Escolar Documentos
Profissional Documentos
Cultura Documentos
Vasc Med 1998 Powell 21 8
Enviado por
Ghadeer EbraheemDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Vasc Med 1998 Powell 21 8
Enviado por
Ghadeer EbraheemDireitos autorais:
Formatos disponíveis
Vascular Medicine
http://vmj.sagepub.com/ Vascular damage from smoking: disease mechanisms at the arterial wall
Janet T Powell Vasc Med 1998 3: 21 DOI: 10.1177/1358836X9800300105 The online version of this article can be found at: http://vmj.sagepub.com/content/3/1/21
Published by:
http://www.sagepublications.com
On behalf of:
Society for Vascular Medicine
Additional services and information for Vascular Medicine can be found at: Email Alerts: http://vmj.sagepub.com/cgi/alerts Subscriptions: http://vmj.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav Citations: http://vmj.sagepub.com/content/3/1/21.refs.html
>> Version of Record - Feb 1, 1998 What is This?
Downloaded from vmj.sagepub.com by guest on June 24, 2013
Vascular Medicine 1998; 3: 2128
Vascular damage from smoking: disease mechanisms at the arterial wall
Janet T Powell Abstract: The products of tobacco combustion are absorbed into the systemic circulation. Absorbed nicotine stimulates the release of catecholamines, whilst other products (perhaps including nicotine) injure the arterial endothelium and promote atherogenesis. Free radicals and aromatic compounds diminish the endothelial synthesis of nitric oxide, causing impaired endothelium-dependent relaxation of arteries, the earliest clinical sign of endothelial dysfunction. Smoking alters the shear forces and rheology at the endothelial surface and these changes enhance the effects of products of tobacco combustion to upregulate leucocyte adhesion molecules on the endothelial surface. The increased oxidation of low density lipoprotein (LDL) in smokers has synergistic effects to promote monocyte adhesion and monocyte migration into the subintimal space. Continued stimulation of intimal cells by oxidized LDL leads to the development of atherosclerosis. Many of these effects are ameliorated by high concentrations of vitamin C. Smoking also potentiates thrombosis at the dysfunctional endothelium by increasing the concentration of plasma brinogen and altering the activity of platelets. All these proatherogenic effects of smoking to injure the endothelium also are observed, albeit to lesser extent, in passive smokers. Key words: atherosclerosis; endothelium; brinogen; nitric oxide; smoking
Introduction
Cigarette smoking is a common cause of premature death, whether from respiratory disease, lung cancer, other cancers or cardiovascular disease. Cigarette smoking is the single most important risk factor for lung cancer, peripheral atherosclerosis and abdominal aortic aneurysm. The association between smoking and lung cancer is readily appreciated. The combustion and partial combustion of tobacco in cigarettes yields hundreds of different chemicals, including aromatic hydrocarbons, aromatic amines, acrolein and carbon monoxide, which on inhalation might injure the cells of the airways and alveoli. These injurious chemicals interfere with a variety of cellular and metabolic processes, including the direct damage of cellular DNA. The more cigarettes a person has smoked the higher the concentration of aromatic DNA adducts that are found in the lung.1,2 In contrast, the concentration of DNA adducts in the vasculature of smokers is low.2 Different mechanisms, attributable to the toxicity of absorbed products of tobacco combustion, must underlie, in large part, the powerful epidemiological evidence showing smoking as a potent, but avoidable, cause of vascular disease. In addition, the effect of smoking to alter dietary habits and exercise tolerance will have indirect effects on the vasculature.
The tar content of cigarettes and vascular disease
Identication of the cigarette components which, when absorbed and metabolized, may damage the vasculature is important. Reluctantly, the tobacco companies have accepted that Smoking can seriously damage your health and there has been a drive to market safer cigarettes, with a lower tar and nicotine content. The tar and nicotine content of cigarettes have been reduced substantially. The average tar content of a cigarette has been reduced from 30 mg in 1970 to 10 mg in 1997, with consequent reduction in the average nicotine content from 2 mg to 1 mg per cigarette.3 There is little evidence to suggest that those who smoke higher tar content cigarettes are at higher risk of either ischaemic heart disease or peripheral arterial disease than those who smoke low tar cigarettes.4,5 However, smokers who inhale deeply appear to have an increased risk of both symptomatic peripheral arterial disease and abdominal aortic aneurysm.5,6
Nicotine, carbon monoxide and other products of tobacco combustion
An indication of the variety of chemical products of tobacco combustion that are inhaled is given in Table 1. The addictive component is nicotine. The pathways through which nicotine affects the release and turnover of neurotransmitters in the central nervous system are beginning to be unravelled.711 Nicotine binds to a subset of cholinergic receptors in the nucleus accumbens to trigger the release of dopamine.8,9 The density of these and other nicotine receptors in the central nervous system is modulated by
1358-863X(98)VM210OA
Department of Vascular Surgery, Imperial College School of Medicine at Charing Cross Hospital, London, UK Address for correspondence: Janet T Powell, Professor of Cardiovascular Biology, Department of Vascular Surgery, Imperial College School of Medicine at Charing Cross Hospital, Fulham Palace Road, London W6 8RF, UK.
Arnold 1998
Downloaded from vmj.sagepub.com by guest on June 24, 2013
22
JT Powell
Table 1 A selection of the chemicals found in mainstream and sidestream tobacco smoke.
