Escolar Documentos
Profissional Documentos
Cultura Documentos
The Role of Probiotic Cultures in The Control of Gastrointestinal Health
Enviado por
Dhayu Mart Hindrasyah PandiaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
The Role of Probiotic Cultures in The Control of Gastrointestinal Health
Enviado por
Dhayu Mart Hindrasyah PandiaDireitos autorais:
Formatos disponíveis
Symposium: Probiotic Bacteria: Implications for Human Health
The Role of Probiotic Cultures in the Control of Gastrointestinal Health1
Rial D. Rolfe
Department of Microbiology and Immunology, Texas Tech University Health Sciences Center, Lubbock, TX 79430
ABSTRACT The use of probiotics to enhance intestinal health has been proposed for many years. Probiotics are traditionally dened as viable microorganisms that have a benecial effect in the prevention and treatment of specic pathologic conditions when they are ingested. There is a relatively large volume of literature that supports the use of probiotics to prevent or treat intestinal disorders. However, the scientic basis of probiotic use has been rmly established only recently, and sound clinical studies have begun to be published. Currently, the best-studied probiotics are the lactic acid bacteria, particularly Lactobacillus sp. and Bidobacterium sp. However, other organisms used as probiotics in humans include Escherichia coli, Streptococcus sp., Enterococcus sp., Bacteroides sp., Bacillus sp., Propionibacterium sp. and various fungi. Some probiotic preparations contain mixtures of more than one bacterial strain. Probiotics have been examined for their effectiveness in the prevention and treatment of a diverse spectrum of gastrointestinal disorders such as antibiotic-associated diarrhea (including Clostridium difcileassociated intestinal disease), infectious bacterial and viral diarrhea (including diarrhea caused by rotavirus, Shigella, Salmonella, enterotoxigenic E. coli, Vibrio cholerae and human immunodeciency virus/ acquired immunodeciency disorder, enteral feeding diarrhea, Helicobacter pylori gastroenteritis, sucrase maltase deciency, inammatory bowel disease, irritable bowel syndrome, small bowel bacterial overgrowth and lactose intolerance. Probiotics have been found to inhibit intestinal bacterial enzymes involved in the synthesis of colonic carcinogens. There are many mechanisms by which probiotics enhance intestinal health, including stimulation of immunity, competition for limited nutrients, inhibition of epithelial and mucosal adherence, inhibition of epithelial invasion and production of antimicrobial substances. Probiotics represent an exciting prophylactic and therapeutic advance, although additional investigations must be undertaken before their role in intestinal health can be delineated clearly. J. Nutr. 130: 396S 402S, 2000. KEY WORDS:
Downloaded from jn.nutrition.org by guest on September 5, 2012
probiotics
intestinal disorders
Despite numerous therapeutic improvements, especially in the eld of antibiotics, gastrointestinal infections and their consequences remain a major clinical problem. In addition, there has been a dramatic increase in the incidence of antibiotic-resistant microbial pathogens. There is a concern that industry will no longer be able to develop effective antibiotics at a rate sufcient to compete with the development of microbial resistance to old antibiotics. These factors have renewed interest in the possibility of deliberately feeding benecial microorganisms to humans as an alternative to antibiotic therapy in gastrointestinal disorders. Probiotics are also an attractive treatment alternative because antibiotics, which further delay recolonization by normal colonic ora, can be avoided. This paper will focus on the evidence that probiotics
1 Presented at the symposium entitled Probiotic Bacteria: Implications for Human Health as part of the Experimental Biology 99 meeting held April 1721 in Washington, DC. This symposium was sponsored by the American Society for Nutritional Sciences and was supported in part by an educational grant from the National Dairy Council. The proceedings of this symposium are published as a supplement to The Journal of Nutrition. Guest editor for this supplement was Douglas B. DiRenzo, National Dairy Council, Rosemont, IL.
are useful in the prevention and treatment of gastrointestinal disorders in humans. Probiotics have been dened as viable microorganisms that (when ingested) have a benecial effect in the prevention and treatment of specic pathologic conditions (Havenaar and Huis int Veld 1992). The principle of using harmless bacteria for conquering pathogens has been recognized for many years. In fact, probiotics have been used for as long as people have eaten fermented foods. However, it was Metchnikoff at the turn of the century who rst suggested that ingested bacteria could have a positive inuence on the normal microbial ora of the intestinal tract (Metchnikoff 1907). He hypothesized that lactobacilli were important for human health and longevity, and promoted yogurt and other fermented foods as healthy. The belief in the benecial effects of probiotics is based on the knowledge that the intestinal ora can protect humans against infection and that disturbance of this ora can increase susceptibility to infection. Numerous in vivo and in vitro studies have shown that the normal intestinal ora is an extremely effective barrier against pathogenic and opportunistic microorganisms (Fuller 1991). Probiotics are usually targeted for use in intestinal disorders in which specic factors
0022-3166/00 $3.00 2000 American Society for Nutritional Sciences.
396S
PROBIOTICS AND GASTROINTENTINAL HEALTH
397S
(such as antibiotics, medication, diet or surgery) disrupt the normal ora of the gastrointestinal tract, making the host animal susceptible to disease. Examples of such diseases include antibiotic-induced diarrhea, pseudomembranous colitis and small bowel bacterial overgrowth. The goal of probiotic therapy is to increase the numbers and activities of those microorganisms suggested to possess health-promoting properties until such time that the normal ora can be reestablished. There are also intestinal disorders in which probiotics have been used prophylactically and/or therapeutically in which the role of disruption of normal ora in the disease process is less clear. These diseases include travelers diarrhea, Helicobacter pylori gastroenteritis and rotavirus diarrhea. Many microorganisms have been used or considered for use as probiotics. A probiotic preparation may contain one or several different strains of microorganisms. Because viable and biologically active microorganisms are usually required at the target site in the host, it is essential that the probiotic be able to withstand the hosts natural barriers against ingested bacteria. The most commonly used probiotics are strains of lactic acid bacteria (e.g., Lactobacillus, Bidobacterium and Streptococcus). The benecial effects of Lactobacillus and Bidobacterium have been discussed for decades. Bacteria in these two genera resist gastric acid, bile salts and pancreatic enzymes, adhere to intestinal mucosa and readily colonize the intestinal tract. They are considered important components of the gastrointestinal ora and are relatively harmless. Lactic acid bacteria have been demonstrated to inhibit the in vitro growth of many enteric pathogens including Salmonella typhimurium, Staphylococcus aureus, Escherichia coli, Clostridium perfringens and Clostridium difcile and have been used in both humans and animals to treat a broad range of gastrointestinal disorders (Meurman et al. 1995, Silva et al. 1987). Saccharomyces boulardii, a patented yeast preparation, is used in many countries as both a preventive and therapeutic agent for diarrhea and other gastrointestinal disorders caused by the administration of antimicrobial agents. S. boulardii possesses many properties that make it a potential probiotic agent; i.e., it inhibits the growth of a number of microbial pathogens in vivo and