Escolar Documentos
Profissional Documentos
Cultura Documentos
Primary Ovarian Abscess in Pregnancy: Case Report
Enviado por
VinnyRevinaAdrianiDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Primary Ovarian Abscess in Pregnancy: Case Report
Enviado por
VinnyRevinaAdrianiDireitos autorais:
Formatos disponíveis
JK SCIENCE
CASE REPORT
Primary Ovarian Abscess in Pregnancy
N. Vimala, Nupur Kothari , Suneeta Mittal , Sunesh Kumar , Vatsla Dadhwal
Abstract Primary ovarian abscess is a rare entity, occurrence of ovarian abscess during pregnancy is even rarer. The clinical presentation is variable ranging from asymptomatic abscess to diffuse peritonitis. A delay in diagnosis may be detrimental to both mother and the fetus. We report a case of asymptomatic primary ovarian abscess associated with a term pregnancy. Key Words Ovarian abscess, pregnancy.
Introduction Primary ovarian abscess in association with pregnancy is a very rare occurrence. A delay in diagnosis and management may be detrimental to both pregnant mother and fetus (1). Modern imaging modalities including ultrasound and MRI may help in making an early diagnosis. We report a case of aysmptomatic primary ovarian abscess in association with a term pregnancy, incidentally diagnosed at caesarean section. Management resulted in birth of a live fetus and an uncomplicated postoperative course for the mother. Case Report A 29 year old primigravida was registered in our antenatal clinic at 9 weeks of gestation. A level two ultrasound at 16 weeks revealed a multiloculated right adnexal mass measuring 6x6 cm size along with a single live fetus with no malformations. The patient was advised surgery for removal of mass, but refused. She had regular prenatal checkups and had an uneventful pregnancy course till term with no complaints of fever or pain in abdomen. She had no past history suggestive of tuberculosis, pelvic inflammatory disease, any pelvic or abdominal surgery, appendicitis, diverticulitis or tonsillitis. Repeat ultrasound scans done at 28 and 34 weeks gestation revealed the adnexal mass to be of same size. At 40 weeks of gestation, she was planned for an elective induction due to development of pregnancyinduced hypertension. On admission, her BP was 140/100mm Hg while other vitals were stable. On per abdominal examination, uterus was term size with vertex presentation, fetal heart rate was 146 beats per minute. As per vaginal examination, cervix was found to be unfavourable with a Bishop score of 4. Cervical priming was done using Dinoprostone gel (0.5mg) followed by augmentation with oxytocin drip (2.5 units in 500 ml Ringer lactate at the rate of 16 drops per minute in escalating doses) after 6 hours.
From the Deptt. of Obstetrics & Gynaecology, All India Institute of Medical Sciences, New Delhi, India. Correspondence to : Dr. Sunesh Kumar, Room No. 3086, 3rd Floor, Deptartment of Obst. & Gynae, AIIMS, New Delhi, India 40 Vol. 6 No. 1, January-March 2004
JK SCIENCE Discussion Adnexal masses in pregnancy requiring surgical intervention occur with a frequency ranging from 1in 81 to 1 in 2500 live births (2). Elective surgical removal is recommended for any mass greater than 6 cm in diameter that continues to exist into the second trimester, unless the mass is suspected to be a uterine leiomyoma. Reports of pelvic abscess complicating pregnancy are rare. It is usually unilateral and more commonly seen in first than in second or third trimesters. Ovarian abscess is a primary infection of the parenchyma of the ovary, an entity distinctly different from tuboovarian abscess. Tuboovarian abscess, by contrast, involves the ovary by secondary spread from the infected fallopian tube (3). Aitken is attributed to give the earliest description of primary ovarian abscess in 1869 (4). Black presented the first major series of 42 cases in 1936. Wetchler and Dunn have reported 120 cases in literature till 1985 (3). The etiology of ovarian abscess in pregnancy is uncertain and in all probability is different from that in nonpregnant state. Ascending infection is the most important mode of infection in non-pregnant women. Barriers to ascending infection in pregnancy include cervical mucus plug, intact fetal membranes and the decidua covering the openings of the fallopian tubes. Friedman & Bobrow (5) have proposed four mechanisms for infection of ovaries during pregnancy: 1. 2. 3. 4. Haematogenous spread as in pelvic tuberculosis. Lymphatic spread especially from vagina and cervix. Infection of a previously existing ovarian cyst. Flare up of an old postabortal infection.
