Escolar Documentos
Profissional Documentos
Cultura Documentos
Anterior Deltopectoral Approach
Enviado por
Netravathi EllurDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Anterior Deltopectoral Approach
Enviado por
Netravathi EllurDireitos autorais:
Formatos disponíveis
Journal of Orthopaedic Surgery 2012;20(1):66-70
Anterior deltopectoral approach for axillary nerve neurotisation
Department of Orthopedics, Hand and Reconstructive Microsurgery, Apollo Specialty Hospitals, KK Nagar, Madurai, India
J Terrence Jose Jerome
ABSTRACT Purpose. To report outcome of axillary nerve neurotisation for brachial plexus injury through the anterior deltopectoral approach. Methods. Nine men aged 20 to 52 (mean, 27.8) years with brachial plexus injury underwent axillary nerve neurotisation through the anterior deltopectoral approach. Three of the patients had complete avulsion of C5-T1 nerve roots. The remaining 6 patients had brachial plexus injury of C5-C6 nerve roots, with associated subluxation of the glenohumeral joint, atrophy of the supraspinatus, deltoid and elbow flexors. They had no active shoulder abduction, external rotation, and elbow flexion. The pectoralis major and minor were cut and/or retracted to expose the underlying infraclavicular plexus. The axillary nerve was identified with respect to the available donor nerves (long head of triceps branch, thoracodorsal nerve, and medial pectoral nerve). In addition to the axillary nerve neurotisation, each patient had a spinal accessory nerve transferred to the
suprascapular nerve for better shoulder animation. Results. Patients were followed up for 24 to 30 (mean, 26) months. In the 3 patients with C5-T1 nerve root injuries, the mean active abduction and external rotation were 63 and 20, respectively, whereas the mean abduction strength was M3 (motion against gravity). In the 6 patients with C5-C6 nerve root injuries, the mean active abduction and external rotation were 133 and 65, respectively, whereas the strength of the deltoids and triceps was M5 (normal) in all. In 4 patients with the pectoralis major cut and repaired, the muscle regained normal strength. Conclusion. The anterior deltopectoral approach enabled easy access to all available donor nerves for axillary nerve neurotisation and achieved good outcomes.
Key words: axilla; brachial plexus neuropathies; nerve transfer
INTRODUCTION Shoulder abduction is important for upper limb functions, as more distal functions depend on a
Address correspondence and reprint requests to: Dr J Terrence Jose Jerome, Department of Orthopedics, Hand and Reconstructive Microsurgery, Apollo Specialty Hospitals, KK Nagar, Madurai 625 020, India. E-mail: terrencejose@gmail.com
Vol. 20 No. 1, April 2012
Anterior deltopectoral approach for axillary nerve neurotisation
67
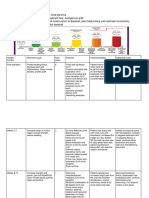
stable shoulder.16 Reconstruction of both axillary and suprascapular nerves can improve shoulder function and glenohumeral joint stability.610 A number of approaches to axillary nerve neurotisation for brachial plexus injuries have been reported, but all have limitations.1113 We report outcomes of axillary nerve neurotisation for brachial plexus injury through the anterior deltopectoral approach. MATERIALS AND METHODS In March 2009, 9 consecutive men aged 20 to 52 (mean, 27.8) years with brachial plexus injury of the right (n=6) and left (n=3) shoulders after falling from a bike underwent axillary nerve neurotisation through the anterior deltopectoral approach. The power of the muscle involved was assessed using the Medical Research Council (British) system. Radiographs, computed tomographic myelography, and/or magnetic resonance imaging of the cervical spine, shoulder, and chest were obtained. The preganglionic injury and nerve root avulsion were confirmed electrophysiologically and clinically (deafferentation pain, Horner syndrome, absent Tinel sign, and weak rhomboid and serratus muscles). Three of the patients had complete avulsion of C5-T1 nerve roots, without any associated chest wall or lung injury. The remaining 6 patients had brachial plexus injury of C5-C6 nerve roots, with associated subluxation of the glenohumeral joint, atrophy of the supraspinatus, deltoid and elbow flexors. They had no active shoulder abduction, external rotation, and elbow flexion. All 9 patients had at least M4 power (motion against resistance) in the triceps. The patient was placed in a supine position, with a sandbag beneath the affected extremity. Under general anaesthesia, the supraclavicular part of the plexus was exposed through a transverse incision 2 cm above the clavicle at the root of the neck. The extent of injury was confirmed by electrical stimulation. The spinal accessory nerve was identified along the superior border of the trapezius and transferred to the suprascapular nerve preserving its proximal branch. For C5-T1 nerve root injuries, the intercostal nerve was transferred to the axillary and musculocutaneous nerves through the anterior deltopectoral approach. For C5-C6 nerve root injuries, the patients underwent the Oberlin procedure (transferring ulnar nerve fascicle to the biceps branch of the musculocutaneous nerve) for elbow flexion through the distal extension of the deltopectoral approach, and the long head of the triceps branch was transferred to the axillary nerve (Fig.).