in vitro; its temperature optimum is 37C; it survives transit through the gastrointestinal tract; it is rapidly eliminated, however, when therapy is discontinued; and it is unaffected by antibiotic therapy (Blehaut et al. 1989, Boddy et al. 1991, Brugier and Patte 1975). This last property is important because many patients administered a probiotic are receiving concurrent antimicrobial therapy for conditions unrelated to the gastrointestinal tract. There have been hundreds of publications describing the use of probiotics to prevent and treat a variety of gastrointestinal disorders. However, only a few have contributed convincingly to our knowledge of the health effects of probiotics in humans. The majority of studies have been poorly designed (e.g., inadequately dened strains of microorganisms, variation in preparation and storage of probiotics, patient groups that are too small in size for statistical analysis or imprecise denitions of end points) and therefore not reproducible by other investigators. Only a relatively few studies have been conducted with sufcient subjects, proper controls and statistical analysis of the results. Intestinal disorders treated with probiotics Probiotics have been studied in the treatment and prevention of various intestinal disorders. However, as will be described below, evidence that probiotics are useful therapeuti-
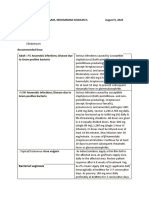
cally or prophylactically is available for only a few of these disorders. Antibiotic-induced diarrheal disease. Diarrhea is the most common side effect of antimicrobial therapy, with 20% of patients receiving an antibiotic developing this condition (Bartlett 1992). The pathogenesis of antibiotic-induced diarrhea is not understood but is undoubtedly related to quantitative and qualitative changes in the intestinal ora (Nord et al. 1986). Many of the studies that have attempted to demonstrate the usefulness of probiotics in antibiotic-associated diarrhea have used it prophylactically. However, because of the low incidence of antibiotic-associated diarrhea and the variable intensity of the diarrhea, it is not practical from a cost-benet viewpoint to treat all patients receiving antibiotic therapy in this way with a probiotic. Furthermore, it is not possible to predict which patients will develop antibiotic-associated diarrhea. Nonetheless, several probiotics have been used in an attempt to prevent antibiotic-associated diarrhea. These agents include Saccharomyces, Lactobacillus, Bidobacterium, and Streptococcus. However, only S. boulardii, E. faecium and Lactobacillus have been shown to be clinically effective in preventing antibiotic-associated diarrhea. Surawicz et al. (1989), in a prospective, double-blind, placebo-controlled study, treated 180 hospitalized patients receiving antibiotic therapy concurrently with either placebo or S. boulardii. The overall incidence of diarrhea in these patients was 26%; 22% of the patients receiving placebo developed diarrhea compared with 9% of patients receiving S. boulardii, a statistically signicant difference. Adam et al. (1977) prospectively treated 388 ambulatory patients, receiving either tetracycline or a -lactam, concurrently with placebo or S. boulardii. The incidence of diarrhea in patients receiving the placebo was 17.5%, whereas in patients receiving S. boulardii, it was 4.5%. These results were conrmed in another study of 193 patients receiving at least one broad-spectrum -lactam antibiotic (McFarland et al. 1995). Of the 97 patients receiving S. boulardii, only 7.2% developed antibiotic-associated diarrhea compared with 14.6% of the 96 patients receiving placebo. Lactinex, a commercial preparation containing Lactobacillus acidophilus and Lactobacillus bulgaricus, was used in a placebo-controlled study of 79 hospitalized patients receiving ampicillin (Gotz et al. 1979). The rationale for using Lactobacillus in these patients is based on the observation that antibiotic therapy often causes a loss or reduction in the number of intestinal Lactobacillus. Thirty-six patients received concurrent Lactinex and 43 patients received placebo. None of the patients receiving Lactinex developed ampicillin-induced diarrhea, whereas 14% of the placebo group developed diarrhea. In a multicenter, double-blind, placebo-controlled clinical trial involving 10 hospitals, Wunderlich et al. (1989) randomly assigned 45 antibiotic-treated patients to receive either concurrent placebo or Enterococcus faecium. Differences in the incidence of diarrhea were signicant; 27% of the placebo group developed diarrhea compared with 9% of the group receiving E. faecium. The general conclusion from these studies is that patients at risk of developing antibiotic-associated diarrhea would benet from prophylactic probiotic therapy. However, this becomes impractical because there is no way to identify these patients. Clostridium difcileassociated intestinal disease. C. difcile is a classic example of the opportunistic proliferation of an intestinal pathogen after breakdown of colonization resistance due to antibiotic administration. After antibiotic intake by animals and humans, C. difcile colonizes the intestine and releases two protein exotoxins, toxin A and toxin B, which
Downloaded from jn.nutrition.org by guest on September 5, 2012
398S
SUPPLEMENT
mediate the diarrhea and colitis caused by this microbe. Toxigenic C. difcile is the cause of 20 40% of cases of antibiotic-associated diarrhea (Clabots et al. 1992, Fekety and Shah 1993, McFarland et al. 1989). In fact, this microorganism is the major identiable cause of nosocomial diarrhea in the U.S., infecting 1525% of adult hospitalized patients. C. difcile can have serious consequences, particularly in the elderly and debilitated; these include pseudomembranous colitis, toxic megacolon, intestinal perforation and death. Standard treatment of C. difcileassociated intestinal disease, which involves either vancomycin or metronidazole, can be expensive and difcult. In addition, 25% of patients relapse with disease once treatment is discontinued (Bartlett et al. 1980, Fekety et al. 1989, Walters et al. 1983, Young et al. 1985). Multiple relapses can occur and the relapses can be more severe that the original disease. The mechanism of relapse is unknown but is probably due to the survival of C. difcile spores in the intestinal tract until the antibiotic is discontinued (Walters et al. 1983). The spores then germinate and produce toxin. The antibiotic therapy prevents the normal ora from reestablishing itself. There is no uniform effective therapy to prevent further C. difcile recurrences in intractable patients. An attractive alternative to antibiotic therapy is to use probiotics to restore intestinal homeostasis. Patients at risk of C. difcile intestinal disease can be identied in the sense that individuals that have had a previous relapse of C. difcile disease are more likely to have another relapse. Several alternative treatments have been used in C. difcileassociated intestinal disease. Rectal administration of feces from healthy adults has been examined in a very limited number of uncontrolled studies (Bowden et al. 1981, Schwan et al. 1984). This treatment appears to be moderately successful, but there is obvious concern about the use of a complex, mixed undened ora that could contain a number of potential pathogens. Additional uncontrolled studies have examined rectal infusion of 10 different aerobic and anaerobic bacteria as well as the use of a nontoxigenic strain of C. difcile (Borriello 1988, Tvede and Rask-Madsen 1989). Presumably these bacteria occupy niches that the toxigenic strain would expect to nd available. S. boulardii has demonstrated the most promise for use in C. difcileassociated intestinal disease. In a placebo-controlled study, McFarland et al. (1994) examined standard antibiotic therapy (metronidazole or vancomycin) with concurrent S. boulardii or placebo in 124 adult patients, 64 patients with an initial episode of C. difcile disease and 60 patients with a history of at least one prior episode of C. difcile disease. The investigators found that in patients with an initial episode of C. difcile, there was no signicant difference in the recurrence of C. difcile disease in the placebo or S. boulardii groups. However, in patients with prior C. difcile disease, S. boulardii signicantly inhibited further recurrences of disease. The investigators concluded that in combination with standard antibiotics, S. boulardii is an effective and safe therapy for patients with recurrent C. difcile. Probiotic treatment of infectious diarrhea It is very difcult to perform a critical analysis of studies that have examined the use of probiotics for the treatment and/or prevention of infectious diarrhea. First, there are many etiological agents that cause infectious diarrhea (e.g., Shigella, Salmonella, C. difcile, rotavirus, enterotoxigenic E. coli), and the majority of the studies do not attempt to dene the cause of the diarrhea. In addition, many of the studies involved only a small number of patients. Two of the more common types of
