Escolar Documentos
Profissional Documentos
Cultura Documentos
Osteoarthritis - Wikipedia, The Free Encyclopedia PDF
Enviado por
Xaythinanh Philama'Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Osteoarthritis - Wikipedia, The Free Encyclopedia PDF
Enviado por
Xaythinanh Philama'Direitos autorais:
Formatos disponíveis
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
Osteoarthritis
From Wikipedia, the free encyclopedia
Osteoarthritis (OA) also known as degenerative arthritis or degenerative joint disease or osteoarthrosis, is a group of mechanical abnormalities involving degradation of joints,[1] including articular cartilage and subchondral bone. Symptoms may include joint pain, tenderness, stiffness, locking, and sometimes an effusion. A variety of causes hereditary, developmental, metabolic, and mechanical deficitsmay initiate processes leading to loss of cartilage. When bone surfaces become less well protected by cartilage, bone may be exposed and damaged. As a result of decreased movement secondary to pain, regional muscles may atrophy, and ligaments may become more lax.[2] Treatment generally involves a combination of exercise, lifestyle modification, and analgesics. If pain becomes debilitating, joint replacement surgery may be used to improve the quality of life. OA is the most common form of arthritis,[2] and the leading cause of chronic disability in the United States.[3] It affects about 8 million people in the United Kingdom and nearly 27 million people in the United States.[4]
Osteoarthritis
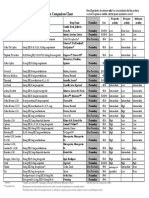
Classification and external resources
ICD-10
M15 (http://apps.who.int /classifications/icd10/browse /2010/en#/M15)-M19 (http://apps.who.int/classifications /icd10/browse/2010/en#/M19), M47 (http://apps.who.int/classifications /icd10/browse/2010/en#/M47)
ICD-9 OMIM
715 (http://www.icd9data.com /getICD9Code.ashx?icd9=715) 165720 (http://omim.org/entry /165720)
DiseasesDB 9313 (http://www.diseasesdatabase.com /ddb9313.htm) MedlinePlus 000423 (http://www.nlm.nih.gov /medlineplus/ency/article /000423.htm) eMedicine med/1682 (http://www.emedicine.com /med/topic1682.htm) orthoped/427 (http://www.emedicine.com/orthoped /topic427.htm#) pmr/93 (http://www.emedicine.com /pmr/topic93.htm#) radio/492 (http://www.emedicine.com/radio /topic492.htm#)
1 of 13
8/3/2013 1:08 PM
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
Contents
1 Signs and symptoms 2 Causes 2.1 Primary 2.2 Secondary 3 Pathophysiology 4 Diagnosis 4.1 Classification 5 Management 5.1 Lifestyle modification 5.2 Physical measures 5.3 Medication 5.4 Surgery 5.5 Alternative medicine 6 Epidemiology 7 Etymology 8 History 9 Research 10 References 11 External links
MeSH
D010003 (http://www.nlm.nih.gov /cgi/mesh/2013/MB_cgi?field=uid& term=D010003)
Signs and symptoms
The main symptom is pain, causing loss of ability and often stiffness. "Pain" is generally described as a sharp ache or a burning sensation in the associated muscles and tendons. OA can cause a crackling noise (called "crepitus") when the affected joint is moved or touched and people may experience muscle spasms and contractions in the tendons. Occasionally, the joints may also be filled with fluid.[5] Some people report increased pain associated with cold temperature, high humidity, and/or a drop in barometric pressure, but studies have had mixed results.[6] OA commonly affects the hands, feet, spine, and the large weight nodes may form in osteoarthritis bearing joints, such as the hips and knees, although in theory, any joint in the body can be affected. As OA progresses, the affected joints appear larger, are stiff and painful, and usually feel better with gentle use but worse with excessive or prolonged use, thus distinguishing it from rheumatoid arthritis. In smaller joints, such as at the fingers, hard bony enlargements, called Heberden's nodes (on the distal interphalangeal joints) and/or Bouchard's nodes (on the proximal interphalangeal joints), may form, and though they are not necessarily painful, they do limit the movement of the fingers significantly. OA at the toes leads to the formation of bunions, rendering them red or swollen. Some people notice these physical changes before they experience any pain.
Bouchard's nodes and Heberden's
2 of 13
8/3/2013 1:08 PM
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
OA is the most common cause of a joint effusion of the knee.[7]
Causes
Damage from mechanical stress with insufficient self repair by joints is believed to be the primary cause of osteoarthritis.[8] Sources of this stress may include: misalignments of bones caused by congenital or pathogenic causes; mechanical injury; excess body weight; loss of strength in the muscles supporting a joint; and impairment of peripheral nerves, leading to sudden or uncoordinated movements.[8] However exercise, including running in the absence of injury, has not been found to increase the risk.[9] Nor has cracking one's knuckles been found to play a role.[10]
Primary
A number of studies have shown that there is a greater prevalence of the disease among siblings and especially identical twins, indicating a hereditary basis.[11] Although a single factor is not generally sufficient to cause the disease, about half of the variation in susceptibility has been assigned to genetic factors.[12] The development of OA is correlated with a history of previous joint injury and with obesity, especially with respect to knees.[13] Since the correlation with obesity has been observed not only for knees but also for non-weight bearing joints and the loss of body fat is more closely related to symptom relief than the loss of body weight, it has been suggested that there may be a metabolic link to body fat as opposed to just mechanical loading.[14] Changes in sex hormone levels may play a role in the development of OA as it is more prevalent among post-menopausal women than among men of the same age.[15][16] A study of mice found natural female hormones to be protective while injections of the male hormone dihydrotestosterone reduced protection.[17]
Primary osteoarthritis of the left knee. Note the osteophytes, narrowing of the joint space (arrow), and increased subchondral bone density (arrow).
Secondary
This type of OA is caused by other factors but the resulting pathology is the same as for primary OA: Alkaptonuria Congenital disorders of joints Diabetes Ehlers-Danlos Syndrome Hemochromatosis and Wilson's disease Inflammatory diseases (such as Perthes' disease), (Lyme disease), and all chronic forms of arthritis (e.g. costochondritis, gout, and rheumatoid arthritis). In gout, uric acid crystals cause the cartilage to degenerate at a faster pace. Injury to joints or ligaments (such as the ACL), as a result of an accident or orthopedic operations. Ligamentous deterioration or instability may be a factor.
3 of 13 8/3/2013 1:08 PM
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
Marfan syndrome Obesity Septic arthritis (infection of a joint)
Pathophysiology
Primary OA is a chronic degenerative disorder related to but not caused by aging, as there are people well into their nineties who have no clinical or functional signs of the disease. As a person ages, the water content of the cartilage decreases[18] as a result of a reduced proteoglycan content, thus causing the cartilage to be less resilient. The water content of healthy cartilage is finely balanced by compressive force driving water out & swelling pressure drawing water in.[19] Collagen fibres exert the compressive force, whereas the Gibbs-Donnan effect & cartilage proteoglycans create osmotic pressure which tends to draw water in.[19] However during onset of OA there is an increase in cartilage water content.[20][21][22][23][24] This increase occurs because whilst there is an overall loss of proteoglycans,[21][25] it is outweighed by a loss of collagen.[19][25] Without the protective effects of the proteoglycans, the collagen fibers of the cartilage can become susceptible to degradation and thus exacerbate the degeneration. Inflammation of the surrounding joint capsule can also occur, though often mild (compared to what occurs in rheumatoid arthritis). This can happen as breakdown products from the cartilage are released into the synovial space, and the cells lining the joint attempt to remove them. New bone outgrowths, called "spurs" or osteophytes, can form on the margins of the joints, possibly in an attempt to improve the congruence of the articular cartilage surfaces. These bone changes, together with the inflammation, can be both painful and debilitating.
