Escolar Documentos
Profissional Documentos
Cultura Documentos
Brisbane, 11th October 2008
Enviado por
Ywagar YwagarDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Brisbane, 11th October 2008
Enviado por
Ywagar YwagarDireitos autorais:
Formatos disponíveis
Brisbane, 11th October 2008
1. Cranial nerve Exam in Head injury 2. Viral rash with arthralgia 3. PROM, 30 weeks 4. Urge Incontinence 5. Celiac disease 6. Fever in Neonate 7. Bee Sting 8. Panic attack 9. Antipsychotic side effect 10. ? Peritonsillar abscess with trismus 11. Breaking Bad news (Bowel Ca) 12. Iron Deficiency Anaemia 13. Post op Fever 14. Multinodular goitre 15. Pneumonia 16. CVS risk factors 1. Euthyroid multinodular goitre Yong girl in her 20s, 2nd presentation to your GP, previously saw your colleague who organized blood test and US. The results are as below: TFT with normal TSH and T4 US showing multinodular goitre. Task: Discuss treatment and its complications with patient. It was an easy case but the exam stress makes even simple things very hard. I went inside, greeted patient and told her the blood results. As she is euthyroid I would not start any medicines on her. I asked her about various symptoms to see if she is having any problem. She was wearing scarf around her neck and was worried about the cosmetic appearance, nil other complaints. I advised her regarding referral to endocrinologist and surgery and complications like: Infection, Bleeding, Injury to laryngeal nerves causing hoarseness, Damage to Parathyroid glands. I also told her that I will follow her further and arrange TFT in future to make sure she is not having hyperthyroidism and in that case I will start anti thyroid drugs like PTU and carbimazole. I was not confident in my approach and examiner asked me if i would like to do some tests. I said anti-thyroid antibodies and then I stopped and said they are for Graves not MNG. Probably he was hinting me on FNAC or nuclear scan but none of them crossed my mind and I did not mention a word about it. Could someone please tell me if it coud be critical error not to further investigate. But I did refer her to specialist. Management of Euthyroid Multinodular Goiter Multinodular goiter, a relatively common condition, has a multifactorial etiology and demonstrates a female predominance. Most multinodular goiters are slow-growing and asymptomatic. These require no operative intervention unless there is a suspicion of
malignancy. Patients with multinodular goiters present for medical management predominantly due to cosmetic concerns or compression of adjacent structures, most notably the trachea, the esophagus, or the large veins of the neck. These patients require a thorough clinical assessment, including noting the position of the trachea, checking for the presence of inspiratory or expiratory stridor, and distension of neck veins or dysphagia. If a dominant nodule is present then fine-needle aspiration is indicated to rule out malignancy. Current evidence suggests that the incidence of unsuspected malignancy within multinodular goiters may be higher than previously reported. As stated, the indications for treatment of a multinodular goiter include compression-induced symptoms, hyperthyroidism, suspected malignancy, and, in some instances, cosmetic concerns. Suppression has been attempted by various clinicians using exogenous T4 (e.g., Synthroid). The likelihood of affecting the size of the multinodular goiter, however, is exceedingly small with T4 suppression. The therapeutic use of radioactive iodine has also been proposed by some clinicians. However, unless the patient has a hyperfunctioning nodular goiter (Plummer's disease), radioactive iodine does not represent appropriate management of these patients. Surgical resection represents the treatment of choice for the majority of patients with multinodular goiter. Options include selective resection of the pathologic tissue, bilateral subtotal thyroid lobectomy, and total thyroidectomy. It has been our policy to perform a total thyroidectomy for patients with multinodular goiter with bilateral disease, or total lobectomy with resection of the isthmus in the minority of patients who have a unilateral nodular goiter. We and others feel that total thyroidectomy can be performed safely and with a morbidity comparable to that of lesser resections. A subtotal thyroidectomy has the potential for the development of recurrent goiter and the increased surgical morbidity associated with reoperation, or, in the case of an unsuspected malignancy, the possibility of performing a less than adequate resection. Although subtotal resection can be performed if the surgeon is less experienced and concerned about potential complications (such as recurrent laryngeal nerve injury), a total thyroidectomy is certainly a reasonable procedure and a more definitive treatment for this disease.
