Escolar Documentos
Profissional Documentos
Cultura Documentos
Laboratory Data (1) L
Enviado por
Aziza HasanTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Laboratory Data (1) L
Enviado por
Aziza HasanDireitos autorais:
Formatos disponíveis
CLINICAL PHARMACY
LABORATORY DATA
The most frequently used laboratory tests are complete blood count, electrolytes, blood chemistries and urinalysis. Normal values may vary from lab to lab depending on techniques and reagents used. Normal values may also vary depending on patients age, gender, weight, height and other factors. Laboratory error is an uncommon error however it can happen. The following are some potential causes of laboratory error: Technical Error. Spoiled Specimen. Specimen Taken At Wrong Time. Incomplete Specimen. Faculty Reagents. Diet; e.g. red meat consumption may cause a false positive hem-occult stool test. Medications; e.g. iron supplements may cause a false positive hem-occult tool test. If laboratory error is suspected the test should be repeated. Important laboratory tests include the following:
Hematology Urinalysis Electrolytes and blood chemistry Cardiac diagnostic tests Lipoprotein panel Endocrine diagnostic tests o Thyroid function tests o Diabetes mellitus o Adrenal gland tests Gastrointestinal/hepatic/pancreatic diagnostic tests Coagulation tests Immunologic diagnostic tests Infectious disease diagnostic tests Hepatitis a Hepatitis b Hepatitis c
CLINICAL PHARMACY
HEMATOLOGY
The complete blood count (CBC) is an extremely common laboratory test that provides values for the following Hemoglobin. Hematocrit. Red Blood Cells. Mean Corpuscular Cell Volume. Mean Corpuscular Cell Hemoglobin. Mean Corpuscular Hemoglobin Concentration. Reticulocytes. White Blood Cells. Neutrophils. Lymphocytes. Monocytes. Eosinophils. Basophils. Platelets.
CLINICAL PHARMACY
1. HEMOGLOBIN: (Hb)
Hemoglobin is the oxygen carrying compound found in the RBCs. Hemoglobin level is a direct indicator of the oxygen carrying capacity of the blood. Adaptation to high altitudes, extreme exercise and pulmonary conditions may causes variations in hemoglobin values.
International Units 14 18 g/dl
SI Units 8.7 11.2 mmol/L 7.4 9.9 mmol/L
Increased Value
Decreased Value
Male
Female 12 16 g/dl
Hemoglobin values may be increased in diseases such as Polycythemia Vera and Chronic Obstructive Lung Disease. Hemoglobin may also be increased in chronic smokers and individuals who engage vigorous exercise or live at high altitudes.
Hemoglobin is decreased in anemia of all types, particularly Iron Deficiency Anemia. Hemoglobin is also reduced with Blood loss, Hemolysis, pregnancy, fluid replacement or increased fluid intake.
2. HEMATOCRIT: (Hct)
The Hematocrit value describes the volume of blood that is occupied by RBCs. It is expressed as a percentage of total blood volume. Another name for hematocrit is packed cell volume. The value of hematocrit is generally about three times the value of hemoglobin.
International Units 42 52%
SI Units 0.42 0. 0.37 0.47 52
Increased Value
Decreased Value
Male
Female 37 47%
Increases in hematocrit value are associated with Polycythemia Vera, chronic obstructive lung disease and individuals who live at high altitudes. Increased hematocrit may also be seen in cases of dehydration and shock.
Hemtocrit is decreased in anemia of all types. Hematocrit is also reduced with blood loss, hemolysis, pregnancy, cirrhosis, hyperthyroidism and leukemia.
CLINICAL PHARMACY
3. RED BLOOD CELLS: (RBCs)
RBCs are produced in the bone marrow. They are released into the systemic circulation and serve to transport oxygen from the lungs to the body tissues. After circulating for a life span of 120 days the RBCs are cleared by the Reticulo-endothelial system.
International Units Male 4.3 5.9 x 106 cells/mm3 Female 3.5 5.5 x 106 cells/mm3
SI Units 4.3 5.9 x 1012 cells/L 3.5 5.5 x 1012 cells/L
Increased Value Increased RBCs counts are associated with Polycythemia Vera, high altitude and strenuous exercise.
Decreased Value
Red blood cell counts are decreased in various types of anemias.
4. MEAN CORPUSCULAR CELL VOLUME: (MCV)
MCV provides an estimate of the average volume of the erythrocyte. Higher the MCV, the larger the average size of the RBCs. Cells with an abnormally large MCV are classified as MACROCYTIC and cells with a low MCV are referred to as MICROCYTIC. NORMOCYTIC RBCs have an MCV that falls within the normal range.
International Units 76 96 um3/cell
SI Units 76 96 fL
Increased Value
Decreased Value
An increase in MCV is associated with folate deficiency, B12 deficiency, alcoholism, chronic liver disease, hyperthyroidism and use of medications such as Valproic Acid, AZT, Stavudine and Antimetabolites.
Decreased MCV may result from iron deficiency anemia, hemolytic anemia, lead poisoning and Thalassemia.
CLINICAL PHARMACY
5. MEAN CORPUSCULAR CELL HEMOGLOBIN: (MCH)
MCH indicates the average weight of hemoglobin in the RBCs. Cells with a low MCH are pale in color and are referred as HYPOCHROMIC. Cells with an increased MCH are HYPERCHROMIC.
International Units 27 33 pg/cell
Increased Value
Decreased Value
Elevated MCH may be caused by folate deficiency. In hyperlipidemia MCH may be falsely elevated because of specimen turbidity.
Decreased MCH is associated with iron deficiency anemia.
6. MEAN CORPUSCULAR CELL HEMOGLOBIN CONCENTRATION: (MCHC)
MCHC is a measure of average hemoglobin concentration concentration in the RBCs.
International Units 32 36 g/dL
SI Units SI 320 360 g/L
Increased Value
Decreased Value
Increased MCHC is associated with hereditary spherocytosis.
MCHC may be decreased in iron deficiency anemia, hemolytic anemia, lead poisoning and thalassemia.
CLINICAL PHARMACY
7. RETICULOCYTES:
Reticulocytes are immature RBCs formed in the bone marrow. An increase in reticulocytes usually indicates an increase in RBCs production but may also be an indicative of a decrease in the circulating number of mature erythrocytes.
International Units 0.5 2 % of RBC
SI Units SI 0.005 0.02 RBC
Increased Value
Decreased Value
Increased reticulocyte counts are associated with hemolytic anemia, hemorrhage and sickle cell disease. Increased reticulocytes are also indicative of response to treatement of Anemias secondary to iron deficiency, B12 deficiency or Folate Deficiency.
Reticulocytes may be decreased as a result of infectious causes, renal disease, toxins, iron deficiency anemia and drug induced bone marrow depression.
8. WHITE BLOOD CELLS : (WBCs)
The WBC count represents the total number of WBCs in a given volume of blood. Mature WBCs exist in many forms including Neutrophils, Lymphocytes, Monocytes, Eosinophils and Basophils.
International Units 3,200 10,000 cells/mm3
SI Units 3.2 10.0 x 109 cells/L
Increased Value
Decreased Value
An increase in WBC count is referred to as LEUKOCYTOSIS. Leukocytosis may be caused by infection, Leukemia, Trauma and Corticosterio use. Emotion, stress and seizures may also increase WBC count.
A decrease in WBC count is referred to as LEUKOPENIA. Decreased WBCs may be seen in Viral infection, Aplastic Anemia and use of Chemotherapy or Anticonvulsants.
CLINICAL PHARMACY
9. NEUTROPHILS:
Neutrophils are the most common type of WBC. Their primary function is to fight bacterial and fungal infections by phagocytizing foreign particles. Neutrophils may also be involved in the pathogenesis of some inflammatory disorders, e.g. Rheumatoid Arthritis and Inflammatory Bowel Disease.
International Units 36 73% 3 5%
SI Units 0.03 0.05 0.36 0.73
Increased Value
Decreased Value
Segs Bands
An increase in circulating neutrophils is called NEUTROPHILIA. Neutrophilia is associated with infection, metabolic disorders (e.g. diabetic ketoacidosis), uremia, response to stress, emotional disturbances, burns, acute inflammation and use of medications such as corticosteroids.
A decrease in the number of circulating neutrophils is called as NEUTROPENIA. Neutropenia may result from viral infections e.g. Momonucleosis, Hepatitis, Septicemia, overwhelming infections and use of chemotherapy agents.
Bands are immature neutrophils. An increase in bands often referred to as a shift to the left during infection or leukemia.