(a)
Axillary nerve Radial nerve
LHTB*
(b)
Figure (a) The locations of the axillary nerve (lateral), radial nerve (middle), and long head of triceps branch (LHTB) [medial] at the posterior cord level. (b) The orientation of the medial pectoral nerve (branch from medial cord), thoracodorsal nerves, and the LHTB (asterisk) with the axillary nerve.
Postoperatively, the patients were put on broad arm sling for 3 weeks. Electrical stimulation was started at week 6. The range of movement and muscle power were regularly assessed. RESULTS The mean interval from injury to surgery was 4.3 (range, 26) months. Patients were followed up for 24 to 30 (mean, 26) months (Table 1). Shoulder control and palpable contractions were noted at postoperative month 2. In the 3 patients with C5T1 nerve root injuries, the mean active abduction
68
JTJ Jerome Table 1 Patient characteristics and outcomes
Journal of Orthopaedic Surgery
Patient Sex/age Side Interval Injury Donor FollowPostop Postop Postop no. (years) involved from area nerve* up shoulder shoulder external injury to (months) abduction range of rotation surgery motion (months) 1 2 3 4 5 6 7 8 9 M/23 M/30 M/52 M/31 M/22 M/25 M/26 M/21 M/20 Left Right Right Left Right Left Right Right Right 2 6 4 4 5 5 3 5 3 C5-T1 C5-T1 C5-C6 C5-T1 C5-C6 C5-C6 C5-C6 C5-C6 C5-C6 IC IC LHTB IC LHTB LHTB LHTB LHTB LHTB 25 24 30 28 24 26 27 26 24 M3 M3 M5 M3 M5 M5 M5 M5 M5 60 70 130 60 140 130 140 130 130 M3 M3 M5 M3 M5 M5 M5 M5 M5
Additional nerve transfers*
IC to MCN, SAN to SSN IC to MCN, SAN to SSN SAN to SSN, Oberlin transfer IC to MCN, SAN to SSN SAN to SSN, Oberlin transfer SAN to SSN, Oberlin transfer SAN to SSN, Oberlin transfer SAN to SSN, Oberlin transfer SAN to SSN, Oberlin transfer
* IC denotes intercostal nerve, LHTB long head of triceps branch, MCN musculocutaneous nerve, SAN spinal accessory nerve, SSN suprascapular nerve, and Oberlin transfer transferring ulnar nerve fascicle to biceps branch of musculocutaneous nerve M3 denotes motion against gravity, M4 motion against resistance, M5 normal strength
and external rotation were 63 and 20, respectively, whereas the mean abduction strength was M3 (motion against gravity). In the 6 patients with C5-C6 nerve root injuries, the mean active abduction and external rotation were 133 and 65, respectively, whereas the strength of the deltoids and triceps was M5 (normal) in all. The outcome of transferring the long head of triceps branch was superior to transferring the intercostal nerve to the axillary nerve. In 4 patients with the pectoralis major cut and repaired, the muscle regained normal strength. DISCUSSION The posterior, lateral, and medial cords of the brachial plexus receive their respective names from their spatial orientation to the second part of the axillary artery. Nonetheless, there are considerable variations in the orientation and interconnections of the cords to each other and to the major vessels. A few specific nerves emerging from the posterior, lateral, and medial cords can be used as donors for neurotisation in brachial plexus injuries.14,15 For axillary nerve neurotisation through the anterior deltopectoral approach, the key landmarks are the cephalic vein (as a guide to the deltopectoral groove), the clavipectoral fascia (covering the infraclavicular brachial plexus as it exits under the tendon of the pectoralis minor), the lateral cord, and the axillary artery. The pectoralis major and pectoralis minor are cut and/or retracted to view the infraclavicular plexus. If exposure is difficult, these muscles are cut and taken up with tie sutures
