Escolar Documentos
Profissional Documentos
Cultura Documentos
Non Ivasive Lasers Review PDF
Enviado por
Navatha MorthaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Non Ivasive Lasers Review PDF
Enviado por
Navatha MorthaDireitos autorais:
Formatos disponíveis
Oral Maxillofacial Surg Clin N Am 16 (2004) 231 237
A brief overview of noninvasive lasers in cosmetic maxillofacial surgery
Derek K. Boyden, DDS
Olympic Surgical Associates, 450 South Kitsap Boulevard, Suite 2220, Port Orchard, WA 98366, USA
It has been said that the skin is a calendar by which the years can be measured. The search for and maintenance of aesthetic beauty is as ancient as human history [1]. In modern society, this quest may even border on intrusion. By simply observing almost any magazine, newspaper, or television program, we can appreciate the pervasiveness and necessity for beauty in our current culture. Advances have allowed surgeons to provide options to patients that were unheard of only a few years ago. Furthermore, todays cosmetic consumer is savvier than in the past. The plethoric print, television, radio, and Internet information allows these patients to be better educated and aware of what options are available. Of paramount importance for any surgeon who specializes in aesthetics is the optimization of the patients skin appearance. Healthy skin will enhance the surgical result, whereas unhealthy, dyspigmented, wrinkled, rough, or irregular skin will detract from even the most exceptional surgical outcome. Contemporary oral and maxillofacial surgical practices encompass more than dentoalveolar procedures and endosseous implant placement. Todays oral and maxillofacial surgeons are leaders in the evolution of elective cosmetic surgery, routinely performing facial cosmetic surgery, liposculpture, reconstruction, grafting, and augmentation. The advent of botulinum toxins, collagens, and hyaluronic acid injectable fillers is expanding the components of modern full-scope practices. Integral to these practices is skin care and skin enhancement. Through the use of pharmaceutic-grade skin care products, also known as cosmeceuticals or skinceuticals, patients
can improve not only the appearance of the skin but also its health. In conjunction with routine skin care, a number of noninvasive cosmetic laser procedures have become available to further improve the skins health and appearance.
Lasers and laser tissue interactions The principle that any individual laser produces a unique wavelength of light energy is the key to cosmetic laser procedures. Choosing a laser that produces a unique wavelength allows for the targeting of a specific chromophore. Chromophores are any molecules (eg, water, melanin, hemoglobin) that preferentially absorb a given wavelength of the electromagnetic spectrum. Also of importance is the ability to avoid certain chromophores and to minimize undesirable absorption of energy. Another important component of laser tissue interaction is the thermal relaxation time. This is the amount of time that a specific chromophore requires to dissipate one half of the heat generated by a laser pulse. The discovery and appreciation of the differing thermal relaxation times of different chromophores were critical steps forward in the use of noninvasive cosmetic lasers. By controlling the length of the laser pulse and by keeping it below the thermal relaxation time of specific chromophores, unwanted thermal damage to adjacent tissues could be minimized. Laser surgery essentially is the control of where and how much heat injury occurs to achieve a particular outcome (Table 1). There are certain physical properties unique to some devices that allow them to be used in a manner similar to a laser. In particular is the use of an
E-mail address: drboyden@olympicsurgical.com
1042-3699/04/$ see front matter D 2004 Elsevier Inc. All rights reserved. doi:10.1016/j.coms.2004.02.006
232
D.K. Boyden / Oral Maxillofacial Surg Clin N Am 16 (2004) 231237
Table 1 Thermal relaxation time of laser targets Target Basal layer Epidermis Erythrocyte Melanosome Approximate diameter (mm) 20 60 5 1 Thermal relaxation time 400 ms 2 ms 5 ms 0.2 ms
Adapted from Goldman MP, Fitzpatrick RE. Laser treatment of cutaneous vascular lesions. In: Cutaneous laser surgery. 2nd edition. St. Louis (MO): Mosby; 1999. p. 42; with permission.
intense pulsed light system (IPL). IPL is not a true laser, in that the light emitted by this device is noncoherent. IPL lacks a single, uniform, in-phase, light emission. The wavelength of an IPL ranges from 500 to 1200 nm and is selected by choosing one of a variety of interchangeable quartz filters. Due to the variety of wavelengths available (and subsequently, the variety of chromophore targets), IPL has been used to treat numerous cosmetic conditions. For the purposes of this overview, IPL will be included with the true lasers. Many of the lasers used for noninvasive procedures use a cooling medium such as a gel or spray or use contact cooling to minimize epithelial heat damage. The specific medium and techniques will vary between lasers; however, the principle of maintaining the tissue heating time below the tissue thermal relaxation time is universal.
