Escolar Documentos
Profissional Documentos
Cultura Documentos
Rheumatoid Arthritis
Enviado por
Franz Jonathan EgiptoDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Rheumatoid Arthritis
Enviado por
Franz Jonathan EgiptoDireitos autorais:
Formatos disponíveis
RHEUMATOID ARTHRITIS
Rheumatoid arthritis (RA) is a chronic, systemic inflammatory disease involving connective tissue and characterized by destruction and proliferation of the synovial membrane, resulting in joint destruction, ankylosis, and deformity. Although the cause is unknown, researchers speculate that a virus may initially trigger the bodys immune response, which then becomes chronically activated and turns on itself (autoimmune response). Immunologic mechanisms appear to play an important role in the initiation and perpetuation of the disease, in which spontaneous remissions and unpredictable exacerbations occur. RA is a disorder of the immune system and, as such, is a wholebody disease that can extend beyond the joints, affecting other organ systems, such as the skin and eyes. RA affects people differently. For some people it lasts only a few months or a year or two and then resolves without causing any noticeable damage. Some people have mild or moderate forms of the disease, with periods of exacerbation (called flares) and remission. Others have a severe form of the disease that is active most of the time, lasts for years or a lifetime and leads to serious joint damage and disability. Care Settings Community level unless surgical procedure is required. Related Concerns Psychosocial aspects of care Total joint replacement Client Assessment Database Data depend on severity and involvement of other organs (e.g., eyes, heart, lungs, kidneys), stage (i.e., acute exacerbation or remission), and coexistence of other forms of arthritis/autoimmune diseases. Activity/Rest May report: Joint pain and tenderness worsened by movement and stress placed on joint; morning stiffness (duration often l hr or more), usually occurs symmetrically Functional limitations affecting ADLs, desired lifestyle, leisure time, and occupation Fatigue; sleep disturbances May exhibit: Malaise Impaired ROM of joints, particularly hand (fingers and wrist), hips, knees, ankles, elbows, and shoulders Muscle atrophy, joint and muscle contractures/deformities Decreased muscle strength, altered gait/posture Cardiovascular May report: Intermittent pallor, cyanosis, then redness of fingers/toes before color returns to normal (Raynauds phenomenon) Ego Integrity
May report:
Acute/chronic stress factors (e.g., financial, employment, disability, relationship factors) Hopelessness and powerlessness (incapacitating situation) Threat to self-concept, body image, personal identity (e.g., dependence on others) Inability to obtain/consume adequate food/fluids (temporomandibular joint [TMJ] involvement) Anorexia, nausea Weight loss Dryness of oral mucous membranes, decreased oral secretions, dental caries (Sjgrens syndrome) Varying difficulty performing self-care activities; dependence on others Numbness/tingling of hands and feet, loss of sensation in fingers Symmetrical joint swelling Acute episodes of pain (may/may not be accompanied by soft-tissue swelling in joints), symmetrical pattern involving joints on both sides of the body Chronic aching pain and stiffness with mornings most difficult Red, swollen, hot joints (during acute exacerbations) Difficulty managing homemaker/maintenance tasks Persistent low-grade fever Dryness of eyes and mucous membranes Pale, shiny, taut skin; subcutaneous rounded, nontender nodules; lesions, leg ulcers Skin/periarticular local warmth, erythema Decreased muscle strength, altered gait, reduced ROM Difficulty engaging in sexual activity as desired/abstinence
Food/Fluid May report:
May exhibit:
Hygiene May report: Neurosensory May report: May exhibit: Pain/Discomfort May report:
May exhibit: Safety May report:
May exhibit:
Sexuality May report:
Social Interaction May report: Impaired interactions with family/others, change in roles, isolation Teaching/Learning May report: Familial history of RA (in juvenile onset) Usual onset between ages 25 and 50, ratio of women to men 3:1 Use of health foods, vitamins, untested arthritis cures History of pericarditis, valvular lesions, pulmonary fibrosis, pleuritis Discharge plan considerations: May require assistance with transportation, self-care activities, and homemaker/maintenance tasks; changes in physical layout of home
Refer to section at end of plan for postdischarge considerations. Diagnostic Studies Inflammatory markers: Cyclic citrullinated peptide (also called anti-CCP) antibody test: Useful in detecting early RA. If both CCP and RF are positive, it is likely the client has a more severe form of the disease. Rheumatoid factor (RF): Positive in more than 80% of cases, but may become positive later in disease process than CCP (Rose-Waaler test). Erythrocyte sedimentation rate (ESR): Usually greatly increased (80100 mm/hr). May return to normal as symptoms improve. Antinuclear antibody (ANA) titer: Screening test for rheumatic disorders, elevated in 25%30% of RA clients. Follow-up tests are needed for the specific rheumatic disorders; e.g., anti-RNP is used for differential diagnosis of systemic rheumatic disease. C-reactive protein (CRP): Test of protein produced only when inflammation is present; may be elevated with RA, but is not specific to RA. Latex fixation: Positive in 75% of typical cases. Agglutination reactions: Positive in more than 50% of typical cases. Serum complement: C3 and C4 increased in acute onset (inflammatory response). Immune disorder/exhaustion results in depressed total complement levels. CBC: Usually reveals moderate anemia (in approximately 80% of clients). WBC is elevated when inflammatory processes are present. Immunoglobulin (Ig) (IgM and IgG): Elevation strongly suggests autoimmune process as cause for RA. Radiographs of involved joints: Reveals soft-tissue swelling, erosion of joints and osteoporosis of adjacent bone (early changes) progressing to bone cyst formation, narrowing of joint space, and subluxation. Concurrent osteoarthritic changes may be noted. CT/MRI scans (joints and cervical spine): Identifies inflamed synovium. MRI may be necessary to demonstrate cord compression. Direct arthroscopy: Visualization of area reveals bone irregularities/degeneration of joint. Synovial/fluid aspirate: May reveal volume greater than normal; opaque, cloudy, yellow appearance (inflammatory response, bleeding, degenerative waste products); elevated levels of WBCs and leukocytes; decreased viscosity and complement (C3 and C4). Synovial membrane biopsy: Reveals inflammatory changes and development of pannus (inflamed synovial granulation tissue). Nursing Priorities 1. Alleviate pain. 2. Increase mobility. 3. Promote positive self-concept. 4. Support independence. 5. Provide information about disease process/prognosis and treatment needs. Discharge Goals
1. Pain relieved/controlled. 2. Client is dealing realistically with current situation. 3. Client is managing ADLs by self/with assistance as appropriate. 4. Disease process/prognosis and therapeutic regimen understood. 5. Plan in place to meet needs after discharge.