for final approximation. The lateral cord and the axillary artery are swept medially to enable access to the posterior cord and axillary nerve. The axillary nerve is neurotised, depending on the length of the donor nerves. The axillary nerve exits the posterior cord at the level of the lower border of the pectoralis minor, curves backward and passes through the quadrangular space together with the posterior circumflex humeral artery,1316 where it divides into anterior and posterior branches. The axillary nerve is located high in the axilla, posterior to the axillary artery, lateral to the radial nerve, and anterior to the subscapularis. The long head of triceps branch (first branch of the radial nerve) is posterior and medial to the radial nerve at this region. These 3 nerves course more or less parallel in their exit at this level of approach. In this region, the axillary nerve is lateral, the radial nerve is in the middle, and the long head of triceps branch is medial (Fig.). The long head of triceps branch is transferred to the axillary nerve. For C5-C6 brachial plexus injuries, the anterior deltopectoral approach enables easy access to various donor nerves. The long head of triceps branch can be transferred to thoracodorsal or mediopectoral nerves. The median nerve fascicles, ulnar nerve fascicles, thoracodorsal and mediopectoral nerves can be transferred to the axillary nerve. The axillary nerve is one of 2 terminal branches of the posterior cord of the brachial plexus. It contains fibres from C5 and C6 ventral rami. The anterior branch innervates the anterior deltoid and the largest posterior branch innervates the teres minor and deltoid. The supraspinatus and deltoid are equally
Vol. 20 No. 1, April 2012
Anterior deltopectoral approach for axillary nerve neurotisation
69
Table 2 Comparison of studies involving axillary nerve neurotisation using the triceps branch for brachial plexus injuries of C5-C6 Studies Lurje,23 1948 Colbert and Mackinnon,2 2008 Vekris et al,21 2010 Bertelli et al,13 2007 Bertelli and Ghizoni,8 2004 Leechavengvongs et al,11 2003 Our study No. of patients 1 1 5 3 7 7 6 Approach Anterior Posterior Posterior Axillary recess Posterior Posterior Anterior deltopectoral Donor nerve Unnamed branch Medial head of triceps branch Long head of triceps branch Long/medial head of triceps branches Long head of triceps branch Long head of triceps branch Long head of triceps branch Mean Deltoid abduction strength* 35 110 45 92 124 133 Good M4- to M4 M4 External rotation Satisfactory 3010 -
M3+ to M4 3 (-10 to 30) M4 M4 M5 M5
* M3 denotes motion against gravity, M4 motion against resistance, M5 normal strength
responsible for producing torque about the shoulder joint in the functional planes of motion, whereas the deltoid is capable of initiating elevation in the plane of the scapula. The infraspinatus is a powerful external rotator, followed by the teres minor and the posterior deltoid.15,16 There are different approaches to neurotise the axillary nerve. The interval between the lateral and the long heads of the triceps is located in the posterior approach11 at the level of the triangular space to expose the radial nerve, nerves to the long head and lateral head of the triceps. Through the posterior approach, excessive retraction of the deltoid is required and may result in injury to the posterior branch of the axillary nerve and limited arm abduction.17,18 Therefore, caution is necessary. The disadvantages of the posterior approach are difficulty in dissecting the teres minor branch, change of position following the brachial plexus exploration and the suprascapular neurotisation procedures, separate incision, and extended operating time. The entire axillary and suprascapular nerves are explored through a sabre-cut incision12 starting anteriorly near the axillary fold and continuing along the deltopectoral groove over the clavicle to the quadrilateral space posteriorly. The success of this extensive procedure depends on a meticulous surgical technique and secure reattachment of muscles. The axillary recess approach13 exposes the axillary nerve in a triangle bounded by the latissimus dorsi tendon, posterior circumflex humeral artery, and subscapular artery. The anterior and middle deltoid branch is the most laterally located, curving around the humerus, whereas the teres minor branch is close to the long head of the triceps. Although the axillary nerve can be exposed by the axillary approach, its proximal portion is difficult to dissect through this approach. Thus, the