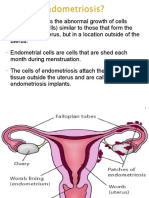
Nonablative skin rejuvenation Aging skin demonstrates many changes including increased laxity, dyspigmentation, telangiectasias, textural irregularities, increased hair growth, and rhytids. Aging skin results from two distinct gross processes: intrinsic aging and photoaging (an indepth discussion of these extensively studied processes is beyond the scope of this article). Rhytids are often the primary presentation for which patients seek cosmetic consultation. Many of the options in a cosmetic surgery practice are directed primarily toward minimizing or eliminating facial wrinkles. There are three general categories of rhytid classification: age-related rhytids, solar-induced rhytids, and expressive rhytids. Although these defects may have a similar appearance, they have been shown to have different histologic presentations [2]. Stated simply, not all wrinkles are created equal. Therefore, the treatment of all wrinkles cannot be approached in an identical fashion. The best cosmetic treatment plan
may be one that uses multiple treatment options. Routine skin care is an important part of most presurgical protocols and equally important in nonsurgical regimens. Many topical skin care products improve skin tone and texture. The development of newer products has led some investigators to examine how topical treatments affect and improve the skins physiologic makeup. For example, Fitzpatrick and Rostan [3] found that topical vitamin C used for 12 weeks resulted in a clinically visible improvement of facial wrinkles. These clinical results were found to correlate with biopsy evidence of new collagen formation. Topical treatments may provide satisfactory improvement in some patients, but for others, nonablative facial rejuvenation allows for more significant improvement. Known by many different trade names depending on the type of laser used, nonablative facial rejuvenation is designed to reduce facial rhytids, improve skin texture, diminish pore size, and ultimately, achieve a younger, healthier appearance (Fig. 1). Lasers that target the hemoglobin chromophore, such as pulsed dye lasers, are believed to release inflammatory mediators through heating of the microvasculature. These mediators may stimulate fibroblasts, resulting in new collagen production and remodeling [4]. Lasers that target water produce nonspecific heating of the upper dermis, with the goal of stimulating new collagen production [5]. Nd:YAG lasers stimulate the dermal and midreticular fibroblasts by thermal stimulation. These methods are truly noninvasive and offer many advantages in an aesthetic maxillofacial practice setting. The lasing procedures are usually performed without anesthesia, although pretreatment with a topical anesthetic may be used. There is no need for wound closure, suction, or evacuation of a laser plume. There is no post-treatment down time. Patients may present for treatment directly from their normal daily activitieseven on their lunch breaks and then return to work or other activities. Postopera-
D.K. Boyden / Oral Maxillofacial Surg Clin N Am 16 (2004) 231237
233
Fig. 1. Nonablative skin rejuvenation. Pretreatment (A) and post-treatment (B) following two treatments with Nd:YAG laser (13 J/cm2, 5-mm spot size, 0.30 milliseconds, and 15,000 pulses each time), 3 weeks apart. Photographs demonstrate diminished vascularity of chin and nasal sill, diminished keratoses on right lip, and improved skin texture. (Photograph property of Olympic Surgical Associates.)
tive pain control medication is unnecessary, and follow-up will generally be limited to the patients next treatment visit.
Infraorbital hyperpigmentation The author successfully has used the following method of treating infraorbital hyperpigmentation or dark circles (Fig. 2): using the Altus Coolglide Nd:YAG laser (Brisbane, California) at 13 J/cm2 with a 5-mm spot size, patients received 750 to 1000 pulses bilaterally in the infraorbital region. The more pulses tolerated by the patient, the better the initial results. Anecdotally, the author found that patients with Fitzpatrick skin types III and IV tolerate many more pulses than patients with Fitzpatrick skin types I and
II. By increasing the fluence to 16 J/cm2, the author is able to deliver more energy to the dermis and improve results. The total time of a given treatment generally is less than 30 minutes, and 3 to 5 treatments may be needed to achieve the desired results. The interval between treatments is 2 to 4 weeks. Protective laser eyeshields or goggles are used. At 1 week following the initial treatment, patients report improvement over the treated area, with the lesser-pigmented areas showing the most remarkable initial improvement. After 3 weeks, the infraorbital region continues to demonstrate normalization of pigmentation. Subsequent treatments at 2- to 4-week intervals bring the lesions to resolution. In addition to improving the appearance of the dark circles, secondary gain in the form of diminished wrinkles, as with nonablative facial rejuvenation, further enhances the final outcome.