CLINICAL PHARMACY
10. LYMPHOCYTES:
Lymphocytes are the second most common type of circulating WBC. They are important in the immune response to foreign antigens.
International Units 20 40 %
Increased Value
Decreased Value
An elevated lymphocyte count is called LYMPHOCYTOSIS. Lymphocytes may be elevated in Hepatitis, Mononucleosis, Chickenpox, Herpes Simplex, Herpes Zoster and other viral infections. Some bacterial infections e.g. Syphilis, Brucellosis, Leukemia and Multiple Myeloma are also associated with lymphocytosis.
A decreased lymphocyte count is referred to as LYMPHOPENIA. Lymphopenia may result from acute infections, burns, trauma, lupus, HIV and lymphoma.
11. MONOCYTES:
Monocytes are synthesized in the bone marrow released into the circulation and subsequently migrate into lymph nodes, spleen, liver, lungs and bone marrow. In these tissues monocytes mature into macrophages and serve as scavengers for foreign substances.
International Units 28%
Increased Value
Decreased Value
An elevated monocyte count is referred to as MONOCYTOSIS. Monocytosis may be observed in the recovery phase of some infections, Sub Acute Bacterial Endocarditis (SBE), Tuberculosis (TB), Syphilis, Leukemia, Lymphoma, Lupus, Rheumatoid Arthritis and Cirrhosis.
A reduced monocyte count is called MONOCYTOPENIA. Monocytopenia is usually not associated with a specific disease but may be seen with use of bone marrow suppressive agents or severe stress.
CLINICAL PHARMACY
12. EOSINOPHILS:
Eosinophils are phagocytic WBCs that assist in the killing of bacteria and yeast. They are also involved in allergic reactios and in the immune response to parasites.
International Units
Increased Value
04%
An increase in eosinophil count is called as EOSINOPHILIA. It is associated with allergic disorders, allergic drug reactions, collagen vascular disease, parasitic infections and some malignancies.
13. BASOPHILS:
Basophils are phagocytic WBCs present in small numbers in the circulating blood. They contain heparin, histamine and leukotrienes. They are probably associated with hypersensitivity reactions.
International Units 01%
Increased Value
Increased basophils may be seen in hypersensitivity reactions to food or other medications, certain leukemias and ulcerative colitis.
CLINICAL PHARMACY
14. PLATELETS:
Platelets are a critical element in blood clot formation. The risk of bleeding is low unless platelets fall below 20,000 50,000/L.
International units 150,000 400,000 /L
SI units 150 400 x 109/L
Increased value
Decreased value
Increased platelets (thrombocytosis, thrombocythemia) may be caused by infection, malignancies, splenectomy, chronic inflammatory disorders e.g. rhrumatoid arthritis, polycythemia vera, severe stress, surgery or trauma.
Decreased platelet count (thrombocytopenia) may occur in autoimmune disorders such as idiopathic thrombocytopenia purpura (ITP) and also with aplastic anemia, radiation, chemotherapy, space occupying lesion in the bone marrow and heparin or valproic acid. Aspirin and NSAIDs do not affect platelet count but impair the platelet function.
10
CLINICAL PHARMACY
URINALYSIS
Urinalysis (UA) is a useful laboratory test that enables the clinician to identify patients with renal disorders, as well as some non renal disorders. Common elements included in the UA are Appearance. pH. Specific Gravity. Protein. Glucose. Ketones. Blood. Bilirubin. Leukocyte esterase. Nitrites.
11
CLINICAL PHARMACY
1. APPEARANCE:
On visual examination the urine color should range from clear to dark yellow. Some cloudiness is normal and may be caused by phosphates or urates which precipitate as the urine cools to room temperature. Abnormal appearances of urine include the following Red Orange color may be caused by presence of myloglobin (from muscle breakdown, from seizures, cocaine or injuries), hemoglobin, medications (Rifampicin, Phenothiazines, Phenazopyridine, Phenolphthalein), or foods (beets, carrots, blackberries). Blue Green color may result from methylene blue or ingestion of beets. Brown Black color may be associated with presence of myoglobin or porphyrins from porphyria or sickle cell. Foamy urine indicates the presence of protein or bile acids.
2. SPECIFIC GRAVITY:
Specific gravity is an indication of the ability of the kidney to concentrate urine. Unusually low specific gravity would suggest that the kidneys are not able to concentrate urine appropriately.
Normal Range 1.010 1.025
Increased Value
Decreased Value
Increased specific gravity may be associated with dehydration, excretion of radiologic contrast media or SIADH. In addition, increased excretion of glucose or protein greater than 2g per day may also increase urine specific gravity.
Decreased specific gravity may occur in chronic renal failure or diabetes insipidus.
3. pH:
Normal urine specimens are acidic. The normal urine pH is approximately 6.
Normal Range 4.5 8
Clinical Significance
Alkaline urine may be found in certain urinary tract infections e.g. infections caused by urea splitting organisms E. coli, Proteus, Klebsiella, renal tubular acidosis and with the use of acetazolamide or thiazide diuretics.
12
CLINICAL PHARMACY
4. PROTEIN:
Trace protein in the urine is a common clinical finding and often has no clinical significance.
Normal Range 0 (<30 mg/dL) to 1+ (30 100 mg/dL)
Clinical Significance
Repeated positive tests or proteinuria of greater than 150 mg/dL may be a marker of renal disease. Causes of protein in urine include diabetic nephropathy, hypertension, fever, exercise, pyelonephritis, multiple myeloma, lupus and severe CHF.
5. GLUCOSE AND KETONES:
Glucose begins to spill into urine when serum blood glucose is greater than 180.
Normal Range
Clinical Significance
Glucose negative Ketones negative.
Glucose in the urine suggests diabetes mellitus or in a known diabetic suggests the need for improved glucose control. Glucose in the urine may also be associated with Cushings disease, pancreatitis and use of thiazide diuretics, steroids or oral contraceptives. Diabetic ketoacidosis (DKA), starvation, the Atkins diet and alcoholism may produce ketones in the urine.
6. BLOOD:
Blood in the urine ( hematuria ) may indicate urinary tract damage.
Normal Range
Clinical Significance
Negative to Trace.
Common causes of hematuria are infection, nephrolithiasis, malignancies and Benign Prostatic Hypertrophy (BRH). False positive results for blood in the urine may occur when povidone iodine is used as a cleansing agent before urine specimen collection. False negative results may occur in patients taking high doses of vitamin C.
13
CLINICAL PHARMACY
7. BILIRUBIN:
Bilirubin in the urine usually produces a dark yellow or brown color.
Normal Range
Clinical Significance
Zero to Trace.
Bilirubin in the urine may be associated with liver diseases (e.g. hepatitis) or obstructive biliary tract disease. Phenazopyridine or phenothiazines may cause a false positive result for bilirubin in the urine.
8. LEUKOCYTE ESTERASE:
Positive leukocyte esterase provides an indication of WBCs in the urine.
Normal Range
Clinical Significance
Zero to Trace.
Leukocyte esterase in the urine is associated with infections and/or inflammation of the urinary tract.
9. NITRITES:
Gram negative bacteria are capable of converting dietary nitrates to nitrites.
Normal Range
Clinical Significance
Negative.
Presence of nitrites in the urine suggests colonization or infection with gram negative organisms
14
CLINICAL PHARMACY
ELECTROLYTES AND BLOOD CHEMISTRY
It includes the following Sodium. Potassium. Chloride. Carbon Dioxide. Anion Gap. Glucose Blood Urea Nitrogen. Creatinine Calcium. Inorganic Phosphorus. Magnesium Uric acid Osmolarity Total Serum Protein
15
CLINICAL PHARMACY
1. SODIUM: (Na+)
Sodium is the most prevalent cation in the extracellular fluid. Sodium is important in regulating serum osmolarity, fluid balance and acid base balance. In addition sodium also assists in maintaining the electric potential necessary for necessary for transmission of nerve impulses.
International Units 135 147 mEq/L
Increased Value
Decreased Value
Increased sodium (HYPERNATREMIA) may result from increased sodium intake or increased fluid loss. Fluid loss from gastroenteritis, diabetes insipidus, Cushings disease, hyperaldosteronism and administration of hypertonic saline solution are causes of hypernatremia.
Decreased sodium (HYPONATREMIA) may be caused by a decrease in total body sodium but is more commonly attributed to excess accumulation of body water (DILUTIONAL HYPONATREMIA). Common causes of dilutional hyponatremia include CHF, cirrhosis and nephrotic syndrome. Sodium depletion may also be seen in SIADH, cystic fibrosis, mineralocorticoid deficiency or fluid replacement with solutions that do not contain sodium. SIADH may be associated with the use of medications including chlorpropamide, thiazide diuretics and carbamazepine.