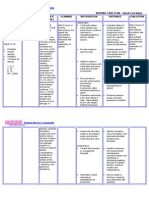
NURSING DIAGNOSIS: acute/chronic Pain May be related to Injuring agents: distention of tissues by accumulation of fluid/inflammatory process, destruction of joint Possibly evidenced by Reports of pain/discomfort, fatigue Self-narrowed focus Distraction behaviors/autonomic responses Guarding/protective behavior DESIRED OUTCOMES/EVALUATION CRITERIACLIENT WILL: Pain Level (NOC) Report pain is relieved/controlled. Appear relaxed, able to sleep/rest and participate in activities appropriately. Pain Control (NOC) Follow prescribed pharmacologic regimen. Incorporate relaxation skills and diversional activities into pain control program. ACTIONS/INTERVENTIONS Pain Management (NIC) Independent Investigate reports of pain, noting location and intensity (using 010/similar scale). Note precipitating factors and nonverbal pain cues. Recommend/provide firm mattress or bedboard, small pillow. Elevate linens with bed cradle as needed. Self-report should be the primary source of pain assessment in determining pain management needs and effectiveness of program. Soft/sagging mattress, large pillows prevent maintenance of proper body alignment, placing stress on affected joints. Elevation of bed linens reduces pressure on inflamed/painful joints. In severe disease/acute exacerbation, total RATIONALE
Suggest client assume position of comfort
while in bed or sitting in chair. Promote bed rest when indicated, but resume movement as soon as possible. .
bedrest may be necessary (until objective and subjective improvements are noted) to limit pain/injury to joint. Note: Immobility is known to worsen arthritis pain and stiffness.
Place/monitor use of pillows, sandbags, trochanter rolls, splints.
Rests painful joints and maintains neutral position. Note: Use of splints can decrease pain and may reduce damage to joint; however, prolonged inactivity can result in loss of joint mobility/function. Prevents general fatigue and joint stiffness. Stabilizes joint, decreasing joint movement and associated pain.
Encourage frequent changes of position. Assist client to move in bed, supporting affected joints above and below, avoiding jerky movements. Recommend that client take warm bath or shower on arising and/or at bedtime. Apply warm, moist compresses to affected joints several times a day. Monitor water temperature of compresses, baths, and so on. Provide gentle massage.
Heat promotes muscle relaxation and mobility, decreases pain, and relieves morning stiffness. Sensitivity to heat may be diminished and dermal injury may occur.
Promotes relaxation/reduces muscle tension.
Encourage use of stress management Promotes relaxation, provides sense of techniques; e.g., progressive relaxation, control, and may enhance coping abilities. biofeedback, visualization, guided imagery, self-hypnosis, and controlled breathing. Provide therapeutic touch. Involve in diversional activities appropriate for individual situation. Refocuses attention, provides stimulation, and enhances self-esteem and feelings of general well-being. Promotes relaxation, reduces muscle tension/spasms, facilitating participation in therapy. Severe/life threatening skin reactions (e.g., toxic epidermal necrolysis, StevensJohnson syndrome, and erythema multiforme) may develop within the first
Medicate before planned activities/exercises as indicated.
Monitor for development of skin rash in clients using COX-2 inhibitors, especially those allergic to sulfur.
two weeks of treatment or later on, indicating need for prompt discontinuation of medication. Collaborative Administer medications as indicated; e.g.: Because irreversible joint damage occurs within the first 2 years, early diagnosis and intervention is necessary. Medications are the mainstay of treatment. DMARDs may be started immediately, but due to their slow onset of action, NSAIDs and glucocorticoids may be prescribed until the antirheumatic drugs take effect. These slow-onset drugs (312 weeks) vary in action and may be used in combinations to reduce pain and swelling, lessening arthritic symptoms over time.
