Escolar Documentos
Profissional Documentos
Cultura Documentos
The Sistrunk Procedure
Enviado por
DrTarek Mahmoud Abo KammerDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
The Sistrunk Procedure
Enviado por
DrTarek Mahmoud Abo KammerDireitos autorais:
Formatos disponíveis
Operative Techniques in Otolaryngology (2004) 15, 220-223
Excision of thyroglossal duct cyst: the Sistrunk procedure
Gisela Wagner, MD, Jesus E. Medina, MD
From the Department of Otorhinolaryngology, College of Medicine, The University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma. Before 1893, the removal of a thyroglossal cyst included simple incision and drainage. The recurrence rate after this procedure was 50%. In 1893, Schlange1 proposed the excision of the cyst along with the central portion of the hyoid bone. This resulted in a drop in the recurrence rate to 20%. However, in 1920, Walter Sistrunk took this operation one step further and recommended not only taking the central portion of the hyoid bone but also carving out a core or tissue one eighth of an inch in radius from the hyoid bone to the foramen cecum.2 He felt there was no point in identifying the suprahyoid portion of the duct, which it is usually hard to do because the duct may be so small and friable that it breaks off easily and thus it is difcult to remove by itself. Today, the Sistrunk procedure is the standard operation to remove thyroglossal cyst, with reported recurrence rates between 0% and 8%.3,4 presence of the thyroid gland in its normal location and to conrm the cystic nature of the mass.5 Computed tomography or magnetic resonance imaging also may be useful but are not routinely indicated. Some clinicians feel that a thyroid-stimulating hormone level must be obtained before surgery and, if the level is high, the thyroid should be scanned. If, on the other hand, the level is normal, then proceed with surgery.6
Surgical technique
A horizontal incision about 2 inches long at or just below the level of the hyoid bone is made in the midline of the neck (Figure 2). The incision is carried down through the subcutaneous tissue and platysma muscle. Once the skin and platysma are elevated, the cyst can be found lying beneath the raphe connecting the sternohyoid muscles (Figure 3). The strap muscles are retracted laterally, and the cyst is dissected free of the thyroid cartilage and surrounding tissue until it is pedicled superiorly to the hyoid bone (Figure 4). The muscles and soft tissue are then dissected off the central segment of the hyoid bone, about 1.5 to 2 cm in length. Dissecting superiorly or inferiorly to the hyoid bone should be avoided because of the risk of transecting the duct. The hyoid bone is then cut on each side of midline (Figure 5). Without isolating the duct, tissue one eighth of an inch in radius is cored out through the tissues up to and including the foramen cecum (Figure 6). The foramen cecum can be reached by drawing a line backward and upward from the hyoid at a 45 angle through the intersection of the horizontal and perpendicular lines at the center of the hyoid. Placing a retractor through the mouth and into the vallecula to pull the tongue base down into the wound may help with this part of the procedure. Placing a large needle from the hyoid into the foramen cecum may also aid in dissecting out the core.
Diagnostic evaluation
A thyroglossal cyst usually presents as a midline neck mass that is not painful unless it is infected (Figure 1). A key to its diagnosis, which can be observed during physical examination, is the elevation of the mass with swallowing or protrusion of the tongue. Sixty percent to 80% of thyroglossal duct cysts are located below the level of the hyoid bone.3 The differential diagnosis includes dermoid and lingual thyroid. No general consensus is found in the literature on the extent of the diagnostic evaluation of a patient with a suspected thyroglossal duct cyst. Some clinicians feel that it is important to rule out the possibility that this midline mass may be the patients only source of thyroid hormone. To that end, an ultrasound of the neck is a simple and inexpensive test to look for the
Address reprint requests and correspondence: Jesus E. Medina, MD, University of Oklahoma Health Sciences Center, Department of Otorhinolaryngology, PO Box 26901, WP 1360, Oklahoma City, OK 73190-3048.
1043-1810/$ -see front matter 2004 Elsevier Inc. All rights reserved.
Wagner and Medina
Excision of Thyroglossal Duct Cyst
221
Figure 1
Origination and descent of thyroglossal duct cyst.
