Escolar Documentos
Profissional Documentos
Cultura Documentos
Early Rehabilitation Protocols Eng - Light
Enviado por
Eric WeertsDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Early Rehabilitation Protocols Eng - Light
Enviado por
Eric WeertsDireitos autorais:
Formatos disponíveis
Demey Didier - Nielsen Susanne - Weerts Eric
Handicap International
Robert Fall (G2 Studio) for HI
EARLY REHABILITATION PROTOCOLS FOR VICTIMS OF NATURAL DISASTER
Training Capitalization Manual
August 2010
Page - 3 Page
EARLY REHABILITATION PROTOCOLS FOR VICTIMS OF NATURAL DISASTER
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Training Capitalization Manual
Rehabilitation The path towards autonomy
The content of this publication is the sole property of Handicap International and can in no way be taken to reflect the views of the co-funders. Please quote the source of the document in case of use. Publication co-funded by Handicap International and:
Sanofi Aventis
Ministry of Foreign Affairs of Luxemburg
French Government
Electricit de France
Brussels Region
Municipality of Paris
Chaine du Bonheur
Rotary Club of Kowloon North
Rotary Club of Shanghai
Belgian Embassy in China
Partnerships for Community Development
EARLY MANAGEMENT
Page - 5 Page
ACKNOWLEDGMENT
We also would like to thank the Hong Kong Rehabilitation Society and, especially Sheila Purves (project director) and Mrs Phoebe (secretary), as well as Mr. Wang Yuling (Deputy Director, Department of Rehabilitation Medicine of First Affiliated Hospital and Secretary, Department of Rehabilitation Therapy of Sun Yat-sen Medical College, Sun Yat-sen University) for their help in revising the accuracy of the content and translation of this document.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Handicap International would like to thank Mr Cai Sheng for the translation of the following documents from English into Chinese. His dedication was greatly appreciated.
EARLY MANAGEMENT
Page - 7 Page
PREFACE Handicap International has been working in China for more than 12 years. Our objective is to improve the autonomy and social inclusion of persons with disabilities, especially in rural areas, through pilot projects run in close cooperation with governmental partners, civil society and associations of people with disabilities. We intervene in both long term development and emergency contexts. The provision of active and quality rehabilitation treatment following an injury, surgery illness is essential to minimize the disabling effects and ensure the optimal recovery function. It is a key component of the comprehensive rehabilitation process promoted Handicap International. This process includes early rehabilitation in hospital, follow-up home and long term support for the social inclusion of people with disabilities. or of by at
Active rehabilitation techniques are however not yet promoted enough in China and there is a huge lack of professionals in this field. This training capitalization manual aims at providing rehabilitation therapists and other medical staffs in China with practical protocols and tools that they can follow to treat injured persons during their hospitalization. Although it was developed in the framework of a post earthquake intervention, it is not restricted to earthquake casualties, but is a transferable resource to other conditions commonly treated in hospital. It is also hoped that it could serve in other contexts than China. I would like to sincerely thank all the persons who contributed to this manual. Special thanks go to Didier Demey, Susanne Nielsen and Eric Weerts whose professionalism and commitment made our emergency interventions in Sichuan and Qinghai possible. They not only provided direct care to the casualties but also had the intelligence to document their work and capitalize on it. Particular thanks as well to all our partners in Chengdu, Mian Zhu and Yushu. Last but not least, I would like to thank our donors without whom our activities would not be possible. Jean Van Wetter Country Director Handicap International China
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
Page - 9 Page
INTRODUCTION
The material was produced to train physiotherapists and other medical staff (surgeons, doctors, nursing staff) in Huaxi and Number 3 Hospitals in Chengdu. Information material was also produced for the victims of the earthquake and their families. The early rehabilitation protocols presented in this document contain basic physiotherapy exercises and techniques that can be used in the early stage (during hospitalization) for most victims of earthquake. Those, in the majority of the cases, suffer from bone fracture, head injury, spinal cord injury, peripheral nerve injury, burns and/or amputation. Because of the prolonged hospitalization, victims from an earthquake may also suffer from common complications due to confinement in bed (bedridden complications). Some of the PT exercises and techniques that are described in the protocols can be used for people having different types of impairment or injury. In order to prevent from repeating in different protocols the same types of exercises, two main types of protocols were created: the protocols by injury and the protocols by technique. The "protocols by injury" are specific to one injury (bone fracture, head injury, spinal cord injury, amputation, bedridden patients, peripheral nerve injury and burns). They contain general information on that specific injury and a detailed protocol (assessment, exercises and techniques to be used during hospitalization and long-term rehabilitation). The "protocols by technique" contains detailed description of specific techniques (passive mobilization, active mobilization and strengthening, balance exercises, stretching, chest therapy, positioning, transfer and mobility and teaching the patient/family). The techniques described in the "protocols by technique" are not described in details in the "protocols by injury". When they are suitable, they are just named and referred in the "protocols by injury". Therefore, both types of protocols have to be used in parallel, as they complement each other.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
This training capitalization manual has been produced by Handicap Internationals experts following the earthquake and emergency intervention in Sichuan in May and June 2008. It has then been revised after the post-emergency intervention in Qinghai province (Yushu earthquake, April 2010).
EARLY MANAGEMENT
Page - 11 Page
CONTENTS This manual is made of 4 different parts:
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. The first part of the manual presents preliminary notes regarding the provision of early rehabilitation services (importance and benefits of early rehabilitation for hospitalized patients, early rehabilitation pathway and patient management) 2. The second part contains the 7 early rehabilitation protocols by injury (bone fracture, head injury, spinal cord injury, amputation, bedridden/ICU patients, burn and peripheral nerve injury). 3. The third part contains the 8 early rehabilitation protocols by technique (passive mobilization, stretching, active mobilization and strengthening, chest therapy, positioning and changing of position, transfer and mobility and teaching the patient/family). 4. The last part contains a list of annexes that are referred to in the other parts of the document. Soft copies of those annexes can be found on the capitalization DVD. Table of content
ACKNOWLEDGMENT ................................................................................................................................. 5 PREFACE .................................................................................................................................................. 7 INTRODUCTION ....................................................................................................................................... 9 CONTENTS ............................................................................................................................................. 11 PART 1. PRELIMINARY NOTES REGARDING THE PROVISION OF EARLY REHABILITATION SERVICES... 13 Note I - Importance and Benefits of Early Rehabilitation for Hospitalized Patients ...........................................13 Note II - The Early Rehabilitation Pathway.................................................................................................18 Note III Patient Management ................................................................................................................19 PART 2. THE EARLY REHABILITATION PROTOCOLS BY INJURY ............................................................. 20 Early Rehabilitation Protocol for Amputation ..............................................................................................21 1. General Information on Amputation...................................................................................................21 2. PT Protocol for Amputees .................................................................................................................27 Early Rehabilitation Protocol for Bone Fracture ...........................................................................................33 1. General Information on Bone Fracture ...............................................................................................33 2. PT Protocol for Patients with Bone Fracture.........................................................................................38 Early Rehabilitation Protocol for Spinal Cord Injury .....................................................................................47 1. General Information on Spinal Cord Injury (SCI).................................................................................47 2. Physiotherapy Protocol for Spinal Cord Injury ....................................................................................53 Early Rehabilitation Protocol for Head Injury ..............................................................................................57 1. General Information on Head Injury ..................................................................................................57 2. PT Protocol for Head Injury ..............................................................................................................61 Early Rehabilitation Protocol for Bedridden/ICU Patients ..............................................................................70 1. General Information on Bedridden and ICU Patients ............................................................................70 2. PT protocol for Bedridden/ICU Patients ..............................................................................................75 Early Rehabilitation Protocol for Peripheral Nerve Injury ..............................................................................78 1. General Information on Peripheral Nerve Injury (PNI)..........................................................................78 2. PT Protocol for Peripheral Nerve Injury ..............................................................................................83 Early Rehabilitation Protocol for Burn ........................................................................................................86 1. General Information on Burn ............................................................................................................86 2. PT Protocol for Burn Patients ............................................................................................................90 PART 3. THE PT PROTOCOLS BY TECHNIQUE.......................................................................................... 93 PT Protocol for Passive and Assisted Mobilizations ......................................................................................94 1. General Information on Passive and Passive Assisted Mobilizations........................................................94 2. Technique ......................................................................................................................................96 PT Protocol for Active Mobilization and Strengthening Exercises ...................................................................99 1. General Information on Active mobilization and Strengthening Exercises................................................99 2. Technique ....................................................................................................................................101 PT Protocol for Stretching Exercises ........................................................................................................106 1. General Information on Stretching Exercises ....................................................................................106 2. Technique ....................................................................................................................................107 PT Protocol for Balance Exercises ...........................................................................................................109 1. General Information on Balance Exercises ........................................................................................109 2. Technique ....................................................................................................................................110 PT Protocol for Chest Therapy ................................................................................................................113
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 12 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Chest Therapy.............................................................................................113 2. Technique ....................................................................................................................................116 PT Protocol for Transfer and Mobility .......................................................................................................119 1. General Information on Transfer and Mobility ...................................................................................119 2. Technique ....................................................................................................................................120 PT Protocol for Positioning and Changing Position .....................................................................................131 1. General Information on Positioning and Changing Position..................................................................131 2. Technique ....................................................................................................................................132 Teaching and Informing the Patient and His/Her Family Members...............................................................134
PART 4. ANNEXES ................................................................................................................................ 137
Page - 13 Page
PART
1.
PRELIMINARY NOTES REGARDING
THE
PROVISION
OF
EARLY
REHABILITATION SERVICES
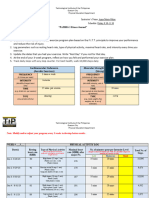
Note I - Importance and Benefits of Early Rehabilitation for Hospitalized Patients This chapter will quantify why rehabilitation needs to be commenced as soon as possible. In a situation after a natural disaster there are many other needs, which will need to be addressed, but rehabilitation must be incorporated into any healthcare plan in order to ensure optimal recovery. Definition of early rehabilitation Early rehabilitation means that a person is assessed immediately following the traumatic event or illness which has brought them to hospital in order to prevent secondary complications and ensure optimal recovery. The benefits of early rehabilitation? Early rehabilitation will ensure that a person has a greater possibility of recovering to their previous level of function before their injury or illness. If the injury or illness is severe, the earlier the rehabilitation is commenced, the more likely is the possibility of the person to reach a more independent life on discharge from hospital. For specific benefits, please see below table. The risks of no rehabilitation? No rehabilitation can lead to short and long-term secondary complications. The table below outlines the most common complications. These complications can lead to disability and in worst cases may cause premature mortality. How soon can detrimental effects occur of having no rehabilitation? This depends on the premorbid condition of the patient. General guidelines are set out in below table. When to start rehabilitation? Some people may not have sustained so severe injuries or illness and will not need rehabilitation, but simply an assessment and recommendations regarding how to prevent secondary complications, which otherwise could result in long-term problems. Some people will have sustained more severe injuries or illness, that will require immediate assessment and start of rehabilitation, following the rehabilitation guidelines (see annexes) and risk assessment (see annexes). ICU to treat or not? ICU All evidence emphasizes the need for early rehabilitation. This means that rehabilitation will start when the respiratory system and haemodynamics have stabilized, normally within 2448 hours. Some patients may be too sick or too sedated to be able to start rehabilitation, but daily monitoring of changes and the window of opportunity of when to start rehabilitation is important. One of the main complaints following critical illness is ICU-acquired neuromuscular weakness. There is now a growing body of evidence, which shows the reduced ICU-related neuromuscular weakness, if rehabilitation is started early.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 14 Page
The earlier the intervention, the less secondary complications. The table below and video clips on the capitalisation DVD underline this need. Who can provide early rehabilitation? If there is a rehabilitation department, the patient should be referred to the rehabilitation staff for assessment and treatment. If there is no rehabilitation staff, then rehabilitation can be provided by staff, who have been trained in providing basic rehabilitation, for example nursing or medical staff. The staff who complete early rehabilitation will need to know how to assess that the patient is ready for rehabilitation (assessing risks and safety), be able to identify the main problems and possible complications with no rehabilitation and make a basic rehabilitation plan. During rehabilitation, they will need to continue to review the risks and safety issues (monitoring of vital signs, contra-indications and precautions during rehabilitation (refer to the risk assessment form in annex), to ensure the rehabilitation is not detrimental to the patient. When the patient is medically stable, the staff can educate family and relatives on how to safely complete the basic positioning, exercises and mobility. This way the patient will get 24/7 care in a rehab-orientated way! and not only rehabilitation during the treatment sessions. How long should an early rehab treatment session be? This really depends on the condition of the patient. Sessions as short as 10-15 minutes may be required increasing to 30-45 minutes of gentle exercise and positioning. Treatment does take longer because it has to be completed with caution and more assistance is required. The most important issue is to carefully review the contra-indications and precautions for early rehabilitation, before the treatment and to monitor the patients vital signs (heart rate, respiratory rate, blood pressure, temperature, saturation of oxygen in the blood (Sp02)), before, during and after treatment. Can early rehabilitation be harmful? No, by assessing the patient properly, using the rehabilitation risk assessment form and monitoring the vital signs (heart rate, respiratory rate, blood pressure, temperature, saturation of oxygen in the blood (Sp02)), then all research has shown the benefits of early rehabilitation. However, there are risks and therefore rehabilitation in the early stage needs to be completed with caution. The problems that may occur are: Dislodgement of medical equipment (lines, tubes, ventilation) Worsening gas exchange and haemodynamics Inadequate patient comfort, pain control
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
References on safety: Kathy Stiller et al. 2007, Schweickert WD, Pohlman MC, Pohlman AS, et al. Lancet. 2009;373:1874-1882. Berney and Denehy (2003) Australian Journal of Physiotherapy 49: 99-105. What equipment is needed to provide early rehabilitation? For early rehabilitation assessment, a copy of the available checklist guidelines, assessment form, risk assessment form provided here (soft version on the capitalisation DVD), are the basic documentation materials needed.
Page - 15 Page
Some basic equipment that will be needed are pillows and rolled up towels for positioning, walking aids for standing and transfers. Depending on the condition a wheelchair may be needed to be able to sit out of bed and a toilet chair for toileting. How can rehabilitation be of benefit for the hospital? All evidence shows that early rehabilitation reduces the long-term impact of the injury or illness and that the actual costs for the hospital itself are not more (Morris et al. Critical Care Medicine (2008) Vol. 36, no. 8). The main benefits are as follows: Early rehabilitation will ensure a faster recovery from injury and illness and reduce the risk of secondary complications (see below table for detailed information). Less secondary complications, means less time spent with the patient, in order to treat the complications, that often take much longer to treat, than initial rehabilitation. A higher turn-over of patients. By providing early rehabilitation, this increases the comprehensiveness of the service provided by the hospital. Overall this means an improved quality healthcare service provision, which in turn will increase the hospital reputation.
Body / System
Risks with no rehab
How soon can detrimental effects occur?
What can be done?
Benefits of rehab
Reference
Van Peppen et al. 2004
Muscles
Muscle shortening Muscle weakness and atrophy Decreased motor unit activity Necrosis of muscle
In a healthy population a reduction of 11.5% of muscle mass occurs per day of bed rest
Active and activeassisted exercises Strengthening exercises Positioning to maintain muscle length Muscle stretching
Maintain muscle length, muscle strength and overall muscle physiology Maintain functional abilities
http://www.hopkinsmed icine.org/Press_releases /2010/04_09_10.html Needham et al., Volume 91, Issue 4, Pages 536542 (April 2010) P. Bailey et al. Crit Care Medicine, 2007 Vol. 35, Paddon-Jones D et al. (2004) J Clin Endocrinol Metab 89:43514358 Honkonen SE et al. (1997) International Orthopaedics, 21:323326
Joints
Joint stiffness and contracture Pain as a result of joint stiffness / contracture
At least within two weeks of bed rest
Joint range of motion exercises Positioning Use of assistive devices to maintain joint range
Reduce risk of joint contractures Maintain functional abilities
Brower, Critical Care Medicine 2009,37 (Suppl 1) S422. Heidi Clavet et al. CMAJ 2008 178 (6)
Bone Health
Reduced bone mineral density, which could lead to onset of osteoporosis and increased fracture risk Poor bone healing following fracture
Bone demineralisation occurs at a rate of 6mg per day calcium. This equals to approx. 2% bone mass per month, which can take up to 2 years to recover
Following fracture: Muscle strengthening exercises to increase the tensile strength of the bones Early weight-bearing (as soon as fracture stabilised and weight-bearing safe) The bedridden patient: Early muscle strengthening exercises and weightbearing to maintain bone
Prevention of bone demineralisation Increase bone healing with early weight-bearing (this will increase the local blood supply) Early rehab (exercises and weight-bearing) following fracture will ensure faster recovery through increased loading of bone, which will
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
For the early rehabilitation treatment, the Early Rehabilitation Equipment Catalogue provides specific details of the early equipment required for rehabilitation (view especially first part of the catalogue). However, most often the initial treatment will consist of positioning, sitting up in bed, joint range of motion exercise (passive, active-assisted and active), sitting over the edge of bed, standing and transfers into chair. For these initial treatments, it is mainly human resources that are needed; 1-2 people, sometimes 3 people in severe conditions, such as hemiplegia, SCI or with people with a low conscious-level.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 16 Page mineral density stimulate local blood supply and bone healing/growth and long-term tensile strength of bone
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Nervous System
Critical illness polyneuropathy (CIP) = Acute primary axonal sensorimotor degeneration Reduced muscle and joint proprioception. This means the sense of movement and position of a particular body part through the proprioceptive nerve endings in the muscles and joints. These are reduced due to immobility
2-5 days after onset of critical illness
Ensure exercise as soon as possible
Reduce risk of muscle atrophy Maintain functional abilities
Pandit and Agrawal Clin Neuro Neurosurg 2006;108:621-7. Hermans et al. (2008. Critical care 12 (6)
Skin
Pressure sore
Skin break-down can happen within 2 hours or even quicker, depending on the person (age, nutritional health, age, incontinence etc.) VO2 Max may decrease up to 0.9% per day The respiratory system deficits will also depend on the pre-morbid condition (for example age, past medical history of respiratory problems)
Position change at least every 2 hours (depending on skin condition) Pressure relieving cushion/mattress
Reduce risk of pressure sore
http://www.nice.org.uk/ nicemedia/pdf/clinicalgu idelinepressuresoreguid ancercn.pdf (2001)
Respiratory System
Decreased oxygen saturation Reduced VO2 Max. - This means the maximum oxygen uptake per minute) Pneumonia Reduced chest compliance
Positioning Early sit up in bed and exercise Standing and mobilising as soon as possibly and frequently Deep breathing exercise
Improve lung function by optimizing Ventilation/Perfusi on, lung volumes and airway clearance Reduce duration of mechanical ventilation
Schweickert WD, Pohlman MC, Pohlman AS, et al Lancet. 2009;373:18741882. Epub 2009 May 14 Trauma: Critical Care By William C. Wilson et al. (2007)
Cardiovascular System
Increased heart rate (needed to maintain the resting V02 max.) Reduced stroke volume (SV). This means the amount of blood, which is pumped out of the left ventricle in one heart beat Decreased aerobic capacity (exercise tolerance) Orthostatic hypotension Thrombo-embolic disease: deep vein thrombosis, pulmonary embolism Decreased cognitive function Confusion and hallucinations (from bed rest and medication) Reduced interaction and communication Depression Anxiety Apathy Decreased pain Tolerance Social withdrawal
Reduced stroke volume (SV) of approx. 28% after 10 days bed rest Depending on pre-morbid condition (for example age, past medical history of cardiovascular problems)
Positioning Regular moving in bed, sitting and standing Early exercise Compression devices
Improve cardiovascular fitness Reduce risk of cardiovascular complications
Trauma: Critical Care By William C. Wilson et al. (2007)
Cognition
Depending on condition, past medical history, medication
Early stimulation Early identification of communication ability Exercise and daily activity Daytime orientation
Improve level of consciousness Reduced delirium with early mobilisation
Schweickert WD, Pohlman MC, Pohlman AS, et al Lancet. 2009;373:18741882. Epub 2009 May 14 Trauma: Critical Care By William C. Wilson et al. (2007)
Psychological Health
Depending on premorbid condition, medical and social factors
Exercise and daily activity Social interaction
Improve psychological well being
Trauma: Critical Care By William C. Wilson et al. (2007)
Page - 17 Page Other factors Complications as a result of ineffective 24/7 care because of lack of knowledge of how to care for patient Education about exercise, positioning, how to regain function through participation in activities of daily living Improve psychological health Optimise recovery of function through appropriate care from relatives
Hospital length of stay
Increased hospital length of stay
Early rehabilitation
Reduced ICU length of stay
Needham et al., Volume 91, Issue 4, Pages 536542 (April 2010) Morris et al. Critical Care Medicine (2008) Vol. 36, no. 8
Daily function
Loss of this ability or poor regain of function due to long duration of bed rest and learned non-use Reduced balance and mobility Reduced physical capacity
Depends on premorbid condition, severity of injury or illness
Functional exercises Participation in activities of daily living as soon as possible
More likely to return to independent function at time of discharge from hospital Increased level of mobility
Van Peppen et al. 2004. Schweickert WD, Pohlman MC, Pohlman AS, et al Lancet. 2009;373:18741882. Epub 2009 May 14 P. Bailey et al. Crit Care Medicine, 2007 Vol. 35, No.1. Perme and Chandrashekar (2009) American Journal of Critical Care Needham et al., Volume 91, Issue 4, Pages 536542 (April 2010)
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Patient and relative education
Rehabilitation after critical illness, NICE Clinical Guidelines 2009, UK
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 18 Page
Note II - The Early Rehabilitation Pathway
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
The below graph presents the different steps through which patients receiving early rehabilitation in a hospital go through.
Admission in the hospital When arriving at the hospital, the patient will first go through admission and registration procedures Emergency care Depending on the patients situation, it might be needed to first provide him with urgent medical care in order to stabilize his condition Early rehabilitation needs assessment Within the first days of hospitalization (even if the patient situation is not totally stabilized), it is important that a doctor or a nurse does an assessment of the patients needs in terms of early rehabilitation. To do so, the person in charge should use the Early Rehabilitation Needs Assessment Form (see below). If the result of the early rehabilitation needs assessment shows that the patient is in need of early rehabilitation, he/she should be referred to the rehabilitation department (or medical staff that received training on early rehabilitation) Risk assessment and rehabilitation assessment After the patient has been referred to the rehabilitation department, a deeper assessment has to be done to identify the exact needs of the patients in terms of early rehabilitation and set up the exercise/treatment plan. To do so, the person in charge should use the Assessment Form (see below). The first step of the assessment should consist in doing a risk assessment. The purpose of the risk assessment is to identify situations in which early rehabilitation is contra-indicated or in which special attention should be paid when providing early rehabilitation services (relative contra-indications and precautions). To do so, the person in charge should use the Rehabilitation Risk Assessment Form (see below). Exercise plan The next step is to set up an exercise plan. This step consists in deciding which exercises need to be done with the patient, using the result and the information gathered during the rehabilitation assessment. To record the exercises that need to be done, the person in charge should use the Exercise Plan (see below). Provision of early rehabilitation and treatment follow-up The exercises that were set up can now be provided to the patient on a regular basis (at least once/day). While providing early rehabilitation services, the person in charge should regularly (once/week) check the patients improvement in order to adapt the treatment plan. This is called treatment follow-up. If the treatment plan needs to be updated, such updates should be recorded in the exercise plan. While providing early rehabilitation services, it is important not to forget about teaching and information to the patient and/or his/her family. The patient should learn exercises he/she can do on his/her own; he/she should also be provided with recommendations and informed on his/her situation. To do so, the person in charge should use the information brochures and the exercise cards (see part 4 of the manual) Discharge and referral to community-based/institution-based rehabilitation services When the patients situation has improved enough, he/she will be discharged from the hospital. If he/she still needs longer-term rehabilitation services and those services are available at community level (communitybased rehabilitation services or institution-based rehabilitation services), the patient should be referred to one of those services.
Page - 19 Page
Note III Patient Management 1. The Blank Forms - The Early Rehabilitation Needs Assessment Form should be used to assess the patients needs in terms of early rehabilitation services. The form aims to help medical staff who lack information on early rehabilitation, identify patients in need of such services. The form is made up of a series of questions and if the answer to one of those questions is yes, it means that the patient is in need of early rehabilitation services and should, therefore, be referred to the rehabilitation department (or a staff that was trained on early rehabilitation). - The Rehabilitation Risk Assessment is a form that should be used to identify contraindications, relative contra-indications and precautions regarding the provision of early rehabilitation services. The form should be filled in before doing the rehabilitation assessment and the result of the risk assessment should be recorded on the rehabilitation assessment form. - The Rehabilitation Checklist Guidelines are guidelines (checklist format) that can be use by medical or rehab staff to identify the needs for early rehabilitation, according to the patients injury (there is one guideline per main injury). The form can also be used to monitor the provision of early rehab services. It is, somehow, a very simplified and summurized version of the PT protocols and, therefore, they should be used in parallel with this manual. - The Assessment Form should be used before starting to provide early rehabilitation services. The purpose of the assessment is to gather information on the patients situation and needs. The result of the assessment will then be used to set up the treatment/exercise plan. - The Exercise Plan is used to record the exercises that were prescribed at the end of the assessment. This form can also be used to record updates and changes made in the initial exercise plan during the treatment follow-up. 2. The Patient File The patient file is used to gather all the forms used for the patient. The file ensures that all the forms and the information they contain will remain available in one place. 3. The Patient Database The patient database is used to record the most important information regarding the patient such as his/her age, sex, address, injury, phone number, registration number, rehabilitation needs Such database has a two-fold purpose: first, it allows tracking the patients (when needed) and, second it allows getting a general picture of the services provided and outcome of services through statistics.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 20 Page
PART 2. THE EARLY REHABILITATION PROTOCOLS BY INJURY
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Early Early Early Early Early Early Early
Rehabilitation Rehabilitation Rehabilitation Rehabilitation Rehabilitation Rehabilitation Rehabilitation
Protocol Protocol Protocol Protocol Protocol Protocol Protocol
for for for for for for for
Amputation Bone Fracture Spinal Cord Injury Head Injury Bedridden Patients Peripheral Nerve Injury Burn
Page - 21 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS Early Rehabilitation Protocol for Amputation
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Amputation
1.1. Definition An amputation is the loss of a part of the body.
1.2. Causes The causes of an amputation can be various. The amputation can be caused by a traumatism (for instance: traffic accident, job accident, a fall), by an illness (cancer, leprosies, diabetes, gangrene caused by frostbite), or by a congenital deformity (a part of the body was missing when the baby was born). 1.3. Types Any part of the body can be amputated. The name given to the amputation depends on the part of the body that is missing. The main types of amputation are: The The The The The The The The The The The shoulder disarticulation (1) arm amputation (2) elbow disarticulation (3) forearm amputation (4) partial amputations of the hand (5) hip disarticulation (6) trans-femoral amputation (AK) (7) knee disarticulation (8) trans-tibial amputation (BK) (9) ankle disarticulation (10) partial amputations of the foot (11)
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 22 Page
1.4. Stump surgery The stump is the part of the amputated limb that remains (for example, in case of BK amputation, the stump is the part of the leg between the amputation and the knee). The quality of the stump depends on the quality of the surgery (the quality of the surgery does not depend only on the surgeon's skill but also on surgery conditions, on the condition of the stump before surgery, and on the general condition of the patient). A good stump condition is important to facilitate the patient's prosthesis fitting. There are rules for this surgery, and we present here 3 of the most important:
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Stump length (a) Bone covering (b) Special rules for the BK (below knee) amputation (c)
(a) Stump length The length of the stump is very important when fitting a patient with a prosthesis: a too short stump will give the patient difficulties in controlling his prosthesis well, and it will be more difficult for the technician to fit (if he has to adapt the prosthesis with, for example, a thigh belt above the knee). A too long stump will also give the technician problems (difficulties making the prosthesis alignment). For these reasons, the ideal length for a stump is when the amputation is made at the level of the medium third of the limb (this means: at least 10 cm below the proximal joint or 8 cm above the distal joint).
Between these 2 points (10 cm below the superior joint and 8cm above the inferior joint), all levels of amputation are possible and considered as ideal. The longest stump (between those two points) will help the patient to control his prosthesis (higher force). (b) Bone covering
After the surgeon cuts the bone and before he closes the stump, the surgeon must cover the bones extremity with smooth tissue (muscle and skin) in order to protect the stump. For that, in general, the anterior muscles of the stump are stitched up with the posterior muscles.