2. Simple case of examining head and CN in patient who came after MVA. He is stable now and spine is ok. No further Hx, only examination. I started it really well and I think I spent oo much time looking at the head for lacerations, bruises, sinus tenderness, and asked examiner re otoscopy and fundoscopy, which he said was normal. Rest I could not finish and bell rang when I was about to test 9th and 10th nerve. Do you think the examiner would fail me for not completing the task. I will send you more soon Please if someone could advise me Getting our result tomorrow but cant stop thinking about it.
3. Q: Young man in late 20s presented with cough and SOB for few days. Also complained of chest pain. Sputum rust coloured. Feeling hot and cold. Temperature was 38.something,O2 saturation 93%,tachycardiac and tachypneic. Task: Focussed Hx Ex findings from examiner Ix and Mx My differentials were pneumonia, pneumothorax, pleural effusion. On Hx, it sounded more like pneumonia. He was non smoker, nil other significant medical history. On asking the examiner about Ex finding, there was reduced air entry in rt middle lobe with percussion dullness in the same area. Nil wheezes , Crepts? Xray was given on asking and it had a clear picture of middle lobe consolidation. I advised that it is pneumonia, need to admit him because of poor saturation. Start IV antibiotics and rest Ix like sputum and blood test. Imp: Ask about allergy as he was allergic to penicillin, so I said ceftriaxone and one more antibiotic to cover atypical pneumonia. I passed this station.
4. Q: A man in his late 30s presented with fever and polyarthralgia with a generalized maculopapular rash all over body(picture provided). Task: Focussed hx, Ix, Ex and Mx It is very important to think about DD when you are outside the room so that you dont miss anything in history. My differentials were IM, HIV, Hepatitis, Ross river virus. IM: no sore throat, on Ex no findings in ENT, no hepatomegaly, no splenomegaly. HIV and Hepatitis: no abnormal sexual Hx, happily married man, no IV drug abuse, no loss of appetite, no weight loss. Ross river Virus: Hx of recent travel to North Australia last week, unwell since then. All joints were tender but no arthritis like deformity. Lymphadenopathy? Ix: FBC, Serology for Hepatitis, EBV and ross river virus. Mx: antipyretics, pain killers, ample fluid, good diet. Important to follow him up so I said I would like to see you soon after your results are back and if your condition gets worse, come to see me immediately. No antibiotics required as yet. I passed this station.
5. Q: Peritonsillar abscess. It was a young female, C/o sore throat for few days, painful swallowing, GP gave antibiotics but not getting better. Task; Hx, Ex, Ix, Mx.
It was a typical History of sore throat. Febrile with high temp. LN palpable. Examiner provided a picture of throat on asking about examination. The picture was not clear and the examiner said it is hard to open the mouth fully. The picture showed only rt tonsil and uvula. The tonsil was red, big and bulging but no pus. Looked like an abscess. I advised to admit the patient as the abscess needs to be drained. To start IV antibiotics. Other blood tests ordered.
6. Q: A young girl coming for prescription of anti-psychotics as she had run out of the medicine. On presentation, you saw tremors. She was recently admitted to hospital for severe depression with severe delusion. Task: Focused Hx and Ex and Mx. I did not do this too well but I passed. Because of previous severe attack, it is important to admit and change her medicines because of relapse. Ex for EPS includes checking tone, power and reflexes of the arm and gait. Prepare it well but the examiners are nice and I think they can see that you know what you are doing and saying.