infectious diarrheal diseases will be described in greater detail below, i.e., travelers diarrhea and rotavirus diarrhea. Travelers diarrhea. The incidence of diarrhea in travelers to foreign countries varies from 20 to 50% depending on the origin and the destination of the traveler, as well as the mode of travel. Although various infectious agents can cause travelers diarrhea, enterotoxigenic E. coli is the most common. Even small attacks can interrupt a holiday, and the traveling public has a great interest in medications that could be used to prevent travelers diarrhea. Thus, a safe, inexpensive and effective drug against travelers diarrhea would have important public health implications. Several probiotics have been examined for their ability to prevent travelers diarrhea, including Lactobacillus, Bidobacterium, Streptococcus and Saccharomyces (Hilton et al. 1997, Oksanen et al. 1990, Scarpignato and Rampal 1995). These studies have involved several different groups of travelers such as Finnish travelers to Turkey, American travelers to Mexico, British soldiers to Belize and European travelers to Egypt. The results from these studies have been extremely variable. For example, in the study of Finnish travelers to Turkey, the travelers had two different destinations (Oksanen et al. 1990). In one destination, Lactobacillus GG provided protection against travelers diarrhea but failed to protect travelers at the other destination. Different etiologic agents may have involved in these two locations, but this possibility was not examined. Rotavirus diarrhea. Rotaviruses are a signicant cause of infant morbidity and mortality, particularly in developing countries (Majamaa et al. 1995, Middleton et al. 1977). The principal means of treatment is oral rehydration, although an effective vaccine that should decrease dramatically the health impact of rotavirus infections has recently become available. Lactobacillus has demonstrated some promise as a treatment for rotavirus infection (Isolauri et al. 1994, Kaila et al. 1992, Majamaa et al. 1995). Isolauri et al. (1991) treated 74 children (ages 4 45 mo) with diarrhea with either Lactobacillus GG or placebo. Approximately 80% of the children with diarrhea were positive for rotavirus. The investigators demonstrated that the duration of diarrhea was signicantly shortened (from 2.4 to 1.4 d) in patients receiving Lactobacillus GG. The effect was even more signicant when only the rotavirus-positive patients were analyzed. Helicobacter pylori gastroenteritis
H. pylori has recently been shown to be an important etiologic agent of chronic gastritis as well as gastric and duodenal ulcers. It has also been postulated that chronic H. pylori infection leads to stomach carcinoma. Lactobacillus has been shown to be antagonistic to H. pylori both in vitro and in a gnotobiotic murine model (Aiba et al. 1998, Kabir et al. 1997, Midolo et al. 1995). The results of the few studies with Lactobacillus that have been performed in humans are conicting, with some showing modest protection and others showing no protection. Hepatic encephalopathy Hepatic encephalopathy is a neurologic disorder caused by increased blood levels of ammonia. The ammonia is produced in the intestine by the action of bacterial ureases. The ammonia is absorbed and, in healthy individuals, is detoxied by the liver. However, in patients with liver failure, the blood concentration of ammonia can reach toxic levels. Investigators have postulated that it may be possible to use probiotics to decrease intestinal urease activity. For example, patients
Downloaded from jn.nutrition.org by guest on September 5, 2012
PROBIOTICS AND GASTROINTENTINAL HEALTH
399S
treated with L. acidophilus and neomycin show a greater decrease in fecal urease activity than patients treated with neomycin alone (Loguercio et al. 1987, Read et al. 1966, Scevola et al. 1989). The decreased fecal urease activities corresponded to lower serum ammonia levels and improvements in the clinical status of patients. HIV/AIDS diarrhea Diarrhea is a very serious consequence of human immunodeciency virus (HIV) infection. The etiology of this diarrhea is frequently unknown and there are no effective treatment modalities. However, S. boulardii was recently used to treat 33 HIV patients with chronic diarrhea (Born et al. 1993, SaintMarc et al. 1991). In these double-blind studies, 56% of patients receiving S. boulardii had resolution of diarrhea compared with only 9% of patients receiving placebo. Sucrase-isomaltase deciency Sucrase-isomaltase deciency is the most frequent primary disaccharidase deciency seen in humans. It is an inherited condition that leads to malabsorption of sucrose. The resulting bacterial fermentation of the sucrose leads to an accumulation of hydrogen in the colon, producing diarrhea, abdominal cramps and bloating. A sucrose-free diet causes a disappearance of symptoms. However, not all patients will follow such a diet. Harms et al. (1987) used Saccharomyces cerevisiae to treat eight children with sucrase-isomaltase deciency. These investigators demonstrated that in children given sucrose followed by S. cerevisiae, there was an improvement in both their hydrogen breath test and gastrointestinal symptoms. The investigators postulated that S. cerevisiae was supplying the missing enzymes. Lactose intolerance People throughout the world suffer from a congenital deciency of the enzyme -galactosidase. This deciency results in an inability to digest and absorb lactose. Bacteria metabolize the lactose and the resulting by-products cause abdominal cramping, bloating, diarrhea and nausea. Lactase-positive strains of bacteria (e.g., Lactobacillus, Bidobacterium and Streptococcus) are commonly added to pasteurized dairy products to increase digestibility of the lactose present in the dairy product (Gilliland and Kim 1984, Kim and Gilliland 1983, Pettoello et al. 1989). There are two probable mechanisms by which the addition of these bacteria is benecial, i.e., the reduction of lactose in the dairy product through fermentation and the replication of the probiotic in the gastrointestinal tract, which releases lactase. Inammatory bowel disease There are two inammatory bowel diseases, Crohns disease and ulcerative colitis; their etiologies are unknown but may be related to disturbances of the intestinal microbial ora (Fabia et al. 1993). Crohns disease is an idiopathic inammatory bowel disease that occurs from the mouth to the anus, although the terminal ileum is most common site of disease. The most common clinical manifestation of ulcerative colitis is an inammation of the colon. No specic treatment is available for either disease. Kruis et al. (1997) examined the Nissle strain of nonpathogenic E. coli (serotype O6:K5:H1) for its ability to prevent relapses of ulcerative colitis. Preliminary results look promising and suggest that this may be another option for maintenance therapy of ulcerative colitis.