Disease-modifying antirheumatic drugs (DMARD); e.g., methotrexate (Rheumatrex), cyclosprine (Neoral), hydroxychloroquine (Plaquenil), sulfasalazine (Azulfidine); gold compounds; e.g., auranofin (Ridaura), azathioprine (Imuran), leflunomide (Arava); Biologicals; e.g., etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira); interleukin-1 receptor agonist; e.g., anakinra (Kinaret);
These injectable drugs are the first genetically engineered medications for arthritis. These anti-TNF compounds block inflammation and rapidly decrease pain and joint swelling. Enbrel is self-injected weekly and may be used in combination with methotrexate. Humira can be selfinjected every other week. Remicade is administered IV at 2- to 6-week intervals initially, then 1- to 3-month intervals. Note: Injection site reactions are the most common side effect noted with Humira and Kinaret, but drug discontinuation is uncommon. One of the mainstays of treatment until the 1990s, ASA is still used to exert an antiinflammatory and mild analgesic effect, decreasing stiffness and increasing mobility. ASA must be taken regularly to sustain a therapeutic blood level. Research indicates that ASA has the lowest toxicity
Salicylates; e.g., aspirin (ASA, buffered and plain) (Acuprin, Ecotrin, ZORprin);
index of commonly prescribed NSAIDs. Nonsteroidal anti-inflammatory drugs (NSAIDs); e.g., ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), sulindac (Clinoril), prioxicam (Feldene), fenoprofen (Nalfon), diclofenac (Voltaren), ketoprofen (Orudis), ketorolac (Toradol), nabumetone (Relafen); Glucocorticosteroids; e.g., prednisone (Deltasone), methylprednisolone (Depo-Medrol), dexamethasone (Decadron); These drugs control mild to moderate pain and inflammation by inhibition of prostaglandin synthesis and allow for improvement in mobility and function.
Low-dose oral glucocorticosteroids should be considered for short-term use, especially in the first 2 years, as drugs modify the immune response and suppress inflammation and progression of joint erosion. A new class of medication, COX-2 inhibitors interfere with prostaglandin production, similarly to NSAIDs, but are less likely to harm the stomach lining or kidneys. May be used in combination with other medications. Note: Recent controversy about these drugs resulted in Vioxx being withdrawn from the market, then restored by the FDA. These drugs should be used with caution in clients with significant hypertension, renal disease, heart disease, or at high risk for cardiac involvement. Characteristics of anti-inflammatory and immune modifier effects coupled with ability to block metalloproteinases (associated with joint destruction) have resulted in modest benefits in research studies.
COX-2 inhibitors; e.g., celecoxib (Celebrex), rofecoxib (Vioxx), valdecoxib (Bextra);
Tetracyclines; e.g., minocycline (Minocin);
D-Penicillamine (Cuprimine)
May control systemic effects of RA synovitis and scleroderma if other therapies have not been successful. High rate of side effects (e.g., thrombocytopenia, leukopenia, aplastic anemia) necessitates
close monitoring. Note: Drug should be given between meals because drug absorption is impaired by food, as well as antacids and iron products. Antacids; e.g., misoprostol (Cytotec), omeprazole (Prilosec); Given with NSAID agents to minimize gastric irritation/discomfort, reducing risk of GI bleed.
Narcotic analgesics; e.g., morphine, Although narcotics are generally oxycodone, hydrocodone combinations. contraindicated because of chronic nature of condition, short-term use of these products may be required to control severe pain during periods of acute exacerbation. Note: Codeine and propoxyphene (Darvon) products should be avoided because of their side effects and limited analgesic effectiveness. Assist with physical therapies; e.g., paraffin glove, whirlpool baths. Apply ice or cold packs when indicated. Provides sustained heat to reduce pain and improve ROM of affected joints. Cold may relieve pain and swelling during acute episodes. Constant low-level electrical stimulus blocks transmission of pain sensations. Prosorba Column is a device similar to a kidney dialysis machine that removes substances from blood plasma that contribute to joint swelling and pain. The plasma is then returned to the clients blood stream. The offending antibodies are gone, decreasing the immune response. Corrective surgical procedures may be indicated to reduce pain and/or improve joint function and mobility.
Instruct in use/monitor effect of transcutaneous electrical nerve stimulator (TENS) unit if used. Assist with other modalities as indicated; e.g., blood filtration.
Prepare for surgical interventions; e.g., synovectomy, total joint replacement, joint fusion; tunnel release procedures, tendon repair.
NURSING DIAGNOSIS: impaired physical Mobility/ impaired Walking May be related to Skeletal deformity Pain, discomfort
Intolerance to activity, decreased muscle strength Possibly evidenced by Reluctance to attempt movement/inability to purposefully move within the physical environment Limited ROM, impaired coordination, decreased muscle strength/control and mass (late stages) DESIRED OUTCOMES/EVALUATION CRITERIACLIENT WILL: Mobility (NOC) Maintain position of function with absence/limitation of contractures. Maintain or increase strength and function of affected and/or compensatory body part. Demonstrate techniques/behaviors that enable resumption/continuation of activities. ACTIONS/INTERVENTIONS Exercise Therapy: Joint Mobility (NIC) Independent RATIONALE
Evaluate/continuously monitor degree of joint inflammation/pain.
Level of activity/exercise depends on progression/resolution of inflammatory process. Person with RA need a good balance between rest and exercise, with more rest when disease is active and more exercise when it is not. Systemic rest is mandatory during acute exacerbations and important throughout all phases of disease to reduce fatigue, improve strength. Maintains/improves joint function, muscle strength, and general stamina. Note: Inadequate exercise leads to joint stiffening, whereas excessive activity can damage joints. Maximizes joint function, maintains mobility.
