Escolar Documentos
Profissional Documentos
Cultura Documentos
Management of Liver Cirrhosis
Enviado por
pet_trinDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Management of Liver Cirrhosis
Enviado por
pet_trinDireitos autorais:
Formatos disponíveis
Prospective Management of Cirrhosis
Mamie H. Dong, MD, and Sammy Saab, MD, MPH, AGAF
Dr. Dong is a fellow in the Department of Gastroenterology at the University of California at San Diego. Dr. Saab is Associate Professor of Medicine and Surgery at the University of California at Los Angeles.
Abstract: An increasing number of patients are presenting with cirrhosis; thus, understanding and taking a prospective approach to their management is becoming essential. Cirrhosis is the final common pathway for many causes of chronic liver disease. Mortality rates dramatically increase when patients progress from compensated to decompensated cirrhosis. Close monitoring and early intervention is needed to delay this progression and improve survival once complications do arise. Patients should be monitored for clinical deterioration and worsening of laboratory values, and care should be taken to ensure adequate nutrition and avoidance of hepatotoxic medications. Susceptible patients may require immunization. Family members should be screened for contagious and inheritable causes of liver diseases, and screening for hepatic encephalopathy, varices, and hepatocellular carcinoma should be routinely performed. Prophylaxis against spontaneous bacterial peritonitis should be instituted in highrisk patients, and referral for liver transplantation should be made at the appropriate time.
Address correspondence to: Dr. Sammy Saab Pfleger Liver Institute UCLA Medical Center 200 Medical Plaza, Suite 214 Los Angeles, CA 90095; Tel: 310-206-6705; Fax: 310-206-4197; E-mail: ssaab@mednet.ucla.edu
Keywords Cirrhosis, prevention, screening
irrhosis is responsible for more than 27,000 deaths annually, making it the 12th leading cause of mortality in the United States.1 The most common causes of cirrhosis in the United States are alcoholic liver disease and chronic viral hepatitis. In the next decade, cirrhosis from fatty liver may emerge as one of the major indications for liver transplantation in this country. Cirrhosis represents a clinical spectrum in which patients are asymptomatic at one end and at the other end they have manifestations of hepatic decompensation, including variceal bleeding, ascites, hepatic encephalopathy, and hepatorenal syndrome. The results of a recent survey of practicing gastroenterologists in a major metropolitan city revealed variability in the adherence to established guidelines in the management of cirrhosis.2 Morbidity and mortality rates rise dramatically when complications of cirrhosis develop; thus, it is important for practitioners to take an active role in the prospective management of the cirrhotic patient rather than just manage complications when they arise.
Gastroenterology & Hepatology Volume 5, Issue 3 March 2009
191
DONG AND SAAB
Table 1. Child-Turcotte-Pugh Scoring System Variable 1 Encephalopathy (grade)* Ascites Bilirubin (mg/dL) For primary biliary cirrhosis: bilirubin (mg/dL) Albumin (g/dL) Prothrombin time (seconds prolonged) OR international normalized ratio None Absent 12 14 Points 2 12 Slight 23 410 3 34 Moderate >3 >10
Table 2. Model for End-Stage Liver Disease (MELD) Scoring System* MELD score = 3.78[Ln serum bilirubin (mg/dL)] + 11.2[Ln INR] + 9.57[Ln serum creatinine (mg/dL)] + 6.43
*The lower limit of all values is 1, and the upper limit of creatinine is 4. If the patient received dialysis at least twice in the last 7 days, the creatinine is entered as 4. INR=international normalized ratio.
>3.5 14 <1.7
2.83.5 46 1.72.3
<2.8 >6 >2.3
Reprinted from Murray KF, Carithers RL Jr.3 *See Table 3. Class A=56 points; Class B=79 points; Class C=1015 points.
and 2 qualitative variables (encephalopathy, ascites) to assign a score between 5 and 15 (Table 1). Patients with scores less than 7 (class A) have compensated cirrhosis, whereas those with scores of 7 or greater (class B/C) are considered decompensated. The MELD score utilizes only 3 quantitative variables (bilirubin, INR, creatinine) for a score between 6 and 40 (Table 2). Patients with MELD scores of 10 or greater are considered decompensated.3 Although the CTP and MELD have both been validated as acceptable predictors of mortality, neither correlates well with quality of life.4 Diet and Medication Considerations Maintaining adequate nutrition is important in patients with cirrhosis. Malnourishment has been shown to cause a higher rate of complications and is an independent predictor of mortality.5,6 Protein-calorie malnutrition is found in 6590% of patients with cirrhosis and almost 100% of candidates awaiting liver transplantation.7,8 Patients with cholestatic liver disease are subject to caloric depletion and deciencies in fat-soluble vitamins, whereas those with noncholestatic disease predominantly experience protein depletion.9 Although the utility of temporary protein restriction in patients with acute encephalopathy unresponsive to medications has been recently debated, it is well established that those with acute or chronic encephalopathy that can be managed with medications should not be protein-restricted. All patients with evidence of encephalopathy should be instructed to consume 45 small meals per day as well as a late evening snack for optimal nitrogen balance.10 Patients with cirrhosis are prone to specic nutrient deciencies. Decreased levels of vitamin A may lead to night blindness, which can be corrected with 25,000 units per day of vitamin A for 412 weeks.11,12 Persistent problems with vision in the dark may result from concomitant zinc deciency, which can be corrected with 600 mg per day of zinc for 3 months.11,13 Zinc deciency
Initial Assessment Once a diagnosis of cirrhosis is established, the focus should be to estimate the severity of hepatic injury. A comprehensive history and physical examination should note symptoms such as fatigue, pruritus, bleeding, and episodes of confusion or mood disturbances; review concurrent medical illnesses and medication use; and assess for ascites, splenomegaly, pedal edema, and asterixis. Initial laboratory studies should consist of a complete blood count (CBC) to check for anemia and thrombocytopenia; a comprehensive metabolic panel (CMP) to detect hyponatremia, renal insuciency, aminotransaminase levels, bilirubin, protein, and albumin; coagulation studies (prothrombin time [PT] and international normalized ratio [INR]) to assess liver synthetic function; and alphafetoprotein (AFP) to screen for hepatocellular carcinoma (HCC). An imaging study such as ultrasound should also be performed at baseline for future comparison and to screen for HCC as well as for ascites. Two widely used clinical staging methods for patients with cirrhosis are the Child-Turcotte-Pugh (CTP) system and the model for end-stage liver disease (MELD) system. The MELD has replaced the CTP system for allocation of organs for liver transplant because the former more accurately predicts mortality. The CTP system utilizes 3 quantitative variables (bilirubin, albumin, PT or INR)