Pouchitis Pouchitis is a complication of ileal reservoir surgery occurring in 10 20% of the patients who undergo surgical treatment for chronic ulcerative colitis. Bacteria overgrow in the pouch, resulting in degradation of the mucus overlaying the epithelial cells (Madden et al. 1990, Mortensen 1992, RuselerVan Embden et al. 1995). This results in inammation and symptoms that include bloody diarrhea, lower abdominal pain and fever. Investigators have postulated that Lactobacillus GG may be an effective therapeutic agent for pouchitis because it does not demonstrate mucus-degrading properties (RuselerVan Embden et al. 1995). Irritable bowel syndrome Irritable bowel syndrome is characterized by chronic, recurrent pain that occurs primarily during childhood. There is no specic treatment of this condition. However, a small, doubleblind, placebo-controlled, crossover study in Poland demonstrated a slight but signicant reduction in the severity of abdominal pain in individuals receiving L. plantarum (Niedzielin and Kordecki 1996). Small bowel bacterial overgrowth
Overgrowth of bacteria in the small intestine can have many causes, including blind loops, stenosis of the intestine, diverticula and motility disorders. Symptoms of small bowel overgrowth are frequently chronic and relapsing. Response to antibiotic treatment is often inadequate or incomplete. Surgical treatment is occasionally possible, but in many cases the underlying cause is not accessible for permanent treatment. Limited studies have suggested that L. plantarum and Lactobacillus GG may be helpful in eliminating the symptoms of small bowel bacterial overgrowth (Vanderhoof et al. 1998). Enteral feedingassociated diarrhea
Patients receiving nasogastric tube feeding frequently develop diarrhea. The mechanism of the diarrhea is not known, but investigators postulate that enteral feeding causes changes in normal ora that result in altered carbohydrate metabolism and subsequent diarrhea (Guenter et al. 1991). Two separate studies (both placebo-controlled and double blind) demonstrated a signicant reduction in diarrhea in these patients when they were given S. boulardii (Bleichner et al. 1997, Tempe et al. 1983). Carcinogenesis
Evidence is accumulating that the normal intestinal ora can inuence carcinogenesis by producing enzymes that transform precarcinogens into active carcinogens. These enzymes include glycosidase, -glucuronidase, azoreductase and nitroreductase (Goldin et al. 1980, Goldin 1990, Ling et al. 1994, Marteau et al. 1990, Pedrosa et al. 1995). There is some evidence that selected microorganisms may actually protect the host from this carcinogenic activity. There are three postulated mechanisms for this protection as follows: 1) the probiotic may inhibit the bacteria that are responsible for converting precarcinogens into carcinogens; 2) animal studies have shown that some probiotics inhibit tumor cell formation directly; and 3) some bacteria have been shown to bind and/or inactivate carcinogens (Orrhage et al. 1994, Rowland and Grasso 1975). Human volunteers receiving either L. acidophilus or L. casei have reduced levels of enzymes that convert
Downloaded from jn.nutrition.org by guest on September 5, 2012
400S
SUPPLEMENT
precarcinogens to carcinogens in their fecal specimens (Hayatsu and Hayatsu 1993, Lee and Salminen 1995, Lidbeck et al. 1992). Whether this leads to a reduced incidence of cancer is unknown. Obviously, more extensive investigations and clinical trials must be conducted before probiotics can be considered for cancer prevention. Mechanisms of action There are many proposed mechanisms by which probiotics may protect the host from intestinal disorders. The sum of all processes by which bacteria inhibit colonization by other strains is called colonization resistance. Much work remains to classify the mechanisms of action of particular probiotics against particular pathogens. In addition, the same probiotic may inhibit different pathogens by different mechanisms. Listed below is a brief description of mechanisms by which probiotics may protect the host against intestinal disease. Production of inhibitory substances. Probiotic bacteria produce a variety of substances that are inhibitory to both gram-positive and gram-negative bacteria. These inhibitory substances include organic acids, hydrogen peroxide and bacteriocins. These compounds may reduce not only the number of viable cells but may also affect bacterial metabolism or toxin production. Blocking of adhesion sites. Competitive inhibition for bacterial adhesion sites on intestinal epithelial surfaces is another mechanism of action for probiotics (Conway et al. 1987, Goldin et al. 1992, Kleeman and Klaenhammer 1982). Consequently, some probiotic strains have been chosen for their ability to adhere to epithelial cells. Competition for nutrients. Competition for nutrients has been proposed as a mechanism for probiotics. Probiotics may utilize nutrients otherwise consumed by pathogenic microorganisms. However, the evidence that this occurs in vivo is lacking. Degradation of toxin receptor. The postulated mechanism by which S. boulardii protects animals against C. difcile intestinal disease is through degradation of the toxin receptor on the intestinal mucosa (Castagliuolo et al. 1996 and 1999, Pothoulakis et al. 1993). Stimulation of immunity. Recent evidence suggests that stimulation of specic and nonspecic immunity may be another mechanism by which probiotics can protect against intestinal disease (Fukushima et al. 1998, Kaila et al. 1992, Link-Amster et al. 1994, Malin et al. 1996, Perdigon et al. 1986, Pouwels et al. 1996, Saavedra et al. 1994). For example, peroral administration of Lactobacillus GG during acute rotavirus diarrhea is associated with an enhanced immune response to rotavirus (Kaila et al. 1992). This may account for the shortened course of diarrhea seen in treated patients. The underlying mechanisms of immune stimulation are not well understood, but specic cell wall components or cell layers may act as adjuvants and increase humoral immune responses. Prebiotics and synbiotics As described above, the oral feeding of external microorganisms is one mechanism to increase the number of benecial bacteria in the intestine. Prebiotics is another mechanism. Prebiotics are dened as food supplements that are nondigestible by the host but that improve health by selectively stimulating the growth and/or activities of selected intestinal bacteria (Ballongue et al. 1997, Gibson and Roberfroid 1995). This increase in indigenous bacteria may in turn inhibit the growth of pathogenic species. Prebiotics are not hydrolyzed or
absorbed in the small intestine but are available as substrates for indigenous bacteria in the large intestine (Molis et al. 1996). All prebiotics to date have been carbohydrates, ranging in size from small sugar alcohols and disaccharides, to oligosaccharides and large polysaccharides. A probiotic can be combined with a prebiotic to form what is called a synbiotic (Gibson and Roberfroid 1995, Lewis and Freedman 1998). Colonization by an exogenous probiotic could be enhanced and extended by simultaneous administration of a prebiotic that the probiotic could utilize in the intestinal tract. To date, no well-conducted clinical trials in humans have tested prebiotics or synbiotics for prevention or treatment of intestinal disorders. SUMMARY Probiotics represent a potentially signicant therapeutic advance. In an effort to decrease reliance on antimicrobials, the time has clearly come to increase the exploration of the therapeutic applications of probiotics. There are too many reports describing the benecial effects of probiotics to dismiss this concept for preventing and treating a variety of intestinal disorders. Probiotics offer dietary means to support the balance of the intestinal ora. They may be used to counteract local immunological dysfunction, to stabilize the intestinal mucosal barrier function, to prevent infectious succession of pathogenic microorganisms and to inuence intestinal metabolism. However, any postulated benet from consumption of probiotics or prebiotics should be accepted as fact only after extensive, multicenter testing in human clinical trials. There are still many unresolved issues that can be answered only by well-designed and well-controlled clinical trials. It is important to remember that in vitro and animal studies are frequently not transferable to humans. There are many potential advantages to probiotics over conventional therapy, including relatively low cost, the fact that probiotics are unlikely to increase the incidence of antibiotic resistance, and the multiple mechanisms by which probiotics presumably inhibit pathogens, thereby decreasing the chances for development of resistance against the probiotic. In the future, probiotics must be subjected to the identical, rigorous scientic studies that are required of chemical drug entities, including randomized, placebo-controlled, doubleblind studies, pharmacokinetic studies (i.e., dose-dependent efcacy, absorption, distribution, metabolism, excretion and duration of effect) and multicenter trials to establish reproducibility. In the past, once efcacy had been demonstrated, few researchers have gone on to dene a pharmacodynamic prole of the probiotic nor have extensive efforts been directed at identifying mechanisms of action. The synbiotic concept must be tested more rigorously as must the use of multiple probiotic strain combinations. It will also be important to dene more clearly the mechanisms of action of various probiotics. This will permit the scientic rationale for the selection of the best species or strains to use against a particular pathogen. It may also permit the application of genetic engineering to enhance the activity of probiotics (Tannock 1997, Wagner et al. 1997). It should be possible to bring together the ability to survive in the intestinal tract with the ability to produce metabolites that are responsible for the probiotic effect. LITERATURE CITED
Adam, J., Barret, A. & Barret-Bellet, C. (1977) Essais cliniques controles en double insu de lultra-levure lyophilise e: e tude multicentrique par 25 me decins de 388 cases. Gaz. Med. Fr. 84: 20722078.