Mainstream smoke (cigarette smokers)
Carbon monoxide Nitrogen oxides Hydrogen cyanide Ammonia Acetaldehyde Acrolein Benzene Benzanthracene Benzapyrene Toluene Phenol Cresols Acrylamide Nitrosonornicotine Nitrosoanatabine
Sidestream smoke (passive smokers)
Carbon monoxide Nitrogen oxides Hydrogen cyanide Ammonia Acetaldehyde Acrolein Benzene Benzanthracene Benzapyrene
Nitric oxide is a free radical, one of many absorbed by the smoker. Absorbed free radicals catalyse the oxidation of low density lipoprotein (LDL) to promote endothelial activation, macrophage activation and the development of atherosclerosis in susceptible regions of the arterial tree. The effect of dietary supplementation with vitamin C, a natural anti-oxidant, to reduce the vascular damage caused by smoking indicates that the generation of free radicals in products of tobacco combustion have an important role in the pathogenesis of vascular disease.18,19
The spectrum of vascular disease caused by smoking
Epidemiological studies have provided clear evidence to associate smoking with almost all forms of arterial disease. In contrast, there are few associations between venous disease and smoking. The earliest epidemiological studies to demonstrate the association between smoking and ischaemic heart disease included the Framingham Study and Sir Richard Dolls classic study of British doctors.20,21 The Framingham Study, together with later studies, also have demonstrated an increased risk of stroke in smokers.20,22 Smoking is associated with an increased risk of both atherothrombotic stroke and cerebral aneurysm.22,23 Nevertheless, smoking is but one of the risk factors for both ischaemic heart disease and stroke, other critical risk factors including hyperlipidaemia, hyperbrinogenaemia and hypertension. In contrast, smoking is the principal risk factor for both abdominal aortic aneurysm and peripheral arterial disease.20,2426 Peripheral arterial disease results from atherothrombosis of the distal aorta and its branches, causing intermittent claudication, ulcers, gangrene and impotence when the penile arteries are affected. Buergers disease is an inammatory disease of the arteries, veins and nerves of the limbs, which also is caused by smoking. Buergers disease is traditionally observed in young adult males and although uncommon in western Europe, it is very common in the Indian subcontinent. Smoking cessation is the most effective therapy for Buergers disease. Smoking cessation is less effective as a treatment for ischaemic heart disease, peripheral vascular disease or abdominal aortic aneurysm, although smoking cessation may reduce the likelihood of a fatal event.2729 When disease of the coronary or distal arteries is very severe, bypass surgery using saphenous vein is considered. Once the vein is used as an arterial conduit it too becomes susceptible to smoking, with smoking increasing the risk of bypass graft occlusion.30 Even in subjects with apparently healthy arteries, smoking initiates vasospasm causing digital blanching and penile artery vasospasm.31,32 Therefore, it is unsurprising that smoking exacerbates Raynauds phenomenon. Smoking damage to umbilical arteries contributes to the low birth weight of children born to smoking mothers.33,34 No artery appears to be immune from the devastating effects of smoking.
Nitrosonornicotine
smoking, as is the activity of the dopamine metabolizing enzyme monoamine oxidase.11 The release of dopamine and stimulation of a variety of neural pathways underlies the effect of smoking to alter mood and appetite. In the peripheral nervous system, nicotine affects the release of the catecholamines, adrenaline and noradrenaline.12 This catecholamine release has important effects on cardiac function, vascular tone and lipid metabolism. There is little evidence to suggest that in man, nicotine, itself, has direct effects on the cells of the blood vessel wall interface, the endothelium, platelets or leucocytes, although in animals the administration of intravenous nicotine has adverse effects on aortic endothelium, with cell blebbing and detachment. In the alveolus, inhaled carbon monoxide diffuses into the capillaries, where it is absorbed by the haemoglobin on erythrocytes to form carboxyhaemoglobin. The extent of carboxyhaemoglobin formation depends on depth of inhalation and lung function in addition to the type and number of cigarettes smoked.13,14 The percentage substitution of haemoglobin with carbon monoxide in a smoker ranges from 2% to 10%. The presence of carboxyhaemoglobin reduces the oxygen carrying capacity of the erythrocytes and often induces a compensatory erythrocytosis with increased haematocrit.15 This erythrocytosis increases the viscosity of the blood and can impair the ow through capillaries. Tobacco elds all too often are farmed intensively and the elds fertilized with nitrates. These nitrates are absorbed into tobacco leaf and the yield of nitrate and nitrogen oxides from cigarettes is directly proportional to the nitrate content of the leaf.16 Some of these nitrogen oxides interact with nicotine and other aromatic components to form nitrosonornicotine and other potentially carcinogenic compounds. Nitrogen oxides also can initiate free radical reactions, although any nitric oxide absorbed into the capillary at the alveolus also is likely to be rapidly absorbed by haemoglobin or plasma proteins. Although nitrosoalbumin derivatives have therapeutic effects as nitrite donors in the experimental situation, the plasma concentrations of these derivatives in smokers is too low to have therapeutic effect.17
Vascular Medicine 1998; 3: 2128
Passive smoking and vascular disease
Society may countenance self-inicted injury to the vasculature by smoking. The accumulating evidence that passive
Downloaded from vmj.sagepub.com by guest on June 24, 2013
Vascular damage from smoking 23
smoking increases a persons risk of ischaemic heart disease by one-quarter,35 should spearhead new legislation to restrict smoking in all public areas. The accumulating evidence to associate passive smoking with an increased risk of vascular disease comes from both epidemiological studies and direct studies of endothelial function in passive smokers.36 Injury to the endothelium is considered to be the earliest forerunner of atherosclerosis,37,38 with endothelial dysfunction being the earliest detectable sign of endothelial injury. These in vivo tests of endothelial function are based on our increasing knowledge of the factors that regulate normal vascular tone and which may be perturbed by smoking, active or passive, to promote vasoconstriction.
