Escolar Documentos
Profissional Documentos
Cultura Documentos
Myxedema Ascites
Enviado por
Priscila Tobar AlcántarDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Myxedema Ascites
Enviado por
Priscila Tobar AlcántarDireitos autorais:
Formatos disponíveis
J Korean Med Sci 2006; 21: 761-4 ISSN 1011-8934
Copyright The Korean Academy of Medical Sciences
Myxedema Ascites
: Case Report and Literature Review
Myxedema ascites caused by hypothyroidism is rare, so its diagnosis is often delayed and patients frequently receive unnecessary procedures such as liver biopsies and exploratory laparotomies. We report a 71-yr-old man with clinical ascites that was the first manifestation of hypothyroidism, and which resolved completely in response to thyroid hormone replacement therapy. To our knowledge, this is the first report of myxedema ascites in Korea. A review of the literature revealed 51 well-documented cases of myxedema ascites. Analyses of ascites from patients in this condition usually show high protein (>2.5 g/dL) and low white blood cell counts, with a high proportion of lymphocytes. A consistent feature is the good response to thyroid hormone replacement therapy, which has always led to resolution of the ascites. Myxedema ascites is thus rare but easy to treat; it should be borne in mind, especially if the ascites fluid has a high protein content.
Jeong-Seon Ji, Hiun-Suk Chae, Young-Seok Cho, Hyung-Keun Kim, Sung-Soo Kim, Chang-Wook Kim, Chang-Don Lee, Bo-In Lee, Hwang Choi, Kang-Moon Lee, Hye-Kyung Lee*, Kyu-Yong Choi
Departments of Internal Medicine and Pathology*, College of Medicine, The Catholic University of Korea, Seoul, Korea Received : 6 April 2005 Accepted : 27 June 2005
Address for correspondence
Hiun-Suk Chae, M.D. Division of Gastroenterology, Department of Internal Medicine, Uijeongbu St. Marys Hospital, The Catholic University of Korea, 65-1 Gumo-dong, Uijeongbu 480-130, Korea Tel : +82.31-820-3046, Fax : +82.31-847-2719 E-mail : chs@catholic.ac.kr
Key Words : Myxedema; Ascites; Hypothyroidism
INTRODUCTION
Primary hypothyroidism is a common clinical condition, complicated by ascites in less than 4% of cases. Myxedema ascites, caused by hypothyroidism, is also a rare cause of ascites in less than 1% of new onsets (1). There is often a delay in diagnosis, and patients may go undiagnosed for a long time (2). In such cases, the use of thyroid hormone replacement usually leads to a progressive decrease in ascites, which ultimately disappear (3). Therefore, when any patient presents with ascites of uncertain etiology, hypothyroidism should be considered as a differential diagnosis. Here, we report a 71-yr-old man with myxedema ascites that resolved completely with thyroid hormone replacement therapy. This may be the first case reported in Korea.
CASE REPORT
A 71-yr-old man presented with abdominal distension and anorexia that had lasted for 10 days. His past medical history was unremarkable except for prostate surgery for benign prostate hyperplasia six years previously. He did not smoke or drink alcoholic beverages. His blood pressure was 140/90 mmHg, the pulse rate 70 beats/min, and he weighed 55 kg.
761
The patient was alert and oriented. No jugular vein distension was found and a cardiopulmonary examination was unremarkable. The abdomen was markedly distended, with taut skin and a circumference of 85 cm. There was shifting dullness and fluid waves evident on palpation. There was no pretibial edema. His white blood cell count was 5,500 cells/ L, hemoglobin was 10.5 g/dL and platelet count was 165,000/ L. The prothrombin time was 11.2 sec (international normalized ratio, INR, 1.0) and the activated partial thromboplastin time was 28 sec. The serum alkaline phosphatase level was 109 U/L, total bilirubin 1.0 mg/dL, aspartate aminotransferase (AST) 70 U/L, alanine aminotransferase (ALT) 18 U/L, amylase 60 mg/dL, and total cholesterol 185 mg/dL. The total protein level was 5.8 g/dL and albumin 3.3 g/dL. Urinalysis results were normal. Hepatitis B and C serologies were negative. His initial chest radiograph showed normal without findings of cardiomegaly or pulmonary edema. Samples of ascitic fluid showed elevated total protein (3.5 g/dL) and a low serum-to-ascites albumin gradient (SAAG; 0.8 g/dL). These were not characteristics of portal hypertension. The white blood cell count in the fluid was 81/ L, and 84% of the cells were lymphocytes. Gram staining and cytology were negative. Bacterial, fungal and mycobacterial cultures were also negative. Given these negative findings, we performed imaging stud-
762
J.-S. Ji, H.-S. Chae, Y.-S. Cho, et al.