Fig. 2. Infraorbital hyperpigmentation. Pretreatment (A) and 3 weeks following initial treatment (B) with Nd:YAG laser (13 J/ cm2, 5-mm spot size, and 400 pulses). (Photograph property of Olympic Surgical Associates.)
234
D.K. Boyden / Oral Maxillofacial Surg Clin N Am 16 (2004) 231237
Although much attention has been drawn to the positive effects of nonablative facial rejuvenation, some investigators have reported that demonstrable clinical improvement is elusive. Leffell [6] reviewed 11 studies based on human clinical trials designed to test the efficacy of nonabalative therapy in reducing wrinkles due to photodamage and found that the studies failed to present consistent data on the efficacy of nonabalative photorejuvenation to improve or eliminate rhytids.
Hair reduction Perhaps one of the most common cosmetic uses of lasers today is for reduction or removal of unwanted hair. Excessive hair growth, particularly within the female facial region, may not be aesthetically pleasing. Although many patients are women seeking treatment for unwanted facial, underarm, leg, or bikini-line hair, increasingly more men also are desirous of hair removal, particularly from the back and shoulder regions (Fig. 4). The original concept of laser hair removal has undergone changes as the science has evolved. Currently, the preferred term to describe this procedure is laser hair reduction. This procedure generally is thought to be consistent with Food and Drug Administration guidelines, which require devices for hair removal to demonstrate a 30% reduction of hair growth at 3 months following a single treatment. Most patients, however, typically will undergo three to five treatments for a given site. The target chromophore for hair removal is melanin. Hair follicles are larger than melanosomes or melanocytes and are better treated with longer pulse durations milliseconds rather than nanoseconds. The long-pulsed ruby (694 nm), alexandrite (755 nm), diode (810 nm), and Nd:YAG (1064 nm) lasers are included in this group. IPL light sources (515 695 nm) also will treat unwanted hair growth. Understanding the growth cycle of human hair is vital to treating excessive hair growth, especially in the head and neck region. Hair comprises fibers made of keratin. The hair follicles are located throughout the skins surface, except for the soles of the feet and the palms of the hands. The number of follicles
Scar treatment The process of postoperative or post-traumatic wound healing is well known. Minimizing scar formation and appearance is critical to achieving optimal surgical results in elective cosmetic surgery. The preplanned placement of incisions within skin folds or creases, oriented parallel to resting skin tension lines, is a time-honored method of minimizing surgical scar appearance. Postoperative wound care is also known to optimize the outcome. Treatment of scarring is dependent on the type of scar present. Use of the previously mentioned, nonablative lasers to stimulate collagen remodeling in hypotrophic scars will help fill in the defect (Fig. 3) [7]. For scars that are hypertrophic in nature, lasers capable of a wavelength in the range of 585 nm are beneficial [7]. Reduction of erythema as well as itching and sensitivity can be seen. Even keloidal scarring may be improved with noninvasive laser treatment. The use of a pulse dye laser, in addition to intralesional steroids, may help minimize the response of fibroblasts [7].
Fig. 3. Scar reduction. Pretreatment (A) and post-treatment (B) following 3 monthly treatments with Nd:YAG laser (13 J/cm2, 0.30 milliseconds, 5-mm spot size, and 650 pulses). (Photograph property of Olympic Surgical Associates.)
