Escolar Documentos
Profissional Documentos
Cultura Documentos
Claudio Solaro Michele Messmer Uccelli
Enviado por
Evangelos SpiridonDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Claudio Solaro Michele Messmer Uccelli
Enviado por
Evangelos SpiridonDireitos autorais:
Formatos disponíveis
C
R State of the Art
Pathophysiology Diagnosis Evaluation Therapy
1
Pain
Cl au di o S o l aro M i che l e Me ssme r Ucce l l i
IN TR OD UCTION Multiple sclerosis (MS) is one of the most common neurological diseases and involves inflammatory demyelination of the central nervous system. MS typically manifests between 20 and 40 years of age, although diagnosis can, less frequently, occur in childhood and later in life. The hallmarks of MS are its unpredictability and variability, across affected subjects as well as within the same individual. Common symptoms, among others, include visual impairment, sensory alterations, limb weakness, urinary dysfunction, fatigue, spasticity, cognitive dysfunction and pain (Paty and Ebers, 1998). Pain may be the most commonly treated symptom in MS, estimated to comprise 30% of all symptomatic treatment (Brichetto et al., 2003). Pain sufferers experience disruption in daily life activities, work, mood, recreation and overall quality of life, and report low satisfaction with pain management (Hadjimichael et al., 2007). Literature on pain management is lacking, particularly reports of randomised, double-blind trials, and treatment decisions are often based on clinicians experience. C L ASSIF ICATION OF PAIN SYNDRO M E S Pain is defined as an unpleasant sensory experience associated with actual or potential tissue damage or described in terms of such damage (IASP). Treede et al. classify pain syndromes as nociceptive somatic/visceral and neuropathic pain (Treede et al., 2008). Nociceptive pain occurs as an appropriate encoding of noxious stimuli and represents a physiological response transmitted to a conscious level when nociceptors in bone, muscle or any body tissue are activated, warning the organism of tissue damage, in turn, eliciting coordinated reflexes and behavioural responses. Neuropathic pain is typically initiated by a primary lesion or dysfunction in the peripheral or central nervous system, with no biological advantage (such as warning), causing suffering
Solaro_capitolo_01.indd 1
12/12/12 14:50
1 Pain
and distress. Clinical hallmarks are burning, dysesthetic, piercing pain, painful responses to non-painful stimuli (allodynia) and/or increased pain sensation when noxious stimuli are applied (hyperalgesia) (Treede et al., 2008). A 2008 report classifies pain associated with MS in four categories: continuous central neuropathic pain; intermittent central neuropathic pain (i.e. trigeminal neuralgia, Lhermittes; glossopharyngeal neuralgia); musculoskeletal pain (i.e. painful tonic spasms, pain secondary to spasticity, pain related to being wheelchair bound) and mixed neuropathic and non-neuropathic pain (i.e. headache) (OConnor et al., 2008). PREVAL ENCE OF PAIN Early estimates of the occurrence of pain in patients with MS ranged from 29% to 86% (Kraft et al., 1986; Moulin et al., 1988; Ehde et al., 2003; Svendsen et al., 2003; Solaro et al., 2004; Hadjimichael et al., 2007) although these numbers have been reconsidered based on more recent studies with large numbers of subjects. One of the largest epidemiological studies performed included 1,672 subjects and reported that 43% of patients with MS experience at least one type of pain (Solaro et al., 2004). In this study the presence of pain correlated with disability, disease course, disease duration and age but not with gender. PAIN SC ALE S Unfortunately, for assessing pain in patients with MS currently only generic pain scales are utilized since no disease-specific scale exists. Studies of pain in MS utilize visual analogue scales and numerical rating scales. While these certainly have some use in assessing pain intensity and unpleasantness, they may lack sufficient depth required to accurately describe the significance of neuropathic pain. PAIN AN D H E ALTH -RE LATE D QUA LI T Y OF LI FE Pain is linked to quality of life (QoL) in MS (Ehde et al., 2003; Kalia and OConnor, 2005). The influence of pain on QoL may be independent of the effect of disease impact, suggesting an interdependent relationship between depression, fatigue and pain. This confirms the importance of addressing MS comprehensively rather than adhering to a singlesymptom approach, since the successful management of one or more symptoms can often impact the status of others. C ON TIN UOUS CENTRAL NE URO PAT H I C PA I N
Pathophysiology
While important advances have been made in peripheral nervous system injury-related changes, the pathophysiology of central neuropathic pain is poorly defined. MS pain is thought to be a type of central pain due to demyelinating lesions in areas involved in pain perception.
Solaro_capitolo_01.indd 2
12/12/12 14:50
1 Pain
Experimental autoimmune encephalomyelitis (EAE) is an animal model of MS, inducible in various rodent strains by immunization with several myelin antigens, widely used in order to better understand the pathophysiology of the disease as well as the efficacy of medication. Although few reports in the literature have specifically studied pain in EAE, the availability of an animal model could represent an important step for understanding the mechanism underlying pain in MS and an opportunity to test pharmacological therapies. Aicher et al. (2004) used proteolipid protein (PLP) to induce active immunization (chronicrelapsing form) and PLP-splenocytes for passive induction in SJL mice. Nociceptive testing was done with withdrawal latencies to a radiant stimulus. In both models hypoalgesia peaked prior to the peak of motor deficits, while during the chronic phase of the disease the animals developed hyperalgesia. Thus, suggesting that EAE may be a useful model for pain. In a chronic-relapsing model of EAE, Olechowski et al. (2009) studied pain sensitivity and found a significant decrease in elicited pain behaviour. This behaviour was found to involve the glutamatergic system, suggesting a potential mechanism underlying neuropathic pain. Thibault et al. (2011) characterised sensory abnormalities including thermal and mechanical hyperalgesia and showed a partial effect of medications (gabapentin, duloxetine and tramadol) in two EAE models. Recently, it has been hypothesized that MS is an acquired channelopathy, sodium channel Nav1.8, of which expression is normally restricted to the peripheral nervous system, present in cerebellar Purkinje cells in a mouse model of MS. The ectopic expression of Nav 1.8 contributes to symptom development in the model. Dysregulated sodium channel expression on sensory fibers can lead to a functional change in axonal conduction contributing to neuropathic pain (Waxman, 2001). Although the theory is intriguing and several hypotheses can be made regarding the mechanisms of action of sodium channel blockers, such as antiepileptic drugs on pain in MS (i.e. carbamazepine), no data are available to draw definitive conclusions. Finally, while the field has gained insights into the pathophysiology of the mechanisms of neuropathic pain, particularly in animal models, their replication in human subjects is unknown.