Downloaded from jn.nutrition.org by guest on September 5, 2012
PROBIOTICS AND GASTROINTENTINAL HEALTH
Aiba, Y., Suzuki, N., Kabir, A. M., Takagi, A. & Koga, Y. (1998) Lactic acidmediated suppression of Helicobacter pylori by the oral administration of Lactobacillus salivarius as a probiotic in a gnotobiotic murine model. Am. J. Gastroenterol. 93: 20972101. Ballongue, J., Schumann, C. & Quignon, P. (1997) Effects of lactulose and lactitol on colonic microora and enzymatic activity. Scand. J. Gastroenterol. (suppl. 222): 41 44. Bartlett, J. G. (1992) Antibiotic-associated diarrhea. Clin. Infect. Dis. 15: 573 581. Bartlett, J. G., Tedesco, F. J., Shull, S., Lowe, B. & Chang, T. (1980) Symptomatic relapse after oral vancomycin therapy of antibiotic-associated pseudomembranous colitis. Gastroenterology 78: 431 434. Blehaut, H., Massot, J., Elmer, G. W. & Levy, R. H. (1989) Disposition kinetics of Saccharomyces boulardii in man and rat. Biopharm. Drug Dispos. 10 4: 353364. Bleichner, G., Blehaut, H., Mentec, H. & Moyse, D. (1997) Saccharomyces boulardii prevents diarrhea in critically ill tube-fed patients. A multicenter, randomized, double-blind placebo-controlled trial. Intensive Care Med. 23: 517523. Boddy, A. V., Elmer, G. W., McFarland, L. V. & Levy, R. H. (1991) Inuence of antibiotics on the recovery and kinetics of Saccharomyces boulardii in rats. Pharm. Res. 8: 796 800. Born, P., Lersch, C., Zimmerhackl, B. & Classen, M. (1993) The Saccharomyces boulardii therapy of HIV-associated diarrhea (letter). Dtsch. Med. Wochenschr. 118: 765. Borriello, S. P. (1988) The application of bacterial antagonism in the prevention and treatment of Clostridium difcile infection of the gut. In: Anaerobes Today (Hardie, J. M., & Borriello, S. P., eds.), pp. 195202. John Wiley and Sons, London, UK. Bowden, T. A., Jr., Mansberger, A. R., Jr. & Lykins, L. E. (1981) Pseudomembraneous enterocolitis: mechanism for restoring oral homeostasis. Am. Surg. 47: 178 183. Brugier, S. & Patte, F. (1975) Antagonisme in vitro entre lultra-levure et diffe rent germes bacte riens. Med. Paris 45: 3 8. Castagliuolo, I., LaMont, J. T., Nikulasson, S. T. & Pothoulakis, C. (1996) Saccharomyces boulardii protease inhibits Clostridium difcile toxin A effects in the rat ileum. Infect. Immun. 64: 52255232. Castagliuolo, I., Riegler, M. F., Valenick, L., LaMont, J. T. & Pothoulakis, C. (1999) Saccharomyces boulardii protease inhibits the effects of Clostridium difcile toxins A and B in human colonic mucosa. Infect. Immun. 67: 302307. Clabots, C. R., Johnson, S., Olson, M. M., Peterson, L. R. & Gerding, D. N. (1992) Acquisition of Clostridium difcile by hospitalized patients: evidence for colonized new admissions as a source of infection. J. Infect. Dis. 166: 561567. Conway, P. L., Gorbach, S. L. & Goldin, B. R. (1987) Survival of lactic acid bacteria in the human stomach and adhesion to intestinal cells. J. Dairy Sci. 70: 112. Fabia, R., ArRajab, A., Johansson, M. L., Andersson, R., Willen, R., Jeppsson, B., Molin, G. & Bengmark, S. (1993) Impairment of bacterial ora in human ulcerative colitis and experimental colitis in the rat. Digestion 54: 248 255. Fekety, R. & Shah, A. B. (1993) Diagnosis and treatment of Clostridium difcile colitis. J. Am. Med. Assoc. 269: 7175. Fekety, R., Silva, J., Kauffman, C., Buggy, B. & Deery, H. G. (1989) Treatment of antibiotic-associated Clostridium difcile colitis with oral vancomycin: comparison of two dosage regimens. Am. J. Med. 86: 1519. Fukushima, Y., Kawata, Y., Hara, H., Terada, A. & Mitsuoka, T. (1998) Effect of a probiotic formula on intestinal immunoglobulin A production in healthy children. Int. J. Food Microbiol. 42: 39 44. Fuller, R. (1991) Probiotics in human medicine. Gut 32: 439 442. Gibson, G. R. & Roberfroid, M. B. (1995) Dietary modulation of the human colonic microbiota: introducing the concept of prebiotics. J. Nutr. 125: 1401 1412. Gilliland, S. E. & Kim, H. S. (1984) Effect of viable starter culture bacteria in yogurt on lactose utilization in humans. J. Dairy Sci. 67: 1 6. Goldin, B. R. (1990) Intestinal microora: metabolism of drugs and carcinogens. Ann. Med. 22: 43 48. Goldin, B. R., Gorbach, S. L., Saxelin, M., Barakat, S., Gualtieri, L. & Salminen, S. (1992) Survival of Lactobacillus species (strain GG) in human gastrointestinal tract. Dig. Dis. Sci. 37: 121128. Goldin, B. R., Swenson, L., Dwyer, J., Sexton, M. & Gorbach, S. L. (1980) Effect of diet and Lactobacillus acidophilus supplements on human fecal bacterial enzymes. J. Natl. Cancer Inst. 64: 255261. Gotz, V., Romankiewicz, J. A., Moss, J. & Murray, H. W. (1979) Prophylaxis against ampicillin-associated diarrhea with a lactobacillus preparation. Am. J. Hosp. Pharm. 36: 754 757. Guenter, P. A., Settle, R. G., Perlmutter, S., Marino, P. L., DeSimone, G. A. & Rolandelli, R. H. (1991) Tube feeding-related diarrhea in acutely ill patients. J. Parent. Enteral Nutr. 15: 277280. Harms, H. K., Bertele-Harms, R. M. & Bruer-Kleis, D. (1987) Enzyme-substitution therapy with the yeast Saccharomyces cerevisiae in congenital sucrase-isomaltase deciency. N. Engl. J. Med. 316: 1306 1309. Havenaar, R. & Huis int Veld, J.H.J. (1992) Probiotics: a general view. In: The Lactic Acid Bacteria in Health and Disease (Wood, B., ed.), pp. 209 224. Elsevier Applied Science, London, UK. Hayatsu, H. & Hayatsu, T. (1993) Suppressing effect of Lactobacillus casei
401S