D.K. Boyden / Oral Maxillofacial Surg Clin N Am 16 (2004) 231237
235
Fig. 4. Hair removal. Pretreatment (A) and post-treatment (B) of hirsutism following a single session with Nd:YAG laser (57 J/cm2, 10-mm spot size, and 0.20 milliseconds). (Photograph property of Olympic Surgical Associates.)
that an individual has is determined during fetal development, and after parturition, no new follicles are produced. There are two major types of hair: terminal and vellus. Terminal hairs are long, thick, and pigmented. These hairs are found on the scalp, face, eyebrows, chest, back, and genitals. Vellus hair is thinner, shorter, and nonpigmented. The fine hairs found on the forehead are examples of vellus hairs. The hair growth cycle may be divided into three distinct phases: anagen, catagen, and telogen. The active phase of hair growth, anagen, may range from 1 to 2 months on the arm to 5 to 7 years in the scalp. Cataphase is a regression phase. During this stage, cell division stops. The duration of cataphase is approximately 3 weeks. Telogen represents the final phase of the growth cycle. During telogen, the hair falls out and the follicle begins preparation for the development of new hair. This stage lasts 2 to 3 months. Because laser hair removal only works efficiently during the telogen phase, multiple temporally spaced treatments may be needed for successful results. The two major types of excessive hair growth are hypertrichosis and hirsutism. Hypertrichosis is excessive hair growth that is not androgenic in nature. It may occur in both men and women and may be found localized or generalized on the body. Hirsutism is an increased hair growth in unusual places. Changes in androgen production such as those associated with menopause may promote male hair growth patterns including facial hair. Women so afflicted find that the fine vellus hairs become coarse terminal hairs. Although the underlying causes of both hirsutism and hypertrichosis may range from endocrine disorders to tumors to common medications, the author has found that most hair reduction
patients are perimenopausal women. When treating excessive hair growth, women traditionally have used tweezing or plucking, electrolysis, shaving, chemical depilatories, or waxing. The use of these methods produces only temporary hair removal and can result in many possible complications and sequelae including scarring, folliculitis, and infection. Electrolysis is particularly uncomfortable to undergo. The use of lasers for hair removal is not new technology. The first device for laser hair removal was marketed in 1996 [8]. Currently, there are a number of lasers approved for hair removal including Lumens Epilight (Santa Clara, California), Photoderm (Santa Clara, California), Palomar Epilaser (Burlington, Massachusetts), Coherent Light Sheer (Santa Clara, California), Altus Coolglide (Brisbane, California), and Xeo. The target site for follicle destruction is an exogenous chromophore (pigment introduced into the hairshaft) or an endogenous chromophore (melanin within the hairshaft). The thermal relaxation time for terminal hair follicles is estimated to be 10 to 100 milliseconds, depending on size. Longer pulses ( >100 microseconds) seem to cause long-term hair removal [8]. The threshold fluence required to damage the follicles is 40 to 70 J/cm2. The preservation of the epidermis is the critical aspect of patient care when performing laser hair removal.
Vascular lesions The use of various lasers for the treatment of vascular lesions is well known. The literature is replete with studies using Nd:YAG, diode, potassium
236
D.K. Boyden / Oral Maxillofacial Surg Clin N Am 16 (2004) 231237
titanyl phosphate, or pulsed dye lasers, and IPL technology. Because of vessel diameter, depth, flow rate variability, and differences in target chromophores, no single option has been established as a gold standard. The goal of treating vascular lesions is the eradication of the lesion. In some cases (eg, port-wine stains or large hemangiomas), however, simply diminishing the size or severity of the lesion may provide an acceptable cosmetic outcome, even without complete resolution. As with all laser procedures, the selection of the appropriate chromophore is the first step in achieving optimal cosmetic outcomes. The target chromophore for vascular lesions is hemoglobin or red blood cells. An indirect target is the vessel wall. The pulse duration must be long enough to allow conduction of heat from the vessel lumen to the vessel wall. Coagulation of the endothelial layer alone is not sufficient for resolution. As the depth of mural damage progresses from the endothelial layer through the intima and the media to the adventitia, greater success is seen [8]. The absorption spectrum of hemoglobin and oxyhemoglobin has several peaks. Lasers that emit energy absorbed by hemoglobin and oxyhemoglobin (approximately 570 590 nm) will be best suited for treatment of vascular lesions. This group of lasers includes argon, krypton, potassium titanyl phosphate, pulsed dye, and IPL. Use of the long-pulse Nd:YAG laser (1064 nm) also is gaining popularity. This laser takes advantage of a smaller peak of absorption in hemoglobin near this wavelength. This peak also coincides with diminished absorption by the melanin