16
CLINICAL PHARMACY
2.POTASSIUM: (K+)
Potassium is the main intracellular cation. Potassium plays an important role in many body functions including regulation of nevre excitability and muscle function. Cardic function and neuromuscular function can be significantly affected by either an increase or decrease in potassium levels.
International Units 3.5 5.0 mEq/L
Increased Value
Decreased Value
Causes of increased potassium (HYPERKALEMIA) include metabolic or respiratory acidosis, renal failure, Addisons disease and massive cell damage from burns, injuries and surgery. Medications such as ACE inhibitors, potassium supplements and potassium sparing diuretics are also contributing factors to hyperkalemia.
Causes of decreased potassium (HYPOKALEMIA) include severe diarrhea and/or vomiting, alkalosis, hyperaldosteronism, Cushings disease and use of amphotericin B or thiazide, loop or osmotic diuretics.
3. CHLORIDE:
Chloride primarily serves a passive role in the maintenance of fluid balance and acid base balance. Serum chloride values are useful in identifying fluid or acid base balance disorders.
International Units 95 105 mEq/L
Increased Value
Decreased Value
HYPERCHLOREMIA may be seen in metabolic acidosis, respiratory alkalosis, dehydration and renal disorders.
HYPOCHLOREMIA may be associated with prolonged vomiting, gastric suctioning, metabolic alkalosis, CHF, SIADH and Addisons disease.
17
CLINICAL PHARMACY
4. CARBON DIOXIDE: (CO2)
The majority of CO2 in the plasma is present as bicarbonate ions and small percentage is dissolved CO2. The CO2 content is the sum of both bicarbonate ions and dissolved CO2.
International Units
SI Units 95 105 mmol/L
Increased Value
Decreased Value
22 - 28 mEq/L
Increased CO2 is seen in metabolic alkalosis.
Decreased CO2 is associated with metabolic acidosis and hyperventilation.
5. ANION GAP:
Anion gap is calculated using the following formula: Anion gap = [Na+ - (Cl- + HCO3-)] Anion gap is useful in evaluating causes of metabolic acidosis.
Normal Range 3 11 mEq/L
Clinical Significance
Anion gap may be increased in conditions such as renal failure, lactic acidosis, ketoacidosis and salicylate, methanol or ethylene glycol toxicity.
18
CLINICAL PHARMACY
6. GLUCOSE:
Glucose is an important energy source for most cellular functions. Blood glucose regulation is achieved through a complex set of mechanisms that involves insulin, glucagon, cortisol, epinephrine and other hormone.
International Units 70 110 mg/dL (fasting)
SI Units 3.9 6.1 mmol/L
Increased Value
Decreased Value
The most common cause of increased glucose (HYPERGLYCEMIA) is DIABETES MELITUS. Causes of hyperglycemia include Cushings disease, sepsis, pancreatitis, shock, trauma, myocardial infarction and use of corticosteroids or niacin.
HYPOGLYCEMIA may result from missing a meal, oral hypoglycemic agents, insulin overdose or Addisons disease.
7. BLOOD UREA NITROGEN: (BUN)
Urea nitrogen is an end product of protein catabolism. It is produced in the liver, transported in the blood and cleared by the kidneys. BUN concentration serves as a marker of renal function.
International Units 8 18 mg/dL
SI Units 3.0 6.5 mmol/L
Increased Value
Decreased Value
Increased BUN may be associated with acute or chronic renal failure, CHF, gastrointestinal bleeding, high protein diet, shock, dehydration and nephrotoxic medications.
Decreased BUN is seen in liver failure because of inability of the liver to synthesize urea.
19
CLINICAL PHARMACY
8. CREATININE:
Muscle creatine and phosphocreatine break down to form creatinine. Creatinine is released into the blood and excreated by glomerular filtration in the kidneys. Thus, serum creatinine is used as a tool to identify patients with renal dysfunction.
International Units 0.6 1.3 mg/dL
SI Units 53 115 mol/L
Increased Value
Decreased Value
Increased creatinine is associated wiyh renal dysfunction, dehydration, urinary tract obstruction, increased exercise, hyperthyroidism, myasthenia gravis and use of nephrotoxic drugs such as cisplatin and amphotericin B.
Serum creatinine may be reduced in cachexia, inactive elderly or comatose patients and spinal cord injury patients.
BUN/CREATENINE RATIO:
Calculating the BUN/Creatinine ratio may suggest an etiology for renal dysfunction. A BUN/Creatinine ratio greater than 20 suggests a prerenal cause such as GI bleeding. A BUN/Creatinine ratio between 10 and 20 indicates intrinsic renal dysfunction.
20
CLINICAL PHARMACY
9. CALCIUM: (Ca++)
Majority of calcium in the body is found in the skeletal bones and teeth. The reminder is found in the blood, muscle and other tissues. In addition to playing a role in bone mineralization, Calcium is important in cardiac and skeletal muscle contraction, blood coagulation, enzyme activity and transmission of impulses. In the blood, approximately half of the calcium is in ionized free state and the other half is bound to proteins or complexed with anions. Only calcium in the Free State may be utilized in physiologic functions. Calcium levels are regulated by a complex system that involves the skeleton, kidneys, intestines, parathyroid hormone, vitamin D and serum phosphate.
International Units 8.5 10.5 mg/dL
SI Units 2.1 2.6 mmol/L
Increased Value
Decreased Value
The most common cause of increased calcium (HYPERCALCEMIA) is malignancies and primary hyperparathyroidism. Other causes include Pagets disease, sarcoidosis, vitamin D intoxication, milk alkali syndrome, Addisons disease and use of thiazide diuretics and lithium.
Causes of decreased calcium (HYPOCALCEMIA) include hypoparathyrodism, vitamin D deficiency, hyperphosphatemia, pancreatitis, alkalosis, renal disease and use of loop diuretics.
PSEUDOHYPOCALCEMIA: One half of serum calcium circulates bound to plasma proteins such as albumin. A decreased albumin concentration may lead to a decreased total calcium concentration and calcium levels may appear falsely low in the presence of low albumin. Serum calcium levels may be corrected for low albumin as follows: Corrected Calcium = Reported Serum Calcium + 0.8 (4.0 patients albumin)
21
CLINICAL PHARMACY
10. INORGANIC PHOSPHATES:
Phosphate is an intracellular anion involved in several critical physiologic functions. Phosphate is necessary for formation of the cellular energy source adenosine tri-phosphate (ATP) and the synthesis of phospholipids. Phosphate also plays a role in protein, fat and carbohydrate metabolism as well as acid base balance.
International units 2.6 4.5 mg/dL
SI units 0.84 1.45 mmol/L
Increased value
Decreased value
Increased Phosphate Decreased Phosphate (HYPERPHOSPHATEMIA) (HYPOPHOSPHATEMIA) can result from renal can be associated with dysfunction, increased overuse of aluminium and vitamin D intake, increased calcium containing phosphate intake, antacids, alcoholism, hypoparathyrodism and malnutrition and bone malignancy. respiratory alkalosis.
11. MAGNESIUM: (Mg++)
Magnesium is a necessary cofactor in physiologic functions utilizing ATP. It is also vital in protein and nucleic acid synthesis, as well as neuromuscular function.
International Units 1.7 2.4 mg/dL
SI Units 0.85 1.2 mmol/L
Increased Value
Decreased Value
reased Magnesium (HYPERMAGNESEMIA) may result from renal failure or Addisons disease. In addition, the administration o Mg supplements or Mg containing antacids or laxatives to patients with renal dysfunction may also fesult in hypermagnesemia.
Decreased Magnesium (HYPOMAGNESEMIA) may be associated with diarrhea, vomiting, malabsorption, alcoholism, hyperaldosteronism, pancreatitis and use of diuretics, amphotericin B or cisplastin.
22
CLINICAL PHARMACY
12. URIC ACID:
Uric acid is the main metabolic end product of the purine bases of DNA.
International Units Male 3.6 8.5mg/dL Female 2.3 6.6 mg/dL
SI Units 214 506 mol/L 137 393 mol/L
Increased Value
Decreased Value
Increased uric acid (HYPERURICEMIA) may be caused by excessive production of purines or inability of the kidney to excrete urate. Common causes of hyperuricemia are renal dysfunction, tumor lysis syndrome, high protein diet and use of furosemide, thiazides and niacin. Hyperuricemia may be associated with the development of gouty arthritis, nephrolithiasis and
Decreased uric acid (HYPOURICEMIA) levels usually occur with a low protein diet or use of allopurinol, probenecid or high doses of aspirin or vitamin C.