Diagnosis
Diagnosis is made with reasonable certainty based on history and clinical examination.[26][27] X-rays may confirm the diagnosis. The typical changes seen on X-ray include: joint space narrowing, subchondral sclerosis (increased bone formation around the joint), subchondral cyst formation, and osteophytes.[28] Plain films may not correlate with the findings on physical examination or with the degree of pain.[29] Usually other imaging techniques are not necessary to clinically diagnose OA. In 1990, the American College of Rheumatology, using data from a multi-center study, developed a set of criteria for the diagnosis of hand OA based on hard tissue enlargement and swelling of certain joints.[30] These criteria were found to be 92% sensitive and 98% specific for hand OA versus other entities such as rheumatoid arthritis and spondyloarthropathies.[31] Related pathologies whose names may be confused with OA include pseudo-arthrosis. This is derived from the Greek words pseudo, meaning "false", and arthrosis, meaning "joint." Radiographic diagnosis results in diagnosis of a fracture within a joint, which is not to be confused with OA which is a degenerative pathology affecting a high incidence of distal phalangeal joints of female patients. A polished ivory-like appearance may also develop on the bones of the affected joints, reflecting a change called eburnation.[32]
4 of 13
8/3/2013 1:08 PM
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
Damaged cartilage from sows. (a) cartilage erosion (b)cartilage ulceration (c)cartilage repair (d)osteophyte (bone spur) formation.
Histopathology of osteoarthrosis of a knee joint in an elderly female.
Histopathology of osteoarthrosis of a knee joint in an elderly female.
Severe osteoarthritis and osteopenia of the carpal joint and 1st carpometacarpel joint.
Classification
OA can be classified into either primary or secondary depending on whether or not there is an identifiable underlying cause. Both primary generalized nodal OA and erosive OA (EOA. also called inflammatory OA) are sub-sets of primary OA. EOA is a much less common, and more aggressive inflammatory form of OA which often affects the distal interphalangeal joints and has characteristic changes on x-ray.
Management
Lifestyle modification (such as weight loss and exercise) and analgesics are the mainstay of treatment. Acetaminophen / paracetamol is used first line and NSAIDs are only recommended as add on therapy if pain relief is not sufficient.[33] This is due to the relative greater safety of acetaminophen.[33]
Lifestyle modification
For overweight people, weight loss may be an important factor. Patient education has been shown to be helpful in the self-management of arthritis. It decreases pain, improves function, reduces stiffness and fatigue, and reduces medical usage.[34] A meta-analysis has shown patient education can provide on average 20% more pain relief when compared to NSAIDs alone in patients with hip OA.[34]
Physical measures
Moderate exercise is beneficial with respect to pain and function in those with osteoathritis of the knee and possibly hip.[35] While some evidence supports certain physical therapies evidence for a combined program is limited.[36] There is not enough evidence to determine the effectiveness of massage therapy.[37] The use of orthoses (commonly referred to as splints, braces or insoles as applicable) can reduce the symptoms of OA. In the lower limb, orthoses are used for the foot and ankle[38] and knee.[39] Knee braces may be useful.[40] In the upper limb, splinting of the base of the thumb leads to improvements after one year.[41]
5 of 13 8/3/2013 1:08 PM
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
The evidence for manual therapy is inconclusive.[42] Functional, gait, and balance training has been recommended to address impairments of position sense, balance, and strength in individuals with lower extremity arthritis as these can contribute to higher falls in older individuals.[43]
Medication
The analgesic paracetamol (INN; acetaminophen is the USA) is the first line treatment for OA.[33][44] For mild to moderate symptoms effectiveness is similar to non-steroidal anti-inflammatory drugs (NSAIDs), though for more severe symptoms NSAIDs may be more effective.[33] NSAIDs such as ibuprofen while more effective in severe cases are associated with greater side effects such as gastrointestinal bleeding.[33] Another class of NSAIDs, COX-2 selective inhibitors (such as celecoxib) are equally effective to NSAIDs with lower rates of adverse gastrointestinal effects but higher rates of cardiovascular disease such as myocardial infarction.[45] They are also much more expensive. Oral steroids are not recommended in the treatment of OA because of their modest benefit and high rate of adverse effects.[citation needed] There are several NSAIDs available for topical use including diclofenac. They have fewer systemic side-effects and at least some therapeutic effect.[46] A Cochrane review concluded that opioid analgesics such as morphine and fentanyl reduce pain, but this benefit is outweighed by frequent adverse events and thus they should not routinely be used.[47] Topical capsaicin is controversial with a 2011 review[48] finding effectiveness and a 2009 review not.[46] Injection of glucocorticoids (such as hydrocortisone) leads to short term pain relief that may last between a few weeks and a few months.[49] Joint injections of hyaluronic acid have not been found to lead to significant improvement.[46][50] Hyaluronic acid injects have been associated with significant harm.[50]
Surgery
If disability is significant and more conservative management is ineffective, joint replacement surgery or resurfacing may be recommended. Evidence supports joint replacement for both knees and hips.[51] For the knee it improves both pain and functioning.[52] Arthroscopic surgical intervention for OA of the knee however has been found to be no better than placebo at relieving symptoms.[53]
Alternative medicine
Dietary supplements Many dietary supplements are sold as treatments for OA and some of them have been found to be effective. Phytodolor,[48] SAMe,[54] and SKI 306X (a Chinese herbal mixture)[55] may be effective in improving pain, and there is some evidence to support the use of cat's claw as an anti-inflammatory.[56] There is tentative evidence to support avocado/soybean unsaponifiables,[57] Boswellia serrata extracts (frankincense),[58][59] MSM[48] and rose hip.[48] The effectiveness of glucosamine is controversial.[60][61] A 2010 meta-analysis found that it is no better than placebo.[62] Some older reviews conclude that glucosamine sulfate was an effective treatment[63][64] while some others have found it ineffective.[65] A difference may exist between glucosamine sulfate and glucosamine hydrochloride, with glucosamine sulfate showing a benefit and glucosamine hydrochloride not.[66] The
6 of 13 8/3/2013 1:08 PM
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
Osteoarthritis Research Society International recommends that glucosamine be discontinued if no effect is observed after six months[67] and the National Institute of Clinical Excellence no longer recommends its use.[68] If there is a benefit it is at best slight.[69] There is little evidence supporting benefits for some supplements, including: the Ayurvedic herbal preparations with brand names Articulin F and Eazmov, collagen, devils claw, Duhuo Jisheng Wan (a Chinese herbal preparation), fish liver oil, ginger, the herbal preparation Gitadyl, glucosamine, hyaluronic acid, omega-3 fatty acids, the brand-name product Reumalax, stinging nettle, turmeric, vitamins A, C, and E in combination, vitamin E alone, vitamin K and willow bark. There is insufficient evidence to make a recommendation about the safety and efficacy of these treatments.[48][56] Chondroitin is not recommended as a treatment for OA.[70] Manual therapies While acupuncture leads to a statistically significant improvement in pain relief, this improvement is small and may be of questionable clinical significance. Waiting list-controlled trials for peripheral joint osteoarthritis do show clinically relevant benefits, but these may be due to placebo effects.[71] Acupuncture does not seem to produce long-term benefits.[72] While electrostimulation techniques such as TENS have been used for twenty years to treat osteoarthritis in the knee, there is no conclusive evidence to show that it reduces pain or disability.[73]
Epidemiology
Globally approximately 250 million people have osteoarthritis of the knee (3.6% of the population).[75] OA affects nearly 27 million people in the United States, accounting for 25% of visits to primary care physicians, and half of all NSAID prescriptions. It is estimated that 80% of the population have radiographic evidence of OA by age 65, although only 60% of those will have symptoms.[76] In the United States, hospitalizations for OA increased from 322,000 in 1993 to 735,000 in 2006.[77] Globally OA causes moderate to severe disability in 43.4 million people as of 2004.[78]
Disability-adjusted life year for OA per 100,000 inhabitants in 2004.[74] no data 200 200220 220240 240260 260280 300320 320340 340360 360380 380400 400
Etymology
OA is derived from the Greek word part osteo-, meaning "of the bone", 280300 combined with arthritis: arthr-, meaning "joint", and -itis, the meaning of which has come to be associated with inflammation. The -itis of OA could be considered misleading as inflammation is not a conspicuous feature. Some clinicians refer to this condition as osteoarthosis to signify the lack of inflammatory response.