chromophore and, therefore, better penetration to the hemaglobin target. All vesselsfrom lower leg varicosities to peripheral angiomascan be treated with laser technology. The maxillofacial surgeon who primarily treats lesions of the head and neck, however, will encounter mainly facial telangectasias, hemangiomas, port-wine stains, or rosacea. Telangiectasias (spider veins) comprise 90% of the vascular lesions treated in the authors practice. Telangectasias most commonly are seen in patients with Fitzpatrick I or II skin types [9]. Telangiectasias can be grouped into four categories: arborized, papular, simple, and spider [9]. These vessels are found most often to be less than 1 mm in diameter. They represent dilated arterioles, venules, or capillaries. Arteriolar vessels are flat, bright-red lesions, whereas venules are blue and may protrude above the skins surface. Capillary lesions are smallest in diameter and red. They may become larger and change to blue or purple as venous backflow increases hydrostatic pressure [9]. The nose, cheeks (malar eminence),
and chin are the most common sites for patients presenting for treatment. Interestingly, all of these sites are near bony foramina of the skull transmitting named vessels. Using the 3-mm spot size of the Altus Coolglide laser, cutaneous vessels can be removed quickly and comfortably. The Photoderm IPL will also remove facial telangiesctasias; however, because the smallest IPL quartz filter measures 12 8 mm, the surrounding normal tissue must be covered to avoid damage. Cutting a slit or hole in a self-adhesive label or sheet of paper or cardboard is effective in isolating specific sites and minimizing adjacent erythema, purpura, or dyspigmentation. To prevent these undesirable side effects of vascular laser therapy, equipment manufacturers have developed methods for cooling the epidermis. Gel is commonly used, especially with the IPL devices. Lasers with cooling devices come in two varieties: (1) contact cooling, whereby the laser tip maintains contact with the skin; or (2) spray cooling, in which a refrigerant medium is delivered to the target area immediately before the laser pulse [10].
Benign pigmented lesions The cosmetic impact of pigmented lesions in the maxillofacial region can be significant. A lesion may be considered unaesthetic due to any number of specific considerations including size, color, location, or number. Laser treatments provide an excellent au lait option to treat localized dyschromias, cafe macules, lentigines, nevus of Ota, and other pigmented lesions. Differentiating between epidermal and dermal lesions is important in achieving an optimal treatment outcome. Epidermal hyperpigmentation is due to an increased rate of melanogenisis or an increased number of melanocytes. Dermal hyperpigmentation is due to excess melanin deposits in the dermis [11]. An excess of melanin contained within melanosomes will cause hyperpigmentation. Disruption of the melanosome leads to the death of the cell containing it, whether it is a melanocyte, keratinocyte, or melanophage [12]. The spectrum of absorption for melanin is broad: 250 to 1200 nm. Longer wavelengths allow for deeper tissue penetration because melanin absorption decreases as the wavelength increases. Therefore, there are numerous laser options to treat these lesions. Initial laser use for human skin in the early 1960s used a ruby laser with a wavelength of 694 nm. Melanocytes were destroyed, but the outcomes were variable. The argon laser (488 514 nm) was used in
D.K. Boyden / Oral Maxillofacial Surg Clin N Am 16 (2004) 231237
237
an attempt to achieve better results; however, these results also were variable [11]. In fact, even carbondioxide lasers, with their much longer wavelength, may be used to treat superficial pigmented lesions of the skin by simple coagulation of the epidermis. Epidermal lesions may be treated in numerous ways. Lesions confined to the epidermis can be removed by any method that removes the epithelium, such as a carbon-dioxide laser. If the junction of the reticular dermis and the papillary dermis is below the level of tissue injury, then these wounds generally heal without scarring. The use of lasers that emit 488- to 532-nm wavelengths is commonplace. Initial darkening of the lesion is often seen, with clearing in 5 to 10 days. Multiple treatments are sometimes required to achieve resolution. Epidermal lesions au lait macules, such as lentigos, keratoses, cafe and ephelides are treated effectively with laser technology. Deeper lesions such as postinflammatory hyperpigmentation, melasma, and some congenital nevi also can be safely treated with laser therapy.
tory. In addition, local, state, or regional rules and regulations may impact the use of laser technology in any given practice. The noninvasive laser and IPL cosmetic procedures covered in this article are only a few of the uses for lasers in cosmetic maxillofacial surgery. These procedures are part of an overall practice philosophy of which skin care and maintenance is a vital component. In conjunction with prescription skin care products, botulinum toxin, microdermabrasion, injectable fillers, and so forth, these laser procedures provide a comprehensive menu of services for contemporary maxillofacial surgery practices.