administration on the urinary mutagenicity arising from ingestion of fried ground beef in the human. Cancer Lett. 73: 173179. Hilton, E., Kolakowski, P., Singer, C. & Smith, M. (1997) Efcacy of Lactobacillus GG as a diarrheal preventive in travelers. J. Travel Med. 4: 41 43. Isolauri, E., Juntunen, M., Rautanen, T., Sillanaukee, P. & Koivula, T. (1991) A human Lactobacillus strain (Lactobacillus casei sp strain GG) promotes recovery from acute diarrhea in children. Pediatrics 88: 90 97. Isolauri, E., Kaila, M., Mykkanen, H., Ling, W. H. & Salminen, S. (1994) Oral bacteriotherapy for viral gastroenteritis. Dig. Dis. Sci. 39: 25952600. Kabir, A. M., Aiba, Y., Takagi, A., Kamiya, S., Miwa, T. & Koga, Y. (1997) Prevention of Helicobacter pylori infection by lactobacilli in a gnotobiotic murine model. Gut 41: 49 55. Kaila, M., Isolauri, E., Soppi, E., Virtanen, E., Laine, S. & Arvilommi, H. (1992) Enhancement of the circulating antibody secreting cell response in human diarrhea by a human Lactobacillus strain. Pediatr. Res. 32: 141144. Kim, H. S. & Gilliland, S. E. (1983) Lactobacillus acidophilus as a dietary adjunct for milk to aid lactose digestion in humans. J. Dairy Sci. 66: 959 966. Kleeman, E. G. & Klaenhammer, T. R. (1982) Adherence of Lactobacillus species to human fetal intestinal cells. J. Dairy Sci. 65: 20632069. Kruis, W., Schutz, E., Fric, P., Fixa, B., Judmaier, G. & Stolte, M. (1997) Double-blind comparison of an oral Escherichia coli preparation and mesalazine in maintaining remission of ulcerative colitis. Aliment. Pharmacol. Ther. 11: 853 858. Lee, Y.-K. & Salminen, S. (1995) The coming age of probiotics. Trends Food Sci. Technol. 6: 241245. Lewis, S. J. & Freedman, A. R. (1998) Review article: the use of biotherapeutic agents in the prevention and treatment of gastrointestinal disease. Aliment. Pharmacol. Ther. 12: 807 822. Lidbeck, A., Nord, C. E., Gustafsson, J. A. & Rafter, J. (1992) Lactobacilli, anticarcinogenic activities and human intestinal microora. Eur. J. Cancer Prev. 1: 341353. Ling, W. H., Korpela, R., Mykkanen, H., Salminen, S. & Hanninen, O. (1994) Lactobacillus strain GG supplementation decreases colonic hydrolytic and reductive enzyme activities in healthy female adults. J. Nutr. 124: 18 23. Link-Amster, H., Rochat, F., Saudan, K. Y., Mignot, O. & Aeschlimann, J. M. (1994) Modulation of a specic humoral immune response and changes in intestinal ora mediated through fermented milk intake. FEMS Immunol. Med. Microbiol. 10: 55 63. Loguercio, C., Del Vecchio Blanco, C. & Coltorti, M. (1987) Enterococcus lactic acid bacteria strain SF68 and lactulose in hepatic encephalopathy: a controlled study. J. Int. Med. Res. 15: 335343. Madden, M. V., Farthing, M. J. & Nicholls, R. J. (1990) Inammation in ileal reservoirs: pouchitis. Gut 31: 247249. Majamaa, H., Isolauri, E., Saxelin, M. & Vesikari, T. (1995) Lactic acid bacteria in the treatment of acute rotavirus gastroenteritis. J. Pediatr. Gastroenterol. Nutr. 20: 333338. Malin, M., Suomalainen, H., Saxelin, M. & Isolauri, E. (1996) Promotion of IgA immune response in patients with Crohns disease by oral bacteriotherapy with Lactobacillus GG. Ann. Nutr. Metab. 40: 137145. Marteau, P., Pochart, P., Flourie, B., Pellier, P., Santos, L., Desjeux, J. F. & Rambaud, J. C. (1990) Effect of chronic ingestion of a fermented dairy product containing Lactobacillus acidophilus and Bidobacterium bidum on metabolic activities of the colonic ora in humans. Am. J. Clin. Nutr. 52: 685 688. McFarland, L. V., Mulligan, M. E., Kwok, R. Y. & Stamm, W. E. (1989) Nosocomial acquisition of Clostridium difcile infection. N. Engl. J. Med. 320: 204 210. McFarland, L. V., Surawicz, C. M., Greenberg, R. N., Elmer, G. W., Moyer, K. A., Melcher, S. A., Bowen, K. E. & Cox, J. L. (1995) Prevention of beta-lactamassociated diarrhea by Saccharomyces boulardii compared with placebo. Am. J. Gastroenterol. 90: 439 448. McFarland, L. V., Surawicz, C. M., Greenberg, R. N., Fekety, R., Elmer, G. W., Moyer, K. A., Melcher, S. A., Bowen, K. E., Cox, J. L., & Noorani, Z. (1994) A randomized placebo-controlled trial of Saccharomyces boulardii in combination with standard antibiotics for Clostridium difcile disease. J. Am. Med. Assoc. 271: 19131918. Metchnikoff, E. (1907) The Prolongation of Life. Heinemann, London, UK. Meurman, J. H., Antila, H., Korhonen, A. & Salminen, S. (1995) Effect of Lactobacillus rhamnosus strain GG (ATCC 53103) on the growth of Streptococcus sobrinus in vitro. Eur. J. Oral Sci. 103: 253258. Middleton, P. J., Szymanski, M. T. & Petric, M. (1977) Viruses associated with acute gastroenteritis in young children. Am. J. Dis. Child. 131: 733737. Midolo, P. D., Lambert, J. R., Hull, R., Luo, F. & Grayson, M. L. (1995) In vitro inhibition of Helicobacter pylori NCTC 11637 by organic acids and lactic acid bacteria. J. Appl. Bacteriol. 79: 475 479. Molis, C., Flourie, B., Ouarne, F., Gailing, M. F., Lartigue, S., Guibert, A., Bornet, F. & Galmiche, J. P. (1996) Digestion, excretion, and energy value of fructooligosaccharides in healthy humans. Am. J. Clin. Nutr. 64: 324 328. Mortensen, N. (1992) Restorative proctocolectomythe pouch operation: good or bad? Scand. J. Gastroenterol. (suppl 192): 130 135. Niedzielin, K. & Kordecki, H. (1996) Therapeutic usefulness of ProViva solution in the treatment of irritable bowel syndrome and hemorrhoids. Presented at the Symposium of Gastroenterology, Heiligenstadt, Germany. Nord, C. E., Heimdal, A. & Kager, L. (1986) Antimicrobial induced alterations of the human oropharyngeal and intestinal microora. Scand. J. Infect. Dis. 49: 64 72.