ies to evaluate the possible cause of the ascites. Ultrasonography and computed tomography (CT) of the abdomen revealed massive ascites and a normal-sized liver and spleen (Fig. 1). Esophagogastroduodenoscopy (EGD) disclosed no evidence of portal hypertension such as esophageal varices or gastropathy. A laparoscopic biopsy of the peritoneum and liver was performed to rule out any common cause of high protein, low SAAG ascites such as peritoneal malignancies, tuberculosis or infections. Laparoscopy showed that the surface of the liver was slightly irregular and the peritoneum was normal in appearance. A microscopic examination of the liver biopsy revealed accumulations of yellow bile pigment in the hepatocytes, suggesting intrahepatic cholestasis without findings of liver cirrhosis (Fig. 2). Histology of the peritoneum yielded nonspecific findings.
We then evaluated the possibility of a cardiogenic origin. Echocardiography showed normal sized cardiac chambers, and the patients left ventricular ejection fraction was 54%. However, there was no evidence of congestive heart failure as the cause of the ascites. To prevent activation of the renin-angiotensin-aldosterone system and sodium retention from a vicious cycle of ascites, we prescribed an aldosterone antagonist (spironolactone 50 mg daily) and an inhibitor of proximal renal tubule sodium
Fig. 1. CT of the abdomen showing massive ascites and normalsized liver and spleen.
Fig. 2. Microscopic finding of the liver showing accumulation of yellow bile pigment in the hepatocytes (H&E, 400).
Fig. 3. Thyroid ultrasonograph revealing atrophic change of both thyroid lobes (arrowheads).
Fig. 4. Technetium-99m thyroid scan showing only two small nodular foci in the thyroid bed.
Myxedema Ascites
763
absorption (furosemide 20 mg daily). However, the patients response to diuretics was poor; his body weight decreased by only 1 kg and the abdominal circumference by only 2 cm after diuretic therapy for 10 days. The patient was discharged with a prescription for 20 mg furosemide and 50 mg spironolactone daily, because of his poor financial status. He did not attend the outpatient clinic for another month, when he was readmitted because of his increased abdominal girth. Compared with discharge, his body weight had increased by 3 kg and the abdominal circumference by 5 cm. The ascitic fluid showed elevated total protein and a low SAAG value, as found previously. We decided to evaluate some relatively unusual causes of ascites. We were interested in the high protein component of the ascites fluid, so we performed thyroid function testing. These showed the following values: T3 0.14 nM/L (normal 0.92-2.78 nM/L); T4 6.0 nM/L (normal 58-140 nM/L); free T4 0.13 pM/L (normal 10.3-35 pM/L); and thyroid-stimulating hormone level (TSH) 70.3 mU/L (normal 0.4-5 mU/L). These findings necessitated further thyroid tests. The antimicrosomal antibody titer was 1:102,400 (normal, <1:100) and the antithyroglobulin antibody titer was negative. Ultrasonography revealed atrophic change to both thyroid lobes (Fig. 3), and a technetium-99m thyroid scan revealed only two small nodular foci in the thyroid bed (Fig. 4). Thyroid hormone replacement therapy was started with gradually increasing doses of levothyroxine, from 0.05 mg to 0.15 mg daily to treat the patients hypothyroidism. Over the following three months, he became euthyroid with complete resolution of his ascites, and the liver function tests returned to normal. His body weight decreased by 9 kg and the abdominal circumference was reduced by 28 cm. There has been no recurrence of ascites and his euthyroid condition was maintained over three years of follow-up with levothyroxine 0.15 mg daily. The latest follow-up thyroid function studies showed a free T4 level of 19.3 pM/L and a TSH of 2.7 mU/L.