Paediatrics 1. Q: 4 year old boy bib father after bee sting. Vitals normal, swelling of the leg where bee stung and generalized itchy rash. Had previous episode of bee stung where he only developed swelling of the feet. Nil allergies, nil other medical problem. In the scenario it was not mentioned if it is a GP set up or ED. So be cautious. Task: Immediate management and subsequent management I went inside, shook hand with father and examiner. Asked examiner about vitals and he said child is stable. I told father i would like to keep him in observation for 4 to 6 hours as his condition might get worse. Give him anti histamine for allergic reaction. It is not anaphylaxis but only allergic. Subsequent Mx same as for anaphylaxis. Gave Epipen and advised father that as 2nd episode was worse than 1st one, it is possible that the next one could be even worse. gave alert bracelet, education regarding protection from bees, make sure no bee nests near playing areas.
2. Q:18 month baby with failure to thrive that is weight and height less than normal. Nil medical problems. task: Hx, Ex, Ix and Mx The scenario was changed for different candidates. The role player gave the history relevant to Coeliac disease and to others it was more like cow milk enteropathy. For me it was typical coeliac disease. Started since weaning. Likes toast, less milk. Family Hx of brother in law on special diet since childhood. It is imp to advise mum that confirmatory Ix is biopsy besides
other blood test and stool culture. Fully immunized. Mx is special diet, refer to dietician and gastroenterologist for biopsy and further management. It is a lifelong condition and has to avoid wheat/oat/rye/barley. (AMC feedback: celiac disease)
3. Q: 4 month baby bib mother because of temperature and lethargic, irritable, reduced feed. Peripheries are botchy and not well perfused. Task: Hx, Ix, Ex and Mx. The mother was very weird and rude. On asking about immunization she said "what is that". I said they are the injection given to babies to prevent serious infections. She was totally ignorant about it and said whatever. It is a typical sepsis case. I told mum that she her baby is at serious risk, especially cos he is not immunized. She said, "are you blaming me for that". I was really scared that I should not have said that. But I handled the situation well saying I am not blaming you but its just that she is at high risk. After she is well, I'll follow you for her immunization as it is not too late. When I advised that she needs to go to the hospital now, she said I've travelled so far to see you and now I have to catch another train. She was not happy about it. Then I suggested that I will call the ambulance. She was happy. I think she was giving me hint to call the ambulance. Regarding IV antibiotics i said that if ambulance is going to be long I have to give him antibiotic now and take the bloods too. Overall a typical case from AMC handbook but with immunization problem.
Obs and Gyne 1. Q: Post vaginal hysterectomy. Inpatient, 3rd post op day, Spiking temperature today. Task: Hx, Ix, Ex and Mx I was not expecting to pass this station but thanks to the examiner. The patient was very worried that she was recovering well and how come she had sudden temp. There were notes provided regarding physical obs, urine output and fluid input. No urinary symptoms, chest clear. On examination there was tenderness in the suprapubic region but no mass palpable. Per speculum exam normal. I did not ask for PV examination and did not order ultrasound. But I did mention, there could be some infection at the surgical site. I will order some blood test and will see you soon. Examiner asked how soon, I said when the blood results are back, in couple of hours. I must have been really lucky to pass this station. Other candidates said it was a case of pelvic abscess. But please ask someone else.
2. Q: Premature rupture of membrane at 30 weeks in primi mum. Leaking clear fluid.
Task: Hx, Ex, Ix, Mx It happened yesterday after sex. Little amount of fluid oozing out. No contractions, baby moving. No blood. Antenatal serology normal. US Normal. On examination, vitals stable, SFH corresponding to Gestational age. Head not engaged. FHR 100 and movements present. It was a GP setting and I asked for CTG which was not available. I advised pt to go to the hospital now. She will have an U/S to check amount of amniotic fluid and biophysical profile of baby. If it is minor leakage and rest is all normal, she will be discharged and I will follow her weekly with U/S coz it is important to keep an eye on amount of fluid loss. But if the leakage is more baby has to be delivered and she will be given steroids to mature the lungs.
3. Q: Urge incontinence Typical history with sudden urge to pass urine and she cant control it. Some symptoms of stress incontinence as well. No prolapse and vaginal examination normal. I advised that I will refer her to specialist for urodynamic studies and physiotherapist. After her urodynamic studies are back, we will discuss further Mx.