More or less 2 centimeters of smooth tissue is necessary to cover the extremity of the bone well. If there is less than 2 cm, the extremity of the bone will be prominent below the skin and could create pain or a wound. If there is too much smooth tissue (more than 2 cm), the extremity of the stump will be too floppy and will complicate the patient's prosthesis fitting.
Page - 23 Page
(c) Special rules for BK amputation For Below Knee amputations, there are 2 rules that must be followed during surgery:
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
The anterior part of the extremity of the tibia should be cut obliquely so it wont hurt and the bone wont grow. The fibula should be cut 2 cm shorter than the tibia.
1.5. Complications Possible amputation complications are varied:
Infection (a) Exostosis (b) Neuroma (c) Phantom pain (d) Muscle shortness (e) Muscle weakness (f) Stump oedema (g)
(a) Infection Like any kind of wound, the scar after an amputation is an open door to bacteria or a virus. An infection could appear easily at the scar. This infection can also go up to the bone and cause a major infection (osteomyelitis). In that case, the patient will need new surgery; otherwise the infection can become general and even kill the patient). (b) Exostosis Exostosis is an abnormal bone growth. After amputation, sometimes the extremity of the cut bone can grow. This bone growth appears below the skin and can cause pain or a wound. The only possible treatment for exostoses is surgery. It often happens when the tibia was not cut well, obliquely, as explained previously.
(c) Neuroma Neuroma is an abnormal growth of a nerve that was cut during amputation. The nerve grows in a ball. If the skin is closed over it (it lies just below the skin), that zone can be very painful (kind of electric shock when we touch it). In this case also, the only solution is surgery.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 24 Page
(d) Phantom pain Phantom pain is an abnormal sensation around the amputated limb. The patient has the impression, for example, that the foot which was amputated is still painful (the patient feels pain in the foot that does not exist anymore). The real cause of this pain is unknown. Some theories say that the part of the brain that was responsible for the sensation of the amputated limb starts to work abnormally, which lead to perception that the body part still exists. Other theories say that the sensory nerve that was cut will still send messages to the brain. Since the messages that were carried by that nerve were coming before the amputation from the amputated limb, the brain interprets them as still coming from the same place (the amputated part of the limb).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Those pains are not dangerous but they can be very boring because they can be present for a long time after amputation. Nevertheless, most patients say that the pain decreases after a while, even without treatment. (e) Muscle shortness After the surgery and before receiving prostheses, the patient wont use his amputated limb much. In that case; some muscles might become shorter very quickly. This mainly happens with the hip flexors, the hip abductors and the knee flexors (for lower limb amputation) and with the shoulder adductors and elbow flexors (for upper limb amputation). Muscle shortness might be a problem for the use of prostheses (if the knee or hip flexors are too short, the ranges of motion in the hip or the knee will be decreased which will make walking difficult) (f) Muscle weakness For the same reason as for the muscle shortness (non-use of the amputated limb), the muscles around the limb might quickly become weaker. Weak muscles will make the use of the prostheses quite difficult as using prostheses requires stronger muscles than usual. This is particularly true with the lower limb amputation; walking with prostheses requires strong hip extensors, hip abductors and (if the amputation is below the knee) knee extensors. (g) Stump oedema Stump oedema very often occurs right after the surgery and is a normal reaction. But if it persists and is not addresses properly, the oedema will make the fitting of prostheses harder. When starting to use the prostheses, the stump will, at first, quickly become thinner (the oedema will decrease). If the stump becomes much thinner (which will happen if there is still swelling in the stump when the prostheses is produced), a new prostheses will be needed after only a few days. 1.6. Notions about the prosthesis Prostheses are fake limbs that are made to replace the missing part of the amputated limb. There are two main kinds of prostheses: The lower limb prostheses (a) The upper limb prostheses (b)
Page - 25 Page
(a) The lower limb prostheses The BK (Below Knee) prosthesis The BK prosthesis corresponds to an amputation at the level of the leg (the tibia -below the knee joint and above the foot). It is composed of 3 main parts:
The socket (1) The pipe (ppp or metal) (2) The foot (3) The AK (Above Knee) prosthesis The AK prosthesis corresponds to an amputation at thigh level (the femur below the hip joint and above the knee joint). It is composed of 4 main parts:
The The The The
socket (1) knee (2) pipe (metal) (3) foot (4)
Note: There are also other types of prostheses for the lower limb amputation, such as the hip disarticulation prosthesis (that includes a hip joint), the knee disarticulation prosthesis (which look like the AK prosthesis but have some particularities with the socket) or the partial foot amputation. In a general way (which is not always true) we can say that the lower the amputation is, the easier it will be for the patient to walk properly with the prostheses. This means that a patient with a foot amputation should be able to walk better than a patient with BK amputation or a patient with knee disarticulation or with AK amputation. This can be explained by the fact that the less joints there are in the prostheses, the easier it gets to control it (controlling the prosthetic knee can be a bit difficult). Also, the weight-bearing site (the place where the patient takes support to bear his body weight on the prostheses) change from one prostheses to another and the weight-bearing site in a BK is better adapted than the weight-bearing site on an AK which makes it easier to walk. (b) The upper limb prostheses The forearm prosthesis Such prosthesis is composed of a socket and a prosthetic hand.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 26 Page
The arm prosthesis Such prosthesis is composed of a socket, a prosthetic elbow and a prosthetic hand.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Note: Nowadays, new technologies allow developing myo-electric upper limb prostheses. Those allow controlling the hand (and the elbow) using the muscles of the shoulder. Electrodes are placed on some muscles of the shoulder and by contracting them, the person can control the movements of the prosthetic hand and elbow. This makes those prostheses more useful because it is possible to control finer movements with mechanic prosthesis, the patient can just open and close the hand, which is not always very functional.
Page - 27 Page
2. PT Protocol for Amputees
After the patient has been hospitalized and, when needed, emergency medical care has been provided in order to stabilize the patient, it is necessary to make an assessment of his/her needs in terms of early rehabilitation. To do so, doctors or nurses in charge of the patient should use the Early Rehabilitation Needs Assessment Form (see annex). This form aims to help medical staffs that lack knowledge on early rehabilitation to identify the patients in needs of such services. Depending on the result of this simple assessment, the patient would or would not be referred to the rehabilitation department (or staff trained on early rehabilitation). Usually, all amputees should be referred for early rehabilitation.
2.1. Assessment Before setting up a treatment plan for an amputated patient, it is important to collect some information on the patient, on his/her history and on the amputation. Such information should be recorder in the assessment form (see annex). Beside the general information on the patient (name, age, sex), here is a non-exhaustive list of the main pieces of information that need to be collected: (a) History of the amputation What is the cause of the amputation? Was it an accident? What kind? Was it an illness? Which one? Is the amputation congenital (present from birth)? When was the patient amputated (date of amputation)? Which part of the body is amputated? The lower limb? Which part of the limb? The upper limb? Which part of the limb? Since the amputation, did the patient receive medical care (beside the normal scar care)? How was the healing of the scar? No infection? No complications? Since the amputation, did the patient receive rehabilitation care? What kind? For how long? What did it consist in? (b) Assessment of the stump How is the scar? Is it healed? Is it infected? Are there other wounds on the stump? How is the shape of the stump? Is it conic? Is it square? Is there oedema (compare the perimeter of the stump with the perimeter of the sound limb to confirm swelling)? How long is the stump? Too long? Too short? Is it the right length to produce a prosthesis? Are there complications such as exostoses? Does the patient feel pain in the stump? What kind of pain? When? (c) Assessment of the muscle strength Are the main muscles strong or is there weakness? Which muscles are weak? (d) Assessment of range of motion Is there any decrease of ROM? What causes that decrease of ROM? Muscle shortness or joint deformity? Which ROM is limited?
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 28 Page
(e) Assessment of the balance (if lower limb amputation) How is the patients balance? Can he maintain standing position? Can he jump? Can pick up something from the ground? (f) Assessment of function Does the patient face difficulties with daily life activities (moving around, feeding, dressing, using toilets)? What kind of difficulties? Gathering those pieces of information is important in order to be able to set up a treatment plan (what exercises to do) and to have a record of the patients situation before starting the treatment (such record will allow the PT evaluating the efficiency of the exercises later on during the treatment - by comparing the present situation and the initial situation such comparison allows to see if the patients abilities and condition are improving). 2.2. Treatment in the hospital (early rehabilitation) Early rehabilitation will take place in the hospital, starting as soon as possible after the amputation. The main purpose of the treatment will be to prevent complications from appearing and to prepare the patient and the stump for receiving a device. In order to do so, and according to the information collected during the assessment, the following exercises should be done with the patient: (a) Starting right after the surgery (day 1) Passive mobilization: Passive mobilization aims to prevent muscle retraction and decrease of ROM as well as other complications such as bedsores and blood circulation problems. All limbs should be mobilized, included (and especially) the amputated limb. For details, refer to the passive mobilization protocol. Active mobilization: Active mobilization aims to prevent muscle retraction and muscle weakness as well as other complications such as bedsores and blood circulation problems. All limbs should be mobilized, included (and especially) the amputated limb. For details, refer to the active mobilization and strengthening protocol. Positioning: The patient should learn which position should be avoided in order to prevent muscle shortness. Some of those positions cannot be completely avoided (for example, the sitting position is not a very good position for AK amputees, but we cannot ask the patient to avoid sitting for the whole day. In that, we should recommend him to avoid that position as much as possible and recommend him other positions which are better Position to prevent (for BK amputation)
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Laying on the back with a pillow under the knee
Sitting with the knee in flexion
Standing with the knee in flexion (taking support on the crutch)
Page - 29 Page
Position to recommend (for BK amputation)
Laying on the back with the knee in complete extension
Sitting with the knee in extension (using support for the stump)
Position to prevent (for AK amputation)
Laying on the back with a pillow under the thigh
Sitting
Standing with the hip in flexion (taking support on the crutch)
Position to recommend (for AK amputation)
Laying on the belly with a pillow under the thigh Other: if the patient has to stay in bed (bedridden patient), other common complications (respiratory problems, bedsores, blood circulation problems) also have to be prevented using specific methods. For details, refer to the bedridden patients protocol. Patient information and training: Information on the patients situation, his/her needs and his/her future should be provided to the patient or to his/her family. Information brochures can be used to do that. Also, when possible, the patient or his/her family should be taught how to do basic exercises by themselves. Material is also available to ease the teaching. For details, refer to the Teaching and informing the patient and his/her family members protocol. (b) Starting on day 2-3 Muscle strengthening: all limbs should be strengthen, included the amputated limb. For lower limb amputation, special attention should be given in strengthening the muscles important for a good gait (the hip extensors, the hip abductors and the knee extensors) and the upper limb (for walking with crutches). For classic muscle strengthening exercises, refer to the active mobilization and strengthening protocol. With lower limb amputees, the following three specific exercises can also be used:
Hip extensors (lift up the pelvis, count until 5, then
Hip abductors (lift up the pelvis, count until 5, then
Knee extensors (lift up the buttocks, count until 5, then
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 30 Page
rest. Repeat the movement 20 times, 3 times/day)
rest. Repeat the movement 20 times, 3 times/day)
rest. Repeat the movement 20 times, 3 times/day)
(c) Starting on day 3-4
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Standing up: The patient should get out of bed as soon as possible to prevent the common complications of bedridden patients. For details, refer to the transfer and mobility protocol. Balance in standing position: Some balance exercises can be done in standing position. For details, refer to the balance exercises protocol. Walking with crutches/walking frame: If the patient is amputated from one of the lower limbs, he should learn how to move around using crutches or a walking frame (if the balance is not good enough to use crutches). For details, refer to the transfer and mobility protocol. Using a wheelchair: If the patient has an amputation of both lower limbs, he should learn how to move around using a wheelchair. For details, refer to the transfer and mobility protocol. (d) Starting after the stitches have been removed (if there is no open wound or signs of infection) Stump bandage: the stump bandage aims to prevent or decrease the stump swelling and give a good shape to the stump. Rules to respect for the stump bandage: A bandage should be made in a figure of "8". We cannot do a circular bandage (this means that the bandage should always go up or down and not go in circles around the stump).
The pressure made by the bandage should be more at the extremity of the stump than at its proximal part (so it won't prevent the blood from circulating normally). The extremity of the stump should be completely covered by the bandage (the skin cannot be visible). There must not be folds in the bandage. The stump must not be painful. If it is, it means that the bandage is too tight. The PT should teach the patient how to do the bandage by himself, so he can put it on alone. The bandage should be reapplied everyday, after treatment, until the day of the first fitting (the day the patient receives his prosthesis).
Technique for AK stump bandage The bandage should be kept the whole day.
Technique for BK stump bandage
Page - 31 Page
Note: The same technique and rules can be used for upper limb amputation too.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
(e) Starting when the scar is healed Scar massage: The purpose of scar massage is to maintain the scar flexible by preventing it from getting attached to underneath tissues (like muscles or bones). This is important because an attached scar will make more difficult for wearing a prosthesis (the scar would be painful and wound can appear). Rules to respect during a scar massage: The patient should be installed in a comfortable position. The PT cannot use talcum powder for this kind of massage (because of the talc, the finger will slip and won't be able to "grab" the scar properly). Only fingers are used during scar massage (not the whole hand). The movements should always be made in the direction of the scar. The massage is not made directly on the scar but around it. The following techniques should be used:
Scar massage should be done for about 10 minutes, 2 times/day. Note: If for some reason the patient has to stay in bed for a long time after the amputation, he/she might develop bedridden complications. Those complications have to be prevented or addressed properly. To do so, PT exercises can be used. For details, refer to the PT protocol for bedridden patients. Note: If the patient complains from phantom pain, the following techniques can be used (their efficiency cannot be guarantied): Before using any kind of treatment, explain to the patient what is happening (the brain misinterprets messages) and that the pain is not linked to any kind of mental illness, its a very common problem that most of the time decreases and disappears after a while. TENS, acupuncture, medications (pain-killers, antidepressant, muscle relaxant), massage, heat or cold, ultrasound are reported as being useful to decrease phantom pain. An innovative technique uses a mirror box in which the sound limb and the stump are placed. The mirrors give the impression to the patient that the amputated limb is still there (the patient, thanks to the arrangement of the mirrors, sees two legs or two arms in the box while there is actually only one). Then, the patient moves the sound limb and he/she has the impression that the amputated limb is also moving. This can help to release phantom pain.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 32 Page
2.3. Treatment in the rehabilitation centre and in the community (long-term rehabilitation) Long-term rehabilitation will take place in a rehabilitation centre (or in a rehabilitation department in a hospital) and in the community. Note: For details on long-term rehabilitation, institution-based rehabilitation and community based rehabilitation, refer to the information brochure (Information on rehabilitation). (a) In a rehabilitation centre The main purposes of the treatment in a rehabilitation centre will be to provide the patient with a prosthesis and to teach him how to use it. In case of problems such as muscle shortness, muscle weakness, poor balance or stump problems, exercises will have to be done to address those problems before producing the prosthesis. Therefore, the treatment in the rehabilitation centre might be composed of the 3 following steps: Pre-fitting treatment (muscle stretching, muscle strengthening, balance exercises, stump bandage, scar massage, care of wounds). Production of the prosthesis Post-fitting treatment (exercises to teach the patient how to use the prostheses properly).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Note: For details on exercises done in a rehabilitation centre, refer to the training document (PT management of patient suffering from lower limb amputation).
(b) In the community Community-based Rehabilitation (CBR) program can be helpful for amputees in various ways: Home visit to check up on the general patients physical situation Home visit to check up on the device (does it still fit? Is it broken?), and referral to specialized structure (rehabilitation centre) if needed Guidance for home accessibility Guidance for access to school or vocational training centre or job Participation to self-help groups Awareness raising activities for the community members on disability-related issue (disability, rehabilitation, disabled persons needs and abilities).
Page - 33 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS Early Rehabilitation Protocol for Bone Fracture
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Bone Fracture
1.1. Definition and causes A bone fracture can be defined as a break in a bone (the bone is "broken"). Fractures generally happen because of a trauma (a hit on the bone, a fall, a car accident), but it also can be the result of a weakened bone (the bone may become weaker because of a disease, such osteoporosis or because of repetitive stress - during intensive sport activities, for example - such as stress fracture).
1.2. Types of fracture Here are some of the main kinds of fracture:
Comminuted fracture A fracture of many relatively small fragments
Open fracture A fracture which breaks the skin
Simple fracture The bone broke into two pieces; the two parts of the bone did not move
Multiple fracture More than one bone is broken or the same bone is broken in different places
Greenstick fracture A fracture in which the bone bent but is not completely broken
Spiral fracture A fracture which runs around the axis of the bone
Displaced fracture: The bone is broken into two pieces and the two parts of the bone moved Closed fracture: The bones which broke do not penetrate the skin
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 34 Page
1.3. Diagnosis In general, doing an X-ray is the best way to confirm a fracture. X-rays are a form of electromagnetic radiation (like light); they are of higher energy, however, and can penetrate the body to form an image on film. Structures that are dense (such as bone) will appear white, air will be black, and other structures will be shades of gray depending on density (the higher is the density, the whiter they appear). The X-ray on the right shows a double fracture (multiple fracture) of the tibia and the fibula.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1.4. Complications The complications of a bone fracture can appear directly or can appear during the consolidation of the bone (the healing process). Direct complications The bones are the place of production of blood cells. Therefore, a fracture of a bone will generally be accompanied by internal bleeding (hemorrhage). If there is displacement of the fractured bone, the fractured extremity of the bone may damage internal organs. This may happen, for example, with a fracture of a rib that will pierce the lung (pneumothorax) or a fracture of the iliac bone that will pierce the bladder.
The fractured extremities of a broken bone may also damage blood vessels or nerves (peripheral nerve injury). This may happen, for example, with a fracture of the head of the fibula that will damage the fibular nerve or with a fracture of the ulna that damages the ulnar nerve. If the patient presents with peripheral nerve injury, refer to the corresponding protocol for details on the exercises that can be done. If the fracture is located on the spine or the skull, it can lead to spinal cord or brain damage and, therefore, paralysis.
Late complications If the fracture was open, it can lead to infection (bone or other tissues)
Page - 35 Page
A fracture can have problem to heal. This phenomenon is called pseudarthrosis (the bone doesn't heal).
Compartment syndrome: compartments are groups of muscles in the limbs that are covered by a tough membrane that cannot expend easily. Within those compartments, there are also nerves and blood vessels. Severe swelling on the fracture site will cause pressure on the blood vessels because the membrane cannot expend much, which would decrease the blood supply to muscles and nerves. The decreased blood supply will lead to nerve damaged and muscle death. This most often happens with fracture of the legs bones (tibia and fibula).
Note: Patients with fractures that require staying in bed for a long time (complex fractures, tractions, fracture of the spine) may develop other types of complications that are linked to the fact that they have to stay in bed. Those are called bedridden patient complications. It is, for example: muscle weakness, muscle retraction, breathing problems, blood circulation problems, digestive problems For details, see below. Note: Plaster or other types of immobilization will generally lead to muscle problems around and close to the fractured bone. Those are: muscle weakness (the muscles dont work, so they become weaker) and muscle shortness (the muscle stay for a long time in a short position and then become shorter). Note: Victims of earthquake (or other natural disaster) that suffer from fracture might also present with crush injury or soft tissues injuries. If the patient suffers from crush injury or soft tissue injury, refer to the reference document on crush injury syndrome (available on the capitalization DVD) 1.5. Medical treatment To heal properly, a fractured bone should be realigned if displaced (the realignment of a displaced fractured bone is called "reduction") and immobilized. There are different ways of reducing and immobilizing a broken bone: Methods of reduction If there is no displacement, no reduction is needed. If there is a slight displacement, the reduction can be done without chirurgical intervention (without operation). This can be done by doing traction on the bone (manual traction or using weights). If the displacement is too important, surgery will be needed to reduce the fracture. In this case, the reduction is said "open reduction" (because the surgeon cuts the skin to reduce the fracture).
Traction
Open reduction
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 36 Page
Methods of immobilization The most common way of immobilizing a bone is using plaster or splint. If the fracture is open, external fixation might be recommended to prevent from having plaster on the wound and risk infection. External fixation involves a surgery. External fixation is done with a device that supports the bone and holds it in the correct position while it is healing. An example of external fixation is shown on the drawing below. If the fracture is complex (comminuted, spiral, multiple), internal fixation might be the only way of stabilizing the bone. Internal fixation involves a surgery. It is generally done by using metal rods, screws or plates that remain in place in the bone after the surgery. Examples of internal fixations are shown on the drawings below.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Note: Unless the internal fixation causes problems, it is not necessary or desirable to remove it.
Plaster and splint
External fixation
Internal fixation
1.6. Healing process Healing is the process of recovery of the integrity of an injured system, such as a fractured bone. The healing process of a fracture bone occurs in 4 different stages: 1. Right after the injury, the integrity of the broken bone is provisionally restored by a blood clot (the blood clot takes the space left by the fracture between the bone fragments). 2. During the second stage, the blood clot will be replaced by fibro-cartilaginous tissue. This fibrocartilaginous tissue is called the callus. The callus is an irregular mass of tissue (it is bigger than the broken part) and it is not yet strong bone tissue. Meanwhile, the dead bone tissue is removed.
Page - 37 Page
The X-rays here below show different stages of the healing process of a broken bone:
The fracture is well visible
Here we can see the callus in the middle of the femur
The callus disappeared and has been replaced by mature bone tissue. The new bone tissue has been remoulded in order to give back the bone its original shape. The new bone tissue is still visible (whiter).
In general, we consider that it takes 6 to 8 weeks for a bone to heal, but in some case a longer immobilization might be required (a vertebra needs 10 to 12 weeks to heal completely). Note: The time necessary for healing is influenced by various factors, such as: The patients age (younger people heal faster than older people) The nutrition (varied food such as milk, rice, vegetables, meat) speed up the healing process The type of immobilization (using internal or external fixation help healing faster because they dont allow any movement in the bone while a plaster doesnt always stabilize the bone very well) The blood supply (more blood means better healing. Blood supply can be increase through exercises such as PT exercises) The type of fracture (complex fractures such as comminuted or displaced or multiple fractures- take more time to heal then simple fractures) The location of the fracture (some bones need more time to heal then others)
The table here below presents the average time needed for healing for the main bones of the body with a cast: Bone fractured Iliac bone Femur Patella Tibia/Fibular Ankle Time for healing 2 to 6 weeks 12 weeks 6 weeks 6 to 8 weeks 6 weeks Bone fractured Humerus Ulna/radius Wrist Vertebra Time for healing 4 weeks 6 weeks 3 to 8 weeks 10 to 12 weeks
Note: The above table is just informative. As already explained, there are so many variables that can influence the time needed for healing that it is always recommended to have the doctors green light for starting exercises such as weight-bearing and mobilization.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
3. The 3rd stage corresponds to the replacement of the fibro-cartilaginous callus by mature bone tissue. At that stage, the bone tissue is not yet lined up with the rest of the bone. 4. The last stage is the remoulding stage. During that stage, the bone tissue is re-organized in the right direction (the bone is ordered into parallel and concentric layers that are aligned in precisely the right way).
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 38 Page
2. PT Protocol for Patients with Bone Fracture
After the patient has been hospitalized and, when needed, emergency medical care has been provided in order to stabilize the patient, it is necessary to make an assessment of his/her needs in terms of early rehabilitation. To do so, doctors or nurses in charge of the patient should use the Early Rehabilitation Needs Assessment Form (see annex). This form aims to help medical staffs that lack knowledge on early rehabilitation to identify the patients in needs of such services. Depending on the result of this simple assessment, the patient would or wouldnt be referred to rehabilitation department (or staff trained on early rehabilitation). Usually, all the patients with fracture should be referred for early rehabilitation.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
2.1. Assessment Before setting up a treatment plan for a patient with bone fracture, it is important to collect some information on the patient, on his/her history and on the complications. Such information should be recorded in the assessment form (see annex). Beside the general information on the patient (name, age, sex), here is a non-exhaustive list of the main pieces of information that need to be collected: (a) History of the fracture and the treatment Which bone is broken? Where? What kind of fracture was it? When and why the bone was fractured? What kind of immobilization is used? Cast? External fixation? Internal fixation? What kind of internal fixation? (b) Assessment of the complications How are the ROM? Is there any decrease of range of motion? If yes, which movements have limitations? How severe is the limitation? How is the muscle strength? Is there any muscle weakness? Which muscles are weak? How severe are the weaknesses? If the patient had surgery, how is the wound? Is there any sign of infection? 2.2. Treatment in the hospital (early rehabilitation) Early rehabilitation will take place in the hospital, starting as soon as possible after the patient has been hospitalized. The main purpose of the treatment will be to prevent complications from appearing or to treat complications that are already present. Doing exercises also helps the fracture to heal faster as they increase blood circulation around the fracture. In order to do so, and according to the information collected during the assessment, the exercises here below should be done with the patient. The exercises are presented by type of fracture. When needed, refer to the protocols by techniques for futher details.
Note: The timeframe given hereafter are only informative and shouldnt be considered as universal reference. Indeed, there are many variables that will influence the healing process and the possibility to start some exercises at the expected time. Before starting exercises such as weight-bearing, mobilization or strengthening, the doctors approval should be sought. Nevertheless, the timeframe given hereafter provides the PTs with a clearer idea on when to seek for such approval.
Page - 39 Page
(a) Shoulder fracture Timeframe Exercise Passive mobilization Description Elbow, forearm, wrist, fingers (and sound upper limbs and lower limbs, if needed). For details, refer to passive mobilization protocol. Elbow, forearm, wrist, fingers and (and sound upper limbs and lower limbs, if needed). For details, refer to active mobilization and strengthening protocol. Forearm and hand muscles. For details, refer to active mobilization and strengthening protocol. Neck, forearm and hand. Use cold (ice or pack) to decrease the pain in the shoulder. See below Shoulder in all direction as tolerated (no stretching) (abduction, flexion, external rotation +++) Shoulder in all direction as tolerated and possible (no stretching) (abduction, flexion, external rotation +++) Deltoid, biceps, triceps Teach the patient how to actively lower the head of the humerus Shoulder in all direction (no resistance) (abduction, flexion, external rotation +++) Light stretching in all directions as tolerated (abduction, flexion, external rotation +++) Shoulder in all directions (abductors, flexors and external rotators +++) Shoulder in all directions (abduction, flexion, external rotation +++)
Active mobilization Day 1 week 3 Strengthening
From day one on
Massage Ice pack/ice cube Pendular exercise relaxing exercise Passive mobilization and
Day 2/3 week 3
Mobilization passive assisted
Form week one
Isometric contractions Humerus head lowering exercises Active mobilization
Week 3 week 6
Stretching
Strengthening From week 6 on Stretching
Here are examples of exercises that the patient can do by him/herself for the elbow fractures: Pendual exercise Stand. Lean forwards. Let your arm hang down. Circle your arm clockwise & anti- clockwise. Repeat 10x2 times.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Note: In the treatment plans described here below, the obvious (such as active mobilization and/or strengthening of sound limbs, prevention of other complications if the patient stays in bed, as well as stretching and/or strengthening of some muscles after immobilization and consolidation) are not always described. The priority in those plans is given to the injured parts of the limb during the time the patient will probably stay in the hospital. It is up to the therapist to complete those plans with other exercises he/she would consider relevant according to the patients situation and needs.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 40 Page
Relaxing exercise
Stand or sit. Let your arm hand down (or the arm can be in the arm sling). Circle you shoulder clockwise and anticlockwise. Repeat 10 times.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Passive mobilization
Lying on your back. Support your operated arm with the other arm and lift it up overhead. Repeat 10 times.
Passive mobilization
Lying on your back. Grasp a stick in both your hands. Lift the stick up and gently take overhead until you feel a gentle stretch in your shoulder. Repeat 10 times.
Active mobilization
Standing in front of a wall. Put you hand on the wall and climb up using your fingers. Try to reach as high as possible. Repeat 10 times.
Stretching internal rotators
Lying or sitting. Put your hands behind your head, and gently stretch the elbows towards the floor/ backwards to feel a gentle stretch on the front of your shoulders. Repeat 5 times. Standing with your hand on the wall. Flex the elbow to 90 degrees & hold the elbow close to your body. Gently turn your body away until you feel a stretch at the front of the shoulder. Hold for 5 seconds. Repeat 10 times. Lying on your back, keeping the elbow to your side. Hold a stick in your hands. Move the stick sideways, gently pushing the hand on your operated arm outwards. Repeat 10 times. Standing with your arms behind your back and grasp a stick between them. Gently lift the stick up away from your body. Repeat 10 times.