Downloaded from jn.nutrition.org by guest on September 5, 2012
402S
SUPPLEMENT
Scarpignato, C. & Rampal, P. (1995) Prevention and treatment of travelers diarrhea: a clinical pharmacological approach. Chemotherapy 41 (suppl. 1): 48 81. Scevola, D., Zambelli, A., Concia, E., Perversi, L. & Candiani, C. (1989) Lactitol and neomycin: monotherapy or combined therapy in the prevention and treatment of hepatic encephalopathy? Clin. Ther. 129: 105111. Schwan, A., Sjolin, S., Trottestam, U. & Aronsson, B. (1984) Relapsing Clostridium difcile enterocolitis cured by rectal infusion of normal faeces. Scand. J. Infect. Dis 16: 211215. Silva, M., Jacobus, N. V., Deneke, C. & Gorbach, S. L. (1987) Antimicrobial substance from a human Lactobacillus strain. Antimicrob. Agents Chemother. 31: 12311233. Surawicz, C. M., Elmer, G. W., Speelman, P., McFarland, L. V., Chinn, J. & van Belle, G. (1989) Prevention of antibiotic-associated diarrhea by Saccharomyces boulardii: a prospective study. Gastroenterology 96: 981988. Tannock, G. W. (1997) Probiotic properties of lactic-acid bacteria: plenty of scope for fundamental R & D. Trends Biotechnol. 15: 270 274. Tempe, J. D., Steidel, A. L., Blehaut, H., Hasselmann, M., Lutun, P. & Maurier, F. (1983) Prevention of diarrhea administering Saccharomyces boulardii during continuous enteral feeding. Sem. Hop. 59: 1409 1412. Tvede, M. & Rask-Madsen, J. (1989) Bacteriotherapy for chronic relapsing Clostridium difcile diarrhoea in six patients. Lancet 1: 1156 1160. Vanderhoof, J. A., Young, R. J., Murray, N. & Kaufman, S. S. (1998) Treatment strategies for small bowel bacterial overgrowth in short bowel syndrome. J. Pediatr. Gastroenterol. Nutr. 27: 155160. Wagner, R. D., Pierson, C., Warner, T., Dohnalek, M., Farmer, J., Roberts, L., Hilty, M. & Balish, E. (1997) Biotherapeutic effects of probiotic bacteria on candidiasis in immunodecient mice. Infect. Immun. 65: 4165 4172. Walters, B. A., Roberts, R., Stafford, R. & Seneviratne, E. (1983) Relapse of antibiotic associated colitis: endogenous persistence of Clostridium difcile during vancomycin therapy. Gut 24: 206 212. Wunderlich, P. F., Braun, L., Fumagalli, I., DApuzzo, V., Heim, F., Karly, M., Lodi, R., Politta, G., Vonbank, F. & Zeltner, L. (1989) Double-blind report on the efcacy of lactic acid-producing Enterococcus SF68 in the prevention of antibiotic-associated diarrhoea and in the treatment of acute diarrhoea. J. Int. Med. Res. 17: 333338. Young, G. P., Ward, P. B., Bayley, N., Gordon, D., Higgins, G., Trapani, J. A., McDonald, M. I., Labrooy, J. & Hecker, R. (1985) Antibiotic-associated colitis due to Clostridium difcile: double-blind comparison of vancomycin with bacitracin. Gastroenterology 89: 1038 1045.
Oksanen, P. J., Salminen, S., Saxelin, M., Hamalainen, P., Ihantola-Vormisto, A., Muurasniemi-Isoviita, L., Nikkari, S., Oksanen, T., Porsti, I., & Salminen, E. (1990) Prevention of travellers diarrhoea by Lactobacillus GG. Ann. Med. 22: 5356. Orrhage, K., Sillerstrom, E., Gustafsson, J. A., Nord, C. E. & Rafter, J. (1994) Binding of mutagenic heterocyclic amines by intestinal and lactic acid bacteria. Mutat. Res. 311: 239 248. Pedrosa, M. C., Golner, B. B., Goldin, B. R., Barakat, S., Dallal, G. E. & Russell, R. M. (1995) Survival of yogurt-containing organisms and Lactobacillus gasseri (ADH) and their effect on bacterial enzyme activity in the gastrointestinal tract of healthy and hypochlorhydric elderly subjects. Am. J. Clin. Nutr. 61: 353359. Perdigon, G., de Macias, M. E., Alvarez, S., Oliver, G. & de Ruiz Holgado, A. A. (1986) Effect of perorally administered lactobacilli on macrophage activation in mice. Infect. Immun. 53: 404 410. Pettoello, M. M., Guandalini, S., Ecuba, P., Corvino, C. & di Martino, L. (1989) Lactose malabsorption in children with symptomatic Giardia lamblia infection: feasibility of yoghurt supplementation. J. Pediatr. Gastroenterol. 9: 295230. Pothoulakis, C., Kelly, C. P., Joshi, M. A., Gao, N., OKeane, C. J., Castagliuolo, I. & Lamont, J. T. (1993) Saccharomyces boulardii inhibits Clostridium difcile toxin A binding and enterotoxicity in rat ileum. Gastroenterology 104: 1108 1115. Pouwels, P. H., Leer, R. J. & Boersma, W. J. (1996) The potential of Lactobacillus as a carrier for oral immunization: development and preliminary characterization of vector systems for targeted delivery of antigens. J. Biotechnol. 44: 183192. Read, A. E., McCarthy, C. F., Heaton, K. W. & Laidlaw, J. (1966) Lactobacillus acidophilus (Enpac) in treatment of hepatic encephalopathy. Br. Med. J. 5498: 12671269. Rowland, I. R. & Grasso, P. (1975) Degradation of N-nitrosamines by intestinal bacteria. Appl. Microbiol. 29: 712. Ruseler-Van Embden, J.G.H., Hazenberg, M. P., Van Lieshout, L.M.C. & Schouten, W. R. (1995) Instability of the pouch ora: cause of pouchitis? Microecol. Ther. 23: 81 88. Saavedra, J. M., Bauman, N. A., Oung, I., Perman, J. A. & Yolken, R. H. (1994) Feeding of Bidobacterium bidum and Streptococcus thermophilus to infants in hospital for prevention of diarrhoea and shedding of rotavirus. Lancet 344: 1046 1049. Saint-Marc, T., Rossello-Prats, L. & Touraine, J. L. (1991) Efcacy of Saccharomyces boulardii in the treatment of diarrhea in AIDS (letter). Ann. Med. Intern. 142: 64 65.