Prevalence of central neuropathic pain
A number of studies have reported central neuropathic pain to be among the most common pain syndrome in MS with a prevalence of nearly 50% (Solaro et al., 2004). The classic signs of central pain such as hyperalgesia and allodynia have been reported in 38% of MS patients, although this frequency may seem lower in clinical practice perhaps in part due to patients difficulty in describing pain (Svendsen et al., 2003). Approximately 40% of patients describe a constant and burning sensation usually involving lower limbs, more frequently distally than proximally. Thirty percent describe this pain as a deep or muscular aching (Beiske et al., 2004). A recent study evaluated the location of lesions in MS patients with or without chronic pain using brain and spinal cord MRI. Thirteen MS patients with chronic pain and ten MS patients without pain were evaluated. There was no association between pain and site of demyelination (spinothalamic tract, dorsal column-medial lemniscus, dorsolateral funiculus, grey substance, thalamus or capsula interna) (Svendsen et al., 2011).
Solaro_capitolo_01.indd 3
12/12/12 14:50
1 Pain
Treatment of central neuropathic pain
The treatment includes tryciclic antidepressants, antiepileptic medications, intrathecal baclofen, opioid analgesics, anesthetic and antiarrhythmic agents, cannabinoids.
T r i c yc l i c a n t i d e p r e s s a n t s For addressing central neuropathic pain in MS amitriptyline, nortriptyline and clomipramine, all tricyclic antidepressants, are the drugs of choice. Drowsiness, constipation, urinary retention and hypotension are common adverse effects. There are no indications, based on randomised, clinical studies, as to overall efficacy or the most advantageous dosing schedules. A n t i e p i l e p t i c m e d i c at i o n s Antiepileptic medications are also used in treating central neuropathic pain associated with MS. Anecdotally, carbamazepine is commonly utilized, although often with inadequate results (Solaro et al., 2005). Adherence is problematic due to adverse effects, particularly when compared to other antiepileptic drugs, like gabapentin and lamotrigine. Discontinuation of carbamazepine occurs even at low doses. Only one randomized, double-blind, placebo-controlled, crossover study of lamotrigine has been reported, with only 12 subjects. At 400 mg/daily there was no difference between the treatment and placebo groups for change on mean pain intensity (Breuer et al., 2007). Levetiracetam has also been studied in a randomized, single-blind, placebo-controlled study, including 20 patients with MS with central pain. Levetiracetam significantly reduced pain at maximum dosage of 3,000 mg daily. Adverse events occurred in eight treated versus five placebo subjects, with one drop-out due to somnolence (Rossi et al., 2009). Gabapentin and pregabalin have not been assessed in randomized, placebo-controlled studies for the treatment of central neuropathic pain in MS. Reports of open-label studies including small numbers of subjects found these drugs to be moderately effective in relieving pain, although the occurrence of adverse events leading to discontinuation is common (Solaro et al., 2009; Houtchens et al., 1997). It is worth noting that in older patients a careful evaluation of the initiation dose and possible drug interactions should be undertaken since pregabalin can have a negative interaction with other drugs that act on the central nervous system, such as benzodiazepine, baclofen and tramadol (Solaro et al., 2009). The overall potential of antiepileptic drugs has not been substantiated in rigorous clinical trials. Unfortunately, many subjects never advance to the dose necessary for ameliorating pain due to intolerable adverse effects (Solaro et al., 2005). I n t r at h e c a l
bac lo f e n , o p i o i d a na lg e s i c s , a na e s t h e t i c
a n d a n t i a r r h y t h m i c ag e n t s
Intrathecal baclofen, opioid analgesics, anaesthetic and antiarrhythmic agents have been tested in patients with MS experiencing neuropathic pain, although with too few subjects and lacking sufficient scientific rigor. At this time, there is inadequate support for these drugs for the treatment of neuropathic pain in MS.
Solaro_capitolo_01.indd 4
12/12/12 14:50
1 Pain
Cannabinoids Cannabinoids (CB) have been rigorously assessed for the treatment of pain in MS. Four clinical trials have been reported in the literature. In one trial dronabinol, a synthetic CB, was successful in lowering pain intensity and improving pain relief at a daily dose of 10 mg, compared to a placebo group (Svendsen et al., 2004). Further, the treatment group reported improvement in bodily pain on the SF-36, a quality of life scale used in MS (Solari, 2005). A second, 5-week trial of an oromucosal spray form of a cannabis extract, D9-tetrahydrocannabinol (D9-THC), reported benefit in the treatment group on pain intensity, although treatment subjects experienced deficits in long-term memory storage. Sixty three of the original subjects continued in an open-label extension trial for up to two years in order to determine long-term tolerability and effectiveness (Rog et al., 2007). Improvement was reported on a VAS, although 51% of subjects experienced adverse events considered to be severe by investigators. A third, 15-week trial involved 630 subjects with a stable disease course experiencing spasticity (Zajicek et al., 2003). Pain was assessed as a secondary outcome, along with a number of other symptoms, using subjective scales. While most subjects in the treatment arm reported improvement in pain, 20% reported worsening while on treatment with CB. Finally, sublingual D9-THC, cannabidiol (CBD), D9-THC:CBD and placebo were compared in a consecutive series of double-blind, randomized, placebo-controlled, singlesubject, crossover trials. The design consisted of 2-week treatment phases and a subsequent double-blind phase of 8 weeks duration. Based on a VAS diary, active treatment significantly improved pain (Wade et al., 2004). In summary, while there does appear to be a positive effect, the efficacy of CB above conventional therapies has not been substantiated. Randomized trials comparing CB to traditional drugs for pain associated with MS is an important next step, in order to determine the most effective therapy, as well as to weigh the impact of adverse events. Studying different origins of pain syndromes associated with MS may also help explain individual response variability. Opioids Only one non-randomized, single-blind, placebo-controlled study of 14 subjects with MS-related central neuropathic pain used intravenous morphine at a median dose of 0.67 mg/kg body weight (Kalman et al., 2002). Four patients reported that pain was reduced by more than 50% after treatment. Clearly, insufficient evidence exists for the use of morphine for neuropathic pain in MS.