Maintain bedrest/chair rest when indicated. Schedule activities providing frequent rest periods and uninterrupted nighttime sleep.
Assist with active/passive ROM and resistive exercises and isometrics when able.
Encourage client to maintain upright and erect posture when sitting, standing, walking.
Discuss/provide safety needs; e.g., raised
Helps prevent accidental injuries/falls.
chairs/toilet seat, use of handrails in tub/shower and toilet, proper use of mobility aids/wheelchair safety. Positioning (NIC) Reposition frequently using adequate personnel. Demonstrate/assist with transfer techniques and use of mobility aids; e.g., walker, cane, trapeze. Position with pillows, sandbags, trochanter roll. Provide joint support with splints. Relieves pressure on tissues and promotes circulation. Facilitates self-care and clients independence. Proper transfer techniques prevent shearing abrasions of skin. Promotes joint stability (reducing risk of injury) and maintains proper joint position and body alignment, minimizing contractures. Prevents flexion of neck.
Suggest using small/thin pillow under neck. Collaborative Provide foam/alternating pressure mattress.
Decreases pressure on fragile tissues to reduce risks of immobility/development of decubitus ulcers.
Exercise Therapy: Joint Mobility (NIC) Consult with physical/occupational therapists and vocational specialist. Useful in formulating exercise/activity program based on individual needs in identifying and reducing impairments in range of motion, flexibility, strength and endurance, and to instruct in joint protection strategies and mobility devices/adjuncts.
Self-Care Assistance: IADL (NIC) Determine appropriateness of/ability to use scooter or special enhancements to automobile (e.g., hand controls, wide mirrors). Facilitates movement within the environment, decreases fatigue, promotes independence.
NURSING DIAGNOSIS: disturbed Body Image/ineffective Role Performance May be related to
Changes in ability to perform usual tasks Increased energy expenditure, impaired mobility Possibly evidenced by Change in structure/function of affected parts Negative self-talk, focus on past strength/function, appearance Change in lifestyle/physical ability to resume roles, loss of employment, dependence on SO for assistance Change in social involvement; sense of isolation Feelings of helplessness, hopelessness DESIRED OUTCOMES/EVALUATION CRITERIACLIENT WILL: Psychosocial Adjustment: Life Change (NOC) Verbalize increased confidence in ability to deal with illness, changes in lifestyle, and possible limitations. Formulate realistic goals/plans for future.
ACTIONS/INTERVENTIONS Body Image [or] Role Enhancement (NIC) Independent Encourage verbalization about concerns of disease process, future expectations.
RATIONALE
Provides opportunity to identify fears/misconceptions and deal with them directly. Identifying how illness affects perception of self and interactions with others will determine need for further intervention/counseling. Verbal/nonverbal cues from SO may have a major impact on how client views self. Constant pain is wearing, and feelings of anger and hostility are common. Acceptance provides feedback that feelings are normal.
Discuss meaning of loss/change to client/SO. Ascertain how client views self in usual lifestyle functioning, including sexual aspects. Discuss clients perception of how SO perceives limitations. Acknowledge and accept feelings of grief, hostility, dependency.
Note withdrawn behavior, use of denial, or overconcern with body/changes.
Set limits on maladaptive behavior. Assist client to identify positive behaviors that will aid in coping. Involve client in planning care and scheduling activities. Assist with grooming needs as necessary. Give positive reinforcement for accomplishments.
May suggest emotional exhaustion or maladaptive coping methods, requiring more in-depth intervention/psychologic support. Helps client maintain self-control, which enhances self-esteem. Enhances feelings of competency/selfworth, encourages independence and participation in therapy. Maintaining appearance enhances selfimage. Allows client to feel good about self. Reinforces positive behavior. Enhances confidence.
Collaborative Refer to psychiatric counseling; e.g., psychiatric clinical nurse specialist, psychiatrist/psychologist, social worker. Administer medications as indicated; e.g., antianxiety and mood-elevating drugs. Client/SO may require ongoing support to deal with long-term/debilitating process.
May be needed in presence of severe depression until client develops more effective coping skills.
NURSING DIAGNOSIS: Self-Care Deficit (specify) May be related to Musculoskeletal impairment, decreased strength/endurance, pain on movement Depression Possibly evidenced by Inability to manage ADLs (feeding, bathing, dressing, and/or toileting) DESIRED OUTCOMES/EVALUATION CRITERIACLIENT WILL: Self-Care: Activities of Daily Living (ADL) (NOC) Perform self-care activities at a level consistent with individual capabilities. Self-Care: Instrumental Activities of Daily Living (IADL) (NOC) Demonstrate techniques/lifestyle changes to meet self-care needs. Identify personal/community resources that can provide needed assistance. ACTIONS/INTERVENTIONS Self-Care Assistance (NIC) Independent RATIONALE
Determine usual level of functioning (Functional Level Classification 04) before onset/exacerbation of illness and potential changes now anticipated. Maintain mobility, pain control, and exercise program. Assess barriers to participation in self-care. Identify/plan for environmental modifications. Allow client sufficient time to complete tasks to fullest extent of ability. Capitalize on individual strengths.
May be able to continue usual activities with necessary adaptations to current limitations.
Support physical/emotional independence.
Prepares for increased independence, which enhances self-esteem.
May need more time to complete tasks by self but provides an opportunity for greater sense of self-confidence and self-worth.