192
Gastroenterology & Hepatology Volume 5, Issue 3 March 2009
MANAGEMENT OF CIRRHOSIS
has also been implicated in the pathogenesis of hepatic encephalopathy.13 Vitamin D and calcium deciencies may result in osteomalacia or osteoporosis, and patients should receive 800 IU per day of vitamin D3 and 1 g per day of calcium indenitely.14 Patients with ascites should adhere to a low-sodium diet (<2 g/day), but uid restriction is not necessary unless there is concomitant severe hyponatremia (serum sodium <120125 mEq/L).15 In patients with a poor clinical response, 24-hour urine sodium levels can be checked. If urinary sodium excretion is higher than the prescribed sodium intake, compliance with a low-salt diet should be questioned. Multiple case reports have described severe or fatal infections with the Vibrio species in patients with cirrhosis; thus, avoiding consumption of raw seafood is recommended.16,17 As the liver is a major site for drug metabolism, the use of any over-the-counter or prescription medications must be closely monitored. Nonsteroidal anti-inammatory drugs should be avoided, as they may predispose patients to bleeding (by inhibiting platelets) and renal failure (due to decreased renal prostaglandin production) and have been rarely reported to cause 10-fold increases in transaminase levels.18 Doses of acetaminophen should be restricted to 2 g per day.19 The use of other medications, particularly those that are metabolized by the cytochrome P450 system (eg, benzodiazepines, warfarin, morphine) should be carefully monitored. Screening of Family Members It is essential to screen for causes of liver disease that are transmissible or inherited. Screening and identication of at-risk family members may potentially lead to earlier diagnosis and intervention. Appropriate counseling should be oered prior to any screening procedures. Alpha-1-antitrypsin deciency is a genetic condition that can lead to early-onset emphysema and hepatic impairment. There is variability in the severity and age of onset, and early diagnosis allows individuals to make informed lifestyle decisions, particularly regarding smoking, which increases the risk of severe pulmonary manifestations. Currently, screening of family members is performed by assessing alpha-1-antitrypsin phenotype and levels.20 Hereditary hemochromatosis is an autosomal recessive inherited disorder of iron overload. Therapeutic phlebotomy, if instituted prior to the development of cirrhosis, can normalize life expectancy.21 Screening is recommended for all rst-degree relatives of aected individuals with genotype testing based upon the proband.22,23 Wilson disease is an autosomal recessive disorder of copper metabolism. Early treatment with copper chelators can slow or prevent multi-organ system failure, and
Table 3. West Haven Criteria for Semiquantitative Grading of Mental State Trivial lack of awareness Euphoria or anxiety Shortened attention span Impaired performance of addition Lethargy or apathy Minimal disorientation for time or place Subtle personality change Inappropriate behavior Impaired performance of subtraction
Grade 1
Grade 2
Grade 3
Somnolence to semistupor, but responsive to verbal stimuli Confusion Gross disorientation Coma (unresponsive to verbal or noxious stimuli)
Grade 4
Adapted from Ferenci P, et al.34
genetic screening of family members of aected individuals is recommended.24 The American Association for the Study of Liver Diseases (AASLD) recommends screening of all rst-degree relatives via liver function tests, CBC, ceruloplasmin level, 24-hour urine test for basal copper level, genotype testing based upon the identied proband, and slit-lamp examination for Kayser-Fleischer rings.25 Hepatitis C virus (HCV), although more commonly acquired through blood inoculation, may also be transmitted through sexual contact. Studies suggest that spouses of patients with HCV who have ongoing viremia are at increased risk and should be screened with HCV antibodies. Children of mothers with HCV should also be screened.26 Hepatitis B virus (HBV) can be transmitted sexually, horizontally, and vertically. Vertical transmission of HBV is an important etiology of chronic HBV infection leading to cirrhosis and HCC worldwide. Screening of all mothers, spouses, siblings, and children of aected individuals is recommended with serologic testing for hepatitis B surface antigen and hepatitis B core antibody.27 Susceptible patients should be vaccinated.28 Vaccination Recommendations All patients with cirrhosis who are not already immune should be vaccinated against hepatitis A, hepatitis B, pneumococcus, and inuenza. Although the risk of hepatitis A transmission is not higher among those with
Gastroenterology & Hepatology Volume 5, Issue 3 March 2009
193
DONG AND SAAB
cirrhosis than the general population, acute hepatitis A infection can lead to rapid clinical decompensation. The decision to test for immunity prior to vaccination should be based upon the likelihood of underlying immunity, as well as the costs of laboratory studies.29 No adverse events are associated with the vaccination of an individual who is already immune. The current recommendations are for 2 doses of vaccination 612 months apart. The response to the vaccination diers according to the degree of liver disease. Patients with advanced liver disease, as well as those with obesity, advanced age, and a history of smoking, have a signicantly decreased response rate to immunization. Postvaccination testing is currently not recommended,30 though it can be considered in this group. The Centers for Disease Control and Prevention recommend 3 doses of hepatitis B vaccination at 0, 1, and 6 months. Because of the decreased seroconversion rate in cirrhotic patients, some physicians have advocated using a higher vaccine dose.31 Pneumococcus vaccination is recommended for all patients with cirrhosis. Those patients over the age of 65 who received their rst dose before turning 65 should receive a second dose after 5 years. Patients who have concomitant HIV or chronic renal disease, are taking steroids, or have undergone liver transplantation should receive a second dose after 5 years regardless of age.32 Inuenza vaccination is recommended annually. Patients with cirrhosis should receive the inactivated inuenza vaccine rather than the live attenuated inuenza vaccine.33 Screening for Hepatic Encephalopathy