Solaro_capitolo_01.indd 5
12/12/12 14:50
1 Pain
IN TERM IT TE NT CE NTRAL NE URO PAT H I C PA I N
Trigeminal neuralgia
The prevalence of trigeminal neuralgia (TN) in subjects with MS ranges from 1.9% to 6.3% (Putzki et al., 2009). Although comparatively uncommon, TN has been extensively studied in MS. TN is exemplified by typically unilateral, intense, lancinating, paroxysmal pain deriving from one or more branches of the trigeminal nerve, although it is unclear whether there is a relationship between trigeminal lesions and clinical symptoms, despite extensive involvement of the entire trigeminal complex in some cases (Mills et al., 2010). The classic description by patients suffering from TN as an electrical discharge, as well as non-altered sensation and clear trigger points, makes idiopathic TN indistinguishable from TN seen in patients with MS.
P at h o p h y s i o l o g y TN is likely due to an electric ectopic discharge caused by a plaque at the TN nerve entry zone in the pons. The presence of a plaque in the proximal part of the trigeminal root was reported in an MS patient who underwent a rhizotomy for TN (Lazar e Kirkpatrick, 1979). Mixed results have been reported using MRI studies demonstrating multiple causes. A study reported enhancement on T1-weighted images and hyperintense lesions on T2weighted images of the cisternal portion of the nerve or at the root entry zone in eight out of 275 scans, although TN was not present (Da Silva et al., 2005). In a study of 74 Japanese subjects studied retrospectively, five (6.8%) showed a T1-hypointense and T2hyperintense, non-enhanced, linear lesion in the pons, in the intramedullary portion of the nerve that was associated with different sensory symptoms. Only one subject had TN (Nakashima et al., 2001). A further study of six MS patients with TN demonstrated that all subjects had a plaque in the pons, while no vascular compression was observed (Gass et al., 1997). The role of neurovascular compromise in TN has also been proposed. Meaney et al. (1995) found a plaque in the pons on MRI in one patient out of seven, while vascular compression of the nerve by an artery at the root entry zone was demonstrated in five subjects. A further study reported nerve compression in 23 of 35 (60%) cases (Broggi et al., 2004), while T2-weighted imaging demonstrated a brainstem lesion in 26 of 35 (74%) subjects. Trigeminal evoked potentials, infrequently used for MS patiens with TN, can help to indicate the site of lesions, as demonstrated in two studies in which 5/5 and 11/13 cases showed abnormal findings (Cruccu et al., 1990; Bergamaschi et al., 1994). M e d i c a l t r e at m e n t TN is reportedly extremely painful and can significantly interfere with everyday life. Due to ethical considerations, placebo-controlled studies are not possible. Treatment of TN in MS is based on studies of idiopathic TN and primarily consists of antiepileptic medications. Carbamazepine (Ramsaransing et al., 2000), lamotrigine (Leandri et al., 2000), gabapentin (Solaro et al., 1998), topiramate (Solaro et al., 2001) and misoprostol (DMKG Study Group, 2003) have all been assessed in open label studies, with small numbers of subjects. Table 1.1 provides a summary. The evidence is inadequate in providing indications as to the effectiveness of these drugs. It should be noted that carbamazepine may result in adverse effects that mimic an MS exacerbation (Ramsaransing et al., 2000).
Solaro_capitolo_01.indd 6
12/12/12 14:50
1 Pain
TabLE 1.1
Studies of medications for trigeminal neuralgia in MS. Authors Medications Number Mean dose of subjects 7 6 6 2 18 7 5 5 18 5 6 Efficacy Number of subjects with ae Not specified 0 0 Not specified 4 0 1 Not specified 0 0 0
Khan (1998) Solaro et al. (1998) Zvartau-Hind et al. (2000) Solaro et al. (2001) DMKG (2003) Reder and Arnason (1995) Espir and Millac (1970) Lunardi et al. (1997) Leandri et al. (2000) Solaro et al. (2000)
GBP GBP TPM TPM Misoprostol Misoprostol* CBZ LMT LMT LMT + GBP CBZ + GBP
1,400 mg/daily 6/7 complete 1/7 partial 900 mg/daily 100 mg/bid 200 mg/daily 200 mcg/tid 570 mcg/daily 760 mg/daily 165 mg/daily 170 mg/daily 140 mg + 650 mg/daily 400 mg + 800 mg/daily 5/6 5/6 2/2 5/18 4/7 complete 2/7 partial 4/5 5/5 17/18 5/5 6/6
*previous therapy maintained; AE: adverse events; CBZ: carbamazepine; GBP: gabapentin; LMT: lamotrigine; TPM: topiramate.
S u rg i c a l i n t e rv e n t i o n s Glicerol injection (Berk et al., 2003), radiofrequency lesioning (Broggi and Franzini, 1982) and radiosurgery (Rogers et al., 2002) are procedures that ablate the retrogasserian ganglion in order to interrupt the trigeminal pathway. These procedures have been used in MS patients with TN who have not responded to pharmacological treatment. These procedures cause nerve damage that may lead to adverse effects including hypoesthesia/hyperesthesia, decreased corneal reflex, transitory masticatory weakness and hearing loss, although these effects are uncommon. Microvascular decompression of the trigeminal root may be effective in carefully selected subjects, although recurrence of pain is relevant suggesting that combined mechanisms other than nerve compression have a role in the generation of TN in MS (Broggi et al., 1999). A lack of long-term benefit and the occurrence of potentially serious adverse effects dictates that surgical interventions should be reserved for critical non-responders to medications.
Atypical facial pain
Atypical facial pain is reported in MS although it is distinct from TN in that it is a dull and nearly continuous pain, whose site of origin is imprecise, without trigger points. One
Solaro_capitolo_01.indd 7
12/12/12 14:50
1 Pain
study underlined the complexity of differentiating facial pain syndromes in MS, finding six subjects out of 83 with TN and MS and two subjects with both atypical facial pain and TN, in addition to MS. Tricyclic antidepressants are commonly used for the treatment of atypical facial pain, with a regimen consisting of a single dose at bedtime of up to 100 mg prolonged over time up to several months (Elrasheed et al., 2004).