Fetal bradycardia developed during the course of labor induction and the patient was finally taken up for an emergency lower segment caesarean section under general anaesthesia. A female infant weighing 3.5 kg with an apgar score of 7/10 at one minute was born with no evidence of meconium staining or cord around the neck. Intra operative findings revealed a 10x10 cm rightsided encysted ovarian abscess extending into the folds of the broad ligament. The right tube appeared normal. The abscess wall inadvertently got ruptured during the process of dissection; approximately 25-30 ml of malodorous frank pus (thick, purulent and foul smelling) was drained. Cyst wall was submitted for histopathological examination and pus for microbiological study. Left tube and ovary were normal. Right ovarian removal was performed followed by thorough peritoneal lavage with saline solution and insertion of a pelvic drain. Postoperatively, patient was put on intravenous antibiotics (Cefotaxime and Amikacin). She had an uneventful postoperative course. Both mother and baby were discharged on 10th postoperative day in a healthy condition. Histopathological examination of the surgical specimen was reported as chronic abscess with oophoritis. Cultures obtained from the purulent discharge of ovarian abscess grew proteus vulgaris.
Fig. 1. Transabdominal picture (ultrasound) showing a multiloculated ovarian cyst on right side.
Cases of ovarian abscess have also been reported due to non-gynaecological conditions such as ruptured appendicitis or diverticulitis or secondary to infection at distant sites as in tonsillitis, typhoid, parotitis and
41
Vol. 6 No. 1, January-March 2004
JK SCIENCE
tuberculosis. Association of ovarian abscess with IUD (Intrauterine device) has been noted and some of them may be secondary to actinomyces. It may also occur due to secondary infection in a dermoid cyst, serous cystadenoma or simple ovarian cyst. Ovarian abscess is also a known complication of transvaginal oocyte retrieval or transcervical embryo transfer, occurring in approximately 0.2-2.2 % of cases (6). It is difficult to state the exact mechanism of development of ovarian abscess in our case. At laparotomy, there was no evidence of spread of infection from adjacent organs as the source of infection. Pre existing salpingitis/ infected ovarian cyst/tumor could not be ruled out. Thus, the proposed mechanism in our patient could be flare up of an underlying adnexal disease or spread from distant infection. Women with ovarian abscess during pregnancy may present with a wide range of clinical symptoms. A woman with a ruptured ovarian abscess presents with features of diffuse peritonitis. An unruptured abscess is more difficult to diagnose because of variable clinical presentation. Most common presenting symptom is an indolent onset of abdominal pain. Diffuse lower abdominal pain may worsen to severe pain associated with anorexia, nausea and vomiting in case of rupture. Low-grade fever may be the only presentation in 50% of cases. Fetal loss rate of 50% has been reported most often as spontaneous septic abortions. A delay in diagnosis may be associated with risk of maternal death and can be detrimental to the fetus as well. Surprisingly, our patient did not have any symptom till term. Noninvasive diagnostic modalities including ultrasound and MRI may help in early diagnosis of this unusual complication of pregnancy. Unruptured abscess may be given supportive care and treated by preoperative broad-spectrum intravenous antibiotics effective against gram positive, gram negative
and anaerobic bacteria for at least 72 hours before operative intervention. Ruptured tuboovarian abscess requires an aggressive and primarily surgical approach in order to minimize catastrophic sequelae. Since most women tend to be young, one should attempt conservative surgery if pathology is limited to only one adnexa (8). Surgical drainage of ovarian abscess and conservative surgical procedure under antibiotics are recommended during pregnancy, albeit there is no consensus on patient management (9). Fertility rate following ovarian abscess management may be relatively better when compared with tuboovarian abscess as tubal mucosa is spared (10).
