Escolar Documentos
Profissional Documentos
Cultura Documentos
EFR PSC Add11 LR
Enviado por
jkarineTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
EFR PSC Add11 LR
Enviado por
jkarineDireitos autorais:
Formatos disponíveis
Primary
Secondary ary y Care
Addendum
and
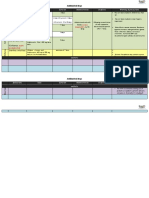
Dear Emergency First Response Course Participant, Re: Recent changes to CPR and first aid protocols In October 2010, the American Heart Association (AHA) and the European Resuscitation Council (ERC), two members of the International Liaison Committee on Resuscitation (ILCOR) slightly modified the CPR and Emergency Cardiac Care (ECC) guidelines. Emergency First Response programs follow guidelines established by these ILCOR member associations and implement changes whenever protocols are revised. The new guidelines do not show a great change to the information found in this Primary and Secondary Care Participant Manual, and further reinforce emphasis on providing effective chest compressions with minimal interruptions. Studies have shown the importance of providing fast, effective chest compressions as a critical aspect in treating a patient who has suffered cardiac arrest. Please note the changes and where in the Primary Care & Secondary Care course manual it applies from the chart below: Rationale & (page) affected New Guideline Old Guideline
No Look, listen, and feel for breathing Look, listen and feel for breathing before administering rescue breaths and chest compressions Minimize the delay in providing chest compressions. (1-25, 1-26, 2-6, 2-8, 2-10, 2-11)
Begin CPR by providing 30 chest compressions, then open the airway and give two breaths. If you suspect possible drowning, begin CPR with rescue breaths before chest compressions Compress adult chest to a depth of at least 2 inches (5 cm)
Give two rescue breaths prior to giving 30 chest compressions
Existing oxygen in the lungs and in the circulatory system is sufficient to provide immediate benefits provided by chest compressions. (1-4, 1-22, 1-23, 1-26, 1-27, 2-10, 2-11, 2-12)
Compress adult chest to a depth of 1 to 2 inches
Emphasis is on providing good quality chest compressions with sufficient depth to provide adequate circulation (2-13)
Give compressions at a rate of at least 100 per minute
Give compression at a rate of approximately 100 per minute
Emphasis is on good quality chest compressions at a rate to provide adequate circulation (2-13) Emphasis is on reducing the number and duration of pauses during chest compressions (1-28, 2-26, 2-27)
To minimize interruptions in chest compressions, if there is more than one rescuer present, continue CPR while the AED is switched on and the pads are being placed on the patient Reduced emphasis on barrier use when providing CPR. Although still recommended, treatment should not be delayed if barriers are not available.
No reference to continuing chest compressions while preparing the AED
Emphasized use of barriers
Research has shown that disease transmission is very rare when providing CPR (1-19, 2-4, 2-5,
emergencyrstresponse.com
Product No. 10341 (3/11) Version 1.0 Emergency First Response Corp. 2011
Primary and Secondary Care Addendum
AHA First Aid Changes Allergic Reactions For patients carrying an epinephrine kit, help patient use it following directions. If symptoms of anaphylaxis persist despite epinephrine administration, seek medical assistance before administering a second dose of epinephrine. In unusual circumstances, when advanced medical assistance is not available, a second dose of epinephrine may be given if symptoms of anaphylaxis persist. Page 3-14 Heart Attack Advise the patient to chew one adult (nonenteric-coated) or two low dose aspirins, if the patient is complaining of chest pains and does not have a history of allergy to aspirin and no recent gastrointestinal bleeding. This may be performed after activating the EMS system. Page 3-11 Venomous Bites and Stings For snake bites, apply a pressure immobilization bandage around the entire length of the bitten extremity. This is an effective and safe way to slow the dissemination of venom. Care must be taken to ensure the pressure bandage is not too tight. You should be able to slide a finger under the bandage. Page 3-18 Treat jellyfish stings by liberally washing the affected area with vinegar (4-6% acetic acid solution) for at least 30 seconds to inactivate venom and prevent further envenomation. After the nematocysts are removed or deactivated, treat pain with hot-water immersion when possible. Page 3-18
Thank you for participating in an Emergency First Response Course.