Stretching internal rotators
Stretching internal rotators
Stretching flexors
Strengthening extensors
Standing with your back against a wall. Keep the arm close to your side, elbow bent. Push the elbow back into the wall. Hold for 5 seconds. Repeat 10 times. Only use less than half your maximum effort.
Page - 41 Page
Strengthening abductors
Standing side on to the wall. Push arm into the wall. Do not allow the operated arm to move. Only use less than half your maximum effort. Hold for 5 seconds. Repeat 10 times.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Strengthening external rotators
Standing, with elbow flexed to 90 degrees, and held close to body, grasp the wrist of the affected arm with the good hand. Attempt to move the hand of the affected arm outward resisting the motion with the good hand. Keep the affected arm still. Only use less than half your maximum effort. Hold for 5 seconds. Repeat 10 times.
(b) Humerus fracture Timeframe Exercise Active mobilization Description Finger and wrist (and sound upper limbs and lower limbs, if needed). For details, refer to active mobilization and strengthening protocol. If cast: Light passive mobilization of shoulder joint (abduction and flexion, no rotations). If internal fixators: Passive-assisted mobilization of shoulder joint (abduction and flexion, no rotations) with good support (from the therapist) on the fracture. If possible: Passive mobilization elbow, wrist and fingers. For details, refer to passive mobilization protocol. Forearm and hand muscles. Isometric contractions of deltoid. For details, refer to active mobilization and strengthening protocol. Neck, forearm and hand. All upper limb. All upper limb. Shoulder and elbow, against light resistance and good support (from the therapist) on the fracture. No resistance applied below the fracture for strengthening exercises of the shoulder. Then increase slowly the resistance, depending on needs.
Passive and passive assisted mobilization
Day 1 week 6 (immobilization period)
Strengthening
From week 6 (after immobilization)
Massage Passive mobilization Active mobilization Strengthening
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 42 Page
(c) Elbow fracture Timeframe Exercise Ice-pack / ice cube Description
Day 1 day 10 (immobilization period)
From day 10 to week 3 Week 3 to week 6
From week 6 on
If possible, apply clod on the elbow to decrease pain. Passive, passive assisted and Shoulder, hand. If there no fracture of the active mobilization epicondyles or the trochlea, the wrist can also be mobilized. Massage Neck, forearm (not too close to the elbow) and hand. No elbow mobilization before 10 days even with internal fixation!!!! Mobilization passive assisted Elbow in flexion-extension and light pronation-supination Active mobilization and All upper limb (except elbow and forearm strengthening and except wrist if fracture of epicondyles or trochlea). Active mobilization Elbow in flexion-extension (+++) and pronation-supination Strengthening Elbow in flexion-extension (+++) and pronation-supintaion (start with light resistance and increase progressively) Stretching Stretching with participation of the patient (active mobilization plus stretching force applied by the therapist) in flexion (+++) and extension (++).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
(d) Forearm fracture Timeframe Exercise Passive, passive assisted and active mobilization Description
During immobilization (1 month if internal fixation / 3 month if cast)
After immobilization
Shoulder, fingers. If internal fixation (after 2 weeks): wrist (flexion-extension) and elbow (flexionextension) Strengthening If cast: isometric contraction wrist flexors-extensors and elbow flexorsextensors No pronation-supination!!!!! All upper limb (no resistance, then light resistance for elbow and wrist in flexion Active mobilization and and extension). strengthening After 8 weeks: active mobilization pronation-supination forearm (no resistance then light resistance)
(e) Wrist fracture Timeframe During immobilization (3 to 6 weeks) After immobilization Exercise Passive, passive assisted and active mobilization Active mobilization strengthening and Description Shoulder, elbow, fingers.
All upper limb (hand, elbow +++) Wrist (flexion-extension). No resistance, then light resistance
Page - 43 Page
(g) Pelvis fracture With pelvic fractures, the time of immobilization might vary a lot depending on the stability of the fracture (which part of the iliac bone is fractured) and the type of immobilization (cast or internal fixation). Timeframe Exercise Massage Chest therapy Active mobilization strengthening. During strict immobilization Description
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Both lower limbs Refer to chest therapy protocol. and Both upper limbs. Ankle, foot, toes. Isometric contractions (back, abdominal muscles, hip extensors and abductors, knee extensors and flexors except the muscles that have insertion on the fractured part of the iliac bone). Passive mobilization Patella. Knee if passive flexion of the hip joint is allowed. No mobilization of the pelvis!!!!!!! Passive mobilization Active mobilization Strengthening Transfers Strengthening Hip (abduction, flexion, extension +++) Hip (abduction, flexion, extension +++) Isometric contractions hip extensors, abductors adnd knee extensors Learning to change position Sitting position and sitting up Lower limb muscles (hip extensors, abductors and knee extensors +++) Standing with partial weight bearing. If the fracture is located on 1 side of the pelvis, the weight bearing is first done on the sound leg. If both sides of the bone are fractured, the weight bearing should be done on the arm. First with walking aids (parallel bars, walking frame, crutches), then without.
After strict immobilization (the patient is still immobilized, but he/she can change position)
After immobilization (2 months)
Weight-bearing
Gait training
(h) Hip fracture If there is no internal fixation, the treatment will look like the one for the pelvis fracture (see above). Here below is a treatment plan for the fracture of the hip joint (neck of femur, intertrochanter line, trochanter fracture) with internal fixation. The timeframe for standing and weight bearing should be confirmed with the doctor because it will depend on the type of fixation that was used, the patients general conditions (age, type of fracture, difficulties during surgery) and the patients weight. Timeframe Exercise Chest therapy Active mobilization Strengthening From day 2/3 on From day 4 on Sitting Passive and active assisted mobilization Description Refer to chest therapy protocol) Upper limbs. Ankle and foot Isometric contraction (knee extensors, hip extensors +++ and knee flexors). Sitting in bed. Hip: flexion-extension adduction and abduction-
From day 1 on
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 44 Page
From day 8 on
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
From day 15 on
From day 21 on
From day 30 on From day 60 on
No hip rotation, no leg elevation (lift up the leg with the knee in extension)!!!! Isometric contraction of hip abductors. Strengthening Knee extensors against resistance (sitting with the legs out of the bed). Without weight-bearing (walking with movement of the lower limb and with the Standing and walking foot touching the ground but without weight bearing). Balance exercises in standing position Balance exercises without weight bearing. For details, refer to balance exercises protocols. Partial weight bearing (a few kilos only) Weight bearing Walking with partial weight-bearing (a few Walking kilos only) Hip and knee muscles, with light Strengthening resistance, then increase. Walking with two crutches Walking Hip internal rotation Active mobilization Walking without crutches Walking Hip external rotation Active mobilization
(i) Femur (body) fracture Without internal fixators: Timeframe Exercise Active mobilization Strengthening Description Ankle, foot, toes. Isometric contraction knee extensors (+++), knee flexors, hip extensors and abductors. After 2/3 weeks, if possible (traction): slight flexion-extension hip and knee Hip and knee (see hip fracture) with good support (from the PT) on the fracture. Standing and walking without weight bearing Partial weight bearing and increasing. The whole lower limb
During immobilization (6 weeks)
Active mobilization Passive, passive assisted and active mobilization Standing and walking Standing and walking Strengthening
After immobilization (week 7 and 8) After consolidation (week 9)
With internal fixators: Timeframe Exercise Active mobilization Strengthening Description Ankle, foot, toes. Isometric contraction knee extensors (+++), knee flexors, hip extensors and abductors. After 2/3 weeks, if possible (traction): slight flexion-extension hip and knee Hip and knee (see hip fracture) with good support (from the PT) on the fracture. Standing and walking without weight bearing Partial weight bearing and increasing. The whole lower limb
During immobilization in bed (2/3 weeks) After immobilization (week 3 to 6) After consolidation (week 7)
Active mobilization Passive, passive assisted and active mobilization Standing and walking Standing and walking Strengthening
Page - 45 Page
(j) Knee fracture With cast: Timeframe During immobilization (6/8 weeks) Exercise Active mobilization Strengthening Active mobilization and strengthening Stretching Passive and passive assisted mobilization Standing and walking After consolidation (after 3 months) Standing and walking Strengthening Description Hip (passive assisted if necessary), ankle, foot, toes. Isometric contraction knee extensors (+++) Hip, ankle and foot Hip, ankle and foot (if needed). Knee (flexion-extension) Standing and walking without weight bearing (but with movement f the leg and the foot touching the ground) Partial weight bearing and increasing. The whole lower limb
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
After immobilization (week 7 to month 3)
With internal fixation: Timeframe Exercise Active mobilization From day 1 Strengthening Passive mobilization Active mobilization strengthening Active mobilization Standing and walking After consolidation (after 3 months) (k) Leg fracture Timeframe Exercise Active mobilization During immobilization in bed Strengthening Description Hip (passive assisted if necessary), foot, toes. Isometric contraction knee extensors, hip extensors and hip abductors (+++) Isometric contraction ankle dorsal and planter flexors. Standing and walking without weight bearing Hip, knee extensors. Knee (flexion-extension) Standing and walking without weight bearing (but with movement f the leg and Standing and walking Strengthening Description Hip (passive assisted if necessary), ankle, foot, toes. Isometric contraction knee extensors (+++) Knee flexion-extension. Hip, ankle and foot Knee flexion-extension (with help) Standing and walking without weight bearing (but with movement f the leg and the foot touching the ground) Partial weight bearing and increasing. The whole lower limb
and
After 10 days
During immobilization (out of bed) (day 8 if internal fixation)
Standing and walking Strengthening Passive and passive assisted mobilization Standing and walking
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 46 Page
the foot touching the ground) Standing and walking Strengthening Partial weight bearing and increasing. The whole lower limb
After consolidation
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
(l) Ankle fracture Timeframe Exercise Active mobilization Strengthening Description Hip, knee (+++), toes. Hip extensors and abductors Isometric contraction knee extensors (+++) Isometric contraction ankle dorsal and planter flexors. Ankle Ankle Standing and walking without weight bearing (but with movement f the leg and the foot touching the ground) Partial weight bearing and increasing. The whole lower limb
During immobilization (cast)
After the cast has been removed
Passive and passive assisted mobilization Active mobilization Standing and walking Standing and walking Strengthening
After consolidation
Note: In case of lower limb fracture (especially lower parts of the lower limb tibia/fibula, ankle or foot), when the patient stands for the first time (usually after staying in bed for a few days), he/she will probably feel pain in the foot (like if the foot was going to explode). This pain is due to the blood that rushes back in the foot when standing for the first time. When this happens, the patient should sit back down when the pain is too high, lift up the foot and move the toes to help the blood to go back up the leg. The patient should then try to stand for a few minutes as often as possible until the pain is gone.
2.3. Treatment in the rehabilitation centre and in the community (long-term rehabilitation) Once they left the hospital, most of patients that suffered bone fracture (unless there are other problems secondary to the fracture peripheral or central nervous system damage, for example- or to the fact that the patient had to stay in bed) wont require long-term rehabilitation. If they do, details can be found in other protocols (according to the reason why the patient needs long-term rehabilitation).
Page - 47 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS Early Rehabilitation Protocol for Spinal Cord Injury
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Spinal Cord Injury (SCI)
1.1. Definition A Spinal Cord Injury (SCI) is a lesion to the spinal cord resulting in a change, either temporary or permanent, of normal motor, sensory, or autonomic function. It can cause paralysis of limbs, loss of sensation and loss of control of body functions (bladder, bowel, temperature,) under the vertebral level of the lesion.
1.2. Causes The causes of SCI can be various. It is mainly caused by trauma (for instance: traffic accident, labor accident, a fall, crushing under heavy objects ). Spinal Cord Lesions can also be caused by illness (cancer, infection to the spine, Tuberculosis).
1.3. Types and classification of SCI The following terminology has developed for SCI: Tetraplegia = upper and lower limbs are affected Paraplegia = lower limbs affected only Complete lesion = no motor or sensory function is preserved in sacral segment S4 S5 Incomplete lesion = motor and sensory function is preserved below the injury level
The most used classification for SCI is the American Spinal Injury score (ASIA). It is done through a motor and sensitive testing on the patient. This motor and sensitive testing provides, together with body exam, one of the following scores to the patient:
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 48 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
A = Complete: No motor or sensory function is preserved in the sacral segments S4-S5. B = Incomplete: Sensory but not motor function is preserved below the neurological level and includes the sacral segments S4-S5. C = Incomplete: Motor function is preserved below the neurological level, and more than half of key muscles below the neurological level have a muscle grade less than 3. D = Incomplete: Motor function is preserved below the neurological level, and at least half of key muscles below the neurological level have a muscle grade of 3 or more. E = Normal: motor and sensory function are normal Example: ASIA score B C7 (= sensory function preserved below C 7 level) The overall treatment process of the SCI patient will be divided in: Acute phase treatment (after onset of SCI in Intensive care and orthopaedic treatment). This period last from onset of injury up to 3 to 4 weeks depending on the level of injury. Rehabilitation phase (Physiotherapy occupational therapy nursing education). This period can last from 5 weeks (low lesions) up to 7 months (high tetraplegic lesions) depending on the injury. Integration phase (home integration economic integration community adjustment) . This period takes up from one year op to three years.
1.4. Orthopaedic treatment of the Spine after Spinal Cord Lesion Generally, after the accident or onset of SCI a patient will get orthopedic treatment after his vital functions are stable (breathing independently, management of shock phase, normal blood pressure, wound care if applicable..). It can consist of:
Immobilization with trunk orthosis
Surgical fixation
Cervical traction
Whatever the orthopedic management is chosen, the main principles of this treatment should ensure: Correct alignment of the spine Avoiding compression between the vertebra
Both principles will avoid more neurological damage in the short and long term. During the orthopedic treatment phase, occurrence of pressure ulcers, loss of range of motion and loss of muscle power in the non affected limbs should be avoided at all cost by: Correct positioning in bed for the patient to prevent pressure ulcers and deformities Basic breathing exercises in relation with treatment in ICU (tracheostomy assisted breathing) Mobilize the affected limbs twice daily Active exercises for the non - affected limbs and body parts .
Page - 49 Page
Monitoring and advice for treatment prescription should be given by the surgeon and referent doctor during this period. 1.5. Complications Varying according the level of injury it can be said that generally the consequences of Spinal Cord Injury are a loss of muscle power, paralysis, muscle tone imbalance, loss of sensation, urinary incontinence, faecal incontinence, orthostatic hypotension and autonomic dysreflexia. If these consequences are not well managed the following main complications can occur: Pressure ulcers Spasticity Loss of range of motion Stiffness and/or retraction Pain Urinary infection Constipation Cardio-vascular deficit Loss of muscle mass Respiratory infections Bone density imbalance
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
To prevent these complications from occurring or becoming a significant problem for the quality of life of the patient, it is important that the medical and paramedical team working around the patient and his family do cooperate and share knowledge with each other. Complications like pressure sores, urinary infections, constipation, bone density imbalance, cardio-vascular deficit, respiratory infections and pain do need an interdisciplinary approach. They are however mainly managed by the doctor and nursing team but do need attention, understanding and participation from the Physiotherapy Team. The complications on which the physiotherapists will mainly act are: a) loss of range of motion and muscle mass b) respiratory infections and cardiovascular fitness c) spasticity d) stiffness and/or retraction Inevitably, the patient with SCI will have difficulty in avoiding these complications. The physiotherapist will act on these from the early acute phase on, through the rehabilitation phase up to the integration phase with a varied treatment plan .
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 50 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
(a) Prevention of loss of Range of Motion and muscle mass In the acute phase the patient should receive passive mobilization once his vital signs are stabilized in ICU. Passive mobilization of upper and lower limbs should be done at least twice a day. Gradually as the patient recovers from the shock phase, the muscles above the lesion should be exercised and strengthened with active and resistive exercise while maintaining maximum range of motion. The muscles and joints below the lesion level should be passively moved in full range of motion and/or stimulated with active assistive exercise if the lesion is incomplete. During the rehabilitation phase, the patient should be familiar already with this exercise routine learned in the acute phase (ideally done by himself or with a member of his family). As the patient will have gained not be dependant on intensive care anymore, he will have to learn now motor skills that will allow him to increase his mobility in bed, from bed to wheelchair and (if possible) community or therapeutical gait. This phase is a key component where the physiotherapist has to play a central role in increasing motor independence for the patient. For the integration phase, the motor skills learned from the Therapist will have to be maintained through self exercise and recreational activity (like sports). The physiotherapist will have to see the patient from time to time on how he manages his mobility and should detect and intervene if sudden loss of muscle power and mass occurs (b) Prevention of respiratory infections and cardio vascular problems During the acute phase cardio - pulmonary monitoring will be central to the recovery of the patient. His breathing movements will not be functioning normally (paralysed breathing muscles, low vital capacity, absent cough reflex, low blood pressure) and secretions in his lungs will not be evacuated by natural way (need for aspiration through tracheo-stomy). Physiotherapists should be stimulating assistive breathing exercises as this stage, clapping combined with posturing (if possible) and upper limb movements to enhance breathing movements and evacuation of secretions. Once the patient can breathe by himself, active breathing exercises should start with incentive spirometry. During the rehabilitation phase, the repetitive exercise programs learned in the acute phase as well as more intensive activity when learning motor skills, will increase the vital capacity and cardio vascular situation of the patient. The PT plays also a role in treating orthostatic hypotension by reconditioning the patient in upright position first (especially for the high lesions and long-term bedridden patients). By using a progressive verticalizing program, the patient will learn again to adjust to the upright position to prepare his mobility in wheelchair and/or gait . During the integration phase, regular recreational exercise will maintain the pulmonary and cardio-vascular situation of the patient . (c) Spasticity Spasticity is a complex problem for the SCI patient. It is the result of a muscle tone imbalance. The patient will have difficulties in controlling certain movements under the lesion (lower limbs more frequently) . Spasticity is often combined with stiffness and pain also. The management of this problem should always be done in cooperation with the doctor (medicine prescription) and orthotist (prescription of positioning devices).
Page - 51 Page
Incertain cases, spasticity can be usefull (for gait exercises or pressure sore prevention) but should be managed at a tolerable level for the quality of life of the patient. During the acute phase, spasticity does not manifest itself often. However, regular joint range of motion exercise and positioning of limbs should prevent its negative effects as soon as possible During the rehabilitation phase, it will appear more likely and the patient will have to be prepared for this.Physiotherapy management focuses on gentle but firm range of motion movements of the affected limbs, Stretching where needed to achieve maximum range of motion, positioning exercises that reduce the intensity of the spasm (like weight bearing using gravity (during verticalisation), avoiding hyper extension of key joints of the lower limbs or limbs affected) and use of physical agents (pressure therapy, topical ice application) known to reduce temporarily the intensity of the spasms. Patient education is here the key. The PT should explain to the patient and give him feedback on the treatment therapies that have the best effect. For the integration phase, it is essential that the patient has learned which strategies of treatment work the best for him . It will be needed to have a regular follow-up by the rehabilitation team to monitor this problem. (d) Stiffness and/or Retraction Both of these complications that appear under the lesion level do have interactions with spasticity, loss of bone density, muscle metabolism after injury, changes in bone structure, around the joints as well as neuropathic pain. During the acute phase the PT will act on its prevention through the active and passive exercise program mentioned in point a). Special attention should be given to the ankle joint to be positioned in 90 degrees at least to avoid ankle foot drop. If the function of the hand needs to be developed (especially for the injury levels C 5 to C 7), the hand should be taped or positioned also to avoid retractions that could jeopardise functional hand grips needed for the rehabilitation phase. The rehabilitation phase will focus on self range of motion, positioning exercises, stretching of joints and muscles, by the PT to avoid the retractions and/or act upon them as soon as they appear by closely monitoring. Special attention should go to the hand function (positioning to prepare the functional hand grips for high lesions) with exercises and teaching new hand skills. During the integration phase, new retractions will appear and will be a part of the life of the patient as he gets older. Monitoring should be done on a regular basis by the rehabilitation team. Note: as a convention these four complications should always be a priority to be prevented managed through the treatment provided by the Physiotherapist . For the other complications the PT has also a role to play in the interdisciplinary setting by cooperating with the other medical professionals .
1.6. Known outcomes for patients with SCI in the long term Known research in spinal Cord Injury care and the results of the outcomes of standard treatment techniques show that a combined approach of medical care, functional rehabilitation and patient education give the best results to reach the best independence possible for the patient. There is no cure for Spinal Cord Injury yet but learning new skills and educating the patients on his options for the most independent life possible is today the best approach available supported by research and studies. As a general guideline the level of vertebral injury (complet lesion) can give clear outcomes on his mobility and level of independence and measuring the neurological injury (provided by the ASIA Score) can give a good basic information on the possible recovery the patient can achieve over a time line of
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 52 Page
one year. All incomplete lesions can give better general functional results then the complete ones. Cervical injuries Injury levels C1 to C3 will be dependant on ventilation support and control on their environment for communicating will depend on the facial muscles (mouth, chin and eyes movement). They will be wheelchair bound depending on outside help. Injury levels C4 to C6 will be able to have shoulder and basic shoulder elbow and hand function allowing feeding, grooming with technical aids. They are wheelchair bound for ambulation. Thoracic injuries Injury levels C7 to T 9: The patients will be able to use wheelchair independently and are independent for their Activities of Daily Living
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Lumbar Injuries Injury levels T10 L1: The patients are independent for wheelchair ambulation ADL and short distance gait is possible with orthotics and walking frame. Sacral Injuries Injury levels L2 S5: Patients are independent for ADL and ambulation with community gait possible for longer distance with technical helps.
Page - 53 Page
2. Physiotherapy Protocol for Spinal Cord Injury
After the patient has been hospitalized and, when needed, emergency medical care has been provided in order to stabilize the patient, it is necessary to make an assessment of his/her needs in terms of early rehabilitation. To do so, doctors or nurses in charge of the patient should use the Early Rehabilitation Needs Assessment Form (see annex). This form aims to help medical staffs that lack knowledge on early rehabilitation to identify the patients in needs of such services. Depending on the result of this simple assessment, the patient would or wouldnt be referred to rehabilitation department (or staff trained on early rehabilitation). Usually, all spinal cord injured should be referred for early rehabilitation.
2.1. Assessment Before setting up a treatment plan for an SCI patient, it is important to collect some information on the patient, on his/her history and on Spinal Cord Injury. Such information should be recorded in the assessment form (see annex). Beside the general information on the patient (name, age, sex), available in most general rehabilitation files in the department, here is a specific list of the main pieces of information that need to be collected if your need to be in line with general data in SCI (SCI data Core set): Name and particulars of the patient Birth date, Injury date, acute admission date, final inpatient discharge, total days of hospitalisation Gender, etiology of injury, spinal surgery, vertebral injury, ventilory assistance, associated injury, place of discharge ASIA Impairment scale at admission and at discharge. Your physiotherapy assessment form includes the basic motor testing for measuring strength and ROM of the patient in detail. Other information on the physical assessment should include: Pain assessment, spasticity assessment, sensitive assessment, balance assessment, transfer skills as well as presence of complications that are to be dealt with . The following scales to measure the progress on your patient are used now more widely: SCIM score (Spinal Cord Injury mesure) WISCI score (Walking index for Spinal Cord Injury) Boubee balance test Analogical visual pain scale Ashworth scale to measure the grade of spasticity of the muscles. These basic scores can help you to measure the progress on your patient (you have to do them regularly on the patient) and are an excellent tool to communicate with the other members of Your team . They also give a good indicator for your patient and his progress. It helps equally for the goal setting that your team and your patient has to do for the long term. 2.2. Treatment in the hospital (Intensive Care Unit acute phase) During this stage (3 days after admission up to two weeks) , the treatment focuses on: The respiratory function of the patient Preserving the range of motion of the upper and lower limbs Mobilize the affected and non affected limbs to ensure a good blood circulation Pay attention to positioning of hand and ankle joints to avoid retractions Pay attention to positioning of patient in Bed in regard to Pressure sore prevention.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 54 Page
Techniques used: Assisted breathing techniques following the chest movements of the patients and accompanying the diaphragm mobility if possible Clapping of chest to evacuate mucus in the lungs, combined with drainage positioning Full range of motion (passive first) of non affected limbs followed by active stimulation and exercise Full range of motion on the affected limbs (passive only) Explain self mobilisation technique to the patient for the non affected limbs Monitor hand and finger mobility Ensure dorsiflexion over 90 degrees for ankle passively and advise on positioning in 90 degrees.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
In this case, these techniques are appropriate no matter the level of injury encountered. The main aim s to conserve mobility, prevent respiratory complications and ensure blood circulation to avoid pressure sores. Ideally this treatment program should be repeated two times per day ing 40 minutes each. For details, refer also to the bedridden patients protocol Patient information: Information on the patients situation, his/her needs and his/her future should be provided to the patient or to his/her family. Information brochures (general information and prevention of pressure sores in the wheelchair) can be used to do that. 2.3. Treatment in the rehabilitation department (Rehabilitation phase) A. For this phase (from 5 weeks (low lesions) up to 7 months (for high lesions), the treatment plan has to be adapted accordingly the level of injury: It is important to inform the patient about the goals that he can achieve and the goals that he should not focus on. It is important to announce this to the patient and his family members (eventually with help from a psychologist or counselor). Level C 4 It is unlikely that patients with this level will come to the rehabilitation department early. Most of the physiotherapy skills this patient has to learn will revolve around: Exercising the facial muscles: chin movements facial expressions cheek movements and eyebrows with the help of a mirror. Explore shoulder movements Focusing on mobility of the muscles around the mouth tongue movements (use a straw as feedback tool) Maintaining the fullest range of motion of all body parts through passive mobilization and teach this to family members or attendants to be done twice a day Explaining the family attendants how to position the patient in relation to pressure sore prevention and grooming. Exploring verticalisation program for cardio-vascular purposes using abdominal binders Chest therapy: active breathing exercises upper respiratory muscles, stimulate cough reflex, incentive spirometry exercises and positive pressure breathing.
Level C4 C6 The patients can follow the exercise program for C4 level and should focus on additional skills relating to the upper limb mainly:
Page - 55 Page
Level C7 T9 The patients can follow all precedent exercise programs. According the outcome under C7, the patient is supposed to be independent on most aspects of life at the end of his rehabilitation program. His exercise program includes furthermore: Transfers from and to different heights and distances Dressing, ADL independently Teach self exercise to the patient for his ROM Muscle strengthening program and muscular mass increase of upper limbs Wheelchair skills for long distance ambulation Use of Standing frame for balance and muscle tone control Fall prevention when using wheelchair Wheelchair sports orientation endurance exercises Selection for tricycle adapted motor vehicle
Level T10 - L1 The patients presenting this level of injury can follow all the above mentioned protocol knowing their breathing function is not affected and hand function intact. They may pursue the following skills: Functional gait with KAFO orthotics, crutches and parallel bars Standing frame for balance and muscle control.
Level L2 S5 All above skills can be developed for these levels adding: Functional gait with AFO orthotics and forearm crutches for longer distances
B. For the treatment of specific complications encountered by the physiotherapists, the following precautions need to be taken into account: For spasticity The PT will play the role of reducing the effects of spasticity by positioning, stretching and mobilization of the fullest range of motion possible. The evolution should be monitored by measure scales. It is known that weight bearing of the spastic limbs (lower limbs mainly) decreases spasticity, stretching of specific spastic joints also as well as topical application of ice on the key muscles. Patient education is the key here to work on For stiffness an retractions If in the initial treatment phase retractions could not be prevented, special attention should be given to it by postural handling, stretching and positioning of joints .