References 1. David M. Sherer, Benjamin M Schwartz, Ovadia Abulafia. Management of pelvic abscess during pregnancy. A Case and Review of the Literature. Obstet Gynecol Survey 1999; 54(10). CME Review Article. 2. Shigeo Akira, Atsuko Yamanaka, Tamaki Ishihara, Toshiyuki Takeshita, Tsutomu Araki. Gasless laparoscopic ovarian cystectomy during pregnancy: Comparison with laparotomy. Am J Obstet Gynecol 1999; 180(3): 554-57. 3. Wetchler SJ, Dunn LT. Ovarian Abscess. Report of a case and review of the literature. Obstet Gynecol Survey 1985; 40(7): 476. 4. Koehn RC. Ovarian abscess complicating pregnancy. US Armed Forces Med J 1957; 8: 1664. 5. Friedman S, Bobrow ML: Pelvic inflammatory disease in pregnancy. Obstet Gynecol 1959;14: 417. 6. Askenazi J, Farhi J, Dicker D et al. Acute pelvic inflammatory disease after oocyte retrieval: adverse effects on the results of implantation. Fertil Steril 1994; 61: 526-28. 7. Blanchard AC, Pastorek JG, Weeks T. Pelvic inflammatory disease during pregnancy. South Med J 1987; 80: 1363-65. 8. Laohaburanakit P, Treevijitsilp P, Tantawichian T, Bunyavechevin S. Ruptured tuboovarian abscess in late pregnancy. A case report. J Reprod Med 1999; 44(6): 551-55. 9. Yalcin OT, Tanir HM, Eskalen M: Unruptured pelvic abscess in pregnancy: Report. Gynecol Obstet Invest 2002; 53(2): 133-34. 10. Ginsberg DS, Stenn JL, Hamod KA et al. Tuboovarian abscess. A retrospective review. Am J Obstet Gynecol 1980; 57: 138.
42
Vol. 6 No. 1, January-March 2004
Você também pode gostar
- Case Report Ghazanfar Page 130-132Documento3 páginasCase Report Ghazanfar Page 130-132sohailurologistAinda não há avaliações
- UC Irvine: Clinical Practice and Cases in Emergency MedicineDocumento6 páginasUC Irvine: Clinical Practice and Cases in Emergency MedicinePatrick NunsioAinda não há avaliações
- Aa 11Documento5 páginasAa 11Eriekafebriayana RAinda não há avaliações
- Ectopic Pregnancy - StatPearls - NCBI BookshelfDocumento6 páginasEctopic Pregnancy - StatPearls - NCBI BookshelfLaura valentina ramos mezaAinda não há avaliações
- Ectopic Pregnancy - StatPearls - NCBI BookshelfDocumento9 páginasEctopic Pregnancy - StatPearls - NCBI BookshelfKatherine DavilaAinda não há avaliações
- Ultrasound of The Pregnant Acute AbdomenDocumento16 páginasUltrasound of The Pregnant Acute Abdomenjohn omariaAinda não há avaliações
- Ovarian Pregnancy: Two Case Reports.: Jayeeta Roy, Anindita Sinha BabuDocumento5 páginasOvarian Pregnancy: Two Case Reports.: Jayeeta Roy, Anindita Sinha BabuAndriyani MuslimAinda não há avaliações
- Ovarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014Documento4 páginasOvarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014alif bagusAinda não há avaliações
- 9.radha Et Al.Documento3 páginas9.radha Et Al.International Journal of Clinical and Biomedical Research (IJCBR)Ainda não há avaliações
- Ruptured Omental Pregnancy A Case Report and Review of LiteratureDocumento4 páginasRuptured Omental Pregnancy A Case Report and Review of LiteratureInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Rare 28-Week Abdominal Ectopic PregnancyDocumento3 páginasRare 28-Week Abdominal Ectopic PregnancynajmulAinda não há avaliações