with portal pressure (4). Ascites fluid associated with portal hypertension shows a low total albumin level, and the SAAG is greater than 1.1 g/dL (high gradient) (5, 6). SAAG is usually high in patients with liver cirrhosis and congestive heart failure. A gradient of <1.1 g/dL (low) usually suggests that the ascites is not caused by portal hypertension. The SAAG is low in patients with peritoneal malignancies, tuberculous peritonitis, pyogenic peritonitis and pancreatic ascites. Therefore, a low gradient ascites should initiate an evaluation for primary peritoneal process, most importantly infections and malignancies. There has been a suggestion that the SAAG may exceed 1.1 in patients with myxedema ascites, based on a review of eight patients (7). Because so few cases have been studied and portal hypertension or heart failure do not seem to be the mechanisms causing ascites in patients with myxedema, we cannot conclude that a high SAAG is a typical feature in this disease (8). Moreover, the patient reported here showed a low SAAG. Portal hypertension secondary to liver cirrhosis is the leading cause of ascites (more than 80% of cases) and peritoneal involvement in patients with malignant diseases is the second at about 10% (9). Therefore, if the composition of ascitic fluid and ultrasonography are not consistent with portal hypertension or other specific diseases, the physician should consider peritoneal malignancy and perform a peritoneal biopsy. If this is negative and the ascitic fluid shows a high protein content, then hypothyroidism should be considered as a differential diagnosis. In this patient, because the SAAG was <1.1 g/dL and there was a lack of esophageal varices or gastropathy on EGD and characteristic findings on ultrasonography, there was no evidence of portal hypertension. Moreover, a peritoneal biopsy showed nonspecific findings. As the ascitic fluid analysis revealed a high protein content, we perTable 1. Characteristics of reported patients with myxedema ascites
Number of Mean Ranges patients Ascites protein (g/dL) 49 3.9 1.8-5.1 Remarks Forty-eight patients (98%) showed ascites protein levels >2.5 g/dL Because of the small number of patients, the characteristics were unclear Predominance of lymphocytes (mean 81%)
DISCUSSION
Hypothyroidism is a relatively rare cause of ascites. However, the importance of its diagnosis is that use of thyroid hormone replacement results in complete resolution. If there is new onset ascites, diagnostic workup should begin with the analysis of ascitic fluid. Usually total protein in the ascitic fluid and the SAAG value give a useful framework for analysis of whether the ascitic fluid is a transudate or an exudate. The total protein in the ascitic fluid was >2.5 g/dL in the exudate and <2.5 g/dL in the transudate. Of the various causes, peritoneal malignancies, tuberculous peritonitis, pyogenic peritonitis and pancreatic ascites can all lead to high-protein ascites. Patients with liver cirrhosis and congestive heart failure show low protein ascites. The SAAG correlates directly
SAAG (g/dL)
11
1.5
0.8-2.3
Ascites WBC count (per L) Duration of ascites
48
60
10-400
51
8 1 month months to 8 yr Regression of ascites
Response to treatment 51
SAAG, serum-to-ascites albumin gradient; WBC, white blood cell.