Vascular pathology
The earliest injurious effects of smoking can be detected as abnormal vasodilator responses of the brachial or femoral arteries. The development of atherosclerotic lesions is a later event, with some vessels, including the distal aorta, being particularly susceptible to atherosclerosis.39 Once atherosclerosis narrows the arterial lumen and disrupts the anti-thrombotic properties of the vessel wall, thrombosis at the diseased arterial wall may trigger acute cardiovascular events.40 Smoking facilitates every facet of this disease process and it is this that will be considered in some detail. Regulation of vascular tone The inhalation of cigarette smoke results in the rapid absorption of nicotine, with consequent systemic release of adrenaline and noradrenaline. These catecholamines bind to 1-adrenergic receptors on vascular smooth muscle to cause muscle contraction and vasoconstriction. In the healthy adult, who does not usually smoke, the vasoconstrictor response is soon counterbalanced by the local release of vasodilators from endothelium. The two best characterized endothelial vasodilators are nitric oxide (NO) and prostacyclin. Nitric oxide is considered to be the dominant local regulator of resting vasomotor tone, with packets of NO being produced at regular intervals. The arterial dilatation of post-occlusive hyperaemia and the recruitment of capillaries in exercising skeletal muscle both depend on the release of nitric oxide from endothelium. This nitric oxide is synthesized by oxidation of l-arginine by an enzyme, nitric oxide synthase, which is expressed constitutively. The activity of this enzyme depends on several cofactors (including NADPH, avin adenine dinucleotide, avin mononucleotide and tetrahydrobiopterin), myristylation to transport the enzyme to the plasma membrane of cells, phosphorylation and the concentration of calcium in the cytosol of the endothelium. Nitric oxide, a molecule containing an electron with unpaired spin, which can initiate free radical chain reactions, normally has a very short halflife, binding readily to proteins with active Fe2+ centres, including guanylate cyclase in smooth muscle and platelets. The activation of this enzyme causes the release of cyclic GMP to trigger smooth muscle relaxation and prevent platelet aggregation respectively. It is this effect to promote smooth muscle cell relaxation that is critical to the maintenance of normal vascular tone in healthy vessels. In disease, the effects of nitric oxide to prevent platelet aggregation, monocyte adhesion and inhibit smooth muscle cell proliferVascular Medicine 1998; 3: 2128
ation assume greater importance. In this respect smoking is both the disease and cause of the disease. Several lines of evidence suggest that smoking impairs the production of nitric oxide by the endothelium. The endothelial production of nitric oxide can be augmented by a variety of physiological stimuli, including an increase in blood ow. Hence, arterial dilation is the normal endothelium-dependent response after removal of an occluding tourniquet. Vasodilatory nitrate drugs, such as sodium nitroprusside and glyceryl trinitrate, provide nitric oxide directly to the vascular smooth muscle cells to bypass the endothelium and stimulate endothelium-independent vasorelaxation. These responses to hyperaemic ow and nitrate vasodilators have been used as the basis of an in vivo assessment of endothelium-dependent responses. In normal, healthy non-smoking adults the brachial and femoral arteries dilate by 11% and 4% respectively in response during reactive hyperaemia.41 In young, apparently healthy, smokers these dilatations are reduced to 4% and 0% respectively, whilst the responses to nitrates are preserved.41 This loss of endothelium-dependent responses is probably the earliest manifestation of injury to the endothelium caused by smoking. Passive smoking also has been shown to be associated with impairment of dilatation of the brachial artery in reactive hyperaemia, with the magnitude of the impairment related directly to the amount of exposure to tobacco smoke.36 The synergistic effects of smoking and hypercholesterolaemia to potentiate endothelial dysfunction have been attributed to the ability of smoking to promote the oxidation of LDL,42 a topic to be revisited (see below). These in vivo ndings are supported by in vitro ndings showing that smoking impairs the endothelial nitric oxide production from saphenous vein rings and from platelets.43,44 The in vitro evidence indicates that the biosynthetic pathway to provide the nitric oxide synthase cofactor tetrahydrobiopterin is impaired in smokers, perhaps through an aromatic product of tobacco combustion inhibiting one of the biosynthetic enzymes.43 When tetrahydrobiopterin concentrations are low the activation of nitric oxide synthase leads to the production of hydrogen peroxide, leading to oxidative vascular injury.45 In keeping with this observation, high concentrations of the antioxidant vitamin C improve the endothelial dysfunction observed in the brachial artery and forearm vessels of smokers.18 To summarize, there is accumulating evidence to indicate that smoking disturbs the endothelial production of nitric oxide, to predispose to the development of atherosclerosis (Figure 1). How many smokers read this journal? Do not despair, there is evidence from both in vivo and in vitro studies to suggest that the endothelial dysfunction associated with smoking is reversible, even within 12 months of smoking cessation.46,47 Since nitric oxide is the principal regulator of resting vascular tone, it has remained the focus of this section. There is also considerable evidence, again both in vivo and in vitro, to show that prostacyclin production is impaired in smokers, with compensatory increase in production of the vasoconstrictor thromboxanes.48 Cellular events in the development of atherosclerotic or inammatory vascular disease Impaired production of vasodilators nitric oxide and prostacyclin is but one manifestation of injury to the endothelium
Downloaded from vmj.sagepub.com by guest on June 24, 2013
24
JT Powell
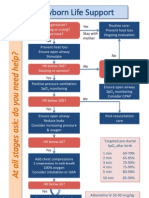
Figure 1 Smoking impairs endothelium-dependent relaxation of vessels. (Left) The immediate response of healthy endothelium to an increase in blood ow (and other physiological stimuli) is an increase in intracellular calcium. This increase in calcium concentration stimulates the synthesis of nitric oxide from l-arginine by the enzyme nitric oxide synthase (NOS). Essential cofactors for this activity include tetrahydrobiopterin, itself synthesized in endothelium. The nitric oxide diffuses out of the endothelium to bind to the Fe2+ in the haem moiety of guanylate cyclase to stimulate the synthesis of cyclic GMP. The increased concentration of cyclic GMP triggers smooth muscle relaxation. (Right) Smoking limits the endothelial synthesis of nitric oxide in two (or more) ways. The increased concentration of blood-borne free radicals accelerates cellular lipid peroxidation. The lipid peroxides avidly bind to available nitric oxide. The synthesis of nitric oxide also is reduced to decreased synthesis of tetrahydrobiopterin. Nitric oxide is no longer available to stimulate endothelium-dependent relaxation.
caused by smoking. The classic response to injury hypothesis of the development of atherosclerosis has been described elegantly by Ross.37,38 In response to injury the adhesive properties of the endothelium change in a manner that supports the recruitment, adhesion and migration of monocytes into the subendothelial space (Figure 2). This migration of monocytes is orchestrated by cytokines and fuelled by the oxidation of LDL.49 Leucocyte recruitment at the vessel wall is a multistep process.50 Chemoattractants recruit the leucocytes to the endothelial surface, where they roll along the endothelium with loose interactions between proteins and glycoproteins on the two cell types. Firm adhesion is then mediated by distinctive protein adhesion molecules on the endothelium (e.g. ICAM-1 and VCAM-1) and activated integrins on the leucocyte. The normal, healthy endothelium has antiadhesive properties and the continued synthesis of nitric oxide is important in this respect.51 With the diminished production of endothelial nitric oxide in smokers (see above) these anti-adhesive properties are lost. Again, in normal healthy endothelium the expression of adhesion molecules, including intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM1), on the endothelium is very low. Using endothelial cells isolated and cultured from human umbilical vein it has been
Vascular Medicine 1998; 3: 2128
shown that smoke condensate causes a rapid increase in expression of both ICAM-1 and VCAM-1 on the surface of the cultured cells.52 The cells have become activated and are poised to grab any rolling leucocytes. Yet again vitamin C may have benecial effects to prevent the increased adhesiveness of monocytes in smokers.53 In addition, smoking alters the haemodynamic forces at the bloodendothelial surface, both directly and indirectly through effects on blood rheology.15,54 The concentration of leucocyte adhesion molecules (ICAM-1 and VCAM-1) on the endothelial surface also is regulated by changes in haemodynamic forces.55 Similarly, endothelial expression of the potent monocyte chemoattractant MCP-1 (monocyte chemoattractant protein-1) is regulated by shear stress. The haemodynamic changes induced by smoking appear likely to favour the upregulation of both MCP-1 and VCAM-1, important in the recruitment of monocyte/macrophages. Therefore, smoking is likely to effect more extensive changes of the endothelial surface than can be observed non-invasively with changes in brachial or femoral artery diameter in response to hyperaemic ow. This invisible endothelial dysfunction leads directly to the recruitment of monocytes/macrophages into the arterial intima. More extensive arterial injury leads to endothelial denudation. There is evidence to indicate that endothelial cells
Downloaded from vmj.sagepub.com by guest on June 24, 2013
Vascular damage from smoking 25
Figure 2 Smoking stimulates monocyte adhesion, migration and activation. The altered shear stress at the endothelial surface induced by smoking and the absorbed products of tobacco combustion have synergistic effect to increase the expression of leucocyte adhesion molecules (ICAM-1 and VCAM-1) on endothelium. The alterations of shear stress induced by smoking also may stimulate the release of monocyte chemoattractants. Reduced nitric oxide synthesis also increases the adhesiveness of the endothelium. The endothelium becomes leaky, permitting the entry of oxidized LDL (oxLDL), which activates the migrated monocyte/macrophages to release cytokines and growth factors to attract more cells (smooth muscle cells and macrophages) to migrate and proliferate in the intima. The atherosclerotic lesion has started to develop, continuously stimulated by smoking.