References
[1] Coleman III WP, Hanke CW. The history of dermatologic cosmetic surgery. In: Coleman III WP, Hanke CW, Alt TH, et al, editors. Cosmetic surgery of the skin. 2nd edition. Saint Louis (MO): Mosby-Year Book; 1997. p. 1 6. [2] Noodleman F.R. Understanding how skin ages. Plastic Surgery Products 2003. ISSN Number 1084 1660. p. 24. [3] Fitzpatrick RE, Rostan EF. Double blind, half-face study comparing topical vitamin C and vehicle for rejuvenation of photodamage. Dermatol Surg 2002; 28:231 6. [4] Bjerring P, Clement M, Heickendorff L, et al. Selective non-ablative wrinkle reduction by laser. J Cut Las Ther 2000;2:9 15. [5] Goldberg D. Full face nonablative dermal remodeling with a 1320 nm Nd:YAG laser. Dermatol Surg 2000; 26:915 8. [6] Leffell DJ. Clinical efficacy of devices for nonablative photorejuvenation. Arch Dermatol 2002;138: 11503 8. [7] Kilmer SL. Cutaneous lasers. Facial Plast Surg Clin N Am 2003;11:229 43. [8] Dierickx CC. Hair removal by lasers and intense pulsed light sources. Dermatol Clin 2002;20:135 46. [9] Goldman MP, Fitzpatrick RE. Laser treatment of cutaneous vascular lesions. In: Goldman MP, Fitzpatrick RE, editors. Cutaneous laser surgery. 2nd edition. St. Louis (MO): Mosby; 1999. p. 19 178. [10] Lang PG. Laser technology: its application in the management of hemangiomas and vascular malformations for the head and neck. Facial Plast Surg Clin North Am 2001;9(4):577 83. [11] Dover JS, Kane KS. Lasers for the treatment of cutaneous pigmented disorders. In: Arndt KA, Dover JS, Olbricht SM, editors. Lasers in cutaneous and aesthetic surgery. Philadelphia: Lippincott-Raven Publishers; 1997. p. 165 87. [12] Klimer SL. Laser eradication of pigmented lesions and tattoos. Dermatol Clin 2002;20(1):37 53.
Summary As patients become more aware of their options related to facial enhancement, nonsurgical offerings will become an ever larger component of the cosmetic practice. Patients will continue to demand rejuvenating options but will desire a minimum of downtime, discomfort, and invasiveness. The use of traditional skin care approaches such as microdermabrasion, botulinum toxin, injectable fillers, and prescription-grade skin care products will be accentuated by the advances in laser and IPL technology. Using these new technologies effectively, knowledgeably, and safely is crucial for the maxillofacial surgeon to maintain the leading role in facial cosmetic surgery. Currently, dozens of lasers exist for noninvasive cosmetic procedures. This wide range of options, with each option having its own claims of efficacy, superiority, and ease of use, is beyond this review. The reader is encouraged to investigate thoroughly any claims, studies, or promises made by any manufacturer. It is wise to test any equipment in the clinic for as long as possible before purchase. A number of the lasers mentioned in this review are those with which the author has had significant experience. Their inclusion is not an endorsement of any individual type of laser or manufacturer. These technologies are not inexpensive to acquire; a complete understanding of the lasers physics, personnel required, and necessary ancillary supplies is manda-
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Pre-Prosthetic Surgery: Mandible: Ental Science - Review ArticleDocumento4 páginasPre-Prosthetic Surgery: Mandible: Ental Science - Review ArticleAdrian ERanggaAinda não há avaliações
- BMP PDFDocumento17 páginasBMP PDFNavatha MorthaAinda não há avaliações