- Acute Non-Puerperal Uterine Inversion Case ReportDocumento4 páginasAcute Non-Puerperal Uterine Inversion Case ReportALfuAinda não há avaliações
- CessarDocumento4 páginasCessarkknsAinda não há avaliações
- Ruptured Ectopic Pregnancy in The Presence of An Intrauterine DeviceDocumento5 páginasRuptured Ectopic Pregnancy in The Presence of An Intrauterine DevicePatrick NunsioAinda não há avaliações
- Case Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyDocumento4 páginasCase Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyChidimma VictoryAinda não há avaliações
- 1 s2.0 S1028455909600802 MainDocumento3 páginas1 s2.0 S1028455909600802 MainSuminten S. Pd.Ainda não há avaliações
- Articles of Abnormal Obstetrics CasesDocumento11 páginasArticles of Abnormal Obstetrics CasesMarjun MejiaAinda não há avaliações
- Omental Pregnancy: Report Case and Literature ReviewDocumento5 páginasOmental Pregnancy: Report Case and Literature ReviewIJAR JOURNALAinda não há avaliações
- Diagnosis and Management of Ectopic Pregnancy: Europe PMC Funders GroupDocumento20 páginasDiagnosis and Management of Ectopic Pregnancy: Europe PMC Funders GroupDeby Nelsya Eka ZeinAinda não há avaliações
- Anesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaDocumento4 páginasAnesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaHanayuki VizureiAinda não há avaliações
- Ectopic PregenancyDocumento69 páginasEctopic PregenancyMahmoud AbbasAinda não há avaliações
- Ectopic Pregnancy: by Amielia Mazwa Rafidah Obstetric and Gynecology DepartmentDocumento43 páginasEctopic Pregnancy: by Amielia Mazwa Rafidah Obstetric and Gynecology DepartmentAlrick AsentistaAinda não há avaliações
- Recurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoDocumento2 páginasRecurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoeditorijmrhsAinda não há avaliações
- Evaluation of Ultrasonography in Various Causes of Pelvic Pain in First Trimester of PregnancyDocumento4 páginasEvaluation of Ultrasonography in Various Causes of Pelvic Pain in First Trimester of PregnancyHASSAN NADEEMAinda não há avaliações
- Ectopic PregnancyDocumento5 páginasEctopic PregnancyFaith FuentevillaAinda não há avaliações
- Spontaneous Heterotopic Pregnancy With Intrauterine Pregnancy Stopped Case Report and Review of LiteratureDocumento3 páginasSpontaneous Heterotopic Pregnancy With Intrauterine Pregnancy Stopped Case Report and Review of LiteratureInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Case Report: Ruptured Ectopic Pregnancy in Caesarean Section Scar: A Case ReportDocumento3 páginasCase Report: Ruptured Ectopic Pregnancy in Caesarean Section Scar: A Case ReportEga MegawatiAinda não há avaliações
- Uterine Rupture in Nulliparous Woman Without Risk Factors: A Case Report and Literature ReviewDocumento6 páginasUterine Rupture in Nulliparous Woman Without Risk Factors: A Case Report and Literature ReviewBOHR International Journal on GynaecologyAinda não há avaliações
- Ectopic Pregnancy22Documento43 páginasEctopic Pregnancy22Sunil YadavAinda não há avaliações
- Uterine Prolapse in A Primigravid Woman JournalDocumento13 páginasUterine Prolapse in A Primigravid Woman JournalFadhlyanyAinda não há avaliações
- Total and Acute Uterine Inversion After Delivery A Case Report PDFDocumento4 páginasTotal and Acute Uterine Inversion After Delivery A Case Report PDFatika sgrtAinda não há avaliações
