Escolar Documentos
Profissional Documentos
Cultura Documentos
563421.v1 Perio
Enviado por
ikeuchi_ogawaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
563421.v1 Perio
Enviado por
ikeuchi_ogawaDireitos autorais:
Formatos disponíveis
Gingival recession: review and strategies in treatment of recession: 3 Case reports Dr. Koppolu Pradeep* Dr.
Palaparthy Rajababu Dr. Durvasula Satyanarayana Dr. Vidya Sagar
*Dept of periodontics, Sri Sai College of dental surgery, Vikarabad. drpradeepk08@gmail.com Dept of periodontics, Kamineni institute of dental sciences, Narketpally. Dept of periodontics, Kamineni institute of dental sciences, Narketpally. satyanarayana_d@yahoo.com Dept of periodontics, Kamineni institute of dental sciences, Narketpally. drsagarperio@gmail.com
Correspondence: Dr .Pradeep.K Dept of periodontics Sri Sai College of dental surgery Andhra Pradesh India drpradeepk08@gmail.com
Word count : 1665
Number of figures : 17 Running title : Strategies in treatment of gingival recession
One-sentence summary describing the key finding(s) .
The present report suggests that the selection of suitable procedure, specific and meticulous surgical technique will provide successful and exceedingly predictable results in the management of gingival recession.
Abstract One of the most common esthetic concerns associated with the periodontal tissues is gingival recession. Gingival recession is the exposure of root surfaces due to apical migration of the gingival tissue margins; gingival margin migrates apical to the cementoenamel junction. Although it rarely results in tooth loss, marginal tissue recession is associated with thermal and tactile sensitivity, esthetic complaints, and a tendency toward root caries. This article reviews etiology, consequences and the available surgical procedures for the coverage of exposed root surfaces, including three case reports. Key words: Recession, Cementoenamel Junction, Aesthetics, Graft
INTRODUCTION Gingival recession is a problem affecting almost all middle and older aged to some degree. Gingival recession is the diagnosis if the gingival margin migrates apical to the cementoenamel junction (CEJ). The distance between the CEJ and gingival margin gives the level of recession. Gingival recession can be caused by periodontal disease, accumulations, inflammation, improper flossing, aggressive tooth brushing, incorrect occlusal relationships, and dominant roots. These can appear as localized or generalized gingival recession. Recession can occur with or without loss of attached tissue. Gingival recession may result in accentuated sensitivity beca use the dentin is exposed, it can be assessed by an appearance of a long clinical tooth and varied proportion of the teeth relative to adjacent teeth.
PREVALENCE According to the US National Survey, 88% of seniors (age 65 and over) and 50% of adults (18 to 64) present recession in one or more sites; progressive increase in frequency and extent of recession is observed with increase in age [1]. In the youngest age cohort (30 to 39 years), the prevalence of recession was 37.8% and the extent averaged 8.6% teeth. In contrast, the oldest cohort, aged 80 to 90 years, had a prevalence of 90.4% (more than twice as high) and the extent averaged 56.3% teeth (more than six times as large) [2].
Gingival recession is associated with the presence of supragingival and subgingival calculus and showed that the lingual surfaces of the lower anterior teeth were most commonly affected in 2034 year age group in Tanzanian adult population [3].
ETIOLOGY 1) Calculus Association between gingival recession with supragingival and subgingival calculus can be noted because of inadequate access to prophylactic dental care. [3] 2) Tooth brushing Khocht et al showed that use of hard tooth brush was associated with recession [4]. 3) High frenal attachment This may impede plaque removal by causing pull on the marginal gingival [5]. 4) Position of the tooth Tooth which erupts close to mucogingival line may show localised gingival recession as there may be very little or no keratinized tissue [6]. 5) Tooth movement by orthodontic forces The movement of tooth such as excessive proclination of incisors and expansion of the arch expansion are associated with greater risk of gingival recession [7]. 6) Improperly designed partial dentures The partial dentures which have been maintained or designed which cause the gingival trauma and aid in the plaque retention have the tendency to cause gingival recession [8]. 7) Smoking The people who smoke have more gingival recession than non smokers. The recession sites were found buccal surfaces of maxillary molars premolars, mandibular central incisors and premolars [9]. 8) Restorations Subgingival restoration margins increase the plaque accumulation, gingival inflammation and alveolar bone loss [10].
9) Chemicals Topical cocaine application causes gingival ulcerations and erosions [11].
CONSEQUENCES
1) Aesthetics The appearance of tooth becomes unattractive [16]. 2) Gingival bleeding and plaque retention The recession may be a site clinically which offers plaque retention. 3) Hypersensitivity Recession will uncover the cervical dentine. Hypersensitivity is usually of a sharp and short duration often associated with cold stimulus. The mechanism of hypersensitivity that is accepted is the hydrodynamic theory of pain, which states that the movement of dental fluid in the dentinal tubules triggers sensory nerve fibers in the inner dentine and dentinopulpal junction [17].