anterior deltopectoral approach is preferable for the proximal dissection of the axillary nerve. In our study, the outcome of transferring the intercostal nerve to the axillary nerve was only moderate. Intercostal nerves contain 500 to 700 nerve fibres. In complete brachial plexus injury, the results of transferring the intercostal nerve vary widely, depending on the level of the intercostal nerve transection, the number of transferred nerves, the level of the nerve anastomosis, and the use of nerve grafts. In 4 patients with complete brachial plexus palsy, shoulder control to a maximum of 30 abduction was achieved using the intercostal, phrenic, and spinal accessory nerves as donors.19 The mean improvement was 10 in abduction when concomitant connection (double nerve transfers) of the suprascapular nerve to the phrenic nerve and the axillary nerve to the cranial nerve XI.19 The overall and useful recovery rates were 63% and 33%, respectively, for the axillary nerve,20 whereas the shoulder abduction was <40 with M3-/M3 motor power.21 None of the above studies provided any results on external rotation recovery. In our study, 3 patients achieved a mean abduction of 65 with M3 grade of external rotation. Shoulder re-animation was achieved with suprascapular nerve neurotisation, because supraspinatus function (rotator cuff) is important in the shoulder arc of motion and stabilisation along with axillary nerve neurotisation. Functional improvement of the shoulder is better in patients with successful re-innervation of the biceps. Although transferring the intercostal nerve to the axillary nerve does not confer muscle strength, speed, range of motion, and endurance,22 it enables better shoulder abduction and external rotation. In C5-C6 nerve root injuries, concomitant neurotisation of the suprascapular nerve and the axillary nerve enabled better outcomes in shoulder
70
JTJ Jerome
Journal of Orthopaedic Surgery
abduction and external rotation.110 Transferring the long head of triceps branch to the axillary nerve is superior, because the nerve is close to the target muscle. It increases the likelihood of reinnervation under voluntary control and is not tied to antagonist co-contractions owing to aberrant axonal growth. Also, it significantly improves the external rotation
when combined with simultaneous transfer of the spinal accessory nerve to the suprascapular nerve. Transferring the long head of triceps branch to the axillary nerve through different approaches has been reported (Table 2).2,8,11,13,21,23 In our study, the anterior deltopectoral approach enabled good exposure and access to various donor nerves within close vicinity.
REFERENCES
1. Terzis JK, Barmpitsioti A. Axillary nerve reconstruction in 176 posttraumatic plexopathy patients. Plast Reconstr Surg 2010;125:23347. 2. Colbert SH, Mackinnon SE. Nerve transfers for brachial plexus reconstruction. Hand Clin 2008;24:34161. 3. Van Ouwerkerk WJ, Uitdehaag BM, Strijers RL, Frans N, Holl K, Fellner FA, et al. Accessory nerve to suprascapular nerve transfer to restore shoulder exorotation in otherwise spontaneously recovered obstetric brachial plexus lesions. Neurosurgery 2006;59:85869. 4. Terzis JK, Kostas I. Suprascapular nerve reconstruction in 118 cases of adult posttraumatic brachial plexus. Plast Reconstr Surg 2006;117:61329. 5. Terzis JK, Kostas I, Soucacos PN. Restoration of shoulder function with nerve transfers in traumatic brachial plexus palsy patients. Microsurgery 2006;26:31624. 6. Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul P, Malungpaishrope K. Combined nerve transfers for C5 and C6 brachial plexus avulsion injury. J Hand Surg Am 2006;31:1839. 7. Malessy MJ, de Ruiter GC, de Boer KS, Thomeer RT. Evaluation of suprascapular nerve neurotization after nerve graft or transfer in the treatment of brachial plexus traction lesions. J Neurosurg 2004;101:37789. 