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Mandatory progressive verticalisation program and upright sitting to prepare for wheelchair . Chest therapy should focus on active breathing exercises and diaphragm stimulation in order to allow the best breathing and airway evacuation possible Incentive spirometry exercises with feedback Consider positive pressure airway management if patient is tired Active assistive exercise on shoulder abduction and elbow flexion C5 Active assistive exercise on wrist extension and passive hand grip for C6 Maintain range of motion of shoulder and avoid over load of shoulder as well as subluxation in standing position. Hand glove taping to avoid retraction of finger extensors. Prevention program for pressure sores in wheelchair to teach to attendant Teaching family attendant to make correct transfers from bed to wheelchair. Prepare patient for introduction to and use of technical aids for upper limbs
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 56 Page
For pain Most of the patients have to deal with pain in their lives. the PT should collect information on the type and occurrence of pain . It is known that mobilization reduces the perception of pain in collusion with treatment from the other members of the team . 2.3. Treatment follow-up in the community (Integration phase) A Community Based Rehabilitation program can be helpful for SCI patients and their families in various ways: Home visit to check up on the general patients physical situation Home visit to check up on the living aids mobility aids and referral to specialized structure if needed Guidance for home accessibility Guidance for access to school or vocational training centre or paid employment Participation to self-help groups Awareness raising activities for the community members on disability-related issue (disability, rehabilitation, disabled persons needs and abilities).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
The treatment of a person with SCI is a Lifelong issue for him and his family members. It is known from research that SCI patients have a tendency to seek less medical attention after one to two years living with the injury. They tend to focus more on economic issues like income generation for their families, continuing education and acceptance in the community. Issues such as sexuality, mental health, marriage, social contacts, fertility will be more in their list of demands. This protocol is only a small guide for caring for SCI patients. You can find more information on the following websites and resources: www.iscos.org.uk; www.ascon.info ; www.pvo.org; www.paradoc.org; www.scire.org
Page - 57 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS Early Rehabilitation Protocol for Head Injury
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Head Injury
1.1. Definition and classification Head injury is a general term used to describe any trauma to the head, and most specifically to the brain itself. The head trauma may or may not result to brain damage (in this document, we will only give attention to the head injury that lead to brain damage because thats were physiotherapy is very important). The brain damage can directly result from the head injury (the head was hit by a hard object during a car accident or a fall or the skull was fractured and the brain was damaged) or it can be as secondary complications of the head injury (internal bleeding that causes lack of oxygen or swelling that causes pressure on the brain). Head injuries can be classified as follows: (a) Minor Head Injury A brief period of unconsciousness, or just feeling sick and dizzy, may result from a person banging their head getting into the car, walking into the top of a low door way, or slipping over in the street. In general, the effects of a minor head injury are not very severe and they only last for a few hours or a few days. They can include nausea, headaches, dizziness, impaired concentration, memory problems, extreme tiredness, intolerance to light and noise. (b) Moderate Head Injury A moderate head injury is defined as loss of consciousness for between 15 minutes and 6 hours, and a period of post-traumatic amnesia of up to 24 hours. Like those with a minor head injury, patients with moderate head injury are likely to suffer from a number of residual symptoms. The most commonly reported symptoms include tiredness, headaches and dizziness (physical effects), difficulties with thinking, attention, memory, planning, organising, concentration and word-finding problems (cognitive effects) and irritability (behaviour problem). For the majority of people these residual symptoms gradually improve, although this can sometimes take 6 to 9 months. (c) Severe Head Injury A severe head injury is usually defined as being a condition where the patient has been in a coma for 6 hours or more. These patients are likely to be hospitalised and will probably need long-term rehabilitation. Depending on the length of time in coma, these patients tend to have more serious physical deficits. 1.2. Causes (a) Primary causes We talk about primary cause when the trauma is the direct cause of the brain damage. Examples of primary causes are:
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 58 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
High acceleration or deceleration of the head (for example when a car hits a wall, the head suffers a high deceleration or when a stopped car is hit by another car, the head suffers a high acceleration). High accelerations and decelerations may result into brain injury if the brain is compressed against the skull.
Direct hit on the head (for example during a car crash or a fall). The direct hit on the head will cause a brain damage if the brain is compressed against the skull. Fracture. The fracture may result from the hit (car accident, fall). The fracture may cause a brain damage if the broken bone pieces damage the brain.
(b) Secondary causes We talk about secondary cause when the cause of the brain damage is not the trauma in itself but the complications of the trauma. There are two main secondary causes: Pressure on the brain. Pressure on the brain is generally caused by the swelling. As any kind of trauma, a trauma on the brain will results into swelling. The problem is that the swelling occurs in the skull, which is not extensible. Therefore, the swelling will create pressure on the brain and may lead to brain damage.
Note that pressure on the brain can also be cause by intracranial (inside the skull) bleeding. Lack of oxygen. The lack of oxygen is generally cause by intracranial bleeding. Indeed, during the trauma, small arteries inside the brain may be injured. If it is the case, the parts of the brain that are supposed to receive blood from those arteries will suffer from lack of oxygen.
Note that lack of oxygen in the brain can result from heavy blood loss in the body because of other injuries (for example, during a car accident, the victim will suffer a head trauma but also other injuries such as bone fractures that may lead to heavy loss of blood. The less blood remains in the body, the less blood can reach the brain). 1.3. Symptoms The symptoms that a person suffering from brain injury due to a head trauma may present are very wide and they depend on the part of the brain that was injured. Here are some examples of symptoms (this list of symptoms is not exhaustive): (a) Motor problems The most common motor problems head injured patients suffer are: Lack of muscle control (paralysis): the patient may suffer from total or partial paralysis of some parts of the body (the part of the body that are affected depend on the part of the brain that was injured). Balance problems: the patient often suffers decreased balance, especially if the cerebellum or the vestibular system (balance system inside the ear) were injured.
Page - 59 Page
(b) Sensory problems The patient may also suffer from total or partial loss of sensitivity in some parts of the body. (c) Cognitive problems Following a brain injury, people may present with a reduced conscious-level and/or cognitive deficit. In addition many people will have a period of stay in the intensive care unit (ICU), with a medically-induced coma to ensure safe mechanical ventilation. There is much clinical practice and evidence to support the early stimulation as part of rehabilitation after a brain injury, even when the conscious-level is reduced. The cognitive improvements can happen through rehabilitation, when areas of the brain not affected by the brain injury learn to take over the role of the damaged areas. What areas of cognition may be affected? Attention: Focused attention; divided attention Concentration Memory: Short term memory; long term memory Comprehension: Interpreting instructions; learning new information Language: Reading; writing; difficulty finding words; forming sentences correctly; describing things or situations Simple and complex mathematics Executive Function: Problem solving; decision making; planning; judgement ; organizing thoughts.
(d) Emotional and behaviour problems Emotional and behaviour problems are often linked with damage of the frontal lobe of the brain. The most common emotional and behaviour problems a head injured patient may suffer from are: Agitation: the patient cannot be quite. Explosive anger and irritability: exaggerated angry reaction to apparently minor annoyances such as misplaced shoes or a noisy vacuum cleaner. Disinhibition: the inhibition is a mechanism that allows us to leave in society as it is the mechanism that prevents us from speaking our mind our walk naked in the street. A patient suffering from disinhibition will, for example, speak his mind no matter what the circumstances, touching people inappropriately, and not considering the consequences of any action. Inability to express right feelings at the right time: the patient laughs or cries easily and not appropriately (the patient cries at an happy moment or laughs at the sad moment). Self-centeredness: the patient is only concerned with personal needs. Apathy: no interest in hobbies enjoyed previously, stay in chair all day
(e) Muscle tone problems The patient might suffer from spasticity or floppiness.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Lack of coordination: the patient has difficulties coordinating movements Dyspraxia: dyspraxia means that the patient has difficulties to do deliberate voluntary actions. It is different from lack of movement control. For example, a patient suffering from dyspraxia will be unable to bend his elbow when asked to by the therapist but that can look at his watch without problem (which involves bending the elbow). Speaking and swallowing problems: the patient may have difficulties controlling the muscles necessary for speaking or for swallowing. Lack of bowel and bladder control.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 60 Page
1.4. Complications Patients that suffered severe head injury might have to stay in bed for a long period of time. Therefore, they might develop the classic complications of bedridden patients such a pressure sores, muscle contracture, muscle weakness, respiratory problems, blood circulation problems (for details, refer to the bedridden patients protocol). Those problems will be worsened by the main problems the patient already has. Indeed, if the patient suffers from paralysis and lack of sensitivity, he/she is even more likely to develop pressure sores. The spasticity and the paralysis will fasten the appearance of muscle contractures. 1.5. Other problems Patient with head injury that occurred during an accident, a fall or an earth quake often will also have other problems such as bone fracture or amputation. Those will have to be addressed too. For details, refer to the relevant protocol.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Page - 61 Page
2. PT Protocol for Head Injury
After the patient has been hospitalized and, when needed, emergency medical care has been provided in order to stabilize the patient, it is necessary to make an assessment of his/her needs in terms of early rehabilitation. To do so, doctors or nurses in charge of the patient should use the Early Rehabilitation Needs Assessment Form (see annex). This form aims to help medical staffs that lack knowledge on early rehabilitation to identify the patients in needs of such services. Depending on the result of this simple assessment, the patient would or wouldnt be referred to rehabilitation department (or staff trained on early rehabilitation). Usually, all patients with head injury should be referred for early rehabilitation.
2.1. Assessment Before setting up a treatment plan for patient suffering from head injury, it is important to collect some information on the patient, on his/her history and on the complications. Such information should be recorded in the assessment form (see annex). Beside the general information on the patient (name, age, sex), here is a non-exhaustive list of the main pieces of information that need to be collected: (a) History What happened? How was the patient injured? When did it happen? Since he/she got injured, what kind of treatment did the patient received (medical, surgical and physical)? Which part of the head was injured? How badly (is there a fracture)? (b) Assessment of the symptoms Is the person conscious? Is he/she in the coma? Is he/she responsive? Is there muscle paralysis? Which muscles? How severe are the paralysis? Complete, partial? Are the paralyzed muscles spastic of floppy? Are there sensitivity problems? Where? Are there cognitive problems? What kind? How severe? Are there behaviour problems? What kind? How serious? (c) Assessment of the complications Besides the problems due to the head injury (the symptoms), is there any other complications linked to the fact that the patient has to stay in bed? How is the muscle strength? Which muscles are strong, which are weak? How is the joint Range of Motion? Is there limitation? In which joint? With which movement? What cause those limitations? Muscle shortness or bone deformity? Are there bedsores? Where? Since when? How do they look? Is there respiratory problem?
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 62 Page
(d) Check for other problem Beside the head injury, does the patient have other problems such as bone fracture or amputation? If yes, specific questions and checks have to be done for tat problem too. For details, refer to the corresponding protocols. 2.2. Treatment in the hospital (early rehabilitation) Early rehabilitation will take place in the hospital, starting as soon as possible after the patient has been hospitalized. The main purpose of the treatment will be to prevent complications from appearing or to treat complications that are already present. In order to do so, and according to the information collected during the assessment, the following exercises should be done with the patient: (a) Starting right after the hospitalization/surgery (day 1) Passive mobilization: Passive mobilization aims to prevent muscle retraction and decrease of ROM as well as other complications such as bedsores and blood circulation problems. As many joints as possible should be mobilized depending on the patients situation (if theres a traction or if the patient just had surgery, some joint cannot be mobilized). For details, refer to the passive mobilization protocol. Positioning: Positioning means to put the patient in a good position. A good position will be a position that helps preventing further problems (such as muscle retraction, joint deformities, bedsores) and that helps with already present problems such as swelling in the limbs. With head injured patients, a good position also takes into account the possible appearance of muscle spasticity (if not there yet). Therefore, the most common spastic muscles (those that are more likely to become spastic) have to be stretched in that position. Here are the best positions for patients with head injury and brain damage: Lying on the back Put a pillow under the head (to keep a slight flexion of the neck) and make sure that the head is straight (dont let the patient with the head falling on one side). Pull the scapula outwards and then put a pillow under the shoulder to keep the scapula in abduction. Put the upper limb in extension and abduction on the pillow, with the hand as opened as possible (if possible, the forearm should be in supination). The lower limb should be in slight flexion, hip abduction and hip external rotation. The ankle should be kept at 90. Lying on the side (unaffected side) The head is kept in slight flexion. Pillows are used to hold the affected shoulder in flexion and to prevent adduction. The elbow is in extension; the wrist in neutral position and the hand is as opened as possible. The lower limb is in flexion. Pillows are used to prevent the hip from being in adduction/internal rotation. Lying on the side (affected side) The head is kept in slight flexion. The affected shoulder in flexion (the adduction cannot be prevented in that position). The elbow is in flexion; the forearm in supination, the wrist in neutral position and the hand is as opened as possible. The lower limb is in extension (while the unaffected lower limb is in flexion on pillows to stabilize the position).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Page - 63 Page
Note: Lying on the back and lying on the unaffected side should be preferred to lying on the affected side as this last position might hurt the affected shoulder. To prevent complications when lying on the affected side, the patient should actually be in half-side lying position not completely on the side) and pillows should be put behind the back to prevent him/her from turning on the back. Note: With patients with brain damage, a good position in bed (head and trunk straight, upper and lower limbs in the recommended positions) is also very important for development. Indeed, a patient that is well positioned will have a better view and what is around him/her, he/she will get much more stimulation than if he/she is in a bad position. And the more stimulation the patient gets, the best he/she has to recover. Therefore, positions like the one shown on the drawing on the right should be prevented. Chest therapy: Chest therapy aims to prevent respiratory problems. It is very important to do with patients that are more likely to develop lung infection (older patients, smokers, patient that have already been in bed for a long period, patients that will probably have to stay in bed for a long time). For details, refer to the chest therapy protocol. Active mobilization: Active mobilization aims to prevent muscle weakness and muscle retraction, as well as blood circulation problems. It also helps to prevent respiratory problem and bedsores. As many joints as possible should be mobilized depending on the patient situation (traction, immobilization, surgery) and abilities (paralyses). For details, refer to the active mobilization and strengthening protocol. Strengthening exercises: Strengthening exercises aim to prevent muscle weakness. As many muscles as possible should be strengthen, depending on the patient situation (traction, immobilization, surgery) and the patient abilities (severe weakness, paralyses). For details, refer to the active mobilization and strengthening protocol. Note: Strengthening exercises should not be used (at least at first) for paralyzed muscles. Indeed, with brain damage, the problem is not with the muscle strength but with the muscle control. What the patient needs at first is to recover a good muscle control, not a good muscle force. Therefore, what he/she really needs is early stimulation exercises, which will help him/her to recover muscle control. Plus, strengthening exercises tend to increase the spasticity. Massage: Deep massages aim to prevent blood circulation problems. Superficial massages help relaxing tensed and painful muscles as well as preventing pressure sores. Deep massages should be mainly done on limbs extremities (calf muscle). Superficial massage should be done on the whole body, especially on tense or painful parts (shoulder, back). Prevention of bedsores: For details, refer to the prevention of bedsores protocol. Patient information and training: Information on the patients situation, his/her needs and his/her future should be provided to the patient or to his/her family. Information brochures can be used to do that. Also, when possible, the patient or his/her family should be taught how to do basic exercises by themselves. Material is also available to ease the teaching. For details, refer to the Teaching and informing the patient and his/her family members protocol.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Sitting position When seated, the patient needs a pillow to support his upper limb in order to protect the shoulder joint (especially if the muscles of the shoulder are floppy). Pillows should also be laced on the sides of the trunk to insure that the patient sits straight.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 64 Page
(b) Starting after a few days (day 2 or 3) and depending on the patients improvements Early stimulation: For the paralysed limbs, basic early stimulation exercises can be used. The main muscles to be stimulated, at first, are the muscles opposite to the commonly spastic muscles an the muscles important for walking and standing and for functionality. This means that the muscles that need to be stimulated as soon as possible are: For the upper limbs: the scapula abductors, the deltoid, the triceps, the wrist extensors and the finger extensors and flexors (for grasping abilities). For the lower limbs: the hip flexors, the hip abductors, the hip external rotators, the knee flexors, the ankle dorsal flexors, the hip extensors, knee extensors and the ankle eversores (for the walking). Remember that with a patient suffering brain damage, the problem with the paralysed muscles is a problem of controlling them, not a problem of weakness (the part of the brain that was damaged cannot send motor messages to the muscles anymore). Therefore, trying to strengthen them by putting resistance wont help for a better control. Stimulation basically aims to have new connections created between the neurones in the brain and other parts of the brain taking over the damaged parts responsibilities. Strengthening doesnt help much at that point (it even might increase spasticity). Also, in the beginning, even if there is no response when trying to do the exercises, explain to the patient that he/she just has to keep trying. Trying to do a movement (thinking about a movement) stimulates the same parts of the brain as actually doing the movement. Therefore, just trying, even without any observable result, still helps for improving muscle control and creating new connections in the brain. To help the patient contracting the muscles, tapping can be used on the muscles that are supposed to be working (tapping means hitting or rubbing the muscles with the top of the fingers). Here are some examples of early stimulation exercises: For the scapula abductors The patient is lying on the back. His upper limb is vertical (the help needed to maintain that position is provided by someone holding the patients arm or by the patient him/her self if he/she can use the other arm to maintain that position). Then, the helper/therapist places his hand a few centimetres above the patients hand and ask him/her to touch the hand. To do so, the patient has to make an abduction of the scalpula to lift up the hand. For the deltoid The patient is lying on the back. The hand is placed on the opposite shoulder (the help needed to maintain that position is provided by the helper/therapist). Then, the patients arm is placed vertically (the elbow is up). In this position, without support, the elbow would fall down. The patient is then asked to try to slow down that fall (excentric contraction). If he/she can do it, then he/she is asked to stop the movement in the middle of the fall (isometric contraction). If he/she can do that, he/she is asked to lift up the elbow (concentric contraction).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Page - 65 Page
For the wrist extensors The patient is in any position. The forearm arm is hold in a way that without support, the hand would fall in flexion of the wrist. The patient is then asked to try to slow down that fall (excentric contraction). If he/she can do it, then he/she is asked to stop the movement in the middle of the fall (isometric contraction). If he/she can do that, he/she is asked to extend the wrist (concentric contraction). For the hand Stimulate the patient to grasp and release objects. Provide the help needed to grasp and release. When the patient grasps, pay attention that the thumb is always opposite to other fingers. For the hip flexors and the knee flexors The patient is lying on the back. The lower limb is put in flexion (hip and knee flexion) (the help needed to maintain that position is provided by the helper/therapist). I that position, without support, the lower limb would fall down in extension (hip and knee extension). The patient is then asked to try to slow down that fall (excentric contraction). If he/she can do it, then he/she is asked to stop the movement in the middle of the fall (isometric contraction). If he/she can do that, he/she is asked to flex the knee and the hip (concentric contraction). For the hip abductors and external rotators The patient is lying on the back. The lower limb is put in flexion (hip and knee in flexion) (the help needed to maintain that position is provided by the helper/therapist). The knee is put a little bit inwards in order that is it would be left without support, the knee would fall in (in adduction). The patient is then asked to try to slow down that fall (excentric contraction). If he/she can do it, then he/she is asked to stop the movement in the middle of the fall (isometric contraction). If he/she can do that, he/she is asked to bring the knee outwards (concentric contraction). For the ankle dorsal flexors and eversors The patient is lying on the back. The lower limb is in flexion (hip and knee in flexion). The help needed to maintain that position is provided by the helper/therapist. In that position, the patient is asked to try to lift up the forefoot from the bed (keeping the heel on the bed). If the patient can do it, the lower limb can be put a little more in extension. The more the limb is in extension, the more difficult the dorsal flexion will be for the patient. To stimulate the eversores, the patient should be asked to do that movement and to try to bring the 5th toe outwards.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
For the triceps The patient is lying on the back. The upper limb is placed vertically (the help needed to maintain that position is provided by the helper/therapist). I that position, without support, the hand and the forearm would fall down (the elbow would flex). The patient is then asked to try to slow down that fall (excentric contraction). If he/she can do it, then he/she is asked to stop the movement in the middle of the fall (isometric contraction). If he/she can do that, he/she is asked to extend the elbow (concentric contraction).
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 66 Page
For the hip extensors Ask the patient to do the bridge exercise.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
For the knee extensors The patient is lying on the back. Put a pillow under the knee and ask the patient to push the pillow down with the knee.
Outline of the first steps towards stimulating alertness and cognitive recovery. 1 Find a method of communication If unable to communicate with voice, then try to find a different method. Often people may be able to understand, if not long complicated sentences, then at least, short basic communication. However, if they are unable to communicate that they do understand, often patients are left with no way of communicating their needs. The long-term risk is a withdrawal, reduced alertness and a complete loss of communication. Therefore as soon as possible it is required to establish a way of communication. This may be possible by eyes (blink or vertical/horizontal eye movements), finger movement, toe movement. Note that it may be difficult to use grasp. If you place your fingers in their palm, this can elicit a grasp reflex. Communication can be helped with low-technology devices such as picture boards or word boards, expressing common needs: toilet, hunger, thirst, pain etc. Alphabet boards can be used as well to increase communication. High-technology devices include various computer assisted devices for patient-specific long-term use. 2 Increase environment stimulation If a patient presents with neglect, try to ensure that most activity happens on the side they are neglecting. Neglect means the patient has lost knowledge of the affected side. This may present in different ways, for example a visual neglect, loss of attention to the affected side or a motor neglect (meaning movement is possible, but is neglected). Overall it means the affected side does not exist in their orientation. Normally the neglected side will be the opposite to the brain injury, but it may be the same side as the brain injury. By orientating the patient to their hemiplegic side, this will facilitate improved cognition as well as normal movement. Position bed so the inattentive side faces the area of most activity, normally the door, where people come in and out. Place the TV or radio towards this side too.
Make sure that everyone addresses the patient from the neglected side. If too difficult, then aim to address the patient from midline (the mid-position) and try to slowly move more towards the neglected side. Advice family and relatives to do the same. 3- Find out your patients premorbid interests If your patient is unable to communicate, then ask family and friends. Make the family and friends bring in favourite music, books, newspaper, radio programme etc. When you know the patients interests you can talk about this during the treatment session. This may stimulate alertness. If the patient presents with reduced conscious level (GCS), it is still
Page - 67 Page
important to communicate with the patient, this may also stimulate an increase in alertness and attention. 4- Enhance sensory stimulation (hearing, vision, smell, sensation, taste)
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Hearing music, communication on topics of interest, radio programme etc. Vision pictures of family, friends, events Smell a favourite perfume, favourite smells (coffee brewing etc.) Sensation touch, massage, brushing/washing hair, passive range of motion exercises Taste Favorite foods and drinks. NB! If patient has a low conscious level and is not eating or drinking, this will not be possible, for safety reasons.
5 Retrain activities of daily living Due to the cognitive damage, the ability to plan, process and complete activities of daily living may be affected (see above description of cognitive deficits). Early rehabilitation focusing on activities of daily living will support the retraining of these skills, if possible. If the brain damage is too severe then compensatory ways of completing tasks of daily living can be trained. As written under point 3, it is important to know their premorbid interests and vocation, as patient treatment will be much more effective when you incorporate this into the rehabilitation session. For example, if a 10-year old boy likes playing football and has a favourite football team, then trying to play games with a football and chat about his favourite team, which may stimulate more alertness and attention versus playing cards. Or if an older lady likes playing cards, then doing activities with a game of cards even simple reaching and grasping, will be of more interest to her, than reaching and grasping for a wooden cone (often found in rehabilitation areas). A man, who has been working as a welder, will most likely also have an increased attention, when presented with common tools that he used in his work (however note safety). Obviously rehabilitation needs to focus on the impaired site (upper limb or lower limb etc.), but if cognition is poor, then firstly focusing on interests, in order to gain more alertness and attention is a priority. After increasing their attention, then it is much easier to work on rehabilitation of the affected area. 6 - Establish a routine with your patient We are all used to routines in our daily life and it is effective for the patient to have a routine established: knowing the day of the week, time of day, activities that will happen and at which time. Making a daily/weekly schedule of activities can help the patient relearn routines. Daily repetition of activities supports the re-learning. As soon as the patient is able to participate in the planning of a weekly schedule, incorporating his interests and joint rehabilitation goals for the week, needs to be done. Asking What do they want to be able to do? Obviously the goals will need to be realistic and the rehabilitation staff need to help the patient formulate, what is realistic. Who can complete early stimulation following a brain injury? Early stimulation as part of the rehabilitation following a brain injury is important and will support the overall recovery. This can be completed by rehabilitation staff or other healthcare staff, who have received training on basic rehabilitation. The family and friends also play a large role in this process and need be a main part of these activities. However, full scale cognitive rehabilitation is a very complex process incorporating problem-solving of basic to complex skills and will require rehabilitation staff, who have received specific training in this area.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 68 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Auto mobilization upper limb: As soon as possible, if only one side of the body is affected, the patient should learn to do automobilization of the upper limb. To do so, the patient uses his sound hand to grasp and hold the affected hand. The he/she lifts up both hand to mobilized the shoulder in all direction. To stimulate the patient to move in all directions, the helper/therapist can ask to touch his/her hand. The helper/therapist then puts his/her hand on different places (high, low, on the side). The patient should do auto-mobilization 3 times a day (each time, the patient does 20 movements). Stretching to decrease the spasticity: If the patient develops spasticity, stretching exercises can help decreasing it. In that case, the stretching techniques are a little bit different as the stretching position will stretch several groups of muscles at the same time, while when doing stretching exercises to make muscle longer, the therapist usually stretches only one group of muscle at a time. Here is a description of the basic stretching exercises for the upper limb and the lower limb:
Stretching for upper limb spastic in flexion 1. The scapula is pulled in abduction and "blocked" with a small pillow placed behind the shoulder. 2. The shoulder is slowly put in abduction-extension and external rotation. 3. The elbow is stretched in extension. 4. The forearm is put in supination 5. The hand and the wrist are put in extension.
Stretching for lower limb spastic in extension 1. The therapist does a flexion, abduction and external rotation of the hip. 2. The knee is flexed, as for the ankle (dorsal flexion).
Sitting in bed: The patient should be placed in sitting position as soon as possible. In the beginning, the sitting position might lead to headaches or dizziness. In such case, the patient maintains the sitting position as long as possible (just for a few minutes), then the next day he/she tries to maintain a little bit more. Balance in sitting position: Once the patient doesnt feel dizziness when sitting, balance exercises can be done in sitting position. To do so, the patient seats on the side of the bed (with the legs outside the bed). The needed support is provided by the helper/therapist. When the patient improves, the support is decreased. Then, when the patient can maintain the position alone, the helper/therapist can push the patient a little bit to improve his/her balance abilities. Another possibility is to ask the patient to move the upper limbs (to reach objects, for example). For other examples of balance exercises, refer to the balance exercise protocol. Transfers: Basic transfers such as moving in bed (turning, moving on the side), sitting up and standing up should be taught to the patient when he/she starts to improve his/her abilities. For details on transfers, refer to the transfer and mobility protocol. The usual exercises used with hemiplegic patients, for example, can be used. For details, refer to the training manual PT management of hemiplegic patients. Standing up: It is important to try to have the patient standing as soon as possible even if it requires a lot of support. Indeed, standing position is a very good position to prevent complications and it would help the patient improving faster. For details on transfers, refer to the transfer and mobility protocol. Balance in standing position: When the patient starts to stand, balance exercises in standing position can be done. One important thing to pay attention to when the patient stands is that he bears weights on the affected lower limb and that he is able to transfer
Page - 69 Page
body weight from one side to the other. Then, balance exercises can be done by pushing the patient, ask him/her to reach for things, or by decreasing the base of sustentation or cosing the eyes. For other examples of balance exercises, refer to the balance exercise protocol. Walking: Depending on the patient recovery speed, walking can be started in the hospital. The patient will need to learn to walk first with support provided by the helper/therapist. Then, he/she will have to learn to walk using walking aids (walking frame or crutches). For details on transfers, refer to the transfer and mobility protocol. Note: Head injured patient, in general, at first, will have to stay in bed for quite a long period of time. If it is the case, they might develop the common complications of bedridden patients. Therefore, some more exercises might need to be recommended. For details, refer to the protocol for bedridden patients. Note: The usual exercises used with hemiplegic patients, for example, can be used. For details, refer to the training manual PT management of hemiplegic patients. 2.3. Treatment in the rehabilitation centre and in the community (long-term rehabilitation) Long-term rehabilitation will take place in a rehabilitation centre (or in a rehabilitation department in a hospital) and in the community. Note: For details on long-term rehabilitation, institution-based rehabilitation and community based rehabilitation, refer to the information brochure (Information on rehabilitation). The needs in term of long-term rehabilitation will depend on the patients situation and his/her abilities and inabilities. Nevertheless, most of the head injured patients that had brain damage will need long-term rehabilitation in a rehabilitation centre and in the community to improve their physical abilities (moving, using the hand). They will also need support to answer their social needs (integration in the family and the community, participation to social activities, access to education or job). (a) In a rehabilitation centre The main purposes of the treatment in a rehabilitation centre will be to improve the patients physical abilities such as: moving around transfers use of hand, managing with daily life activities (feeding, dressing, using toilets). In the rehabilitation centre, the patient can also received assistive and orthopaedic devices. Note: For details on exercises done in a rehabilitation centre, refer to the training document (PT management of patient suffering from head injury). (b) In the community CBR program can be helpful for head injured patients in various ways: Home visit to check up on the general patients physical situation Home visit to do exercises and check up on the exercises done by the family and the patient (do they do correctly and regularly the exercises, are they still adapted?) Home visit to check up on the device (does it still fit? Is it broken?), and referral to specialized structure (rehabilitation centre) if needed Guidance for home accessibility Guidance for access to school or vocational training centre or job Participation to self-help groups Awareness raising activities for the community members on disability-related issue (disability, rehabilitation, disabled persons needs and abilities).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 70 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS Early Rehabilitation Protocol for Bedridden/ICU Patients
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Note: The information presented in this chapter usually applies for patients in ICU (Intensive Care Unit). Nevertheless, with ICU patients, due to their medical situation, further precautions need to be taken when providing early rehabilitation. For details, refer to the notes at the end of this chapter.
