Escolar Documentos
Profissional Documentos
Cultura Documentos
643189771
Enviado por
Jam RapaconDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
643189771
Enviado por
Jam RapaconDireitos autorais:
Formatos disponíveis
JAN
REVIEW PAPER
JOURNAL OF ADVANCED NURSING
Quality of nursing documentation and approaches to its evaluation: a mixed-method systematic review
Ning Wang, David Hailey & Ping Yu
Accepted for publication 22 January 2011
Correspondence to P. Yu: e-mail: ping@uow.edu.au Ning Wang RN PhD Candidate Health Informatics Research Lab, School of Information and Technology, Faculty of Informatics, University of Wollongong, New South Wales, Australia David Hailey PhD Research Fellow Health Informatics Research Lab, School of Information and Technology, Faculty of Informatics, University of Wollongong, New South Wales, Australia Ping Yu PhD Senior Lecturer, Research Director Health Informatics Research Lab, School of Information and Technology, Faculty of Informatics, University of Wollongong, New South Wales, Australia
W A N G N . , H A I L E Y D . & Y U P . ( 2 0 1 1 ) Quality of nursing documentation and approaches to its evaluation: a mixed-method systematic review. Journal of Advanced Nursing 67(9), 18581875. doi: 10.1111/j.1365-2648.2011.05634.x
Abstract
Aims. This paper reports a review that identied and synthesized nursing documentation audit studies, with a focus on exploring audit approaches, identifying audit instruments and describing the quality status of nursing documentation. Introduction. Quality nursing documentation promotes effective communication between caregivers, which facilitates continuity and individuality of care. The quality of nursing documentation has been measured by using various audit instruments, which reected variations in the perception of documentation quality among researchers across countries and settings. Data sources. Searches were made of seven electronic databases. The keywords nursing documentation, audit, evaluation, quality, both singly and in combination, were used to identify articles published in English between 2000 and 2010. Review methods. A mixed-method systematic review of quantitative and qualitative studies concerning nursing documentation audit and reports of audit instrument development was undertaken. Relevant data were extracted and a narrative synthesis was conducted. Results. Seventy-seven publications were included. Audit approaches focused on three natural dimensions of nursing documentation: structure or format, process and content. Numerous audit instruments were identied and their psychometric properties were described. Flaws of nursing documentation were identied and the effects of study interventions on its quality. Conclusion. Research should pay more attention to the accuracy of nursing documentation, factors leading to variation in practice and aws in documentation quality and the effects of these on nursing practice and patient outcomes, and the evaluation of quality measurement. Keywords: audit, evaluation approaches, instruments, nursing documentation, quality, quality criteria, systematic review
1858
2011 Blackwell Publishing Ltd
JAN: REVIEW PAPER
Quality of nursing documentation and audit
Introduction
In modern healthcare organizations, the quality and coordination of care depend on the communication between different caregivers about their patients. Documentation is a communication tool for exchange of information stored in records between nurses and other caregivers (Urquhart et al. 2009). Quality nursing documentation promotes structured, consistent and effective communication between caregivers and facilitates continuity and individuality of care and safety of patients (Bjo rvell et al. 2000, Voutilainen et al. 2004). Nursing documentation is dened as the record of nursing care that is planned and given to individual patients and clients by qualied nurses or by other caregivers under the direction of a qualied nurse (Urquhart et al. 2009). It attempts to show what happens in the nursing process and what decision-making is based on by presenting information about admission, nursing diagnoses, interventions, and the evaluation of progress and outcome (Nilsson & Willman 2000, Karkkainen & Eriksson 2003). In addition, nursing documentation can be used for other purposes such as quality assurance, legal purposes, health planning, allocation of resources and nursing development and research. For achieving these purposes, nursing documentation needs to hold valid and reliable information and comply with established standards (Idvall & Ehrenberg 2002, Karkkainen & Eriksson 2003, Urquhart et al. 2009). Nursing has been concerned with patient data since the early days of Nightingale (Gogler et al. 2008). It was advanced with the introduction of the nursing process into the clinical setting (Oroviogoicoechea et al. 2008). The nursing process is a structured problem-solving approach to nursing practice and education and was rst explained by Yura and Walsh in 1967. It originally comprised of four stages: assessment, planning, implementation and evaluation of care and lately included nursing problem or diagnosis (Bjo rvell et al. 2000). The nursing process model has been widely used as a theoretical basis for nursing practice and documentation. Over the last few decades, more efforts have been made to advance nursing documentation to increase its usability. One of these initiatives was the development and use of researchbased standardized nursing terminologies such as the International Classication of Nursing Practice (ICNP) and the International Nursing Diagnoses Classication (NANDA International). Standardized nursing languages provide common denitions of nursing concepts and allow for theorybased and comparable nursing data to emerge. Therefore,
2011 Blackwell Publishing Ltd
they promote shared understanding and continuity of care and make it possible to use records for research and management purposes (Mu ller-Staub et al. 2007, Thoroddsen & Ehnfors 2007). The introduction of electronic documentation systems into care practice has led to the transformation of nursing record-keeping. Electronic documentation systems can improve health professionals access to more complete, accurate, legible and up-to-date patient data (Larrabee et al. 2001, Oroviogoicoechea et al. 2008), although their effects on patient outcomes are inconclusive (Urquhart et al. 2009). With the widespread use of information technologies in nursing practice, standardized nursing language becomes essential because a uniform and controlled vocabulary enables electronic documentation systems to aggregate data (Ehrenberg et al. 2001, Mu ller-Staub et al. 2008b). Despite the wide recognition of the importance of quality nursing documentation and efforts made to enhance it, there are inconsistencies in the denition of good nursing documentation because of variations in nursing documentation practice based on different local requirements, documentation systems and terminologies across countries and settings. In research settings, the quality of nursing documentation has been assessed by various auditing instruments with different criteria reecting how quality was perceived by the researchers. There have been several recent reviews of nursing documentation. A systematic review conducted by Saranto and Kinnunen (2009) covered 41 studies on evaluating nursing documentation and focused on research designs and methods, which were not limited to record audit. The review provided insights into several audit instruments and issues relating to documentation quality, but quality measures were not fully addressed. Other reviews on nursing documentation have had different focuses (Mu ller-Staub et al. 2006, Oroviogoicoechea et al. 2008, Urquhart et al. 2009, Jefferies et al. 2010). None of them has concentrated on overall measurement standards and outcomes of nursing documentation itself, although segmental relevant information was found. This review attempts to provide such information to ll in the gap.
The review
Aim
To identify and synthesize nursing documentation audit studies. The objectives include: exploring nursing documentation auditing approaches, identifying audit instruments and
1859
N. Wang et al.
their measurement criteria and describing issues with nursing documentation identied by auditing.
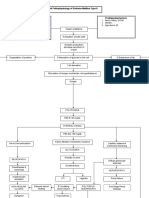
1763 citations identified from electronic search, and screened 219 citations identified from 4 reviews, and screened
Design
A mixed-method systematic literature review was conducted, following the guidelines of the Centre for Reviews and Dissemination (2008).
1797 citations excluded
185 potentially relevant publications retrieved for scrutiny 108 publications excluded
Search methods
A search for relevant publications was mainly undertaken in November and December 2009 on seven electronic databases (CINAHL, the Cochrane Library, Health Reference Center, ProQuest Nursing, Wiley InterScience, Medline 1996 and Nursing Resource Centre). The search terms nursing documentation, nursing records, audit, evaluation and quality, both singly and in combination, were used to identify articles. The search was restricted to articles published in English from 2000 to 2009. However, a new search for update evidence was carried out on August 2010. The following criteria were used in selecting papers: Inclusion criteria Publications of nursing documentation audit studies. Reports on the development or testing of nursing documentation audit instruments. Any type of nursing documentation system, either paperbased, electronic, terminologically standardized, preformatted or structured. Any component of nursing documentation such as nursing assessment forms, care plan and progress notes. Audit studies conducted in any setting: hospital, aged care facility and community etc. Exclusion criteria Papers not dealing with nursing documentation. Review and contextual papers, editorials, letters and case studies. Publications about nursing documentation requirements or guidelines. Papers on issues of nursing documentation other than its quality, e.g. development of documentation systems, factors affecting the quality of documentation and how to complete nursing documentation. Papers on evaluating nursing documentation through surveys and interviews. Papers concerning documentation of health professions other than nursing. Duplicated papers on the same study.
1860
77 publications included
Figure 1 Publication search process.
Search outcome
The titles and abstracts from the primary search were manually screened by the rst author. Reference lists from good quality literature review were also scrutinized for relevant articles. Uncertain papers were checked by the third author to determine their relevance. Seventy-seven papers were nally included in the review following a screening process as shown in Figure 1.
Quality appraisal
As determining the methodological adequacy of studies was not essential for the purpose of the review, a formal quality assessment of review studies was not conducted; however, some consideration was given to prioritizing studies for analysis according to the level of detail given on the audit instruments, and the relevancy and signicance of auditing approaches to nursing practice.
Data abstraction
Extracted data were placed in an Endnote le. These data included study aim, design, study intervention, country of origin, setting, sample size, documentation audit instrument, quality criteria, source of criteria, validation of instrument, approach of evaluation and key ndings of the studies.
Synthesis
Given the purpose of the review, meta-analysis was neither appropriate nor feasible for data synthesis. The papers were grouped by the type of studies. A narrative synthesis of extracted data was undertaken using tables with emerging thematic headings.