Patients without overt hepatic encephalopathy (HE) may still have minimal encephalopathy (Table 3).34 Recent data show that minimal encephalopathy is common, and although the condition is subclinical, patients do have impairments in daily functioning and quality of life, and it may be unsafe for them to drive cars.35-37 There are currently no easily accessible methods for evaluating minimal encephalopathy. Some physicians have advocated a combination of psychometric tests (trail-making, block design, digit symbol) and neurophysiologic tests (brainstem auditory evoked potential, electroencephalography with mean dominant frequency).38 Patients with evidence of overt HE should be treated and advised not to operate motor vehicles. Screening and Management of Varices Esophageal varices are present in 30% of patients with compensated cirrhosis and 60% of patients with decompensated cirrhosis.39 Each episode of bleeding carries a 20% mortality rate.40 Untreated patients have a 70% rebleeding risk within 1 year.41 Varices are a direct con-
sequence of portal hypertension, and patients are at risk with portal pressures greater than 10 mmHg. The AASLD recommends classication of varices into 2 groups, small versus large, with 5 mm being the cuto size. All patients should undergo upper endoscopy screening when they are diagnosed with cirrhosis. The frequency of repeat endoscopies depends upon the presence or absence of decompensation and endoscopic ndings. Patients with small varices that show evidence of red wale signs (red marks or red spots) should be started on nonselective betablocker therapy. Those with small varices without red wale signs may also be treated with beta blockers, but the longterm benets are unclear and no formal recommendations have been made. If beta-blocker therapy is initiated, no further screening endoscopies are needed. If beta-blocker therapy is not used, screening should be continued every 23 years unless there is evidence of hepatic decompensation, at which point screening should be increased to yearly. Patients with large varices should be treated with nonselective beta blockers, and further screening can be discontinued. Those patients who are unable to tolerate beta blockers should undergo endoscopic variceal ligation (EVL) every 12 weeks until the varices are obliterated. A screening upper endoscopy should be performed 13 months afterwards, and then every 612 months thereafter for surveillance of variceal recurrence. Nitrates, either alone or in combination with beta blockers or EVL, surgical shunts, and sclerotherapy, should not be used as primary prophylaxis.42,43 Nonselective beta-blocker therapy can decrease overall upper gastrointestinal bleeding by 40%.44 The dose of beta blockers should be titrated up to produce a 25% reduction in the patients baseline heart rate, or until a resting heart rate of 5560 beats per minute is reached.45 Once patients have had an episode of variceal bleeding, further prophylaxis is warranted with nonselective beta-blocker therapy in addition to EVL. Repeat endoscopy should be performed 13 months after obliteration of varices and then every 612 months. Patients who are transplant candidates should be referred for liver transplantation evaluation at this time. Approximately 20% of patients will have recurrent bleeding or persistent bleeding despite rst-line therapy.46 In this patient population, portal decompression should be considered with either a transjugular intrahepatic portosystemic shunt (TIPS) or a surgical shunt. Patients who bleed from gastric varices can undergo gastric variceal obliteration using tissue adhesives such as cyanoacrylate or sclerotherapy with agents such as ethanol. However, these modalities are not US Food and Drug Administrationindicated and may not be readily available. TIPS is often used for refractory gastric variceal
194
Gastroenterology & Hepatology Volume 5, Issue 3 March 2009
MANAGEMENT OF CIRRHOSIS
Table 4. Frequency of Outpatient Screening Modality 3 Clinic visit Compensated Decompensated* Upper endoscopy No varices Compensated Decompensated Small varices Not on beta blockers On beta blockers Large varices Abdominal ultrasound Alpha-fetoprotein Laboratory work Compensated Decompensated X X X X No further screening No further screening X X X X X 6 Frequency (months) 12 24 36
*Decompensation is dened as a Child-Turcotte-Pugh score 7 (class B/C), model for end-stage liver disease score 10, or after the rst complication (variceal bleeding, ascites, hepatic encephalopathy, hepatorenal syndrome, hepatopulmonary syndrome). Complete metabolic panel, complete blood cell count, prothrombin time/international normalized ratio, albumin.
bleeding. Portal decompression is indicated for those patients who continue to bleed from gastric varices. Screening for Hepatocellular Carcinoma In patients with hepatitis C, the annual incidence of developing HCC is 1.4% in patients with compensated cirrhosis and 4% in patients with decompensated cirrhosis.47 The AASLD recommends routine screening of all individuals with cirrhosis with an ultrasound every 612 months.48 As the sensitivity and specicity of AFP in diagnosing HCC is low, it is generally agreed that AFP should not be used alone for screening purposes.48 Cost-eectiveness studies have demonstrated that the combination of AFP plus ultrasound every 6 months is the most cost-eective screening strategy.49 Prophylaxis for Spontaneous Bacterial Peritonitis Spontaneous bacterial peritonitis (SBP) is a frequent complication of ascites, seen in up to 30% of patients with ascites who are hospitalized for any reason.15,50 Both the
AASLD and the International Ascites Club recommend performing a diagnostic paracentesis when clinically apparent ascites is rst diagnosed.17,50 Ascites uid should be sent for cell count with dierential, total protein, and albumin. A concomitant serum albumin should be sent for calculation of the serum-ascites albumin gradient. Patients who have had a prior episode of SBP have a 1-year recurrence rate of 4070%.51 Clinical trials show that SBP prophylaxis reduces morbidity and mortality.52 Prophylactic treatments include 400 mg per day of noroxacin, 750 mg per week of ciprooxacin, or 160 mg per day of trimethoprim/sulfamethoxazole for at least 5 days each week. All cirrhotic patients who present with upper gastrointestinal bleeding are at high risk for developing SBP and should receive prophylactic antibiotics for 7 days. Validated regimens include noroxacin 400 mg orally twice daily, trimethoprim/sulfamethoxazole 160 mg orally twice daily, or ooxacin 400 mg intravenously once daily.15,50 High serum bilirubin (>2.5 mg/dL) and low ascites total protein (<1 g/dL) are also predictors of increased SBP. However, the use of primary prophylaxis in this group remains controversial.