are lost into the circulation in response to smoking.56 The exposed collagen of the subendothelial matrix supports platelet adhesion and aggregation. The aggregated platelets secrete potent paracrine factors including platelet derived growth factor (PDGF), which acts as a mitogen for smooth muscle cells. With the migration of monocytes into the intima and the secretion of smooth muscle cell mitogens the scene has been set for the development of a traditional atherosclerotic lesion.49 This atherosclerotic lesion is both living and dying. In response to the elaboration of growth factors and cytokines, macrophages and smooth muscle cells proliferate, the latter secreting a connective tissue matrix, which may stabilize the atherosclerotic plaque. These cells also engulf oxidized LDL, taken up through the now leaky endothelium, to form foam cells. The very avidity of these cells in taking up oxidized LDL fuels the cycle of inammatory cytokine release, but also eventually causes cell death. The cholesterol crystals of the atherosclerotic plaque are the gravestones of these cells. Hence, smoking has initiated a self-propagating pathway of disease and destruction. The variety of free radicals generated by tobacco combustion exacerbate this process further by provoking the oxidation of LDL.57 Again, the anti-oxidant vitamin C has been found to interrupt this process, by diminishing the oxidation of LDL.19 Smoking, through its ability to modulate nitric oxide production, alter haemodynamic forces at the vessel wall,
Vascular Medicine 1998; 3: 2128
increase the adhesivity of endothelium and generate free radicals to promote the oxidation of LDL, has pleiotropic effects to exacerbate the cellular changes critical to the development of atherosclerosis. Thrombosis at the injured vessel wall Critical atherosclerotic events, myocardial infarction and stroke, appear to be initiated by instability in the atherosclerotic plaque to favour the development of an acute thrombus, which occludes the vessel locally or more distally by embolization. Smoking has particular effects on platelets and coagulation factors, which promote the development of thrombosis. As discussed above, smoking may initiate endothelial denudation, exposing the underlying matrix to promote platelet adhesion and diminish the amount of platelet nitric oxide production to remove protection against aggregation. There is a shortened half-life of platelet survival in the apparently healthy smoker.58 Through analysis of urinary prostanoid metabolites it has been demonstrated that chronic smoking causes an increase in the principal platelet product of arachidonic acid metabolism, thromboxane A2.59 Both these changes, observed in vivo, would suggest that smoking is associated with a heightened sensitivity of platelets to activation and aggregation. These ndings contrast with in vitro experiments, which show that platelets isolated
Downloaded from vmj.sagepub.com by guest on June 24, 2013
26
JT Powell
from smokers have a diminished sensitivity to activation in response to agonists such as ATP.60,61 The identication of increased plasma concentrations of brinogen and factor VII as major risk factors for ischaemic heart disease must be credited to the Northwick Park Heart Study.62 Fibrinogen also is a risk factor for other forms of vascular disease, including the occlusion of venous bypass grafts and restenosis after coronary artery angioplasty.30,63 Both factor VII and brinogen are critical to the development of brin clot on the surface of damaged endothelium and atherosclerotic plaque, with its exposed tissue factor. Smoking increases the plasma concentration of brinogen but appears to have little effect on the concentration of factor VII.64,65 Cessation of smoking is associated with a slow but steady reduction of plasma brinogen concentrations, achieving a reduction of 5% after 5 years of abstinence.64 The role of brinogen to increase blood viscosity is well established. However, increasing recognition is being given to the role of brin(ogen) as an inammatory mediator, promoting the adhesion of leucocytes to activated endothelium and stimulating the release of inammatory cytokines (MCP-1 an IL-8) from cultured endothelial cells.6668 Hence, the action of smoking to increase plasma brinogen concentrations will favour the recruitment of inammatory cells into the vessel wall to stimulate the development of atherosclerosis, long before acute thrombosis on the damaged vessel becomes problematic. This role of brinogen as an inammatory mediator might underlie the recently reported association between brinogen concentration and intimal thickening of the carotid arteries.69 As the atherosclerotic disease progresses from fatty streak to raised lesion, the increased ow through stenotic areas exacerbates the deposition of both platelets and brinogen at the apex of the stenosis.70 Fibrin(ogen) deposition is also prominent in the thrombus area so often observed adjacent to discrete stenoses.70 Therefore, in the presence of endothelial dysfunction, the effect of smoking to increase plasma brinogen concentrations and activate platelets in vivo is important in accelerating all future stages of disease progression.
with a rare polymorphic variant of the endothelial nitric oxide synthase gene (ecNOS4a) are over-represented in patients found to have severe stenotic lesions on coronary artery angiography.76 These ndings are probably only the tip of an iceberg: the environmentalgenotype interactions may predict which smokers will develop early onset and severe vascular disease. Diet Demographic evidence underscores the contribution of diet to the development of atherosclerosis. There is strong evidence to suggest that the dietary habits of smokers are different from those of non-smokers. Smokers eat less frequently than non-smokers and eat more sugar and animal fat than non-smokers.77 Smokers have a lower intake of polyunsaturated fat and anti-oxidant vitamins than nonsmokers.77 Within Europe there will be a gradient in these differences, the most signicant effects of smoking being found in north-west Europe, rather than Mediterranean south-east Europe. Therefore it is not surprising that there are several Scottish studies to show that smoking is associated with a reduced intake/plasma concentration of antioxidants and unsaturated fatty acids.78,79 The altered dietary patterns of smokers also are likely to favour large swings in insulin secretion, an important factor in the development of atherosclerosis. Further, the meta-analyses show that cholesterol concentrations are raised in smokers, even teenage smokers.80,81 These cumulative interactions between diet and smoking all feedback on the mechanisms discussed above to favour the development of endothelial dysfunction, inammatory cell recruitment and the development of the atherosclerotic plaque.