History
Evidence for OA found in the fossil record is studied by paleopathologists, specialists in ancient disease and injury. OA has been reported in fossils of the large carnivorous dinosaur Allosaurus fragilis.[79]
7 of 13
8/3/2013 1:08 PM
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
Research
There are ongoing efforts to determine if there are agents that modify outcomes in OA. Sprifermin is one candidate drug. There is also tentative evidence that strontium ranelate may decrease degeneration in OA and improve outcomes.[80][81]
References
1. ^ "osteoarthritis (http://web.archive.org /web/20090616022448/http://www.mercksource.com /pp/us/cns/cns_hl_dorlands_split.jsp?pg=/ppdocs /us/common/dorlands/dorland/six/000076356.htm)" at Dorland's Medical Dictionary 2. ^ a b Conaghan, Phillip. "Osteoarthritis National clinical guideline for care and management in adults" (http://www.nice.org.uk/nicemedia /pdf/CG059FullGuideline.pdf) (PDF). Retrieved 2008-04-29. 3. ^ Centers for Disease Control and Prevention (CDC) (February 2001). "Prevalence of disabilities and associated health conditions among adultsUnited States, 1999". MMWR Morb Mortal Wkly Rep. 50 (7): 1205. PMID 11393491 (//www.ncbi.nlm.nih.gov /pubmed/11393491). 4. ^ Van Manen, MD; Nace, J; Mont, MA (November 2012). "Management of primary knee osteoarthritis and indications for total knee arthroplasty for general practitioners." (http://www.ncbi.nlm.nih.gov/pubmed /23139341). The Journal of the American Osteopathic Association 112 (11): 709715. PMID 23139341 (//www.ncbi.nlm.nih.gov/pubmed/23139341). 5. ^ MedlinePlus Encyclopedia Osteoarthritis (http://www.nlm.nih.gov/medlineplus/ency/article /000423.htm) 6. ^ de Figueiredo EC, Figueiredo GC, Dantas RT (2011 Dec). "Influence of meteorological elements on osteoarthritis pain: a review of the literature". Rev Bras Reumatol. 51 (6): 6228. PMID 22124595 (//www.ncbi.nlm.nih.gov/pubmed/22124595). 7. ^ Water on the knee (http://www.mayoclinic.com /health/water-on-the-knee/DS00662), MayoClinic.com 8. ^ a b Brandt KD, Dieppe P, Radin E (January 2009). "Etiopathogenesis of osteoarthritis". Med. Clin. North Am. 93 (1): 124, xv. doi:10.1016/j.mcna.2008.08.009 (http://dx.doi.org /10.1016%2Fj.mcna.2008.08.009). PMID 19059018 (//www.ncbi.nlm.nih.gov/pubmed/19059018). 9. ^ Bosomworth NJ (September 2009). "Exercise and knee osteoarthritis: benefit or hazard?" (http://www.ncbi.nlm.nih.gov/pmc/articles /PMC2743580). Can Fam Physician 55 (9): 8718. PMC 2743580 (//www.ncbi.nlm.nih.gov/pmc/articles /PMC2743580). PMID 19752252 (//www.ncbi.nlm.nih.gov/pubmed/19752252). ^ Deweber, K; Olszewski, M, Ortolano, R (Mar-Apr 2011). "Knuckle cracking and hand osteoarthritis". Journal of the American Board of Family Medicine : JABFM 24 (2): 16974. doi:10.3122/jabfm.2011.02.100156 (http://dx.doi.org /10.3122%2Fjabfm.2011.02.100156). PMID 21383216 (//www.ncbi.nlm.nih.gov/pubmed /21383216). ^ Valdes AM, Spector TD (August 2008). "The contribution of genes to osteoarthritis". Rheum Dis Clin North Am. 34 (3): 581603. doi:10.1016/j.rdc.2008.04.008 (http://dx.doi.org /10.1016%2Fj.rdc.2008.04.008). PMID 18687274 (//www.ncbi.nlm.nih.gov/pubmed/18687274). ^ Spector TD, MacGregor AJ (2004). "Risk factors for osteoarthritis: genetics" (http://www.ncbi.nlm.nih.gov/pubmed/14698640). OsteoArthritis and Cartilage 12: S3944. doi:10.1016/j.joca.2003.09.005 (http://dx.doi.org /10.1016%2Fj.joca.2003.09.005). PMID 14698640 (//www.ncbi.nlm.nih.gov/pubmed/14698640). ^ Coggon D, Reading I (May 2001). "Knee osteoarthritis and obesity" (http://www.ncbi.nlm.nih.gov/pubmed/11360143). International Journal of Obesity Related Metabolic Disorders 25 (5): 622627. doi:10.1038/sj.ijo.0801585 (http://dx.doi.org /10.1038%2Fsj.ijo.0801585). PMID 11360143 (//www.ncbi.nlm.nih.gov/pubmed/11360143). ^ P Pottie, N Presle (2006). "Obesity and osteoarthritis: more complex than predicted!" (http://ard.bmj.com/content/65/11/1403.full). Annals of the Rheumatic Diseases 65 (11): 14031405. doi:10.1136/ard.2006.061994 (http://dx.doi.org /10.1136%2Fard.2006.061994). PMC 1798356 (//www.ncbi.nlm.nih.gov/pmc/articles/PMC1798356). PMID 17038451 (//www.ncbi.nlm.nih.gov/pubmed /17038451). ^ Linn, Sarah; Murtaugh, Bryan; Casey, Ellen (May 2012). "Role of Sex Hormones in the Development of Osteoarthritis". Physical Medicine and Rehabilitation 4 (5): 169173. doi:10.1016/j.pmrj.2012.01.013
8/3/2013 1:08 PM
10.
11.
12.
13.
14.
15.
8 of 13
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
(http://dx.doi.org/10.1016%2Fj.pmrj.2012.01.013). 16. ^ Tanamas, SK; Wijethilake, Pushpika; Wluka, Anita E.; Davies-Tuck, Miranda L.; Urquhart, Donna M.; Wang, Yuanyuan; Cicuttini, Flavia M. (June 2011). "Sex hormones and structural changes in osteoarthritis: a systematic review". Maturitas 69 (2): 141156. doi:10.1016/j.maturitas.2011.03.019 (http://dx.doi.org /10.1016%2Fj.maturitas.2011.03.019). PMID 21481553 (//www.ncbi.nlm.nih.gov/pubmed /21481553). 17. ^ Ma, H.L.; Blanchet, T.J.; Peluso, D.; Hopkins, B.; Morris, E.A.; Glasson, S.S. (June 2007). "Osteoarthritis severity is sex dependent in a surgical mouse model". OsteoArthritis and Cartilage 15 (6): 695700. doi:10.1016/j.joca.2006.11.005 (http://dx.doi.org/10.1016%2Fj.joca.2006.11.005). PMID 17207643 (//www.ncbi.nlm.nih.gov/pubmed /17207643). 18. ^ Simon, H; Zieve D (2005-05-08). "Osteoarthritis" (http://www.umm.edu/patiented/articles /what_osteoarthritis_000035_1.htm). University of Maryland Medical Center. Retrieved 2009-04-25. 19. ^ a b c Maroudas, A. (1976). "Balance between swelling pressure and collagen tension in normal and degenerate cartilage". Nature 260 (5554): 808809. doi:10.1038/260808a0 (http://dx.doi.org /10.1038%2F260808a0). PMID 1264261 (//www.ncbi.nlm.nih.gov/pubmed/1264261). 20. ^ Bollet, A. J.; Nance, J. L. (1966). "Biochemical Findings in Normal and Osteoarthritic Articular Cartilage. II. Chondroitin Sulfate Concentration and Chain Length, Water, and Ash Content*" (http://www.ncbi.nlm.nih.gov/pmc/articles /PMC292789). Journal of Clinical Investigation 45 (7): 11701177. doi:10.1172/JCI105423 (http://dx.doi.org/10.1172%2FJCI105423). PMC 292789 (//www.ncbi.nlm.nih.gov/pmc/articles /PMC292789). PMID 16695915 (//www.ncbi.nlm.nih.gov/pubmed/16695915). 21. ^ a b Brocklehurst, R.; Bayliss, M. T.; Maroudas, A.; Coysh, H. L.; Freeman, M. A.; Revell, P. A.; Ali, S. Y. (1984). "The composition of normal and osteoarthritic articular cartilage from human knee joints. With special reference to unicompartmental replacement and osteotomy of the knee". The Journal of bone and joint surgery. American volume 66 (1): 95106. PMID 6690447 (//www.ncbi.nlm.nih.gov /pubmed/6690447). 22. ^ Chou, M. -C.; Tsai, P. -H.; Huang, G. -S.; Lee, H. -S.; Lee, C. -H.; Lin, M. -H.; Lin, C. -Y.; Chung, H. -W. (2009). "Correlation between the MR T2 value at 4.7 T and relative water content in articular cartilage in experimental osteoarthritis induced by ACL transection". Osteoarthritis and Cartilage 17 (4):
9 of 13
23.