13. OSMOLALITY:
Plasma osmolality describes the osmotic concentration or number of osmotically active particles in the plasma. Sodium, glucose and blood urea nitrogen are the main components that determine serum osmolality. The serum osmolality may be calculated as follows: Serum Osmolality = 1.86 [Na+] + glucose/18 + BUN/2.8
International Units 280 295 mOsm/kg
Increased Value
Decreased Value
Increased Serum Osmolality may occur with dehydration, diabetic ketoacidosis (DKA), diabetes Insipidus and ethanol, methanol or ethylene glycol toxicity.
Decreased Serum Osmolality may be caused by overhydration or SIADH.
23
CLINICAL PHARMACY 14. TOTAL SERUM PROTEIN: Total serum protein is the sum of albumin, globulin and other circulating proteins in the serum. Albumin and globulins are indicators of nutritional status.
International Units 6.0 8.5 g/dL
Increased Value
Decreased Value
Increased Protein (HYPERPROTEINEMIA) may be associated with collagen vascular diseases (lupus, rheumatoid arthritis, and scleroderma), sarcoidosis, multiple myeloma and dehydration.
Decreased Protein (HYPOPROTEINEMIA) may result from a decreased ability to synthesize protein (liver disease) or an increased protein wasting as seen in renal disease, nephritic syndrome and third degree burns.
24
CLINICAL PHARMACY
CARDIC DIAGNOSTIC TESTS
Following two tests fall into this category Creatine Kinase Troponin
25
CLINICAL PHARMACY
1. CREATINE KINASE: (CK)
Creatine Kinase is an enzyme found primarily in skeletal muscles and in smaller fractions in the brain and cardic muscle. CK MB ( cardic tissue) is an important marker in the diagnosis of acute myocardial infarction ( AMI ).
Normal Range Total CK Male 40 200 IU/L
Clinical Significance The CK MB levels begin to rise 4 to 8 hours after onset of Acute Myocardial Infarction. The concentration usually peaks between 12 and 24 hours and levels return to normal 2 to 3 days after Acute Myocardial Infarction. Serial CK MB tests are useful in the diagnosis of Acute Myocardial Infarction. An elevated CK MB level greater than 4 5% of total CK is suggestive of Acute Myocardial Infarction. An elevation of total CK may be seen with trauma, surgery, shock, tonic clonic seizures, muscular dystrophy, polymyositis, dermatomyositis, chronic alcoholism, malignant hyperthermia and cerebrovascular accident.
Female 35 150 IU/L
CK MB <12 IU/L or 4% of total CK.
2. TROPONIN: Troponin I and T are sensitive markers of cardiac injury.
Normal Range
Clinical Significance
Troponin I Troponin T
< 1.5ng/mL 0.1- 0.2ng/mL
Troponin levels begin to rise within 4 hours of onset of chest pain. Patients with elevated troponin levels are considered at high risk for a significant cardic event.
26
CLINICAL PHARMACY
LIPOPROTEIN PANEL
This includes the following four Total Serum Cholesterol. Low Density Lipoproteins. High Density Lipoproteins. Triglycerides.
27
CLINICAL PHARMACY
1. TOTAL SERUM CHOLESTEROL:
Cholesterol is an important component of cell membranes and is necessary for the synthesis of many hormones and bile salts. Elevated total serum cholesterol is a useful screening test to determine Coronary Heart Disease (CHD).
Desired Range
SI Units
Clinical Significance
Desirable Level <200 mg/Dl
<5.17 mmol/L
Border Line High 200 239 mg/dL
5.2 6.21 mmol/L
High Cholesterol 240 mg/dL
6.22 mmol/L
In cases of elevated cholesterol, the need for diet or drug therapy should be based on the individual components of the lipid profile and the number of Coronary Heart Disease risk disease. Decreased cholesterol levels may be seen in malabsorption, malnutrition, hyperthyroidism, chronic anemia or severe liver disease.
2. LOW DENSITY LIPOPROTEINS: (LDL) Low density lipoprotein is a major cholesterol transport protein. LDL is considered the bad cholesterol and has been linked to atherogenesis.
Desired Range
SI Units
Clinical Significance
No CHD and <2 CHD risk factors <160 mg/dL No CHD and 2 CHD risk factors <130 mg/ dL With CHD or Diabetes <100 mg/ dL
4.11 mmol/L
3.36 mmol/L
2.6 mmol/L
Dietary therapy should be initiated when LDL is above the desired range. Drug therpy should be considered when LDL is 30 mg/dL or more above the desired range. In patients with two or more CHD risk factors and a 10 year risk of CHD of 10 20%, drug therapy may be initiated when the LDL is greater than 130 mg/dL. In addition to lipid disorders, elevated LDL may also be associated with diabetes mellitus, hypothyroidism and nephrotic syndrome.
28
CLINICAL PHARMACY
3. HIGH DENSITY LIPOPROTEINS: (HDL)
High density lipoproteins are responsible for transport of 20% to 30% of serum cholesterol. HDL removes excess cholesterol from peripheral tissues. It is considered the good cholesterol and elevated HDL levels are associated with a decreased risk for CHD.
Blood Levels
SI Units
Clinical Significance
Normal Range 30 70 mg/dL Desired Range >40 mg/dL
SI 0.78 1.81 mmol/L
SI >1.04 mmol/L
Decreased HDL may be associated with cigarette smoking, diabetes mellitus, lack of exercise and use of anabolic/androgenic steroids or Beta blockers. Elevated HDL may be seen with moderate alcohol intake or in patients taking estrogens, oral contraceptives or nicotinic acid.
4. TRIGLYCERIDES:
Triglycerides are the main storage form of fatty acids.
Blood Levels
SI Units
Clinical Significance
Normal Range <150 mg/dL Borderline High 150 199 mg/dL High 200 499 mg/Dl Very High 500 mg/Dl
1.7 mmol/L 1.7 2.26 mmol/L 2.26 5.64 mmol/L
>5.64 mmol/L
Triglycerides may be significantly elevated in the nonfasting state and should be measured after a fast of at least 12 14 hours. In addition to lipid disorders, elevated triglycerides may be associated with a nonfesting sample, diabetes mellitus, pancreatitis, nephrotic syndrome, chronic renal failure, alcoholism, gout and use of oral contraceptives or intravenous lipid infusions.
29
CLINICAL PHARMACY
ENDOCRINE DIAGNOSTIC TESTS
1. THYROID FUNCTION TESTS Thyroid stimulating hormone Thyroxin Free thyroxin Total tri-iodothyronine
2. DIABETES MELLITUS
Hemoglobin A 1c
3. ADRENAL GLAND TESTS Cortisol Dexamethasone suppression test Adrenocorticotropic hormone Adrenocorticotropic hormone stimulation test
30
CLINICAL PHARMACY
1. THYROID FUNCTION TESTS:
It includes the following four tests Thyroid stimulating hormone Thyroxin Free thyroxin Total tri-iodothyronine
i) THYROID STIMULATING HORMONE: (TSH)
Thyroid Stimulating Hormone is sensitive screening test used to detect hypothyroidism or hyperthyroidism.
International Units
SI Units
Elevated Thyroid Stimulating Hormone
Low Thyroid Stimulating Hormone
0.3 5 U/Ml
0.3 5 mU/L
Elevated thyroid stimulating hormone levels are indicative of hypothyroidism. TSH may be falsely elevated in the first trimester of pregnancy.
Abnormally low TSH levels (< 10) are associated with hyperthyroidism. Medications with dopaminergic activity can decrease TSH levels. Abnormal TSH levels should be followed up with the thyroid hormone test (T3 or T4).TSH should be monitored 6 to 8 weeks afer initiation or a change in therapy.
31
CLINICAL PHARMACY
ii) THYROXINE: (T4)
T4 is the predominant circulating thyroid hormone. T4 levels are a measure of the functional status of the thyroid gland. T4 may also be used to monitor thyroid therapy. T4 levels may be affected by conditions that increase or decrease the thyroxin binding proteins.
International Units 4 12 g/dL
SI Units 51 154 nmol/L
Increased T4
Decreased T4
T4 can be increased in hyperthyroidism, pregnancy, hepatitis and the use of estrogen replacement therapy or oral contraceptives.