195
Gastroenterology & Hepatology Volume 5, Issue 3 March 2009
DONG AND SAAB
Follow-Up Visits Patients with well-compensated cirrhosis can be followed every 6 months, whereas those with decompensated cirrhosis should be seen every 3 months. At each visit, patients should be assessed for signs of clinical deterioration, including the development of ascites or hepatic encephalopathy. All preventive measures should be reviewed and updated appropriately, and all medication lists should be reviewed. Laboratory studies, including CBC, CMP, PT/INR, and albumin should be checked at each visit, and MELD and/or CTP scores should be recalculated. Liver Transplantation Liver transplantation is the ultimate treatment for patients with complicated liver disease. Patients who are otherwise transplant candidates should be referred for evaluation when their MELD score reaches 10 or their CTP score reaches 7. However, for most patients, the 1-year survival benets outweigh the risks only when the MELD score is above 15.3 Other indications for referral are uncontrollable pruritus in cholestatic liver diseases, amyloidosis, development of type I hepatorenal syndrome, hepatopulmonary syndrome, or after the rst major complication (ascites, encephalopathy, variceal bleeding). Patients with HCC conned to the liver with a single lesion less than 5 cm in size or no more than 3 lesions all less than 3 cm who are not candidates for surgical resection should also be referred for transplant evaluation.3 Recently, there has been increasing enthusiasm for expanding the criteria by which patients with HCC are accepted as candidates for liver transplantation.53,54 Pretreatment viral load has important post-transplant prognostication. Both elevated hepatitis B and C viral levels predict early disease recurrence. Although antiviral therapy prior to liver transplant using oral nucleotides/ nucleosides is safe for hepatitis B, the use of interferon in patients with decompensated liver disease from hepatitis C is not routinely employed, as it can lead to further hepatic decompensation. If interferon therapy is contemplated in patients with any degree of hepatic decompensation, it should be administered by providers associated with a liver transplant center. Alternatively, liver transplant recipients can be treated for recurrent hepatitis C with interferon-based therapy. Prognosis The rate of transition from compensated to decompensated cirrhosis is approximately 57% each year, and median
survival for the former is more than 12 years compared to approximately 2 years for the latter.55 In a systematic review of 118 studies, DAmico and associates characterized 4 stages of cirrhosis.55 Stage 1 is dened by the absence of esophageal varices and ascites, and the mortality rate is low at 1% per year. Stage 2 is characterized by esophageal varices without bleeding and without ascites, and the mortality rate is 3.4% per year. Patients in stage 3 have ascites with or without varices, but without bleeding. Mortality in this group is 20% per year. Patients in stage 4 have gastrointestinal bleeding with or without ascites, and 1-year mortality for this group is 57%. Stages 1 and 2 correspond to compensated cirrhosis, whereas stages 3 and 4 are decompensated. Summary Cirrhosis is a complex disease entity with a spectrum of clinical manifestations. Mortality rates dramatically increase when patients develop decompensated disease. Close monitoring (Table 4) and early intervention by the vigilant practitioner can delay disease progression and improve survival. References
1. Kochanek KD, Murphy SL, Anderson RN, Scott C. Deaths: nal data for 2002. Natl Vital Stat Rep. 2004;53:1-115. 2. Saab S, Nguyen S, Ibrahim A, Vierling JM, Tong MJ. Management of patients with cirrhosis in southern California: results of a practitioner survey. J Clin Gastroenterol. 2006;40:156-161. 3. Murray KF, Carithers RL Jr. AASLD Practice Guidelines: Evaluation of the patient for liver transplantation. Hepatology. 2005;41:1407-1432. 4. Saab S, Ibrahim AB, Shpaner A, Younossi ZM, Lee C, et al. MELD fails to measure quality of life in liver transplant candidates. Liver Transpl. 2005;11: 218-223. 5. Alberino F, Gatta A, Amodio P, Merkel C, Di Pascoli L, et al. Nutrition and survival in patients with liver cirrhosis. Nutrition. 2001;17:445-450. 6. Caregaro L, Alberino F, Amodio P, Merkel C, Bolognesi M, et al. Malnutrition in alcoholic and virus-related cirrhosis. Am J Clin Nutr. 1996;63:602-609. 7. Lautz HU, Selberg O, Krber J, Brger M, Mller MJ. Protein-calorie malnutrition in liver cirrhosis. Clin Investig. 1992;70:478-486. 8. DiCecco SR, Wieners EJ, Wiesner RH, Southorn PA, Plevak DJ, Krom RA. Assessment of nutritional status in patients with end-stage liver disease undergoing liver transplantation. Mayo Clin Proc. 1989;64:95-102. 9. Zaina FE, Parolin MB, Lopes RW, Coelho JC. Prevalence of malnutrition in liver transplant candidates. Transplant Proc. 2004;36:923-925. 10. Swart GR, Zillikens MC, van Vuure JK, van den Berg JW. Eect of a late evening meal on nitrogen balance in patients with cirrhosis of the liver. BMJ. 1989;299:1202-1203. 11. Herlong HF, Russell RM, Maddrey WC. Vitamin A and zinc therapy in primary biliary cirrhosis. Hepatology. 1981;1:348-351. 12. Janczewska I, Ericzon BG, Eriksson LS. Inuence of orthotopic liver transplantation on serum vitamin A levels in patients with chronic liver disease. Scand J Gastroenterol. 1995;30:68-71. 13. Marchesini G, Fabbri A, Bianchi G, Brizi M, Zoli M. Zinc supplementation and amino acid-nitrogen metabolism in patients with advanced cirrhosis. Hepatology. 1996;23:1084-1092. 14. Collier JD, Ninkovic M, Compston JE. Guidelines on the management of osteoporosis associated with chronic liver disease. Gut. 2002;50:1-9. 15. Runyon BA. AASLD Practice Guidelines: Management of adult patients with ascites due to cirrhosis. Hepatology. 2004;39:841-856.