Você também pode gostar
- Long Case Surgery Exam QuestionDocumento25 páginasLong Case Surgery Exam Questionwhee182Ainda não há avaliações
- USA Physician DirectoryDocumento265 páginasUSA Physician Directorysonukarma321Ainda não há avaliações
- Sept Recall PlabDocumento19 páginasSept Recall PlabDr-Jahanzaib GondalAinda não há avaliações
- Friends Ccs CasesDocumento23 páginasFriends Ccs Casesvivekmo100% (2)
- 1700 Files Explained by DRDocumento224 páginas1700 Files Explained by DRSana NabeelAinda não há avaliações
- Med and Surg RecallDocumento15 páginasMed and Surg RecallSherif ElbadrawyAinda não há avaliações
- Plab Big Mock October 2023Documento89 páginasPlab Big Mock October 2023MASONEJIAinda não há avaliações
- September 2023 Part 3Documento238 páginasSeptember 2023 Part 3Fatinha Lucia FC Pinto100% (1)
- MasterDocumento22 páginasMasterAppu ayyala100% (1)
- AMC-2007 Clinical Examination RecallsDocumento156 páginasAMC-2007 Clinical Examination Recallsbreezingthru100% (1)
- March 2021 USMLE Recalls Actual Exam Questions: Click To Get MoreDocumento8 páginasMarch 2021 USMLE Recalls Actual Exam Questions: Click To Get MoreRushi Shah75% (4)
- OSCE Melb11Nov06Documento7 páginasOSCE Melb11Nov06janaka1022Ainda não há avaliações
- CK 9Documento11 páginasCK 9nreena aslamAinda não há avaliações
- M/DN MIS Intramedullary Femoral Fixation Surgical TechniqueDocumento32 páginasM/DN MIS Intramedullary Femoral Fixation Surgical TechniqueVamby SabidoAinda não há avaliações
- Examination: (Look, Listen, Feel !!!!)Documento13 páginasExamination: (Look, Listen, Feel !!!!)Sherif Elbadrawy100% (1)
- TSRA Review of Cardiothoracic PDFDocumento298 páginasTSRA Review of Cardiothoracic PDFvamshidhAinda não há avaliações
- 68 Important Scenarios For ST 5 PracticeDocumento20 páginas68 Important Scenarios For ST 5 PracticeSalem ELsayed Abdel AzizAinda não há avaliações
- Picu Case StudyDocumento3 páginasPicu Case Studyapi-455545776Ainda não há avaliações
- BrisDocumento9 páginasBrisYwagar YwagarAinda não há avaliações
- BrisDocumento9 páginasBrisYwagar YwagarAinda não há avaliações
- Case Clerking ApendicDocumento15 páginasCase Clerking ApendicMelvin Khung100% (1)
- AMC Clinical Recall 138, Sum 16.2.13Documento15 páginasAMC Clinical Recall 138, Sum 16.2.13AMMARAAinda não há avaliações
- Paces Exam Cases 2nd Version PDFDocumento471 páginasPaces Exam Cases 2nd Version PDFMuntadher Kareem100% (1)
- Anesthesia For EntDocumento44 páginasAnesthesia For EntDrshoaib KhanAinda não há avaliações
- Day 13th October 2023 RecallDocumento12 páginasDay 13th October 2023 RecallprathibaAinda não há avaliações
- May 31Documento6 páginasMay 31Sherif ElbadrawyAinda não há avaliações
- PE Recall AMC ExamDocumento9 páginasPE Recall AMC ExamSherif Elbadrawy100% (1)
- MCQ2 QuestionDocumento100 páginasMCQ2 Question9hjk6wpxyfAinda não há avaliações
- Medicine Long CaseDocumento26 páginasMedicine Long Casewhee182Ainda não há avaliações
- December 2008final FRCA VivaDocumento43 páginasDecember 2008final FRCA Vivajahangirealam100% (2)
- GPDocumento3 páginasGPYwagar YwagarAinda não há avaliações
- Powder PharmaceuticsDocumento58 páginasPowder PharmaceuticskishnapraveenAinda não há avaliações
- Feb 2023Documento11 páginasFeb 2023Parsaant SinghAinda não há avaliações