Lhermittes sign
Lhermittes sign, experienced by 40% of MS patients, is described as a painful electrical sensation that runs down the back and into the limbs from involvement of the posterior columns. Pain is elicited by flexing or extending the neck. Lhermittes sign is a common feature of MS but is not exclusive to the disease. Patients rarely request treatment (Al-Araji and Oger, 2005).
Glossopharyngeal neuralgia
Glossopharyngeal neuralgia is rare in MS. Pain is intense and occurs in the posterior pharynx, tonsillar fossa and base of the tongue. One report on three individuals with MS found a daily mean dose of 633 mg of carbamazepine to be successful in reducing pain (Minagar and Sheremata, 2000). M USC ULO SK E LE TAL PAIN
Painful tonic spasms
Painful tonic spasms (PTS) are described as cramping, pulling pain, more commonly occurring in the lower extremities although upper limbs can be affected as well, triggered by movements or sensory stimuli, often occurring during the night. It is estimated that 11% of subjects with MS experience PTS (Solaro et al., 2004). In MS the origin of the pain in PTS is caused by noxious stimuli of the muscle although the lesion eliciting the painful spasm is in the central nervous system.
T r e at m e n t o f P T S Anecdotally, medications such as baclofen, benzodiazepines, gabapentin and carbamazepine are used for treating PTS. Reports in the literature are limited to open-label studies of small numbers of subjects and thus cannot provide sufficient evidence for treatment recommendations.
Pain related to being wheelchair bound
In MS, patients with a moderate to advanced level of disability may have abnormal gait and often require technical aids for mobility and, for those more disabled, many may spend the majority of time in a wheelchair. Compromised posture, incorrect use of technical aids and prolonged wheelchair use can be causes of nociceptive pain in these patients. Specific studies regarding treatment are not available. Anecdotally treatment consists of anti-inflammatory drugs or opioids.
Solaro_capitolo_01.indd 8
12/12/12 14:50
1 Pain
C ON C L USIONS Unfortunately the literature on the treatment of pain in MS is seriously lacking and therefore does not provide indications based on rigorous scientific methods. Clinicians facing patients with MS and pain base treatment decisions on experience and on reports involving too few subjects in studies with insufficient levels of evidence. Studies on CB have produced useful scientific evidence, based on careful study design and adequate numbers of subjects, compared to studies on other medications for pain associated with MS. CB does appear to be useful for pain treatment, although a complete profile of adverse effects is lacking, including long-term data. Randomized trials comparing CB to traditional drugs for pain associated with MS is an important next step in order to examine whether CB is superior to conventional therapies. Further, since pain in MS is quite heterogeneous, future studies of CB should differentiate the origins of pain syndromes in order to help identify CB responders. Unfortunately MS does not occur in isolation and patients often have co-morbidities, particularly in the aging segment of the MS population. Clinicians should be aware that pain may have various origins and can be unrelated to MS. Pain can significantly impact quality of life, influencing everyday activities, work, recreation, mood, as well as other aspects. Therefore its correct identification and effective management are crucial. In addition to the complex nature of pain in MS, there are other factors that influence the approach to treatment. Firstly, scales are only partially effective in evaluating pain since they are based on subjectivity that can be influenced by various external factors. A further important aspect for clinicians to consider is that MS patients have difficulty describing neuropathic pain and this of course has a bearing on the clinical evaluation and subsequent decision-making regarding treatment. Progress in the area of pain associated with MS will depend on the development of multiple-arm, randomized, clinical trials with adequate numbers of subjects with specific pain characteristics, in order to produce useful scientific evidence as to the optimal treatment strategies.
REF ER EN CES
Aicher SA, Silverman MB, Winkler CW, Bebo Jr BF. Hyperalgesia in an animal model of multiple sclerosis. Pain 2004;110:560-570. Al-Araji AH, Oger J. Reappraisal of Lhermittes sign in multiple sclerosis. Mult Scler 2005; 11(4):398-402. Beiske AG, Pedersen ED, Czujko B, Myhr KM. Pain and sensory complaints in multiple sclerosis. Eur J Neurol 2004;1:479-482. Bergamaschi R, Romani A, Versino M, Callieco R, Gaspari D, Citterio A, Cosi V. Usefullness of trigeminal somatosensory evoked potentials to detect subclinical trigeminal impairment in multiple sclerosis patients. Acta Neurol Scand 1994;89:412-414. Berk C, Constantoyannis C, Honey CR. The treatment of trigeminal neuralgia in patients with multiple sclerosis using percutaneous radiofrequency rhizotomy. Can J Neurol Sci 2003;30:220-223. Breuer B, Pappagallo M, Knotkova H, Guleyupoglu N, Wallenstein S, Portenoy RK. A randomized double-blind, placebo-controlled two period crossover pilot trial of lamotrigine in patients with
Solaro_capitolo_01.indd 9
12/12/12 14:50
10
1 Pain