Decreased T4 is most commonly seen in hypothyroidism but may also be associated with renal function, malnutrition, cirrhosis and use of medications that compete for T4 binding sites on T4 binding proteins.
iii) FREE THYROXINE: (Free T4)
Total T4 levels can be affected by conditions that alter the amount of thyroxin binding proteins, freeT 4 is the most accurate reflection of clinical thyroid status.
International Units 0.8 2.7 ng/dL
SI Units 10 35 pmol/L
Increased T4
Free T4 is a diagnostic test that may be used to confirm the diagnosis of hypothyroidism or hyperthyroidism. Free T4 levels may be increased or decreased by amiodarone and iodides and decreased with sulfonamides and lithium.
32
CLINICAL PHARMACY
iv) TOTAL TRIIODOTHYRONINE: (T3)
The majority of T3 is formed from de-iodination of T4 in the kidney and liver. Total T3 measures both bound and unbound T3. T3 is usually used in the diagnosis of hyperthyroidism or T3 toxicosis but has little utility in the diagnosis of hypothyroidism.
International Units
SI Units
Increased T3
Decreased T3
80 160 ng/dL
1.2 2.5 nmol/L
Increased T3 is seen in hyperthyroidism, T3 toxicosis, high doses of levothyroxine and other conditions that also increase T4
Decreased T3 may be associated with hypothryodism and malnutrition. Glucocorticoids and propranolol decrease peripheral conversion of T4 to T3 and may result in reduced T3 levels.
33
CLINICAL PHARMACY
2. DIABETES MELLITUS:
It includes only the following test
HEMOGLOBIN A1C: (HbA1C)
HbA1C measures the percentage of hemoglobin molecules that are bound to glucose. During the life span of RBC, glucose binds irreversibly to hemoglobin in the RBC. As the serum glucose becomes more elevated, more glucose binds to the hemoglobin. Because the RBC has a life span of approximately 120 days, the HbA1C reflects blood glucose control for the 2 to 3 months preceding the test.
Normal Range
Clinical Significance
46%
The HbA1C may be used to assess blood sugar control over the 2 to 3 months preceding the test. An HbA1C greater than 7 % indicates the need for improved diabetic control through adjustment of diet, exercise or medication regimen.
From the HbA1C, the average blood glucose may be calculated as follows: Mean Blood Glucose = 33.3 (HbA1C) 86
34
CLINICAL PHARMACY
3. ADRENAL GLAND TESTS:
This test includes Cortisol Dexamethasone suppression test Adrenocorticotropic hormone Adrenocorticotropic hormone stimulation test
i) CORTISOL:
Cortisol is a hormone produced by the adrenal cortex. It plays a critical role in carbohydrate metabolism and response to stress. Cortisol plasma levels undergo a normal diurnal variation and are highest in the early morning.
International Units
SI Units
Increased Cortisol
Decreased Cortisol
Morning 6 25 g/dL Evening 3 12 g/dL
165 690 nmol/L 83 331 nmol/L
Increased cortisol levels are associated with Cushings disease, Cushings syndrome, hyperthyroidism, oral contraceptive use, pregnancy, stress and morbid obesity.
Decreased cortisol may be secondary to Addisons disease, hypothyroidism or decreased pituitary function.
ii) DEXAMETHASONE SUPPRESSION TEST:
In this test, 1mg of dexamethasone is given at midnight and plasma cortisol levels are drawn at 8:00 a.m. In a normal patient, the administration of exogenous steroid (dexamethasone) should suppress the release of cortisol from the adrenal gland. The dexamethasone suppression test is useful in the diagnosis of Cushings syndrome.
Normal Range
Clinical Significance
Cortisol <5 g/dL at 8:00 a.m.
A plasma level >5 g/dL suggests the diagnosis of Cushings syndrome. Elevated cortisol levels may also be seen in patients who are under various types of stress, including acute illness, pregnancy and psychiatric disorders. Results should be interpreted with caution un these populations.
35
CLINICAL PHARMACY
iii) ADRENOCORTICOTROPIC HORMONE: (ACTH)
Adrenocorticotropic Hormone is a hormone secreated from the anterior pituitary. It controls the release of cortisol from the adrenal gland.
International Units
SI Units
Increased Adrenocorticotropic Hormone
Decreased Adrenocorticotropic Hormone
< 60 pg/Ml
<13.2 pmol/L
Increased Adrenocorticotropic Hormone may be associated with Cushings disease, adrenal hyperplasia, Addisons disease or atopic pregnancy.
Decreased Adrenocorticotropic Hormone may be seen in adrenal maliganancy or states of pituitary insufficiency.
iv) ADRENOCORTICOTROPIC HORMONE STIMULATION TEST: (COSYNTROPIN)
In the Adrenocorticotropic Hormone test, a baseline cortisol level is drawn. Then synthetic ACTH (COSYNTROPIN) is administered and cortisol levels are collected 30 and 60 minutes post administration.
Normal
Abnormal
A normal response is doubling of the baseline cortisol level. A rise in cortisol greater than 10g/dL above baseline may be considered a normal response.
If plasma cortisol remains low and fails to rise greater than 10 g/dL above baseline, this is indicative of adrenal insufficiency. Further testing is necessary to determine if the cause of the adrenal insufficiency is related to failure of the adrenal or malfunction of the pituitary.
36
CLINICAL PHARMACY
GASTROINTESTINAL / HEPATIC/ PANCREATIC DIAGNOSTIC TESTS
They include the following important tests Alanine Aminotransferase Aspartate Aminotransferase Alkaline Phosphate Ammonia Bilirubin Glutamyl Transpeptidase Lactate Dehydrogenase Amylase Lipase Helicobacter pylori IgG Hemoccult
37
CLINICAL PHARMACY
1. ALANINE AMINOTRANSFERASE: (ALT)
Formerly called as Serum Glutamic Pyruvic Transaminase (SGPT) ALT is an intracellular enzyme present in liver tissues. It is also located in myocardial muscle and renal tissues.
Normal Range 0 35 U/L
SI Units 0 0.58 kat/L (varies with assay)
Clinical Significance
High serum ALT concentrations are indicative of hepatocellular disease. Elevations greater than two times the upper limit of normal are considered significant. ALT is much more concentrated in liver tissue than the aminotransferase AST and is considered more specific marker for liver disease. Increased levels of ALT may occur with hepatitis, alcoholic liver disease, CHF, mononucleosis and cholestasis. Elevated ALT may be caused by a number of medications including HMG-CoA reductase inhibitors and niacin.
2. ASPARTATE AMINOTRANSFERASE: (AST) Formerly called as Serum Glutamic Oxolacetic Transaminase (SGOT) AST is another intracellular aminotransferase found in the liver. It is also present in the heart, kidney, pancreas, lungs and skeletal muscle. Injury to these tissues will release AST into the systemic circulation and result in serum AST elevation.
Normal Range 0 40 U/L
SI Units 0 0.67 kat/L (varies with assay)
Clinical Significance
Elevated AST is associated with hepatitis, alcoholic liver disease, cholestasis, pericarditis, acute myocardial infarction, trauma, CHF, mononucleosis, severe burns, renal infarction, pulmonary infarction, pulmonary embolus and acute pancreatitis. In alcoholic liver disease, the ratio of AST to ALT is usually greater than 2:1. Elevations of AST may also be seen with drug toxicity. Erythromycin, Levodopa, Methyl dopa and Tolbutamide may falsely elevate AST by interfering with the assay.
38
CLINICAL PHARMACY
3. ALKALINE PHOSPHATE: (Alk Phos)
Alkaline Phosphatases are a group of isoenzymes located in bones, liver, intestine and the placenta.
Normal range
Clinical significance
This varies with age and assay used.
Elevated concentrations of alkaline phosphatase may be seen in a variety of conditions including obstructive liver disease, cholestasis, and cirrhosis, healing bone fractures, Pagets disease, bone metastases, hyperthyroidism, pregnancy and sepsis. If the source of elevated alkaline phosphatase is unclear the isoenzyme may be fractionated to discern if the cause is liver, bone or other. Alternatively, an increased glutamyl transpeptidase (GGT) with an elevated alkaline phosphatase is highly suggestive of a live source for the increased alkaline phosphatase.
4. AMMONIA: (NH3)
Ammonia is generated through metabolism of protein by intestinal bacteria. Usually ammonia is absorbed into the systemic circulation, metabolized by the liver and the by-product urea is excreted by the kidneys. Ammonia concentration is most often used in the diagnosis and monitoring of hepatic encephalopathy.