2011 Blackwell Publishing Ltd
JAN: REVIEW PAPER
Quality of nursing documentation and audit
Results
Characteristics of studies
The 77 eligible papers consisted of different types of studies carried out in various healthcare settings across 15 countries. The sample sizes ranged from 15 to 13,776 presented as the number of records, number of patients, number of documentation items and number of patient visits. Nursing documentation was audited for different purposes. These were either explicitly or indirectly stated by the authors primarily to address the quality of description of care or the quality of described care. Summarized information on the studies is shown in Table 1. Detailed information is displayed in Tables S1S3.
Different auditing approaches were identied in the study instruments. These approaches were classied into three thematic categories, which reected natural dimensions of nursing documentation: structure and format, process and content. In 47 studies, a single approach was used, while a mixture of approaches was applied in the other. Detailed quality criteria are presented in Table 2. Different types of auditing approaches are displayed in Table 3.
Approach concerning documentation format and structure
The approach concerning the format or structure dealt with constructiveormaterialfeaturesratherthanthemessageofdata. Itfocusedondatasphysicalpresentationssuchasthequantityof records, completeness, legibility, readability, redundancy and the use of abbreviations. Twenty studies applied this approach.
Approaches to nursing documentation audit
Nursing documentation was assessed by quantitative and qualitative content analysis methods, mostly with one or more formally dened instruments. Commonly, each nursing record was graded quantitatively using yes/no tick box or 3, 4, 5 and/or 6 point Likert scales. A few studies, however, used qualitative content analysis methods such as critical discourse analysis (Karlsen 2007), constant comparative analysis (Laitinen et al. 2010) and a case-by-case approach to draw out themes from nursing records (Hegarty et al. 2005).
Approach concerning documentation process
The process approach focused on procedural issues of capturing patients data such as signature, designation, date, timeliness, regularity of documentation and its accuracy to reality. The accuracy of documentation was measured by the concordance between different notes, or between documentation content and the results of patient assessment (Gunningberg & Ehrenberg 2004, Voyer et al. 2008), nurses self reports (Lamond 2000), interviews with nurses and patients (Ekman & Ehrenberg 2002, Wong 2009) and observation of nurse performance (Marinis et al. 2010). The process approach was used in 23 studies.
Table 1 Summary of included publications (n = 77)
Study type (number of studies) Descriptive studies (45) Analytic studies (25): pre-post intervention test (12), quasi-experimental studies (7), randomized controlled trials (3), cluster-randomized trial (1), prospective (1), stratied and randomized intervention study (1), prospective cohort study (1) Instrument development and testing reports (7) Sweden (27), USA (11), Australia (8), Finland (8), Switzerland (4), Norway (4), UK (3), Germany (2), Canada (2), Iceland (2), Italy (1), Netherlands (2), Ireland (1), Rwanda (1), Denmark (1) Auditing studies: Hospital (51), long-term care (7), primary care (6), community care (4), school health centre (1), mixture of hospital and nursing home (1) Reports of instrument development and testing (7): six instruments were reported in the seven papers and were developed based on hospital settings
Approach concerning nursing documentation content
The content approach focused on the meaning of data about care process. This approach was adopted in nearly all of the studies included, where the content of documentation was reviewed in general or specically in relation to a range of focused care issues. When nursing care or nurses knowledge about care was concerned, the authors made judgments based on an underlying assumption that the information documented in the nursing records was complete and accurately reecting reality. Two quality aspects of documentation content were assessed in this approach: what documentation has recorded and how good it is.
Countries of origin (number of studies)
Study setting (number of studies)
What has documentation recorded?
This approach referred to the comprehensiveness of documentation content. It concerned the presence of data about a
1861
2011 Blackwell Publishing Ltd
N. Wang et al.
Table 2 Quality criteria of nursing documentation
Category Quality criteria of documentation structure and format Quality criteria Completeness, quantity, legibility, appearance, plausibility, patient identication, abbreviations, correction of error, linguistic correctness (objective or factual language and scientic terms), chronological report of events, the colour of the ink, blank spaces and gaps within the text, documentation in a correct section, the phrases of recording, succinct and clear language, avoidance of use of jargon or technical terms Signature, date, timeliness, chronological report of events, designation, regularity, accuracy in comparison with reality and accessibility Presence of specic types of documentation (e.g., nursing history and discharge note), presence of specic variables (e.g., patients background information, cause of admission, address of discharging unit), comprehensiveness of ve phases of nursing process, scope of care (e.g., FHP), presence of information about specic care topics (e.g., teaching and learning of the patient, emotional and physical support of the patient or family, patient preference)
Quality criteria of documentation process Quality criteria of documentation content Comprehensiveness of description of care (or care)
Appropriateness of description of care (or care) s Nursing assessment
Nursing problem/diagnosis Goal Intervention
s s
s s
Evaluation General
Presence of specic assessment variables in relation to the problem according to guideline (e.g. grade, size and location and risk assessment for pressure ulcer), use of specic keywords dened in the system in relation to the problem concerned (e.g., pedagogically related assessment keywords dened in the VIPS model). Adequacy or accuracy of problem statement in accordance with NANDA standardised terminologies (e.g., PES format), the relevance within PES Being clear rather than abstract and vague Presence of particular types of intervention in relation to the nursing problem according to guidelines (e.g., uid intake, turning schedule for pressure ulcer), use of specic keywords dened in the system in relation to the nursing problem (e.g., intervention keyword of health promotion for school nursing programmed in the computer system), presence of NIC interventions Presence of NOC (nursing outcome classication) outcomes Internal relationship with ve steps of nursing process
care process at a general level, without considering its logical connection to a particular care issue or the patients condition. Issues measured included whether documentation contained certain types of data such as nursing history, nursing status (Bjo rvell et al. 2002, Gjevjon & Helles 2010), baseline data and discharge summary (Mbabazi & Cassimjees 2006); whether documented nursing care was sufcient to the scope of care needs dened by the study, such as the Health-Related Quality of Life (HRQOL) models seven dimensions (Davis et al. 2000); and most commonly, whether information about the ve steps of nursing process was adequately documented (Ehrenberg & Birgersson 2003, Bjo rvell et al. 2002, Mahler et al. 2007, Thoroddsen et al. 2010, Hayrinen et al. 2010).
(Gunningberg et al. 2009) or postoperative pain (Idvall & Ehrenberg 2002). Documentation content about each step of the nursing process was measured through seeking data specically related to the concerned clinical issue: could be particular keywords preformatted in a standardized documentation system (Bergh et al. 2007), variables of clinical policies or guidelines (Considine & Potter 2006, Junttila et al. 2010, Gartlan et al. 2010) or standardized terminologies (Lunney 2006, Hayrinen et al. 2010). The structure and format of the diagnostic statement (PES format: problem, aetiologies and signs and symptoms) and the internal linkage between the ve phases of the nursing process (Florin et al. 2005, Mu ller-Staub et al. 2009, Paans et al. 2010b) were also covered by this approach.
How good is nursing documentation content?
This approach addressed the appropriateness of nursing documentation or documented care at a level specic to a particular clinical care issue such as pressure ulcers
1862
Nursing documentation audit instruments
The majority of papers described the development or use of nursing documentation auditing instruments, which adopted
2011 Blackwell Publishing Ltd
JAN: REVIEW PAPER
Quality of nursing documentation and audit
Table 3 Nursing documentation audit instruments and measurement details
Reference Instrument Audit approaches Content Measurement details
Bergh et al. (2007)
Ehrenberg & Birgersson (2003) Idvall & Ehrenberg (2002)
ESCI* Quantitative and qualitative keywords analysis ESCI* Nominal scale ESCI* Tentative model NANDA* characteristics of acute pain ESCI* Record audit ESCI* EPUAP *
Content
Content
Using ve-point scales to measure the comprehensiveness of documentation of ve steps of nursing process Quantity of documentation of pedagogically related keyword; presentation in thematic form See Bergh et al. (2007) Documentation of specic signs and symptoms related to leg ulcer and their accordance with guidelines See Bergh et al. (2007) Documentation of indicators/categories related to how to conduct postoperative pain management Documentation of pain characteristics
Ehrenberg et al. (2004) Gunningberg & Ehrenberg (2004)
Content
Content and process
Gunningberg (2004) Gunningberg et al. (2009) Gjevjon & Helles (2010)
ESCI* Record audit protocol ESCI* EPUAP* Level one VIPS* categories Modied ESCI*
Content
Content
Content
Gunningberg et al. (2000) Gunningberg et al. (2001) Baath et al. (2007) Fribeg et al. (2006) Bjo rvell et al. (2000)
Audit protocol ESCI* Audit protocol Audit protocol ESCI* Protocol ESCI* Cat-ch-Ing instrument
Content
Content Content Content
See Bergh et al. (2007) Documentation of specic aspects of nursing assessment and nursing interventions for patients with CHF See Bergh et al. (2007) Documentation of patients background data, pressure ulcer grade, size and location, risk assessment and preventive care Comparing results of documentation audit with results of patient assessment See Bergh et al. (2007) Documentation of risk factors, risk assessment, prevention and treatment of pressure ulcer See Bergh et al. (2007) Documentation of patient background data, pressure ulcer grade, size and location, risk assessment and nursing interventions Presence of documentation according to level one categories of VIPS* model such as nursing history, nursing status and dis charge notes An additional scale of 0 to the original ve-point scales of ESCI* instrument concerning the ve steps of nursing process Documentation of strategies for prevention and treatment of pressure ulcers See Bergh et al. (2007) See Gunningberg et al. (2000) See Gunningberg et al. (2000) See Bergh et al. (2007) Documentation of patient teaching; patients need for knowledge and nurses teaching interventions See Bergh et al. (2007) Using four-point scales or yes/no to measure the quantity and quality of documentation of nursing process; the use of VIPS keywords; the presence of date, signatures and clarication of signatures; linguistic correctness and legibility See Bjo rvell et al. (2000) See Bjo rvell et al. (2000) See Bjo rvell et al. (2000)
Structure, process and content
Bjo rvell et al. (2002) Tornvall et al. (2004) Tornvall et al. (2007)
Cat-ch-Ing Instrument Cat-ch-Ing instrument Cat-ch-Ing audit instrument
Structure, process and content Structure, process and content Structure, process and content