Conclusion
This review has focused on how smoking impacts on and potentiates the mechanisms at three separate stages of the development of vascular disease (atherosclerosis): 1) endothelial dysfunction 2) monocyte recruitment and development of the plaque 3) thrombosis at the damaged vessel wall. Other aspects of smoking toxicity, such as the possible effects of carbon monoxide on endothelial permeability and vasospasm or interactions between smoking and homocysteine. The author would like also to acknowledge all those whose work she has read, but not cited. There is no doubt that smoking damages the vasculature. Equally, given the diverse mechanisms whereby smoking potentiates the development of vascular disease it is difcult to envisage the production of a safe cigarette, where all the vascular toxins had been removed. All the scientic evidence suggests that a high intake of vitamin C can ameliorate or abolish the smoking-induced endothelial dysfunction and the imbalance in anti-oxidants. There is, as yet, no evidence from clinical trials that vitamin C (or vitamin E) supplementation reduces cardiovascular events.8284 Until evidence becomes available the best advice to a smoker remains stop smoking.
Other factors inuencing the toxic effects of smoking on the vasculature
With the number of toxins delivered into the lungs and absorbed into the circulation of cigarette smokers it is surprising that some committed smokers live so long in apparent rude good health. Perhaps the answer to this paradox is to be found in the interaction of smoking with genes, diet and other lifestyle factors. Genetic background There is accumulating evidence for strong smokinggenotype interactions. The interaction between polymorphisms in the apolipoprotein and cholesterol ester transfer protein genes has important effects.7173 In the presence of specic genotypes, smoking acts to increase the plasma concentration of cholesterol and lower the concentration of high density lipoprotein, both changes being pro-atherogenic. Other evidence shows that persons of specic brinogen genotype, who choose to smoke, will show accentuated elevation of plasma brinogen concentrations.74,75 Smokers
Vascular Medicine 1998; 3: 2128
Downloaded from vmj.sagepub.com by guest on June 24, 2013
Vascular damage from smoking 27
References
1 Phillips DH, Hewer A, Martin CN, Garner RC, King MM. Correlation of DNA adduct levels in human lung with cigarette smoking. Nature 1988; 336: 79092. 2 Randerath E, Miller RH, Mittal D, Avitts TA, Dunsford HA, Randerath K. Covalent DNA damage in tissues of cigarette smokers as determined by 32P-postlabeling assay. J Natl Cancer Inst 1989; 81: 34147. 3 Kiryluk S, Wald N. Trends in smoking habits in the United Kingdom. In: Wald N, Froggat P eds. Nicotine, smoking and the low tar programme. Oxford: Oxford Medical Publications, 1989: 5369. 4 Negri E, Franzosi MG, La Vecchia C, Santoro L, Nobili A, Tognoni G. Tar yields of cigarettes and risk of acute myocardial infarction. Br Med J 1993; 306: 156770. 5 Powell JT, Edwards RJ, Worrell PC, Franks PJ, Greeenhalgh RM, Poulter NR. Risk factors associated with the development of peripheral arterial disease in smokers. Atherosclerosis 1997; 129: 4148. 6 Franks PJ, Edwards RJ, Greenhalgh RM, Powell JT. Risk factors for the development of abdominal aortic aneurysm in smokers. Eur J Vasc Surg 1996; 11: 48792. 7 Nutt DJ. Addiction: brain mechanisms and their treatment implications. Lancet 1996; 347: 3136. 8 Benwell MEM, Balfour DJK, Birrell CE. Desensitization of the nicotine-induced mesolimbic dopamine responses during constant infusion with nicotine. Br J Pharmacol 1995; 114: 45460. 9 Pontieri FE, Tanda G, Orzi F, di Chiara G. Effects of nicotine on the nucleus accumbens and similarity to those of addictive drugs. Nature 1996; 382: 25557. 10 Benwell MEM, Balfour DJK, Anderson JM. Evidence that tobacco smoking increases the density of [3H]nicotine binding sites in human brain. J Neurochem 1988; 50: 124347. 11 Fowler JS, Volkow ND, G-J Wang et al. Inhibition of monoamine oxidase B in the brains of smokers. Nature 1996; 379: 73336. 12 Benowitz NL. Pharmacologic aspects of cigarette smoking and nicotine addiction. N Engl J Med 1988; 319: 131830. 13 Wald NJ, Boreham J, Bailey A. Relative intakes of tar, nicotine and carbon monoxide from cigarettes of different yield. Thorax 1984; 39: 36164. 14 Worrell PC, Edwards RJ, Powell JT. Smoking markers as a reection of the smoking habit. J Smoking Relat Dis 1995; 6: 8998. 15 Ernst E, Matrai A, Schmolzl C, Magyarosy I. Doseeffect relationship between smoking and blood rheology. Br J Haemotol 1987; 65: 48587. 16 Fischer S, Spiegelhalter B, Preussmann R. Tobacco-specic nitrosamines in commercial cigarettes: possibilities for reducing exposure. IARC Sci Publ 1991; 105: 48992. 17 Marks DS, Vita JA, Folts JD, Keaney JF, Welch GN, Loscalzo J. Inhibition of neointimal proliferation in rabbits after vascular injury by a single treatment with a protein adduct of nitric oxide. J Clin Invest 1995; 96: 263038. 18 Heitzer T, Just H, Munzel T. Antioxidant vitamin C improves endothelial dysfunction in chronic smokers. Circulation 1996; 94: 69. 19 Fuller CJ, Grundy SM, Norkus EP, Jiala I. Effect of ascorbate supplementation on low density lipoprotein oxidation in smokers. Atherosclerosis 1996; 119: 13950. 20 Hammond EC, Garnkel L. Coronary heart disease, stroke and abdominal aortic aneurysm. Factors in etiology. Arch Environ Health 1967; 19: 16782. 21 Doll R, Peto R. Mortality in relation to smoking: 20 years observations on male British doctors. Br Med J 1976; ii: 152536. 22 Abbott RD, Yin Y, Reed DM, Yano K. Risk of stroke in male cigarette smokers. N Engl J Med 1986; 315: 71720. 23 Adamson J, Humphries SE, Voldby B, Ostergaard J, Richards P, Powell JT. Are cerebral aneurysms atherosclerotic? Stroke 1994; 25: 96366. 24 Kannel WB, Shurtleff D. The Framingham Study: cigarettes and the development of intermittent claudication. Geriatrics 1973; 28: 6168.