Once the specimen in removed, the wound is irrigated, and the opening into the pharynx at the foramen cecum is closed with 2-3 absorbable sutures (Figure 7). The strap muscles are approximated, a Penrose drain is placed in the wound, and the subcutaneous tissues and the skin are closed (Figure 8).
Complications
Major complications include recurrence, abscess or hematoma requiring surgical drainage, entry into the airway, the need for tracheotomy, nerve paralysis, hypothyroidism, and death. Reports of these major complications
Figure 2 Skin incision is made midline overlying cyst and thyroid cartilage.
Figure 3 After splitting strap muscles down the middle, the cyst can be grabbed and lifted up as it is dissected free from the surrounding tissues.
222
Operative Techniques in Otolaryngology, Vol 15, No 3, September 2004
Figure 4 Once freed up inferiorly, the cyst can be seen pedicled to the hyoid bone superiorly. Also notice the close relationship between the cyst and the underlying airway.
Figure 6 excised.
The tract can be followed to the foramen cecum and
are rare.7 By identifying the thyroid notch and the thyrohyoid membrane intraoperatively, one can decrease the likelihood of entering the airway. The hypoglossal nerve can be injured if one divides the hyoid too laterally or
dissects too aggressively in the superior direction. Dividing the hyoid medial to the lesser cornu and dissecting superiorly medial to the anterior digastric muscle can avoid this type of injury. Hypothyroidism can be avoided with the proper preoperative evaluation to determine the
Figure 5
The hyoid bone is then cut on each side of the midline.
Figure 7
The opening at the foramen cecum is then closed.
Wagner and Medina
Excision of Thyroglossal Duct Cyst
223 wound infection, and stitch abscess. All were treated with conservative management and resolved without any further sequela.7
References
1. Schlange H: Uber die stual colli congenita. Arch Klin Chir 46:390392, 1893 2. Sistrunk WE: The surgical treatment of cysts of the thyroglossal tract. Ann Surg 71:121-126, 1920 3. Allard R: The throglossal cyst. Head Neck Surg 5:134-146, 1982 4. Pelausa M, Forte V: Sistrunk revisited: A 10-year review of revision thyroglossal duct surgery at Torontos Hospital for Sick Children. J Otolaryngol 18:325-333, 1989 5. Gupta P, Maddalozzo J: Preoperative sonography in presumed thyroglossal duct cysts. Arch Otolaryngol Head Neck Surg 127:200-202, 2001 6. Radkowski D, Arnold J, Healy GB, et al: Thyroglossal duct remnants: Preoperative evaluation and management. Arch Otolaryngol Head Neck Surg 117:1378-1381, 1991 7. Maddalozzo J, Venkatesan TK, Gupta P: Complications associated with Sistrunk procedure. Laryngoscope 111:119-123, 2001
Figure 8 The strap muscles are reapproximated and the skin then closed.