764
J.-S. Ji, H.-S. Chae, Y.-S. Cho, et al.
formed thyroid function testing, which proved decisive. A review of the literature turned up 51 well-documented cases of myxedema ascites (Table 1) (2, 3, 7, 8, 10-20). A very consistent finding was the high total protein level (>2.5 g/ dL) (7). Total protein levels exceeded 2.5 g/dL in almost all cases, with a mean of 3.9 g/dL. The mean SAAG was 1.5 g/ dL with a range of 0.8-2.3 g/dL. White blood cell counts were rather low, usually with a predominance of lymphocytes; the mean white blood cell count was 60/ L with a mean of 81% lymphocytes. In our patient, white blood cell count was 81/ L and lymphocyte proportion, 84%. There was usually a significant delay in the diagnosis, with a mean of eight months. Prompt recognition of myxedema ascites prevents the inappropriate use of diuretics and unnecessary procedures, including repeated paracenteses, liver biopsies and exploratory laparotomies (10). A constant feature was the good response to thyroid hormone replacement therapy, which led to elimination of the ascites in every instance. The mechanism of ascites fluid formation in patients with myxedema is unclear. There are two main hypotheses. The first is that low levels of circulating thyroid hormones cause increased extravasation of plasma proteins because of abnormal capillary permeability and the lack of a compensatory increase in lymph flow and protein return rate (21). The second hypothesis is that hyaluronic acid accumulates in the skin and produces edema by a direct hygroscopic effect. However, hyaluronic acid has only been found in minute quantities in patients with myxedema ascites: not large enough to exert a direct hygroscopic effect. However, it could interact with albumin to form complexes that prevent the lymphatic drainage of extravasated albumin (22). To our knowledge, this is the first report of myxedema ascites in Korea. Although the diagnosis was delayed for about one and half months, treatment by thyroid hormone replacement medication led to complete regression of the ascites and normalization of liver function in this patient. In conclusion, myxedema ascites is rare but easy to treat. Treatment with thyroid hormone replacement therapy leads to complete regression of the ascites. A very prominent feature in such cases is the high total protein level (>2.5 g/dL). Once routine evaluation of ascites excludes common causes such as liver cirrhosis, peritoneal malignancies and infections, congestive heart failure and pancreatic ascites, thyroid function tests should be performed on patients with high protein levels in the ascites fluid.
REFERENCES
1. Watanakunakorn C, Hodges RE, Evans TC. Myxedema: a study of 400 cases. Arch Intern Med 1965; 116: 183-90. 2. McDonough CH, Lee L, de Beur SJ, Arai S, Vogelsang GB. Myxede-
ma ascites in the posttransplant setting: case report. Am J Hematol 2002; 71: 216-8. 3. De Feudis L, Scudieri M, Orlando D, Traisci G. Ascites as preeminent manifestation of primary hypothyroidism: clinical case. Ann Ital Med Int 1999; 14: 294-7. 4. Hoefs JC. Serum protein concentration and portal pressure determine the ascitic fluid protein concentration in patient with chronic liver disease. J Lab Clin Med 1983; 102: 260-73. 5. Rector WG Jr, Reynolds TB. Superiority of the serum-ascites albumin difference over the ascites total protein concentration in separation of transudative and exudative ascites. Am J Med 1984; 77: 83-5. 6. Hoefs JC. Diagnostic paracentesis: a potent clinical tool. Gastroenterology 1990; 98: 230-6. 