2011 Blackwell Publishing Ltd
1863
N. Wang et al.
Table 3 (Continued)
Reference Instrument Audit approaches Structure and content Content Measurement details
Aling (2006)
Tornvall et al. (2009)
Cat-ch-Ing instrument (modied) Cat-ch-Ing instrument (part) Record audit for clinical issues
Darmer et al. (2006) Nilsson & Willman (2000)
Cat-ch-Ing instrument (modied) Cat-ch-ing instrument (part) NoGA instrument* Modied Cat-ch-ing instrument Modied Cat-ch-Ing instrument Quantity of nursing documentation Cat-ch-Ing instrument (part) QOD instrument* The Cat-ch-Ing EPI instrument
Structure, process and content Structure, process and content
Rykkje (2009) Hayrinen et al. (2010)
Structure, process and content Structure, process and content
Florin et al. (2005)
Content
Larson et al. (2004)
Process and content
Mu ller-Staub et al. (2009) Mu ller-Staub et al. (2008a) Mu ller-Staub et al. (2007) Mu ller-Staub et al. (2008b) Altken et al. (2006)
Q-DIO instrument*
Content
Q-DIO instrument* Q-DIO instrument* Q-DIO instrument (part) * 3-part medication audit instrument Checklist
Content Content Content Content
Questions related to discharge note, signing and using VIPS keywords were removed. Language, grammar and abbreviations were concerned. Maximum of 57 points instead of 80 Audit of date, signatures; clarication of signatures and legibility were excluded Documentation of important clinical nursing issues with regard to aspects in relation to leg ulcer such as health history, knowledge/ development, breathing/circulation, nutrition, wound status, rel evant interventions and evaluation The item of nursing discharge note in the Cat-ch-Ing instrument was excluded; the measurement of nursing diagnosis item was simplied The rst part of the instrument (preliminary?) Item concerning clarication of signature was excluded. Details not fully clear Quantity of the ve steps of nursing process Adding two items related to the quantity and quality of nursing transfer note and nursing discharge summary See Bjo rvell et al. (2000). Adding measure of the use of nursing classications (FiCNI and FiCND) and the relationships between classication Frequency of the nursing diagnoses, aims for care, nursing interventions and nursing outcomes Only the quantity and quality variables of nursing diagnosis were used Structure and format of diagnostic statement and the relevance in PES Using four-point scale to measure the quantity and quality of documentation in discharge note concerning given care, continued nursing needs, planned care, and general data including signature and data Using 3- and 5-point scales to measure the quality of documented nursing diagnosis (as process and product), interventions, out comes and their internal relationships See Mu ller-Staub et al. (2009) See Mu ller-Staub et al. (2009) See Mu ller-Staub et al. (2009). The category nursing diagnosis as process was excluded Documentation of patients demographic information, medications and detailed data about nurses medication management including assessment, planning care, medication administration and evaluation of outcomes Objective quality measurements (e.g. number of stated nursing aims, completeness) and subjective quality measurements (e.g. legibility, plausibility, overall quality judgment) Documentation of admission assessment about patients home bowel care management and preferences for care Documentation of nineteen parameters of initial nursing assessment, historical variables and primary survey assessment Documentation of health status in accordance with seven dimensions of the model
Ammenwerth et al. (2001) Cadd et al. (2000) Considine & Potter (2006) Davis et al. (2000)
Structure and content Content Content Content
Proforma Standardized audit tool HRQOL* model
1864
2011 Blackwell Publishing Ltd
JAN: REVIEW PAPER
Quality of nursing documentation and audit
Table 3 (Continued)
Reference Instrument Audit approaches Content Structure Content Measurement details
Dalton et al. (2001) Daly et al. (2002) Delaney et al. (2000) Dochterman et al. (2005) Ehrenberg & Ehnfors (2001)
Audit instrument Standardized instruments An auditing tool
Documentation of items about pain assessment and management: e.g. pain history, type and intensity, and follow up evaluation Quantity of nursing diagnosis and nursing interventions Presence of data in accordance with items listed in the instrument including NANDA diagnostic label, dening characteristics and related factors of impaired physical mobility Amount and patterns of NIC* interventions used for patients with heart failure, hip fracture procedure and risk of falls Documentation with regard to the topics such as patients problems relating to urinary incontinence, mental condition, mobility, nutritional intake, skin condition and uid intake Concordance between audit results and the results of interviews with residents and nurses concerning the same topics Patient demographic data, diagnosis, co-morbidities, type of operation, information on pain assessment, management and education Formal structure approach (adherence to law and regulations), process comprehensiveness [ESCI-see Bergh et al. (2007)], and knowledge based approaches Nominal scale to measure the frequency of 10 characteristics of fatigue from NANDA*; comparison of audit results with the results of interviews with patients Focusing on wound documentation about assessment of clinical history in relation to the wound and documentation of the physical characteristics of a wound Identication and coding of entries about patient cultural background information; quantity of documented data according to the categories of Sunrise Model Compliance to documentation policy (no detailed information reported), documentation of baseline assessment, episodes of care, patients overall status, ongoing management plan; objective assessment Documentation of the VIPS keywords; presentation in appropriate category in the theoretical framework of palliative care Documentation of patients demographic information, cognitive and behavioural changes, preexisting, conrmed diagnosis of dementia, confusion on admission, cause of confusion and behavioural descriptors and nurses use of formal cognitive assessment tools Amount of care plan, daily notes and steps of nursing process, the nature of interventions, the language used for documentation, clarity of documentation, amount of documented triggered RAPs and accordance of documented items in care plans to triggered RAPs, etc Quantity, format and accuracy of the documentation of nursing diagnoses, nursing care aims, nursing interventions (planned/ performed) and nursing outcomes Documentation of comprehensive nursing assessment, appropriate nursing interventions and the outcomes of the interventions for patients with end-of-life care; case-by-case approach to draw out themes within the categories
NIC* (250/514) interventions Record audit protocol
Content Content and process
Eid & Bucknall (2008) Ehrenberg et al. (2001) Ekman & Ehrenberg (2002) Gartlan et al. (2010) Gebru et al. (2007)
PDAT*
Content
Approaches derived from a literature review FIS*
Structure, process and content Process and content Content
A paper-based audit tool Qualitative content analysis Leiningers Sunrise Model Documentation audit tool
Content
Gregory et al. (2008)
Content (structure and process?)
Gunhardsson et al. (2007) Hare et al. (2008)
Qualitative and quantitative content analysis Tickbox list
Content
Content
Hansebo & Kihlgren Quantitative content (2004) analyses RAPs* Intervention guidelines Hayrinen & Saranto (2009) Narrative content analysis