4) Caries There may be a risk of the development of root caries as root surfaces are exposed to oral environment and aid in the withholding of plaque. Patients on periodontal maintenance with an average of 64.7 exposed root surfaces per patient, the mean number of caries lesions which were detected were 4.3 in a prevalence study [18].
TREATMENT 1) Restorations, crowns and veneers Crowns may be placed to widen the clinical crown which may camouflage the exposed root surface 2) Construction of gingival mask Patients who have several teeth with recession may have unaesthetic appearance because of black triangles. In these cases where surgical procedure is not appropriate silicone flexible gingival veneer or mask may be used. 3) Root conditioning Application of tetracycline HCL or citric acid to root surface before placement of soft tissue graft. 4) Frenectomy When the recession is caused by frenal pull in those cases frenectomy is advised. If appropriate hygiene aids does not enable the patient to maintain the area plaque free then frenectomy is advised to give ease to entrance to the site [19].
5) Surgical root coverage techniques
Free epithelialised gingival graft [20]. Subepithelial connective tissue graft [21]. Semilunar flap [22]. Coronally advanced flap [23]. Guided tissue regeneration [GTR] [24].
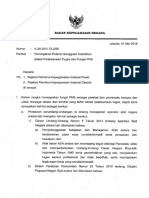
Case report 1 A 43 old female patient complained of hypersensitivity inspite of using anti hypersensitivity paste since 2 months and was also concerned about the esthetics. Patient had gingival recession on the maxillary left canine and first premolar at the first examination (fig 1). The recession measured 2 mm on the canine and 3 mm on the first premolar, respectively. The clinical attachment loss was 4 mm from the CEJ for the canine and 5 mm for the first premolar, respectively. Oral prophylaxis has been done and oral hygiene instructions were given so as to achieve satisfactory plaque control prior to periodontal surgery. After reevaluation a Semilunar incision and intracrevicular incisions have been given using Tarnow technique22 (fig 2). The roots were planed with hand curettes to remove the flecks of the calculus and to obtain smooth surfaces and then treated with tetracycline for 3 minutes (using a burnishing technique) (fig3). The root surfaces were then rinsed with saline. The flap was positioned as coronally as possible. The post operative healing after 2 months revealed an increase in 2mm of increase root coverage was achieved (fig 5).
Fig 1 Facial view of gingival recession on 1st premolar and canine. The patient complained of root sensitivity in addition to the unaesthetic appearance when smiling.
Fig 2 Semilunar incision placed apically
Fig 3 Root conditioning with tetracycline
Fig 4 Coronally repositioned flap
Fig 5 One -year postoperative view. Complete root coverage is observed.
Case 2 A 31 old female patient complained of a black triangle in the upper front teeth region since 6 months and was concerned about the esthetics and whistling sound while speaking (fig 6). The interdental papilla between maxillary right central and lateral incisor was blunt (fig 6). Oral prophylaxis has been done and oral hygiene instructions were given so as to achieve satisfactory plaque control prior to surgery. An intrasulcular incision is made at the tooth surfaces facing the interdental area to be reconstructed(fig7), consequently an incision is placed across the facial aspect of the interdental area and an envelope-type, split- thickness flap is elevated simultaneously a Semilunar incision was given apical to the mucogingival junction and the flap was coronally displaced using Langers technique. A connective tissue graft is harvested from palate (fig8) and placed under the flap in interdental area (fig 9) and sutured back (fig 10). Fig 11 post operative healing after 6 months revealed the excellent closure of black triangle between the left upper central and lateral incisors.
Fig 6 Blunting of interdental papilla between central and lateral incisor
Fig 7 Intrasulcular incision
Fig 8 Connective tissue graft taken from palate
Fig 9 Graft placement under the flap
Fig 10 Placement of suture
Fig 11 Closure of interdental papilla 6 months Post operative
Case 3 A 25 old female patient complained of hypersensitivity in the lower front teeth region since 2 months and was concerned about the esthetics. Patient had gingival recession on the mandibular right central incisor at the first examination (fig 12). The clinical attachment loss was 5 mm from the CEJ. Oral prophylaxis has been done and oral hygiene instructions were given so as to achieve satisfactory plaque control prior to periodonta l surgery. The root surface was gently scaled and planed; instrumentation was done by utilizing manual and power driven scalers and curets. The shape of the root was not altered. The root surface was then treated with a tetracycline 500 mg by attempting to burnish, with small cotton pledgets. The donor tissue was removed from the palate and trimmed to a thickness of 2 to 3 mm (fig 15). Within minutes of removal, the donor tissue was placed at the recipient site. Vertical stabilizing sutures (4-0 silk) were used to secure the graft (fig 16). Post operative (fig 17) after 6 months.