1. General Information on Bedridden and ICU Patients
1.1. Definition A bedridden patient is a patient that, for some reason, as to stay in bed for a long period of time. Such patient might quickly develop serious complications that are not directly linked with the reason why he has to stay in bed. Some of those complications might be life threatening, most of them might be disabling (leading to a disability even if the first problem wouldnt have lead to disability), and all of them will make the treatment more difficult (the patient will need more time to recover because the complications will also have to be addressed during the treatment- and/or he might not recover as well as he would have without complications). Most of those complications can be very easily prevented using simple exercises and teaching the patient or the caretaker. Therefore, adapted exercises have to be done to prevent the complications from appearing 1.2. Reasons for which a patient has to stay in bed The reason why a patient has to stay in bed can be various: multiple trauma, fracture of the spine, paralysis, severe disease, coma, surgery, head injury 1.3. Common complications The most common complications of bedridden patients are: Muscles weakness/atrophy (a) Muscle shortness (b) Pressure sores (bed ulcerations) (c) Respiratory problems (lung infection) (d) Blood circulation problems (e) Bone demineralization (f)
Physiotherapy exercises will aim to prevent thoses complications from appearing.
Page - 71 Page
(a) Muscle weakness/atrophy Description: A patient that has to stay in bed wont use much (or wont use at all) his muscles. Muscles that are not used regularly will quickly become weaker. Indeed, regular use of the muscle is needed to maintain proper and functional muscle strength. This weakening process is due to the fact that, when not usd, muscles will loose part of their cells (the less cell there is, the weaker the muscle becomes) and the remaining cell will become thinner and, therefore, less strong. The result is a thinner and weaker muscle (this process is also called muscle atrophy). Consequences: Muscle weakness would make it more difficult later on for the patient to stand (weakness in the muscles of the legs) or even to sit (weakness of the muscles of the trunk) or to use the hands (weakness of the muscles of the upper limbs). (b) Muscle shortness Description: If the patient always remains in the same position (lying or sitting), some of his muscles will stay in a short position (a position in which those muscles are relaxed). The muscles quickly adapt their length to the position in which they remain. This means that if a muscle remains in a short position for a certain time, it will become shorter. Once the muscle is shorter, it cannot be stretched as usual. This will result in decreased possibilities of movements in the joint (decrease of Range Of Motion or ROM). A classical example is the knee and hip flexors that become shorter when the patent remains in sitting position. Or the plantar flexors (calf muscle) that becomes shorter when the patient is in lying position (with drop foot). Consequences: Short muscles and consequent decreased ROM will lead to functional difficulties such as standing, walking or using the upper limbs. Indeed, if the knee flexors became shorter, the patient wont be able to extend the knee. Without knee extension, standing and walking is very hard.
(c) Pressure sores Description: Pressure sores are wounds that will appear on parts of the body where there is pressure on the skin close to a bone prominence. This is, for example the case on the side of the hip where the greater trochanter (of the femur) comes out and theres not much muscle around it. When the patient is lying on the side, the greater trochanter creates a point of pressure on the skin and stops the blood supply from reaching the skin on that particular area. Without blood supply, the skin dies and an ulcer (a wound) appear. Such wound is generally quite hard to heal.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 72 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Classic locations of pressure sores: Iliac crest (a) Greater trochanter (b) Patella and head of fibula (c) External malleolus (d) Internal condyle of femur (e) Internal malleolus and base of 1st toe (f) Back of the head (g) Shoulder (h) Elbow (i) Inside of the knees (j) Heel (k) Ischial tuberosity (l) Lower back (posterior part of sacrum) (m) Shoulder blades (scapula) (n)
Pressure sores can appear with any patient that stays in bed (or in a wheelchair), but patients with sensory problems (patients that can not feel), are even more likely to have pressure sores (patient that can feel will feel the pain before the pressure sore appear and they will change position automatically; but he cannot feel the pain, the patient wont change position). Consequences: Pressure sores are difficult to heal and require heavy medical attention. This will generally increase the length of the treatment (the patient will have to stay even longer I bed). Most important, pressure sores can easily get infected and such infection can be life threatening (the patient can die from such infection if it spreads to the rest of the body). (d) Respiratory problems Description: Respiratory problems means that the respiratory system will get infected (lung infection such as pneumonia). With bedridden patients, lung infection will occur because the patient, when staying in bed, as a lower breathing magnitude than usual (he will do smaller breathing movements).
Consequences: The lower breathing results in a lower flow of air in the respiratory tracts (trachea, bronchii and bronchioles). The lower flow of air in the respiratory tracts will results in a less efficient expectoration system (the expectoration system is the system that allows the pulmonary secretions to climb up the respiratory tracts and to get out of the lungs). The decreased expectoration system leads to accumulation of secretions in the lungs, which can easily get infected (if the secretions stay in the lungs they will easily get infected which leads to lung infection).
Page - 73 Page
(e) Blood circulation problems Description: The two main blood circulation problems that bedridden patients might suffer from are thrombosis and embolism. Both of them are caused by callus (clot of blood) that will form in the blood vessels. Normally, the blood stays liquid unless it is in contact with air (like when you cut yourself). When the blood is in contact with air, it start to form a clot to close the wound. But if the blood circulation is decreased in some part of the body, the blood might also form clot inside the vessel (a callus or a thrombus). This callus will decrease and eventually stop the blood circulation (the callus forms an obstacle to the blood) creating thrombosis (a stop of blood circulation). In other cases, the callus will get loose in the blood circulation. We then call it an embolus. This embolus will then reach smaller blood vessels, get stuck and stop the blood circulation there. We call that an embolism.
Blood clots will form faster when the blood circulation decreases (the speed of the blood circulating in the vessels decreases). This is the case with bedridden patients (indeed, blood circulation is stimulated by movements and bedridden patients dont move much so their blood circulation decreases). Consequences: Thrombosis and embolism will lead to tissue damages (the tissues that wont receive blood supply will die). Depending on where the thrombosis or the embolism is located, it can have huge consequences. For example, if an embolus gets stuck in a vessel that supplies a part of the heart in blood, it will lead to a heart attack. Another common type of embolism is called pulmonary embolism and it is caused by an embolus that gets stuck in a pulmonary artery. This will lead to breathing difficulties and in some case to death. (f) Bone demineralization Description: Bone demineralization (also called bone mineral density loss or disuse osteoporosis) means that the bone become weaker (it looses too much minerals and minerals make the bone strong). This happens when the bones are not simulated enough. Bones are stimulated when constraints are applied on them (for example, when walking, constraints the body weight- are applied on the bones. Those constraints help the bone to remain strong. Thats why astronauts also suffer from bone demineralization when they come back on earth). When a patient stays in bed, there are less constraints applied on the bones; this results in bone demineralization.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
The extra secretions staying in the lung (because of the less efficient expectoration system) will also influence blood oxygenation (the level of oxygen reaching the blood). Indeed, if there are extra secretions, they will decrease the oxygen reaching the end of the respiratory tract and reaching the blood. Oxygen is very important for a good recovery, so a lower oxygenation of the blood might also influence the speed at which the patient will recover.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 74 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Consequences: a demineralised bone is more fragile and would break quite easily. This might be a serious problem when the patient starts to stand after a long period in bed. If the bones of the legs are too weak, they might be able to bear the body weight.
Page - 75 Page
2. PT protocol for Bedridden/ICU Patients
After the patient has been hospitalized and, when needed, emergency medical care has been provided in order to stabilize the patient, it is necessary to make an assessment of his/her needs in terms of early rehabilitation. To do so, doctors or nurses in charge of the patient should use the Early Rehabilitation Needs Assessment Form (see annex). This form aims to help medical staffs that lack knowledge on early rehabilitation to identify the patients in needs of such services. Depending on the result of this simple assessment, the patient would or wouldnt be referred to rehabilitation department (or staff trained on early rehabilitation). Usually, all bedridden/ICU patients should be referred for early rehabilitation.
2.1. Assessment Before setting up a treatment plan for bedridden patient, it is important to collect some information on the patient, on his/her history and on the complications. Such information should be recorded in the assessment form (see annex). Beside the general information on the patient (name, age, sex), here is a non-exhaustive list of the main pieces of information that need to be collected: (a) History Why does the patient have to stay in bed? What pathology does is suffer from? Since when is in bed? For how will he/she have to stay in bed? Since he/she is in bed, did the patient receive medical care? Since he/she is in bed, did the patient receive rehabilitation care? What kind? For how long? What did it consist in? (b) Assessment of the main reason why the patient is in bed Depending on why the patient is in bed in the first place (the primary problem), specific information will have to be collected on that problem. For example, if the patient is in bed because of spinal cord injury, specific information needs to be collected, specific questions have to be asked and specific test have to be done. (c) Assessment of the complications Besides the problems due to the primary problem (the main reason why the patient has to stay in bed), is there any other complications linked to the fact that he/she has to stay in bed? How is the muscle strength? Which muscles are strong, which are weak? How is the joint Range of Motion? Is there limitation? In which joint? With which movement? What cause those limitations? Muscle shortness or bone deformity? Is there bedsores? Where? Since when? How do they look? Is there respiratory problem? 2.2. Treatment in the hospital (early rehabilitation) Early rehabilitation will take place in the hospital, starting as soon as possible after the patient has been hospitalized. The main purpose of the treatment will be to prevent complications from appearing or to treat complications that are already present.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 76 Page
In order to do so, and according to the information collected during the assessment, the following exercises should be done with the patient: (a) Starting right after the hospitalization/surgery (day 1) Passive mobilization: Passive mobilization aims to prevent muscle retraction and decrease of ROM as well as other complications such as bedsores and blood circulation problems. As many joints as possible should be mobilized depending on the patients situation (if theres a traction or if the patient just had surgery, some joint cannot be mobilized). For details, refer to the passive mobilization protocol. Active mobilization: Active mobilization aims to prevent muscle weakness and muscle retraction, as well as blood circulation problems. It also helps to prevent respiratory problem and bedsores. As many joints as possible should be mobilized depending on the patient situation (traction, immobilization, surgery) and abilities (severe weakness, paralyses). In case of paralyses or severe weakness, passive-assisted mobilization can be used (the PT does the mobilization, but the patient helps as much as possible). For details, refer to the active mobilization and strengthening protocol. Chest therapy: Chest therapy aims to prevent respiratory problems. It is very important to do with patients that are more likely to develop lung infection (older patients, smokers, patient that have already been in bed for a long period, patients that will probably have to stay in bed for a long time). For details, refer to the chest therapy protocol. Strengthening exercises: Strengthening exercises aim to prevent muscle weakness. As many muscles as possible should be strengthen, depending on the patient situation (traction, immobilization, surgery) and the patient abilities (severe weakness, paralyses). In case of paralyses or severe weakness, passive-assisted mobilization can be used (the PT does the mobilization, but the patient helps as much as possible). Importance should be given to strengthen lower limbs muscles important for walking (hip extensors, hip abductors and knee extensors) and to the upper limb muscles important for walking with crutches and transfers (shoulder adductors shoulder abductors, elbow extensors). For details, refer to the active mobilization and strengthening protocol. Massage: Deep massages aim to prevent blood circulation problems. Superficial massages help relaxing tensed and painful muscles as well as preventing pressure sores. Deep massages should be mainly done on limbs extremities (calf muscle). Superficial massage should be done on the whole body, especially on tense or painful parts (shoulder, back). Prevention of bedsores: For details, refer to the prevention of bedsores protocol. Muscle stretching: If limitations of range of motion is already present, stretching exercises can be done to stretch the muscles or, at least, to prevent the muscle shorter from becoming worse. For details, refer to the muscle stretching protocol. Positioning: Positioning means to put the patient in a good position. For any bedridden patient, a good position will be a position that helps preventing muscle shortness and to decrease possible swelling. Depending on the primary problem of the patients, other rules will have to be followed as well for deciding which position is the best for the patient. Also, the therapist and the family should always keep in mind that any position, if it is kept for two long, will lead to complications (such as bedsores and muscle contracture). That is why, even if a position, for some specific reason, is good for a patient, the position has to be changed every two hours. Here are some rules that can be followed for good positioning of bedridden patients: When lying on the back, the patient should keep his/her head straight. If the patient always keeps the head on the side, he/she should be reminded to keep it straight.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Page - 77 Page
Attention should be given to the general position of the patient. On the drawings above are two examples: on the left, the wrong position and on the side the right one.
To prevent muscle contracture of the calf muscle (because of drop foot), special pillows can be used to hold the leg and the foot in neutral position. If such pillows are not available, normal pillows can also be used as shown on the above drawing.
In order to decrease or prevent swelling of the limbs, it is always better to try to keep the extremities of the limbs (hand and foot) a little bit higher than the rest of the body (elevation). This helps blood circulation and, therefore, help preventing and decreasing swelling. Besides those rules, it should always be recommended (when possible) that the patient try to sit up in bed as soon as possible. If the sitting position leads to dizziness, the patient should be asked to only stay in the position for as long as he can hold, then go back in lying position. Then the next day, he/she tries to hold the position a little bit longer. Patient information and training: Information on the patients situation, his/her needs and his/her future should be provided to the patient or to his/her family. Information brochures can be used to do that. Also, when possible, the patient or his/her family should be taught how to do basic exercises by themselves. Material is also available to ease the teaching. For details, refer to the Teaching and informing the patient and his/her family members protocol. 2.3. Treatment in the rehabilitation centre and in the community (long-term rehabilitation) Long-term rehabilitation will take place in a rehabilitation centre (or in a rehabilitation department in a hospital) and in the community. Note: For details on long-term rehabilitation, institution-based rehabilitation and community based rehabilitation refer to the information brochure (Information on rehabilitation). The needs in term of long-term rehabilitation will depend on the patient primary pathology. For details, refer to the corresponding PT protocol. Notes: Points to remember when providing early rehabilitation to ICU patients 1. Monitor physiological responses such as heart rate, blood pressure, respiratory rate, oxygen saturation and changes in level of consciousness at all times. 2. The physiotherapist should be aware of effects of positioning and mobility of the patient on the various monitoring devices and their readings. 3. The physiotherapist should always deal with the patient as if he/she were conscious and awake even if the patient appears not to be (talk to him and explain all procedures he is going through, and do not talk about his condition within his hearing). This may help to relax the patient and decrease patient anxiety and possible subsequent increase in muscle tone. 4. Frequency and intensity of treatment sessions will be determined by patient condition, but should generally be at least twice a day. 5. Treatment should be carried out at least 1 1/2 hrs after feeding time. 6. The physiotherapist must be aware of patient's medication, pertinent laboratory test result, patient's management by other health care team, and patient's / family concerns. 7. The physiotherapist should be familiar with all ICU procedures and equipment. For further details, refer to the PT protocol for ICU patients, in annex (on the capitalization DVD in English only)
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 78 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS Early Rehabilitation Protocol for Peripheral Nerve Injury
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Peripheral Nerve Injury (PNI)
1.1. Basics of the peripheral nervous system The peripheral nervous system is composed by the motor and sensory nerves that carry information. The motor nerves carry information (motor messages) from the brain to the muscles; the sensory nerves carry information (sensory messages) from the whole body to the brain. In case of peripheral nerve injury, some of the messages carried by the injured nerve may be stopped. In such case, the injury may result in paralysis and/or loss of sensitivity. The spinal nerves are made up of a certain number of axons, as we can see on the drawing on the right (cut of a nerve). (1) is the nerve; (2) are the axons.
The axon of a neuron is covered with a myelin sheet (A). This myelin sheet has a double purpose. First it protects the axons and, second, it increases the speed of the neural impulse (the nervous message). Indeed, if we look at the drawing, we can see that the myelin sheet presents some spaces between two sheets. Those spaces are called Ranvier's nodes. The neural impulse will actually jump from one Ranvier's node to the next one. Therefore, the neural impulse travels a shorter distance and so goes faster.
1.2. Definition of peripheral nerve injury A peripheral nerve injury means that a nerve has been damaged. The damage can be either partial or complete. Both sensory and motor nerves can be damaged.
1.3. Types of peripheral nerve injury There are different kinds of PNI. The main types are:
The total rupture of a nerve (or neurotmesis) (a) The partial rupture of a nerve (or axonotmesis) (b) The compression of a nerve (or neurapraxia) (c)
Page - 79 Page
(a) Total rupture of a nerve In case of total rupture, the nerve is completely cut into two parts. All the axons are cut. The messages cannot go through anymore; they all are blocked. (b) Partial rupture of a nerve In case of partial rupture, the nerve is not completely cut. Only a part of the axons are cut. Some of the messages can still pass. (c) Compression of a nerve In this case, the nerve is not cut, but it has been compressed for a while. Some of the axons may be destroyed or just inflamed. Depending on the gravity of the compression (duration, force), the messages may be completely stopped for a while. 1.4. Causes There can be quite a lot of causes to peripheral nerve injury. Here is a list of the most common causes: Open injury, such as a knife cut, bullet wound Closed injury, such as a pressure on the nerve (plaster, person stuck under a pile of rocks, wrong use of axillary crutches, bad position -"Friday night paralysis"), overstretching of the nerve (joint subluxation), bone fracture (the broken extremity of the bone damages a nerve), joint luxation (the luxated bone damages the nerve shoulder, elbow). Disease, such as tumour (the tumour compresses the nerve), nerve infection Circulatory problems (the blood circulation is cut and a nerve doesn't receive blood supply) Drugs, alcohol, poison
1.5. Symptoms Depending on the kind of nerve that is injured, the main symptoms are the following: If a motor nerve is damaged, it will result in flaccid paralysis or paresis of the muscles innerved by the damaged nerve. In case of paralysis, the muscles are completely paralysed (they don't work at all). In case of paresis, the muscles are slightly or incompletely paralysed (the muscles are "weak"). If a sensory nerve is damaged, it will result in loss or decrease of sensitivity. Peripheral nerve injury can also result in loss of reflexes.
Note: See below for a description of the most common nerve injuries (symptoms).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 80 Page
1.6. Evolution The evolution of the nerve injury depends on the kind of injury. If the rupture is not complete, the distal part of the injured axons will die, but the proximal part will grow again. Since the nerve was not completely cut, in general, the axons will grow back in the right direction. In such case, the paralysis may decrease or even disappear. Unfortunately, the growth speed for new axons is very slow (research till date shows that the growth speed is 11.5mm a day, depending on the extent of the nerve injury). If the rupture is complete, the distal part of the nerve will die. The proximal part of the nerve will grow, but since there is no more nerve girdle to guide the nerve growth, there is very little chances that the nerve will grow in the right direction. Very often, the nerve grows in a irregular way and forms a bundle. This nerve bundle is called a neuroma. In case of compression, the evolution really depends on the magnitude and time of the compression. In some case, if the compression was not too long or too hard, the axons won't get damaged; they will just be inflamed. When this happens, the paralysis may disappear once the inflammation reduces. If the compression was harder or longer, the axons may be partially or totally destroyed. In this case, the paralysis may remain until the damaged axons can grow back. 1.7. Complications Beside the symptoms explained previously, some complications may appear: Because of the paralysis, the paralysed muscles may suffer atrophy (muscle wasting). Indeed, the paralysed muscles won't be used as they are supposed to be used, therefore they will atrophy. Some muscles may become shortened. This contracture can occur at the level of paralysed muscles (because they stay in a short position) or at the level of the antagonist (opposite) muscles (because of muscle strength imbalance). If there is loss of sensation, the patient may suffer from infections. Indeed, if the feeling is lost, attention won't be paid to small wounds. Therefore, there is a risk that these wounds get infected. With loss of sensation there is also an increased risk of wounds, cuts and burns, if increased consideration is not paid to the environment and extra care taken. 1.8. The most common peripheral nerve injuries
Injured nerve Location Possible causes for injury - Shoulder dislocation - Compression on the shoulder pit (by axillary crutches) - Overstretching of the shoulder (during delivery) - Fracture of the neck of the humerus Innervation Symptoms
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Axillary nerve
Shoulder abductors
- Loss of shoulder abduction - Loss of sensation on the lateral aspect of the arm.
Page - 81 Page
Extensors of elbow, wrist and fingers
Elbow subluxation or fracture - Wrist subluxation or fracture - Knife cut - Fracture of the ulna or the radius
Pronators of forearm, flexors of wrist and fingers and oppositio n of the thumb
- Loss of forearm pronation - Loss of wrist and finger flexion Loss of thumb opposition - Loss of sensation on the anterior aspect of the hand and the three external fingers
Median nerve
- Compression of the nerve at the level of the elbow (posterior-internal face) - Fracture of the medial epicondyle of the humerus - Knife cut
Flexors of the fingers and abductor s and adductor s of the fingers
Obturator nerve
Ulnar nerve
- Loss of finger flexion - Loss of abduction and adduction of the fingers (the patient cannot hold a piece of paper between the fingers) - "Claw hand" (see picture)
- Fracture of the iliac bone - Surgery in the pelvic region
Adductor s and external rotators of the hip
- Loss of hip adduction - Loss of sensation on the internal aspect of the thigh
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
High level injury: - Shoulder dislocation Compression on the shoulder pit Overstretching of the shoulder Middle level injury: - Fracture of the humerus Compression on the humerus - Knife cut Low level injury: - Fracture of the radius - Knife cut
High level injury: - Loss of elbow, wrist and finger extension (wrist drop) - Loss of sensation on the posterior aspect of the arm and the hand and the three external fingers Middle level injury: - Loss of wrist and finger extension (wrist drop) - Loss of sensation on the posterior aspect of the hand and the three external fingers Low level injury: Loss of finger extension - Loss of sensation on the posterior aspect of the three external fingers
Radial nerve
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE Sciatic nerve VICTIMS
Page - 82 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
- Injection in the buttocks - Hip joint subluxation - Hip joint fracture
Knee flexors + muscles innerved by tibial and fibular nerves (see below)
- Loss of knee flexion - Loss of sensation on the posterior side of the leg, the sole of the foot and the external aspect of the foot. - + loss of movements controlled by tibial and fibular nerves (see below)
Rarely injured
Plantar flexors, inversore s and flexors of the toes
Tibial nerve
Loss of plantar flexion, inversion and flexion of the toes
- Compression of the nerve below the head of fibula (position, plaster, complication of surgery) - Fracture of the head of fibula
Dorsal flexors, eversores and extensors of the toes.
- Loss of dorsal flexion of the foot (drop foot) - Loss of eversion of the foot and extension of the toes. - Loss of sensation on the anterior aspect of the leg and the back of the foot
Fibular nerve
Page - 83 Page
2. PT Protocol for Peripheral Nerve Injury
After the patient has been hospitalized and, when needed, emergency medical care has been provided in order to stabilize the patient, it is necessary to make an assessment of his/her needs in terms of early rehabilitation. To do so, doctors or nurses in charge of the patient should use the Early Rehabilitation Needs Assessment Form (see annex). This form aims to help medical staffs that lack knowledge on early rehabilitation to identify the patients in needs of such services. Depending on the result of this simple assessment, the patient would or wouldnt be referred to rehabilitation department (or staff trained on early rehabilitation). Usually, all patients with peripheral nerve injury should be referred for early rehabilitation.
2.1. Assessment Before setting up a treatment plan for bedridden patient, it is important to collect some information on the patient, on his/her history and on the complications. Such information should be recorded in the assessment form (see annex). Beside the general information on the patient (name, age, sex), here is a non-exhaustive list of the main information that need to be collected: (a) History When and how did the problem appear? What seems to be the cause of the injury? (b) Location and type of the injury Which nerve seems to be injured? To identify the injured nerve, the therapist should take into account the cause of the injury (depending on the cause, some nerves may be injured, some other may not) and the symptoms (which muscles are paralysed and which parts of the body suffer from loss of sensation?). According to the symptoms (complete or partial paralysis) and the cause, the therapist should try to identify the type of injury (total rupture, partial rupture or compression). (c) Muscle evaluation The purpose of the muscle evaluation is to identify the paralysed muscles. During the muscle test, the PT "measures" the muscular strength of the patient. In general, a complete muscle evaluation is not necessary with patients suffering from PNI, since the paralysis or the weakness will be limited only to the muscles that are innervated by the injured nerve. This means that if the patient suffers an injury of the radial nerve of the left upper limb, muscle evaluation of the lower limbs or the right upper limb is probably not necessary; only the muscles of the left upper limb will have to be evaluated to identify which ones are weak or paralysed. (d) Sensation evaluation As we saw previously, when a patient suffers from peripheral nerve injury, beside the paralysis or the paresis, he may suffer from deficits in the superficial sensation; this means that he may not have normal feeling on some parts of the body. This can lead to skin complications (wounds, infections, burns). That's why it is important to test the sensation. Knowing the location of the reduced sensation may also help to identify the nerve that has been injured. Indeed, if the patient has lost sensation at the level of the back of the hand, it probably means that it is the radial nerve that has been injured.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 84 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
To check the superficial sensation, the therapist asks the patient to close his eyes and touches some parts of his body with 1. Something soft (cotton wool), 2. A sharp blunt item, 3. A test tube or other device with a hot substance (hot water) and cold substance (ice/very cold water). Caution needs to be taken with the assessment of hot and cold. The patient has to show where he was touched. If the patient is unable to show the place he was touched, it can mean that he has reduced sensation.
Note: The superficial sensation is the sensation of the skin. It is the sensation that allows us to know if something is hot or cold or if we are touching something. It is also the sensation that tells us when something is painful. (e) Joint evaluation We saw that one of the complications a patient may suffer is decreased range of motion. This decrease of ROM may appear at the level of the paralysed muscles (if they are not use, they will become shorter) or at the level of the antagonist muscles (because of muscle strength imbalance). That is why, it is important to test the ROM of the joints of the limb that suffers from the nerve injury (again, it is not necessary to test the joints of the lower limbs if the left upper limb radial nerve is injured). (f) Functional evaluation During the functional evaluation, the therapist should try to identify the difficulties the patient faces during his daily life activities (walking, eating, dressing, grasping). 2.2. Treatment in the hospital (early rehabilitation) Early rehabilitation will take place in the hospital, starting as soon as possible after the patient has been hospitalized. The main purpose of the treatment will be to prevent complications from appearing or to treat complications that are already present. (a) Starting right after the hospitalization (day 1) The principles of PT treatment for patients suffering from peripheral nerve injury are: Maintain muscles strength and strengthen the weak muscles Prevent muscle contracture Increase ROM if muscle shortening or contracture present Improve the patient's function Promote sensory re-education, to increase the normal sensory input
Therefore, the following PT techniques can be used: Active mobilization and muscle strengthening: Active mobilization and muscle strengthening aims to maintain muscle strength of the non-affected muscles, prevent muscle shortening and increase muscle strength of the affected muscles. Different techniques of active mobilization and muscle strengthening can be used (see the corresponding protocol for details Active mobilization and muscle strengthening protocol). Such exercises should be done for all weak muscles (muscles with paresis or incomplete paralysis). Active mobilization should also be prescribed even if the muscles seem to be completely paralyzed. Indeed, early stimulation of those paralyzed muscles may speed up the recovery of the damaged nerve.