25 Fowkes FGR. Epidemiology of atherosclerotic arterial disease in the lower limbs. Eur J Vasc Surg 1988; 2: 28391. 26 Fowkes FGR, Housley E, Riemersma RA et al. Smoking, lipids, glucose intolerance and blood pressure as risk factors for peripheral atherosclerosis in the Edinburgh Artery Study. Am J Epidemiol 1992; 135: 33140. 27 Pocock SJ, Cook DG, Shaper AG, Kussick SJ. Giving up smoking and the risk of heart attacks: A report from the British Regional Heart Study. Lancet 1986; ii: 137679. 28 Smith I, Franks PJ, Greenhalgh RM, Poulter NR, Powell JT. The inuence of smoking cessation and hypertriglyceridaemia on the progression of peripheral arterial disease and the onset of critical ischaemia. Eur J Vasc Surg 1996; 11: 48792. 29 MacSweeney STR, Ellis M, Worrell PC, Greenhalgh RM, Powell JT. Smoking and growth rate of small abdominal aortic aneurysms. Lancet 1994; 344: 65152. 30 Wiseman S, Kenchington G, Dain R, McCollum C, Greenhalgh RM, Powell JT. Inuence of smoking and plasma factors on patency of femoropopliteal vein grafts. Br Med J 1989; 299: 64346. 31 Bornmyr S, Soensson H. Thermomography and laser-Doppler owmetry for monitoring changes in nger skin blood ow upon cigarette smoking. Clin Physiol 1991; 11: 13541. 32 Levine LA, Gerber GS. Acute vasospasm of penile arteries in response to cigarette smoking. Urology 1990; 36: 99100. 33 Asmussen I, Kjeldsen K. Intimal ultrastructure of human umbilical arteries. Observations on arteries from newborn children of smoking and non-smoking mothers. Circulation Res 1975; 36: 57989. 34 Brooke OG, Anderson HR, Bland JM, Peacock JL, Stewart CM. Effects on birth weight of smoking, alcohol, caffeine, socioeconomic factors and psychosocial stress. Br Med J 1989; 298: 795801. 35 Law MR, Morris JK, Wald NJ. Environmental tobacco smoke exposure and ischaemic heart disease: an evaluation of the evidence. Br Med J 1997; 315: 97380. 36 Celermajer DS, Adams MR, Clarkson P et al. Passive smoking and impaired endothelium-dependent arterial dilation in healthy young adults. N Engl J Med 1996; 334: 15054. 37 Ross R. The pathogenesis of atherosclerosis: an update. N Engl J Med 1986; 314: 488500. 38 Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 1993; 362: 801809. 39 Strong JP, Richards ML. Cigarette smoking and atherosclerosis in autopsied men. Atherosclerosis 1976; 23: 45176. 40 Davies M, Bland J, Haugartner J, Angelini A, Thomas A. Factors inuencing the presence or absence of acute coronary artery thrombi in sudden ischaemic death. Eur Heart J 1989; 10: 203208. 41 Celermajer DS, Sorensen KE, Gooch VM et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992; 340: 111115. 42 Heitzer T, Yla-Herttuala S, Luoma J et al. Cigarette smoking potentiates endothelial dysfunction of forearm resistance vessels in patients with hypercholesterolemia. Role of oxidized LDL. Circulation 1996; 93: 134653. 43 Higman DJ, Strachan AMJ, Buttery L et al. Smoking impairs the activity of endothelial nitric oxide synthase in saphenous vein. Arterioscler Thromb Vasc Biol 1996; 16: 54652. 44 Ichiki K, Ikeda H, Haramaki N, Ueno T, Imaizumi T. Long-term smoking impairs platelet-derived nitric oxide release. Circulation 1996; 94: 310914. 45 Cosentino F, Katusic. Tetrahydrobiopterin and dysfunction of endothelial nitric oxide synthase in coronary arteries. Circulation 1995; 91: 13944. 46 Celermajer DS, Sorensen KE, Georgakopoulos D et al. Cigarette smoking is associated with dose-related and potentially reversible impairment of endothelium-dependent dilation in healthy young adults. Circulation 1993; 88: 214955. 47 Higman DJ, Strachan AMJ, Powell JT. Reversibility of smokinginduced endothelial dysfunction. Br J Surg 1994; 81: 97778. 48 Lassila R, Seyberth HW, Haapanen A et al. Vasoactive and atherog-
Vascular Medicine 1998; 3: 2128
Downloaded from vmj.sagepub.com by guest on June 24, 2013
28
JT Powell
49 50 51
52
53
54
55 56
57
58
59
60 61
62
63
64
65
66
67 68
enic effects of cigarette smoking: a study of monozygotic twins discordant for smoking. Br Med J 1988; 297: 95557. Davies MJ, Woolf N. Atherosclerosis: what is it and why does it occur? Br Heart J 1993; 69(suppl): S3S11. Springer TA. Trafc signals for lymphocyte recirculation and leucocyte emigration: the multistep paradigm. Cell 1994; 76: 30114. Tsao PS, Lewis NP, Alpert S, Cooke JP. Exposure to shear stress alters endothelial adhesiveness. Role of nitric oxide. Circulation 1995; 92: 351319. Shen Y, Rattan V, Sultana L, Kalra VK. Cigarette smoke condensateinduced adhesion molecule expression and transendothelial migration of monocytes. Am J Physiol 1996; 270: H1624H33. Weber C, Erl W, Weber K, Weber PC. Increased adhesiveness of isolated monocytes to endothelium is prevented by vitamin C intake in smokers. Circulation 1996; 93: 148892. Caro CG, Lever MJ, Parker KH, Fish PJ. Effect of cigarette smoking on pattern of arterial blood ow: possible insight into mechanism and the underlying development of atherosclerosis. Lancet 1987; ii: 1113. Resnick N, Gimbrone MA. Haemodynamic forces are complex regulators of endothelial gene expression. FASEB J 1995; 9: 85260. Sbarbati