Fig 12 recession of right central incisor
Fig 13 Incisions for the removal of graft
Fig 14 Palate after removal of the graft
Fig 15 The donor tissue
Fig 16 Suturing
Fig 17 Six months postoperative healing
Discussion The main goal of periodontal therapy is to improve periodontal health and thereby to maintain a patients functional dentition right through his/her life. However, aesthetics symbolize an inseparable part of todays oral therapy, and numerous procedures have been proposed to
preserve or enhance patient aesthetics. This treatment has principally been justified by the patients wish to advance the aesthetic appearance when there is an exposed root. Etiology and the contributing factors are chief when deciding on appropriate treatment procedures for patients with localized gingival recession. In the cases presented, the etiologies of the gingival recession were scarce vestibular depth and inadequate width of keratinized gingiva. If malposition of teeth is supposed to be the etiology for recession then orthodontic t reatment needs to be given a thought with or without periodontal therapy. Due to the existence of multiple mucogingival problems, it was decided to use a free gingival graft to accomplish root coverage and to form functional attached gingiva. The band of keratinized tissue was determined to be adequate in all cases. The color match and the tissue contour were satisfactory to the patients in all cases mentioned above. In some cases the color match and tissue contour match were good enough to make it complex to determine the position of the original defect. The outcome of the current cases conrm aesthetics as the primary indication for root coverage. A recent survey showing that aesthetic concern was the foremost indication for root coverage procedures.[25] Indications other than aesthetic, root sensitivity were low and were grouped in the other category, accounting for 1.84% of the indications.
Conclusion Gingival recession is one of the main esthetic complaints of patients. This also exposes patients to sensitivity and greater risk for root caries. Mucogingival surgery strives to re-establish the periodontium to a healthy functional state. Periodontal pla stic surgery strives to restore the periodontium to a healthy, efficient, and aesthetic state. For coverage of exposed roots, there is a vast range of mucogingival grafting procedures available in the present era. These procedures are quite predictable and produce satisfactory solutions to the problems presented by gingival recessions. Choice of the suitable procedure, specific and thorough surgical technique will offer successful and exceedingly predictable results in the management of gingival recessions. References 1. Miller AJ, Brunelle JA, Carlos JP, Brown LJ, Le H. Oral Health of United States Adults. The National Survey of Oral Health in U.S. Employed Adults and Seniors: 19851986; NIH publication no. 87-2868. 2. Albandar JM and Kingman A. Gingival recession ,gingival bleeding and adults 30 years of age and older in united states J Periodontol, vol. 70, pp. 30-43, 1999
3. Van Palenstein Helderman WH, Lembariti BS, van der Weijden GA, Vant Hof MA. Gingival recession and its association with calculus in subjects deprived of prophylactic dental care. J Clin Periodontol, vol. 25, pp. 106-111, 1998.
4. Khocht A, Simon G, Person P et al. Gingival recession in relation to history of hard toothbrush use J Periodontol, vol. 64, pp. 900-905, 1993. 5. Trott JR and Love B. An analysis of localised recession in 766 Winnipeg high school students. Dent Pract Dent Rec, vol. 16, pp. 209-213, 1966. 6. Zachrisson BU orthodontics and periodontics In: Lindhe J, editor, Clinical periodontology and implant dentistry, 3 rd ed. Copenhagen: Munksgaard, pp, 741-793, 1998
7. Jon Artun and Olaf krogstad. Periodontal status of mandibular incisors following excessive proclination A study in adults with surgically treated mandibular prognathism Am J Orthod Dentofacial Orthop, vol. 91,pp. 225-232, 1987.
8. Wright PS, Hellyer PH. Gingival recession related to removable partial dentures in older patients. J Prosthet Dent , vol. 74, pp. 602-607, 1995. 9. Gunsolley JC, Quinn SM, Tew J et al. The effect of smoking on individuals with minimal periodontal destruction. J Clin Periodontol, vol. 69, pp.165-170, 1998. 10. Parma Benfenati S, Fugazzato PA, Ruben MP. He effect of restorative margins on post surgical development and nature of periodontium. Int J periodontics restor dent , vol 5, pp. 31-51, 1985. 11. Quart A M, Butkus Small C, Klein RS. The cocaine connection: users imperil their gingiva. J Am Dent Assoc, vol.122, pp. 85-87, 1991. 12. Miller PD Jr. A classication of marginal tissue recession. Int J Periodontics Restorative Dent , vol. 5, pp. 9-13, 1985. 13. Sullivan H and Atkins. Free autogenous gingival grafts. Principles of successful grafting. J Periodontol, vol. 6, pp. 5-13, 1968. 14. Smith RG. Gingival recession: reappraisal of an enigmatic condition and a new index for monitoring. J Clin Periodontol, vol.24, pp. 201-205, 1997. 15. Nordland WP and Tarnow DP. A classification system for loss of papillary height. J Periodontol, vol. 69, pp.1124-1126, 1998. 16. Greene PR. The flexible gingival mask: an aesthetic solution in periodontal practice. Br Dent J, vol.184, pp. 536-540, 1998.