Structure and content
Content
Hegarty et al. (2005) Quantitative and qualitative data analysis
Content
2011 Blackwell Publishing Ltd
1865
N. Wang et al.
Table 3 (Continued)
Reference Instrument Audit approaches Structure and content Measurement details
Helleso (2006)
TWEEAM instrument* Language functions of Svennevigs typologies
Irving et al. (2006)
A Focucauldian approach to discourse analysis List of nursing diagnoses in the PNDS Categorization table
Structure and content
Junttila et al. (2010)
Content
Using a three-point scale to measure the completeness of items in the discharge notes in accordance with six sections of the instrument; the completeness of 12 keywords in the section of Patients Current Status; data of discharge notes Three language functions (expression, interpersonal and referential) Qualitative analysis; medical, nursing and informal; types, content/message, and terminologies of documentation of assessment, the tone of nurses expression and its implications, nursing models underlying nursing documentation Prevalence of nursing diagnoses listed in the PNDS by perioperative phases Documentation of planning, implementation and evaluation of perioperative care and additional information with subcategories such as physical and psychological safety and asepsis in perioperative care The nurses language expression in assessing patients needs, formulating goals and making a care plan, diagnostic systems and documentation parlance Four-point scale to measure the documentation according to categories such as patient analysis and its recording, patient teaching and learning, evaluation of the nursing care, prevention of complications and errors See Karkkainen & Eriksson (2003) Documentation of BMI calculation, an obesity diagnosis, and inclusion of heights and current weights Documentation of comprehensiveness variables concerning patient assessment; concordance of information between the patient notes and the nurse shift report Documentation of NANDA diagnoses, diagnoses relating to health promotion, NIC* interventions and NOC* outcomes Documentation of VIPS keywords covering 10 key areas of leg ulcer care and treatment Concepts obtained through a series of qualitative data analysis steps were organized into four components of the paradigm model: conditions, interaction, emotions and consequences Documentation of nurse assessments of patient outcomes (NASSESS), achievement of patient outcomes (NGOAL), nursing interventions done (NQUAL) and routine assessment (e.g. vital signs) Quantity and quality aspects of description of the course of care, participation of the patient in care planning, formal aspects of data entry, plausibility and value-free documentation Consistency between recorded and observed nursing assessment activities and interventions Documentation of baseline data, diagnosis, treatments, evaluations and discharge summary; regularity of vital sign measurement, use of scientic terms and chronological report of events
Junttila et al. (2000)
Content
Karlsen (2007)
Critical discourse analysis Lukanders Nursing Audit instrument
Structure and content Content
Karkkainen & Eriksson (2003)
Karkkainen & Eriksson (2005) Lemay et al. (2004) Lamond (2000)
Lukanders Nursing Audit instrument Abstraction tool
Content Content
Coding scheme of MSA* NNN* Checklist Strauss and Corbins paradigm model NCPDCI*
Content and process Content Content Content
Lunney (2006) Lagerin et al. (2007) Laitinen et al. (2010) Larrabee et al. (2001)
Structure and content
Mahler et al. (2007) Marinis et al. (2010) Mbabazi & Cassimjee (2006)
Quantitative and qualitative checklist Checklists 3-section quality measurement checklist
Structure, process and content Content and process Structure, process and content
1866
2011 Blackwell Publishing Ltd
JAN: REVIEW PAPER
Quality of nursing documentation and audit
Table 3 (Continued)
Reference Instrument Audit approaches Structure, process and content Structure, process and content Measurement details
Moult et al. (2004) Paans et al. (2010a)
EQIP*
D-Catch instrument
Paans et al. (2010b) Souder & OSullivan (2000) Thoroddsen & Ehnfors (2007) Thoroddsen et al. (2010)
D-Catch instrument Chart Review Form Established protocol
Structure, process and content Content
Using yes/no and a 4-point scale to measure the completeness, appearance, understandability and usefulness of documented information for patients Quantity and quality of nursing documentation such as adequacy of admission information, presence and accuracy of nursing diagnosis, interventions and outcome evaluations, logical relationship in notes, linguistic correctness of documentation, timeliness and date See Paans et al. (2010a) Documentation of impaired cognitive status Patient assessment using several brief screening measures of cognitive status Agreement of different measures was addressed Presence of different types of documentation, FHP assessment items, nursing diagnosis, PES format, expected outcomes, nursing interventions; internal linkages between steps of nursing process Presence of information according to demographics and 41 items reecting nursing assessment, nursing diagnosis, signs and symptoms, aetiologies, care plan (goal and nursing interventions) and progress notes Accuracy of the documentation of delirium symptoms, namely the sensitivity and specicity of the nursing notes, in comparison with results of patient assessment by using CAM Documentation in accordance to criteria under seven sections such as planning nursing care, meeting the patients needs, care of terminally ill patient and evaluating nursing care objectives Documentation of the postfall evaluation processes that consists of three concepts: diagnosis, management and monitoring stages of falls management guideline Concerning issues with documentation including essential components of documentation and physical presentation of documented data such as chronological order, date, time, designation, illegal alteration of error, abbreviations and meaningless phrases Documentation of specic patient assessment and care data, timeliness, clarity, documenting in a chronological order, appropriate abbreviations and terminologies Comparing the patient care summary with the results of patients bedside assessment and interviews with nurses of provided care Using 3-points scale to measure the documentation in accordance with categories such as Level of Response (command and/or interaction recall and visual stimuli) and Motor (location and description of movement)
An instrument
Content
A structured data collection tool
Content
Voyer et al. (2008) Voutilainen et al. (2004) Wagner et al. (2008) Whyte (2005)
Chart review using a series of measures The Senior Monitor instrument FMAT*
Content and process Content
Content
Audit tool
Structure, process and content
Wong (2009)
Chart audit form
Structure, process and content
Wulf (2000)
Audit form and score sheet
Content
CAM, Confusion Assessment Method; CHF, Chronic Heart Failure; EPUAP, The European Pressure Ulcer Assessment Advisory Panel data collection form; EQIP, The Ensuring Quality Information for Patient; ESCI, Ehnfors & Smedbys comprehensiveness in recording instrument; FHP, Functional Health Patterns; FIS, Fatigue Interview Schedule; FiCND, the Finnish Classication of Nursing Interventions (FiCNI); FiCNI, the Finnish Classication of Nursing Diagnoses; FMAT, The Falls Management Audit Tool; MSA, multidimensional scalogram analysis; NCPDCI, The Nursing Care Plan Data Collection Instrument; Q-DIO, Quality of Diagnosis, Intervention and Outcomes; NANDA, North America Nursing Diagnosis Association; NIC, Nursing Intervention Classication; NOC, Nursing Outcome Classication; NNN, NANDA Diagnosis, NIC and NOC; NoGA, not reported, PDAT, The Pain Documentation Audit tool; PES, problem, aetiologies and signs and symptoms; PNDS, Perioperative Nursing Data Set; QOD, Quality of Nursing Diagnosis Instrument; RAPs, Resident Assessment Protocols; TWEEAM, not reported; VIPS, an acronym formed from the Swedish words for wellbeing, integrity, prevention and security.
2011 Blackwell Publishing Ltd
1867
N. Wang et al.
part or all of the audit approaches described above. It was common that more than one instrument was used in a study. On the other hand, some instruments such as Ehnfors instrument (Bergh et al. 2007), the Cat-ch-Ing instrument (Bjo rvell et al. 2000) and the Q-DIO instrument (Mu llerStaub et al. 2009) were used in a range of studies. Details about the instruments are summarized in Table 3.
Validation of instruments
Most of the studies reported the criteria generation for the development of the instruments. Development was based primarily on the nursing process model, previous audit instruments, relevant local law and regulations, organizational policies and practice guidelines/protocols/models, focus group interviews with clinical experts, literature review, theoretical frameworks, existing documentation forms and standardized terminologies. The psychometric properties of the instruments were reported with different levels of details in 54 of 77 publications (70%). The general results were as follows. Content validity: in nine studies, content validity of the instruments was formally established (CVI > 080) with a group of experts using a consensus model and focus group approach (Mu ller-Staub et al. 2009). The number of experts ranged from 3 to 20. Face validity: three studies measured face validity by having experts review the instruments and judge their accuracy (Lamond 2000, Eid & Bucknall 2008, Mu ller-Staub et al. 2009). Construct validity: In a study by Paans et al. (2010a), construct validity was assessed on 245 records by explorative factor analysis with principal components and varimax rotation. In Lamonds (2000) study, it was assessed by comparing information obtained in the study with measures identied from previous research to see the correspondence between their varieties of classication schemes. In the study by Larson et al. (2004), factor analysis was performed by 20 auditors on 180 records using principal component analysis for extraction and the varimax orthogonal rotation of the instrument items to determine the interdependencies between observed variables. External validity: in the study by Gjevjon and Helles (2010), external validity was strengthened through the auditor acquiring in-depth knowledge from reading, practising and testing the procedures before initiating the actual study. Criterion-related validity: three instruments were tested for their criterion-related validity using a second instrument having similar objectives to the one being tested to audit a
1868
proportion of sampled records (Bjo rvell et al. 2000, Moult et al. 2004, Tornvall et al. 2004). Internal consistency: ten publications reported the estimation of internal consistency of the instruments. The resulting Cronbachs Alpha were acceptable as mostly above 070. Inter-rater reliability: forty studies reported the inter-rater reliability of the instruments. This was evaluated through involving two to eight persons to audit the same records independently. One study reported that the inter-rater reliability of the instrument was ensured by using the same researchers (Considine & Potter 2006). The number of records for estimation ranged from 4 to 310. About 10% of total sample was used in eight studies. Inter-rater agreements ranged from 40% to 100%, most were more than 80%. Cohens kappa values were estimated from 037 to 10 with the majority more than 07. In three studies, the inter-rater reliability was estimated by calculating the Spearmans rank correlation coefcient and the values were 078 (P < 0001) in the study by Tornvall et al.s (2009) and 090098 in the study by Larson et al. (2004). Two studies have reported the use of a coding book or user manual and training for the auditors, which might help establish interrater reliability (Junttila et al. 2010, Thoroddsen et al. 2010). Intra-rater reliability was reported in ve studies with varying degrees of agreement, from fair to very good (Larson et al. 2004, Helleso 2006, Mu ller-Staub et al. 2007, 2008a, Wagner et al. 2008). Usability: the usability of the instrument was tested in a the study of Bjo rvell et al. (2000) by three nurses auditing ve records in terms of understanding questions and the phrasing of the instrument. The instrument was revised after this process. In the study of Moult et al. (2004), the instrument was read by parents, volunteers and clinicians to test its usability.
Summary of study ndings
The results of the nursing documentation audit are summarized in two themes: issues of nursing documentation and study interventions and their effects on nursing documentation.