Collaborative Consult with rehabilitation specialists; e.g., occupational therapist. Helpful in determining assistive devices to meet individual needs; e.g., button hooks, long-handled shoehorn, reacher, hand-held shower head. Identifies problems that may be encountered because of current level of disability. Provides for more successful team efforts with others who are involved in care; e.g., occupational therapy team. May need additional kinds of assistance to continue in home setting.
Arrange home-health evaluation before discharge, with follow-up afterward.
Arrange for consult with other agencies; e.g., Meals on Wheels, home care service, nutritionist.
NURSING DIAGNOSIS: risk for impaired Home Maintenance Risk factors may include Long-term degenerative disease process Inadequate support systems Possibly evidenced by [Not applicable; presence of signs and symptoms establishes an actual diagnosis.] DESIRED OUTCOMES/EVALUATION CRITERIACLIENT WILL: Self-Care: Instrumental Activities of Daily Living (IADL) (NOC)
Maintain safe, growth-promoting environment. Demonstrate appropriate, effective use of resources. ACTIONS/INTERVENTIONS Home Maintenance Assistance (NIC) Independent Determine level of physical functioning using Functional Level Classification 04. Identifies degree of assistance/support required. For example, the level 0 client is completely able to perform usual activities of daily living (self-care, vocational, and avocational), whereas the level 4 client is limited in all these areas and does not participate in activity. Determines feasibility of remaining in/changing home layout to meet individual needs. Availability of personal resources and community supports will affect ability to problem-solve and choice of solutions. RATIONALE
Evaluate environment to assess ability to care for self.
Determine financial resources to meet needs of individual situation. Identify support systems available to client; e.g., extended family, friends/neighbors. Develop plan for maintaining a clean, healthful environment; e.g., sharing of household repair/tasks between family members or by contract services. Identify sources for necessary equipment; e.g., lifts, elevated toilet seat, wheelchair/scooter. Collaborative Coordinate home evaluation by occupational therapist/rehabilitation team.
Ensures that needs will be met on an ongoing basis.
Provides opportunity to acquire equipment before discharge.
Useful for identifying adaptive equipment, ways to modify tasks to maintain independence. Can facilitate transfer to/support continuation in home setting.
Identify/meet with community resources; e.g., visiting nurse, homemaker service, social services, senior citizens groups.
NURSING DIAGNOSIS: deficient Knowledge [Learning Need] regarding disease, prognosis, treatment, self-care, and discharge needs May be related to Lack of exposure/recall Information misinterpretation Possibly evidenced by Questions/request for information, statement of misconception Inaccurate follow-through of instructions, development of preventable complications DESIRED outcomes/evaluation criteriaclient will: Knowledge: Disease Process (NOC) Verbalize understanding of condition/prognosis, and potential complications. Knowledge: Treatment Regimen (NOC) Verbalize understanding of therapeutic needs. Develop a plan for self-care, including lifestyle modifications consistent with mobility and/or activity restrictions. ACTIONS/INTERVENTIONS Teaching: Disease Process (NIC) Independent Review disease process, prognosis, and future expectations. Discuss clients role in management of disease process through nutrition, medication, and balanced program of exercise and rest. Assist in planning a realistic and integrated schedule of activity, rest, personal care, drug administration, physical therapy, and stress management. Identify individually appropriate exercise program components; e.g., swimming, stationary bike, nonimpact aerobics. Provides knowledge base from which client can make informed choices. Goal of disease control is to suppress inflammation in joints/other tissues to maintain joint function and prevent deformities. Provides structure and defuses anxiety when managing a complex chronic disease process. RATIONALE
Can increase clients energy level and mental alertness, minimize functional limitations. Program needs to be customized based on joints involved/clients general condition to maximize effect and reduce risk of injury.
Stress importance of continued pharmacotherapeutic management.
Benefits of drug therapy depend on correct dosage; e.g., aspirin must be taken regularly to sustain therapeutic blood levels of 1825 mg/dL. Coated/buffered preparations ingested with food minimize gastric irritation, reducing risk of bleeding/hemorrhage. Note: Nonacetylated products have a longer halflife, requiring less frequent administration in addition to producing less gastric irritation. Limits gastric irritation. Reduction of pain at hs enhances sleep, and increased blood level decreases early-morning stiffness.
Recommend use of enteric-coated/buffered aspirin or nonacetylated salicylates; e.g., choline salicylate (Arthropan) or choline magnesium trisalicylate (Trilisate).
Suggest taking medications, such as NSAIDs, with meals, milk products, or antacids and at bedtime.
Identify adverse drug effects; e.g., tinnitus, gastric intolerance, GI bleeding, purpuric rash.
Prolonged, maximal doses of aspirin may result in overdose. Tinnitus usually indicates high therapeutic blood levels. If tinnitus occurs, the dosage is usually decreased by 1 tablet every 23 days until it stops. Many products (e.g., cold remedies, antidiarrheals) contain hidden salicylates that increase risk of drug overdose/harmful side effects. Promotes general well-being and tissue repair/regeneration. Weight loss reduces stress on joints, especially hips, knees, ankles, feet.
Stress importance of reading product labels and refraining from OTC drug usage without prior medical approval.