17. Brannstrom M and Astrom A. The hydrodynamics of the dentine; its possible relationship to dentinal pain. Int Dent J, vol. 22, pp. 219-227, 1972. 18. Reiker J, Galloway R, Orchardson R. A cross-sectional study into prevalence of root caries in periodontal maintenance patients. J Clin Periodontol, vol. 26, pp. 26-32, 1999. 19. Wenstrom JL. Mucogingival therapy Ann of periodontology vol.1, pp. 671-701, 1996. 20. Sullivan HC and Atkins JH. Free autogenous principles of successive grafting Periodontics, vol. 6, pp. 121-129, 1968. 21. Langer B and Langer L. Subepithelial connective tissue graft coverage J Periodontol, vol. 56, pp. 715-720, 1985. technique for root
22. Tarnow DP. Semilunar coronally repositioned flap. J Clin Periodontol, vol.13, pp.182185, 1986. 23. Sumner CF. Surgical repair of recession on maxillary cuspid: incisionally repositioned flap. J Periodontol ,vol.40, pp.119-121, 1969. 24. Pini Prato GP, Tinti C, Vincenzi G, Mangani C, Cortellini P, Clauser C : Guided tissue regeneration versus mucogingiva l s urgery in the treatment of human buccal gingiva l recession. J Periodontol , vol. 63, pp. 919, 1992. 25. Zaher, CA, Hachem J, Puhan MA, Mombelli A. Interest in periodontology and preferences for treatment of localized gingival recessions. J Clin Periodontol, vol. 32, pp. 375382, 2005.
Você também pode gostar
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentAinda não há avaliações
- Gingival ResesiDocumento7 páginasGingival ResesiannysaAinda não há avaliações
- Jurnal Resesi 2 PDFDocumento7 páginasJurnal Resesi 2 PDFviena mutmainnahAinda não há avaliações
- Esthetic Zone Root Coverage With Lateral Pedicle Flap - A CaseDocumento5 páginasEsthetic Zone Root Coverage With Lateral Pedicle Flap - A CaseHiroj BagdeAinda não há avaliações
- Jurnal Resesi Gingiva 2Documento7 páginasJurnal Resesi Gingiva 2Muhammad KholisAinda não há avaliações
- Free Gingival Grafting To Increase The Zone of Keratinized Tissue Around ImplantsDocumento5 páginasFree Gingival Grafting To Increase The Zone of Keratinized Tissue Around ImplantsWinfield LiongAinda não há avaliações
- Dens Evaginatus and Type V Canal Configuration: A Case ReportDocumento4 páginasDens Evaginatus and Type V Canal Configuration: A Case ReportAmee PatelAinda não há avaliações
- Treatment of Perforating Internal Root Resorption With MTA: A Case ReportDocumento5 páginasTreatment of Perforating Internal Root Resorption With MTA: A Case ReportvishalbalpandeAinda não há avaliações
- 3 - Use of Mucogingival Surgical Procedures To Enhance EstheticsDocumento24 páginas3 - Use of Mucogingival Surgical Procedures To Enhance EstheticsStefanie Lais Kreutz RosaAinda não há avaliações
- Nasopalatine Duct Cyst - A Delayed Complication To Successful Dental Implant Placement - Diagnosis and Surgical Management - As Published in The JOIDocumento6 páginasNasopalatine Duct Cyst - A Delayed Complication To Successful Dental Implant Placement - Diagnosis and Surgical Management - As Published in The JOIHashem Motahir Ali Al-ShamiriAinda não há avaliações
- Internal Root Resorption Sixty Four ThouDocumento8 páginasInternal Root Resorption Sixty Four ThouMihaela TuculinaAinda não há avaliações
- Gingival Mask A Case Report On Enhancing SmilesDocumento3 páginasGingival Mask A Case Report On Enhancing SmilesLouis HutahaeanAinda não há avaliações
- Gingival Mask: A Case Report On Enhancing Smiles: ASE EportDocumento3 páginasGingival Mask: A Case Report On Enhancing Smiles: ASE EportLouis HutahaeanAinda não há avaliações
- Prosthodontic Management of Severely ResorbedDocumento2 páginasProsthodontic Management of Severely ResorbedAamir BugtiAinda não há avaliações
- Surgical Exposure and Fix Orthondontic Combination For Maxilla Canine Impacted TreatmentDocumento5 páginasSurgical Exposure and Fix Orthondontic Combination For Maxilla Canine Impacted TreatmentRAKERNAS PDGI XIAinda não há avaliações