- Detect Ectopic Pregnancy with UltrasoundDocumento13 páginasDetect Ectopic Pregnancy with Ultrasoundnautilus81Ainda não há avaliações
- Diagnosis and Management of Ectopic Pregnancy-A Basic View Through LiteratureDocumento2 páginasDiagnosis and Management of Ectopic Pregnancy-A Basic View Through LiteraturefprasasyaaAinda não há avaliações
- Myoma 1Documento3 páginasMyoma 1clarintauchaAinda não há avaliações
- PREGNANC1Documento20 páginasPREGNANC1SriramAinda não há avaliações
- Cases Journal: Torsion of Ovarian Cyst During Pregnancy: A Case ReportDocumento3 páginasCases Journal: Torsion of Ovarian Cyst During Pregnancy: A Case ReportAde Gustina SiahaanAinda não há avaliações
- Ovarian TorsionDocumento4 páginasOvarian TorsionRiko KuswaraAinda não há avaliações
- Abrasio PlacentaDocumento3 páginasAbrasio Placentamuhammad azamAinda não há avaliações
- Tubalpregnancy DiagnosisandmanagementDocumento12 páginasTubalpregnancy DiagnosisandmanagementAndreaAlexandraAinda não há avaliações
- Ectopic Pregnancy: Clinical PracticeDocumento9 páginasEctopic Pregnancy: Clinical PracticeNurul WulandariAinda não há avaliações
- Ectopic PregnancyDocumento14 páginasEctopic PregnancytaufiqAinda não há avaliações
- Heterotopic Pregnancy Cervical and TubalDocumento9 páginasHeterotopic Pregnancy Cervical and Tubalvictorubong404Ainda não há avaliações
- 1 s2.0 S0090825804003610 Main PDFDocumento3 páginas1 s2.0 S0090825804003610 Main PDFRirin WahyuniAinda não há avaliações
- Prolonged PregnancyDocumento41 páginasProlonged PregnancyArif Febrianto100% (1)
- The Back Alley Revisited: Sepsis After Attempted Self-Induced AbortionDocumento3 páginasThe Back Alley Revisited: Sepsis After Attempted Self-Induced Abortionmila nurmalaAinda não há avaliações
- Spontaneous Rupture of An Unscarred GravidDocumento4 páginasSpontaneous Rupture of An Unscarred GraviddelaAinda não há avaliações
- Criog2015 596826Documento3 páginasCriog2015 596826charles limbuAinda não há avaliações
- Medical and Surgical Complications of Pregnancy 08 ADocumento139 páginasMedical and Surgical Complications of Pregnancy 08 A2012Ainda não há avaliações
- 1 s2.0 S1028455911001823 MainDocumento6 páginas1 s2.0 S1028455911001823 MainFatimah AssagafAinda não há avaliações
- Interstitial Ectopic Pregnancy A Case ReportDocumento4 páginasInterstitial Ectopic Pregnancy A Case ReportRina Auliya WahdahAinda não há avaliações
- Brief DescriptionDocumento7 páginasBrief DescriptionPrincess Pilove GawongnaAinda não há avaliações
- Obstetric Emergencies: First - Trimester Pregnancy EmergenciesDocumento14 páginasObstetric Emergencies: First - Trimester Pregnancy EmergenciesdianAinda não há avaliações
- Rare Case of Bicornuate Uterus With Fetal Death in A Multipara WomanDocumento2 páginasRare Case of Bicornuate Uterus With Fetal Death in A Multipara WomanInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Challenges in The Management of A Case of 2nd Abdominal Pregnancy - OJOG - 2015092815302981Documento3 páginasChallenges in The Management of A Case of 2nd Abdominal Pregnancy - OJOG - 2015092815302981Stella Putri WandaAinda não há avaliações