24.
25.
26.
27.
28.
29.
30.
441447. doi:10.1016/j.joca.2008.09.009 (http://dx.doi.org/10.1016%2Fj.joca.2008.09.009). PMID 18990590 (//www.ncbi.nlm.nih.gov/pubmed /18990590). ^ Grushko, G.; Schneiderman, R.; Maroudas, A. (1989). "Some biochemical and biophysical parameters for the study of the pathogenesis of osteoarthritis: A comparison between the processes of ageing and degeneration in human hip cartilage". Connective tissue research 19 (24): 149176. doi:10.3109/03008208909043895 (http://dx.doi.org /10.3109%2F03008208909043895). PMID 2805680 (//www.ncbi.nlm.nih.gov/pubmed/2805680). ^ Mankin, H. J.; Thrasher, A. Z. (1975). "Water content and binding in normal and osteoarthritic human cartilage". The Journal of bone and joint surgery. American volume 57 (1): 7680. PMID 1123375 (//www.ncbi.nlm.nih.gov/pubmed /1123375). ^ a b Venn, M.; Maroudas, A. (1977). "Chemical composition and swelling of normal and osteoarthrotic femoral head cartilage. I. Chemical composition" (http://www.ncbi.nlm.nih.gov /pmc/articles/PMC1006646). Annals of the Rheumatic Diseases 36 (2): 121129. doi:10.1136/ard.36.2.121 (http://dx.doi.org/10.1136%2Fard.36.2.121). PMC 1006646 (//www.ncbi.nlm.nih.gov/pmc/articles /PMC1006646). PMID 856064 (//www.ncbi.nlm.nih.gov/pubmed/856064). ^ Zhang W, Doherty M, Peat G et al. (March 2010). "EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis". Ann. Rheum. Dis. 69 (3): 4839. doi:10.1136/ard.2009.113100 (http://dx.doi.org/10.1136%2Fard.2009.113100). PMID 19762361 (//www.ncbi.nlm.nih.gov/pubmed /19762361). ^ Bierma-Zeinstra SM, Oster JD, Bernsen RM, Verhaar JA, Ginai AZ, Bohnen AM (August 2002). "Joint space narrowing and relationship with symptoms and signs in adults consulting for hip pain in primary care" (http://www.jrheum.org /cgi/pmidlookup?view=long&pmid=12180735). J. Rheumatol. 29 (8): 17138. PMID 12180735 (//www.ncbi.nlm.nih.gov/pubmed/12180735). ^ Osteoarthritis (OA): Joint Disorders (http://www.merck.com/mmpe/sec04/ch034 /ch034e.html) at Merck Manual of Diagnosis and Therapy Professional Edition ^ Phillips CR, Brasington RD (2010). "Osteoarthritis treatment update: Are NSAIDs still in the picture?" (http://www.musculoskeletalnetwork.com/display /article/1145622/1517357). Journal of Musculoskeletal Medicine 27 (2). ^ Kalunian, Kenneth C (2013). "Patient information: Osteoarthritis symptoms and diagnosis (Beyond the
8/3/2013 1:08 PM
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
31.
32.
33.
34.
35.
36.
37.
38. 39.
10 of 13
Basics)" (http://www.uptodate.com/patients/content /topic.do?topicKey=~77ll0j9jfS9fuD). UpToDate. Retrieved 15 February 2013. ^ Altman R, Alarcn G, Appelrouth D et al. (1990). "The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hand". Arthritis Rheum. 33 (11): 160110. doi:10.1002/art.1780331101 (http://dx.doi.org /10.1002%2Fart.1780331101). PMID 2242058 (//www.ncbi.nlm.nih.gov/pubmed/2242058). ^ Neil Vasan; Le, Tao; Bhushan, Vikas (2010). First Aid for the USMLE Step 1, 2010 (First Aid USMLE) (http://books.google.se/books?id=eVAtPktgw0UC& pg=PA169). McGraw-Hill Medical. p. 378. ISBN 0-07-163340-5. ^ a b c d e Flood J (March 2010). "The role of acetaminophen in the treatment of osteoarthritis" (http://www.ajmc.com/publications/supplement /2010/A278_10mar_Pain/A278_2010mar_Flood/). Am J Manag Care 16 (Suppl Management): S4854. PMID 20297877 (//www.ncbi.nlm.nih.gov/pubmed /20297877). ^ a b Cibulka MT, White DM, Woehrle J, et al. (April 2009). "Hip pain and mobility deficitship osteoarthritis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association". J Orthop Sports Phys Ther 39 (4): A125. doi:10.2519/jospt.2009.0301 (http://dx.doi.org /10.2519%2Fjospt.2009.0301). PMID 19352008 (//www.ncbi.nlm.nih.gov/pubmed/19352008). ^ Hagen, KB; Dagfinrud, H; Moe, RH; sters, N; Kjeken, I; Grotle, M; Smedslund, G (2012 Dec 19). "Exercise therapy for bone and muscle health: an overview of systematic reviews.". BMC medicine 10: 167. PMID 23253613 (//www.ncbi.nlm.nih.gov /pubmed/23253613). ^ Wang, SY; Olson-Kellogg, B; Shamliyan, TA; Choi, JY; Ramakrishnan, R; Kane, RL (2012 Nov 6). "Physical therapy interventions for knee pain secondary to osteoarthritis: a systematic review". Annals of internal medicine 157 (9): 63244. doi:10.7326/0003-4819-157-9-201211060-00007 (http://dx.doi.org /10.7326%2F0003-4819-157-9-201211060-00007). PMID 23128863 (//www.ncbi.nlm.nih.gov/pubmed /23128863). ^ De Luigi, AJ (2012 May). "Complementary and alternative medicine in osteoarthritis.". PM & R : the journal of injury, function, and rehabilitation 4 (5 Suppl): S12233. PMID 22632691 (//www.ncbi.nlm.nih.gov/pubmed/22632691). ^ http://www.japmaonline.org/content/82/3/136.short ^ http://onlinelibrary.wiley.com/doi/10.1002
/14651858.CD004020.pub2/pdf/standard 40. ^ Page CJ, Hinman RS, Bennell KL (2011). "Physiotherapy management of knee osteoarthritis". Int J Rheum Dis 14 (2): 145152. doi:10.1111/j.1756-185X.2011.01612.x (http://dx.doi.org /10.1111%2Fj.1756-185X.2011.01612.x). PMID 21518313 (//www.ncbi.nlm.nih.gov/pubmed /21518313). 41. ^ Rannou F, Dimet J, Boutron I, et al. (May 2009). "Splint for base-of-thumb osteoarthritis: a randomized trial" (http://www.annals.org /article.aspx?volume=150&page=661). Ann. Intern. Med. 150 (10): 6619. doi:10.7326/0003-4819-150-10-200905190-00003 (http://dx.doi.org /10.7326%2F0003-4819-150-10-200905190-00003). PMID 19451573 (//www.ncbi.nlm.nih.gov/pubmed /19451573). 42. ^ French HP, Brennan A, White B, Cusack T (2011). "Manual therapy for osteoarthritis of the hip or knee a systematic review". Man Ther 16 (2): 109117. doi:10.1016/j.math.2010.10.011 (http://dx.doi.org /10.1016%2Fj.math.2010.10.011). PMID 21146444 (//www.ncbi.nlm.nih.gov/pubmed/21146444). 43. ^ Sturnieks DL, Tiedemann A, Chapman K, Munro B, Murray SM, Lord SR (November 2004). "Physiological risk factors for falls in older people with lower limb arthritis" (http://www.jrheum.org /cgi/pmidlookup?view=long&pmid=15517643). J. Rheumatol. 31 (11): 22729. PMID 15517643 (//www.ncbi.nlm.nih.gov/pubmed/15517643). 44. ^ Zhang W, Moskowitz RW, Nuki G et al. (September 2007). "OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence". Osteoarthr. Cartil. 15 (9): 9811000. doi:10.1016/j.joca.2007.06.014 (http://dx.doi.org /10.1016%2Fj.joca.2007.06.014). PMID 17719803 (//www.ncbi.nlm.nih.gov/pubmed/17719803). 45. ^ Chen, YF; Jobanputra, P; Barton, P; Bryan, S; Fry-Smith, A; Harris, G; Taylor, RS (April 2008). "Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation". Health technology assessment 12 (11): 1278, iii. PMID 18405470 (//www.ncbi.nlm.nih.gov /pubmed/18405470). 46. ^ a b c Altman R, Barkin RL (March 2009). "Topical therapy for osteoarthritis: clinical and pharmacologic perspectives". Postgrad Med 121 (2): 13947. doi:10.3810/pgm.2009.03.1986 (http://dx.doi.org
8/3/2013 1:08 PM
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
47.