Review importance of balanced diet with foods high in vitamins, protein, and iron. Encourage obese client to lose weight, and supply with weight reduction information as appropriate. Provide information about/resources for assistive devices; e.g., wheeled dolly/wagon for moving items, pickup sticks, lightweight dishes and pans, raised toilet seat, safety handlebars. Discuss energy-saving techniques; e.g. sitting instead of standing to prepare meals,
Reduces force exerted on joints and enables individual to participate more comfortably in needed/desired activities.
Prevents fatigue; facilitates self-care and independence.
shower, shave/apply make-up. Encourage maintenance of correct body position and posture both at rest and during activity; e.g., keeping joints extended, not flexed, wearing splints for prescribed periods, avoiding remaining in a single position for extended periods, positioning hands near center of body during use, and sliding rather than lifting objects when possible. Review safety issues related to mobility devices, especially electric scooters. Suggest use of a pennant when traveling on open streets. Good body mechanics must become a part of clients lifestyle to lessen joint stress and pain.
Ability to travel over uneven surfaces or gravel/soft ground is dependent upon specific scooter model. In addition, speed and safe maneuvering is equally important for the driver and other individuals in the vicinity. A pennant can be seen by other motorists.
Review necessity of frequent inspection of Reduces risk of skin irritation/breakdown. skin and meticulous skin care under splints, casts, supporting devices. Demonstrate proper padding. Discuss necessity of medical followup/laboratory studies; e.g., ESR, salicylate levels, PT. Drug therapy requires frequent assessment/refinement to ensure optimal effect and to prevent overdose/dangerous side effects; e.g., aspirin prolongs PT, increasing risk of bleeding. Information about different positions and techniques and/or other options for sexual fulfillment may enhance personal relationships and feelings of selfworth/self-esteem. Note: A large number of clients with RA are in childbearing years and need counseling, support, and medical interventions. Assistance/support from others promotes maximal recovery.
Provide for sexual and childbirth counseling as necessary.
Identify community resources; e.g., chapters of National Institute of Arthritis and Muscular and Skin Diseases (NIAMS), Arthritis Foundation.
POTENTIAL CONSIDERATIONS following acute hospitalization (dependent on clients age, physical condition/presence of complications, personal resources, and life responsibilities) Fatigueincreased energy requirements to perform ADLs, states of discomfort. chronic Painaccumulation of fluid/inflammation, destruction of joint. impaired physical Mobilityskeletal deformity, pain/discomfort, decreased muscle strength, intolerance to activity. Self-Care Deficit/ impaired Home Maintenancemusculoskeletal impairment, decreased strength/endurance, pain on movement, inadequate support systems, insufficient finances, unfamiliarity with neighborhood resources.
Você também pode gostar
- Rheumatoid ArthritisDocumento13 páginasRheumatoid ArthritisjhodaneAinda não há avaliações
- Juvenile Rheumatoid ArthritisDocumento3 páginasJuvenile Rheumatoid ArthritisYnos Sta TeresaAinda não há avaliações
- Juvenile Rheumatoid Arthritis: Jeffrey A. LuceroDocumento10 páginasJuvenile Rheumatoid Arthritis: Jeffrey A. LucerojamilliumAinda não há avaliações
- Case Study Rheumatoid ArthritisDocumento16 páginasCase Study Rheumatoid ArthritisJessy Mallo100% (2)
- Ra Case StudyDocumento52 páginasRa Case StudyMiracle Guillermo100% (4)
- NANDA NursingDocumento13 páginasNANDA NursingWaqas Javed0% (1)
- Nursing Process NUTRITIONDocumento82 páginasNursing Process NUTRITIONNoci M. FrenkAinda não há avaliações
- Geria Rle Week 6 Pain 1Documento1 páginaGeria Rle Week 6 Pain 1Maica LectanaAinda não há avaliações
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocumento4 páginasAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationMara Jon Ocden CasibenAinda não há avaliações
- Unit-Iii Gordon's Functional Health PatternsDocumento3 páginasUnit-Iii Gordon's Functional Health Patternsalphabennydelta4468Ainda não há avaliações
- Case Presentation OsteomylitisDocumento64 páginasCase Presentation OsteomylitisDemi Rose Bolivar100% (1)
- NCP-fluid Volume DeficitDocumento4 páginasNCP-fluid Volume DeficitChrissa Mae Aranilla MayoAinda não há avaliações
- CARE PLAN Case Study #2 PDFDocumento2 páginasCARE PLAN Case Study #2 PDFania ojedaAinda não há avaliações
- NCPDocumento10 páginasNCPNefre Dayap DarrocaAinda não há avaliações