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Use of "Zingiber Officinale Roscoe L" Root in Various DiseasesDocumento8 páginasUse of "Zingiber Officinale Roscoe L" Root in Various DiseasesCentral Asian StudiesAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Chapter 7 - Hannah Wilder - ChorioamnionitisDocumento7 páginasChapter 7 - Hannah Wilder - ChorioamnionitisEunice CortésAinda não há avaliações
- Cosmetic Surgery PDFDocumento3 páginasCosmetic Surgery PDFDa Young Anna Choi100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- of M.pharmDocumento13 páginasof M.pharmVivek Patel ViksAinda não há avaliações
- Literature & MedicineDocumento14 páginasLiterature & MedicineJoyce LeungAinda não há avaliações
- Disabilities Act 1995Documento4 páginasDisabilities Act 1995directdeoAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Indications Dose Duration Administration Stability Warning & PrecautionsDocumento2 páginasIndications Dose Duration Administration Stability Warning & PrecautionsFatma HasanAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- HarveyDocumento6 páginasHarveyapi-276953527Ainda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Laboratory Investigation Report: HaematologyDocumento3 páginasLaboratory Investigation Report: HaematologyHarshitAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Rab Flow CHT 3 PeopleDocumento2 páginasRab Flow CHT 3 PeopleWDIV/ClickOnDetroitAinda não há avaliações
- Nur 300-Nursing Philosophy-CdDocumento7 páginasNur 300-Nursing Philosophy-Cdapi-501578262Ainda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Anemia Proposal RefinedDocumento13 páginasAnemia Proposal RefinedAxel BlazeAinda não há avaliações
- RECORDING Form 1: Masterlist of Grade 1 StudentsDocumento4 páginasRECORDING Form 1: Masterlist of Grade 1 StudentsGirlie Harical GangawanAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Conference & Workshop ScheduleDocumento5 páginasConference & Workshop ScheduleglmoningkaAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Daily Vagus Nerve Exercises A Self-Help G - Sherman SanderDocumento90 páginasDaily Vagus Nerve Exercises A Self-Help G - Sherman Sanderscriberone100% (6)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
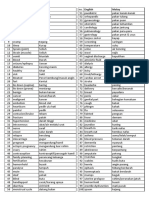
- Medic Term English MalayDocumento1 páginaMedic Term English MalaySyamimi SuhaimiAinda não há avaliações
- ProjectDocumento3 páginasProjectAnshul PaunikarAinda não há avaliações
- Hemisphere SpecializationDocumento7 páginasHemisphere SpecializationLisa MartinezAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Hipertensi KrisisDocumento30 páginasHipertensi KrisisLuthfan HakimAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- PeritonitisDocumento21 páginasPeritonitischrisyenAinda não há avaliações
- Gambaran Penggunaan Antibiotik Pada Pasien Pediatri Infeksi Saluran Pernapasan Akut (Ispa) Di Klinik Sint. Carolus BengkuluDocumento8 páginasGambaran Penggunaan Antibiotik Pada Pasien Pediatri Infeksi Saluran Pernapasan Akut (Ispa) Di Klinik Sint. Carolus BengkuluLuli Corvelo SarmentoAinda não há avaliações
- Thyroid Crisis... FinalDocumento53 páginasThyroid Crisis... FinalYhanaAdarneAinda não há avaliações
- Wilkins 6 - Neurological Assessment - AssignmentDocumento33 páginasWilkins 6 - Neurological Assessment - AssignmentArifurRahman100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Fractures in ChildrenDocumento26 páginasFractures in ChildrenRafli SoehadakAinda não há avaliações
- Category Class Merit Round2 MBBS-BDSDocumento102 páginasCategory Class Merit Round2 MBBS-BDSSUSHIL LAKRAAinda não há avaliações
- Ozone Therapy by Saul Pressman at Oxygen Therapies Support Forum, Topic 443552 PDFDocumento15 páginasOzone Therapy by Saul Pressman at Oxygen Therapies Support Forum, Topic 443552 PDFHello MisterAinda não há avaliações
- First Aid / CPR: HSE Training 2005Documento36 páginasFirst Aid / CPR: HSE Training 2005Martin griffinAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- InhalantDocumento8 páginasInhalantArvin Ian Penaflor100% (1)
- Roles & Responsibilities of CRADocumento26 páginasRoles & Responsibilities of CRANaresh Kumar RapoluAinda não há avaliações
- Vit KDocumento2 páginasVit KBilly Jeremia TandoAinda não há avaliações