- Sydney 2008 MarchDocumento8 páginasSydney 2008 MarchYwagar YwagarAinda não há avaliações
- Long Case Mmbs 06 11Documento110 páginasLong Case Mmbs 06 11whee182Ainda não há avaliações
- Recall Brisbane February 2008Documento7 páginasRecall Brisbane February 2008Ywagar YwagarAinda não há avaliações
- Meniere's Disease - Case StudyDocumento3 páginasMeniere's Disease - Case StudyZORANASNAinda não há avaliações
- MED4000Documento28 páginasMED4000eunice_lee_48Ainda não há avaliações
- April 21st Recalls With Approaches and AMC Feedback Recollected From Several Posted MaterialsDocumento6 páginasApril 21st Recalls With Approaches and AMC Feedback Recollected From Several Posted MaterialsqurbanAinda não há avaliações
- Next Step Advanced Medical Coding and Auditing 2017 2018 Edition 1st Edition Buck Test BankDocumento25 páginasNext Step Advanced Medical Coding and Auditing 2017 2018 Edition 1st Edition Buck Test BankAllisonPowersrjqo100% (49)
- Attending Osteomyelitis ModuleDocumento9 páginasAttending Osteomyelitis ModuleMrLarry DolorAinda não há avaliações
- 9 RFTCXDocumento24 páginas9 RFTCXpotnic44Ainda não há avaliações
- 1 A 2018 March RecallsDocumento16 páginas1 A 2018 March RecallsqurbanAinda não há avaliações
- Brisbane February 2008: Peanut Induced AnaphylaxisDocumento7 páginasBrisbane February 2008: Peanut Induced AnaphylaxisYwagar YwagarAinda não há avaliações
- HHD 9 Accident EmergencyDocumento6 páginasHHD 9 Accident Emergencymusy9999Ainda não há avaliações
- Mel 2005 Jun 4 RetestDocumento5 páginasMel 2005 Jun 4 RetestZweAinda não há avaliações
- Clinical Signs in PaediatricsDocumento24 páginasClinical Signs in PaediatricsNURUL AFZA MOHD SHAMSUL KAMALAinda não há avaliações
- Case StudyDocumento3 páginasCase StudyAmila RahmahAinda não há avaliações
- Pathology I Review 10Documento30 páginasPathology I Review 10i_areinamoAinda não há avaliações
- "Don't Take My Breath Away" A Case Presentation On Pneumocystis PneumoniaDocumento20 páginas"Don't Take My Breath Away" A Case Presentation On Pneumocystis PneumoniaNikki DiocampoAinda não há avaliações
- Dha GP 2 July 2018Documento8 páginasDha GP 2 July 2018Nilufar EasminAinda não há avaliações
- 2019 IteDocumento188 páginas2019 IteBHAinda não há avaliações
- Clerk GCPDocumento19 páginasClerk GCPNikki DiocampoAinda não há avaliações
- MS Case PresDocumento33 páginasMS Case PresShaine_Thompso_6877Ainda não há avaliações
- Case Report Tuberculous Otitis MediaDocumento23 páginasCase Report Tuberculous Otitis MediahwelpAinda não há avaliações
- Home Assignment I - Adrian Crișan and Istrate Cristian (Series A, Group 4)Documento9 páginasHome Assignment I - Adrian Crișan and Istrate Cristian (Series A, Group 4)Istrate CristianAinda não há avaliações
- TCD Thyroid-6-1Documento72 páginasTCD Thyroid-6-1amrsameerAinda não há avaliações
- Melbourne 14 May 2005: Case 1: Rotator Cuff InjuryDocumento9 páginasMelbourne 14 May 2005: Case 1: Rotator Cuff InjuryZweAinda não há avaliações
- Contoh Soal MCQDocumento13 páginasContoh Soal MCQrororukmiAinda não há avaliações
- Abuajela Sreh - St5 Gastroenterology - Sheffield Teaching Hospitals 1 4 / 0 1 / 2 0 2 2Documento48 páginasAbuajela Sreh - St5 Gastroenterology - Sheffield Teaching Hospitals 1 4 / 0 1 / 2 0 2 2sryh2012Ainda não há avaliações