- Jurnal Resesi Gingiva 6Documento6 páginasJurnal Resesi Gingiva 6Muhammad KholisAinda não há avaliações
- Interdisciplinary Sequencing of Aesthetic Treatment 2015 Dental Clinics of North AmericaDocumento16 páginasInterdisciplinary Sequencing of Aesthetic Treatment 2015 Dental Clinics of North AmericaAndré Louiz FerreiraAinda não há avaliações
- Clinical Considerations of Open Gingival Embrasures: Jae Hyun Park, Kiyoshi Tai, John Morris and Dorotea ModrinDocumento15 páginasClinical Considerations of Open Gingival Embrasures: Jae Hyun Park, Kiyoshi Tai, John Morris and Dorotea ModrinSamra NausheenAinda não há avaliações
- Restoration of The Severely Decayed Tooth Using Crown Lengthening With Simultaneous Tooth-PreparationDocumento5 páginasRestoration of The Severely Decayed Tooth Using Crown Lengthening With Simultaneous Tooth-PreparationIntelligentiaAinda não há avaliações
- A Case Report On Combination of Vista With Connective Tissue Graft As A Predictable Surgical Approach in Management of Multiple Gingival RecessionDocumento5 páginasA Case Report On Combination of Vista With Connective Tissue Graft As A Predictable Surgical Approach in Management of Multiple Gingival RecessionInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Vestibular Deepening To Improve Periodontal Pre-ProstheticDocumento5 páginasVestibular Deepening To Improve Periodontal Pre-ProstheticRAKERNAS PDGI XIAinda não há avaliações
- Crown LengtheningDocumento89 páginasCrown LengtheningMohamadAl-askar83% (6)
- Crown Lengthening Techniques and IndicationsDocumento5 páginasCrown Lengthening Techniques and IndicationsAnil NepalAinda não há avaliações
- Pal A To Gingival GrooveDocumento5 páginasPal A To Gingival GrooveValonia IreneAinda não há avaliações
- Pin-Retained Restoration With Resin Bonded Composite of A Badly Broken ToothDocumento3 páginasPin-Retained Restoration With Resin Bonded Composite of A Badly Broken ToothIOSRjournalAinda não há avaliações
- Periodontal Plastic SurgeryDocumento5 páginasPeriodontal Plastic Surgeryudhai170819Ainda não há avaliações
- Principles of Crown Lengthening Surgery: PeriodontologyDocumento4 páginasPrinciples of Crown Lengthening Surgery: PeriodontologyGreen Sleeves100% (1)
- Radicular Cyst: A Case Report: Harshitha KR, Varsha VK, Deepa. CDocumento3 páginasRadicular Cyst: A Case Report: Harshitha KR, Varsha VK, Deepa. CEzza RiezaAinda não há avaliações
- ContempClinDent32219 6162101 - 170701 2Documento4 páginasContempClinDent32219 6162101 - 170701 2Andres CoboAinda não há avaliações
- Anterior Esthetic Crown-Lengthening Surgery: A Case ReportDocumento4 páginasAnterior Esthetic Crown-Lengthening Surgery: A Case ReportSAinda não há avaliações
- Surgical Reconstruction of Interdental PDocumento11 páginasSurgical Reconstruction of Interdental PMaria Jose GodoyAinda não há avaliações
- 1 Three Years Follow Up of Combined Perio EndoDocumento3 páginas1 Three Years Follow Up of Combined Perio EndohanAinda não há avaliações
- Treatment of Multiple Adjacent Recession Type Defects Using Semilunar Incision: A Case ReportDocumento24 páginasTreatment of Multiple Adjacent Recession Type Defects Using Semilunar Incision: A Case Reportdhwanit31Ainda não há avaliações
- NpeltzDocumento4 páginasNpeltzCristinaAinda não há avaliações
- Quiste DentigeroDocumento5 páginasQuiste DentigeroAlicia Ajahuana PariAinda não há avaliações
- Tre Atm Ent of Gingiva L Re Cession: Moawia M. Kassab,, Hala Badawi,, Andrew R. DentinoDocumento12 páginasTre Atm Ent of Gingiva L Re Cession: Moawia M. Kassab,, Hala Badawi,, Andrew R. Dentinodhwanit31100% (1)
- Kassab2010 PDFDocumento12 páginasKassab2010 PDFdhwanit31Ainda não há avaliações
- Biologic Width - The No Encroachment Zone: I J D ADocumento8 páginasBiologic Width - The No Encroachment Zone: I J D AJinny ShawAinda não há avaliações