Issues of nursing documentation
This review reveals many shortcomings in nursing documentation. One of the major issues was the lack of documentation concerning a series of nursing care topics. Many studies showed the predominance of documentation of a biomedical nature and insufcient recording of psychological, social, cultural and spiritual aspects of care (Hegarty et al. 2005,
2011 Blackwell Publishing Ltd
JAN: REVIEW PAPER
Quality of nursing documentation and audit
Altken et al. 2006, Gebru et al. 2007, Gunhardsson et al. 2007, Tornvall et al. 2007). There was also inadequate documentation about assessment of patients preferences and needs for knowledge, previous health behaviour, general health perceptions and quality of life (Cadd et al. 2000, Davis et al. 2000, Laitinen et al. 2010). In addition, patient teaching was rarely evidenced in the records (Karkkainen & Eriksson 2003, Fribeg et al. 2006). A number of studies showed inadequate documentation of the ve steps of the nursing process (Ehrenberg & Birgersson 2003, Bergh et al. 2007, Gjevjon & Helles 2010). In regard to specic care issues, identied deciencies included insufcient documentation of assessment and the rare use of an assessment tool for pain and cognitive impairment (Eid & Bucknall 2008, Hare et al. 2008). Gaps were also found in documentation of assessment, treatment and prevention of pressure ulcers (Gunningberg et al. 2000, Ehrenberg & Birgersson 2003, Baath et al. 2007), assessment of physical characteristics of wound (Gartlan et al. 2010), specic assessment and interventions for older patients with chronic heart failure (Ehrenberg et al. 2004), nursing actions and evaluation for patients in palliative care (Gunhardsson et al. 2007), and assessment of mental ability and interventions to support independent functioning for patients with dementia (Souder & OSullivan 2000, Voutilainen et al. 2004). Additionally, some studies showed a lack of documentation of specic patient data such as vital signs, pupil reaction and mental state, the diagnosis for hospitalization and electrocardiography ECT results. Issues were also found with the use of standardized nursing terminologies. Paans et al. (2010b) found inaccurate documentation of nursing diagnoses and interventions, despite the use of nursing process-based documentation systems. These included lack of PES format with nursing diagnoses, outcome-oriented selection of nursing interventions and incoherence between steps of nursing process. Junttila et al. (2010) identied deciencies in the clinical usability of nursing diagnoses during the intra-operative phase of care. The use of various local diagnostic systems was shown in Karlsens (2007) study. In relation to the structure and process features of nursing documentation, problems included inconsistence in terminologies and timing for documentation (Wong 2009), abstract and unclear recording, inappropriate phrasing of statements (Karlsen 2007); and documenting under a wrong section (Hayrinen & Saranto 2009). Issues identied by Ammenwerth et al. (2001) included incomplete documentation and poor legibility with paper-based documentation and unspecic and too long care plan with electronic records. Importantly, poor concordance between record content and results
2011 Blackwell Publishing Ltd
from patient assessment, interviews with patients and nurses and observations of nurses performance (Lamond 2000, Ehrenberg & Ehnfors 2001, Gunningberg & Ehrenberg 2004, Voyer et al. 2008, Marinis et al. 2010) indicated that data documented in the nursing records were not fully adequate and accurate to reect reality.
Study interventions and their effects on nursing documentation
In 25 analytic studies, various study interventions were implemented and their effects were assessed. These interventions included: electronic health record systems (EHRs) (Ammenwerth et al. 2001, Mahler et al. 2007), standardized documentation systems such as the VIPS model (Darmer et al. 2006), a menu-driven incident reporting system (Wagner et al. 2008), standardized nursing languages (Mu ller-Staub et al. 2007), changing ward organization (Hansebo & Kihlgren 2004), nursing process model (Ehrenberg & Ehnfors 2001), ED nursing documentation standards (Considine & Potter 2006), specic nursing care theories (Karkkainen & Eriksson 2005, Aling 2006), education on specic care issues such as postoperative pain (Dalton et al. 2001) and a mixture of some of these interventions. Nursing documentation could be improved to some extent by the study interventions, as shown in most of the study results, although at times no effect or even some negative effects were reported. The implementation of EHRs integrated with standardized structure and language could improve the completeness of common mandatory elds (Helleso 2006), the comprehensiveness of documentation of the nursing process (Larrabee et al. 2001, Daly et al. 2002, Darmer et al. 2006, Gunningberg et al. 2009), the use of standardized languages (Larrabee et al. 2001) and the recording of specic items about particular patient issues (Gunningberg et al. 2009). Improvement was also noted in the relevance of the message (Helleso 2006, Tornvall et al. 2009) and structure and process features of documentation such as dating, signing, abbreviations and symbols (Rykkje 2009, Mahler et al. 2007). Education and organizational support for documentation of the nursing process and the use of standardized nursing languages (NNN) could improve documentation. This helped nurses understand nursing process theory and improve clinical reasoning skills in conducting systematic nursing assessment, formulating accurate nursing diagnoses, planning concrete and effective nursing interventions and documenting observable nursing outcomes (Nilsson & Willman 2000, Bjo rvell et al. 2002, Florin et al. 2005, Mu ller-Staub et al. 2007, 2008b).
1869
N. Wang et al.
Education was effective in the study by Dalton et al. (2001) about documentation of acute postoperative pain management, but had no obvious effect in Gunningbergs (2004) study about documentation of ulcer prevention. Considine and Potter (2006) showed that a series of written ED standards augmented by an in-service education session could improve initial nursing assessment. Additionally, body mass index tables placed in examination rooms could encourage nurses to document BMI, thus leading to a statistically signicant increase in the diagnosis of obesity (Lemay et al. 2004). In regard to nursing theories, Karkkainen and Eriksson (2005) reported that introducing Erikssons caring theory to the clinical context could improve the recording of the patients experiences and health behaviour. Alings (2006) study showed that introducing ve different nursing theories was associated with the increase in the documentation of nursing history and status upon patients arrival.
Discussion
This review constitutes a cross-sectional survey of nursing documentation audit studies with different designs and study aims. A large number of publications were included. Its strength is that the review provides an overview of current measurement of nursing documentation, from which the denitions, measurement approaches and issues with the quality of nursing documentation can be identied. In addition, the review identies the means by which the quality of nursing documentation could be improved. While conceptually comprehensive, less critical was a limitation of the review. The results of the review were briey presented without describing many details in the original papers. There was no formal appraisal of study quality, so various types of potential bias were not assessed. The review also lacks a critique of nursing documentation audit approaches. The psychometric properties of the audit instruments were generally presented without details about each individual item and without statistical signicance data. This review identies a range of nursing documentation audit instruments. Four instruments were most commonly used in the studies: Ehnfors and Smedbys comprehensiveness-in-recording instrument, the Cat-ch-Ing instrument, the Q-DIO instrument and a protocol including strategies for prevention and treatment of pressure ulcers. The former three were developed in 1993, 2000 and 2007 respectively. They may reect the development of nursing documentation over the past two decades, from the use of a nursing process model to the implementation of standardized nursing documentation systems, then to the application of standardized nursing
1870
terminologies. The latter was a typical instrument for measuring documented care content in relation to a particular clinical issue. In addition, a special instrument was used to measure the quality of information for patients rather than for communication among health professionals (Moult et al. 2004). These instruments, together with other instruments identied, addressed different aspects of nursing documentation quality. They applied various approaches and reected a complete picture of the quality of nursing documentation as perceived by researchers from different countries. The audit approaches mainly addressed three natural dimensions of nursing documentation: structure or format, process and content, which constitute a complete prole of nursing documentation. Quality structure and format of nursing documentation are essential in ensuring that patients data are presented in a friendly way to facilitate nurses or other health professionals easy access to information essential for clinical decision-making. A proper process of data capture is expected as it enables documentation of valid and reliable information about patients and care. The content of nursing documentation should be the central focus of audit because of its implications for nursing care practice. In sum, nursing care should be fully expressed in the content of the nursing documentation, in a quality structure and format and through an appropriate documentation process. The accuracy of documentation content in relation to patients actual conditions and the care given is an important process feature of documentation quality. If there is no assurance of nursing documentation holding valid and reliable data, there would be no value to discuss its quality. The concordance between documentation content and patient assessment or interviews with nurses and patients can reect the accuracy of data. However, this corroboration of evidence from different sources rather than in situ observation is still an indirect method to approve the accuracy of nursing documentation and has potential bias. The content of nursing documentation, which contains evidence about care, is closely associated with nurses professional expertise. Urquhart et al. (2009) stated that nursing documentation had been used to support different philosophies of nursing practice. While the theoretical knowledge and concepts the nurses have of nursing can be embodied in the written text, the evaluation of nursing documentation should have implications for the advancement of nursing profession. The two basic quality elements, comprehensiveness and appropriateness of nursing documentation, dene how well the content of nursing documentation should be for each step of the nursing process. Important information sources included standardized nursing terminologies, clinical policies or guidelines and standardized nursing
2011 Blackwell Publishing Ltd
JAN: REVIEW PAPER
Quality of nursing documentation and audit
What is already known about this topic
Quality nursing documentation facilitates better care through enabling effective communication between nurses and other caregivers. Stages in the development of nursing documentation have included the introduction of the nursing process model to the clinical setting, application of electronic documentation systems and the use of standardized nursing languages. Denitions of nursing documentation quality can differ because of variations in practice across countries and settings.