Normal Range 30 70 g/dL
SI Units 17 41 mol/L
Clinical Significance
Elevated concentrations of ammonia are associated with cirrhosis, other liver diseases, Reyes syndrome and inherited disorders of the urea cycle.
39
CLINICAL PHARMACY
5. BILIRUBIN: (Bili)
Bilirubin is a breakdown product of hemoglobin. The bilirubin produced from hemoglobin metabolism is referred to as unconjugated or indirect bilirubin. Unconjugated bilirubin is converted to conjugated or direct bilirubin by the liver through the process of glucuronidation. Conjugated bilirubin is excreted into the bile and subsequently into the intestine. In the intestine, some bilirubin is excreted in the feces and the remainder is broken down to urobilinogen. Urobilinogen is later excreted renally.
Normal Range
SI Units
Clinical Significance
Total Bili 0.1 1.0 mg/Dl Indirect 0.2 0.7 mg/Dl Direct 0 0.2 mg/Dl
2 18 mol/L 3.4 12 mol/L 0 3.4 mol/L
Increased levels of indirect bilirubin may result from hemolysis, large hematomas and the inherited disorder Gilberts syndrome. Elevated direct bilirubin may be associated with hepatpcellular disease, hepatitis, cirrhosis and cholestasis. Jaundice is a classic sign of hyperbilirubinemia that usually occurs when total bilirubin exceeds 2 4 mg/dL.
6. GLUTAMYL TRANSPEPTIDASE: (GGT, GGTP) Glutamyl transpeptidase is an enzyme found in the liver, kidney and prostate. GGT levels are useful in the diagnosis and monitoring of alcoholic liver disease
Normal Range 0 65 U/L
SI Units 0.1 1.08 kat/L 0 0.67 kat/L
Clinical Significance:
Male
Female 0 40 U/L
Increased GGT activity may be seen in alcoholic liver disease, metastatic liver disease, obstructive jaundice, cholelithiasis, pancreatitis, myocardial infarction and CHF. Enzyme inducers that cause microsomal proliferation such as Phenobarbital, rifampicin, phenytoin and carbamazepine may also increase GGT levels.
40
CLINICAL PHARMACY
7. LACTATE DEHYDROGENASE: (LDH)
Lactate dehydrogenase is an enzyme involved in the interconversion of lactate and pyruvate. It is found in many tissues, including heart, brain, liver, skeletal muscle, kidneys and RBCs.
Normal Range 100 210 IU/L
SI Units 1.67 3.5 kat/L
Clinical Significance
Elevated levels of LDH5 are indicative of liver disease and may be seen in hepatitis, cirrhosis and biliary tract obstruction. LDH1 and LDH2 may be used to confirm the diagnosis of myocardial infarction. Other conditions associated with increased LDH include hemolysis, trauma, muscular dystrophy, pulmonary embolism, pulmonary infarction, acute renal infarction, malignancy and myocarditis.
8. AMYLASE:
Amylase is an enzyme that aids digestion by breaking down starch into glucose. The majority of amylase originates from the pancreas and salivary glands and lesser amounts are secreated by the fallopian tubes, lungs, thyroid and tonsils.
Normal Range
Clinical Significance
20 128 IU/L
Increased concentrations of amylase may be seen in acute pancreatitis, exacerbationof chronic pancreatitis, cholecystitis, appendix, ruptured ectopic pregnancy, mumps, alcoholism and diabetic ketoacidosis.
41
CLINICAL PHARMACY
9. LIPASE:
Lipase is an enzyme that aids in the digestion of fat. Lipase is primarily secreted by the pancreas and is useful in the diagnosis of pancreatitis. The lipase level begins to rise within 2 to 6 hours of onset of acute pancreatitis.
Normal Range
Clinical Significance
< 15 U/Dl
Elevations of lipase are associated with pancreatitis. It may also be elevated with cholecystitis, cirrhosis, pancreatic cancer and small bowel obstruction. If lipase is normal and amylase is elevated this suggests a non pancreatic origin for the increased amylase.
10. Helicobacter pylori IgG:
It is a curved gram negative rod that is responsible for the majority of cases of peptic ulcer disease . H.pylori can be detected in 90% to 100% of patients with duodenal ulcers and 70% to 80% of patients with gastric ulcers.
Normal Value Negative
Clinical Significance
A positive H.pylori IgG in presence of dyspeptic symptoms is highly suggestive of peptic ulcer disease and a course of antibiotic therapy is warranted. H.pylori IgG may remain positive for many months after treatment of the infection.
11. HEMOCCULT: It is most commonly used to detect the presence of occult blood in the stool.
Normal Value
Clinical Significance
Negative
A positive hemoccult test indicates blood loss in the GIT. A false positive result may be obtained if the patient is receiving iron supplementation or has eaten red meat, broccoli, turnips or radish within 3 days of the test. False negatives may occur in patients taking high doses of vitamin C.
42
CLINICAL PHARMACY
HEMATOLOGIC DIAGNOSTIC TESTS
It includes the following Iron Ferritin Total Iron Binding Capacity (TIBC) Vitamin B12 (Cyanocobalamin) Folate
43
CLINICAL PHARMACY
1. IRON:
Serum iron measures the concentration of iron bound to the iron transport protein transferring. Approximately one third of transferring molecules are bound to iron.
Normal Range
SI Units
Increased Serum Iron
Decreased Serum Iron
Male 50 160 g/dL
9 29 mol/L 7 27 mol/L
Female 40 150 g/dL
Increased iron may be associated with excessive iron therapy, frequent transfusions, pernicious anemia, hemolytic anemia, thalassemia and hemochromatosis (iron overload).
Reduced serum iron is most commonly associated with iron deficiency anemias. Causes include poor dietary intake, pregnancy, blood loss associated with menses, peptic ulcer, gastrointestinal bleeding and inflammatory bowel disease. Other causes of decreased iron are malignancies, anemia of chronic disease, chronic renal disease, hemodialysis and some infections.
2. FERRITIN:
Ferritin is the storage form of iron. The serum ferritin level provides an accurate reflection of total blood capacity.
Normal Range
Increased Serum Ferritin
Decreased Serum Ferritin
Male 15 200 ng/mL Female 12 150 ng/ mL
Increased ferritin may result from hemochromatosis, mligancies, inflammation, acute hepatitis and liver disease.
Decreased serum ferritin is associated with iron deficiency anemia.
44
CLINICAL PHARMACY
3. TOTAL IRON BINDING CAPACITY: (TIBC)
It is an indirect measurement of serum transferring. The test is performed by adding an excess of iron to a plasma sample. Any excess unbound iron is removed from the sample and serum iron concentration in the sample is measured.
Normal Range 250 400 g/dL
SI Units 44.8 71.6 mol/L
Increased TIBC
Decreased TIBC
Increased TIBC may be associated with iron deficiency anemia, pregnancy and oral contraceptive use.
Decreased TIBC may be caused by anemia of chronic disease, malignancy, infections, uremia and hemochromtosis.
4. VITAMIN B12 : (Cyanocobalamin)
This test measures serum levels of vitamin B12. Vitamin B12 is important in DNA synthesis, neurological function and malnutrition of RBCs. Deficiency of vitamin B12 produces macrocytic anemia. Patients may also present with glossitis, paresthesias, muscle weakness, gastrointestinal symptoms, loss of coordination, tremors and irritability.
Normal Range 100 90 pg/mL
SI Units 74 664 pmol/L
Clinical Significance
Decreased vitamin B12 may be caused by inadequate dietary intake, decreased production of intrinstic factor or decreased absorption of B12. Decreased levels of B12 are associated with pernicious anemia, gastrectomy, Chrons disease, small bowel resection, intestinal infections and use of colchicines or neomycin.
45
CLINICAL PHARMACY
5. FOLATE:
This test measures serum folate and is necessary for the synthesis of DNA. Deficiency of folic acid results in a megaloblastic anemia.
Normal Range
SI Units
Clinical Significance
3.1 12.4 ng/mL
7.0 28.1 nmol/L
Inadequate intake, decreased absorption or inability to convert folic acid to the active form tetrahydrofolic acid may cause decreased folic acid levels. Folate deficiency is associated with alcoholism, poor nutrition, pregnancy, hyperthyroidism, Crohns disease, small bowel resection, celiac disease and use of medications such as trimethoprim, sulfamethoxazole, methotrexate and sulfasalazine.
46
CLINICAL PHARMACY
COAGULATION TESTS
It includes the following:
Prothrombin time (PT) Activated partial thromboplastin time International normalized ratio (INR)
47
CLINICAL PHARMACY
1. PROTHROMBIN TIME:
The prothrombin test is sensitive to changes in the levels of clotting factors prothrombin (factor II), factor (VII) and factor (X). it is performed by adding thromboplastin and calcium to a plasma sample. After addition of these reagents, the time it takes the blood to clot is measured.