- A Case Report Abdominal Pregnancy MRI Vs USG RevisedDocumento14 páginasA Case Report Abdominal Pregnancy MRI Vs USG Revisedarnovareswari28Ainda não há avaliações
- 12283-Article Text-26421-1-10-20061102Documento2 páginas12283-Article Text-26421-1-10-20061102zacAinda não há avaliações
- Treatment Strategy for Unexplained Infertility and Recurrent MiscarriageNo EverandTreatment Strategy for Unexplained Infertility and Recurrent MiscarriageKeiji KurodaAinda não há avaliações
- Guide to Pediatric Urology and Surgery in Clinical PracticeNo EverandGuide to Pediatric Urology and Surgery in Clinical PracticeAinda não há avaliações
- Hypertention Stage II Da IIDocumento38 páginasHypertention Stage II Da IIVinnyRevinaAdrianiAinda não há avaliações
- Manage Chronich Hep B-CDocumento4 páginasManage Chronich Hep B-CVinnyRevinaAdrianiAinda não há avaliações
- J 1751-7133 2010 00164 XDocumento4 páginasJ 1751-7133 2010 00164 XVinnyRevinaAdrianiAinda não há avaliações
- Small Incision Cataract Surgery (SICS)Documento2 páginasSmall Incision Cataract Surgery (SICS)Zaki AkbarAinda não há avaliações
- Hepatitis A WHODocumento41 páginasHepatitis A WHOLatira Lestiyani IIAinda não há avaliações
- 100720090108Documento4 páginas100720090108VinnyRevinaAdrianiAinda não há avaliações
- 139 FullDocumento6 páginas139 FullVinnyRevinaAdrianiAinda não há avaliações
- Manage Chronich Hep B-CDocumento4 páginasManage Chronich Hep B-CVinnyRevinaAdrianiAinda não há avaliações
- 06 Small Incision Cataract SurgeryDocumento21 páginas06 Small Incision Cataract SurgeryApriliani SanitiAinda não há avaliações
- An Update On The Management of Acute Pelvic Inflammatory DiseaseDocumento3 páginasAn Update On The Management of Acute Pelvic Inflammatory DiseaseVinnyRevinaAdrianiAinda não há avaliações
- Fungal Sinus 2012 01Documento7 páginasFungal Sinus 2012 01VinnyRevinaAdrianiAinda não há avaliações
- Allergic Fungal Sinusitis - CT FindingsDocumento6 páginasAllergic Fungal Sinusitis - CT Findingssomeone that you used to knowAinda não há avaliações
- Bio Essays 23Documento12 páginasBio Essays 23VinnyRevinaAdrianiAinda não há avaliações
- Narco LongsDocumento20 páginasNarco LongsVinnyRevinaAdrianiAinda não há avaliações
- Schizophrenia Booket 2009Documento22 páginasSchizophrenia Booket 2009Tracy100% (1)
- Alergic FungalDocumento4 páginasAlergic FungalVinnyRevinaAdrianiAinda não há avaliações
- Spinal Cord InjuryDocumento2 páginasSpinal Cord InjuryVinnyRevinaAdrianiAinda não há avaliações
- MethylprednisoloneDocumento7 páginasMethylprednisoloneVinnyRevinaAdrianiAinda não há avaliações
- Andreas C. Widjaja-01Documento9 páginasAndreas C. Widjaja-01Legina AdityaAinda não há avaliações
- 80 CleftLipDocumento2 páginas80 CleftLipVinnyRevinaAdrianiAinda não há avaliações
- AIIMS Mental Health Nursing Exam ReviewDocumento28 páginasAIIMS Mental Health Nursing Exam ReviewImraan KhanAinda não há avaliações
- Digital Transformation of Healthcare at Singapore's Juroaghealth ServiceDocumento3 páginasDigital Transformation of Healthcare at Singapore's Juroaghealth ServiceUsama TahirAinda não há avaliações
- Manajemen Pada ObesitasDocumento11 páginasManajemen Pada ObesitasahmadAinda não há avaliações
- International Conference on Victimology Detail ScheduleDocumento5 páginasInternational Conference on Victimology Detail ScheduleMarinda KardionoAinda não há avaliações