48.
49.
50.
51.
52.
/10.3810%2Fpgm.2009.03.1986). PMID 19332972 (//www.ncbi.nlm.nih.gov/pubmed/19332972). ^ Nesch E, Rutjes AW, Husni E, Welch V, Jni P (2009). "Oral or transdermal opioids for osteoarthritis of the knee or hip". In Nesch, Eveline. Cochrane Database Syst Rev (4): CD003115. doi:10.1002/14651858.CD003115.pub3 (http://dx.doi.org /10.1002%2F14651858.CD003115.pub3). PMID 19821302 (//www.ncbi.nlm.nih.gov/pubmed /19821302). ^ a b c d e De Silva, V; El-Metwally, A; Ernst, E; Lewith, G; Macfarlane, GJ; Arthritis Research UK Working Group on Complementary and Alternative, Medicines (2011 May). "Evidence for the efficacy of complementary and alternative medicines in the management of osteoarthritis: a systematic review.". Rheumatology (Oxford, England) 50 (5): 91120. PMID 21169345 (//www.ncbi.nlm.nih.gov/pubmed /21169345). ^ Arroll B, Goodyear-Smith F (April 2004). "Corticosteroid injections for osteoarthritis of the knee: meta-analysis" (http://www.ncbi.nlm.nih.gov /pmc/articles/PMC387479). BMJ 328 (7444): 869. doi:10.1136/bmj.38039.573970.7C (http://dx.doi.org /10.1136%2Fbmj.38039.573970.7C). PMC 387479 (//www.ncbi.nlm.nih.gov/pmc/articles/PMC387479). PMID 15039276 (//www.ncbi.nlm.nih.gov/pubmed /15039276). ^ a b Rutjes AW, Jni P, da Costa BR, Trelle S, Nesch E, Reichenbach S (August 2012). "Viscosupplementation for osteoarthritis of the knee: a systematic review and meta-analysis" (http://www.annals.org/article.aspx?volume=157& page=180). Ann. Intern. Med. 157 (3): 18091. doi:10.7326/0003-4819-157-3-201208070-00473 (http://dx.doi.org /10.7326%2F0003-4819-157-3-201208070-00473). PMID 22868835 (//www.ncbi.nlm.nih.gov/pubmed /22868835). ^ Santaguida, PL; Hawker, GA, Hudak, PL, Glazier, R, Mahomed, NN, Kreder, HJ, Coyte, PC, Wright, JG (December 2008). "Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review" (http://www.ncbi.nlm.nih.gov /pmc/articles/PMC2592576). Canadian journal of surgery. Journal canadien de chirurgie 51 (6): 42836. PMC 2592576 (//www.ncbi.nlm.nih.gov /pmc/articles/PMC2592576). PMID 19057730 (//www.ncbi.nlm.nih.gov/pubmed/19057730). ^ Carr, AJ; Robertsson, O; Graves, S; Price, AJ; Arden, NK; Judge, A; Beard, DJ (7 April 2012). "Knee replacement". Lancet 379 (9823): 133140. doi:10.1016/S0140-6736(11)60752-6 (http://dx.doi.org
53.
54.
55. 56.
57.
58.
59.
60. 61.
62.
/10.1016%2FS0140-6736%2811%2960752-6). PMID 22398175 (//www.ncbi.nlm.nih.gov/pubmed /22398175). ^ Moseley JB, O'Malley K, Petersen NJ et al. (2002). "A controlled trial of arthroscopic surgery for osteoarthritis of the knee is proven to bring an improvement lasting for about two years" (http://content.nejm.org/cgi/content/full/347/2/81). The New England Journal of Medicine 347 (2): 818. doi:10.1056/NEJMoa013259 (http://dx.doi.org /10.1056%2FNEJMoa013259). PMID 12110735 (//www.ncbi.nlm.nih.gov/pubmed/12110735). ^ Lopez, HL (2012 May). "Nutritional interventions to prevent and treat osteoarthritis. Part II: focus on micronutrients and supportive nutraceuticals.". PM & R : the journal of injury, function, and rehabilitation 4 (5 Suppl): S15568. PMID 22632695 (//www.ncbi.nlm.nih.gov/pubmed/22632695). ^ . PMID 19856319 (//www.ncbi.nlm.nih.gov /pubmed/19856319). Missing or empty |title= (help) ^ a b Rosenbaum CC, O'Mathna DP, Chavez M, Shields K (2010). "Antioxidants and antiinflammatory dietary supplements for osteoarthritis and rheumatoid arthritis". Altern Ther Health Med 16 (2): 3240. PMID 20232616 (//www.ncbi.nlm.nih.gov/pubmed/20232616). ^ Pirotta, M (2010 Sep). "Arthritis disease - the use of complementary therapies.". Australian family physician 39 (9): 63840. PMID 20877766 (//www.ncbi.nlm.nih.gov/pubmed/20877766). ^ Ernst, E (2008 Dec 17). "Frankincense: systematic review.". BMJ (Clinical research ed.) 337: a2813. PMID 19091760 (//www.ncbi.nlm.nih.gov/pubmed /19091760). ^ Rosenbaum, CC; O'Mathna, DP; Chavez, M; Shields, K (2010 Mar-Apr). "Antioxidants and antiinflammatory dietary supplements for osteoarthritis and rheumatoid arthritis.". Alternative therapies in health and medicine 16 (2): 3240. PMID 21553931 (//www.ncbi.nlm.nih.gov/pubmed /21553931). ^ The effects of Glucosamine Sulphate on OA of the knee joint (http://www.bestbets.org /bets/bet.php?id=979). BestBets. ^ Burdett, N; McNeil, JD (2012 Sep). "Difficulties with assessing the benefit of glucosamine sulphate as a treatment for osteoarthritis.". International journal of evidence-based healthcare 10 (3): 2226. PMID 22925619 (//www.ncbi.nlm.nih.gov/pubmed /22925619). ^ Wandel, S; Jni, P; Tendal, B; Nesch, E; Villiger, PM; Welton, NJ; Reichenbach, S; Trelle, S (2010 Sep 16). "Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network
8/3/2013 1:08 PM
11 of 13
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
63.