- Urinary IncontinenceDocumento5 páginasUrinary IncontinencefakrulnersmudaAinda não há avaliações
- Impaired Physical MobilityDocumento2 páginasImpaired Physical MobilityHanya Bint PotawanAinda não há avaliações
- Final Major Case StudyDocumento17 páginasFinal Major Case Studyapi-546876878Ainda não há avaliações
- ArcoxiaDocumento27 páginasArcoxiaClarissa Mundo OlmilloAinda não há avaliações
- Cva Case StudyDocumento31 páginasCva Case StudyZoe AnnaAinda não há avaliações
- Multiple Sclerosis: Case Study by Trcoski ElenaDocumento43 páginasMultiple Sclerosis: Case Study by Trcoski ElenaElena TrcoskiAinda não há avaliações
- HyperphosphatemiaDocumento2 páginasHyperphosphatemiatephAinda não há avaliações
- Lupus Case ReportDocumento1 páginaLupus Case ReportMendy HararyAinda não há avaliações
- ScriptDocumento12 páginasScriptWaleed Nadeem50% (2)
- CellulitisDocumento12 páginasCellulitisAlma Bertos-Agub100% (1)
- 6 Nursing Care Plan 1Documento2 páginas6 Nursing Care Plan 1Denise Louise PoAinda não há avaliações
- Physical Assessment Appendix FinalDocumento6 páginasPhysical Assessment Appendix FinalLucelle ArellanoAinda não há avaliações
- Nasogastric Tube Feeding ML4763 PDFDocumento7 páginasNasogastric Tube Feeding ML4763 PDFStereo PodAinda não há avaliações
- NCP For OsteomyleitisDocumento5 páginasNCP For OsteomyleitisAyaBasilioAinda não há avaliações
- Chronic Pain NandaDocumento7 páginasChronic Pain NandaJude Bello-AlvearAinda não há avaliações
- AcknowledgementDocumento9 páginasAcknowledgementjhzenAinda não há avaliações
- Narratives Case NotesDocumento4 páginasNarratives Case NotesKnigh RiderAinda não há avaliações
- Goal Not MetDocumento4 páginasGoal Not MetAyaBasilioAinda não há avaliações
- Case Study Fracture 2 (Drug Study and NCP)Documento8 páginasCase Study Fracture 2 (Drug Study and NCP)chrom17Ainda não há avaliações
- Cholecystitis IntroductionDocumento4 páginasCholecystitis IntroductionJechelle Ann Pabustan Martin-BoniquitAinda não há avaliações
- Malnutrition in Older AdultsDocumento44 páginasMalnutrition in Older Adultsjohnjoe subaynoAinda não há avaliações
- Case Study 2Documento7 páginasCase Study 2desdav100% (1)
- Assessment Healt H Patte RN Nursing Diagnosis Desired Outcome (Edit) Intervention (Edit) Evaluation (EDIT) Rema RKSDocumento3 páginasAssessment Healt H Patte RN Nursing Diagnosis Desired Outcome (Edit) Intervention (Edit) Evaluation (EDIT) Rema RKStflorenzAinda não há avaliações
- Assess For Signs of HyperglycemiaDocumento9 páginasAssess For Signs of HyperglycemiaSheril Sularte CasanesAinda não há avaliações
- What Are The Signs and Symptoms of Heart Failure?Documento4 páginasWhat Are The Signs and Symptoms of Heart Failure?Lara TechiesAinda não há avaliações
- Nursing Care Plan ProjectDocumento12 páginasNursing Care Plan ProjectMj WilliamsAinda não há avaliações
- Nursing Care PlanDocumento4 páginasNursing Care Planssairej06100% (3)
- Treatment and Management of Rheumatoid ArthritisDocumento32 páginasTreatment and Management of Rheumatoid ArthritisamirthaAinda não há avaliações
- Ineffective Tissue Perfusion Secondary To Cellulitis DM Type 2Documento3 páginasIneffective Tissue Perfusion Secondary To Cellulitis DM Type 2MichaelaKatrinaTrinidadAinda não há avaliações
- GBS Management, Medications and Nursing ConsiderationsDocumento4 páginasGBS Management, Medications and Nursing Considerationssouledg3100% (1)
- GeriaDocumento2 páginasGeriaJackRolunaBernalesAinda não há avaliações
- Nursing Diagnosis: Urinary Retention: NOC Outcomes (Nursing Outcomes Classification)Documento4 páginasNursing Diagnosis: Urinary Retention: NOC Outcomes (Nursing Outcomes Classification)rem_Ainda não há avaliações
- General ObjectivesDocumento1 páginaGeneral ObjectivesErwin DegraciaAinda não há avaliações
- Impaired Physical MobilityDocumento2 páginasImpaired Physical Mobilitygianne121391Ainda não há avaliações
- Multiple SclerosisDocumento35 páginasMultiple SclerosisJc SeguiAinda não há avaliações
- Risk For Fall and Risk For Imbalanced Nutrition Less Than Body Requirements Pantoprazole, Ketorolac, Cefoxitin Drug StudyDocumento4 páginasRisk For Fall and Risk For Imbalanced Nutrition Less Than Body Requirements Pantoprazole, Ketorolac, Cefoxitin Drug StudyKevin John ReaLubit SaLisiAinda não há avaliações
- NCPDocumento9 páginasNCPLeolene Grace BautistaAinda não há avaliações
- Rheumatoid Arthritis Case DiscussionDocumento23 páginasRheumatoid Arthritis Case DiscussionJanieross LambosoAinda não há avaliações
- Cognitive Disorder QuizDocumento35 páginasCognitive Disorder QuizCamille Joy BaliliAinda não há avaliações
- Cellulitis Discharge PlanDocumento1 páginaCellulitis Discharge PlanJuvy Rose Tinga YeeAinda não há avaliações
- Nursing Care Plan For HematuriaDocumento2 páginasNursing Care Plan For HematuriaTee Wood63% (8)