- Case Report Massive Radicular Cyst in The Maxillary Sinus As A Result of Deciduous Molar Tooth Pulp NecrosisDocumento5 páginasCase Report Massive Radicular Cyst in The Maxillary Sinus As A Result of Deciduous Molar Tooth Pulp NecrosisSarah Ariefah SantriAinda não há avaliações
- Aesthetic Crown LengtheningDocumento4 páginasAesthetic Crown LengtheningGopuAinda não há avaliações
- Treatment of A Large Maxillary Cyst With Marsupial PDFDocumento4 páginasTreatment of A Large Maxillary Cyst With Marsupial PDFSalem WalyAinda não há avaliações
- Ectopic Tooth in Maxillary Sinus: Case SeriesDocumento0 páginaEctopic Tooth in Maxillary Sinus: Case Seriestitis istya aAinda não há avaliações
- Severe Gingival Recession Caused by Orthodontic Rubber Band: A Case ReportDocumento5 páginasSevere Gingival Recession Caused by Orthodontic Rubber Band: A Case ReportanjozzAinda não há avaliações
- Treatment of a Large Maxillary Cyst with Marsupialization and Staged SurgeryDocumento8 páginasTreatment of a Large Maxillary Cyst with Marsupialization and Staged SurgeryDinesh SolankiAinda não há avaliações
- An Innovative Cosmetic Technique Called Lip Repositioning: Case ReportDocumento4 páginasAn Innovative Cosmetic Technique Called Lip Repositioning: Case ReportsevattapillaiAinda não há avaliações
- Dens Invaginate..Documento4 páginasDens Invaginate..Hawzheen SaeedAinda não há avaliações
- Immediate Temporization Crown Lengthening: April 2011 Volume 32, Issue 3Documento6 páginasImmediate Temporization Crown Lengthening: April 2011 Volume 32, Issue 3Kyoko C.LAinda não há avaliações
- Dental ReviewDocumento5 páginasDental ReviewUmarsyah AliAinda não há avaliações
- Dentigerous Cyst Associated With Permanent Maxillary Central Incisor: Report of Two CasesDocumento4 páginasDentigerous Cyst Associated With Permanent Maxillary Central Incisor: Report of Two CasesAhmad MustafaAinda não há avaliações
- Root Resorption A 6-Year Follow-Up Case ReportDocumento3 páginasRoot Resorption A 6-Year Follow-Up Case Reportpaola lopezAinda não há avaliações
- Extraction or Nonextraction in Orthodontic Cases - A Review - PMCDocumento6 páginasExtraction or Nonextraction in Orthodontic Cases - A Review - PMCManorama WakleAinda não há avaliações
- Serial ExtractionDocumento38 páginasSerial ExtractionRamy HanyAinda não há avaliações
- Coronally Advanced Flap With Connective Tissue GraDocumento13 páginasCoronally Advanced Flap With Connective Tissue GrasutriAinda não há avaliações
- Article JCDocumento3 páginasArticle JCSaurabh NagrathAinda não há avaliações
- Reimplantation of Avulsed Teeth After Dry Storage For One WeekDocumento5 páginasReimplantation of Avulsed Teeth After Dry Storage For One WeekHesti RahayuAinda não há avaliações
- Multiple Supernumerary Teeth Associated With An Impacted Maxillary Central Incisor: Surgical and Orthodontic ManagementDocumento4 páginasMultiple Supernumerary Teeth Associated With An Impacted Maxillary Central Incisor: Surgical and Orthodontic ManagementCalin CristianAinda não há avaliações
- Management of Infected Radicular Cyst by Surgical Approach: Case ReportDocumento2 páginasManagement of Infected Radicular Cyst by Surgical Approach: Case ReportEzza RiezaAinda não há avaliações
- Crid2022 5981020Documento10 páginasCrid2022 5981020lily oktarizaAinda não há avaliações
- 2000 J C. H S W A: Udson Ickey Cientific Riting WardDocumento6 páginas2000 J C. H S W A: Udson Ickey Cientific Riting WardPremshith CpAinda não há avaliações
- ParesthesiaoftheupperlipDocumento4 páginasParesthesiaoftheupperlipikeuchi_ogawaAinda não há avaliações
- Text BookDocumento1 páginaText Bookikeuchi_ogawaAinda não há avaliações
- European Journal of OrthodonticsDocumento288 páginasEuropean Journal of Orthodonticsikeuchi_ogawaAinda não há avaliações