- Azazim 2012 PDFDocumento27 páginasAzazim 2012 PDFShowmik PaulAinda não há avaliações
- Thornton 2016Documento5 páginasThornton 2016AfdhalRuslanAinda não há avaliações
- Mitral Stenosis Case PresentationDocumento7 páginasMitral Stenosis Case PresentationOM BAWNEAinda não há avaliações
- Metabolic Disease Case Study Learning ActivityDocumento8 páginasMetabolic Disease Case Study Learning ActivityKhali Sciola0% (1)
- Nursing Management of A Patient With: HyperthyroidismDocumento31 páginasNursing Management of A Patient With: Hyperthyroidismember parkAinda não há avaliações
- Acute Hypotonia in An Infant (2017)Documento3 páginasAcute Hypotonia in An Infant (2017)nikos.alexandrAinda não há avaliações
- Walhalla Gold MineDocumento1 páginaWalhalla Gold MineYwagar YwagarAinda não há avaliações
- Clinical Tutorial 2008.11.05Documento31 páginasClinical Tutorial 2008.11.05Ywagar Ywagar100% (1)
- Sydney 2008 MarchDocumento8 páginasSydney 2008 MarchYwagar YwagarAinda não há avaliações
- Recall Brisbane February 2008Documento7 páginasRecall Brisbane February 2008Ywagar YwagarAinda não há avaliações
- Clinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeDocumento14 páginasClinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeYwagar YwagarAinda não há avaliações
- Adelaide, 5 April, 2008: PaediatricsDocumento17 páginasAdelaide, 5 April, 2008: PaediatricsYwagar YwagarAinda não há avaliações
- Brisbane July 2008 RecallDocumento11 páginasBrisbane July 2008 RecallYwagar YwagarAinda não há avaliações
- Draft May 08 WES ProgramDocumento2 páginasDraft May 08 WES ProgramYwagar YwagarAinda não há avaliações
- Adelaide 13th September 2008Documento16 páginasAdelaide 13th September 2008Ywagar YwagarAinda não há avaliações
- Adelaide, 5 April, 2008: PaediatricsDocumento17 páginasAdelaide, 5 April, 2008: PaediatricsYwagar YwagarAinda não há avaliações
- Melb RetestDocumento4 páginasMelb RetestYwagar YwagarAinda não há avaliações
- ACln2007!09!08MEL Retest Wd97Documento6 páginasACln2007!09!08MEL Retest Wd97Ywagar YwagarAinda não há avaliações
- Melbourne 2008 Nov 8Documento10 páginasMelbourne 2008 Nov 8Ywagar YwagarAinda não há avaliações
- Paediatrics:: Case 1nsionDocumento16 páginasPaediatrics:: Case 1nsionYwagar YwagarAinda não há avaliações
- Brisbane February 2008: Peanut Induced AnaphylaxisDocumento7 páginasBrisbane February 2008: Peanut Induced AnaphylaxisYwagar YwagarAinda não há avaliações
- Clinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeDocumento14 páginasClinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeYwagar YwagarAinda não há avaliações
- 15th March 2008 SydneyDocumento3 páginas15th March 2008 SydneyYwagar YwagarAinda não há avaliações
- Melbourne, 9 February 2008: AMC Feedback: Paranoid Schizophrenia (Relapse)Documento13 páginasMelbourne, 9 February 2008: AMC Feedback: Paranoid Schizophrenia (Relapse)Ywagar YwagarAinda não há avaliações
- 3rd May 2008 SydneyDocumento9 páginas3rd May 2008 SydneyYwagar YwagarAinda não há avaliações
- Grammar and VocabularyDocumento2 páginasGrammar and Vocabularythiên bình trầnAinda não há avaliações
- Andrew Eastman Resume 3Documento2 páginasAndrew Eastman Resume 3api-281509868Ainda não há avaliações