Page - 85 Page
Passive mobilization: Passive mobilization mainly aims to prevent muscle shortening. As we saw above, either the paralyzed muscles or the opposite muscles to the paralyzed muscles (the antagonist muscles) are at risk of becoming shorter due to the nerve injury and the paralysis. For details about passive mobilization exercises, refer to the corresponding protocol Passive and passive assisted mobilization protocol. Note: To prevent muscle shortening, when available, splints can also be used. A splint is a device that maintains a part of a limb (for example the hand) in an anatomically good position in order to prevent muscle shortening. Muscle stretching: Some muscles will be prone to shortening and on assessment may already have shortened. Stretching exercises can be used to maintain current muscle length, prevent them from further shortening and to increase length if already shortened. For details on stretching exercises, refer to the corresponding protocol Stretching exercises protocol. Fine motor and functional exercises: If the injured nerve is a nerve of the upper limb and if this injury led to weakness or paralysis of certain muscles of the hand, fine motor exercises can be done. To do so, the therapist should use the material available (such as puzzles, small objects, balls). Sensory re-education: If the peripheral nerve injury has caused sensory loss, sensory re-education will be important. This rehabilitation covers the use of various objects and materials to be used on the affected body part, in order to stimulate normal afferent input to the affected sensory nerves. Examples of sensory stimulation can be massage, placing the hand/foot in sand/rice, on beads, stroking the skin with soft material (cotton wool), rough material (Velcro, coarse cloth), water (warm/cold). If sensory re-education is not addressed, this can lead to complications such as hyperesthesia (increased sensitivity to stimulation of the affected area), allodynia (feeling of pain on stimuli, which should not normally cause pain sensation) and most severely complex regional pain syndrome. Patient education: If the patient suffers from loss of sensation due to the nerve injury, the patient should be taught about paying special attention to prevention of wounds (e.g.: if the patient has loss of sensation of the foot, check his shoe to make sure theres no stone that he might not feel and that would hurt his foot; or if the patient loss sensation of the hand, special attention should be paid when carrying hot plates or handling hot/boiling water), checking for wounds (daily checking of the area where he lost sensation to see if there is any wound) and early care of wounds (how to properly wash and dress wounds). This is important to prevent wounds from getting infected, which might lead to an amputation if not addressed properly.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 86 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS Early Rehabilitation Protocol for Burn
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Burn
1.1. Definition of burn A burn is a damage to the skin and, sometimes, to the other tissues lying under the skin (muscles, tendons). It is, in general, caused by extremely high temperatures (see below).
1.2. The skin and its purpose The skin is the largest organ of our body. It has various purposes, such as: Protection against external organisms (virus, bacteria); It also plays an important role in the temperature regulation system (the system that allows our body to always be at a constant temperature -around 37 degrees centigrade- whether the environment is very cold or very hot or when we do exercises). The skin is the place where most of the vitamin D that we need is produced (when the skin is exposed to the sun light). The vitamin D is very important to have strong bones (the vitamin D allows the calcium to enter the bones). The skin also protects the tissues underneath it that are more sensitive against shocks. The skin is the place where receptors are located and that allow us to feel (the sense of touch).
The skin is made of three layers: the epidermis (a), the dermis (b) and the subcutaneous layer (or fat cells) (c). Other important parts of the skin are: The pores (1) or the small holes that allow the sweat to come out The sweat glands (2) that produce and stock the sweat The blood vessels (3) that carry the blood (to bring nutrients to the skin but also for temperature regulation) The nerves (4) that carry the information from the receptors to the central nervous system The sebaceous glands (5) that produce and stock the sebum (a greasy liquid that covers the skin and protects it) The hairs (6) that also play a role for the body temperature regulation The arrector pili muscles (7) which are very small muscles that will allow the hairs to erect when the body gets cold (creating the "chicken skin")
Page - 87 Page
1.3. Types of burn Depending on the severity and the part of the skin and other tissues that have been damaged, burns are classified in three different types:
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
The first-degree burn (also called "superficial burn"): A firstdegree burn means that the superficial layer of the skin (the epidermis) has been damaged. In such case, the skin is red and the burn is painful. A common first-degree burn is a sunburn (too long exposure to the sun without protective cream). Such burn heals by itself within a few days (the cells of the epidermis are replaced by new cells).
The second-degree burn (also called "partial thickness burn"): A second-degree burn is more serious as the dermis (the second layer of the skin) is also damaged. Such burn will results in redness, pain and blisters (like small sacs of water). Depending on the severity of a second-degree burn, medical treatment will be required.
The third-degree burn (also call "full thickness burn"): such burn means that the three layers of the skins have been damage (and sometimes, also the tissues under the skins such as the muscles or the tendons). The burn is bleeding and usually black or grey. This kind of burn is much more serious and always requires medical attention to prevent infection and ease healing.
1.4. Causes The main cause of burn is a contact (direct or indirect) with source of high heat such as a fire, boiling water or oil, a heater or an oven. But burns can also be caused by chemical products (acids) or by electricity (power, lightning). 1.5. Complications of burns On short-term, the greatest danger for burn patients is infection of the burn and dehydration. Indeed, if the burned areas are not well addressed (cleaned and dressed), the burn may become infected very fast. Such infection, if extended, will lead to severe complications. As for dehydration (the body losses more water than usual because of the burn), it may lead to kidneys problems and/or bladder infection. Burn patients are also at risk of organ failures. Those complications are life threatening and, therefore, should be medically addressed properly. On longer-term (and disability-wise), the main complication of severe burns (second and third degree) is skin retraction (or skin shortness). Indeed, when healing, the skin tends to become as "small" as possible (this means that there will be less skin than before and that the new skin will be less elastic than the normal skin). Such skin retraction often leads to joint limitation (decrease of range of motion in the joints near the burn).
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 88 Page
A more severe type of complication is when the burned skin stick together around a joint. This happens when the patient, during the healing process, stays with the burned skin touching another part of the body. In that case, the new skin will stick to the other part of the body decreasing severely the possibility of moving a part of the body. In general, the burn patient tends to take such position because it is less painful. But, as we will see, such position as to be prevented even if it's much more painful because once the skin sticks together, only surgery (and not always) can help separate the attached parts of the body.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Depending on the cause of the burn, some other complications may also appear, such a respiratory problems if the persons had been burned in a building fire for example (because the person inhaled smoke). 1.6. Estimate the size of the burn Estimate the size of the burn (what percentage of the skin was damaged) might be important for the medical treatment. Indeed, if a high percentage has been burned, skin graft (see below) might not be possible in on time. Also, if the burn is very extended, the risks of death are higher (the bigger is the burn, the more risk there is of developing infection or dehydration). There are different ways of estimating the size of a burn. The moss commonly used (which is quite easy but not very accurate), for adults, is called the "rule of nine". This method divides the body's surface area into percentages: The front and back of the head and neck equal 9% of the body's surface area. The front and back of each arm and hand equal 9% of the body's surface area. The chest equals 9% and the stomach equals 9% of the body's surface area. The upper back equals 9% and the lower back equals 9% of the body's surface area. The front and back of each leg and foot equal 18% of the body's surface area. The groin area equals 1% of the body's surface area.
Based on that, it is possible to estimate, quickly, the size of a burn. Note: for children, the system is a bit different as the proportions of the different parts of the body are not the same as for an adult.
1.7. Medical treatment of burn Medical treatment of burn will include: First aid (cold tap water run or sponged over the burn area for 30 minutes) Tetanus immunisation, if required Pain management (burns are very painfull and aggressive pain management might be necessary at first). Painkillers are also needed before dressing change and, sometimes, before mobilization exercises.
Page - 89 Page
Wound care dressing in order to keep the wound clean and to protect it from further damage. Antibiotics if infection is present (not prophylactically) Skin graft, if needed.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Note about skin graft Skin graft is a surgical act during which small pieces of healthy skin are removed from a non-affected area of the body and put on the damaged area. Then, the small pieces of skin will attach to the burn area and start to create new skin that, finally, will cover the burned area. This is done to speed up the healing process.
A piece of skin is taken form a healthy part of the body.
The piece of skin goes through a machine that makes the piece larger.
The piece of healthy skin is place on the burned area.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 90 Page
2. PT Protocol for Burn Patients
After the patient has been hospitalized and, when needed, emergency medical cares have been provided in order to stabilize the patient, it is necessary to make an assessment of his/her needs in terms of early rehabilitation. To do so, doctors or nurses in charge of the patient should use the Early Rehabilitation Needs Assessment Form (see annex). This form aims to help medical staffs that lack knowledge on early rehabilitation to identify the patients in needs of such services. Depending on the result of this simple assessment, the patient would or wouldnt be referred to rehabilitation department (or staff trained on early rehabilitation). Usually, all burn patients should be referred for early rehabilitation.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
2.1. Assessment Before setting up a treatment plan for burn patient, it is important to collect some information on the patient, on his/her history and on the complications. Such information should be recorder in the assessment form (see annex). Beside the general information on the patient (name, age, sex), here is a non-exhaustive list of the main pieces of information that need to be collected: (a) History What caused the burn? How did it happen? When did the burn occur? Is the patient receiving medical cares? What kind? How is the patientsituation (medically)? (b) Type, size and location of burn What is the size of the burn? Which parts of the body have been burn? Is the burn located around joints? How severe is the burn (1st, 2nd or 3rd degree)? (c) Burn healing Is the burn healing well? (d) Complications Is there infection? Is there dehydration? Is there organ failure? Is there respiratory problems? (e) Joint evaluation Is there decrease of range of motion? Can the patient move the joints actively?
Page - 91 Page
(f) Functional evaluation Is the patient functionality decreased? What and how? 2.2. Treatment in the hospital (early rehabilitation) Early rehabilitation will take place in the hospital, starting as soon as possible after the patient has been hospitalized. The main purpose of the treatment will be to prevent complications from appearing or to treat complications that are already present. In order to do so, and according to the information collected during the assessment, the following exercises should be done with the patient: (a) Starting right after the hospitalization (day 1) Mobilization (active, assisted and/or passive): All the areas affected by a burn need to be exercised through full range of motion. Such mobilization is especially important for the joints that are covered by the burn or that are adjacent to burn. Dressing should not restrict the movements. Therefore, it is better to mobilize the joint without dressing (dressing change can be taken as an opportunity to mobilized the joints without dressing). If mobilization is done without dressing, it is important that the burn remains moist during the mobilization. Mobilization should be done actively if possible. If not, assisted or passive mobilization can be done as well to ensure a full range mobilization. When needed, analgesia should be provided prior to mobilization. Mobilization of some joints not adjacent to burn might also be required if the joint is immobilized due to posture. If the patient stays in bed, all the joints not affected by burn (even if not immobilized) should be mobilized (actively or passively) to prevent muscle retraction and blood circulation problem (bedridden patient complications). Such mobilization should be provided at least 3 times per day. For details on mobilization techniques, refer to the relevant protocols. Positioning: Positioning means to "put" the patient is a good position. A "good position", with burned patients, means a position that prevents the skin retraction (the joints should be in a position that stretches the burned skin). Examples of good position: if the inside of the hand is burned, the good position is an opened hand with the fingers in extension. If the posterior part of the thigh is burned, then the knee should stay in extension. If the anterior part of the arm is burned, then the elbow should be in extension Good position can be helped by using pillows or splints.
Chest therapy: If the patient suffers from chest problems, breathing exercises might be required. For details on chest therapy, refer to the Chest Therapy Protocol. Functional exercises: The patient must be encouraged to make functional activities as soon as possible. For example, the patient should try to sit, stand and feed himself as soon as possible. Such activities are very good to prevent skin retraction, but also to prevent
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 92 Page
muscle weakness. Also, the sooner the patient starts, the less he will have to depend on other persons.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Note: Patients with skin graft - If the patient had had skin graft (a surgical treatment which consists in taking small pieces of healthy skin on parts of the body that were not burned to replace the burned), the same exercises should be done, but not right away. Indeed, after skin graft, the skin needs time to attach well. Therefore, if mobilization is done too early, the graft might not take and the skin will die. Therefore, after a skin graft, in general (but this has to be confirmed by a doctor) it is better to wait for 8 to 10 days before starting mobilization and other exercises.
(b) Srarting when the scar is healed Scar management: Moisturising lotion should be massaged into all scars 2-3 times per day as long as the scar is red. During scar healing, pressure might be required on the scar to prevent hypertrophic scarring (the skin over the burnt area becomes red, raised and hard to touch). Note: A burn that heals within two weeks usually leaves no permanent scarring. A burn that takes longer than 3 weeks to heal will scar. The longer it takes to heal the worse the scarring. Pressure is required until the burn scar matures, approximatively 12 to 18 months. Sun protection: It is important, even after the scar as healed, that it remains protected from the sun. Indeed, burnt area is particularly susceptible to further damage from the sun. Burnt areas should not be exposed to the sun between 10.30 am and 4.00 pm. 2.3. Treatment in the rehabilitation centre and in the community (long-term rehabilitation) Long-term rehabilitation will take place in a rehabilitation centre (or in a rehabilitation department in a hospital) and in the community. Such long-term treatment might be necessary when the skin is retracted or joint motions are decreased. Indeed, when that is the case, those complications usually lead to decreased functionnality and some level of disability. During long-term rehabilitation, stretching exercises, mobilization and massages will be provided to try to stretch the skin and increase range of motion. Functional exercises and advices can be alos provided to try to address the functionality difficulties. Note: For details on long-term rehabilitation, institution-based rehabilitation and community based rehabilitation, refer to the information brochure (Information on rehabilitation).
Page - 93 Page
PART 3. THE PT PROTOCOLS BY TECHNIQUE
PT PT PT PT PT PT PT PT
Protocol Protocol Protocol Protocol Protocol Protocol Protocol Protocol
for for for for for for for for
Passive and Assisted Mobilization Active Mobilization and Strengthening Stretching Exercises Balance Exercises Chest Therapy Transfers and Mobility Positioning and Changing Position Teaching and Training the Patient/Family
Note: Most of the exercises presented in the below protocols are available in movie format on the capitalization DVD.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 94 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS PT Protocol for Passive and Assisted Mobilizations
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Passive and Passive Assisted Mobilizations
1.1. Definition Passive mobilization means that the therapist or the helper will move the patients limbs in a passive way (the patient doesnt help). Passive assisted mobilization means that the therapist or the helper will move the patients limbs while the patient tries to help actively the movements. Such way of doing mobilization has the advantage of both active and passive mobilization (meaning that by helping the movement, the patients muscles are stimulated; but by having the helper finishing the movement, we insure that the all range of motion is used which helps preventing muscle shortness). Such technique is also called active assisted mobilization as the patient is, somehow, actively mobilizing his joint and receives help from another person to full range of motion mobilization. Note: There is one more way of doing passive mobilization using equipment that would mobilize a limb (or part of a limb). Such equipment is called CPM. When using CPM, the patient limb that needs to be mobilized is placed in the device and the device will mobilize the limb in a fixed amplitude for a fixed duration (usually an hour or more, depending on the patients situation). Such devices are interesting only in some cases (when the patient has one joint that needs to be mobilized for a long duration and in only one direction for example: knee flexion/extension). The use of CPM is limited when the patient needs more than one joint to be mobilized and when the joints need to be mobilized in different directions (for example, hip flexion/extension and abduction/adduction) as the device usually doesnt allow more than one type of movement. When the patients needs more than one joint mobilized in more than one direction, manual mobilization is better indicated.
1.2. Purposes Passive and passive assisted mobilization will be used with any patient that cannot or wont move the limbs at all or much (because of his/her situation, such as paralysis, muscle weakness, traction, immobilization or the need to stay in bed for a long time). A patient that doesnt move enough some parts of the body will quickly develop complications such as muscle shortness, muscle weakness, pressure sore or blood circulation problems. Passive and passive assisted mobilizations aim to prevent those problems from appearing, or at least to slow down their appearance. 1.3. Prescription In general, passive mobilization can be started directly after the accident. Passive assisted mobilization should be used whenever it is possible.
Page - 95 Page
According to the patients situation, as many joints as possible should be mobilized in as many movements as possible. To be efficient, passive and passive assisted mobilizations should be done at least 3 times a day (each movement should be repeated 20 times).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 96 Page
2. Technique
Here below is a description of the mobilizations for the main joints of the body. The same movements and techniques can be used for both passive and passive assisted mobilization (the only difference is the patient that helps or not to do the movement). 2.1. Passive mobilization for the lower limbs
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Mobilization in abduction-adduction of the hip Position of the patient: lying on the back Movement: the therapist makes hip abduction and adduction. He holds the limb at the calcaneus and the knee (posterior part of the knee).
Mobilization in triple flexion-extension Position of the patient: lying on the back Movement: the therapist makes hip, knee and ankle flexion and extension (triple flexion, triple extension). He secures the limb at the level of the calcaneus and the knee.
Mobilization in rotation of the hip Position of the patient: lying on the back Movement: the therapist makes hip rotations (makes the limb "roll" on the table).
Mobilization in eversion-inversion of the ankle Position of the patient: lying on the back Movement: the therapist secures the foot at the level of the calcaneus and makes movements of inversion (turn inwards) and eversion (turn outwards).
Mobilization in flexion-extension of the toes Position of the patient: lying on the back Movement: the therapist mobilizes the toes in flexion and extension.
2.2. Passive mobilization for the upper limbs
Mobilization of the scapula Position of the patient: lying on the side Movement: the therapist secures the scapula and mobilizes it in abduction-adduction and updown.
Mobilization in flexion-extension of the shoulder Position of the patient: lying on the back Movement: the therapist secures the patient's upper limb at the level of the wrist and the elbow. He makes movements of flexion and extension of the shoulder.
Page - 97 Page
Mobilization in abduction-adduction of the shoulder Position of the patient: lying on the back Movement: the therapist secures the patient's upper limb at the level of the wrist and the elbow. He makes movements of abduction and adduction of the shoulder.
Mobilization in horizontal abductionadduction of the shoulder Position of the patient: lying on the back Movement: the therapist secures the patient's upper limb at the level of the wrist and the elbow. The shoulder is at 90 degrees of abduction. The therapist makes movements of horizontal abduction and adduction of the shoulder.
Mobilization internal-external rotation of the shoulder Position of the patient: lying on the back Movement: the therapist secures the patient's upper limb at the level of the wrist and the elbow. The shoulder is at 90 degrees of abduction and the elbow is at 90 degrees of flexion. The therapist makes movements of shoulder rotation.
Mobilization in flexion-extension of the elbow Position of the patient: lying on the back Movement: the therapist secures the patient's upper limb at the level of the wrist and the elbow. The therapist makes movements of flexion and extension of the elbow.
Mobilization in pronation-supination of the forearm Position of the patient: lying on the back Movement: the therapist secures the patient's upper limb at the level of the wrist and the elbow. The elbow is at 90 degrees of flexion. The therapist makes movements of pronation and supination (he turns the forearm inwards and outwards).
Mobilization in flexion-extension of the wrist Position of the patient: lying on the back Movement: the therapist secures the patient's hand and wrist. The elbow is at 90 degrees of flexion. The therapist makes movements of flexion and extension of the wrist.
Mobilization in flexion-extension of the fingers Position of the patient: lying on the back Movement: the therapist secures the patient's finger above and below the joint he wants to mobilize. Than he mobilize the joint in flexion and extension.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 98 Page
2.3. Passive mobilization for the trunk
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Mobilization in flexion of the spine The patient is on the back and he brings back his knees on his chest. If he cannot do it alone, the therapist can help to make this movement.
Mobilization rotation of the spine From the position described just before (flexion of the spine), the patient (or the therapist) can bring the knees on one side to mobilize the spine in rotation.
Page - 99 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS PT Protocol for Active Mobilization and Strengthening Exercises
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Active mobilization and Strengthening Exercises
1.1. Definition Active mobilization means that the patient will move parts of his/her body actively (by him/her self). It is the first stage of strengthening (the easiest stage). There is no external resistance (nor manual nor mechanic such as weights) applied against the movement. As mentioned in the passive and passive assisted mobilization protocol, another way of doing active mobilization, when the patient cannot actively mobilize the joint in full range of motion, is to use active assisted mobilization (also called passive assisted mobilization). This means that the patient is actively mobilization his joint (active mobilization) and the PT (or the helper) helps the patient to finish the movment and ensure a full range of motion mobilization. For details, refer to the passive and passive assisted mobilization protocol. Strengthening exercise mean that the patient will move actively parts of his/her body (by him/her self) against a resistance. Resistance means a force that is applied against the movement. At first, the resistance applied against the movement is only the weight of the part of the body that is moved; we called such exercises auto-strengthening. Later on, an external resistance can be applied against the movement. The external resistance can be applied manually (the therapist/helper pushes with his/her hands against the movement) or mechanically (using weights such as sand bags). When the resistance is applied manual, we talk about manual strengthening; when sand bags or other weights are used we talked about mechanic strengthening. 1.2. Purposes Active mobilization and strengthening exercises will be used with any patient that doesnt move much because he/she needs to stay in bed for a long time. Active mobilization will be used when the patient is too weak to do strengthening exercises. When the muscles get stronger, external resistance can be applied. A patient that doesnt move enough some parts of the body will quickly develop complications such as muscle shortness, muscle weakness, pressure sore or blood circulation problems. Active mobilizations and strengthening exercises aim to prevent those problems from appearing, or at least to slow down their appearance. 2.3. Prescription Active mobilization and strengthening exercises ca be started right away. At least, the parts of the body that are not immobilized or fractures or paralysed should be actively mobilized and strengthen from day 1 after the hospitalization. For the other parts of the body, the time when active mobilization and strengthening exercises can start depends on the patients situation. For details, refer to the corresponding protocols.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 100 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
When doing active mobilization and strengthening exercises, special attention should be given to the muscles that are important for functionality (the muscles important for walking the hip extensors, the hip abductors, the knee extensors; the muscles important for transfers or walking with crutches the shoulder adductors, the elbow extensors; the muscles important to reach and hold objects the shoulder flexors and abductors, the elbow flexors). To be efficient, active mobilizations and strengthening exercises should be done at least 3 times a day (each exercise should be maintained for 10 seconds and repeated 10 times).
Page - 101 Page
2. Technique
Here below is a description of the active mobilizations and strengthening exercises for the main joints and muscles of the body. 2.1. Active mobilization
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Active mobilization in flexion and extension of the lower limb The patient is lying on the back and he actively does flexion and extension of the leg (the foot stays on the bed).
Active mobilization in hip abduction and adduction The patient is lying on the back and he does abduction and adduction of on leg (he opens and closes the leg).
Active mobilization in ankle dorsal and flexions The patient is lying on the back (or seated) and makes movement of dorsal (up) and plantar (down) flexion.
Active mobilization in ankle rotation The patient is lying on the back (or seated) and he makes rotations of the ankle (he makes circle with his foot.
Active mobilization in flexion and extension of the toes The patient is lying on the back flexes and extends his toes.
Active mobilization of the upper limbs The patient is lying on the back (or seated) and makes movements of the upper limbs in all directions
Active mobilization of the wrist The patient makes movements of flexion/extension or rotation of the wrist.
Active mobilization of the hands and fingers The patient opens and closes his hand.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 102 Page
2.2. Auto-strengthening
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Auto-strengthening of the hip extensors The patient is lying on the back with the hips and knees in flexion (the feet are on the ground). Then the patient lifts up the pelvis (make the bridge).
Auto-strengthening of the hip abductors The patient is lying on the side and makes the abduction of the hip by lifting up the lower limb.
Auto-strengthening of the knee extensors The patient is lying on the back with a pillow under his knee. He then extend his knee (lifts up the foot)
Auto-strengthening of the knee extensors Put a pillow under the patients knee and ask him to push the pillow down.
Auto-strengthening of the knee extensors (and hip flexors) The patient is lying on his back and makes the flexion of the hip by lifting up the lower limb. The knee should remain in extension (strengthening of knee extensors).
Auto-strengthening of the knee extensors The patient is in sitting (or lying) position with the legs out of the bed. He makes the extension of the knee by lifting up the leg.
Auto-strengthening for the upper limbs (push-ups) The patient is seated (on the bed or in the wheelchair). Pushing up on the upper limbs, he lifts up the pelvis.
Page - 103 Page
2.3. Manual strengthening
Manual strengthening for the hip extensors The patient is lying on the belly. He tries to lift up his lower limb while the therapist pushes the limb down.
Manual strengthening for the hip abductors The patient is lying on the side. He tries to lift up his lower limb while the therapist pushes the limb down.
Manual strengthening for the knee extensors The patient is lying on the back or in sitting position. He tries to extend the knee while the therapist pushes the leg down.
Manual strengthening for the dorsal flexors The patient is in sitting position. He tries to make a dorsal flexion while the therapist pushes the foot down.
Manual strengthening of the shoulder abductors The patient is in sitting position. He tries to make the abduction of the shoulder by lifting up the upper limb on the side while the therapist pushes the limb down.
Manual strengthening of the shoulder flexors The patient is in sitting position. He tries to make the flexion of the shoulder by lifting up the upper limb in front while the therapist pushes the limb down.
Manual strengthening for the shoulder adductors The patient is in sitting or lying position. The therapist puts the patient shoulder in abduction. Then the patient tries to bring the upper limb along his side while the therapist pushes outwards.
Manual strengthening of the elbow flexors The patient is in sitting (or lying) position with support under the elbow. He tries to make the flexion of the elbow while the therapist pushes the forearm down.
Manual strengthening of the elbow extensors The patient is in sitting (or lying) position with support under the elbow. He tries to make the extension of the elbow while the therapist pushes the forearm up.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 104 Page
2.4. Mechanic strengthening
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Mechanic strengthening for the hip extensors using sand bag
Mechanic strengthening for the hip abductors using sand bags
Mechanic strengthening for the hip abductors using elastic band
Mechanic strengthening for the hip adductors using a pillow
Mechanic strengthening for the knee extensors using sand bag
Mechanic strengthening for the knee extensors using sand bag
Mechanic strengthening for the knee extensors using sand bag
Mechanic strengthening for the knee extensors using elastic band
Mechanic strengthening for the plantar flexors using elastic band
Mechanic strengthening for the dorsal flexors using sand bag
Mechanic strengthening for the shoulder abductors using sand bags or dumbbell
Mechanic strengthening for the shoulder adductors (horizontal adduction) using sand bags or dumbbell
Mechanic strengthening for the elbow flexors using sand bags or dumbbell
Page - 105 Page
Mechanic strengthening for the elbow extensors using sand bags or dumbbell
Mechanic strengthening for the wrist flexors and extensors using dumbbell
Mechanic strengthening for the hand using a soft ball
2.4. Isometric contractions Isometric contractions are contractions during which the muscle doesnt become shorter nor longer. The muscle length remains the same. This kind of contracture doesnt create any movement in the joints. Therefore, it can be very useful when, for some reason, the joint should not or cannot be moved (for example, whe there is a fracture or when there is an immobilization). All the muscles of the body can be contracted isometrically.
When possible, the patient should first be asked to do isometric contraction on a muscle that can be seen (for example o the other limb if only one limb is fractured or immobilized) to insure that he understands what he/she is asked to do and that he does it correctly. Then, the exercise can be done with other muscles.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 106 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS PT Protocol for Stretching Exercises
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Stretching Exercises
1.1. Definition Stretching exercises are exercises that are used to stretch the muscles and the other soft tissues around the joint (the skin, the ligaments, the capsule). Stretching exercises use a force that is applied on a part of the limb in order to stretch the muscles and the other soft tissues. That force can be applied directly by the therapist/helper (in that case we talk about manual stretching) or by the patient him/herself (in that case we talk about auto-stretching) or through the use of external weights (in that case, we talk about mechanic stretching). Each technique has its advantages and its inconvenient. To decide which one to use, the therapist should take into account the patients situation. 1.2. Purposes The purpose of stretching exercises is to make he muscles and/or he other soft tissue longer in order to increase the range of motion in a joint. When a patient doesnt move enough or stays for a long time in the same position, some muscles and soft tissue will become shorter. Short muscles/soft tissue will stop the movements in a joint before reaching the normal magnitude of the movement (they will decrease the range of motion). Decreased ranges of motion will have functional consequences (if he knee cannot be completely extended, it will be difficult for the patient to stand and walk; if the shoulder abduction and flexion is limited, it will be hard for the patient to reach for objects; if the elbow cannot be well flexed, it will be hard for feeding). Note: Stretching exercises can also be used with patients that have spasticity with the purpose of decreasing the spasticity, even if there is no muscle contracture. In that case, the stretching techniques are a little bit different as the stretching position will stretch several groups of muscles at the same time, while when doing stretching exercises to make muscle longer, the therapist usually stretches only one group of muscle at a time. For details, refer to the Head Injury protocol. 1.3. Prescription If basic exercises explained in the other protocols were started early and done correctly and regularly, there shouldnt be muscle or soft tissue retraction. Therefore, stretching shouldnt be needed. Nevertheless, in one hand, some retractions cannot always be prevented even with early and adapted treatment (if the patient has a cast, some joints cannot be mobilized) and, in the other hand, some patient arrive to the hospitals with contractures already present. In both those cases, stretching exercises will be necessary to try to stretch the tissues (muscles and/or other) in order to increase the range of motion is the concerned joints. To be efficient, stretching exercises should be done at least 3 times a day (each stretching position is maintained for 20 seconds and repeated for 5 to 10 times).