8. Bertelli JA, Ghizoni MF. Reconstruction of C5 and C6 brachial plexus avulsion injury by multiple nerve transfers: spinal accessory to suprascapular, ulnar fascicles to biceps branch, and triceps long or lateral head branch to axillary nerve. J Hand Surg Am 2004;29:1319. 9. Merrell GA, Barrie KA, Katz DL, Wolfe SW. Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a meta-analysis of the English literature. J Hand Surg Am 2001;26:30314. 10. Bahm J, Noaman H, Becker M. The dorsal approach to the suprascapular nerve in neuromuscular reanimation for obstetric brachial plexus lesions. Plast Reconstr Surg 2005;115:2404. 11. Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul P. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part II: a report of 7 cases. J Hand Surg Am 2003;28:6338. 12. Ochiai N, Nagano A, Mikami Y, Yamamoto S. Full exposure of the axillary and suprascapular nerves. J Bone Joint Surg Br 1997;79:5323. 13. Bertelli JA, Kechele PR, Santos MA, Duarte H, Ghizoni MF. Axillary nerve repair by triceps motor branch transfer through an axillary access: anatomical basis and clinical results. J Neurosurg 2007;107:3707. 14. Perry J. Biomechanics and functional anatomy of the shoulder. In: Chapman MW, editor. Chapmans orthopaedic surgery. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2001:20632077. 15. Wolock B, Millesi H. Brachial plexus: applied anatomy and operative exposure. In: Gilberman RH, editor. Operative nerve repair and reconstruction. Philadelphia: JB Lippincott; 1991:1255. 16. Broome R. Practical anatomy, clinical assessment and surgical exposure. In: Broome RS, editor. The brachial plexus. New York: Churchill Livingstone; 1977:9. 17. Ball CM, Steger T, Galatz LM, Yamaguchi K. The posterior branch of the axillary nerve: an anatomic study. J Bone Joint Surg Am 2003;85:1497501. 18. Hong TC, Kumar VP, Nather A. The posterior neuromuscular compartment of the deltoid. Plast Reconstr Surg 2005;115:1660 4. 19. Chuang DC, Lee GW, Hashem F, Wei FC. Restoration of shoulder abduction by nerve transfer in avulsed brachial plexus injury: evaluation of 99 patients with various nerve transfers. Plast Reconstr Surg 1995;96:1228. 20. Samardzic M, Rasulic L, Grujicic D, Milicic B. Results of nerve transfers to the musculocutaneous and axillary nerves. Neurosurgery 2000;46:93103. 21. Vekris MD, Beris AE, Pafilas D, Lykissas MG, Xenakis TA, Soucacos PN. Shoulder reanimation in posttraumatic brachial plexus paralysis. Injury 2010;41:3128. 22. Moiyadi AV, Devi BI, Nair KP. Brachial plexus injuries: outcome following neurotization with intercostal nerve. J Neurosurg 2007;107:30813. 23. Lurje A. Concerning surgical treatment of traumatic injury to the upper division of the brachial plexus (Erbs type). Ann Surg 1948;127:31726.
Você também pode gostar
- Multiple Nerve Transfers For The Reanimation of Shoulder and Elbow Functions in Irreparable C5, C6 and Upper Truncal Lesions of The Brachial PlexusDocumento10 páginasMultiple Nerve Transfers For The Reanimation of Shoulder and Elbow Functions in Irreparable C5, C6 and Upper Truncal Lesions of The Brachial PlexusNetravathi EllurAinda não há avaliações
- (OBQ04.162) What Is The Main Blood Supply To The Abductor Digiti Minimi?Documento19 páginas(OBQ04.162) What Is The Main Blood Supply To The Abductor Digiti Minimi?Yoedi YuAinda não há avaliações
- Nerve Transfers To The Biceps and Brachialis Branches To Improve Elbow Flexion Strength After Brachial Plexus InjuriesDocumento6 páginasNerve Transfers To The Biceps and Brachialis Branches To Improve Elbow Flexion Strength After Brachial Plexus InjuriesVina RafmaAinda não há avaliações
- Leech Aveng Von Gs 2016Documento12 páginasLeech Aveng Von Gs 2016Andrés Urrego NietoAinda não há avaliações
- AnatomyDocumento18 páginasAnatomyYoedi YuAinda não há avaliações
- Brachial Plexus InjuryDocumento18 páginasBrachial Plexus InjuryZunnoorain RaeAinda não há avaliações