7. de Castro F, Bonacini M, Walden JM, Schubert TT. Myxedema ascites: report of two cases and review of the literature. J Clin Gastroenterol 1991; 13: 411-4. 8. Otero Bedoya J, Landeira G, Corino M, Tamashiro A, Fassio E. Ascites due to hypothyroidism in a patient with alcoholic cirrhosis. Acta Gastroenterol Latinoam 2001; 31: 77-81. 9. Runyon BA. Care of patients with ascites. N Engl J Med 1994; 330: 337-42. 10. Chiprut RO, Knudsen KB, Liebermann TR, Dyck WP. Myxedema ascites. Am J Dig Dis 1976; 21: 807-8. 11. Hazard J, Merot J, Klotz A, Potel M. Ascites revealing thyroid deficiency. Ann Med Interne 1969; 120: 755-9. 12. Kinney EL. Myxedema ascites. Am Fam Physician 1987; 36: 134. 13. Kocen RS, Atkinson M. Ascites in hypothyroidism. Lancet 1963; 1: 527-30. 14. Leung FW, Nortman DF, Shinaberger JH. Myxedema ascites in a patient undergoing chronic hemodyalisis. Dyalisis Transplant 1982; 11: 708-9. 15. Madenberg F, Byfield GV, Baker LA. Occurrence of ascites in myxedema. Arch Intern Med 1954; 93: 787-95. 16. Desrame J, Mathurin P, Rozov R, Sabate JM, Poynard T, Opolon P, Denis J. Isolated ascites revealing a hypothyroidism: study of 2 cases. Gastroenterol Clin Biol 1998; 22: 732-5. 17. Skinner J. Mixedema with thyroid antibodies presenting with ascites. Proc R Soc Med 1962; 55: 997. 18. Turner JA, Rapoport J. Mixedema ascites. Postgrad Med J 1977; 53: 343-4. 19. Von Knorring J, Friman C. Mechanism of myxedema formation. N Engl J Med 1980; 302: 469. 20. Alberti LE, Lopez-Gomez A, Alberti-Flor JJ. Spontaneous bacterial peritonitis in a patient with myxedema ascites. Digestion 2003; 68: 91-3. 21. Parving HH, Hansen JM, Nielsen SL, Rossing N, Munck O, Lassen NA. Mechanisms of edema formation in myxedema increased protein extravasation and relatively slow lymphatic drainage. N Engl J Med 1979; 301: 460-5. 22. Bonvalet JP, David R, Baglin A, Hatt PY. Myxedema with inappropriate antidiuresis and hyperaldosteronism. Ann Med Interne 1970; 121: 949-55.
Você também pode gostar
- The Predominantly Plant-Based Pregnancy GuideDocumento179 páginasThe Predominantly Plant-Based Pregnancy GuidePriscila Tobar Alcántar100% (1)
- Ajuste de Dosis de Medicamentos en Paciente RenalDocumento46 páginasAjuste de Dosis de Medicamentos en Paciente RenalThelma Cantillo RochaAinda não há avaliações
- La Teta Cansada - Montserrat Reverte PDFDocumento4 páginasLa Teta Cansada - Montserrat Reverte PDFIpAinda não há avaliações
- HGO Aplicaciones Clinicas JamaDocumento4 páginasHGO Aplicaciones Clinicas JamaPriscila Tobar AlcántarAinda não há avaliações
- Breastfeeding Medicine Protocol on GalactogoguesDocumento8 páginasBreastfeeding Medicine Protocol on GalactogoguespaulinaovAinda não há avaliações
- Diabetic KetoacidosisDocumento16 páginasDiabetic Ketoacidosisdrtpk100% (2)
- Hiper Hipoparatir NejmDocumento13 páginasHiper Hipoparatir NejmPriscila Tobar AlcántarAinda não há avaliações
- MayoClinProc Anemia in Adults A Contemporary Approach To DiagnosisDocumento7 páginasMayoClinProc Anemia in Adults A Contemporary Approach To DiagnosisBarbarita Alvarado CamposAinda não há avaliações
- Acute Appendicitis in AdultsDocumento20 páginasAcute Appendicitis in AdultsPriscila Tobar AlcántarAinda não há avaliações
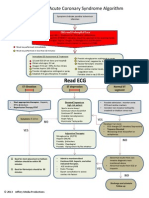
- ACS Algorithm DiagramDocumento1 páginaACS Algorithm DiagramPriscila Tobar Alcántar100% (1)
- Acute Appendicitis in Adults ManagementDocumento16 páginasAcute Appendicitis in Adults ManagementPriscila Tobar AlcántarAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Case NoDocumento13 páginasCase NoLaurente JessicaAinda não há avaliações