Page - 107 Page
2. Technique
Here below is a description of the main stretching techniques.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
2.1. Manual stretching
Manual stretching for the hip flexors Position of the patient: lying on the back, on the edge of the table. The patient secures the opposite leg in flexion (the leg that won't be stretched). This is important to protect the back during the stretching. Movement: the PT stretches the hip flexors pushing the thigh downwards. He helps, with the second hand, to secure the opposite leg in maximal flexion.
Manual stretching for the hip adductors Position of the patient: lying on the back or seated with both legs in flexion (hip and knees are flexed, the feet are on the mattress) Movement: the therapist pushes both knees apart (pushes down) to stretch the hip adductors.
Manual stretching for the knee flexors Position of the patient: lying on the back. The PT is sitting on the table and put the patient's leg on his shoulder. Movement: the PT does the stretching pushing the knee down. He can use his both hands or use the second hand to secure the opposite leg.
Manual stretching for the knee flexors Position of the patient: lying on the back. Movement: the PT does the stretching pulling the leg up with one hand (securing the ankle). The other hand pushes down on the tight.
Manual stretching for the plantar flexors Position of the patient: lying on the back. Movement: With one hand, the PT secures the foot the level of the heel; the other hand keeps the knee in a slight flexion. The PT does the stretching pushing the foot up (using his forearm) and pulling the heel down.
Manual stretching for the extensors and adductors of the shoulder Position of the patient: lying on the back Movement: the therapist secures the patient's upper limb at the level of the wrist and the elbow. He stretches the extensors and adductors of the elbow by making a flexion of the elbow and maintaining the position.
Manual stretching for the flexors of the elbow Position of the patient: lying on the back Movement: the therapist secures the patient's upper limb at the level of the wrist and the elbow. The therapist stretches the elbow flexors by pulling the elbow in extension and maintaining the position.
Manual stretching for the flexors of the wrist Position of the patient: lying on the back Movement: the therapist secures the patient's hand and wrist. The elbow is at 90 degrees of flexion. The therapist stretches the flexors of the wrist by making an extension of the wrist and maintaining the position.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 108 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Manual stretching of the flexors of the fingers Position of the patient: lying on the back Movement: the therapist secures the patient's fingers and the thumb. He then stretches the finger flexors by making an extension of the fingers and maintaining the position.
2.2. Auto-stretching
Auto-stretching of the knee flexors The patient is seated with the legs in extension. He then leans forward keeping the knees in extension.
Auto-stretching of the knee extensors using a belt (or a towel) The patient uses a belt or a towel (not elastic) that is placed above the foot to pull the foot and flex the knee
Auto stretching of the plantar flexors using a belt The patient uses a belt (not elastic) that is placed on the foot to pull the foot up and stretch the plantar flexors
Page - 109 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS PT Protocol for Balance Exercises
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Balance Exercises
1.1. Definition Balance exercises are exercises in which the patient will be asked to maintained a balanced position. The position that the patent has to maintain has to be a difficult position in order to have him/her improving his/her balance abilities. 1.2. Purposes The main purpose of balance exercise is to improve the patients balance abilities. A good balance is important to maintain position (such as sitting or standing position). A good balance in sitting or standing position is also important to allow a good use of the upper limbs (indeed, using the upper limbs creates imbalance, so if the patient doesnt have a good balance, he/she wont be able to use the upper limbs). A good balance in standing position is very important for waking (walking is a succession of imbalanced and balanced positions). Another purpose of balance exercise is to stimulate the use of the muscles (of the trunk or the lower limbs). Using balance exercises to improve the muscle control and muscle strength allows the therapist or the helper to vary the exercises. Varying the exercises has a double advantage: it allows adapting better the exercise to the patients abilities and it makes the treatment less boring for the patient (repetitions in exercises can quickly become boring for the patient and, therefore, make the exercises less efficient because the patient is less willing to do them). 1.3. Prescription Balance exercises can be prescribed to all the patients that have difficulties maintaining a balanced position. It is also very important for the patients that have difficulties for walking or that need a very good balance to walk (such as amputees). Balance exercises should be done 3 times a day for 10 to 20 minutes.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 110 Page
2. Technique
Here below are examples of balance exercises in sitting and standing position. But before presenting those exercises, it is important to explain general principles on how vary balance exercises I order to adapt them better to the patients abilities. 2.1. General principle of progression for balance exercises There are a lot of possibilities t do balance exercise. The main principle to follow is to put the patient in an imbalanced position and stimulate him/her to maintain it. The following progressions can be followed when doing balance exercises: At first, the patient has to maintain the balance exercise with the required support (the therapist/helper or with parallel bars or standing frame). When the patients abilities to maintain the position with support, the support is slowly decreased. When decreasing the support, it is very important to let the patent feel when he/she looses his/her balance. If the position is directly corrected by the helper/therapist when the patient looses his/her balance, he/she wont try to correct the position alone and, therefore, wont improve his/her balance. When the patient can maintain a balanced position alone, imbalance can be created using the following means: Push the patient forwards, backwards and on the sides and ask him/her to try to maintain the balanced position. Have the patient using the upper limbs to reach for objects put in front or on the side of hi/her. By trying to reach for object, the patient creates imbalance. Decrease the base of sustentation. The base of sustentation is the surface that is delimited by the supports of the patient on the ground or the bed). In standing position, the base of sustentation can be decreased by asking the patient to stand with the feet close to each other or with one feet in front of the other or by standing on one foot. Decrease the stability of the support. This can be done by using unstable objects such as a Bobath ball, or a matress or an unstable board to sit or stand on. Ask the patient to close his/her eyes. By closing the eyes, the patient looses a canal of information (the view) that is very important for the balance. Therefore, maintaining a balanced position becomes more difficult with closed eyes. Ask the patient to move quickly the head. By moving the head the patient losses a canal of information (the vestibular system in the inner ear) that is very important for balance. Therefore, maintaining a balanced position becomes more difficult when moving the head quickly. Then, those means can be combined (ask the patient to move the upper limb while sitting or standing on an instable support with smaller base of sustentation with close eyes and/or moving the head).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
2.2. Balance exercises in sitting position
Help the patient to maintain sitting position on a stable support (hard mattress or bed). Provide the support that he needs. The support can be provided by the therapist and/or by a table in front of the patient.
When the patient gets better, push him on the sides a little bit.
Page - 111 Page
Then, change the support on which the patient sits to make it more unstable. Use a round pillow, a Bobath ball or an unstable board. First have the patient maintaining the position alone, and then push him on the sides.
To make those exercises even more difficult, decrease the possibility that the patient has to take support with the feet on the ground. To do so, have the patient doing the exercise with one foot on an unstable board or a ball. Then do it with both feet on unstable boards or balls.
Another possibility is to have the patient using his upper limbs and making movements with the trunk. Those movements will create imbalance. For example: have the patient reaching for an object on one side and putting it on the other side (a ball or a piece of a puzzle). Or have him throwing a ball in a basket.
Ask the patient to do some of those exercises with closed eyes. For example, ask him to try to find an object that is on his side but with closed eyes.
Combine the unstable supports with the movements of the upper limb and the trunk. The patient is seated on a round pillow or a Bobath ball and has to reach for objects on the side or throw a ball.
Finally, combine the unstable supports with the movements of the upper limbs and the trunk and the closed eyes. Such exercises are very difficult
2.3. Balance exercises in standing position
Help the patient to maintain standing position providing support (the support can be the therapist, the parallel bars, a table, a round pillow, a Bobath ball or a rope). In this position, let the patient "feel" his balance (don't support too much).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 112 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
When the patient is in standing position, the therapist pushes him forwards, backwards and sideways.
The patient tries to maintain a stable position on an unstable board.
The patient reaches for objects in different locations (far, close, high, low) or he throws a ball in a basket.
The patient stands on one foot with opened or closed eyes.
Ask the patient to stand on one foot and pick up an object on the ground.
Ask the patient to jump on one foot above small obstacles.
Or to skip on one foot.
Ask the patient to try to maintain a stable position on un unstable board with closed eyes.
Have the patient maintaining a stable position on an unstable board and throw a ball in a basket (or to the therapist) or reach for objects.
When the patient is on the unstable board, with opened or closed eyes, push him on the side and in front and backwards.
The patient stands on one leg on a mattress with opened or closed eyes.
The patient is on one leg on a mattress and throws a ball or reaches for objects.
Page - 113 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS PT Protocol for Chest Therapy
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Chest Therapy
1.1. Definition Chest therapy uses exercises to help the patient getting pulmonary secretion out of the lungs. Such therapy also includes the use of medication and nebulizers that help the expectoration of secretions. 1.2. Purposes The main purpose of chest therapy with hospitalzed patients is to help the patient better mobilizing his lung secretions up the airways to get them out of the respiratory tract. Helping the patient to get the extra secretion out of the lungs has two positive effects: first, it helps preventing lung infection (indeed, the more secretions there rae in the lungs, the higher the risk of having them getting infected). Secondly, by cleaning the lungs of extra secretions, chest therapy also helps to have better oxygenation of the blood (more oxygen can reach the blood is the lungs are clean). But, to better understand the effects and purpose of chest therapy, we need to understand basics of ventilatory mechanics, secretion production and lung clearance mechanisms, as well as the effects that an injury or bed rest may have on those mechanisms. (a) Basics of ventilatory mechanics Ventilatory meachanism means the way things work when we breathe. It mainly involves the lungs, airways (or respiratory tract) and the respiratory muscles. The lungs are kind of bags in which gas exchanges between the air and the blood occur. The air that enters the lungs brings in oxygen (O2). When reaching the end of the airways (the alveoli), gas exchange occurs with the blood reach in carbon dioxide (CO2). The O2 gets in the blood while the CO2 leaves the blood. We usually divide the respiratory tract (the tubes that bring the air from outside to the blood) into 3 segments: the upper respiratory tract (the nose, and the pharynx or thoat), the respiratory airways (the larynx, the trachea, the bronchi and the larger bronchioles) and the lower respiratory tract (the bronchioli and the alveoli). The muscles that help breathing are called the respiratory muscles. The respiratory muscles mainly work for inspiration (breathing in). The main of those muscles is the diaphragm. When the diaphragm contacts, it pushes down and forward our
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 114 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
abdominal organs (thats why, usually, when we breathe in, the belly comes out) and lifts up the lower ribs (thats why, when breathing in, the thorax goes up a little bit). This movement inflate the lungs (the size of the lungs increases), creating a lower pression in the lungs and the air enters the lungs. In case of efforts (sport, for example) or shortness of breath, accessory muscles may help to inflate even more the lungs by pulling up on the upper ribs. Breathing out is mainly a passive process: the diaphragm stops contracting, returning in its relaxing position and pushing up the lungs. At the same time, the lower ribs come back down, deflating the lungs and pushing the air out of the lungs. In case of coughing (forced and fast expiration), the abdominal muscles deflating by increasing the abdominal pressure and pushing the diaphragm up (b) Secretion production and lung clearance mechanisms There are a lot of things in the air we breathe other than air itself: dust, pollen, germs To maintain a healthy respiratory system, it is important that only air reaches the end of the respitaory tract. Therefore, there is a system that helps preventing dust, pollen and germs to reach the alveoli. This system is composed of three different mechanisms at different levels of the respiratory tract that helps trapping the particles present in the air. First, the biggest particules will be trapped in the mucosa of the nose and throat (thanks to the twists and turns of the inner walls of the nose and throat). They are then evacuated thanks to snizzing or cough. The middle particules will be trapped in a sticky blanket (the mucus) that covers the inside of the trachea, the bronchi and the bronchioles (the middle part of the respiratory tract). The mucus and the particules will form what we call the secretions and those will be cleared out of the lungs thanks to the mucociliary clearance (or mucociliary escalator see note below) and coghing. The smaller particules that reach the alveoli will be eliminated by macrophages (the cleaning cells of our body).
Note: As just mentioned, the mucociliary clearance is a mechanism that helps to mobilize the secretions (mucus plus dust/pollen/germs) up the respiratory tract. This mechanism is possible thanks to small hairs (or cilia) that make small movements and carry the secretions from the lower part of the respiratory tract to the throat where they can be either swallod or expectorated (coughing). Mucociliary clearance is stimulated by the air flow inside the respiratory tract. This means that the more air travels in and out the lungs, the better the mucociliary clearance works.
(c) Consequences of injury and/or bedrest on ventilatory and lung clearance mechanisme When a patient stays in bed or suffers from paralysis or weakness of the respiratory muscles or feels pain when breathing (rib fracture, surgery on the abdomen), the air flow in the pulmonary system decreases because the patient only takes small breaths (he/she doesnt breathe in much and he/she doesnt exhale completely). Because of that decrease of air flow, the muociliary clearance mechanism doesnt work as well as normally. Also, hospitalized patient (for the same reasons as mentioned just above) often have difficulties to cough. This is often worsen by the fact that tey remain in lying position in bed, which makes coughing even more difficult (because in lying position, the abdomen muscles cannot increase abdominal pressure as much as in sitting or standing position because the
Page - 115 Page
abdominal organs cannot be pushed up easily against the diaphragm). The consequence is that the secretions tend to stay in the lungs where they can easily get infected, which will lead to lung infection (pneumonia). Extra secretions in the lungs also have a negative influence on the gas exchanges that occur in the lung (O2 from the air against CO2 from the blood), impacting on the level of oxygen in the blood. Since oxygen is necessary for the cells to live and properly function (which includes healing), a lower level of oxygen in the blood might influence the speed at which a patient recovers (with less oxygen reaching the cells, the patient might need more time to recover from wathever illness or injury he has). (d) Purpose of chest therapy As mentioned above, the purpose of chest therapy is to help the patient to get the secretions out of the lungs and the respiratory tract. Indeed, chest therapy will help maintaining a good and effective mucociliary clearance mechanism (that tends to decrease with hopsitalized patients due to lower air flow, paralysis or pain) and it will help them for coughing to get the secretions out of the respiratory tract. To help maintaining effective mucociliary clearance system through chest therapy exercises, we have to stimulate air flow in the lungs (make sure that the patient breathes in and out deeply). Other techniques will also help the patient to cough more effectively. The positive effects of having lungs cleared of extra secretions is that: 1. It helps preventing further complications such as lung infection and 2. It helps maintaining a good level of oxygen in the blood, which influence the speed at which the patient recovers from whatever illness or injury he has. 1.3. Prescription Taking into account the respiratory risks that any bedridden patient faces, chest therapy should be prescribed to all patients that have to stay in bed for a long time. Special attention should be given to the patients that are more likely to develop lung infection or that usually have extra secretions, such as smokers and older patients. Chest therapy should be systematic with paralyzed patients, such as patients with Spinal Cord Injury. Chest therapy should be done at least 2 times a day for 10 to 15 minutes.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 116 Page
2. Technique
Here below is a description of basic techniques that can be used for chest therapy. 2.1. Postural drainage Postural drainage is technique that uses gravity to assist drainage of secretions. The patient will be lying in a position in which the area to be drained is up. That way, the weight of the secretion will help to bring them up the central airway where they can be removed by cough. To help drain the left lung, the patient should be in right sidelying position (lying on the right side of the body); the opposite position helps draining the right lung. If possible and tolerated, the bed should be inclined (the head of bed lower than the foot of the bed). Each position requires 10 minutes to be effective. Postural drainage is effective if it provides symptomatic relief. Thin secretions are more responsive to postural drainage than thick secretions. Also, secretions in large ariways (upper airways) are more rsponsive to gravity than secretions in smaller airways. Postural drainage is indicated if the patient has difficulties to use more active methods such as slow expiration, cough stimulation or forced expiration techniques. It is also interesting because the patient can use that method on his own (daily routine). 2.2. Manual techniques percussions and vibrations Manual technique consists in performing percussions and/or vibrations on the patients chest in a drainage position (or sitting position). It is a controversal technique, as some sudies seem to have proven its ineffectiveness while other show that it actually helps mobilizing the secretions by lossing them from the airways wall and by speeding up the mucociliary transport. Nevertheless, such technique can be used, if there is no contra-indication (see below) as it, for sure, doesnt make the patients situation worse (if it doesnt work, all there is to loose is a few minutes). Percussions consist of rhythmic clapping on the chest with cupped hand creating an energy wave that is transmitted to the airways, helping the secretions to get loose. It is important, when doing clapping, to not have the hands flat. Clapping should be done for a couple of minutes, all over the thorax (front, side and back) Vibrations consist in doing small amplitude and fast oscillations of the hand against the chest, performed at the end of slow and deep expiration (see below details on slow expiration technique).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Manual techniques are contra-indicated if the patient presents rib fracture, osteoporosis (fragile bones), pain or loss of skin integrity (wound or scar on the chest).
Page - 117 Page
2.3. Slow expiration technique Slow expiration is a technique that consists in asking and stimulating the patient to take a normal inspiration and to breathe out slowly and deeply. Such technique helps mobilization the lower secretions up the airways where they can be removed using coughing or forced expiration technique. To ensure that the patient exhales as much as possible, stimulation techniques can be used: the PT can either apply pressure on the thorax and abdomen to help the patient empty his lungs or we can use incentive spirometry (special device to stimulate the patient exhaling as much as possible or more simply, using a bottle of water and a straw and ask the patient to blow up boobles in the bottle for a long as possible).
Incentive spirometry
Making boobles
Slow expiration technique can be done in sitting, half sitting or sidelying position. At the end of each expiration, vbrations can be used to loose the secreton and help them travelling up the airways. Slow expirations should be 4 or 5 times, at the end of which cough (or cough facilitation, if needed) or forced expiration technique can be used to get the secretion out of the upper airways. Then, the patient should rest for a minute or two to prevent hyperventilation and diziness.
Note about slow expiration technique with babies For slow expiration technique with babies, the baby should be lying on the back. The PT has one hand on the thorax and one hand on the abdomen. The PT should feel the breathing; at the end of the expiration, he pushess gently with both hands to prolong the expiration but without trying to get a complete expiration at once, he then prevents the baby from breathing in completely and pushes down a bit more at the time of next expiration. He should do this about 3 times so that he get a complete expiration then let the baby breathe a few times before starting again.
2.4. Cough facilitation Coughing is a fast expiration and it is the most efficient way to get secretions out from upper airways; it is the way that we all usually do when having extra secretions. If the patient has difficulties to cough, coughing facilitation technique can be used. Coughing facilitation consists in 4 steps: 1. The patient takes a deep breath, locking the glottis; 2. He locks his glottis; 3 He makes a contraction of the expiratory muscles (tries to get the air out but keeping the glottis locked) and; 4. He opens his glottis and fastly exhales. Coughing is not effective to mobilize the secretions in lower airways (small bronchi and bronchiolis), as the accelerated airflow that occurs during coughing tends to collapse those lower airways.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 118 Page
2.5. Forced expiration technique Forced expiration also helps to get the secretions out of the upper airways. It uses the same technique as the coughing facilitation, except that the patient doesnt close his glottis. Such technique is less traumatizing, as the pressure inside the lung doesnt increase as much as it does when the patient contracts his expiratory muscles with the glottis locked. As for coughing, collapse may occure during in lower airways during forced expiration. It is, therefore, not effective to mobilize the secretions in those airways. 2.6. Positioning according to the lung problem If the patient suffers from a lung complication (such as shortness of breath, coughing, lung infection), it is important to take into account the position in which he stays during the day. Indeed, some positions are to be recommended to help improving the patientsituation. (a) Shortness of breath If the patient complains of shortness of breath, the position to recommend is stitting (or, at least half seated) as such position will help the inspiratory muscles work more easily. Indeed, in sitting position, the weight of the abdominal organs doesnt push on the diaphgram; it can than work more freely. If needed, the patient can, in this position, take support or lean on his knees, a table or the bed/chair armrest and use more easily his accessory inspiratory muscles. (b) Coughing As we saw above, coughing is a forced and fast expiration which uses the abdominal muscles to be effective. The best position to help the abdominal muscles working effectively is sitting position, if possible with the upper body slightly leaning forward. That way, the abdominal pressure will increase even more when the abdominal muscles contract and cough will be more effective. (c) Pneumonia (lung infection) In case of pneumonia, one part of the lung is infected. That infected region is not well supplied in air and oxygen. Therefore, in order to increase oxygenation, the patient should be placed in sidelying position, keeping the infected zone up. Indeed, when lying on the side, the upper lung opens more than the lower lung. This means, for example, if the left lung is infected, we should avoid sidelying on the left and keep the patient lying on his right side (to keep the left lung up). Such position would also help for postural drainage of the infected lung.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Page - 119 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS PT Protocol for Transfer and Mobility
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. General Information on Transfer and Mobility
1.1. Definition "Transfer" means to go from one position to another position (for example, sitting up -going from lay down position to sitting position- is a transfer). Other transfers are, for example: moving in bed, standing up, sitting down, going from one chair to another chair "Mobility" means the ability to move. Moving around can be done with walking or by using a wheelchair. Walking can be done without support or with the help of a person or with the support of a mobility aid (cane, crutches, walking frame or even a wheelchair). 1.2. Purposes Learning to make transfer or to move around alone (or with as little as possible) is very important for hospitalized patients. Indeed, depending on the injury, some patients might have difficulties, when recovering, to make such transfers or to walk. Re-learning how to sit up, standing and/walking is an important step of the rehabilitation process because from those abilities depend a lot of daily life activities. Also, staying in lying position too long is not very good for the patient. He/she should try to get out of bed (when possible), or at least seat in bed (or in a chair) as soon as possible. Indeed, lying position is not a very good position as it may lead to further complication (refer to the bedridden protocol for further information on the common complication of bedridden patients). 1.3. Prescription Transfers and mobility should be taught to all the patients that might have difficulties to change position or move around. Most injured patients will stay in bed for a while. When it is time for them to move (change position, stand and walk), advices should be provided to ensure that they do that in a proper way.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 120 Page
2. Technique
Here below are advices on how to properly make transfers (with or without help) and how to properly move around (with or without the help of a person or a mobility device). Preliminary notes on body mechanics when helping for transfers It is very important for the person that helps a patient to change position to have good body mechanics. By body mechanics, we mean the way the helper positions and uses his/her body to perform a transfer. Good body mechanics is important to prevent back injury and keep onself and he patient safe during the transfer. In terms of body mechanics and transfer, there are 4 very important points that the helper should pay attention to: - The helper should make sure to keep his feet flat on ground (when possible) and apart from each other. Such position will ensure a good balance and stability while doing the transfers. - When doing transfer, the helper should bend his knees and keep his back straight. Beding the knees will ensure that he will use his leg muscles (strong muscles) instead of his back muscle (weaker) to make the transfer. Keeping the back straight helps preventing back injury during transfers. - The helper should make sure to keep the object/weight (in this case, the patient) close to his body. That way, it prevents from leaning forward (and risking to damage his back) and it increases stability by keeping the object/weight close to his center of gravity. - During the transfer, the helper should keep his feet pointed in the direction of the weight. This helps preventing twisting motion of the back during the transfer. Twisting motion of the back while lifting a patient increases the risks of back injury for the helper. Keeping the feet pointed in the direction of the weight might require moving them (turning them) during the transfer (for example when helping a patient to go from bed to chair). When doing so, the helper should make sure that the patient is balanced before moving his own feet. Preliminary notes on safety consideration when helping for transfers and mobility To ensure safety while helping a patient to change position or to move around, the helper should take the below recommendations into account. Those recommendations should be taken into account before starting the transfer! - Know the patient abilities (know what he can do and how much he will be able to help). This helps to better apply a basic rule of transfer, which his provide as less help as possible. Providing as less help as possible will help the patient to improve his transfer abilities, it will protect the helper from getting hurt (the helper wont have to do the transfer all alone) and it will increase the patients confidence (if the patient helps, he will be les scared during the transfer). - Get the equipment needed ready (transfer belt, transfer board, wheelchair, chair) and inspect it beforehand (make sure that the equipment is safe wheelchaire brakes, wheelchair footrest up, chair against a wall or secured to prevent it from slipping away when the patient sits in it). - Make sure that the patient has proper clothing (trousers or robe that wont fall when the patient moves, shoes and not slippers or high heal shoes). - Make sure nothing will be in the way (obstacles). - Make sure that, when possible and when they are not needed for the tranfer, the bed handels are down. If they stay up, they might get in the way while trsnafering the patient. - Finaly, explain every step of the transfer to the patient (before and during the transfer).
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
2.1. Transfers (a) Moving in bed alone In terms of moving in bed, the patient might need to: turn from back to side (or side to back), moving laterally in the bed (go from one side of the bed to the other) or go up the bed.
Page - 121 Page
To turn from back to side and side to back, follow the below steps: First, the patient should flex both legs (if he cannot flex both legs, he should at least flex the leg opposite to the side he is going to turn on) and puts the arms up (as shown in the drawing). Once he is in this position, the patient has to turn on the side. When turning on the side, it is important that the patient turns in one block. This means that he has to turn the shoulders and the pelvis at the same time, preventing torsion in the spine. This is very important for patients that have back problems (such as fracture, surgey, pain). To move from one side of the bed to the other side, the patient can follow the below steps: The patient first needs to take the bridge position, meaning that he has to bend both his legs and then lift up the pelvis. In this position, he can move his pelvis on the side, and then move his legs and shoulder. This can be repeated as often as necessary for the patient to reach the side of the bed. To go up the bed, the patient should First do the bridge position (see above). He then can lift up his head and pushe on the legs to go up the bed. If the patient has a trapez above his head, he can grasp it and help lifting up is upper body by pulling on the trapeze. If the bed allows, you can also lift up the lower extremity of the bed (where the feet are) so that gravity will help the patient to go push up his body (towards the head of the bed). This can be repeated as often as necessary for the patient to reach the top of the bed. (b) Moving in bed with help If the patient cannot move in bed alone as described above, he/she will need help from another (or more) person. Here is how those persons can help the patient moving in bed: To help the patient turning on the side, the helper should provide the help necessary for the patient to be able to follow the same steps as if he were moving alone; meaning: first help the patient to flex the legs (or at least the one opposite to the side the patient is going to turn on) and then help him to roll over the side, making sure that the patient turns in one block (shoulder and pelvis at once, preventing torsion in the spine). Help can be providing when turning at the level of the shoulder and the hip. Another way to help a patient roll on the side is to use the bedsheet underneath him to make him turn.
To help a person going from one side of the bed to the other, the helper can help the patient to first flex the legs. The helper will then have to secure the patient feet to prevent them from slipping ways when lifting up the pelevis and help him to lift up his pelvis and move it on the side (the helper can use his own knees to secure the patients feet so that he would have both hands free to help lifting up the pelvis and moving it on the side). The helper can then help the patient moving his feet and shoulder on the side. To help the patient going up the bed, it is usually required to have two persons to help (one on each side of the bed). The helpers will first help the patient to flex his legs. Each
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 122 Page
one of them will then secure the patient pelvis and one shoulder and, together (on account of three), lift up the patient towards the head of the bed. (c) Sitting up and laying down alone
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
The easiest and most secure way to sit up from lying position is the go through the following steps:
First, the person has to turn on the side.
Once he/she is lying on the side, the person can put the legs out of the bed.
Then, pushing with both arms, the person sits up.
Note: If the person has difficulties to bring one of the legs out of the bed (because one leg is weaker than the other), he/she can use the other leg to "bring" the weak leg out of the bed.
Note: This way of sitting up is easier because the person can use the arms to push him/her up. Also, the legs out of the bed will make like a counterweight and help the person to sit up. Finally, this way of sitting up is safer then sitting up straight because sitting up straight might hurt the person's back.
To lie down, the same steps should be followed, but the other way around (first lie on the side using the arms), then put the legs on the bed and then turn on the back). (d) Sitting up and laying down with help To sit up with somebody's help, the same steps should be followed as sitting alone (turn on the side, put the legs out of the bed and then sit up using the arms). The helper first helps the person to turn on the side. Then, the helper secures the person's neck with one hand and the knee with the other hand and helps the person to sit up.