R, de Boer M, Marzilli M, Scarlattini M, Rossi G, van Mourik JA. Immunologic detection of endothelial cells in human whole blood. Blood 1991; 77: 764769. Frei B, Forte TM, Ames BN, Cross CE. Gas phase oxidants of cigarette smoke induce lipid peroxidation and changes in lipoprotein properties in human blood plasma. Biochem J 1991; 277: 13338. Fuster V, Chesebro JH, Frye R, Elveback LR. Platelet survival and the development of coronary artery disease in young adults. Circulation 1981; 63: 54651. Nowak J, Murray JJ, Oates JA, FitzGerald GA. Biochemical evidence of a chronic abnormality in platelet and vascular function in healthy individuals who smoke cigarettes. Circulation 1987; 76: 614. Ashby P, Dalby AM, Millar JH. Smoking and platelet stickiness. Lancet 1965; ii: 15860. Mansouri A, Perry CA. Inhibition of platelet ADP and serotonin release by carbon monoxide in cigarette smokers. Experimentia 1984; 40: 51517. Meade TW, Mellows S, Brozovic M et al. Haemostatic function and ischaemic heart disease; principal results of the Northwick Park Heart Study [see comments]. Lancet 1986; ii: 53337. Montalescot G, Ankri A, Vicaut E, Drobinski G, Grosgogeat Y, Thomas D. Fibrinogen after coronary angioplasty as a risk factor for restenosis. Circulation 1995; 92: 3138. Meade TW, Imeson J, Stirling Y. Effects of changes in smoking and other characteristics on clotting factors and the risk of ischaemic heart disease. Lancet 1987; ii: 98688. Gris JC, Schved JF, Feugeas O et al. Impact of smoking, physical training and weight reduction on FVII, PAI-1 and hemostatic markers in sedentary men. Thromb Haemost 1990; 64: 51620. Languino LR, Plescia J, Duperray A et al. Fibrinogen mediates leucocyte adhesion to vascualr endothelium through an ICAM-1 dependent pathway. Cell 1993; 73: 142334. Qi J, Kreutzer DZ. Fibrin activation of vascular endothelial cells: induction of IL-8 expression. J Immunol 1995; 155: 86776. Harley SL, Walton LJ, Powell JT. Fibrinogen mediated leucocyte
69
70
71
72
73
74
75
76
77
78
79
80
81
82
83 84
attraction and adhesion to human saphenous vein endothelial cells. Immunology 1996; 89: 60. Joensuu T, Salonen R, Winblad I, Korpela H, Salonen JT. Determinants of femoral and carotid artery atherosclerosis. J Intern Med 1994; 236: 7984. Mailhac A, Badimon JJ, Fallon JT et al. Effect of an eccentric severe stenosis on brin(ogen) deposition on severely damaged vessel wall in arterial thrombosis. Circulation 1994; 90: 98896. Reilly SL, Ferrell RE, Kottke BA, Sing CF. The gender-specic apolipoprotein E genotype inuence on the distribution of plasma lipids and apolipoproteins in the population of Rochester, Minnesota. Am J Hum Genet 1992; 51(6): 131124. Glisic S, Savic I, Alavantic D. Polipoprotein B gene DNA polymorphisms (EcoRI and Mspl) and serum lipid levels in the Serbian healthy population: interaction of rare alleles and smoking and cholersterol levels. Genet Epidemiol 1995; 12(5): 499508. Freeman DJ, Grifn BA, Holmes AP, Gaffney D, Packard CJ, Shepherd J. Regulation of plasma HDL cholesterol and subfraction distribution by genetic and environmental factors. Arterioscler Thromb Vasc Biol 1994; 14: 33644. Thomas AE, Green FR, Kelleher CH et al. Variation in the promotor region of the -brinogen gene is associated with plasma brinogen levels in smokers and non-smokers. Thromb Haemost 1991; 65: 48790. Behague I, Poirier O, Nicaud V et al. -brinogen gene polymorphisms are associated with plasma brinogen and coronary artery disease in patients with myocardial infarction. The ECTIM Study. Circulation 1996; 93: 44049. Wang XL, Sim AS, Badenhop RF, McCredie RM, Wilcken DE. A smoking-dependent risk of coronary artery disease associated with a polymorphism of the endothelial nitric oxide synthase gene. Nat Med 1996; 1: 4145. Margetts BM, Jackson AA. The interactions between peoples diet and their smoking habits, the dietary and nutritional survey of British adults. BMJ 1993; 307: 138184. Leng GC, Horrobin DF, Fowkes FG et al. Plasma essential fatty acids, cigarette smoking, and dietary antioxidants in peripheral arterial disease. A population-based casecontrol study. Arterioscler Thromb 1994; 3: 47178. Brown K, Morrice PC, Duthie GG. Erythrocyte vitamin E and plasma ascorbate concentrations in relation to erythrocyte peroxidation in smokers and nonsmokers: dose response to vitamin E supplementation. Am J Clin Nutr 1997; 2: 496502. Craig WY, Palomaki GE, Haddow JE. Cigarette smoking and serum lipid and lipoprotein concentrations: an analysis of published data. BMJ 1989; 6676: 78488. Craig WY, Palomaki GE, Johnson AM, Haddow JE. Cigarette smoking-associated changes in blood lipid and lipoprotein levels in the 8 to 19 year old age group. Pediatrics 1990; 2: 15558. Romm EB, Stampfer MJ, Ascherio A, Giovannucci E, Colditz GA, Willett WC. Vitamin E consumption and the risk of coronary heart disease in men. N Engl J Med 1993; 328: 145056. Steinberg D. Antioxidant vitamins and coronary heart disease. N Engl J Med 1993; 328: 148789. Oliver M. Antioxidant nutrients, atherosclerosis and coronary heart disease. Br Heart J 1995; 73: 299301.