64.
65.
66.
67.
68.
69.
meta-analysis.". BMJ (Clinical research ed.) 341: c4675. PMID 20847017 (//www.ncbi.nlm.nih.gov /pubmed/20847017). ^ Poolsup N, Suthisisang C, Channark P, Kittikulsuth W (2005). "Glucosamine long-term treatment and the progression of knee osteoarthritis: systematic review of randomized controlled trials". The Annals of pharmacotherapy 39 (6): 10807. doi:10.1345/aph.1E576 (http://dx.doi.org /10.1345%2Faph.1E576). PMID 15855241 (//www.ncbi.nlm.nih.gov/pubmed/15855241). ^ Black C, Clar C, Henderson R et al. (November 2009). "The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation" (http://www.hta.ac.uk/execsumm/summ1352.htm). Health Technol Assess 13 (52): 1148. doi:10.3310/hta13520 (http://dx.doi.org /10.3310%2Fhta13520). PMID 19903416 (//www.ncbi.nlm.nih.gov/pubmed/19903416). ^ Vlad SC, Lavalley MP, McAlindon TE, Felson DT (2007). "Glucosamine for pain in osteoarthritis: Why do trial results differ?". Arthritis & Rheumatism 56 (7): 226777. doi:10.1002/art.22728 (http://dx.doi.org /10.1002%2Fart.22728). PMID 17599746 (//www.ncbi.nlm.nih.gov/pubmed/17599746). ^ Rovati, LC; Girolami, F; Persiani, S (2012 Jun). "Crystalline glucosamine sulfate in the management of knee osteoarthritis: efficacy, safety, and pharmacokinetic properties.". Therapeutic advances in musculoskeletal disease 4 (3): 16780. PMID 22850875 (//www.ncbi.nlm.nih.gov/pubmed /22850875). ^ Zhang W, Moskowitz RW, Nuki G et al. (February 2008). "OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines" (http://www.oarsi.org /pdfs/part_II_OARSI_recommendations_for_manage ment_of_hipknee_OA_2007.pdf). Osteoarthr. Cartil. 16 (2): 13762. doi:10.1016/j.joca.2007.12.013 (http://dx.doi.org/10.1016%2Fj.joca.2007.12.013). PMID 18279766 (//www.ncbi.nlm.nih.gov/pubmed /18279766). ^ Henrotin, Y; Mobasheri, A; Marty, M (2012 Jan 30). "Is there any scientific evidence for the use of glucosamine in the management of human osteoarthritis?". Arthritis research & therapy 14 (1): 201. PMID 22293240 (//www.ncbi.nlm.nih.gov /pubmed/22293240). ^ Miller KL, Clegg DO (February 2011). "Glucosamine and chondroitin sulfate". Rheum. Dis. Clin. North Am. 37 (1): 10318. doi:10.1016/j.rdc.2010.11.007 (http://dx.doi.org
70.
71.
72.
73.
74.
75.
76.
/10.1016%2Fj.rdc.2010.11.007). PMID 21220090 (//www.ncbi.nlm.nih.gov/pubmed/21220090). "The best current evidence suggests that the effect of these supplements, alone or in combination, on OA pain, function, and radiographic change is marginal at best." ^ Reichenbach S, Sterchi R, Scherer M et al. (2007). "Meta-analysis: chondroitin for osteoarthritis of the knee or hip". Ann. Intern. Med. 146 (8): 58090. PMID 17438317 (//www.ncbi.nlm.nih.gov/pubmed /17438317). ^ Manheimer E, Cheng K, Linde K et al. (2010). "Acupuncture for peripheral joint osteoarthritis" (http://www.ncbi.nlm.nih.gov/pmc/articles /PMC3169099). In Manheimer, Eric. Cochrane Database Syst Rev (1): CD001977. doi:10.1002/14651858.CD001977.pub2 (http://dx.doi.org /10.1002%2F14651858.CD001977.pub2). PMC 3169099 (//www.ncbi.nlm.nih.gov/pmc/articles /PMC3169099). PMID 20091527 (//www.ncbi.nlm.nih.gov/pubmed/20091527). ^ Wang, S; Kain ZN; White PF (2008). "Acupuncture Analgesia: II. Clinical Considerations" (http://www.thecochranelibrary.com/.../file /Acupuncture.../CD001977.pdf). Anesth Analg 106 (2): 61121. doi:10.1213/ane.0b013e318160644d (http://dx.doi.org /10.1213%2Fane.0b013e318160644d). PMID 18227323 (//www.ncbi.nlm.nih.gov/pubmed /18227323). ^ Rutjes AW, Nesch E, Sterchi R et al. (2009). "Transcutaneous electrostimulation for osteoarthritis of the knee". In Rutjes, Anne WS. Cochrane Database Syst Rev (4): CD002823. doi:10.1002/14651858.CD002823.pub2 (http://dx.doi.org /10.1002%2F14651858.CD002823.pub2). PMID 19821296 (//www.ncbi.nlm.nih.gov/pubmed /19821296). ^ "WHO Disease and injury country estimates" (http://www.who.int/healthinfo /global_burden_disease/estimates_country /en/index.html). World Health Organization. 2009. Retrieved Nov. 11, 2009. ^ Vos, T (2012 Dec 15). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010.". Lancet 380 (9859): 216396. PMID 23245607 (//www.ncbi.nlm.nih.gov/pubmed/23245607). ^ Green GA (2001). "Understanding NSAIDs: from aspirin to COX-2". Clin Cornerstone 3 (5): 5060. doi:10.1016/S1098-3597(01)90069-9 (http://dx.doi.org
12 of 13
8/3/2013 1:08 PM
Osteoarthritis - Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Osteoarthritis
77. 78.
79.
80.
/10.1016%2FS1098-3597%2801%2990069-9). PMID 11464731 (//www.ncbi.nlm.nih.gov/pubmed /11464731). ^ Hospitalizations for Osteoarthritis Rising Sharply (http://newswise.com/articles/view/544029/) Newswise, Retrieved on September 4, 2008. ^ The global burden of disease : 2004 update.. [Online-Ausg.] ed. Geneva, Switzerland: World Health Organization; 2008. ISBN 9789241563710. p. 35. ^ Molnar, R. E., 2001, Theropod paleopathology: a literature survey: In: Mesozoic Vertebrate Life, edited by Tanke, D. H., and Carpenter, K., Indiana University Press, p. 337-363. ^ Civjan, Natanya (2012). Chemical Biology:
Approaches to Drug Discovery and Development to Targeting Disease (http://books.google.com /books?id=ezXLFlwfJycC&pg=PA313). John Wiley & Sons. p. 313. ISBN 9781118437674. 81. ^ Bruyre, O; Burlet, N; Delmas, PD; Rizzoli, R; Cooper, C; Reginster, JY (16 December 2008). "Evaluation of symptomatic slow-acting drugs in osteoarthritis using the GRADE system" (http://www.ncbi.nlm.nih.gov/pmc/articles /PMC2627841). BMC musculoskeletal disorders 9: 165. doi:10.1186/1471-2474-9-165 (http://dx.doi.org /10.1186%2F1471-2474-9-165). PMC 2627841 (//www.ncbi.nlm.nih.gov/pmc/articles/PMC2627841). PMID 19087296 (//www.ncbi.nlm.nih.gov/pubmed /19087296).