Normal range 11 13 seconds (varies)
Clinical significance
The PT is used to monitor warfarin therapy. PT may vary according to the thromboplastin used to test the sample, the international normalized ratio is a better monitoring tool. The normal PT in a person not on anticoagulation therapy is 11 13 sec. an increase in PT may be see with anticoagulation therapy, liver diasease, vitamin K deficiency and clotting factor deficiencies.
2.ACTIVATED PARTIAL THROMBOPLASTIN TIME :(aPTT)
The aPPT is sensitive to changes in the clotting factors thrombin (factor IIa), factor (Xa) and factor (IXa). It is used to monitor heparin therapy.
Normal Range 20 45 seconds (varies)
Clinical Significance
The normal value represents a control range for patients not on anticoagulation therapy. Patients on heparin therapy will have an elevated aPTT.Much like the prothrombin time; the aPTT can vary depending on the reagent (partial thromboplastin) used to test the sample.
48
CLINICAL PHARMACY
3. INTERNATIONAL NORMALIZED RATIO :(INR)
PT may vary due to the thromboplastin used, the INR is used to standardize the PT. the INR adjusts the PT ratio based on the sensitivity of the thromboplastin used to perform the test. INR = [(patient PT) / (mean normal PT)]ISI ISI is the international sensitivity index rating assigned to a particular thromboplastin. Desired ranges for the INR are as follows. INR 2.0 3.0 Atrial fibrillation DVT treatment PE treatment Prophylaxis of venous thrombosis Tissue heart valves Valvular heart disease INR 2.5 3.5 Mechanical prosthetic valve
Desired Range
Clinical Significance
Depends on indication for anti coagulation
INR below range indicates suboptimal anti coagulation and a need to increase warfarin dosge. An INR above the deired range indicates a need to reduce the warfarin dosage. Patient should be questioned regarding dosage of warfarin, missed doses, dietary intake and concomitant medications.
49
CLINICAL PHARMACY
IMMUNOLOGICAL DIAGNOSTIC TESTS
This includes the following: Anti nuclear anti bodies (ANA Titer) Rheumatoid factor (RF) Erythrocyte sedimentation rate (ESR)
50
CLINICAL PHARMACY
1.ANTI NUCLEAR ANTI BODIES :(ANA Titer)
Antinuclear antibodies (ANA Titer) are antibodies directed against nucleic acids and other nucleic proteins. The ANA test is used as a diagnostic tool for autoimmune and connective tissue diseases, particularly systemic lupus erythematosus (SLE).
Normal Value
Clinical Significance
< 1:20 or < 1:40 (varies)
High titers may be associated with SLE, rheumatoid arthritis, scleroderma, Sjogens symdrome, polymyositis, dermatomyositis and drug induced lupus (hydralazine, procanamide). False positive ANA test may occur in 2 5 % of healthy patients. False positive results may be caused by use of certain medications, including Carbamazepine, Chloropromazine, Methyldopa and Phenytoin.
2.RHEUMATOID FACTOR: (RF)
Rheumatoid factor is an immunoglobulin whose activity is directed against IgG. Thus, a positive FR test (titer 1:160 or greater) is indicative of an autoimmune process.
Normal Value
Clinical Significance
< 1 : 160
A positive rheumatoid factor test is most commonly associated with rheumatoid arthritis but may also be seen with SLE, scleroderma, Sjogrens syndrome, malignancy and infectious diseases such as tuberculosis, syphilis and endocarditis.
3. ERYTHROCYTE SEDIMENTATION RATE: (ESR)
ESR measures the rate of erythrocyte settlement in anticoagulated blood. In the presence of proteins known as acute phase reactants, erythrocytes settle much more quickly. Acute phase reactants are often associated with infectious or inflammatory disorders. ESR is a nonspecific diagnostic test that may be used to support a diagnosis or monitor the progress of an inflammatory or infectious process.
Normal Range Male 1 15 mm/hr (increases with age) Female 1 20 mm/hr (increases with age)
Clinical Significance
The ESR may be elevated in infections such as tuberculosis and syphilis, maliganancies, ulcerative colitis, polymyalgaia rheumatic, temporal arteritis, rheumatoid arthritis, SLE, scleroderma and other collagen vascular disease.
51
CLINICAL PHARMACY
INFECTIOUS DISEASE DIAGNOSTIC TESTS
Following tests are included in this section ENZYME LINKED IMMUNOSORBENT ASSAY (ELISA) for HIV WESTERN BLOT CD4 (T4 LYMPHOCYTES) HIV VIRAL LOAD RAPID PLASMA REAGIN (RPR) VENEREAL DISEASE RESEARCH LABORATORY TEST (VDRL)
52
CLINICAL PHARMACY
1. ENZYME LINKED IMMUNOSORBENT ASSAY (ELISA) for HIV:
The ELISA test for HIV detects anti bodies to HIV. It is a highly sensitive and specific testand is most commonly used for screening test for HIV.
False Positive
False Negative
False positive results may occur in patients with lupus, syphilis, influenza, hepatitis B vaccine, chronic hepatitis and malaria. Positive tests should be repeated to assure positive results. Repeatedly positive samples should be confirmed with the western blot test.
False negative results may be seen in early HIV infections, malignancy nd bone marrow transplant.
2. WESTERN BLOT:
It is a confirmatory test used following a positive ELISA result. It detects antibodies to specific HIV proteins and glycoprotein.
Positive Result
False Negative / Indeterminate
A positive result following a positive ELISA test confirms the diagnosis of HIV.
False negative or indeterminate results may occur if seroconversion is not complete. Individuals should be retested at a later date.
53
CLINICAL PHARMACY
3. T4 LYMPHOCYTES: (CD4)
CD4 cells are a subset of lymphocytes also known as helper cells. CD4 cells are responsible for cell mediated immunity and are good marker of immune function.
Normal Range 400 1185/mm3
Clinical Significance
As the CD4 cell count decreases, the patient is at increased risk of acquiring opportunistic infections. When the absolute CD4 cell count falls to less than 200, the diagnosis is no longer just HIV but AIDS.CD4 cell counts are used as an indicator for starting prophylaxis in HIV patients (e.g., PCP prophylaxis is initiated at a CD4 <200).With appropriate medications CD4 count May increase.
4. HIV VIRAL LOAD:
HIV viral load measures the amount of HIV virus detectable per milliliter of plasma. Higher viral loads are associated with a poorer prognosis and progression of disease. Viral loads are measured at baseline 2 to 4 weeks after initiation of therapy and approximately every 3 months thereafter.
Range Of Assay HIV I RNA by PCR 400 750,000 copies/ml (varies)
Clinical Significance
Increasing viral loads may indicate viral resistance or no adherence to therapy. Patients with undetectable viral loads may be followed up with an ultrasensitive assay that is capable of detecting viral loads as low as 50copies/ml.
54
CLINICAL PHARMACY
5. RAPID PLASMA REAGIN (RPR):
RPR is a non treponemal serological test used to screen for syphilis. It may also be used to assess response to syphilis therapy.
Normal Value
False Positive
False Negative
Non reactive
It may occur with other infectious diseases such as measles, chickenpox, malaria, mononucleosis, hepatitis, early HIV infections and conditions such as pregnancy, lupus and connective tissue disease.
They may be seen early in infection and in late infection the test may also be non reactive. A fourfold decline in the RPR titer after 1 year may also be considered an adequate response to treatment.
6. VENERAL DISEASE RESEARCH LABORATORY TEST:(VDRL)
The VDRL is a nontreponemal serologic test to screen for syphilis. It may also be used to assess response to syphilis therapy.
Normal Value
False Positive
False Negative
Non reactive
May be caused by infectious diseases such as measles, chickenpox, malaria, mononucleosis, hepatitis, early HIV infections and other conditions such as pregnancy, lupus and connective tissue disease.
False negative results may be seen in early infection and in late infection the test may also be nonreactive Most patients revert to a non reactive test following successful treatment. A fourfold decline in the VDRL titer after 1 year may also be considered an adequate response to treatment.
55
CLINICAL PHARMACY
HEPATITIS A
This includes the following two Anti HAV IgM Anti HAV IgG
56
CLINICAL PHARMACY
1. ANTI - HAV IgM:
Hepatitis A IgM antibodies may be detected in the serum 4 6 weeks after exposure to hepatitis A and often coincide with the onset of jaundice.