- General Appearance: Ital SignDocumento4 páginasGeneral Appearance: Ital SignLiza Estrabo100% (1)
- Spinal Cord InjuryDocumento3 páginasSpinal Cord InjuryDan Leo UnicoAinda não há avaliações
- University of Cape Town Division of Occupational Therapy - Ahs3107W ArthritisDocumento7 páginasUniversity of Cape Town Division of Occupational Therapy - Ahs3107W ArthritisAlexaAinda não há avaliações
- Rheumatoid Arthritis: Case StudyDocumento9 páginasRheumatoid Arthritis: Case StudyMelody B. Miguel100% (1)
- Assignment Submitted To DR Iqra Naz 70063678 Habiba Jameel DPT 10 Semester. Topic: ArthritisDocumento10 páginasAssignment Submitted To DR Iqra Naz 70063678 Habiba Jameel DPT 10 Semester. Topic: ArthritisMuiz SaddozaiAinda não há avaliações
- Assumptions and Nature of ArtDocumento20 páginasAssumptions and Nature of ArtROLAND ROBLESAinda não há avaliações
- Career 1.Documento17 páginasCareer 1.[deeper]Ainda não há avaliações
- Teaching Presentation Rubric: Name of Student: Miss Daniela GalinganDocumento3 páginasTeaching Presentation Rubric: Name of Student: Miss Daniela GalinganDaniela GalinganAinda não há avaliações
- How Research Benefits Nonprofits Shao Chee SimDocumento24 páginasHow Research Benefits Nonprofits Shao Chee SimCamille Candy Perdon WambangcoAinda não há avaliações
- Assessment of The Prof. Level .Group 3Documento64 páginasAssessment of The Prof. Level .Group 3Patricia Vea Mae MalangisAinda não há avaliações
- Click Here: Thesis About Broken Family in The PhilippinesDocumento1 páginaClick Here: Thesis About Broken Family in The PhilippinesMary Anntoneth100% (1)
- Dont Just Memorize Your Next Presentation - Know It ColdDocumento5 páginasDont Just Memorize Your Next Presentation - Know It ColdatirapeguiAinda não há avaliações
- A Detailed Lesson Plan in EnglishDocumento2 páginasA Detailed Lesson Plan in EnglishMaria Vallerie FulgarAinda não há avaliações
- Assessing Alternate Sexualities: An Analysis of Mahesh Dattani's Play On A Muggy Night in MumbaiDocumento5 páginasAssessing Alternate Sexualities: An Analysis of Mahesh Dattani's Play On A Muggy Night in MumbaiYashika MalhotraAinda não há avaliações
- Job EvaluationDocumento11 páginasJob EvaluationAmirShahAinda não há avaliações
- MiskinDocumento8 páginasMiskinSam LinscottAinda não há avaliações
- Fun GamesDocumento7 páginasFun Gamesフェブリ クルニアントAinda não há avaliações
- Mid Term Report First Term 2014Documento13 páginasMid Term Report First Term 2014samclayAinda não há avaliações
- OCFINALEXAM2019Documento6 páginasOCFINALEXAM2019DA FT100% (1)
- Module 2 Personality Definition and Its ComponentsDocumento23 páginasModule 2 Personality Definition and Its ComponentsreignxeibcatimbangAinda não há avaliações
- OPVL Work-Activity Sheet - de MorgaDocumento2 páginasOPVL Work-Activity Sheet - de MorgaRachel Miranda GacutanAinda não há avaliações
- Week 4 - Developing Therapeutic Communication SkillsDocumento66 páginasWeek 4 - Developing Therapeutic Communication SkillsMuhammad Arsyad SubuAinda não há avaliações
- Ed 4265 - Introduction To The BreadwinnerDocumento6 páginasEd 4265 - Introduction To The Breadwinnerapi-239318668Ainda não há avaliações
- Generic Letter of Rec - Natalia Lopez Medrano 1Documento2 páginasGeneric Letter of Rec - Natalia Lopez Medrano 1api-460367917Ainda não há avaliações
- Top 10 Qualities of A Project ManagerDocumento3 páginasTop 10 Qualities of A Project ManagerAnonymous ggwJDMh8Ainda não há avaliações
- Helpling A Depressed Friend or Loved OneDocumento1 páginaHelpling A Depressed Friend or Loved OneCharles CilliersAinda não há avaliações
- Aqa Cat RM Criteria 2013-14Documento32 páginasAqa Cat RM Criteria 2013-14aneeshj1Ainda não há avaliações
- Case of Nico: Before The GloomDocumento5 páginasCase of Nico: Before The GloomHERALD LISINGAinda não há avaliações
- Revised-QAME-FORMS Upadated 2023Documento17 páginasRevised-QAME-FORMS Upadated 2023Ma. Theresia HiposAinda não há avaliações
- One Step Beyond Is The Public Sector Ready PDFDocumento27 páginasOne Step Beyond Is The Public Sector Ready PDFMuhammad makhrojalAinda não há avaliações
- GCS Assessment Aid English PDFDocumento1 páginaGCS Assessment Aid English PDFSila OntitaAinda não há avaliações
- Leadership Skills: BY Imitini, Elo Merit (Project Engineer)Documento16 páginasLeadership Skills: BY Imitini, Elo Merit (Project Engineer)Merit EloAinda não há avaliações
- ConclusionDocumento6 páginasConclusioncoribrooks4Ainda não há avaliações
- Communicating Assurance Engagement Outcomes and Performing Follow-Up ProceduresDocumento16 páginasCommunicating Assurance Engagement Outcomes and Performing Follow-Up ProceduresNuzul DwiAinda não há avaliações
- NCMHCE Sample Case StudiesDocumento17 páginasNCMHCE Sample Case Studiesbishakha styles100% (1)