presence of a normal thyroid. Although Maddalozza reported no major complications in his series of 35 patients undergoing a Sistrunk procedure, he did have a 29% occurrence of minor complications such as seroma, local
Você também pode gostar
- AP Statistics Final Examination Multiple-Choice Questions Answers in BoldDocumento17 páginasAP Statistics Final Examination Multiple-Choice Questions Answers in BoldDrTarek Mahmoud Abo KammerAinda não há avaliações
- StridorDocumento3 páginasStridorDrTarek Mahmoud Abo KammerAinda não há avaliações
- Biostatistics A Sample of Questions For The Final ExamDocumento3 páginasBiostatistics A Sample of Questions For The Final ExamDrTarek Mahmoud Abo KammerAinda não há avaliações
- BiostatisticsQUIZ AnswersDocumento5 páginasBiostatisticsQUIZ AnswersDipankar RoyAinda não há avaliações
- Rhinitis in InfancyDocumento3 páginasRhinitis in InfancyDrTarek Mahmoud Abo KammerAinda não há avaliações
- PGRTPPTDocumento95 páginasPGRTPPTDrTarek Mahmoud Abo KammerAinda não há avaliações
- Practice Guidelines For Family Physicians 4 Infection by MansdocsDocumento92 páginasPractice Guidelines For Family Physicians 4 Infection by MansdocsDrTarek Mahmoud Abo KammerAinda não há avaliações
- Rxexam'S Biostatistics Questions & Answers: 2019-2020 EditionDocumento15 páginasRxexam'S Biostatistics Questions & Answers: 2019-2020 EditionPrakash100% (2)
- Answers To Practice Exam 2Documento3 páginasAnswers To Practice Exam 2monerch JoserAinda não há avaliações
- Blood Supply of CochleaDocumento2 páginasBlood Supply of CochleaDrTarek Mahmoud Abo KammerAinda não há avaliações
- Tympanoplasty 120522063636 Phpapp01Documento29 páginasTympanoplasty 120522063636 Phpapp01DrTarek Mahmoud Abo Kammer100% (1)
- Anatomy of A Long BoneDocumento4 páginasAnatomy of A Long BoneDrTarek Mahmoud Abo KammerAinda não há avaliações
- Cochlear Rotation and Its RelevanceDocumento7 páginasCochlear Rotation and Its RelevanceDrTarek Mahmoud Abo KammerAinda não há avaliações
- Eponymous ENT SignsDocumento11 páginasEponymous ENT SignsDrTarek Mahmoud Abo KammerAinda não há avaliações
- Courses in Ainshams - Doc Reviewed 2010 10Documento1 páginaCourses in Ainshams - Doc Reviewed 2010 10DrTarek Mahmoud Abo KammerAinda não há avaliações
- Stridor 1Documento5 páginasStridor 1DrTarek Mahmoud Abo KammerAinda não há avaliações
- Mastoidectomy and EpitympanectomyDocumento18 páginasMastoidectomy and EpitympanectomyDrTarek Mahmoud Abo KammerAinda não há avaliações
- CSF LeaksDocumento3 páginasCSF LeaksDrTarek Mahmoud Abo KammerAinda não há avaliações
- CH 22 - Olfactory Function and DysfunctionDocumento3 páginasCH 22 - Olfactory Function and DysfunctionDrTarek Mahmoud Abo KammerAinda não há avaliações
- Cholesterol Granuloma of Maxillary SinusDocumento6 páginasCholesterol Granuloma of Maxillary SinusDrTarek Mahmoud Abo KammerAinda não há avaliações
- Laryngeal and Tracheal StentsDocumento15 páginasLaryngeal and Tracheal StentsDrTarek Mahmoud Abo KammerAinda não há avaliações
- The Development of The Middle Ear Spaces and Their Surgical SignificanceDocumento15 páginasThe Development of The Middle Ear Spaces and Their Surgical SignificanceDrTarek Mahmoud Abo Kammer100% (2)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- BOM Eligibility CriterionDocumento5 páginasBOM Eligibility CriterionDisara WulandariAinda não há avaliações
- 22Documento22 páginas22vanhau24Ainda não há avaliações
- CIVIL BILL OF QUANTITIESDocumento16 páginasCIVIL BILL OF QUANTITIESTomAinda não há avaliações
- Is411 8Documento1 páginaIs411 8amoghimiAinda não há avaliações
- Marine Pollution Bulletin: Sivanandham Vignesh, Krishnan Muthukumar, Rathinam Arthur JamesDocumento11 páginasMarine Pollution Bulletin: Sivanandham Vignesh, Krishnan Muthukumar, Rathinam Arthur JamesGeorgiana-LuizaAinda não há avaliações