What this paper adds
The paper is a comprehensive review and presents description of nursing documentation audit instruments that have acceptable psychometric properties. Flaws in nursing documentation include lack of documentation on psychological and social aspects of care; insufcient documentation about the steps of the nursing process and lack of specic data in relation to a particular clinical care issue. Approaches to improving nursing documentation include the use of electronic health records, standardized documentation systems, application of specic nursing theories, education and organizational changes.
that nursing care was not fully expressed in the records, so written communication between different caregivers about patients was inadequate. Furthermore, inaccurate formulation of nursing diagnoses and incoherence in documentation of nursing process (Paans et al. 2010b) have reected the nurses lack of knowledge and skill in clinical reasoning and connecting the reasoning process to nursing process. The structure and process of nursing documentation can be improved by the implementation of standardized electronic nursing documentation systems. Approaches such as the implementation of standardized documentation systems with prestructured keywords, standardized nursing terminologies, nursing theories and nursing practice standards or guidelines were shown to help improve the content of nursing documentation.
Conclusion
Nursing documentation has continuously developed with increasing research on the nursing process. In the reviewed studies, the concept of quality of nursing documentation has been operationally dened by various audit instruments, which have focused on different aspects of documentation quality and revealed variations in practices worldwide. All the audit studies use local standards to evaluate local practice. It may not be practical to seek a universal instrument that ts all study settings because of the use of different nursing documentation systems and terminologies based on the local circumstances. However, the underlying factors causing this and its effects on patient outcomes need to be addressed in further research. Several other areas of documentation would also benet from further research. The causes of documentation aws and their effects on patient outcomes need to be investigated. More attention needs to be paid to the concordance between nursing documentation and care delivery on the oor. This is especially important with increasing application of electronic documentation systems in health care with capacity to increase aggregation and the accuracy of data by a more structured and uniform format of data organization. Examination of causes for inaccuracy of data and factors leading to improvement should shed light for better system designs. There is a need to evaluate the quality of audit instruments from conceptual, theoretical and technical perspectives. Conceptual analysis of measurement standards helps to improve understanding of the denition of quality of nursing documentation and to clarify ambiguous concepts and reach precise operational attributes. Theoretical analysis can help determine whether audit standards are relevant to nursing. Critiques of measurement techniques used in audit instru1871
Implications for practice and/or policy
The quality of nursing documentation has multiple dimensions, which can be evaluated by applying various instruments and inuenced by using technological, educational and organizational interventions. Factors leading to varying practice and aws in documentation quality and their effects on nursing practice and patient outcomes need to be further investigated. Attention needs to be paid to the accuracy of nursing documentation in comparison with reality of practice. documentation systems with preformatted items or keywords. These information sources support nurses in documenting nursing process and in making decisions on care-delivery to the patients. They can also generate quality criteria for the evaluation of documentation content. The shortcomings in nursing documentation included deciencies at different levels of the content. This indicated
2011 Blackwell Publishing Ltd
N. Wang et al.
ments are essential in determining whether instruments are valid and reliable and can produce strong evidence reecting the quality of nursing documentation. Nursing documentation has come a long way but still has deciencies. Further research and more consistent application of established standards will lead to improvements, with associated benets for practice management and patient outcomes.
Funding
This research is a part of a PhD project supported by Australia Research Council (ARC) industry linkage project LP0882430. Five Australian aged-care organizations: Aged and Community Services Australia, Illawarra Retirement Trust, RSL Care, Uniting Care Ageing South Eastern Region and Warrigal care partially funded the project.
Conict of interest
The authors declare that there is no conict of interest.
Author contributions
NW, DH and PY were responsible for the conceptualization and design of the study. NW collected the data, performed the data analysis and drafted the manuscript. PY reviewed the papers included and the data extraction. DH and PY supervised the study and made intellectual input through critical revisions to the manuscript.
Supporting Information Online
Additional Supporting Information may be found in the online version of this article: Table S1. Characteristics of descriptive studies Table S2. Characteristics of analytic studies Table S3. Auditing instrument and measurement details Please note: Wiley-Blackwell are not responsible for the content or functionality of any supporting materials supported by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
Aling M. (2006) Implementation of nursing theory does it have an impact on nursing documentation? Theoria Journal of Nursing Theory 15(3), 3036. Altken R., Manias E. & Dunning T. (2006) Documentation of medication management by graduate nurses in patient
progress notes: away forward for patient safety. Collegian 13(4), 511. Ammenwerth E., Eichstadter R., Haux R., Pohl U., Rebel S. & Ziegler S. (2001) A randomized evaluation of a computer-based nursing documentation system. Methods of Information in Medicine 40, 6168. Baath C., Hall-Lord M.L., Johansson I. & Larsson B.W. (2007) Nursing assessment documentation and care of hip fracture patients skin. Journal of Orthopaedic Nursing 11(1), 414. Bergh A.L., Bergh C.H. & Friberg F. (2007) How do nurses record pedagogical activities? Nurses documentation in patient records in a cardiac rehabilitation unit for patients who have undergone coronary artery bypass surgery. Journal of Clinical Nursing 16, 18981907. Bjo rvell C., Thorell-Ekstrand I. & Wredling R. (2000) Development of an audit instrument for nursing care plans in the patient record. Quality in Health Care 9, 613. Bjo rvell C., Wredling R. & Thorell-Ekstrand I. (2002) Long-term increase in quality of nursing documentation: effects of a comprehensive intervention. Scandinavian Journal of Caring Sciences 16(1), 3442. Cadd A., Keatinge D., Henssen M., OBrien L., Parker D., Rohr U., Schneider J. & Thompson J. (2000) Assessment and documentation of bowel care management in palliative care: incorporating patient preferences into the care regimen. Journal of Clinical Nursing 9, 228235. Centre for Reviews and Dissemination (2008) Systematic Reviews CRDs Guidance for Undertaking Reviews in Health Care. University of York, Heslington. Considine J. & Potter R. (2006) Can written nursing practice standards improve documentation of initial assessment of ED patients? Australasian Emergency Nursing Journal 9, 1118. Dalton J.A., Carlson J., Blau W., Lindley C., Greer S.M. & Youngblood R. (2001) Documentation of pain assessment and treatment: how are we doing? Pain Management Nursing 2(2), 5464. Daly J.M., Buckwalter K. & Maas M. (2002) Written and computerized care plans. Journal of Gerontological Nursing 28(9), 1423. Darmer M.R., Ankersen L., Nielsen B.G., Landberger G., Lippert E. & Egerod I. (2006) Nursing documentation audit the effect of a VIPS implementation programme in Denmark. Journal of Clinical Nursing 15, 525534. Davis A.L., Holman E.J. & Sousa K.H. (2000) Documentation of care outcomes in academic nursing clinic: assessment. Journal of the American Academy of Nurse Practitioner 12(12), 497502. Delaney C., Herr K., Maas M. & Specht J. (2000) Reliability of nursing diagnoses documented in a computerized nursing information system. Nursing Diagnosis 11(3), 121134. Dochterman J., Titler M., Wang J., Reed D., Pettit D., MathewWilson M., Budreau G., Bulechek G., Kraus V. & Kanak M. (2005) Describing use of nursing interventions for three groups of patients. Journal of Nursing Scholarship 37(1), 5766. Ehrenberg A. & Birgersson C. (2003) Nursing documentation of leg ulcers: adherence to clinical guidelines in a Swedish primary health care district. Scandinavian Journal of Caring Sciences 17, 278 284. Ehrenberg A. & Ehnfors M. (2001) The accuracy of patient records in Swedish nursing homes: congruence of record content and
1872
2011 Blackwell Publishing Ltd
JAN: REVIEW PAPER nurses and patients descriptions. Scandinavian Journal of Caring Sciences 15, 303310. Ehrenberg A., Ehnfors M. & Smedby B. (2001) Auditing nursing content in patient records. Scandinavian Journal of Caring Sciences 15, 133141. Ehrenberg A., Ehnfors M. & Ekman I. (2004) Older patients with chronic heart failure within Swedish community health care: a record review of nursing assessments and interventions. Journal of Clinical Nursing 13, 9096. Eid T. & Bucknall T. (2008) Documenting and implementing evidence-based post-operative pain management in older patients with hip fractures. Journal of Orthopaedic Nursing 12(2), 90 98. Ekman I. & Ehrenberg A. (2002) Fatigued elderly patients with chronic heart failure: do patient reports and nurse recordings correspond? International Journal of Nursing Terminologies and Classications 13(4), 127136. Florin J., Ehrenberg A. & Ehnfors M. (2005) Quality of nursing diagnoses: evaluation of an educational intervention. International Journal of Nursing Terminologies and Classications 16(2), 33 43. Fribeg F., Bergh A.L. & Lepp M. (2006) In search of details of patient teaching in nursing documentation an analysis of patient records in a medical ward in Sweden. Journal of Clinical Nursing 15, 15501558. Gartlan J., Smith A., Clennett S., Walshe D., Tomlinson-Smith A., Boas L. & Robinson A. (2010) An audit of the adequacy of acute wound care documentation of surgical inpatients. Journal of Clinical Nursing 19(15-16), 22072214. Gebru K., Ahsberg E. & Willman A. (2007) Nursing and medical documentation on patients cultural background. Journal of Clinical Nursing 16(11), 20562065. Gjevjon E.R. & Helles R. (2010) The quality of home care nurses documentation in new electronic patient records. Journal of Clinical Nursing 19(1-2), 100108. Gogler J., Hullin C., Monaghan V. & Searle C. (2008) The chaos in primary nursing data: good information reduces risk. HIC 2008 Australias Health Informatics Conference ISBN 978 0 9805520 0 3. Gregory L., Millar R., Tasker N. & Tranter S. (2008) Nurse led initiative to improve assessment and documentation. Australian Nursing Journal 10(3), 19. Gunhardsson I., Svensson A. & Bertero C. (2007) Documentation in palliative care: nursing documentation in a palliative care unita pilot study. The American Journal of Hospice & Palliative Care 25(1), 4551. Gunningberg L. (2004) Pressure ulcer prevention: evaluation of an education programme for Swedish nurses. Journal of Wound Care 13(3), 8589. Gunningberg L., Lindholm C., Carlsson M. & Sjoden P.O. (2000) The development of pressure ulcers in patients with hip fractures: inadequate nursing documentation is still a problem. Journal of Advanced Nursing 31(5), 11551164. Gunningberg L., Lindholm C., Carlsson M. & Sjoden P.O. (2001) Risk, prevention and treatment of pressure ulcers nursing staff knowledge and documentation. Scandinavian Journal of Caring Sciences 15, 257263. Gunningberg L. & Ehrenberg A. (2004) Accuracy and quality in the nursing documentation of pressure ulcers: a comparison of record