- Beaulieu J. Y. 2006 Cerebral Plasticity in Crossed C7 Grafts of The Brachial Plexus An fMRI StudyDocumento8 páginasBeaulieu J. Y. 2006 Cerebral Plasticity in Crossed C7 Grafts of The Brachial Plexus An fMRI StudyTatiane SantosAinda não há avaliações
- Brachial Plexus Injury in Adult: Comparative Effectiveness of Anterior and Posterior Approach For Shoulder FunctionDocumento4 páginasBrachial Plexus Injury in Adult: Comparative Effectiveness of Anterior and Posterior Approach For Shoulder FunctionMedical JournalAinda não há avaliações
- Suprascapular Neuropathy in Volleyball Players: Original StudyDocumento4 páginasSuprascapular Neuropathy in Volleyball Players: Original StudyborninbrooklynAinda não há avaliações
- Fractures of The Scapular Neck: Diagnosis, Classifications and TreatmentDocumento11 páginasFractures of The Scapular Neck: Diagnosis, Classifications and Treatmentsoheil ostovanAinda não há avaliações
- Songcharoen 1995Documento5 páginasSongcharoen 1995Le Manh ThuongAinda não há avaliações
- Unstable Burst Fractures of The Thoraco-Lumbar Junction TreatmentDocumento8 páginasUnstable Burst Fractures of The Thoraco-Lumbar Junction TreatmentRafael Jardim de MouraAinda não há avaliações
- Svoa Ne 02 020Documento10 páginasSvoa Ne 02 020Trina ViskhawatAinda não há avaliações
- Aaos 2002Documento120 páginasAaos 2002Yusufa ArdyAinda não há avaliações
- Jain Extrapleural ApproachDocumento5 páginasJain Extrapleural ApproachOj AlimbuyuguenAinda não há avaliações
- Paid Orthobullet MCQs - Trauma PDFDocumento316 páginasPaid Orthobullet MCQs - Trauma PDFMohamad Ramadan100% (2)
- Burst Fracture FinDocumento11 páginasBurst Fracture Finbosnia agusAinda não há avaliações
- Mayer 2018Documento7 páginasMayer 2018Mirna Gallardo ValderramaAinda não há avaliações
- Pedicle Screw Fixation in Fracture of Thoraco-Lumbar SpineDocumento21 páginasPedicle Screw Fixation in Fracture of Thoraco-Lumbar SpineNiyati SharmaAinda não há avaliações
- Elbow Study 1Documento8 páginasElbow Study 1Prashant SurtiAinda não há avaliações
- Loukas Et Al-2013-Clinical AnatomyDocumento3 páginasLoukas Et Al-2013-Clinical AnatomyChrissAinda não há avaliações
- Neurofibromatosis Pada Tulang BelakangDocumento8 páginasNeurofibromatosis Pada Tulang Belakangdadakan16Ainda não há avaliações
- AAOS2003 SpineDocumento61 páginasAAOS2003 SpineHizkyas KassayeAinda não há avaliações
- AAOS2002 ShoulderDocumento70 páginasAAOS2002 ShoulderHéctor Pando SánchezAinda não há avaliações
- Innervation The Human Shoulder Joint and Its Implications For SurgeryDocumento6 páginasInnervation The Human Shoulder Joint and Its Implications For SurgerymitroisergiuAinda não há avaliações
- Obstetric Brachial Plexus Injury: Prof. Mira Sen (Banerjee) C.M.E. ArticleDocumento34 páginasObstetric Brachial Plexus Injury: Prof. Mira Sen (Banerjee) C.M.E. ArticleAdhi HermaAinda não há avaliações
- Pre-Ganglionic Brachial Plexus InjuryDocumento34 páginasPre-Ganglionic Brachial Plexus InjuryZach OkhahAinda não há avaliações
- NeuralRegenRes102328-144177 040017Documento6 páginasNeuralRegenRes102328-144177 040017Le Manh ThuongAinda não há avaliações
- Position Paper For Orthogonally-Based Upper Cervical Chiropractic CareDocumento11 páginasPosition Paper For Orthogonally-Based Upper Cervical Chiropractic CareRodrigo LimaAinda não há avaliações
- Tendon Transfer For Radial Nerve Palsy: Michael E. Rettig, MD, and Keith B. Raskin, MDDocumento12 páginasTendon Transfer For Radial Nerve Palsy: Michael E. Rettig, MD, and Keith B. Raskin, MDFernando Martín Arce AlvaAinda não há avaliações
- Double Crush SyndromeDocumento6 páginasDouble Crush SyndromemesrickAinda não há avaliações
- Spinal Cord Injury - NeuroanatomyDocumento12 páginasSpinal Cord Injury - Neuroanatomyapi-425897805Ainda não há avaliações
- Clune Al Nerve 20Documento20 páginasClune Al Nerve 20ironbody4lifeAinda não há avaliações
- Spine Ant CompDocumento6 páginasSpine Ant CompSadashivayya SoppimathAinda não há avaliações