- Rasmussen Fernhoff Scanlon B12 Deficiencyinchildrenandadolescents JPediatrics 2001Documento9 páginasRasmussen Fernhoff Scanlon B12 Deficiencyinchildrenandadolescents JPediatrics 2001Navatha MorthaAinda não há avaliações
- BMP PDFDocumento17 páginasBMP PDFNavatha MorthaAinda não há avaliações
- Carotido Cavernous Fistula PDFDocumento34 páginasCarotido Cavernous Fistula PDFNavatha Mortha100% (1)
- LGM LGM H 15 11Documento9 páginasLGM LGM H 15 11Nur Ainie PutriAinda não há avaliações
- Collagen Disorders PDFDocumento6 páginasCollagen Disorders PDFNavatha MorthaAinda não há avaliações
- Palatoplasty: Evolution and Controversies: Aik-Ming Leow, MD Lun-Jou Lo, MDDocumento11 páginasPalatoplasty: Evolution and Controversies: Aik-Ming Leow, MD Lun-Jou Lo, MDNavatha MorthaAinda não há avaliações
- Condylar InjuriesDocumento16 páginasCondylar InjuriesNavatha MorthaAinda não há avaliações
- Osteomyelitis Classification Read PDFDocumento33 páginasOsteomyelitis Classification Read PDFNavatha MorthaAinda não há avaliações
- Phisiology of Saliva PDFDocumento12 páginasPhisiology of Saliva PDFNavatha MorthaAinda não há avaliações
- Sailedinitis PDFDocumento8 páginasSailedinitis PDFNavatha MorthaAinda não há avaliações
- CSF Leak 091120Documento9 páginasCSF Leak 091120Ullyaty RachmahAinda não há avaliações
- Fluid Managemnt PDFDocumento11 páginasFluid Managemnt PDFNavatha MorthaAinda não há avaliações
- Alloplastic Reconstruction of The TMJ PDFDocumento20 páginasAlloplastic Reconstruction of The TMJ PDFNavatha Mortha100% (1)
- CSF Leak 091120Documento9 páginasCSF Leak 091120Ullyaty RachmahAinda não há avaliações
- Genioplasty PDFDocumento5 páginasGenioplasty PDFNavatha Mortha100% (1)
- Primary Cleft Lip and Palate Amit PapnejaDocumento5 páginasPrimary Cleft Lip and Palate Amit PapnejaAmit PapnejaAinda não há avaliações
- Jurnal Radiology DentalDocumento10 páginasJurnal Radiology DentalpremolarpAinda não há avaliações
- Thesis DiscussionDocumento6 páginasThesis DiscussionNavatha MorthaAinda não há avaliações
- Thesis MethodologyDocumento4 páginasThesis MethodologyNavatha MorthaAinda não há avaliações
- Biomechanical Comparison of Different Plating Techniques in Repair of Mandibular Angle FracturesDocumento5 páginasBiomechanical Comparison of Different Plating Techniques in Repair of Mandibular Angle FracturesNavatha MorthaAinda não há avaliações
- Cerebrospinal Fluid Rhinorrhoea Diagnosis and ManagementDocumento4 páginasCerebrospinal Fluid Rhinorrhoea Diagnosis and ManagementSukhvinder Singh RanaAinda não há avaliações
- Third Molar Economy PDFDocumento9 páginasThird Molar Economy PDFNavatha MorthaAinda não há avaliações
- Hamangiomas Review PDFDocumento10 páginasHamangiomas Review PDFNavatha MorthaAinda não há avaliações
- Complications Ofthird Molar PDFDocumento4 páginasComplications Ofthird Molar PDFNavatha MorthaAinda não há avaliações
- Impact of 3rd Molar Pain On Oral Health and Quality of Life PDFDocumento7 páginasImpact of 3rd Molar Pain On Oral Health and Quality of Life PDFNavatha MorthaAinda não há avaliações
- JOMS 2004. Risk Factors For 3rd Molar Extraction Difficulty PDFDocumento9 páginasJOMS 2004. Risk Factors For 3rd Molar Extraction Difficulty PDFNavatha MorthaAinda não há avaliações
- Pigmented Lesions Review PDFDocumento16 páginasPigmented Lesions Review PDFNavatha MorthaAinda não há avaliações
- Management of Pregnent Wonan PDFDocumento15 páginasManagement of Pregnent Wonan PDFNavatha MorthaAinda não há avaliações
- Perry2008 2Documento12 páginasPerry2008 2luis castroAinda não há avaliações