- 2012 West Central Ohio Medical Directory - Fall and WinterDocumento64 páginas2012 West Central Ohio Medical Directory - Fall and WinterThe Lima NewsAinda não há avaliações
- Katherine E. Paton Honored As 2018 Professional of The Year in Ocular OncologyDocumento2 páginasKatherine E. Paton Honored As 2018 Professional of The Year in Ocular OncologyPR.comAinda não há avaliações
- 2 1 Acute InflammationDocumento5 páginas2 1 Acute InflammationFaten AwadAinda não há avaliações
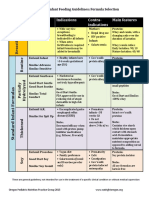
- Formula Selection OPNPGDocumento2 páginasFormula Selection OPNPGRina PratiwiAinda não há avaliações
- Failure Patterns of Different Bracket Systems and Their Influence On Treatment Duration - A Retrospective Cohort StudyDocumento10 páginasFailure Patterns of Different Bracket Systems and Their Influence On Treatment Duration - A Retrospective Cohort StudyHuma SaleemAinda não há avaliações
- Periodic Medical ExaminationDocumento4 páginasPeriodic Medical ExaminationAndreeaRedheadAinda não há avaliações
- Library GenesisDocumento10 páginasLibrary Genesismusic cisumAinda não há avaliações
- The DentistDocumento4 páginasThe DentistuvkiniAinda não há avaliações
- Academic Coach Resource List - Jan 2020Documento2 páginasAcademic Coach Resource List - Jan 2020OsamaAinda não há avaliações
- Evaluation of Primigravida in Labour Using Modified WHO Partograph: Comparative Study of 100 CasesDocumento6 páginasEvaluation of Primigravida in Labour Using Modified WHO Partograph: Comparative Study of 100 CasesShobhitAinda não há avaliações
- AprobacijaDocumento4 páginasAprobacijaMario Marco Del TintorettoAinda não há avaliações
- Anatomy of The KidneyDocumento13 páginasAnatomy of The KidneyChristi NaldoAinda não há avaliações
- Can Rotation PlanDocumento18 páginasCan Rotation PlanMadhuAinda não há avaliações
- Tu IomDocumento10 páginasTu Iomtsc madanpurAinda não há avaliações
- Guideline For Establishing Emergency Medical and Trauma CentersDocumento32 páginasGuideline For Establishing Emergency Medical and Trauma CentersHoussein YoussoufAinda não há avaliações
- ResumeDocumento2 páginasResumeJune TorrionAinda não há avaliações
- February April 2009 Part 2 FRCOphth Examination Final ReportDocumento20 páginasFebruary April 2009 Part 2 FRCOphth Examination Final Reportsafasayed0% (1)
- Managing Medical and Obstetric Emergencies and Trauma A Practical Approach 4Th Edition Rosamunde Burns Editor Full ChapterDocumento65 páginasManaging Medical and Obstetric Emergencies and Trauma A Practical Approach 4Th Edition Rosamunde Burns Editor Full Chaptersteven.webb781100% (4)
- Prevention and Management of Acute Kidney InjuryDocumento30 páginasPrevention and Management of Acute Kidney InjuryIren DawsonAinda não há avaliações
- Case Report: Aesthetic Depigmentation of Gingival Smoker's Melanosis Using Carbon Dioxide LasersDocumento6 páginasCase Report: Aesthetic Depigmentation of Gingival Smoker's Melanosis Using Carbon Dioxide LasersAsy-syifa Brillian AvicennaAinda não há avaliações
- Hospital Management TaskDocumento3 páginasHospital Management TaskJoecelyn AnastasiaAinda não há avaliações
- Mock CodeDocumento4 páginasMock CodeKrezielDulosEscobarAinda não há avaliações