- Anterior Interosseuos Nerve Transfer To The Motor Branch of The Ulnar Nerve - HaaseDocumento6 páginasAnterior Interosseuos Nerve Transfer To The Motor Branch of The Ulnar Nerve - HaaseJoaquin GarciaAinda não há avaliações
- 264 2005 Article 52Documento4 páginas264 2005 Article 52novera wardaliaAinda não há avaliações
- Edx Braquial PlexusDocumento30 páginasEdx Braquial PlexusMariana GAinda não há avaliações
- Adult Brachial Plexus InjuryDocumento13 páginasAdult Brachial Plexus Injurysunshine bloomAinda não há avaliações
- Adult Traumatic Brachial Plexus InjuriesDocumento15 páginasAdult Traumatic Brachial Plexus Injuriesapi-241264935Ainda não há avaliações
- Low Thoracic Erector Spinae Plane Block For PeriopDocumento10 páginasLow Thoracic Erector Spinae Plane Block For Periopmelanicahyani4646Ainda não há avaliações
- Spinal Anatomy & Surgical ApproachesDocumento37 páginasSpinal Anatomy & Surgical Approachestachyonemc2Ainda não há avaliações
- Kam 2018Documento11 páginasKam 2018JT DanielsAinda não há avaliações
- Brachial Plexus InjuriesDocumento46 páginasBrachial Plexus Injuriesnams orthoAinda não há avaliações
- J Jhsa 2017 10 014Documento5 páginasJ Jhsa 2017 10 014Nicolas AdrianoAinda não há avaliações
- Ultrasound-Guided Block of TheDocumento6 páginasUltrasound-Guided Block of Theandrew herringAinda não há avaliações
- Use of Reverse Lateral Arm Flap For Coverage of Elbow in Burn PatientsDocumento3 páginasUse of Reverse Lateral Arm Flap For Coverage of Elbow in Burn PatientsPalwasha MalikAinda não há avaliações
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocumento37 páginasOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreYoAmoNYCAinda não há avaliações
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocumento37 páginasOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreabctutorAinda não há avaliações
- An Anatomic Arthroscopic Description of The Hip Capsular Ligaments For The Hip ArthroscopistDocumento9 páginasAn Anatomic Arthroscopic Description of The Hip Capsular Ligaments For The Hip Arthroscopistxekar59382Ainda não há avaliações
- Kim 2009Documento5 páginasKim 2009ĐàoQuỳnhNhưAinda não há avaliações
- Doi 1 and 2Documento11 páginasDoi 1 and 2zia malikAinda não há avaliações
- (Journal of Neurosurgery - Spine) The Lateral Extracavitary Approach To The Thoracolumbar Spine - A Case Series and Systematic ReviewDocumento10 páginas(Journal of Neurosurgery - Spine) The Lateral Extracavitary Approach To The Thoracolumbar Spine - A Case Series and Systematic Reviewkarine cim assençoAinda não há avaliações
- Yulisa 2Documento7 páginasYulisa 2Ardi WidiatmikaAinda não há avaliações
- Implications For The Treatment of Chronic HeadachesDocumento5 páginasImplications For The Treatment of Chronic HeadachesCloé SzcAinda não há avaliações
- 2010 Lateral Root of Ulnar NerveDocumento4 páginas2010 Lateral Root of Ulnar Nerve정광익Ainda não há avaliações
- Intrathoracic Fracture-Dislocation of The Humeral Head: A Case ReportDocumento4 páginasIntrathoracic Fracture-Dislocation of The Humeral Head: A Case ReportRachmawan WijayaAinda não há avaliações
- Fagan 2004Documento11 páginasFagan 2004Hari25885Ainda não há avaliações
- Anatomy and Landmarks For Branches of The Brachial Plexus: A Vade MecumDocumento10 páginasAnatomy and Landmarks For Branches of The Brachial Plexus: A Vade MecumRocoso StonesAinda não há avaliações
- Anaesthesia For Shoulder Surgery 5: Alain Borgeat Georgios EkatodramisDocumento15 páginasAnaesthesia For Shoulder Surgery 5: Alain Borgeat Georgios EkatodramisMathew MattAinda não há avaliações
- World's Largest Science, Technology & Medicine Open Access Book PublisherDocumento26 páginasWorld's Largest Science, Technology & Medicine Open Access Book PublisherNetravathi EllurAinda não há avaliações
- Biaxial Serial Excision' or Polyaxial Serial Excision'Documento3 páginasBiaxial Serial Excision' or Polyaxial Serial Excision'Netravathi EllurAinda não há avaliações
