavelet For Solving The Inverse Point Kinetics EquationsDocumento8 páginas2018 Haar Wavelet For Solving The Inverse Point Kinetics EquationsGeraldinAinda não há avaliações
- Homoeopathic Treatment of Complicated Sebaceous Cyst - A Case StudyDocumento5 páginasHomoeopathic Treatment of Complicated Sebaceous Cyst - A Case StudyDr deepakAinda não há avaliações
- API 572 Practise QuestionDocumento58 páginasAPI 572 Practise Questionbelonk_182100% (6)
- Souvenir Mushrooms 1986Documento106 páginasSouvenir Mushrooms 1986Ankit MishraAinda não há avaliações
- Blood Anatomy and Physiology ReviewDocumento20 páginasBlood Anatomy and Physiology ReviewStacey CamilleAinda não há avaliações
- Risk Management Policy StatementDocumento13 páginasRisk Management Policy StatementRatnakumar ManivannanAinda não há avaliações
- WW.04.05 Contraction Stress Test (Oxytocin Challenge Test) PDFDocumento3 páginasWW.04.05 Contraction Stress Test (Oxytocin Challenge Test) PDFDiah Kurniawati100% (1)
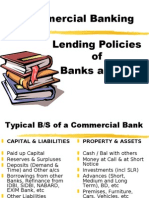
- Lending Policies of Indian BanksDocumento47 páginasLending Policies of Indian BanksProf Dr Chowdari Prasad80% (5)