External links
American College of Rheumatology Factsheet on OA (http://www.rheumatology.org/practice/clinical /patients/diseases_and_conditions/osteoarthritis.asp) Osteoarthritis (http://www.arthritis.org/disease-center.php?disease_id=32) The Arthritis Foundation Treatment Guidelines. (http://www.oarsi.org/index2.cfm?section=Publications_and_Newsroom& content=OAGuidelines) Osteoarthritis Research Society International. Recommendations for the management of hip and knee osteoarthritis. Part II OARSI Recommendations for Management of Hip & Knee OA 2007. Part III Changes in Evidence 2010. Retrieved from "http://en.wikipedia.org/w/index.php?title=Osteoarthritis&oldid=564458906" Categories: Arthritis Skeletal disorders This page was last modified on 16 July 2013 at 04:34. Text is available under the Creative Commons Attribution-ShareAlike License; additional terms may apply. By using this site, you agree to the Terms of Use and Privacy Policy. Wikipedia is a registered trademark of the Wikimedia Foundation, Inc., a non-profit organization.
13 of 13
8/3/2013 1:08 PM
Você também pode gostar
- OsteoarthritisDocumento3 páginasOsteoarthritisVanessa Da CruzAinda não há avaliações
- AnatomyDocumento10 páginasAnatomyapi-3845840Ainda não há avaliações
- Typical Clinical Symptoms Are Pain, Particularly After ProlongedDocumento12 páginasTypical Clinical Symptoms Are Pain, Particularly After Prolongedifa afifahAinda não há avaliações
- Review Article: Aging and Osteoarthritis: An Inevitable Encounter?Documento7 páginasReview Article: Aging and Osteoarthritis: An Inevitable Encounter?Iicha Phine'ToxicAinda não há avaliações
- PrimaryOsteoarthritis StatPearls NCBIBookshelfDocumento7 páginasPrimaryOsteoarthritis StatPearls NCBIBookshelfWALKING MORE STORE IDAinda não há avaliações
- OsteoarthritisDocumento23 páginasOsteoarthritisGoutham VGouthamAinda não há avaliações
- Osteoarthritis: BackgroundDocumento9 páginasOsteoarthritis: BackgroundNathania LongkutoyAinda não há avaliações
- Osteoarthritis and Fibromyalgia: by Tamara MitchellDocumento13 páginasOsteoarthritis and Fibromyalgia: by Tamara MitchellmailbabuAinda não há avaliações
- Understanding Medical PaperDocumento4 páginasUnderstanding Medical Paperrhn 5b1coolAinda não há avaliações
- Effects of Exercise and Physical Activity On Knee OsteoarthritisDocumento9 páginasEffects of Exercise and Physical Activity On Knee OsteoarthritisJoseph LimAinda não há avaliações
- Chapter 24 - Arthritis - Osteoarthritis, Gout, & Amp Rheumatoid ArthritisDocumento23 páginasChapter 24 - Arthritis - Osteoarthritis, Gout, & Amp Rheumatoid ArthritisHarris GhifaryAinda não há avaliações
- Bilateral OsteoarthritisDocumento58 páginasBilateral OsteoarthritisMaya VilAinda não há avaliações
- Jact13i2p154 Arya Osteoarthritis of The Knee Joint An OverviewDocumento9 páginasJact13i2p154 Arya Osteoarthritis of The Knee Joint An OverviewErwynk EriantoAinda não há avaliações
- ArthritisDocumento8 páginasArthritissdorji72Ainda não há avaliações
- OsteoarthritisDocumento5 páginasOsteoarthritisprincess0fdeathAinda não há avaliações
- Biomechanics and Pathomechanisms of Osteoarthritis: Christian Egloff, Thomas Hügle, Victor ValderrabanoDocumento14 páginasBiomechanics and Pathomechanisms of Osteoarthritis: Christian Egloff, Thomas Hügle, Victor ValderrabanobertouwAinda não há avaliações
- BMJ 2006 p639Documento5 páginasBMJ 2006 p639Wahab RasyidAinda não há avaliações
- 08 Brandt EtiologyOA Review RheumClinNADocumento29 páginas08 Brandt EtiologyOA Review RheumClinNAPrincessDianna SulitAinda não há avaliações
- عرض تقديمي 28Documento33 páginasعرض تقديمي 28saifmajidhammadiAinda não há avaliações
- ArthritisDocumento6 páginasArthritisChristel Mariz SantellaAinda não há avaliações
- OsteoarthritisDocumento6 páginasOsteoarthritisKristine ValenciaAinda não há avaliações
- What Is Osteoarthritis?: ArthritisDocumento4 páginasWhat Is Osteoarthritis?: ArthritisJohn Mark Alvin TorresAinda não há avaliações
- Oa Ar GoutDocumento18 páginasOa Ar GoutnerdwaldoAinda não há avaliações
- OsteoarthritisDocumento15 páginasOsteoarthritisMichael BanksAinda não há avaliações
- Common Causes of Severe Knee PainDocumento8 páginasCommon Causes of Severe Knee PainRatnaPrasadNalamAinda não há avaliações
- OA Fact SheetDocumento3 páginasOA Fact SheetGamal AzmiAinda não há avaliações
- OsteoarthritisDocumento8 páginasOsteoarthritisNianurmayanti983278Ainda não há avaliações
- OsteoarthritsDocumento34 páginasOsteoarthritssamiul bashirAinda não há avaliações
- Arthritis: Osteoarthritis (OA or Degenerative Arthritis) Osteoarthritis FactsDocumento6 páginasArthritis: Osteoarthritis (OA or Degenerative Arthritis) Osteoarthritis FactsFelisitas FellAinda não há avaliações
- What Causes Osteoarthritis?Documento9 páginasWhat Causes Osteoarthritis?jajabsAinda não há avaliações
- What Is OsteoarthritisDocumento12 páginasWhat Is OsteoarthritischicktankAinda não há avaliações
- Osteoarthritis PDFDocumento15 páginasOsteoarthritis PDFعبدالرحمن علىAinda não há avaliações
- Osteoarthritis: Major Cause of Morbidity and InabilityDocumento10 páginasOsteoarthritis: Major Cause of Morbidity and Inabilitymanuel124Ainda não há avaliações
- Thesis On Osteoarthritis KneeDocumento4 páginasThesis On Osteoarthritis Kneednrrt4fr100% (2)
- Arthritis (From Greek Arthro-, Joint + - Itis, Inflammation Plural: Arthritides) Is A Group ofDocumento11 páginasArthritis (From Greek Arthro-, Joint + - Itis, Inflammation Plural: Arthritides) Is A Group ofDebbie Martir-PuyaoanAinda não há avaliações
- Osteoarthritis 2018Documento45 páginasOsteoarthritis 2018Rizcky Naldy Eka PutraAinda não há avaliações
- OsteoarthritisDocumento26 páginasOsteoarthritisRidwan MuttaqinAinda não há avaliações
- Skeletal System: Univ. Ovidius Facultatea de Medicina Iosub Elena Iordache Cristina Sursa:WikipediaDocumento26 páginasSkeletal System: Univ. Ovidius Facultatea de Medicina Iosub Elena Iordache Cristina Sursa:WikipediaCristian LuncasuAinda não há avaliações
- Artrosis Libro ClevelandDocumento3 páginasArtrosis Libro ClevelandFrancisco Palma CarvajalAinda não há avaliações
- Digestive SystemDocumento13 páginasDigestive SystemGino R. MonteloyolaAinda não há avaliações
- Osteoarthritis and GoutDocumento69 páginasOsteoarthritis and Goutadamu mohammadAinda não há avaliações
- Disorders of BonesDocumento3 páginasDisorders of BonesAnonymous 0pSLjJYAinda não há avaliações
- Osteoarthritis PDFDocumento25 páginasOsteoarthritis PDFJa KovAinda não há avaliações
- Pharmaceutical Care of Patients With OsteoarthritisDocumento16 páginasPharmaceutical Care of Patients With Osteoarthritiskhairul hudaAinda não há avaliações
- عرض تقديمي 28Documento33 páginasعرض تقديمي 28saifmajidhammadiAinda não há avaliações