- Rozgar Sutra EnglishDocumento105 páginasRozgar Sutra EnglishRisingsun PradhanAinda não há avaliações
- 45 - Altivar 61 Plus Variable Speed DrivesDocumento130 páginas45 - Altivar 61 Plus Variable Speed Drivesabdul aziz alfiAinda não há avaliações
- Method Statement Pressure TestingDocumento15 páginasMethod Statement Pressure TestingAkmaldeen AhamedAinda não há avaliações
- 09 Lift Cylinder Drift (Bulldozer) - CheckDocumento2 páginas09 Lift Cylinder Drift (Bulldozer) - CheckFredy Manrique AstoAinda não há avaliações
- Entrepreneurial Intentions of Cavite Business StudentsDocumento12 páginasEntrepreneurial Intentions of Cavite Business StudentsKevin Pereña GuinsisanaAinda não há avaliações
- The NicotinaDocumento8 páginasThe Nicotinab0beiiiAinda não há avaliações
- Dinflo DFCSDocumento2 páginasDinflo DFCSvictorharijantoAinda não há avaliações
- Attribute Achievement FormDocumento15 páginasAttribute Achievement FormMiguel MenesesAinda não há avaliações
- Facebook Facing Off Againt TencentDocumento6 páginasFacebook Facing Off Againt TencentWai Shan Lee0% (1)
- Isaac Asimov - "Nightfall"Documento20 páginasIsaac Asimov - "Nightfall"Aditya Sharma100% (1)
- India's 1991 Economic ReformsDocumento5 páginasIndia's 1991 Economic ReformsLive AspireAinda não há avaliações
- Subtracting-Fractions-Unlike DenominatorsDocumento2 páginasSubtracting-Fractions-Unlike Denominatorsapi-3953531900% (1)
- On-Chip ESD Protection Design For IcsDocumento14 páginasOn-Chip ESD Protection Design For IcsMK BricksAinda não há avaliações
- The English Center Articulation AgreementDocumento9 páginasThe English Center Articulation AgreementJose CabreraAinda não há avaliações
- Asset Valuation: Debt Investments: Analysis and Valuation: 1 2 N M 1 2 N MDocumento23 páginasAsset Valuation: Debt Investments: Analysis and Valuation: 1 2 N M 1 2 N MSirSmirkAinda não há avaliações
- Ecma L1221BR3 PD02 05172016Documento2 páginasEcma L1221BR3 PD02 05172016Anil JindalAinda não há avaliações
- EMC Design Guide For PCBDocumento78 páginasEMC Design Guide For PCBFaruq AhmedAinda não há avaliações
- Regional Office X: Republic of The PhilippinesDocumento2 páginasRegional Office X: Republic of The PhilippinesCoreine Imee ValledorAinda não há avaliações
- Physics Force and BuoyancyDocumento28 páginasPhysics Force and BuoyancySohan PattanayakAinda não há avaliações
- Valhalla Repair ManualDocumento8 páginasValhalla Repair ManualKirby AllenAinda não há avaliações
- Site AnalysisDocumento15 páginasSite Analysismaanik005Ainda não há avaliações
- XLVI ESAN INTERNATIONAL WEEK (MBA Only - July 2023)Documento38 páginasXLVI ESAN INTERNATIONAL WEEK (MBA Only - July 2023)Juan Diego Fernández CastilloAinda não há avaliações
- Securing Obligations Through Pledge and MortgageDocumento4 páginasSecuring Obligations Through Pledge and MortgagePrincessAngelaDeLeon100% (1)
- Protección Fuego MetalDocumento16 páginasProtección Fuego MetalTracy Mora ChAinda não há avaliações
- Flexural Analysis of Beams (Part 2)Documento7 páginasFlexural Analysis of Beams (Part 2)Johnnette Nafuerza AggabaoAinda não há avaliações
- TheSun 2008-11-04 Page16 Asian Stocks Rally Continues On Policy HopesDocumento1 páginaTheSun 2008-11-04 Page16 Asian Stocks Rally Continues On Policy HopesImpulsive collectorAinda não há avaliações
- NYU Stern Evaluation NewsletterDocumento25 páginasNYU Stern Evaluation NewsletterCanadianValueAinda não há avaliações
- Anna University CTDocumento3 páginasAnna University CTprayog8Ainda não há avaliações
- VNACS Final Case ReportDocumento9 páginasVNACS Final Case ReportVikram Singh TomarAinda não há avaliações