196
Gastroenterology & Hepatology Volume 5, Issue 3 March 2009
MANAGEMENT OF CIRRHOSIS
16. Chen Y, Satoh T, Tokunaga O. Vibrio vulnicus infection in patients with liver disease: report of ve autopsy cases. Virchows Arch. 2002;441:88-92. 17. Rodrguez Ramos C, Garca Martos P, Galn Snchez F, Soria de la Cruz MJ, Martn Herrera L. Spontaneous non-O1 Vibrio cholerae peritonitis after raw oyster ingestion in a patient with cirrhosis. Eur J Clin Microbiol Infect Dis. 1998;17:362-363. 18. Carson JL, Willett LR. Toxicity of nonsteroidal anti-inammatory drugs: an overview of the epidemiological evidence. Drugs. 1993;46:243-248. 19. Riley TR, Smith JP. Preventive care in chronic liver disease. J Gen Intern Med. 1999;14:699-704. 20. Strange C, Dickson R, Carter C, Carpenter MJ, Holladay B, et al. Genetic testing for alpha1-antitrypsin deciency. Genet Med. 2004;6:204-210. 21. ONeil J, Powell L. Clinical aspects of hemochromatosis. Semin Liver Dis. 2005;25:381-391. 22. Ombiga J, Adams LA, Tang K, Trinder D, Olynyk JK. Screening for HFE and iron overload. Semin Liver Dis. 2005;25:402-410. 23. Tavill AS. AASLD Practice Guidelines: Diagnosis and management of hemochromatosis. Hepatology. 2001;33:1321-1328. 24. Langner C, Denk H. Wilson disease. Virchow Arch. 2004;445:111-118. 25. Roberts EA, Schilsky ML. AASLD Practice Guideline: A practice guideline on Wilson disease. Hepatology. 2003;37:1475-1492. 26. Strader DB, Wright T, Thomas DL, See LB. AASLD Practice Guidelines: Diagnosis, management, and treatment of hepatitis C. Hepatology. 2004;39: 1147-1171. 27. Chakravarty R, Chowdhury A, Chaudhuri S, Santra A, Neogi M, et al. Hepatitis B infection in Eastern Indian families: need for screening of adult siblings and mothers of adult index cases. Public Health. 2005;119:647-654. 28. Lok ASF, McMahon BJ. AASLD Practice Guidelines: Chronic hepatitis B. Hepatology. 2007;45:507-539. 29. Saab S, Martin P, Yee HF Jr. A simple cost-decision analysis model comparing two strategies for hepatitis A vaccination. Am J Med. 2000;109:241-244. 30. Fiore AE, Wasley A, Bell BP. Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2006;55(RR-7):1-23. 31. Keee EB. Acute hepatitis A and B in patients with chronic liver disease: prevention through vaccination. Am J Med. 2005;118:21S-27S. 32. Prevention of pneumococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1997; 46(RR-8):1-24. 33. Fiore AE, Shay DK, Haber P, Iskander JK, Uyeki TM, et al. Prevention and control of inuenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2007;56(RR-6):1-54. 34. Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT. Hepatic encephalopathydenition, nomenclature, diagnosis, and quantication: nal report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716-721. 35. Groeneweg M, Quero JC, De Bruijn I, Hartmann IJ, Essink-bot ML, et al. Subclinical hepatic encephalopathy impairs daily functioning. Hepatology. 1998;28:45-49. 36. Bajaj JS, Hafeezullah M, Homann RG, Varma RR, Franco J, et al. Navigation skill impairment: Another dimension of the driving diculties in minimal hepatic encephalopathy. Hepatology. 2008;47:596-604.