- Osteoarthritis Facts: ArthritisDocumento2 páginasOsteoarthritis Facts: ArthritisparciAinda não há avaliações
- Knee Arthritis - Johns HopkinsDocumento4 páginasKnee Arthritis - Johns HopkinsCarmel HarelAinda não há avaliações
- Apley OA 2Documento11 páginasApley OA 2Koko AgungAinda não há avaliações
- Group 3 Fact Sheet Degenerative Joint Disease OsteoarthritisDocumento6 páginasGroup 3 Fact Sheet Degenerative Joint Disease OsteoarthritisJoe Aire SalvediaAinda não há avaliações
- Osteoarthritis - Dont EraseDocumento3 páginasOsteoarthritis - Dont EraseLynlyn AlforqueAinda não há avaliações
- Pathophysiology 7 EDITION: Concepts of Health and Disease: American Academy of Orthopedic Surgeons (Orthoinfo)Documento2 páginasPathophysiology 7 EDITION: Concepts of Health and Disease: American Academy of Orthopedic Surgeons (Orthoinfo)Justine Simeon lagunzadAinda não há avaliações
- Osteoarthritis: Pathology, Diagnosis, and Treatment OptionsDocumento19 páginasOsteoarthritis: Pathology, Diagnosis, and Treatment OptionsTrino Rangel FonsecaAinda não há avaliações
- Osteoarthrosis / Osteoarthritis: Entitlement Eligibility GuidelinesDocumento26 páginasOsteoarthrosis / Osteoarthritis: Entitlement Eligibility GuidelinesNinaAinda não há avaliações
- Common Rheumatologic Disease (Reichel's)Documento9 páginasCommon Rheumatologic Disease (Reichel's)AhmedAinda não há avaliações
- Achilles TendinitisDocumento3 páginasAchilles Tendinitisapi-242361004Ainda não há avaliações
- Degenerative Joint DiseasesDocumento30 páginasDegenerative Joint DiseasesBahaa ShaabanAinda não há avaliações
- Apyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiDocumento131 páginasApyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiFathimathAinda não há avaliações
- Literature Review On Knee OsteoarthritisDocumento4 páginasLiterature Review On Knee Osteoarthritiseyewhyvkg100% (1)
- Review Injeksi Intraartikular Pada OA LututDocumento12 páginasReview Injeksi Intraartikular Pada OA LututUmmu Qonitah AfnidawatiAinda não há avaliações
- Smithing - Skyrim Wiki Guide - IGNDocumento10 páginasSmithing - Skyrim Wiki Guide - IGNXaythinanh Philama'Ainda não há avaliações
- Building Clearing, Tactical RaidDocumento17 páginasBuilding Clearing, Tactical Raidcarabinieri2100% (1)
- Procurement - EProcurement - E-Bidding Req-Bidding Req..Documento1 páginaProcurement - EProcurement - E-Bidding Req-Bidding Req..Xaythinanh Philama'Ainda não há avaliações
- Procurement - Prequalification - Section IDocumento6 páginasProcurement - Prequalification - Section IXaythinanh Philama'Ainda não há avaliações
- Heavy Equipment (Construction) - Wikipedia, The Free EncyclopediaDocumento7 páginasHeavy Equipment (Construction) - Wikipedia, The Free EncyclopediaXaythinanh Philama'Ainda não há avaliações
- Lac CaninumDocumento4 páginasLac CaninumByron José Cerda PalaciosAinda não há avaliações
- Risk Factors For Postoperative Nausea and VomitingDocumento21 páginasRisk Factors For Postoperative Nausea and VomitingmusafirlautAinda não há avaliações
- Autonomic HyperreflexiaDocumento3 páginasAutonomic HyperreflexiaGibe BebitaAinda não há avaliações
- Updated Activity Analysis Using The Occupational Therapy Practice Framework IIIDocumento49 páginasUpdated Activity Analysis Using The Occupational Therapy Practice Framework IIIIan Russ Bautista100% (2)
- Contraceptive Comparison ChartDocumento1 páginaContraceptive Comparison ChartdryasirsaeedAinda não há avaliações
- Satiereal Product Sheet - 2016Documento2 páginasSatiereal Product Sheet - 2016JudyCobbettAinda não há avaliações
- Skin Diseases Affecting The VulvaDocumento7 páginasSkin Diseases Affecting The VulvaNoraAinda não há avaliações
- Ccu PSG en DysphagiaDocumento52 páginasCcu PSG en DysphagiaTni JolieAinda não há avaliações
- Ameloblastoma of The Jaw and Maxillary Bone: Clinical Study and Report of Our ExperienceDocumento7 páginasAmeloblastoma of The Jaw and Maxillary Bone: Clinical Study and Report of Our ExperienceKharismaNisaAinda não há avaliações
- Treating Double VisionDocumento2 páginasTreating Double VisionNi Kadek Sri WidiyantiAinda não há avaliações
- NCP-Ineffective AirwayDocumento5 páginasNCP-Ineffective Airwayjava_biscocho1229Ainda não há avaliações
- NCP MyomaDocumento6 páginasNCP MyomaIzza Mae Ferrancol PastranaAinda não há avaliações
- Apically Extruded Sealers - Fate and Influence On Treatment OutcomeDocumento8 páginasApically Extruded Sealers - Fate and Influence On Treatment OutcomeDumitruCheleAinda não há avaliações
- When People Are Dying: Palliative CareDocumento17 páginasWhen People Are Dying: Palliative Carenerlyn100% (1)
- Prelim List of DrugsDocumento20 páginasPrelim List of DrugsJayson Izon SantosAinda não há avaliações
- Personal Statement For Master in Public Health - 2Documento2 páginasPersonal Statement For Master in Public Health - 2fopoku2k2100% (2)
- Vitality Atlas 3.3 FINALDocumento10 páginasVitality Atlas 3.3 FINALJakarta ClinicAinda não há avaliações
- Cpi Final Assessment ErmcDocumento9 páginasCpi Final Assessment Ermcapi-528037163Ainda não há avaliações
- Drug StudyDocumento5 páginasDrug StudyColleen De la RosaAinda não há avaliações
- Classification of Iatrogenic Bile Duct Injury - 2Documento5 páginasClassification of Iatrogenic Bile Duct Injury - 2RameshKumarAinda não há avaliações
- Scas Boys 8 11 ScorerDocumento4 páginasScas Boys 8 11 ScorerJuan Jesús Ruiz CornelloAinda não há avaliações
- CHAPTER 7: Mood Disorders and SuicideDocumento13 páginasCHAPTER 7: Mood Disorders and SuicideDana Mikaella CervaAinda não há avaliações
- David BurnsDocumento2 páginasDavid Burnspsic7loga7martos100% (1)
- OrthodonticsDocumento18 páginasOrthodonticsSorinAinda não há avaliações
- Gracewell Product Faq's & Competetor KnockoutsDocumento25 páginasGracewell Product Faq's & Competetor KnockoutskurutalaAinda não há avaliações
- UG Curriculum PMRDocumento3 páginasUG Curriculum PMRSudhir MishraAinda não há avaliações
- Hemorrhoids - Causes, Treatments, and PreventionDocumento5 páginasHemorrhoids - Causes, Treatments, and PreventionSAIFUL ISLAMAinda não há avaliações
- Bhamashah Swasthya Bima Yojana 2017-19: S. No. Final Package Name Package Type Proposed Rate Speciality Code Short NameDocumento21 páginasBhamashah Swasthya Bima Yojana 2017-19: S. No. Final Package Name Package Type Proposed Rate Speciality Code Short Nameswastik hospitalAinda não há avaliações
- DR Mark Sircus - Multiple SclerosisDocumento9 páginasDR Mark Sircus - Multiple Sclerosiswritingbox100% (1)
- EFT Tapping Manual: The Basics of Emotional Freedom TechniquesDocumento29 páginasEFT Tapping Manual: The Basics of Emotional Freedom TechniquesSeriusAinda não há avaliações