Quality of nursing documentation and audit content and patient examination. Journal of Wound, Ostomy, and Continence Nursing 31(6), 328335. Gunningberg L., Fogelberg-Dahm M. & Ehrenberg A. (2009) Improved quality and comprehensiveness in nursing documentation of pressure ulcers after implementing an electronic health record in hospital care. Journal of Clinical Nursing 18, 1557 1564. Hansebo G. & Kihlgren M. (2004) Nursing home care: changes after supervision. Journal of Advanced Nursing 45(3), 269279. Hare M., McGowan S., Wynaden D., Speed G. & Landsborough I. (2008) Nurses descriptions of changes in cognitive function in the acute care setting. Australian Journal of Advanced Nursing 26(1), 2125. Hayrinen K. & Saranto K. (2009) The use of nursing terminology in electronic documentation. Studies in Health Technology & Informatics 146, 342346. Hayrinen K., Lammintakanen J. & Saranto K. (2010) Evaluation of electronic nursing documentation nursing process model and standardized terminologies as keys to visible and transparent nursing. International Journal of Medical Informatics 79, 554564. Hegarty M., Hammond L., Parish K., Glaetzer K., McHugh A. & Grbich C. (2005) Nursing documentation: non-physical dimensions of end-of-life care in acute wards. International Journal of Palliative Nursing 11(12), 632636. Helleso R. (2006) Information handling in the nursing discharge note. Journal of Clinical Nursing 15, 1121. Idvall E. & Ehrenberg A. (2002) Nursing documentation of postoperative pain management. Journal of Clinical Nursing 11, 734742. Irving K., Treacy M., Scott A., Hyde A., Butler M. & MacNeela P. (2006) Discursive practices in the documentation of patient assessments. Journal of Advanced Nursing 53(2), 151159. Jefferies D., Johnson M. & Griffiths R. (2010) A meta-study of the essentials of quality nursing documentation. International Journal of Nursing Practice 16, 112124. Junttila K., Salantera S. & Hupli M. (2000) Perioperative documentation in Finland. Association of Operating Room Nurses 72(5), 862877. Junttila K., Hupli M. & Salantera S. (2010) The use of nursing diagnoses in perioperative documentation. International Journal of Nursing Terminologies and Classications 21(2), 5768. Karkkainen O. & Eriksson K. (2003) Evaluation of patient records as part of developing a nursing care classification. Journal of Clinical Nursing 12, 198205. Karkkainen O. & Eriksson K. (2005) Recording the content of the caring process. Journal of Nursing Management 13, 202208. Karlsen R. (2007) Improving the nursing documentation: professional consciousness-raising in a Northern-Norwegian psychiatric hospital. Journal of Psychiatric and Mental Health Nursing 14, 573577. Lagerin A., Nilsson G. & Trnkvist L. (2007) An educational intervention for district nurses: use of electronic records in leg ulcer management. Journal of Wound Care 16(1), 2932. Laitinen H., Kaunonen M. & Astedt-Kurki P. (2010) Patient-focused nursing documentation expressed by nurses. Journal of Clinical Nursing 19, 489497. Lamond D. (2000) The information content of the nurse change of shift report: a comparative study. Journal of Advanced Nursing 31(4), 794804.
2011 Blackwell Publishing Ltd
1873
N. Wang et al. Larrabee J., Boldreghini B., Elder-Sorrells K., Turner Z.M., Wender R.G., Hart J.M. & Lenzi P.S. (2001) Evaluation of documentation before and after implementation of a nursing information system in an acute care hospital. Computers in Nursing 19(2), 5665. Larson J., Bjo rvell C., Billing E. & Wredling R. (2004) Testing of an audit instrument for the nursing discharge note in the patient record. Scandinavian Journal of Caring Sciences 18, 318324. Lemay C.A., Cashman S.B., Savageau J.A. & Reidy P.A. (2004) Effect of a low-cost intervention on recording body mass index in patients records. Journal of Nursing Scholarship 36(4), 312315. Lunney M. (2006) NANDA diagnoses, NIC interventions, and NOC outcomes used in an electronic health record with elementary school children. The Journal of School Nursing 22(2), 94101. Mahler C., Ammenwerth E., Wagner A., Tautz A., Happek T., Hoppe B. & Eichstadter R. (2007) Effects of a computer-based nursing documentation system on the quality of nursing documentation. Journal of Medical Systems 31, 274282. Marinis M.G.D., Piredda M., Pascarella M.C., Vincenzi B., Spiga F., Tartaglini D., Alvaro R. & Matarese M. (2010) If it is not recorded, it has not been done!? consistency between nursing records and observed nursing care in an Italian hospital. Journal of Clinical Nursing 19(11-12), 15441552. Mbabazi P. & Cassimjee R. (2006) The quality of nursing documentation in a hospital in Rwanda. Africa Journal of Nursing & Midwifery 8(1), 3142. Moult B., Franck L. & Brady H.S. (2004) Ensuring quality information for patients: development and preliminary validation of a new instrument to improve the quality of written health care information. Health Expectation 7, 165175. Mu ller-Staub M., Lavin M.A., Needham I. & van Achterberg T. (2006) Nursing diagnoses, intervention and outcomes application and impact on nursing practice: systematic review. Journal of Advanced Nursing 56(5), 514531. Mu ller-Staub M., Needham I., Odenbreit M., Lavin M.A. & van Achterberg T. (2007) Improved quality of nursing documentation: results of a nursing diagnoses, interventions, and outcomes implementation study. International Journal of Nursing Terminologies and Classications 18(1), 517. Mu ller-Staub M., Lunney M., Lavin M.A., Needham I., Odenbreit M. & van Achterberg T. (2008a) Testing the Q-DIO as an instrument to measure the documented quality of nursing diagnoses, interventions, and outcomes. International Journal of Nursing Terminologies and Classications 19(1), 2027. Mu ller-Staub M., Needham I., Odenbreit M., Lavin M.A. & van Achterberg T. (2008b) Implementing nursing diagnostics effectively: cluster randomized trial. Journal of Advanced Nursing 63(3), 291301. Mu ller-Staub M., Lunney M., Odenbreit M., Needham I., Lavin A. & van Achterberg T. (2009) Development of an instrument to measure the quality of documented nursing diagnoses, interventions and outcomes: the Q-DIO. Journal of Clinical Nursing 18, 10271037. Nilsson U.B. & Willman A. (2000) Evaluation of nursing documentation. Scandinavian Journal of Caring Sciences 14(3), 199206. Oroviogoicoechea C., Elliott B. & Watson S. (2008) Review: evaluating information systems in nursing. Journal of Clinical Nursing 17, 567575. Paans W., Sermeus W., Nieweg R.M.B. & Van Der Schans C.P. (2010a) D-Catch instrument: development and psychometric testing of a measurement instrument for nursing documentation in hospitals. Journal of Advanced Nursing 66(6), 13881400. Paans W., Sermeus W., Nieweg R.M.B. & Van Der Schans C.P. (2010b) Prevalence of accurate nursing documentation in patient records. Journal of Advanced Nursing 66(11), 24812489. Rykkje L. (2009) Implementing electronic patient record and VIPS in medical hospital wards: evaluating change in quantity and quality of nursing documentation by using the audit instrument cat-ch-Ing. Nursing Science & Research in Nordic Countries 29(2), 913. Saranto K. & Kinnunen U.M. (2009) Evaluating nursing documentation research designs and methods: systematic review. Journal of Advanced Nursing 65(3), 464476. Souder E. & OSullivan P.S. (2000) Nursing documentation versus standardized assessment of cognitive status in hospitalized medical patients. Applied Nursing Research 13(1), 2936. Thoroddsen A. & Ehnfors M. (2007) Putting policy into practice: pre- and posttests of implementing standardized languages for nursing documentation. Journal of Clinical Nursing 16, 1826 1838. Thoroddsen A., Ehnfors M. & Ehrenberg A. (2010) Nursing specialty knowledge as expressed by standardized nursing languages. International Journal of Nursing Terminologies and Classications 21(2), 6979. Tornvall E., Wilhelmsson S. & Wahren L.K. (2004) Electronic nursing documentation in primary health care. Scandinavian Journal of Caring Sciences 18, 310317. Tornvall E., Wahren L.K. & Wilhelmsson S. (2007) Impact of primary care management on nursing documentation. Journal of Nursing Management 15, 634642. Tornvall E., Wahren L.K. & Wilhelmsson S. (2009) Advancing nursing documentation an intervention study using patients with leg ulcer as an example. International Journal of Medical Informatics 78, 605617. Urquhart C., Currell R., Grant M.J. & Hardiker N.R. (2009) Nursing record systems: effects on nursing practice and healthcare outcomes. Cochrane Database of Systematic Reviews (1), 166. Voutilainen P., Isola A. & Muurinen S. (2004) Nursing documentation in nursing homes state-of-the-art and implications for quality improvement. Scandinavian Journal of Caring Sciences 18, 7281. Voyer P., Cole M.G., McCusker J., St-Jacques S. & Laplante J. (2008) Accuracy of nurse documentation of delirium symptoms in medical charts. International Journal of Nursing Practice 14, 165 177. Wagner L.M., Capezuti E., Clark P.C., Parmelee P.A. & Ouslander J.G. (2008) Use of a falls incident reporting system to improve care process documentation in nursing homes. Quality & Safety in Health Care 17, 104108. Whyte M. (2005) Computerised versus handwritten records. Paediatric Nursing 17(7), 1518. Wong F.W.H. (2009) Chart audit. Journal for Nurses in Staff Development 25(2), E1E6. Wulf J.A. (2000) Evaluation of seizure observation and documentation. Journal of Neuroscience Nursing 32(1), 2736.