- Preoperative & Postoperative EvaluationDocumento61 páginasPreoperative & Postoperative EvaluationSonntagsschule St. Antonius Kloster in KröffelbachAinda não há avaliações
- Development of The Urogenital SystemDocumento37 páginasDevelopment of The Urogenital SystemPatience RimamAinda não há avaliações
- Anatomy ReviewerDocumento5 páginasAnatomy ReviewerPHILYP EPHRAIM PARANGALANAinda não há avaliações
- 295 QsDocumento3 páginas295 Qsujangketul62Ainda não há avaliações
- Renap Update Pre-Kt - MDJDocumento46 páginasRenap Update Pre-Kt - MDJRenalNursesPhAinda não há avaliações
- Case Study Presentation KPJ JohorDocumento131 páginasCase Study Presentation KPJ JohorAmar Nur Arif ZazuliAinda não há avaliações
- Articulo RevisionDocumento8 páginasArticulo RevisionvictorAinda não há avaliações
- Nursing ICUDocumento2 páginasNursing ICUKomal Tomar50% (2)
- CFPC 99 Topics Starter Study DocumentDocumento372 páginasCFPC 99 Topics Starter Study DocumentaayceeAinda não há avaliações
- Lect 32 Unit IV EndometriosisDocumento13 páginasLect 32 Unit IV EndometriosisAsifa BhuttoAinda não há avaliações
- Management of Post Burn ContracturesDocumento65 páginasManagement of Post Burn ContracturesJetto TubeAinda não há avaliações
- Gyne: Abnormal Uterine Bleeding: Structural Abnormalities (PALM)Documento6 páginasGyne: Abnormal Uterine Bleeding: Structural Abnormalities (PALM)M MAinda não há avaliações
- CystosDocumento1 páginaCystosgeorgeloto12Ainda não há avaliações
- Preventive DentistryDocumento3 páginasPreventive DentistryMoataz Mohamed BarakatAinda não há avaliações
- Peripheral, Head and Neck Surgery: Brendon J. Coventry EditorDocumento167 páginasPeripheral, Head and Neck Surgery: Brendon J. Coventry EditorMariaAinda não há avaliações
- Assessment of Right Ventricular FunctionDocumento41 páginasAssessment of Right Ventricular FunctionAditya MadhavpeddiAinda não há avaliações
- GENESIS II Surgical Technique DCFDocumento46 páginasGENESIS II Surgical Technique DCFMazilo VictorAinda não há avaliações
- VAMA Poster DefinitivoDocumento1 páginaVAMA Poster Definitivocedivadenia8084Ainda não há avaliações
- Biopsy Needle For BARD MAGNUMDocumento1 páginaBiopsy Needle For BARD MAGNUMNelson LebronAinda não há avaliações
- IntracranialsurgeryDocumento17 páginasIntracranialsurgeryJona Kristin EnclunaAinda não há avaliações
- Slow Maxillary Expansion: A Comparison Between Banded and Bonded AppliancesDocumento10 páginasSlow Maxillary Expansion: A Comparison Between Banded and Bonded AppliancesmalifaragAinda não há avaliações
- Syngo Velocity Vector Imaging Syngo Velocity Vector Imaging Technology-00163641Documento2 páginasSyngo Velocity Vector Imaging Syngo Velocity Vector Imaging Technology-00163641Duchung TranAinda não há avaliações
- Mastectomy: Presenter: DR Janardhan T Post GraduateDocumento49 páginasMastectomy: Presenter: DR Janardhan T Post GraduateASHUTOSH KUMARAinda não há avaliações
- Basal Cell Carcinoma Workup - Approach Considerations, Skin Biopsy, CytologyDocumento12 páginasBasal Cell Carcinoma Workup - Approach Considerations, Skin Biopsy, CytologyyanuarrisaldiAinda não há avaliações
- ESC Guideline NSTEMI PDFDocumento59 páginasESC Guideline NSTEMI PDFsisrinovritaAinda não há avaliações
- CH 071 Acute Kidney Injury in ChildrenDocumento9 páginasCH 071 Acute Kidney Injury in Childrenarun babuAinda não há avaliações
- HybaseDocumento6 páginasHybaseSreejith SwaminathanAinda não há avaliações
- Post-Op Teaching ProjectDocumento18 páginasPost-Op Teaching Projectapi-283536133Ainda não há avaliações