- Volume Xliv Number 1 JANUARY 2010: 19 2009 Practice StudyDocumento1 páginaVolume Xliv Number 1 JANUARY 2010: 19 2009 Practice Studyikeuchi_ogawaAinda não há avaliações
- Asian Journal of Pharmaceutical and Clinical ResearchDocumento2 páginasAsian Journal of Pharmaceutical and Clinical Researchikeuchi_ogawaAinda não há avaliações
- Anterior Crossbite Correction in Primary and Mixed Dentition With Removable Inclined Plane (Bruckl Appliance)Documento5 páginasAnterior Crossbite Correction in Primary and Mixed Dentition With Removable Inclined Plane (Bruckl Appliance)Amr Eldok100% (1)
- Matakuliah S2Documento4 páginasMatakuliah S2Bayu Aji KurniawanAinda não há avaliações
- Pertamina PertashopDocumento4 páginasPertamina Pertashopikeuchi_ogawa79% (19)
- WelcomeDocumento5 páginasWelcomeCatAinda não há avaliações
- Forced Eruption of Adjoining Maxillary Premolars Using A Removable Orthodontic Appliance: A Case ReportDocumento4 páginasForced Eruption of Adjoining Maxillary Premolars Using A Removable Orthodontic Appliance: A Case Reportikeuchi_ogawaAinda não há avaliações
- Soal CPNS Paket 3Documento8 páginasSoal CPNS Paket 3icoirs 2016Ainda não há avaliações
- Retention of Teeth for OverdenturesDocumento29 páginasRetention of Teeth for OverdenturesShyam K MaharjanAinda não há avaliações
- Surat Kepala BKN Nomor K.26 30V.72 299Documento4 páginasSurat Kepala BKN Nomor K.26 30V.72 299ikeuchi_ogawaAinda não há avaliações
- 084 05Documento1 página084 05ikeuchi_ogawaAinda não há avaliações
- The Editor'S Corner: Mouthguards and OrthodonticsDocumento2 páginasThe Editor'S Corner: Mouthguards and Orthodonticsikeuchi_ogawaAinda não há avaliações
- Iatrogenic Mandibular Fracture Associated With Third Molar RemovalDocumento3 páginasIatrogenic Mandibular Fracture Associated With Third Molar Removalikeuchi_ogawaAinda não há avaliações
- 12 Ectopic Supernumerary Nasal Tooth Case Report 2Documento3 páginas12 Ectopic Supernumerary Nasal Tooth Case Report 2ikeuchi_ogawaAinda não há avaliações
- Improper Reduction and Fixation of Bilateral AnteriorDocumento3 páginasImproper Reduction and Fixation of Bilateral Anteriorikeuchi_ogawaAinda não há avaliações
- 10.conservative Management of A Dentigerous Cyst Secondary To PrimaryDocumento4 páginas10.conservative Management of A Dentigerous Cyst Secondary To Primaryikeuchi_ogawaAinda não há avaliações
- Correction of An Anterior Crossbite With A Fixed Partial DentureDocumento4 páginasCorrection of An Anterior Crossbite With A Fixed Partial Dentureikeuchi_ogawaAinda não há avaliações
- Maat 08 I 2 P 173Documento2 páginasMaat 08 I 2 P 173ikeuchi_ogawaAinda não há avaliações
- Asian Journal of Pharmaceutical and Clinical ResearchDocumento2 páginasAsian Journal of Pharmaceutical and Clinical Researchikeuchi_ogawaAinda não há avaliações
- Interesting - Case - Report - of - Tooth - Inside - Nasal - Cavity (+)Documento3 páginasInteresting - Case - Report - of - Tooth - Inside - Nasal - Cavity (+)ikeuchi_ogawaAinda não há avaliações
- Bds Tutorial Overdentures 1Documento7 páginasBds Tutorial Overdentures 1ikeuchi_ogawaAinda não há avaliações
- 6 TissueManagementDocumento4 páginas6 TissueManagementikeuchi_ogawaAinda não há avaliações
- A Denture Swallowed. Case Report 1995Documento3 páginasA Denture Swallowed. Case Report 1995ikeuchi_ogawaAinda não há avaliações
- Grafik, PersentilDocumento22 páginasGrafik, PersentilkadekpramithaAinda não há avaliações
- E Plaque PDFDocumento10 páginasE Plaque PDFjemmysenseiAinda não há avaliações
- 85-6403 e (C) F (T) PF1 (MH) Pfa (H)Documento3 páginas85-6403 e (C) F (T) PF1 (MH) Pfa (H)ikeuchi_ogawaAinda não há avaliações
- A Denture Swallowed. Case Report 1995Documento3 páginasA Denture Swallowed. Case Report 1995ikeuchi_ogawaAinda não há avaliações
- Case Report UnpriDocumento17 páginasCase Report UnpriChandra SusantoAinda não há avaliações