1874
2011 Blackwell Publishing Ltd
JAN: REVIEW PAPER
Quality of nursing documentation and audit
The Journal of Advanced Nursing (JAN) is an international, peer-reviewed, scientic journal. JAN contributes to the advancement of evidence-based nursing, midwifery and health care by disseminating high quality research and scholarship of contemporary relevance and with potential to advance knowledge for practice, education, management or policy. JAN publishes research reviews, original research reports and methodological and theoretical papers. For further information, please visit JAN on the Wiley Online Library website: www.wileyonlinelibrary.com/journal/jan Reasons to publish your work in JAN: High-impact forum: the worlds most cited nursing journal and with an Impact Factor of 1540 ranked 9th of 85 in the 2010 Thomson Reuters Journal Citation Report (Social Science Nursing). JAN has been in the top ten every year for a decade. Most read nursing journal in the world: over 3 million articles downloaded online per year and accessible in over 10,000 libraries worldwide (including over 6,000 in developing countries with free or low cost access). Fast and easy online submission: online submission at http://mc.manuscriptcentral.com/jan. Positive publishing experience: rapid double-blind peer review with constructive feedback. Early View: rapid online publication (with doi for referencing) for accepted articles in nal form, and fully citable. Faster print publication than most competitor journals: as quickly as four months after acceptance, rarely longer than seven months. Online Open: the option to pay to make your article freely and openly accessible to non-subscribers upon publication on Wiley Online Library, as well as the option to deposit the article in your own or your funding agencys preferred archive (e.g. PubMed).
2011 Blackwell Publishing Ltd
1875
This document is a scanned copy of a printed document. No warranty is given about the accuracy of the copy. Users should refer to the original published version of the material.
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Fieldtrip ReportDocumento16 páginasFieldtrip ReportJam RapaconAinda não há avaliações
- DamDocumento3 páginasDamJam RapaconAinda não há avaliações
- Market, Technical & Socio-Economic Feasibility of Horsetail SoapDocumento3 páginasMarket, Technical & Socio-Economic Feasibility of Horsetail SoapJam RapaconAinda não há avaliações
- Hypertension PathophysiologyDocumento1 páginaHypertension PathophysiologyJam RapaconAinda não há avaliações
- Linear Expansion 2dryDocumento3 páginasLinear Expansion 2dryJam RapaconAinda não há avaliações
- PathoPhysiology of Hypertension DiagrampDocumento4 páginasPathoPhysiology of Hypertension DiagrampJam RapaconAinda não há avaliações
- Pathophysiology of Diabetes Mellitus Type 2Documento4 páginasPathophysiology of Diabetes Mellitus Type 2jo_annamae4413100% (3)
- Pathophysiology of Diabetes Mellitus Type 2Documento7 páginasPathophysiology of Diabetes Mellitus Type 2jnrue_aerith96% (28)
- Hypertension PathophysiologyDocumento1 páginaHypertension PathophysiologyJam RapaconAinda não há avaliações
- #BemineagainDocumento472 páginas#BemineagainJam RapaconAinda não há avaliações
- Bronchopneumonia TreatmentDocumento2 páginasBronchopneumonia TreatmentJam RapaconAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Honey Commission InternationalDocumento62 páginasHoney Commission Internationallevsoy672173Ainda não há avaliações
- Консп 1Documento48 páginasКонсп 1VadymAinda não há avaliações
- Imports System - data.SqlClient Imports System - Data Imports System PartialDocumento2 páginasImports System - data.SqlClient Imports System - Data Imports System PartialStuart_Lonnon_1068Ainda não há avaliações
- Embedded Systems - RTOSDocumento23 páginasEmbedded Systems - RTOSCheril MehtaAinda não há avaliações
- Studies On Diffusion Approach of MN Ions Onto Granular Activated CarbonDocumento7 páginasStudies On Diffusion Approach of MN Ions Onto Granular Activated CarbonInternational Journal of Application or Innovation in Engineering & ManagementAinda não há avaliações
- PSPO I Question AnswerDocumento11 páginasPSPO I Question AnswerAurélie ROUEAinda não há avaliações
- PLC 2 Ladder DiagramDocumento53 páginasPLC 2 Ladder DiagramAnkur GuptaAinda não há avaliações
- JEE Test Series ScheduleDocumento4 páginasJEE Test Series ScheduleB.K.Sivaraj rajAinda não há avaliações
- Recording and reporting in hospitals and nursing collegesDocumento48 páginasRecording and reporting in hospitals and nursing collegesRaja100% (2)
- 【小马过河】35 TOEFL iBT Speaking Frequent WordsDocumento10 páginas【小马过河】35 TOEFL iBT Speaking Frequent WordskakiwnAinda não há avaliações
- COS1512 202 - 2015 - 1 - BDocumento33 páginasCOS1512 202 - 2015 - 1 - BLina Slabbert-van Der Walt100% (1)
- CV Raman's Discovery of the Raman EffectDocumento10 páginasCV Raman's Discovery of the Raman EffectjaarthiAinda não há avaliações
- Moment Baseplate DesignDocumento10 páginasMoment Baseplate DesignNeil JonesAinda não há avaliações
- Navid DDLDocumento7 páginasNavid DDLVaibhav KarambeAinda não há avaliações
- Shaft design exercisesDocumento8 páginasShaft design exercisesIvanRosellAgustíAinda não há avaliações
- Navier-Stokes EquationsDocumento395 páginasNavier-Stokes EquationsBouhadjar Meguenni100% (7)
- Career DevelopmentDocumento23 páginasCareer DevelopmentHaris Khan100% (1)
- User Manual: Swift S3Documento97 páginasUser Manual: Swift S3smnguyenAinda não há avaliações
- Paaralan Tungo Sa Magandang Kinabukasan" The Campaign Kicked Off in All The PublicDocumento7 páginasPaaralan Tungo Sa Magandang Kinabukasan" The Campaign Kicked Off in All The PublicJOHN FRANCIS OCTAVIANOAinda não há avaliações
- Radical Candor: Fully Revised and Updated Edition: How To Get What You Want by Saying What You Mean - Kim ScottDocumento5 páginasRadical Candor: Fully Revised and Updated Edition: How To Get What You Want by Saying What You Mean - Kim Scottzafytuwa17% (12)
- Discourse Community 2Documento7 páginasDiscourse Community 2api-272763663Ainda não há avaliações
- The History of American School Libraries: Presented By: Jacob Noodwang, Mary Othic and Noelle NightingaleDocumento21 páginasThe History of American School Libraries: Presented By: Jacob Noodwang, Mary Othic and Noelle Nightingaleapi-166902455Ainda não há avaliações
- McKinsey & Co - Nonprofit Board Self-Assessment Tool Short FormDocumento6 páginasMcKinsey & Co - Nonprofit Board Self-Assessment Tool Short Formmoctapka088100% (1)
- BUDDlab Volume2, BUDDcamp 2011: The City of Euphemia, Brescia / ItalyDocumento34 páginasBUDDlab Volume2, BUDDcamp 2011: The City of Euphemia, Brescia / ItalyThe Bartlett Development Planning Unit - UCLAinda não há avaliações
- Space Gass 12 5 Help Manual PDFDocumento841 páginasSpace Gass 12 5 Help Manual PDFNita NabanitaAinda não há avaliações
- 4idealism Realism and Pragmatigsm in EducationDocumento41 páginas4idealism Realism and Pragmatigsm in EducationGaiLe Ann100% (1)
- Tutor Marked Assignment (TMA) SR Secondary 2018 19Documento98 páginasTutor Marked Assignment (TMA) SR Secondary 2018 19kanna2750% (1)
- Windows Server 2016 Editions ComparisonDocumento4 páginasWindows Server 2016 Editions ComparisonmasterredhardAinda não há avaliações
- Lenovo IdeaPad U350 UserGuide V1.0Documento138 páginasLenovo IdeaPad U350 UserGuide V1.0Marc BengtssonAinda não há avaliações
- Failure Reporting, Analysis, and Corrective Action SystemDocumento46 páginasFailure Reporting, Analysis, and Corrective Action Systemjwpaprk1100% (1)