Normal Value
Clinical Significance
Negative
The presence of anti HAV IgM indicates acute hepatitis A 2, 5.22. Anti HAV IgM becomes negative within 2 3 months after acute hepatitis.
2.ANTI - HAV IgG:
Anti- HAV IgG can be detected 6 12 weeks after exposure to Hepatitis A.
Normal Value
Clinical Significance
Negative
Presence of anti HAV IgG indicates previous infection with HAV and immunity to the virus 2, 22, 32.
57
CLINICAL PHARMACY
HEPATITIS B
This includes the following Hepatitis B Surface Antigen (HBsAg) Hepatitis B e Antigen (HBeAg) Hepatitis B Core Antibody (anti HBc) Hepatitis B Surface (anti HBs)
58
CLINICAL PHARMACY
1. HEPATITIS B SURFACE ANTIGEN: (HBsAg)
HBsAg is a protein coat that surrounds the hepatitis B virus. It can be detected in the serum 4 12 weeks after infection.
Normal Value
Clinical Significance
Negative
A positive test for HBsAg indicates acute hepatitis B. persistence of HBsAg for 20 weeks or more after acute infection is indicative of chronic hepatitis B.
2. HEPATITIS B e ANTIGEN: (HBeAg)
HBeAg is used to assess the degree of infectivity of patients with hepatitis B.
Normal value
Clinical significance
Negative
Presence of HBeAg is associated with active viral replication and a high degree if infectivity. HBeAg is usully present for 2 6 weeks after acute infection. Persistence of HBeAg is indicative of chronic hepatitis.
3. HEPATITIS B CORE ANTIBODY: (ANTI HBc)
Anti HBc may be detected in the blood a few weeks after the appearance of HBsAg.
Normal Value
Clinical Significance
Negative
Positive results for anti HBc indicate past infection with hepatitis B. these antibodies seem to persist for life.
59
CLINICAL PHARMACY
4. HEPATITIS B SURFACE ANTIBODY: (ANTI HBs)
Anti HBs is usually detected in the blood 5 6 months after infection.
Normal Range
Clinical Significance Presence of anti HBs indicates recovery and immunity to hepatitis B Individuals who been vaccinated for hepatitis B will test positive for anti HBs. Because anti HBs levels may decline or disappear over time, revaccination at 5 7 years is recommended.
Negative
60
CLINICAL PHARMACY
HEPATITIS C
HEPATITIS C ANTIBODY: (ANTI HCV)
Anti HCV is used as a screening test for hepatitis C virus.
Normal Range
Clinical Significance
Negative
Presence of anti HCV indicates prior exposure to or chronic infection with hepatitis C. unlike antibodies to hepatitis A and hepatitis B, antibodies to hepatitis C do not confer immunity. Antibodies may not be present until 6 - 12 weeks after acute infection. A positive test for anti HCV should be followed by a confirmatory test such as radioimmunoblot assay (RIBA) or hepatitis C viral load (HCV RNA by PCR).22,34
61
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
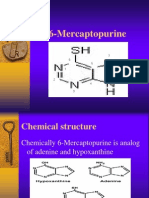
- 6 MercatopurineDocumento12 páginas6 MercatopurineAziza HasanAinda não há avaliações
- BarbituratesDocumento33 páginasBarbituratesAziza HasanAinda não há avaliações
- Pharmacy Design & LayoutDocumento35 páginasPharmacy Design & LayoutAziza Hasan50% (24)
- Case Study New 03Documento24 páginasCase Study New 03Aziza HasanAinda não há avaliações
- Marketing ChannelsDocumento37 páginasMarketing ChannelsAziza HasanAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Myocarditis: Mark A. Fischione, M.D. Pathological Sciences School of Osteopathic Medicine in ArizonaDocumento28 páginasMyocarditis: Mark A. Fischione, M.D. Pathological Sciences School of Osteopathic Medicine in ArizonaTony ZiherlAinda não há avaliações
- Paediatrics III (A)Documento1 páginaPaediatrics III (A)AlolikaAinda não há avaliações
- CV SAMEEP - PathologistDocumento7 páginasCV SAMEEP - PathologistMumtaj AnsariAinda não há avaliações
- Patient Information From Your Surgeon & Sages Laparoscopic Gallbladder RemovalDocumento5 páginasPatient Information From Your Surgeon & Sages Laparoscopic Gallbladder RemovalolarrozaAinda não há avaliações
- Keratosis ObturansDocumento12 páginasKeratosis ObturansRahma LuthfaAinda não há avaliações
- Asymptomatic Bacteriuria in Adults - UpToDateDocumento20 páginasAsymptomatic Bacteriuria in Adults - UpToDatefilipiAinda não há avaliações
- Case ProgressionDocumento2 páginasCase Progressionczeremar chanAinda não há avaliações
- Managing Dystonia through Exercise and PhysiotherapyDocumento15 páginasManaging Dystonia through Exercise and PhysiotherapyMohd AsadAinda não há avaliações
- Preeclampsia With HELLP SyndromeDocumento8 páginasPreeclampsia With HELLP SyndromeWely Tiffani YpAinda não há avaliações
- Cerebrospinal Fluid (CSF) Sample RequirementsDocumento7 páginasCerebrospinal Fluid (CSF) Sample RequirementsDr.Nouf alhasawiAinda não há avaliações
- RANZCO 2012 PosterDocumento7 páginasRANZCO 2012 PosterGray Design GroupAinda não há avaliações
- Torticolis OdtDocumento25 páginasTorticolis OdtAndreea CimpoiAinda não há avaliações
- Clinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenDocumento4 páginasClinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenNurul Huda KowitaAinda não há avaliações
- Oglej Case Study 4300 1Documento20 páginasOglej Case Study 4300 1api-533010905Ainda não há avaliações
- Left Thigh Pain: I. Chief Complaint/ Other ComplaintsDocumento9 páginasLeft Thigh Pain: I. Chief Complaint/ Other ComplaintsDominic BristolAinda não há avaliações
- Status of PPR in Nepal 2007Documento14 páginasStatus of PPR in Nepal 2007anon-921861100% (2)
- Curs Prim Ajutor 2023 - MG An V - Șocul Hemoragic - English-1Documento18 páginasCurs Prim Ajutor 2023 - MG An V - Șocul Hemoragic - English-1hulia jokoAinda não há avaliações
- Transfusion - March April 1966 - Allen - Choice of Blood For Exchange TransfusionDocumento3 páginasTransfusion - March April 1966 - Allen - Choice of Blood For Exchange TransfusionDR. KHANAinda não há avaliações
- Fast Scan 2022Documento9 páginasFast Scan 2022rosieAinda não há avaliações
- BREESIDocumento1 páginaBREESIJulie MorenoAinda não há avaliações
- Screening Script and Procedure For Reception and SchedulingDocumento3 páginasScreening Script and Procedure For Reception and SchedulingJobert NarvaezAinda não há avaliações
- The Role of Nuclear Medicine in Breast Cancer ManagementDocumento53 páginasThe Role of Nuclear Medicine in Breast Cancer ManagementLadipo Temitope AyodejiAinda não há avaliações
- PPPVD Fecal Scoring Chart UPDATE EN FINALDocumento2 páginasPPPVD Fecal Scoring Chart UPDATE EN FINALJon DoughballAinda não há avaliações
- NSG 123 Reflective Summary Post Surgical Patients 2Documento4 páginasNSG 123 Reflective Summary Post Surgical Patients 2api-725909264Ainda não há avaliações
- The Essential Role of Eyelids in Eye HealthDocumento96 páginasThe Essential Role of Eyelids in Eye HealthArwa QishtaAinda não há avaliações
- ANGIOEDEM: SIGNS, SYMPTOMS, TESTS AND TREATMENTDocumento18 páginasANGIOEDEM: SIGNS, SYMPTOMS, TESTS AND TREATMENTpalAinda não há avaliações
- TB Diagnosis, Treatment & ControlDocumento16 páginasTB Diagnosis, Treatment & ControlwiwonAinda não há avaliações
- MouthDocumento12 páginasMouthRodolfo MartinezAinda não há avaliações
- The Joint Philippine Society of Gastroenterology and Philippine Society of Digestive Endoscopy Consensus Guidelines PDFDocumento16 páginasThe Joint Philippine Society of Gastroenterology and Philippine Society of Digestive Endoscopy Consensus Guidelines PDFaxxoAinda não há avaliações
- Appendicitis NCPDocumento5 páginasAppendicitis NCPEarl Joseph DezaAinda não há avaliações