central pain due to multiple sclerosis Clin Ther 2007;29:2022-2030. Brichetto G, Messmer Uccelli M, Mancardi GL, Solaro C. Symptomatic medication use in multiple sclerosis. Mult Scler 2003;9(5):458-460. Broggi G, Ferroli P, Franzini A, Nazzi V, Farina L, La Mantia L, Milanese C. Operative findings and outcomes of microvascular decompression for trig eminal neuralgia in 35 patients affected by multiple sclerosis. Neurosurgery 2004;55(4):830838; discussion 838-839. Broggi G, Ferroli P, Franzini A, Pluderi M, La Mantia L, Milanese C. Role of microvascular decompression in trigeminal neuralgia and multiple sclerosis. Lancet 1999;354:1878-1879. Broggi G, Franzini A. Radiofrequency trigeminal rhizotomy in treatment of symptomatic nonneoplastic facial pain. J Neurosurg 1982;57: 483-486. Cruccu G, Leandri M, Feliciani M, Manfredi M. Idiopathic and symptomatic trigeminal pain. J Neurol Neurosurg Psychiatry 1990;53(12): 1034-1042. Da Silva CJ, Da Rocha AJ, Mendes MF, Maja Jr ACM, Braga FT, Tilbery CP. Trigeminal involvement in multiple sclerosis: magnetic resonance imaging findings with clinical correlation in a series of patients. Mult Scler 2005;11:282-285. DMKG study group. Misoprostol in the treatment of trigeminal neuralgia associated with multiple sclerosis. J Neurol 2003;250(5):542-545. Ehde DM, Gibbons LE, Chwastiak L, Bombardier CH, Sullivan MD, Kraft GH. Chronic pain in a large community sample of persons with multiple sclerosis. Mult Scler 2003;(6):605-611. Elrasheed AA, Worthington HV, Ariyaratnam S, Duxbury AJ. Opinions of UK specialists about terminology, diagnosis, and treatment of atypical facial pain: a survey. Br J Oral Maxillofac Surg 2004;42:566-571. Espir ML, Millac P. Treatment of paroxysmal disorders in multiple sclerosis with carbamazepine (Tegretol). J Neurol Neurosurg Psychiatry 1970;33(4):528-531. Gass A, Kitchen N, MacManus DG, Moseley IF, Hennerici MG, Miller DH. Trigeminal neuralgia in patients with multiple sclerosis: lesion localization with magnetic resonance imaging. Neurology 1997;49(4):1142-1144. Hadjimichael O, Kerns RD, Rizzo MA, Cutter G, Vollmer T. Persistent pain and uncomfortable
sensations in persons with multiple sclerosis. Pain 2007;127(1-2):34-41. Houtchens MK, Richert JR, Sami A, Rose JW. Open label gabapentin treatment for pain in multiple sclerosis. Mult Scler 1997;3(4):250-253. Kalia LV, OConnor PW. Severity of chronic pain and its relationship to quality of life in multiple sclerosis. Mult Scler 2005;11(3):322-327. Kalman S, sterbergn A, Srensenn J, Boivie J, Bertler A. Morphine responsiveness in a group of well-defined multiple sclerosis patients: a study with i.v. morphine. Eur J Pain 2002;6:69-80. Khan OA. Gabapentin relieves trigeminal neuralgia in multiple sclerosis patients. Neurology 1998;51(2):611-614. Lazar ML, Kirkpatrick JB Trigeminal neuralgia and multiple sclerosis: demonstration of the plaque in an operative case. Neurosurgery 1979;5:711-717. Leandri M, Lunardi G, Inglese M, Messmer Uccelli M, Mancardi GL, Gottlieb A et al. Lamotrigine in trigeminal neuralgia secondary to multiple sclerosis. J Neurol 2000;247(7):556-558. Lunardi G, Leandri M, Albano C, Cultrera S, Fracassi M, Rubino V, Favale E. Clinical effectiveness of lamotrigine and plasma levels in essential and symptomatic trigeminal neuralgia. Neurology 1997;48:1714-1717. Meaney JFM, Watt JMG, Eldridge PR, Whitehouse GH, Wells JCD, Miles JB. Association between trigeminal neuralgia and multiple sclerosis: role of magnetic resonance imaging. J Neurol Neurosurg Psychiatry 1995;59:253-259. Merskey H, Bogduk N. Part III: Pain terms, a current list with definitions and notes on usage. In Merskey H, Bogduk N (eds). Classification of chronic pain, IASP Task Force on Taxonomy, Seattle, WA, IASP Press, 2nd ed., pp. 209-214. Mills RJ, Young CA, Smith ET. Central trigeminal involvement in multiple sclerosis using highresolution MRI at 3T. BJR 2010;83:493-498. Minagar A, Sheremata WA. Glossopharyngeal neuralgia and MS. Neurology 2000;54:13681370. Nakashima I, Fujihara K, Kimpara T, Okita N, Takase S, Itoyama Y. Linear pontine trigeminal root lesions in multiple sclerosis: clinical and magnetic resonance imaging studies in 5 cases. Arch Neurol 2001;58:101-104. OConnor AB, Schwid SR, Herrmann DN, Markman JD, Dworkin RH. Pain associated with multiple sclerosis: systematic review and proposed classification. Pain 2008;137:96-111.
Solaro_capitolo_01.indd 10
12/12/12 14:50
1 Pain
11
Olechowski CJ, Truong JJ, Kerr BJ. Neuropathic pain behaviours in a chronic-relapsing model of experimental autoimmune encephalomyelitis (EAE). Pain 2009;141(1-2):156-164 Paty DW, Ebers GC. Clinical features. In Paty DW, Ebers GC (eds). Multiple sclerosis. Philadelphia, FA Davis Company, 1998, pp. 135-191. Piwko C, Desjardins O, Bereza B et al. Pain due to multiple sclerosis: Analysis of the prevalence and economic burden in Canada. Pain Res Manage 2007;12(4):259-265. Putzki N, Pfriem A, Limmroth V, Yaldizli O, Tettenborn B, Diener HC, Katsarava Z. Prevalence of migraine, tension-type headache and trigeminal neuralgia in multiple sclerosis. Eur J Neurol 2009;16(2):262-267. Ramsaransing G, Zwanikken C, De Keyser J. Worsening of symptoms of multiple sclerosis associated with carbamazepine. BMJ 2000;320:1113. Reder AT, Arnason BGW. Trigeminal neuralgia in multiple sclerosis relieved by a prostaglandin E analogue. Neurology 1995;45:1097-1100. Rog DJ, Nurmikko TJ, Young CA. Oromucosal delta9-tetrahydrocannabinol/cannabidiol for neuropathic pain associated with multiple sclerosis: an uncontrolled, open-label, 2-year extension trial. Clin Ther 2007;29(9):20682079. Rogers CL, Shetter AG, Ponce FA, Fiedler JA, Smith KA, Speiser BL. Gamma knife radiosurgery for trigeminal neuralgia associated with multiple sclerosis. J Neurosurg 2002;97(Suppl. 5):529-532. Rossi S, Mataluni G, Codec C, Fiore S, Buttari F, Musella A, Castelli M, Bernardi G, Centonze D. Effects of levetiracetam on chronic pain in multiple sclerosis: results of a randomized placebo-controlled study. Eur J Neurol 2009;16:360-366. Solari A. Role of health-related quality of life measures in the routine care of people with multiple sclerosis. Health Qual Life Outcomes 2005;18(3):16. Solaro C, Boemker M, Tanganelli P. Pregabalin for treating paroxysmal symptoms in multiple sclerosis: a pilot study. J Neurol 2009;256(10):1773-1774. Solaro C, Brichetto G, Amato MP, et al. The prevalence of pain in multiple sclerosis. A multicenter cross-sectional study. Neurology 2004;63:919-921.