Vascular Medicine 1998; 3: 2128
Downloaded from vmj.sagepub.com by guest on June 24, 2013
Você também pode gostar
- Usmle Surgery Mcqs PDFDocumento2 páginasUsmle Surgery Mcqs PDFGhadeer Ebraheem75% (4)
- English Time 3Documento79 páginasEnglish Time 3Ghadeer Ebraheem100% (2)
- HIV and HIV CounsellingDocumento12 páginasHIV and HIV CounsellingGhadeer EbraheemAinda não há avaliações
- Leach and Lily Stanley - Last Updated On: Edit This Article View RevisionsDocumento7 páginasLeach and Lily Stanley - Last Updated On: Edit This Article View RevisionsGhadeer EbraheemAinda não há avaliações
- ATLS DRDocumento45 páginasATLS DRNeNeei HenNieAinda não há avaliações
- Antibody Tests Reveal Red Blood Cell AntibodiesDocumento2 páginasAntibody Tests Reveal Red Blood Cell AntibodiesGhadeer EbraheemAinda não há avaliações
- Myotomes of The Upper LimbDocumento2 páginasMyotomes of The Upper LimbGhadeer Ebraheem0% (1)
- One Hundred YearsDocumento18 páginasOne Hundred YearsolziichAinda não há avaliações
- GcsDocumento1 páginaGcsGhadeer EbraheemAinda não há avaliações
- Mansmed Surgery QbankDocumento7 páginasMansmed Surgery QbankGhadeer EbraheemAinda não há avaliações
- Medical Therapies for Antibody DeficienciesDocumento5 páginasMedical Therapies for Antibody DeficienciesGhadeer EbraheemAinda não há avaliações
- Leach and Lily Stanley - Last Updated On: Edit This Article View RevisionsDocumento7 páginasLeach and Lily Stanley - Last Updated On: Edit This Article View RevisionsGhadeer EbraheemAinda não há avaliações
- Arc Neonatal FlowchartDocumento1 páginaArc Neonatal FlowchartChander KantaAinda não há avaliações
- HIV and HIV CounsellingDocumento12 páginasHIV and HIV CounsellingGhadeer EbraheemAinda não há avaliações
- Neuro ExaminationDocumento82 páginasNeuro ExaminationGhadeer Ebraheem100% (1)
- Acid Base PhysiologyDocumento4 páginasAcid Base PhysiologyGhadeer EbraheemAinda não há avaliações
- RicketsDocumento7 páginasRicketsGhadeer EbraheemAinda não há avaliações
- PalsDocumento12 páginasPalsGhadeer EbraheemAinda não há avaliações
- 5 - Health Care System Awad Etc 2009Documento11 páginas5 - Health Care System Awad Etc 2009Ghadeer EbraheemAinda não há avaliações
- Inflamatory Bowel Disease: Dr. Samir IsmailDocumento82 páginasInflamatory Bowel Disease: Dr. Samir IsmailGhadeer EbraheemAinda não há avaliações
- Drugs Causing HirsutismDocumento1 páginaDrugs Causing HirsutismGhadeer EbraheemAinda não há avaliações
- Anatomy 2 MnemonicsDocumento46 páginasAnatomy 2 MnemonicsGhadeer EbraheemAinda não há avaliações
- Drugs Causing HirsutismDocumento1 páginaDrugs Causing HirsutismGhadeer EbraheemAinda não há avaliações
- Nephrotic SyndromeDocumento1 páginaNephrotic SyndromeGhadeer EbraheemAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Nicotine-Induced Conditioned Place Preference and Conditioned Place Aversion in MiceDocumento5 páginasNicotine-Induced Conditioned Place Preference and Conditioned Place Aversion in MiceAulas EspañolAinda não há avaliações
- Nicotine Replacement Therapy A Friend or FoeDocumento6 páginasNicotine Replacement Therapy A Friend or FoeVsh SngAinda não há avaliações
- Nicotine Dependence SyndromeDocumento51 páginasNicotine Dependence SyndromeTesitaAinda não há avaliações
- Accounting EstimatesniceDocumento34 páginasAccounting EstimatesniceAnthony Tunying MantuhacAinda não há avaliações
- Bio Investigatory ProjectDocumento16 páginasBio Investigatory Projectprism1702Ainda não há avaliações
- Alcohol and Tobacco AddictionDocumento6 páginasAlcohol and Tobacco AddictionVijayAinda não há avaliações
- Gateway Drugs: The Dangers of Cigarette SmokingDocumento20 páginasGateway Drugs: The Dangers of Cigarette SmokingAllorasaxAinda não há avaliações
- Forced Smoking Stories I'Ve CollectedDocumento241 páginasForced Smoking Stories I'Ve CollectedErnesto PazAinda não há avaliações
- Grade 9 IGCSE DRUGS ResourceDocumento18 páginasGrade 9 IGCSE DRUGS ResourceAnushka YadavAinda não há avaliações
- Vaping Effects and StatisticsDocumento5 páginasVaping Effects and StatisticsKanmaneAinda não há avaliações
- Principles of Drug Use During LactationDocumento18 páginasPrinciples of Drug Use During LactationMade SuryaAinda não há avaliações
- Quit SmokingDocumento44 páginasQuit SmokingTbwc UmiAinda não há avaliações
- Alkaloids Physiological EffectsDocumento25 páginasAlkaloids Physiological EffectsGiang Lam100% (1)
- Project Report On Drugs AddictionDocumento6 páginasProject Report On Drugs Addictionapi-246586162Ainda não há avaliações
- Cigarette Smoking Outline and EssayDocumento2 páginasCigarette Smoking Outline and Essaygie100% (1)
- Signals 2020 Tabex Update 02Documento5 páginasSignals 2020 Tabex Update 02Na MoAinda não há avaliações
- Tobacco and Vaping WorksheetDocumento8 páginasTobacco and Vaping Worksheetyork.yfzhouAinda não há avaliações
- Gangguan Yang Berhubungan Dengan Zat (Substance Abuse)Documento44 páginasGangguan Yang Berhubungan Dengan Zat (Substance Abuse)Mohamad Arifudin syahAinda não há avaliações
- Takashi NagaiDocumento11 páginasTakashi Nagaierni pabateAinda não há avaliações
- Bupropion and Other Non-Nicotine PharmacotherapiesDocumento3 páginasBupropion and Other Non-Nicotine PharmacotherapiesEstigma Universidad Del RosarioAinda não há avaliações
- Bidee Vs CigaretteDocumento6 páginasBidee Vs Cigarettescribd_427Ainda não há avaliações
- Botanical Pesticidesand Their Modeof ActionDocumento28 páginasBotanical Pesticidesand Their Modeof ActionChileshe SimonAinda não há avaliações
- Big Picture: AddictionDocumento16 páginasBig Picture: AddictionWellcome Trust100% (1)
- Nicotine and Its Overdose EffectsDocumento4 páginasNicotine and Its Overdose EffectsahmedaliAinda não há avaliações
- 2011 Mini Mock Trial Materials - FinalDocumento59 páginas2011 Mini Mock Trial Materials - FinalJacob Van BaalenAinda não há avaliações
- E-Cigarettes A 1-Way Street To Traditional Smoking and Nicotine Addiction For YouthDocumento4 páginasE-Cigarettes A 1-Way Street To Traditional Smoking and Nicotine Addiction For YouthAsd EfgAinda não há avaliações
- Drug Addiction: Biology ProjectDocumento9 páginasDrug Addiction: Biology Projectalan spacaerAinda não há avaliações
- Smoking EffectsDocumento7 páginasSmoking EffectstsikiAinda não há avaliações
- Effects of Tobacco Smoking and AlcoholDocumento13 páginasEffects of Tobacco Smoking and AlcoholRubiya TufailAinda não há avaliações
- Ieltsfever Academic Reading Practice Test 3 PDFDocumento10 páginasIeltsfever Academic Reading Practice Test 3 PDFchandaAinda não há avaliações