37. Bajaj JS, Hafeezullah M, Homann RG, Saeian K. Minimal hepatic encephalopathy: a vehicle for accidents and trac violations. Am J Gastroenterol. 2007;102:1903-1909. 38. Kharbanda PS, Saraswat VA, Dhiman RK. Minimal hepatic encephalopathy: diagnosis by neuropsychological and neurophysiologic methods. Indian J Gastroenterol. 2003;22(Suppl 2):S37-S41. 39. DAmico G, Pagliaro L, Bosch J. The treatment of portal hypertension: a meta-analytic review. Hepatology. 1995;22:332-354. 40. McCormick PA, OKeefe C. Improving prognosis following a rst variceal hemorrhage over four decades. Gut. 2001;49:682-685. 41. Graham DY, Smith JL. The course of patients after variceal hemorrhage. Gastroenterology. 1981;80:800-809. 42. Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922-938. 43. de Francis R. Evolving consensus in portal hypertension: report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2005;43:167-176. 44. Lowe RC, Grace ND. Primary prophylaxis of variceal hemorrhage. Clin Liver Dis. 2001;5:665-676. 45. Poynard T, Cals P, Pasta L, Ideo G, Pascal JP, et al. Beta-adrenergic-antagonist drugs in the prevention of gastrointestinal bleeding in patients with cirrhosis and esophageal varices: an analysis of data and prognostic factors in 589 patients from four randomized clinical trials. N Engl J Med. 1991;324:1532-1538. 46. Henderson JM. Surgery versus transjugular intrahepatic portal systemic shunt in the treatment of severe variceal bleeding. Clin Liver Dis. 2006;10:599-612. 47. Fattovich G, Giustina G, Degos F, Tremolada F, Diodati G, et al. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology. 1997;112:463-472. 48. Bruix J, Sherman M. AASLD Practice Guidelines: Management of hepatocellular carcinoma. Hepatology. 2005;42:1208-1236. 49. Saab S, Ly D, Nieto J, Kanwal F, Lu D, et al. Hepatocellular carcinoma screening in patients waiting for liver transplantation: a decision analytic model. Liver Transpl. 2003;9:672-681. 50. Rimola A, Garca-Tsao G, Navasa M, Piddock LJ, Planas R, et al. Diagnosis, treatment, and prophylaxis of spontaneous bacterial peritonitis: a consensus document. International Ascites Club. J Hepatol. 2000;32:142-153. 51. Tit L, Rimola A, Gins P, Llach J, Arroyo V, Rods J. Recurrence of spontaneous bacterial peritonitis: frequency and predictive factors. Hepatology. 1988;8:27-31. 52. Fernndez J, Navasa M, Planas R, Montoliu S, Monfort D, et al. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology. 2007;133:818-824. 53. Lee HS. Liver transplantation for hepatocellular carcinoma beyond the Milan criteria: the controversies continue. Dig Dis. 2007;25:296-298. 54. Duy JP, Vardanian A, Benjamin E, Watson M, Farmer DG, et al. Liver transplantation criteria for hepatocellular carcinoma should be expanded: a 22-year experience with 467 patients at UCLA. Ann Surg. 2007;246:502-509. 55. DAmico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-231.
Gastroenterology & Hepatology Volume 5, Issue 3 March 2009
197
Você também pode gostar
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesNo EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesAinda não há avaliações
- Case Study On Alcoholic Liver DiseaseDocumento20 páginasCase Study On Alcoholic Liver DiseaseHomework PingAinda não há avaliações
- Cholecystitis And Gallstones, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandCholecystitis And Gallstones, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNota: 5 de 5 estrelas5/5 (1)
- Anatomy & PhysiologyDocumento9 páginasAnatomy & Physiologyrachael80% (5)
- Gastrointestinal Bleeding, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandGastrointestinal Bleeding, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- NCLEX GI Disorders Practice QuizDocumento251 páginasNCLEX GI Disorders Practice QuizLilis Suryani100% (1)
- By: Leila Floresca Esteban BSNIII-BDocumento38 páginasBy: Leila Floresca Esteban BSNIII-BMonica Morales100% (2)
- ST - Lukes Casepress.Documento31 páginasST - Lukes Casepress.Justin EduardoAinda não há avaliações
- Pathology of Alcoholic Liver DiseaseDocumento7 páginasPathology of Alcoholic Liver DiseasehghAinda não há avaliações
- Renal Case Study Final1Documento41 páginasRenal Case Study Final1api-202881815100% (1)
- Liver Cirrhosis CaseDocumento8 páginasLiver Cirrhosis Casemarlx5Ainda não há avaliações
- Hypertension Case StudyDocumento2 páginasHypertension Case Studyapi-344630051Ainda não há avaliações
- Treatment of Liver CirrhosisDocumento85 páginasTreatment of Liver CirrhosisPetru Boaghi100% (1)
- Chaffin - Diverticulosis Case StudyDocumento24 páginasChaffin - Diverticulosis Case StudymollychaffinAinda não há avaliações
- Hepatomegaly 1Documento5 páginasHepatomegaly 1Bobby ParksAinda não há avaliações
- Liver Cirrhosis Patient Case StudyDocumento6 páginasLiver Cirrhosis Patient Case StudyAngelica Barcelona Yumang67% (3)
- Case StudyDocumento5 páginasCase Studyapi-247850107Ainda não há avaliações
- Liver Cirrhosis: Causes, Symptoms, and TreatmentDocumento20 páginasLiver Cirrhosis: Causes, Symptoms, and TreatmentFate ZephyrAinda não há avaliações
- Alcoholic Liver DiseaseDocumento5 páginasAlcoholic Liver Diseaseamt12202Ainda não há avaliações
- Liver Cirrhosis: By: Bandna Kumari M.SC (N) 1 YRDocumento66 páginasLiver Cirrhosis: By: Bandna Kumari M.SC (N) 1 YRrSAinda não há avaliações
- Assessment 2 - Nursing Case Study - 2019Documento2 páginasAssessment 2 - Nursing Case Study - 2019Chinney ArceAinda não há avaliações
- Liver CirrhosisDocumento6 páginasLiver CirrhosisBaharudin WahyuAinda não há avaliações