- The Baking and Frozen Dough MarketDocumento4 páginasThe Baking and Frozen Dough MarketMilling and Grain magazineAinda não há avaliações
- Deck Damage and Penetrations: Prepared by Richard B. Heagler, P.EDocumento9 páginasDeck Damage and Penetrations: Prepared by Richard B. Heagler, P.ENelzon MamaniAinda não há avaliações
- Hoja de Seguridad Magnafloc 155 (EN) PDFDocumento6 páginasHoja de Seguridad Magnafloc 155 (EN) PDFIván Martínez-CostaAinda não há avaliações
- Financial Plan Checklist: Planning For EmergenciesDocumento2 páginasFinancial Plan Checklist: Planning For EmergenciesInsan CornerAinda não há avaliações
- Lembar Latihan - P1 - PD MitraDocumento123 páginasLembar Latihan - P1 - PD MitratiengcityAinda não há avaliações
- Maternal and Child Health Nursing, 8 Edition.: LESSON PREVIEW/REVIEW (5 Minutes)Documento7 páginasMaternal and Child Health Nursing, 8 Edition.: LESSON PREVIEW/REVIEW (5 Minutes)raker boiAinda não há avaliações
- Technical PaperDocumento10 páginasTechnical Paperalfosoa5505Ainda não há avaliações
- Iveco F4ge PDFDocumento142 páginasIveco F4ge PDFHandy Lee67% (3)
- B Cell Cytokine SDocumento11 páginasB Cell Cytokine Smthorn1348Ainda não há avaliações
- Definitions of Abnormality by Dr. Kanwal QadeerDocumento7 páginasDefinitions of Abnormality by Dr. Kanwal QadeerHaya EishaAinda não há avaliações
- Study To Assess The Effectiveness of Planned Teaching Programme Regarding Knowledge of Traffic Rules Among Higher Secondary Students 15 18 Years in Selected Schools of DehradunDocumento14 páginasStudy To Assess The Effectiveness of Planned Teaching Programme Regarding Knowledge of Traffic Rules Among Higher Secondary Students 15 18 Years in Selected Schools of DehradunEditor IJTSRDAinda não há avaliações
- Chapter 2 ManojDocumento4 páginasChapter 2 ManojBro FistoAinda não há avaliações
- Case Study - BronchopneumoniaDocumento45 páginasCase Study - Bronchopneumoniazeverino castillo91% (33)
- High Containment Labs and Other Facilities of The US Bio Defense ProgramDocumento1 páginaHigh Containment Labs and Other Facilities of The US Bio Defense ProgramHRCAinda não há avaliações
- F6003 5W40 Synthetic Oil Technical Data SheetDocumento1 páginaF6003 5W40 Synthetic Oil Technical Data SheetValeriy ValkovetsAinda não há avaliações
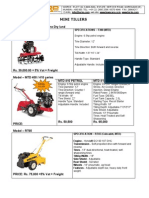
- Optimize soil preparation with a versatile mini tillerDocumento2 páginasOptimize soil preparation with a versatile mini tillerRickson Viahul Rayan C100% (1)
- Process Description of Gambat South Gas Processing FacilityDocumento13 páginasProcess Description of Gambat South Gas Processing FacilitywaheedAinda não há avaliações
- Courses at NeevDocumento10 páginasCourses at NeevDr Mohan SavadeAinda não há avaliações
- Reglas para Añadir Al Verbo Principal: Am Is Are ReadDocumento8 páginasReglas para Añadir Al Verbo Principal: Am Is Are ReadBrandon Sneider Garcia AriasAinda não há avaliações
- Análisis de Estabilidad de TaludesDocumento4 páginasAnálisis de Estabilidad de TaludesJosue Acosta EspinozaAinda não há avaliações
- FLSPfister IB05000 I GBTRWSD0216 MailDocumento26 páginasFLSPfister IB05000 I GBTRWSD0216 MailLuis Angel BusturiaAinda não há avaliações
- Oral Dislocation Rehabilitation Program - FirstDocumento2 páginasOral Dislocation Rehabilitation Program - FirstPriyaki SebastianAinda não há avaliações
- ESD Control Experts: Electrical Overstress (EOS) and Electrostatic Discharge (ESD) EventDocumento39 páginasESD Control Experts: Electrical Overstress (EOS) and Electrostatic Discharge (ESD) EventDaiana SilvaAinda não há avaliações
- FAQ For Company Law 2013Documento24 páginasFAQ For Company Law 2013Archanat07100% (1)
- Tle 7 - 8 Curriculum MapDocumento11 páginasTle 7 - 8 Curriculum MapKristianTubagaAinda não há avaliações