- Heart Rate TrainingDocumento3 páginasHeart Rate TrainingNetravathi EllurAinda não há avaliações
- Maneesha PanchakamDocumento106 páginasManeesha PanchakamHimalayanWisdom100% (6)
- Peripheral Nerves and Plexus. QuestionsDocumento33 páginasPeripheral Nerves and Plexus. QuestionsAmanuelAinda não há avaliações
- Mri Price ListDocumento2 páginasMri Price ListsafasayedAinda não há avaliações
- Pectoral MusclesDocumento28 páginasPectoral MusclesShivanshu BhardwajAinda não há avaliações
- Rehab Plan UclDocumento5 páginasRehab Plan Uclapi-709811480Ainda não há avaliações
- Vertical Humeral Osteotomy For Stem Revision in Total Shoulder ArthroplastyDocumento5 páginasVertical Humeral Osteotomy For Stem Revision in Total Shoulder ArthroplastyngoyalnAinda não há avaliações
- Poster Trigger PointDocumento2 páginasPoster Trigger Pointcarne2394% (51)
- Upper Extremity Rom NormsDocumento3 páginasUpper Extremity Rom Normsapi-336924644Ainda não há avaliações
- Fracture Classifications in Clinical Practice PDFDocumento132 páginasFracture Classifications in Clinical Practice PDFAkbar Khan100% (1)
- Upper Extremity Nerve Blocks: Transducer Placement Ultrasound Imaging Cross-Sectional AnatomyDocumento1 páginaUpper Extremity Nerve Blocks: Transducer Placement Ultrasound Imaging Cross-Sectional Anatomyana salasAinda não há avaliações
- Surgical ApproachDocumento124 páginasSurgical ApproachHendra AjahAinda não há avaliações
- MC ScriptDocumento3 páginasMC ScriptKathrina Doroneo (rina)Ainda não há avaliações
- Activity Analysis Sample PedrettiDocumento4 páginasActivity Analysis Sample PedrettiLenard Yel FernandezAinda não há avaliações
- Frozen Shoulder - Loss of Scapulohumeral RhythmDocumento9 páginasFrozen Shoulder - Loss of Scapulohumeral RhythmWasemBhatAinda não há avaliações
- Bones Flash CardDocumento22 páginasBones Flash CardMiki AberaAinda não há avaliações
- Exercise-7C - Answer Sheet Group-3Documento3 páginasExercise-7C - Answer Sheet Group-3Ma. Glaiza MarifosqueAinda não há avaliações
- Joint Mobilization AssignmentDocumento6 páginasJoint Mobilization AssignmentPC LaptopAinda não há avaliações
- Forearm Fractures PDFDocumento4 páginasForearm Fractures PDFNur Ashriawati BurhanAinda não há avaliações
- Week 10:title: Drill That Will Further Develop The Skill in Playing Volleyball. DrillsDocumento13 páginasWeek 10:title: Drill That Will Further Develop The Skill in Playing Volleyball. DrillsMarvin OccianoAinda não há avaliações
- The Evolution of The Human HandDocumento16 páginasThe Evolution of The Human HandDaran EdwardAinda não há avaliações
- The Clinical Anatomyof CrucifixionDocumento11 páginasThe Clinical Anatomyof CrucifixionAntonio José Martínez GámezAinda não há avaliações
- IB Singh - Textbook of Human Osteology, 3rd Edition PDFDocumento350 páginasIB Singh - Textbook of Human Osteology, 3rd Edition PDFKeerthanKp86% (14)
- King I C - How To Use Jiu JitsuDocumento25 páginasKing I C - How To Use Jiu JitsuRodre PalmuAinda não há avaliações
- A Clinicians Guide To The Active Movement Scale (AMS)Documento14 páginasA Clinicians Guide To The Active Movement Scale (AMS)Bow Bow PhysioAinda não há avaliações
- Shoulder Injuries in Dogs - Ridge ReferralsDocumento5 páginasShoulder Injuries in Dogs - Ridge ReferralsZullyAinda não há avaliações
- Swimming Warm Up StretchesDocumento9 páginasSwimming Warm Up StretchesMark CastreyAinda não há avaliações
- Axillary Node DissectionDocumento71 páginasAxillary Node DissectionKartik Kaistha100% (1)
- Suprascapular Neuropathy in Volleyball Players: Original StudyDocumento4 páginasSuprascapular Neuropathy in Volleyball Players: Original StudyborninbrooklynAinda não há avaliações
- Presentation1 150221070554 Conversion Gate01Documento75 páginasPresentation1 150221070554 Conversion Gate01yellymarlianapatuAinda não há avaliações
- Shoulder MobilizationsDocumento33 páginasShoulder MobilizationsEASHWARAinda não há avaliações
- Nyeri Pada Tennis Elbow Tipe IIDocumento14 páginasNyeri Pada Tennis Elbow Tipe IIlisaAinda não há avaliações