Solaro C, Brichetto G, Battaglia MA, Messmer Uccelli M, Mancardi GL. Antiepileptic medications in multiple sclerosis: adverse effects in a three-year follow-up study. Neurol Sci 2005;25:307-310. Solaro C, Lunardi GL, Capello E, Inglese M, Messmer UM, Uccelli A et al. An open-label trial of gabapentin treatment of paroxysmal symptoms in multiple sclerosis patients. Neurology 1998;51(2):609-611. Solaro C, Messmer UM, Uccelli A, Leandri M, Mancardi GL. Low-dose gabapentin combined with either lamotrigine or carbamazepine can be useful therapies for trigeminal neuralgia in multiple sclerosis. Eur Neurol 2000;44(1):45-48. Solaro C, Tanganelli P. Acute delirium in patients with multiple sclerosis treated with pregabalin. Clin Neuropharmacol 2009;32(4):236-237. Solaro C, Tanganelli P. Tiagabine for treating painful tonic spasms in multiple sclerosis: a pilot study. J Neurol Neurosurg Psychiatry 2004;75:341. Solaro C, Uccelli MM, Brichetto G, Gasperini C, Mancardi GL. Topiramate relieves idiopathic and symptomatic trigeminal neuralgia. J Pain Symptom Manage 2001;21(5):367-376. Svendsen KB, Jensen TS, Bach FW. Does the cannabinoid dronabinol reduce central pain in multiple sclerosis? Randomised doubleblind placebo-controlled crossover trial. BMJ 2004;329:253. Svendsen KB, Jensen TS, Overvad K et al. Pain in patients with multiple sclerosis: a populationbased study. Arch Neurol 2003;60:1089-1094. Svendsen KB, Srensen L, Jensen TS, Hansen HJ, Bach FW. MRI of the central nervous system in MS patients with and without pain. Eur J Pain 2011;15:395-340. ThibaultK,Calvino B,Pezet S. Characterisation of sensory abnormalities observed in an animal model of multiple sclerosis: a behavioural and pharmacological study. Eur J Pain 2011;15(3):231. Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW, Hansson P, Hughes R, Nurmikko T, Serra J. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology 2008;70:16301635. Wade DT, Makela P, Robson P, House H, Bateman C. Do cannabis-based medicinal extracts have general or specific effects on symptoms in
Solaro_capitolo_01.indd 11
12/12/12 14:50
12
1 Pain
multiple sclerosis? A double-blind, randomized, placebo-controlled study on 160 patients. Mult Scler 2004;10:434-441. Waxman SG. Acquired channelopathies in nerve injury and MS. Neurology 2001;26;56(12): 1621-1627. Zajicek J, Fox P, Sanders H, Wright D, Vickery J, Nunn A, Thompson A. Cannabinoids for
treatment of spasticity and other symptoms related to multiple sclerosis (CAMS study): multicentre randomised placebo-controlled trial. Lancet 2003;362:1517-1526. Zvartau-Hind M, Din MU, Gilani A, Lisak RP, Khan OA. Topiramate relieves refractory trigeminal neuralgia in MS patients. Neurology 2000;55(10):1587-1588.
Solaro_capitolo_01.indd 12
12/12/12 14:50
Você também pode gostar
- Managing Neuropathic PainDocumento10 páginasManaging Neuropathic PainAgusBhakti100% (1)
- Dealing With Phantom Limb Pain After AmputationDocumento3 páginasDealing With Phantom Limb Pain After AmputationConnie SianiparAinda não há avaliações
- 234 Neuropathic PainDocumento10 páginas234 Neuropathic PainDr. Anish GolchhaAinda não há avaliações
- tmp41EE TMPDocumento35 páginastmp41EE TMPFrontiersAinda não há avaliações
- ICC Pollard 2013 1Documento8 páginasICC Pollard 2013 1Nuriah JnAinda não há avaliações
- Neuropathies: Essential Oils Show Promising Results in The Fight Against SymptomsDocumento17 páginasNeuropathies: Essential Oils Show Promising Results in The Fight Against Symptomskcc2012Ainda não há avaliações
- Mert 2017Documento8 páginasMert 2017G PalaAinda não há avaliações
- Pharmacotherapy 2007 27 (11) 1571-1587Documento17 páginasPharmacotherapy 2007 27 (11) 1571-1587Paulo MaurícioAinda não há avaliações
- Pharmacological Pain Management: For Better or For Worse?: Gisèle Pickering and David LussierDocumento48 páginasPharmacological Pain Management: For Better or For Worse?: Gisèle Pickering and David LussierYEILING LORENA GUERRERO GRANADOSAinda não há avaliações
- Alleviating Cancer PainDocumento9 páginasAlleviating Cancer PainSuresh KumarAinda não há avaliações
- Ketoprofen and Its Role in The Management of OsteoarthritisDocumento12 páginasKetoprofen and Its Role in The Management of OsteoarthritisLiam O'HalloranAinda não há avaliações
- Orofacial Musculoskeletal Pain. An Evidence-Based Bio-Psycho-Social Matrix ModelDocumento27 páginasOrofacial Musculoskeletal Pain. An Evidence-Based Bio-Psycho-Social Matrix ModelAMBAR JOSEFA ALEJANDRA MORAGA VALENZUELAAinda não há avaliações
- Painful NeuropathiesDocumento6 páginasPainful NeuropathiesAgusBhaktiAinda não há avaliações
- Understanding Peripheral Neuropathic Pain in Primary Care: Diagnosis and ManagementDocumento7 páginasUnderstanding Peripheral Neuropathic Pain in Primary Care: Diagnosis and ManagementInês Beatriz Clemente CasinhasAinda não há avaliações
- Frontiers in Bioscience 14, 5291-5338, June 1, 2009Documento48 páginasFrontiers in Bioscience 14, 5291-5338, June 1, 2009graciasAinda não há avaliações
- Managing Post-Operative PainDocumento8 páginasManaging Post-Operative PainAminn Alhassan ContehAinda não há avaliações
- Treatment of Fibromyalgia, Myofascial Pain, and Related DisordersDocumento20 páginasTreatment of Fibromyalgia, Myofascial Pain, and Related DisordersEva PopoviciAinda não há avaliações