- Assessment and Management of Patients With Biliary DisordersDocumento26 páginasAssessment and Management of Patients With Biliary DisordersBav VAansoqnuaetz100% (1)
- Chirosis HepaticDocumento8 páginasChirosis HepaticCikalHrAinda não há avaliações
- Cirrhosis of The Liver: Handout and Information SheetDocumento3 páginasCirrhosis of The Liver: Handout and Information SheetRobert G. Gish, MDAinda não há avaliações
- Liver CirrhosisDocumento31 páginasLiver CirrhosisMarisol Jane Jomaya50% (2)
- Case Study Cirrhosis of The LiverDocumento35 páginasCase Study Cirrhosis of The Liverapi-24237671967% (3)
- Case 16 Pediatric t1dmDocumento12 páginasCase 16 Pediatric t1dmapi-501730091Ainda não há avaliações
- Nursing Management Pancreatic CancerDocumento2 páginasNursing Management Pancreatic CancerKit NameKo100% (2)
- Case Study FinalDocumento77 páginasCase Study FinalMacey Malonzo100% (1)
- Nutrition in Chronic Liver Disease: Clinical Practice GuidelinesDocumento37 páginasNutrition in Chronic Liver Disease: Clinical Practice GuidelinesCarla BustiosAinda não há avaliações
- Liver Anatomy and PhysiologyDocumento8 páginasLiver Anatomy and PhysiologyZzzemajAinda não há avaliações
- Pathophysiology of GERD and Its ComplicationDocumento25 páginasPathophysiology of GERD and Its ComplicationalmiraAinda não há avaliações
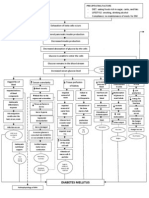
- Pa Tho Physiology of Diabetes MellitusDocumento3 páginasPa Tho Physiology of Diabetes MellitusPong's Teodoro SalvadorAinda não há avaliações
- Intro-ESRD Case StudyDocumento2 páginasIntro-ESRD Case StudyAngel SamonteAinda não há avaliações
- Management of Patients With Gastric and Duodenal DisordersDocumento47 páginasManagement of Patients With Gastric and Duodenal DisordersJor GarciaAinda não há avaliações
- Liver CirrhosisDocumento5 páginasLiver CirrhosisRLLTAinda não há avaliações
- Irritable Bowel SyndromeDocumento22 páginasIrritable Bowel SyndromeMarium NabeelAinda não há avaliações
- Portal Hypertension in Adults - UpToDateDocumento12 páginasPortal Hypertension in Adults - UpToDateyessyAinda não há avaliações
- KNH 411 - Case Study 22Documento17 páginasKNH 411 - Case Study 22api-301118772100% (3)
- Renal TransplantationDocumento33 páginasRenal TransplantationRohini Rai100% (1)
- Case Study For Chronic Renal FailureDocumento6 páginasCase Study For Chronic Renal FailureGabbii CincoAinda não há avaliações
- Liver CirrhosisDocumento76 páginasLiver Cirrhosiskathy100% (2)
- Esrd FinalDocumento26 páginasEsrd FinalCreighton A. BayonganAinda não há avaliações
- Pathophysiology of Alcoholic Liver DiseaseDocumento4 páginasPathophysiology of Alcoholic Liver Diseaseshailendra tripathiAinda não há avaliações
- IA. Background of The StudyDocumento49 páginasIA. Background of The Studyraffakervin50% (2)
- Chronic Renal FailureDocumento37 páginasChronic Renal Failuredorkiebaby100% (10)
- Medical Nutrition Therapy For Hemodialysis PatientsDocumento24 páginasMedical Nutrition Therapy For Hemodialysis Patientsraquelt_65Ainda não há avaliações
- Liver Cirrhosis - NCPDocumento18 páginasLiver Cirrhosis - NCPIshmael Solamillo83% (6)
- ConstipationDocumento5 páginasConstipationNader SmadiAinda não há avaliações
- Pancretic Cancer Case Study - BurkeDocumento52 páginasPancretic Cancer Case Study - Burkeapi-282999254Ainda não há avaliações
- Case StudyDocumento12 páginasCase Studyapi-242211536100% (1)
- Liver Cirrhosis Pathophysiology and EvaluationDocumento91 páginasLiver Cirrhosis Pathophysiology and EvaluationGiorgi PopiashviliAinda não há avaliações
- Liver Cirrhosis Care PlanDocumento3 páginasLiver Cirrhosis Care PlanWendy EscalanteAinda não há avaliações
- Acute Liver Failure in ChildrenDocumento34 páginasAcute Liver Failure in ChildrenEpahAinda não há avaliações
- Nutr 409 Case Study 12Documento5 páginasNutr 409 Case Study 12api-314354953100% (2)
- Clinical Paper Liver CirrhosisDocumento65 páginasClinical Paper Liver CirrhosisNeølie Abello LatúrnasAinda não há avaliações
- UROLITHIASISDocumento84 páginasUROLITHIASISJheanAlphonsineT.MeansAinda não há avaliações
- Diabetic Emergencies Case StudiesDocumento32 páginasDiabetic Emergencies Case StudiesLamria Maloni Siahaan0% (1)
- Nursing Care of Patients With Diabetes MellitusDocumento11 páginasNursing Care of Patients With Diabetes MellitusMarcus, RN100% (32)
- Kandungan Mangosten AllDocumento8 páginasKandungan Mangosten Allpet_trinAinda não há avaliações
- Fac Sheet About ScabiesDocumento6 páginasFac Sheet About Scabiespet_trinAinda não há avaliações
- Hubungan Antara Hygiene Perorangan Dan Lingkungan Dengan Kejadian PiodermaDocumento7 páginasHubungan Antara Hygiene Perorangan Dan Lingkungan Dengan Kejadian Piodermacute_chooeyAinda não há avaliações
- Kesling 2 1 02Documento9 páginasKesling 2 1 02Vidqha VioletAinda não há avaliações
- SCABIESDocumento3 páginasSCABIESNabilah Rashid RedzaAinda não há avaliações
- Perilaku Santri DLM Upaya PNCGHN Peny Skabies D Ponpes YogyaDocumento0 páginaPerilaku Santri DLM Upaya PNCGHN Peny Skabies D Ponpes Yogyapet_trinAinda não há avaliações
- SCABIESDocumento3 páginasSCABIESNabilah Rashid RedzaAinda não há avaliações
- Scabies Management: Community Control of ScabiesDocumento3 páginasScabies Management: Community Control of Scabiespet_trinAinda não há avaliações
- Prevention and Control of ScabiesDocumento20 páginasPrevention and Control of Scabiespet_trinAinda não há avaliações
- Kode Gigi BpjsDocumento4 páginasKode Gigi Bpjskurnia s100% (1)
- Organ Transplantatio1Documento26 páginasOrgan Transplantatio1Bindashboy0Ainda não há avaliações