- Suturing Techniques in Periodontal Plastic SurgeryDocumento9 páginasSuturing Techniques in Periodontal Plastic SurgeryNishtha Kumar100% (1)
- Dental Decks Periodontics DR GhadeerDocumento162 páginasDental Decks Periodontics DR GhadeerGhadeerHassaan100% (11)
- General Principles of Periodontal SurgeryDocumento10 páginasGeneral Principles of Periodontal SurgeryPurwana NasirAinda não há avaliações
- Article 009Documento9 páginasArticle 009MedstudAinda não há avaliações
- Free Gingival Graft Procedure OverviewDocumento1 páginaFree Gingival Graft Procedure OverviewTenzin WangyalAinda não há avaliações
- Periodontalplastic and Esthetic ProceduresDocumento26 páginasPeriodontalplastic and Esthetic ProceduresShelly JohnsonAinda não há avaliações
- E PonticDocumento16 páginasE Ponticanton50% (2)
- Segunda Fase ArticuloDocumento7 páginasSegunda Fase ArticuloDanielaAinda não há avaliações
- Cosmetic DentistryDocumento52 páginasCosmetic DentistryPaul Chen60% (5)
- Periodontal Soft Tissue Root Coverage Procedures - A Systematic Review From The AAP Regeneration WorkshopDocumento44 páginasPeriodontal Soft Tissue Root Coverage Procedures - A Systematic Review From The AAP Regeneration WorkshopSusan Mallqui De la CruzAinda não há avaliações
- Gingival Depigmentation TechniquesDocumento27 páginasGingival Depigmentation TechniquesAshaAgrawalAinda não há avaliações
- ACC Soft Tissue Development Around Pontic SiteDocumento5 páginasACC Soft Tissue Development Around Pontic SiteJayarti Rohmadani MarsaAinda não há avaliações
- Zucchelli Et Al-2015-Periodontology 2000Documento36 páginasZucchelli Et Al-2015-Periodontology 2000Abad Salcedo100% (1)
- كل أسئلة اللثة لامتحان الهيئةDocumento40 páginasكل أسئلة اللثة لامتحان الهيئةMohamed Kudaih100% (1)
- CARLO TINTI. The Free Rotated Papilla Autograft A New Bilaminar Grafting Procedure For The Coverage of Multiple Shallow Gingival Recessions.Documento9 páginasCARLO TINTI. The Free Rotated Papilla Autograft A New Bilaminar Grafting Procedure For The Coverage of Multiple Shallow Gingival Recessions.Julio César PlataAinda não há avaliações
- Esthetic Localized Soft Tissue Ridge Augmentation in A Fixed Partial Denture A Case Report PDFDocumento3 páginasEsthetic Localized Soft Tissue Ridge Augmentation in A Fixed Partial Denture A Case Report PDFAmar Bhochhibhoya0% (1)
- Periodontal Plastic SurgeryDocumento5 páginasPeriodontal Plastic Surgeryudhai170819Ainda não há avaliações
- Criteria For Root Coverage ProceduresDocumento14 páginasCriteria For Root Coverage ProceduresGabriel OgandoAinda não há avaliações
- Basic Principles of Periodontal SurgeryDocumento100 páginasBasic Principles of Periodontal SurgerySandip Ladani100% (2)
- Pini Prato Et AlDocumento35 páginasPini Prato Et AlFernando CursachAinda não há avaliações
- Implantfailurepankajfinal 160120192933Documento104 páginasImplantfailurepankajfinal 160120192933DrIbrahimShaikh100% (1)
- Gummy Smile - IntegrativeDocumento3 páginasGummy Smile - IntegrativeNingombam Robinson SinghAinda não há avaliações
- PLPF PDFDocumento88 páginasPLPF PDFmaxAinda não há avaliações
- Vestibuloplasty and Free Gingival Grafts Improve Perio Health in Cleft PatientsDocumento7 páginasVestibuloplasty and Free Gingival Grafts Improve Perio Health in Cleft PatientsSergio Losada AmayaAinda não há avaliações
- ORTODONCIA1Documento12 páginasORTODONCIA1Orlando RodríguezAinda não há avaliações
- Zucchelli 2010Documento8 páginasZucchelli 2010Evan BlackwellAinda não há avaliações
- Perio-Prog Class 2012Documento80 páginasPerio-Prog Class 2012moorenAinda não há avaliações
- Anja Ainamo 1992 in His 18 Year Follow Up Study AfterDocumento215 páginasAnja Ainamo 1992 in His 18 Year Follow Up Study AfterSuperna TiwariAinda não há avaliações
- Electro Cauter UlDocumento3 páginasElectro Cauter UlbusagaAinda não há avaliações