- Management of Mixed PainDocumento19 páginasManagement of Mixed PainGita FitrianiAinda não há avaliações
- Halpern 2016Documento25 páginasHalpern 2016SAYDE ILEANA NAJERA DOMINGUEZAinda não há avaliações
- Muscle Pain, Mechanisms and Clinical SignificanceDocumento7 páginasMuscle Pain, Mechanisms and Clinical SignificanceTote Cifuentes AmigoAinda não há avaliações
- Pain Classifitation 2 PDFDocumento11 páginasPain Classifitation 2 PDFAnnisa BrilianAinda não há avaliações
- A Randomized Controlled Study of Segment PDFDocumento7 páginasA Randomized Controlled Study of Segment PDFFauzan IndraAinda não há avaliações
- The Effectiveness of Transcutaneous Electric Nerve Stimulation (TENS) in The Management of Painful Diabetic Peripheral Neuropathy (DPN) - A CritiquingDocumento6 páginasThe Effectiveness of Transcutaneous Electric Nerve Stimulation (TENS) in The Management of Painful Diabetic Peripheral Neuropathy (DPN) - A CritiquingIOSRjournalAinda não há avaliações
- Veterinary Pain ManagementDocumento8 páginasVeterinary Pain ManagementMenaAinda não há avaliações
- Neuropathic Pain: Vanja Basic-Kes/ Iris Zavoreo/ Marijana Bosnar Mira Ivankovic", Milan Bitunjac'Documento7 páginasNeuropathic Pain: Vanja Basic-Kes/ Iris Zavoreo/ Marijana Bosnar Mira Ivankovic", Milan Bitunjac'Meidy ShadanaAinda não há avaliações
- Pathophysiologyofpain 0899 p349-357Documento12 páginasPathophysiologyofpain 0899 p349-357Barbara Sakura RiawanAinda não há avaliações
- Human Brain Mechanisms of Pain PerceptionDocumento22 páginasHuman Brain Mechanisms of Pain Perceptionnynaeve_almeeraAinda não há avaliações
- Demystifying Poststroke Pain: From Etiology To TreatmentDocumento13 páginasDemystifying Poststroke Pain: From Etiology To TreatmentNelLyAinda não há avaliações
- Central Sensitization in Patients With Rheumatoid Arthritis: A Systematic Literature ReviewDocumento12 páginasCentral Sensitization in Patients With Rheumatoid Arthritis: A Systematic Literature ReviewJuliana FeronAinda não há avaliações
- An Option Overview: Neuropathic PainDocumento3 páginasAn Option Overview: Neuropathic PainAndi Tri SutrisnoAinda não há avaliações
- Vulnerabilidade A Dor 2014Documento9 páginasVulnerabilidade A Dor 2014Ellen AmaralAinda não há avaliações
- The Relationship Between Adverse Life Events and EDocumento14 páginasThe Relationship Between Adverse Life Events and ESandra PahlmAinda não há avaliações
- EFNS Guideline 2004 Neuropathic Pain AssessmentDocumento10 páginasEFNS Guideline 2004 Neuropathic Pain AssessmentDeni Andre AtmadinataAinda não há avaliações
- PMT 11 88Documento3 páginasPMT 11 88Sri RamadhaniAinda não há avaliações
- Anxiety July 2011Documento8 páginasAnxiety July 2011aswadiibrahimAinda não há avaliações
- AliliDocumento3 páginasAliliSaf Tanggo DiampuanAinda não há avaliações
- Pain Threshold Is Reduced in DepressionDocumento4 páginasPain Threshold Is Reduced in DepressionAmer WasimAinda não há avaliações
- Pain Neuroscience EducationDocumento26 páginasPain Neuroscience EducationGustavo Cabanas100% (1)
- Journal On Pain - RHUBY ABENOJADocumento3 páginasJournal On Pain - RHUBY ABENOJARHUBY ABENOJAAinda não há avaliações
- 1fd9 PDFDocumento26 páginas1fd9 PDFpedroAinda não há avaliações
- Practical Application of Hypnosis in Treatment of Phantom Limb PainDocumento11 páginasPractical Application of Hypnosis in Treatment of Phantom Limb PainCarlos CondeAinda não há avaliações
- What Is Depression in Epilepsy?: Christian E. Elger and Christian HoppeDocumento3 páginasWhat Is Depression in Epilepsy?: Christian E. Elger and Christian HoppedeadcorpsesAinda não há avaliações
- Neuropathic Pain Feb 2012Documento8 páginasNeuropathic Pain Feb 2012Santiago HerreraAinda não há avaliações
- Tracey (2007) - The Cerebral Signature For Pain Perception and Its ModulationDocumento15 páginasTracey (2007) - The Cerebral Signature For Pain Perception and Its ModulationLuciana AraújoAinda não há avaliações
- Sindrome MiofacialDocumento13 páginasSindrome MiofacialAngie Paola RodriguezAinda não há avaliações
- Evaluating MyopathyDocumento17 páginasEvaluating MyopathyAbulSayeedDoulahAinda não há avaliações
- 2013 - Malfait - A Commentary On Modelling of Osteoarthritis Pain in Small AnimalsDocumento11 páginas2013 - Malfait - A Commentary On Modelling of Osteoarthritis Pain in Small AnimalsSanjeev SaxenaAinda não há avaliações
- Efficacy of Pain Treatment On Mood Syndrome in Patients With Dementia: A Randomized Clinical TrialDocumento7 páginasEfficacy of Pain Treatment On Mood Syndrome in Patients With Dementia: A Randomized Clinical TrialLofita Surya DewiAinda não há avaliações
- In The Spine or in The Brain? Recent Advances in Pain Neuroscience Applied in The Intervention For Low Back PainDocumento8 páginasIn The Spine or in The Brain? Recent Advances in Pain Neuroscience Applied in The Intervention For Low Back PainVizaAinda não há avaliações
- Patogenesis Neuropatik DiabetikDocumento8 páginasPatogenesis Neuropatik DiabetikStephanie AureliaAinda não há avaliações
- The Role of Antidepressants in The Management of Fibromyalgia SyndromeDocumento11 páginasThe Role of Antidepressants in The Management of Fibromyalgia SyndromefilipemateusoliveiraAinda não há avaliações