- Managing Fatigue During PregnancyDocumento2 páginasManaging Fatigue During PregnancyBlanz Irybelle KindomAinda não há avaliações
- Fundamentals of Nursing10-19Documento19 páginasFundamentals of Nursing10-19escolarAinda não há avaliações
- The Hair Bible A Complete Guide To Health and Care PDFDocumento205 páginasThe Hair Bible A Complete Guide To Health and Care PDFDaniel Drop100% (1)
- Bulimia NervosaDocumento17 páginasBulimia NervosaJheanAlphonsineT.Means100% (1)
- ICU One Pager Enteral NutritionDocumento1 páginaICU One Pager Enteral NutritionjalilAinda não há avaliações
- Med Surg Nurse Brain SheetDocumento2 páginasMed Surg Nurse Brain SheetJan Marcus95% (20)
- E PortfolioDocumento3 páginasE Portfolioapi-337945337Ainda não há avaliações
- Hand When You Need Them MostDocumento9 páginasHand When You Need Them MostJim SchotterAinda não há avaliações
- Target Client List For NCD Prevention and Control SERVICES (Part 1)Documento9 páginasTarget Client List For NCD Prevention and Control SERVICES (Part 1)Lchg KrvyAinda não há avaliações
- 10.6 Health Issues Related To The Human Circulatory SystemDocumento7 páginas10.6 Health Issues Related To The Human Circulatory SystemrynAinda não há avaliações
- Dr. Nicole Carreau Joins New York Cancer and Blood Specialists' Central Park Oncology TeamDocumento2 páginasDr. Nicole Carreau Joins New York Cancer and Blood Specialists' Central Park Oncology TeamPR.comAinda não há avaliações
- Soal Tes TOEFL Dan Pembahasan Jawaban Written Expression (Complete Test 2 by Longman)Documento23 páginasSoal Tes TOEFL Dan Pembahasan Jawaban Written Expression (Complete Test 2 by Longman)Prakoso JatiAinda não há avaliações
- Comp ReviewDocumento99 páginasComp ReviewTHAO DANGAinda não há avaliações
- PEGS CatalogDocumento88 páginasPEGS CatalogMAinda não há avaliações
- The Impact of Life Cycles on Family HealthDocumento27 páginasThe Impact of Life Cycles on Family Healthmarcial_745578124Ainda não há avaliações
- Pathophysiology of Respiratory Diseases: Obstructed AlveoliDocumento3 páginasPathophysiology of Respiratory Diseases: Obstructed AlveoliApril Dianne ParungaoAinda não há avaliações
- Cellular Detox Smoothies PDFDocumento20 páginasCellular Detox Smoothies PDFRuth Engelthaler100% (2)
- Jurnal DMDocumento13 páginasJurnal DMidaAinda não há avaliações
- Krok 2 - 2021 - 26 JulyDocumento19 páginasKrok 2 - 2021 - 26 JulyNicole VinnikAinda não há avaliações
- Budwig Cancer GuideDocumento116 páginasBudwig Cancer GuideStanley ChanAinda não há avaliações
- How Can Women Make The RulesDocumento0 páginaHow Can Women Make The Ruleshme_s100% (2)
- Reducing Waste in ICUDocumento10 páginasReducing Waste in ICUzorbini69Ainda não há avaliações
- Oman New Health Application FormDocumento3 páginasOman New Health Application FormAravind AlavantharAinda não há avaliações
- Approach To The Jaundiced Cat - WSAVA 2015 Congress - VINDocumento6 páginasApproach To The Jaundiced Cat - WSAVA 2015 Congress - VINdmantsioAinda não há avaliações
- Slides 6 - ObturationDocumento22 páginasSlides 6 - Obturationبراءة أحمد السلاماتAinda não há avaliações
- Nat Ag Winter Wheat in N Europe by Marc BonfilsDocumento5 páginasNat Ag Winter Wheat in N Europe by Marc BonfilsOrto di CartaAinda não há avaliações
- - - - - شاهينDocumento101 páginas- - - - شاهينDdsa FaaaAinda não há avaliações
- Homeoapthy For InfantsDocumento9 páginasHomeoapthy For Infantspavani_upAinda não há avaliações
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNo EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNota: 4.5 de 5 estrelas4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesNo EverandThe Ultimate Guide To Memory Improvement TechniquesNota: 5 de 5 estrelas5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementNo EverandTechniques Exercises And Tricks For Memory ImprovementNota: 4.5 de 5 estrelas4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 3.5 de 5 estrelas3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeAinda não há avaliações
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 5 de 5 estrelas5/5 (78)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNo EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNota: 4 de 5 estrelas4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 3.5 de 5 estrelas3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsAinda não há avaliações
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 5 de 5 estrelas5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingNo EverandThe Happiness Trap: How to Stop Struggling and Start LivingNota: 4 de 5 estrelas4/5 (1)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingNo EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingNota: 5 de 5 estrelas5/5 (4)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingNo EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingNota: 3.5 de 5 estrelas3.5/5 (31)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNo EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNota: 4.5 de 5 estrelas4.5/5 (169)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsAinda não há avaliações
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (41)
- The Tennis Partner: A Doctor's Story of Friendship and LossNo EverandThe Tennis Partner: A Doctor's Story of Friendship and LossNota: 4.5 de 5 estrelas4.5/5 (4)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisNo EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisNota: 5 de 5 estrelas5/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisNo EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisNota: 5 de 5 estrelas5/5 (8)