Downloaded from jn.nutrition.org by guest on September 5, 2012
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Every Patient Tells A Story by Lisa Sanders, M.D. - ExcerptDocumento24 páginasEvery Patient Tells A Story by Lisa Sanders, M.D. - ExcerptCrown Publishing Group76% (17)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Pedoman Pws KiaDocumento76 páginasPedoman Pws KiaDhayu Mart Hindrasyah PandiaAinda não há avaliações
- HWKKS Oncology Posting Mos HandbookDocumento11 páginasHWKKS Oncology Posting Mos HandbookJing WongAinda não há avaliações
- Kunci Jawaban Soal To 1 RegulerDocumento1 páginaKunci Jawaban Soal To 1 RegulerDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Algo Acs PDFDocumento1 páginaAlgo Acs PDFNety Pandung SalembanAinda não há avaliações
- Prodia Awam Brosur PremaritalDocumento2 páginasProdia Awam Brosur PremaritalDhayu Mart Hindrasyah PandiaAinda não há avaliações
- 1 Efficacy and Safety of GabapentinDocumento9 páginas1 Efficacy and Safety of GabapentinDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Environmental Diseases Environmental Diseases From A To ZDocumento8 páginasEnvironmental Diseases Environmental Diseases From A To ZDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Glue Ear - Picture SummaryDocumento4 páginasGlue Ear - Picture SummaryDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Occupational Health ServicesDocumento6 páginasOccupational Health ServicesDhayu Mart Hindrasyah PandiaAinda não há avaliações
- On The Job Foot HealthDocumento2 páginasOn The Job Foot HealthDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Sexually Transmitted InfectionsDocumento6 páginasSexually Transmitted InfectionsDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Venue ListDocumento6 páginasVenue ListDhayu Mart Hindrasyah PandiaAinda não há avaliações
- FBPZ 3 12 2009 FB17 OgataDocumento24 páginasFBPZ 3 12 2009 FB17 OgataDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Preventive Occ HealthDocumento1 páginaPreventive Occ HealthDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Glue EarDocumento5 páginasGlue EarDhayu Mart Hindrasyah PandiaAinda não há avaliações
- HaemorrhoidsDocumento4 páginasHaemorrhoidsDhayu Mart Hindrasyah PandiaAinda não há avaliações
- UriDocumento3 páginasUriDhayu Mart Hindrasyah PandiaAinda não há avaliações
- DyspepsiaDocumento5 páginasDyspepsiaDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Sore ThroatDocumento3 páginasSore ThroatDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Nonspecific Lower Back Pain in AdultsDocumento6 páginasNonspecific Lower Back Pain in AdultsDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Cough MedicinesDocumento4 páginasCough MedicinesDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Tests For Sexually Transmitted InfectionsDocumento5 páginasTests For Sexually Transmitted InfectionsDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Acid Reflux and OesophagitisDocumento4 páginasAcid Reflux and OesophagitisDhayu Mart Hindrasyah PandiaAinda não há avaliações
- H2 BlockersDocumento3 páginasH2 BlockersDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Proton Pump InhibitorsDocumento4 páginasProton Pump InhibitorsDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Stomach (Gastric) UlcerDocumento4 páginasStomach (Gastric) UlcerDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Ear Infection (Otitis Media)Documento3 páginasEar Infection (Otitis Media)Dhayu Mart Hindrasyah PandiaAinda não há avaliações
- AntacidsDocumento3 páginasAntacidsDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Cramps in The LegDocumento3 páginasCramps in The LegDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Blocked Nose in Babies ('Snuffles')Documento2 páginasBlocked Nose in Babies ('Snuffles')Dhayu Mart Hindrasyah PandiaAinda não há avaliações
- Antihelmintics - Medicines For WormsDocumento3 páginasAntihelmintics - Medicines For WormsDhayu Mart Hindrasyah PandiaAinda não há avaliações
- Stool Specimen Collection PDFDocumento8 páginasStool Specimen Collection PDFJane CalderonAinda não há avaliações
- Clindamycin Dose, Uses, Side EffectsDocumento4 páginasClindamycin Dose, Uses, Side EffectsKenMAinda não há avaliações
- Ranicef Tablets Cefdinir Tablets 300MG FidsonDocumento13 páginasRanicef Tablets Cefdinir Tablets 300MG FidsonWright JohnAinda não há avaliações
- Diagnostic CD RecentDocumento9 páginasDiagnostic CD Recenthealing hopeAinda não há avaliações
- Clostridium Difficile-Associated Diarrhea (CDAD) Has Been Reported. Evaluate Patients If Diarrhea Occurs. (5.2)Documento2 páginasClostridium Difficile-Associated Diarrhea (CDAD) Has Been Reported. Evaluate Patients If Diarrhea Occurs. (5.2)Alokh Saha RajAinda não há avaliações
- Amoxicillin Clavulanic Acid Prescribing InformationDocumento25 páginasAmoxicillin Clavulanic Acid Prescribing InformationMohammed shamiul ShahidAinda não há avaliações
- Patient Guide: Everything You Need To Know About Your Stay at Houston Methodist Baytown HospitalDocumento42 páginasPatient Guide: Everything You Need To Know About Your Stay at Houston Methodist Baytown HospitalFirst Baptist ChurchAinda não há avaliações
- MDRO - IS - TrainingSlides Multidrug Resistant Organism (MDRO)Documento42 páginasMDRO - IS - TrainingSlides Multidrug Resistant Organism (MDRO)Isworo RukmiAinda não há avaliações
- Dalbavancin drug application formDocumento6 páginasDalbavancin drug application formMd. Abdur RahmanAinda não há avaliações
- 2013 AAFP Acute Diarrhea PDFDocumento11 páginas2013 AAFP Acute Diarrhea PDFJoseph AndradeAinda não há avaliações
- PDF Share Prescribing Information: Mechanism of ActionDocumento3 páginasPDF Share Prescribing Information: Mechanism of Actionmehul da aviatorAinda não há avaliações
- eMRCS Microbiology 19 QuestionsDocumento7 páginaseMRCS Microbiology 19 QuestionsSaad KhanAinda não há avaliações
- El Malo El ClostridiumDocumento10 páginasEl Malo El Clostridiumocamb774340Ainda não há avaliações
- Stahlmann-2013-Risk Associated With Therapeutic Use of FQ-Expert Opinion Drug SafetyDocumento9 páginasStahlmann-2013-Risk Associated With Therapeutic Use of FQ-Expert Opinion Drug SafetyAndy KumarAinda não há avaliações
- 50 Gen Questions With Ans CKLRDocumento7 páginas50 Gen Questions With Ans CKLRSeanmarie CabralesAinda não há avaliações
- The Brigham Intensive Review of Internal Medicine Question Amp Answer Companion e Book 2nbsped 9780323597210 2017042502Documento552 páginasThe Brigham Intensive Review of Internal Medicine Question Amp Answer Companion e Book 2nbsped 9780323597210 2017042502Taha SabahAinda não há avaliações
- Ciprofloxacin TAB MonographDocumento56 páginasCiprofloxacin TAB MonographSelvi RahmatiaAinda não há avaliações
- Clinical Manifestations, Diagnosis, and Prognosis of Crohn Disease in Adults - UpToDateDocumento45 páginasClinical Manifestations, Diagnosis, and Prognosis of Crohn Disease in Adults - UpToDateAsclepioAinda não há avaliações
- 0218 Acute Gastroenteritis EvidenceDocumento25 páginas0218 Acute Gastroenteritis EvidenceCristian C BecerraAinda não há avaliações
- Phenoxymethyl Penicillin Penicillin V Tablet Prescribing InformationDocumento2 páginasPhenoxymethyl Penicillin Penicillin V Tablet Prescribing InformationitsshuvroAinda não há avaliações
- Super MrsaDocumento26 páginasSuper Mrsaapi-239003516Ainda não há avaliações
- Clindamycin 1Documento21 páginasClindamycin 1ksachchuAinda não há avaliações
- Birao Sas 13 Microbiology and ParasitologyDocumento9 páginasBirao Sas 13 Microbiology and ParasitologyFrancis Jacob Dejecacion GarcesAinda não há avaliações
- GIT SurgeryDocumento24 páginasGIT SurgerySaja Hussein95Ainda não há avaliações
- Pseudomembranous colitis causes beyond C difficileDocumento7 páginasPseudomembranous colitis causes beyond C difficileFitria FieraAinda não há avaliações
- Om Biomerieux Reagents Ot-43871 Package Insert-43871Documento3 páginasOm Biomerieux Reagents Ot-43871 Package Insert-43871Salomon SalomonAinda não há avaliações
- DRUG STUDY FOR 14-YEAR-OLD FEMALE PATIENTDocumento2 páginasDRUG STUDY FOR 14-YEAR-OLD FEMALE PATIENTBenjamin CañalitaAinda não há avaliações
- Health Care-Associated Infections - Best PracticesDocumento9 páginasHealth Care-Associated Infections - Best PracticesJoshua DiaoAinda não há avaliações