- Central Poststroke PainDocumento7 páginasCentral Poststroke PainPrimas Shahibba RidhwanaAinda não há avaliações
- Nri2022 8336561Documento14 páginasNri2022 8336561Carolina SidabutarAinda não há avaliações
- Descending Pain Modulation and Chronification of Pain: ReviewDocumento9 páginasDescending Pain Modulation and Chronification of Pain: ReviewJose PerezAinda não há avaliações
- PainDocumento4 páginasPainKabirAinda não há avaliações
- Myofascial PainDocumento8 páginasMyofascial PainEnyaw Droffats100% (1)
- Euroscience: Molecular, Cellular and Circuit Basis of Cholinergic Modulation of PainDocumento14 páginasEuroscience: Molecular, Cellular and Circuit Basis of Cholinergic Modulation of PainPriyabrata HalderAinda não há avaliações
- Fibromyalgia SyndromeNo EverandFibromyalgia SyndromeJacob N. AblinAinda não há avaliações
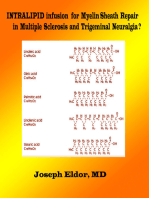
- Intralipid infusion for Myelin Sheath Repair in Multiple Sclerosis and Trigeminal Neuralgia?No EverandIntralipid infusion for Myelin Sheath Repair in Multiple Sclerosis and Trigeminal Neuralgia?Ainda não há avaliações
- Manual Book Isuzu Panther PDFDocumento23 páginasManual Book Isuzu Panther PDFZidna IlmaAinda não há avaliações
- Analysis of Factors That Influence OTC Purchasing BehaviorDocumento6 páginasAnalysis of Factors That Influence OTC Purchasing BehaviorkookyinAinda não há avaliações
- List ObatDocumento3 páginasList ObatAhmad AmsoryAinda não há avaliações
- Pengaruh Kombinasi Hidroksipropil Metilselulosa-Xanthan Gum Sebagai Matriks Pada Profil Pelepasan Tablet Teofilin Lepas TerkendaliDocumento13 páginasPengaruh Kombinasi Hidroksipropil Metilselulosa-Xanthan Gum Sebagai Matriks Pada Profil Pelepasan Tablet Teofilin Lepas TerkendaliHasan MunadiAinda não há avaliações
- Academic Sciences: An Improved Method For The Synthesis of MetoclopramideDocumento4 páginasAcademic Sciences: An Improved Method For The Synthesis of MetoclopramideYeni IngrianiAinda não há avaliações
- Drug Discovery Today Reviews - Hot-melt extrusion in the pharmaceutical industry: toward filing a new drug applicationDocumento20 páginasDrug Discovery Today Reviews - Hot-melt extrusion in the pharmaceutical industry: toward filing a new drug applicationKamran AlamAinda não há avaliações
- Vitamin KDocumento1 páginaVitamin Kambet100% (2)
- Antonio Nanci - Ten Cate's Oral Histology - Development, Structure, and Function (2017, Elsevier) - Part3 PDFDocumento3 páginasAntonio Nanci - Ten Cate's Oral Histology - Development, Structure, and Function (2017, Elsevier) - Part3 PDFRadwa Mohamed100% (1)
- PAIN and Pain Management PDFDocumento56 páginasPAIN and Pain Management PDFcj bariasAinda não há avaliações
- Manjistha remedy for striae gravidarumDocumento6 páginasManjistha remedy for striae gravidarumDrMansi Yeragi SabnisAinda não há avaliações
- BPI Banking Parental CellsDocumento4 páginasBPI Banking Parental CellsAjay KumarAinda não há avaliações
- Appendix G Medication Audit ToolDocumento12 páginasAppendix G Medication Audit ToolAdina OlteanuAinda não há avaliações
- Emergency Cart and Code Blue ResponseDocumento10 páginasEmergency Cart and Code Blue ResponseKath100% (1)
- Bmab 023Documento7 páginasBmab 023Hasna NoerAinda não há avaliações
- Urticaria Diagnosis and Treatment 2014Documento74 páginasUrticaria Diagnosis and Treatment 2014sandraldiraAinda não há avaliações
- Export of Indian Pharmaceuticals To NamibiaDocumento58 páginasExport of Indian Pharmaceuticals To NamibiahabeebsheriffAinda não há avaliações
- EagleBurgmann Burachem Brown 9655 R enDocumento1 páginaEagleBurgmann Burachem Brown 9655 R enkeyur1109Ainda não há avaliações
- Pediatric DosaPediatric Dosages Based On Body Weightges Based On Body WeightDocumento7 páginasPediatric DosaPediatric Dosages Based On Body Weightges Based On Body WeightdjbhetaAinda não há avaliações
- Scale Up Factors With An Industrial PerspectiveDocumento14 páginasScale Up Factors With An Industrial PerspectiverajuAinda não há avaliações
- Vit C Brand Names Phils.Documento10 páginasVit C Brand Names Phils.Jason MontesaAinda não há avaliações
- Drug ExpiryDocumento3 páginasDrug Expiryhap hazardAinda não há avaliações
- New Drug Application (NDA)Documento13 páginasNew Drug Application (NDA)Dipak ShindeAinda não há avaliações
- Making LSDDocumento59 páginasMaking LSDma7ka50% (2)
- Manufacture Tablets and Capsules Pharmaceutical Formulations UnitDocumento10 páginasManufacture Tablets and Capsules Pharmaceutical Formulations UnitVpn SinghAinda não há avaliações
- Food and Drug Interactions NotesDocumento8 páginasFood and Drug Interactions NotesSUDHEER SAinda não há avaliações
- Eliminating Error-Prone Abbreviations, Symbols, and Dose DesignationsDocumento23 páginasEliminating Error-Prone Abbreviations, Symbols, and Dose DesignationsRubenVelazquezAinda não há avaliações
- Alpha Gan P DropsDocumento6 páginasAlpha Gan P DropsbangunngawiAinda não há avaliações
- IVFDocumento20 páginasIVFAntonette RendalAinda não há avaliações
- Mpeg 350Documento2 páginasMpeg 350sudhir5441Ainda não há avaliações
- Pharma Industry AnalysisDocumento8 páginasPharma Industry AnalysisVenkataramanan VaidyanathanAinda não há avaliações