- Family Psychology QuestionnaireDocumento5 páginasFamily Psychology QuestionnairemuffinshuffleeffieAinda não há avaliações
- Crush Injury SlideDocumento73 páginasCrush Injury SlideChe HaniffAinda não há avaliações
- Ticket Report-23.05.2023 11-44Documento205 páginasTicket Report-23.05.2023 11-44Heamalatha Raja ManickamAinda não há avaliações
- Case Scenario 1 PDFDocumento11 páginasCase Scenario 1 PDFMariano MarbellaAinda não há avaliações
- Journal #4 (Sambuhay) : "Come and Celebrate With The Joy of Your Master."Documento2 páginasJournal #4 (Sambuhay) : "Come and Celebrate With The Joy of Your Master."Keanu PeraltaAinda não há avaliações
- LABORATORY SAFETY: A Self-Assessment Workbook - CHAPTERS 1 & 2Documento5 páginasLABORATORY SAFETY: A Self-Assessment Workbook - CHAPTERS 1 & 2PA2014Ainda não há avaliações
- David Epston Down Under 1 110Documento110 páginasDavid Epston Down Under 1 110Diego FajardoAinda não há avaliações
- Evs Assignment May 2018Documento4 páginasEvs Assignment May 2018sam_antony2005Ainda não há avaliações
- SRSG A 74 259 EnglishDocumento16 páginasSRSG A 74 259 EnglishsofiabloemAinda não há avaliações
- The Belly Fat Diet John ChathamDocumento92 páginasThe Belly Fat Diet John ChathamGurpreet Kaur100% (3)
- A Beginner Guide To Smart ContractsDocumento15 páginasA Beginner Guide To Smart ContractsMikeAinda não há avaliações
- Hypertension FinalDocumento24 páginasHypertension FinalFlorencio D. Santos IVAinda não há avaliações
- IELTS Writing Task 1 - Bài Mẫu IELTS FighterDocumento39 páginasIELTS Writing Task 1 - Bài Mẫu IELTS FighterThùyy VyAinda não há avaliações
- 1.application To Market A New DrugDocumento4 páginas1.application To Market A New DrugcardiacanesthesiaAinda não há avaliações
- Receiving Faculty Approval For The Following:: WWW - Aut.ac - Nz/health-AddendumDocumento2 páginasReceiving Faculty Approval For The Following:: WWW - Aut.ac - Nz/health-AddendumsajithzxAinda não há avaliações
- Chapter 3Documento3 páginasChapter 3Black PantherAinda não há avaliações
- MCC SaeDocumento98 páginasMCC SaeAllison100% (1)
- Candela Gentle Pro - 16026752105746Documento6 páginasCandela Gentle Pro - 16026752105746Andrea Mejia100% (1)
- Assessing and Managing Ineffective Tissue PerfusionDocumento1 páginaAssessing and Managing Ineffective Tissue PerfusionKryza CastilloAinda não há avaliações
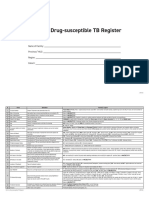
- Form 6a. Drug Susceptible TB RegisterDocumento4 páginasForm 6a. Drug Susceptible TB RegisterAllen ChesterAinda não há avaliações
- 2016 CHBC Titlte 8Documento38 páginas2016 CHBC Titlte 8Jing YAinda não há avaliações
- CHN-RLE Module 3 (Bag Technique)Documento5 páginasCHN-RLE Module 3 (Bag Technique)Ems Rio BalAinda não há avaliações
- Your NAET Information GuideDocumento8 páginasYour NAET Information GuideRicard Revuelto Orengo50% (2)
- Chapter 12 Social Welfare MeasuresDocumento44 páginasChapter 12 Social Welfare MeasuresChandan ChanduAinda não há avaliações
- Lesson345.67 PEH John Andrei AlcantaraDocumento15 páginasLesson345.67 PEH John Andrei AlcantaraMiguel, Nathaniel T.Ainda não há avaliações
- Manufacturer SDSDocumento10 páginasManufacturer SDSJack AultAinda não há avaliações