To lie down, the same steps should be followed, but the other way around (first lie on the side using the arms), then put the legs on the bed and then turn on the back). (e) Standing up and sitting down alone In order to ease standing up, a few important points should be respected:
The higher the chair (or the bed) is the easier it will be to stand up and sit down (as long as the person still can touch the ground with the foot when seated. If the chair is so high that the foot don't touch the ground in sitting position, it means that the chair is too high and standing alone from such a chair is dangerous).
Page - 123 Page
Feet flat on the ground Sit on the edge of the chair Bring the feet backwards Lean forwards when standing up
To sit down, a few recommendations can be given:
Before sitting down, the person should make sure that he/she feels the chair (or the bed) in the back of the knees. When he/she feels the chair, he/she can sit down. When sitting down, the person should lean forward.
Feel the chair at the back of the knee
Lean forwards when sitting down
(f) Standing up and sitting down with help To stand up and sit down with help, the same steps and recommendations should be followed as when standing up or sitting down alone. There are different ways help can be provided to someone to help him/her stand or sit. The main way is to provide help on one side by securing the person's arm. To do so, follow those rules:
The helper secures the person with one hand under the armpit. If needed, the helper can also help securing the person's knee using his/her own knee.
The helper let the person grasp his/her thumb and hand.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
When seated and before standing, the person should sit on the edge of the chair (or bed). To do so, if the chair as backrest, the person can push against the backrest with his/her back to push the buttock forward. If the person is well on the edge of the chair (or the bed) it will be easier to stand up. When seated and before standing, the person should bring the feet backwards. If the person keeps the feet in front, it will make it more difficult to stand up. When standing, the person should lean forward. If the person maintain the back backwards (or even straight), it is quite difficult to stand.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 124 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Note: When receiving help to standing or walking, an older person, in general, will feel more confident if he/she can hold the helper's hand (or thumb) instead of having the helper grasping his/her hand. Also, the helper's hand that is placed under the person's armpit provides the person security as he/she feels that he/she can squeeze it with his/her arm if he/she doesn't feel secure enough. Note: If the person sits up from a wheelchair or sits down in a wheelchair, for security and prevent falls, it is very important to make sure that: 1. The brakes are tight to prevent the chair from moving when the person sits or stands; and 2. That the footrests are up. Another way of helping somebody to stand and sit is by using a transfer belt. A transfer belt is a special belt that allows the helper to secure the person when standing up or sitting down. If transfer belt are not available, they can be changed by normal belt, even though a normal belt won't allow securing the person as well as a transfer belt does. (g) Transfer from bed to chair with a person that cannot stand If the person cannot help at all to move from the bed to a chair or to the toilets, here is how that person can be carried the most easily: One helper is behind the person and secures the person's both arms (the persons' arms are crossed to make the grasp more secure). A second helper secures both legs. 2.2. Mobility (a) Walking - Securing the person The main way of providing support to an elderly is using the same way of securing him/her then for standing up or sitting down:
The helper secures the person with one hand under the armpit. (b) Walking Using a belt
The helper let the person grasp his/her thumb and hand.
If the person doesn't need much help but there are risks of fall, the helper can secure the person using a belt (normal belt) that is placed around the person's waist. That way, the helper can secure the person if he/she losses balance and prevent the fall, but in the other hand he/she doesn't provide too much help and the person can improve better his/her walking abilities.
Page - 125 Page
(c) Walking Using mobility device Mobility devices are devices that help a person to move around. Walking stick or cane If a person has balance problems or is afraid of walking, a simple can help the person to feel more secure. A walking cane is the simplest walking aid. It is not very stable but it won't bring difficulties for the stairs or for obstacles. To adjust the height of the hand grip, do as follows: when the person stands with arms beside the body, the handgrip should be at the level of the wrist.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Tripod cane A tripod cane is a little bit like a simple cane except that it has three feet. Those three feet give more stability to the cane, which would give more stability to the person. In the same time, such a cane doesn't bring much more disadvantages then the simple cane (except that it is a bit heavier).
Note: When walking with a cane or a stick, if the person has a weaker leg, the cane or the stick should be hold by the opposite hand (people often tend to have the cane on the weak side, but it's the wrong way of walking with a cane).
Crutches Crutches are more stable than canes but it becomes a little bit more difficult to go up or down stairs. There are two main types of crutches: the elbow crutches and the axillary crutches. In China, people mainly use axillary crutches. If they are not well adapted to the person's height, axillary crutches can lead to nerve or blood circulation problems under the armpit. Therefore, the crutches' height should be adapted as described here below: To adjust the height of the hand grip (distant A), do as follows: when the person stands with arms beside the body, the handgrip should be at the level of the wrist. To adjust the height of the crutches (distant B), do as follows: when the person stands, top of the crutch should be three finger widths below the armpit (this is very important because there are many nerves and blood vessels that pass the armpit area. If the crutch is too high, the person will push on it and compress the nerves and blood vessels). There are various techniques of walking with crutches. Each person will, quickly, find the more adapted way to use his/her crutches. But, we present here 3 basics techniques that could help the caretakers to teach the person how to use his/her crutches.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 126 Page
The 4 points gait 1. 2. 3. 4. One crutch forward Opposite foot forward Other crutch forward Opposite foot forward
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
It is the most stable way, but it is a very slow gait The 3 points gait 1. Two crutches forward 2. The weaker leg forward 3. The stronger leg forward
The 2 points gait 1. One crutch and the opposite foot (at the same time) 2. The other crutch and the opposite foot (also at the same time)
It is the fastest gait and the closest to normal walking (arm and opposite leg at the same time) Going up and down the stairs When the person goes up or down the stairs, some basics rules must be observed: To go upstairs, the patient steps up with the stronger leg first To go downstairs, the patient steps down with the weaker leg first The crutches always follow the weaker leg The helper should always stay on the down-stair side of the patient (to stop him from falling)
Tip: To remember which leg goes first when going up or down, the person should remember the following: heaven is in the sky (up) while hell is in the earth (down). Therefore, they should use first the strong (good) leg to go up, and the weak one (bad) to go down.
Page - 127 Page
(d) Using a wheelchair with help
Note: The different parts of the wheelchair are the following
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1 2 3 4
= = = =
The The The The
seat backrest armrest tires
5 6 7 8 9
= = = = =
The The The The The
hand rim back wheel front wheel brakes footrests
Here are some security recommendations when using a wheelchair: If the person sits up from a wheelchair or sits down in a wheelchair, make sure that: 1. The brakes are tight to prevent the chair from moving when the person sits or stands; and 2. That the footrests are up. When going down a slope, the person in the wheelchair should lean backwards to prevent to chair from falling over.
When going down obstacles (one step), it is easier to go backwards. The helper secures the wheelchair's handle and brings the backwheels down the obstacles. He then lifts up the front wheels while going backwards and then brings them down the obstacle.
When going up obstacles (one step), the helper secures the wheelchair's handles and lift up the front wheels and brings them up the obstacle. Then, he lifts up the back wheels, pushing the chair forward to bring the wheels up the obstacle. The helper should be careful with holes in the ground as the front wheels may fall in the hole and the wheel may fall over. In such case, it might be better to push the chair on the back wheels or the pull the chair backwards. (d) Using a wheelchair alone The patient should be able to:
Move forward Move backward Turn Climb a slope Go down a slope Go over obstacles Go down obstacles Put the wheelchair back on its wheels
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 128 Page
Move forward To move forward, the patient secures the hand rims on both side and pushes in front (both side on the same time otherwise the chair will turn). To make the movement more efficient, the patient should make a movement in front with the trunk.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Move backward To move backward, the patient does the same as to go forward but he pulls the hand rims backward. Turn To turn the wheelchair, one arm pulls the wheel backward while the other arm pushes the opposite wheel forward. For example: to turn toward the right, the right arm pulls the wheel backward and the left arm pushes the wheel forward.
While riding, to turn, the patient can just push on one wheel (to turn right, the patient pushes on left wheel). He also can brake with his hand on one wheel (to turn right, the patient brakes with his hand on the left right wheel). Go up a slope To go up a slope, the patient has to do exactly the same as to go forward, but to make it easier he should always keep the trunk in front. If the slope is very stiff, the patient can move only one wheel while blocking the other one and then move the second wheel while blocking the first one.
Go down a slope To go down a slope, the patient brakes with his hands on both hand rims. He also should keep his trunk backward to prevent falling in front. If the slope is very stiff, he can go down backward. Go over obstacles To go over obstacles easily, the patient should be able to lift the front wheels off the ground. To do so, he has to pull the wheels backward (A) and give a quick push forward (B).
Page - 129 Page
While training to lift up the front wheels, the therapist should be behind the patient to prevent from falling backward. To make it easier, this exercise can be done on a mattress to make the chair more stable.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Note: The patient has to be able to maintain balance on the back wheels.
To go over the obstacle, the patient has to bring the wheelchair as close as possible form the obstacle. Then, he lifts up the front wheels to bring them on the obstacle. He bends the trunk in front and come up the obstacle by pushing on the hand rim.
Go down obstacles The technique to use to go down obstacles depends on the height of the obstacle. For a low obstacle, the patient can go down frontward. To do so, he has to lift up the front wheels and go down the obstacles on the back wheels to prevent from falling in front.
If the obstacle is too high or if the patient is afraid to go down frontward, he can go down backward. To do so safely, the patient should lean forward to prevent the wheelchair from tripping over. He then move the wheelchair at the edge of the obstacle and control the descent with the hand rims.
To go down stairs, the patient can go down backward as shown on the drawing. He secures the banister to slow down the descent.
Put the wheelchair back on its 4 wheels If the patient felt back with his wheelchair, he should be able to put it back on its wheels without getting out of the chair.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 130 Page
Here is how to do: First, the patient should flex his legs as much as possible to transfer the weight backward. Then he takes support on the ground with one hand while the other hand secures the opposite hand rim. He pushes on the ground with the hand and pushes the hand rim frontward with the other hand. He can then put the wheelchair back on its wheels.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Note: If the person that uses the wheelchair has feelings problems (doesn't feel very well when pinched), which can happen with hemiplegia for example, it is important that the person doesn't stay too long in the chair withoput moving. Indeed, if the person cannot feel very well and doesn'tchange position in the chair, pressure sores (holes in the skin) may appear very quickly. Such wounds can get infected and are difficult to heal.
Page - 131 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
PT Protocol for Positioning and Changing Position
1. General Information on Positioning and Changing Position
1.1. Definition Positioning means to put the patient in a good position (in bed or in a chair). Changing position means to change the patients position during the day so that he wont stay the whole day in the same position. 1.2. Purposes A good position is important to prevent complications that bedridden patient may face such as muscle retraction. A good position might also help with problem specific to one type of injury such as decreasing swelling in fracture or amputation or prevent pressure sore for patients with spinal cord or head injury (patients with sensitivity problems) or patients in coma (patient that dont move). Good positioning is also important to provide the patient with more stimulation. Indeed, if the patient is not well positioned, he wont see well what is around him and get less stimulation form environment. A good position also helps the patient to participate to daily life activities better. Changing position during the day (every two hours, at least), help preventing pressure sore by releasing pressure from some part of the body and allowing a better blood flow. Note: When the patients condition allows, it is necessary to sit him up (either in bed or better on the edge of the bed) as soon as possible. Indeed, lying position is not a very good position as it often leads to blood circulation problems blood clots- and other bedridden problems. Therefore, as soon as possible, the patient should be in sitting position. Putting the patient in sitting position with the feet out of the bed is called dangeling and such technique should be used as soon as possible see below). 1.3. Prescription Positioning and changing position should be prescribed to any patient that is in bed. Note: For some patients, depending on their injury, special recommendations should be provided regarding positiong nd changing of position. This is the case for patients with amputation, spinal cord injury, head injury or burn. For details, refer to the corresponding protocols.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 132 Page
2. Technique
Here below are general recommendations regarding positioning and changing position. 2.1. Positioning When lying on the back, the patient should keep his/her head straight. If the patient always keeps the head on the side, he/she should be reminded to keep it straight.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Attention should be given to the general position of the patient. On the drawings above are two examples: on the left, the wrong position and on the side the right one.
To prevent muscle contracture of the calf muscle (because of drop foot), special pillows can be used to hold the leg and the foot in neutral position. If such pillows are not available, normal pillows can also be used as shown on the above drawing.
In order to decrease or prevent swelling of the limbs, it is always better to try to keep the extremities of the limbs (hand and foot) a little bit higher than the rest of the body (elevation). This helps blood circulation and, therefore, help preventing and decreasing swelling. To prevent back lordosis leading to back pain, pillows can be placed under the patients knees to induce a slight flexion of the knees and the hips and straighten the back.
To prevent pressure sore, if special pillows or pads are not available, surgical gloves filled in with water or hot water bootle can be placed under the usual locations of pressure sores (heel, ankles, back of the shoulder). When lying on the side, pillows should be placed under or between the knees to prevent pressure sores and torsion in the back. A pillow should also be placed under the patients head to keep it straight. If needed, pillows can be placed behind the patients back to prevent him from turning on the back. In sitting position, attention should be paid to balance (make sure that the patient is stable and can maintain the position without risks of fall) and the persons position (back and head straight, feet flat on the ground if possible).
Page - 133 Page
Note: For specific recommendation on position for patients with head injury, spinal cord injury, amputation or burn, refer to corresponding protocols.
2.2. Changing position As a general rule, the patient position should be changed, at least, every two hours in order to prevent pressure sores and muscle retraction. The patient should change from lying on the back to lying on the side and, whenever possible, sitting position. For details on how to help a patient changing position, refer to the above protocol on transfer and mobility. Note on dangling As mentioned above, it is very important for the patient to sit up as early as possible, when his situation allows. Indeed, being lying down the whole day very quickly leads to further complications such as blood circulation problems, muscle shortness, respiratory or digestive problems. Therefore, the patient should be sitted in bed or better on the edge of the bed as soon as possible. Sitting the patient on the edge of the bed is called dangling. When doing dangling with a patient, it is important to follow the below recommendations: - If possible, lift up the head of the bed so that the patient is already in sitting position in the bed before sitting on the edge of the bed. This has 2 advantages: first, it will make it easier for the patient to sit on the edge of the bed from a sitting position. Secondly, sitting up the patient by lifting up the head of the bed helps preventing dizziness by sitting up the patient slowly (if the patient goes at once from lying position to sitting position, he might feel dizzy). - Once the patient is sitting on the edge of the bed, the helper should make sure that the patient is stable. If needed, pillows can be placed behind the patient to provide better stability. - The helper can then ask the patient to make small pendular movements with the legs and to move the feet and toes. - While the patient is in sitting position, the helper should keep an eye on the patient (see if he becomes pale) and asks him how he feels. If the patient feels more pain in such position or start to feel dizzy, he should go back to lying position. - Sitting on the edge of the bed should be done as soon as possible and as often as possible during the day until the patient feels better and more secure in that position and is ready to stand up.
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
To ensure a good position, make sure that the seat provides good support for the back and the head (if needed). If the patient cannot maintain a straight sitting position, use pillows to provide more support to the back and/or the head. If the seat is too high, put a flat object (such as a small stool) under the patients feet to make sure that they are flat on the ground. Having the feet flat on the ground or a support also helps improving th patients balance.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 134 Page
TRAINING OF REHABILITATION STAFF, NURSES AND DOCTORS IN HOSPITALS Teaching and Informing the Patient and His/Her Family Members
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
1. Introduction When providing early bedside PT treatment and guidance, it is very important to involve the patient and his/her family in the treatment. Indeed, and especially when there is an increased flow of patients (like it happen after a natural catastrophe such as an earth quake), there might not be the human resources to provide close follow-up of the treatment. Nevertheless, in order to be efficient, early rehabilitation exercises have to be done on a regular basis (2 to 3 times every day). This means that the therapists have to rely on the patient or his/her family to do the exercises by themselves under a distant follow-up from the therapist. Learning correct ways to do exercises might not be as easy as it seems. The exercises that should be taught to the patient are on purpose, very simple and basic exercises. Therefore for a professional therapist who is used and drilled with such exercises, it might seem that learning them shouldnt be a problem. The therapist will then spend only a few minutes explaining or demonstrating the exercise one or two times and expect the patient or his/her family do be able to reproduce them without any problem. This is a natural way of doing, but it might not be very efficient. Therefore, some principles have to be followed when teaching how to do exercises (those principles are detailed below). In order to insure a good involvement of the patient and his/her family in the treatment, it is also very important to provide them with clear and complete information on the patients situation and his/her needs. The patient and his/her family have to understand why doing exercises is important and how doing those exercises on a regular basis will actually help the patient. If the patient and his/her family have a good understanding on the patients needs and the purpose of the exercises (how they help), they will be much more keen to do them regularly. If they dont understand why they have to do them, they might just not do them. This document aims to explain the rules and principles that should be followed when informing and teaching patients/family, as well as the material available to ease such activities. 2. Principle for teaching As just explained, when teaching the patient or his/family how to do exercises, it is important to respect some principle and not consider that after just one or two demonstration by the therapist, the family will be able to do the exercises by themselves. Such way of doing might lead to misunderstanding and mistakes from the part of the patient/family when doing the exercises o their own (and in some case, doing an exercise in a wrong way might do more bad than good and make the patients situation even worse). Here are the steps that should be followed when teaching exercises to a patient or one of his family members: First, make sure that the person that will learn how to do the exercise (if he/she is a member of the family or a care-take) will be available for doing those exercises. It would be a waste of time to teach somebody that is just there for visiting. The person responsible for doing the exercises should be one of the patient care-takers. Then, show once or twice the correct way of doing the exercise.
Page - 135 Page
After you explained and demonstrate the exercise, ask the patient of the family member to do it. At first do it with him (place his/her hand correctly, correct the position, guide the movement). Then, ask him/her to do it a few times on his/her own. When the person does it on his/her own, correct him/her if necessary. Provide clear indications on how many times the exercise should be done and how often For example: Make this movement 20 times, three times a day. Use the material available for teaching such as the exercises cards and the small equipment. When possible, a distant follow-up should be done. This means, coming back to the same patient after a few days to make sure that the exercises are done regularly and correctly. During such visit, the patient/family member should be asked to demonstrate the way he/she does the exercises and new guidance or correction should be provided if necessary. Those follow-up visits can also be used to adapt the exercise plan (teach new exercises) depending on the patients improvement. Adapting the exercise plan by teaching new exercise insure that the patient will keep improving (if they keep doing the same exercises over and over, the patients improvement wont be as good).
3. Principles for informing When providing information on the patients situation and the patient needs, it is important to follow the following principles: When informing, use simple language that can be understood by everybody even if they dont have medical background. Technical words can be used (such as spasticity or muscle retraction or bedsores, because they might be difficult to replace with other words, but you have to explain them and make sure that the patient/family understands them correctly). Use the informative material available such as the information booklets. When possible, try to quickly go through it with the patient or the family members, pointing out the most important information. If they are left on their own with the material, they might not understand it very well. When you are finished explaining what you considered to be the most relevant information, give the opportunity to the patient/family members to ask questions. Indeed, they might have concerns that are not addressed in the general information booklets.
4. Material available for teaching and informing the patient/family There different types of material and equipment that ca be used to ease and make more efficient teaching and informing the patient/family. Those are:
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Explain what you are doing, how you are doing and why you are doing it. When doing that, try to use understandable vocabulary try to avoid, as much as possible, too technical words that the person would not understand. For example, say: Now, I am moving the leg up and down. This is important to prevent the muscles from becoming shorter because if they do become shorter, after the patient wont be able to extend the leg and it will be very difficult to stand and walk. I use one hand to secure the heel while the other hand is behind the knee. Then, I go up and down
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 136 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
The information folders o pathologies: Those are small booklets that provide general information on a specific pathology such as Information on brain damage or Information on spinal cord injury. Those booklets are very general. They content general information on the pathology (what it is, what causes it, what complications may appear, how the patient might evolve) as well as information on the patient needs (what type of exercise should be done and why those exercises have to be done). The information booklets on specific subjects: Those are small booklets that provide more detailed information on a specific subject such as Bedsore prevention or Catheterisation. They are not specific to one type of pathology (the information booklet on bedsore prevention can be useful for patients suffering from spinal cord injury but also for patient suffering from brain damage).
The exercises cards: Those are small cards describing one specific exercise (for example: Ankle passive mobilization). Those exercises are general, basic and easy-to-learn exercises. Most of them are not specific to pathology. Using those cards insures that the exercises can be adapted to the exact needs of the patient (some spinal cord injured patients will need to do some exercises that would be irrelevant for other spinal cord injured patients). Small equipment: When equipment is needed to perform the exercise, the small equipment can be used to demonstrate and teach the patient or the family member. Such equipment is easy to carry (no big equipment), easy to purchase (so that the family can easily by one on their own) and cheap.
Page - 137 Page
PART 4. ANNEXES The documents here below were referred to in the above protocols. Soft copies of those annexed documents are available on the capitalization DVD. Teaching and information material for the patients and their family The below documents can be found on the DVD Follow the link For the patients. Information Brochures Information Information Information Information Information Information Information Information Information Information Brochure Brochure Brochure Brochure Brochure Brochure Brochure Brochure Brochure Brochure Amputation Bedridden Burn Devices (orthopeadic/assistive) Fracture Head injury Prevention of pressure ulcers (bedsores) Rehabilitation Spinal Cord Injury Use of of Mobility Devices
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Exercises Cards Exercises Exercises Exercises Exercises Exercises Exercises Exercises Exercises Exercises Exercises Exercises Card Card Card Card Card Card Card Card Card Card Card Active Mobilization and Strengthening Amputation Balance Chest Therapy Shoulder Fracture Head Injury Passive and Assisted Mobilization Positioning Stretching Transfer and <mobility All
Patient management (blank forms) The below documents can be found on the DVD Follow the link Patient management. Patient File Early Rehabilitation Needs Assessment Form Rehabilitation Risk Assessment Form Assessment From Exercise Plan Patient Database ASIA Scale Barthel Index Glasgow Scale
Rehabilitation checklist guidelines The below documents can be found on the DVD Follow the link Guidelines.
EARLY MANAGEMENT
EARLY MANAGEMENT OF EARTHQUAKE VICTIMS
Page - 138 Page
EARLY REHABILITATION PROTOCOLS FOR V ICTIMS OF NATURAL DISASTER
Rehabilitation Rehabilitation Rehabilitation Rehabilitation Rehabilitation Rehabilitation Rehabilitation
checklist checklist checklist checklist checklist checklist checklist
guideline guideline guideline guideline guideline guideline guideline
amputation bedridden/ICU burn crush syndrom fracture head injury SCI
Você também pode gostar
- Clinical Protection Handbook: for Healthcare Workers against COVID-19No EverandClinical Protection Handbook: for Healthcare Workers against COVID-19Ainda não há avaliações
- Rehabilitation interventions in the patient with obesityNo EverandRehabilitation interventions in the patient with obesityPaolo CapodaglioAinda não há avaliações
- Eng PDFDocumento116 páginasEng PDFOluz WangiAinda não há avaliações
- Guidance For Physiotherapists - Paediatric Manual HandlingDocumento50 páginasGuidance For Physiotherapists - Paediatric Manual HandlingPT Depart AMCHAinda não há avaliações
- 82110732Documento1 página82110732Firas DrAinda não há avaliações
- (Practical Issues in Geriatrics) Paolo Falaschi, David R. Marsh (Eds.) - Orthogeriatrics-Springer International Publishing (2017)Documento214 páginas(Practical Issues in Geriatrics) Paolo Falaschi, David R. Marsh (Eds.) - Orthogeriatrics-Springer International Publishing (2017)Sevtap Günay UçurumAinda não há avaliações
- Safe Hospitals ManualDocumento43 páginasSafe Hospitals ManualMaeDaphneYapAinda não há avaliações
- Physical Therapy ProtocolsDocumento237 páginasPhysical Therapy ProtocolsMani Physio100% (25)
- Pta 1500 Term ProjectDocumento17 páginasPta 1500 Term Projectapi-270787423Ainda não há avaliações
- Acute Care Surgery Handbook: General Aspects, Non-Gastrointestinai and Critical Care EmergenciesDocumento512 páginasAcute Care Surgery Handbook: General Aspects, Non-Gastrointestinai and Critical Care EmergenciesOscar Villacres100% (6)
- Early Rehabilitation: in Conflicts and DisastersDocumento220 páginasEarly Rehabilitation: in Conflicts and DisastersRita MoreiraAinda não há avaliações
- Hospital Disaster Risk Reduction GuidelinesDocumento43 páginasHospital Disaster Risk Reduction GuidelinesEdjey Luis F. MatinongAinda não há avaliações
- Infográfico Interativo Com Atividade Formativa Reabilitação e Qualidade de Vida Do Idoso Com Deficiência Após AVE - Validacao - VictorDocumento6 páginasInfográfico Interativo Com Atividade Formativa Reabilitação e Qualidade de Vida Do Idoso Com Deficiência Após AVE - Validacao - VictorVictor NogueiraAinda não há avaliações
- Rehab After Shoulder SurgeryDocumento11 páginasRehab After Shoulder Surgerymarcelogascon.oAinda não há avaliações
- Must Know ETC Manual At-New-LayoutDocumento170 páginasMust Know ETC Manual At-New-LayoutMihai Salceanu0% (1)
- Hierarchy of Rehabilitation Needs Case Study SampleDocumento6 páginasHierarchy of Rehabilitation Needs Case Study Samplepeng kulongAinda não há avaliações
- Bilateral Transtibial Amputation With Concomitant Thoracolumbar Vertebral Collapse in A Sichuan Earthquake SurvivorDocumento9 páginasBilateral Transtibial Amputation With Concomitant Thoracolumbar Vertebral Collapse in A Sichuan Earthquake Survivorjehinson peaAinda não há avaliações
- Strok Stroke Rehabilitation e Rehabilitation: Pathway Last Updated: March 2017Documento16 páginasStrok Stroke Rehabilitation e Rehabilitation: Pathway Last Updated: March 2017blaeghAinda não há avaliações
- Advanced Rehabilitation Technologyfor LLDocumento10 páginasAdvanced Rehabilitation Technologyfor LLqqwwaAinda não há avaliações
- IHFG Part B Rehabilitation Allied HealthDocumento19 páginasIHFG Part B Rehabilitation Allied Healthamir alamAinda não há avaliações
- Checklist For Field Use IASC MHPSSDocumento40 páginasChecklist For Field Use IASC MHPSSconnecting07Ainda não há avaliações
- Handicap International RehabilitationDocumento80 páginasHandicap International RehabilitationMuhammad Shadi Al-RajehAinda não há avaliações
- Technology Guidelines For A District Eye Care Programme: July 2006Documento53 páginasTechnology Guidelines For A District Eye Care Programme: July 2006Peter AbikoyeAinda não há avaliações
- Muscle Strength and Physical FitnessDocumento20 páginasMuscle Strength and Physical FitnesschristinaAinda não há avaliações
- NS 01 YohanaDocumento16 páginasNS 01 YohanaYohanaAbeysinghe100% (1)
- 2016 Toronto ERAS - STOMA - BPS - FINAL - 2018Documento25 páginas2016 Toronto ERAS - STOMA - BPS - FINAL - 2018durdane palabiyik yilmazAinda não há avaliações
- Author Information: Lakhey S Jha N Shrestha BP Niraula SDocumento3 páginasAuthor Information: Lakhey S Jha N Shrestha BP Niraula SSabina RanabhatAinda não há avaliações
- Role of The HospitalDocumento11 páginasRole of The HospitalChan Keng ChunAinda não há avaliações
- Spinal Cord Injuries: Guide ToDocumento42 páginasSpinal Cord Injuries: Guide ToKezAinda não há avaliações
- AnkleSprain PCG 27032009Documento30 páginasAnkleSprain PCG 27032009Rachel BlackburnAinda não há avaliações
- Chapter II: Review of Related LiteratureDocumento11 páginasChapter II: Review of Related LiteratureJohn Gabriel SamsonAinda não há avaliações
- LN Ecology FinalDocumento93 páginasLN Ecology Finalমাসুদ প্রামাণিকAinda não há avaliações
- Aichner 2002Documento15 páginasAichner 2002cah bagusAinda não há avaliações
- Clinical Skill Books PDFDocumento384 páginasClinical Skill Books PDFnamitaAinda não há avaliações
- 2.rehabilitation NursingDocumento7 páginas2.rehabilitation Nursingarava.swapnaAinda não há avaliações
- Whiplash InjuriesDocumento393 páginasWhiplash InjuriesWilliam VenegasAinda não há avaliações
- WHO Plan of ActionDocumento7 páginasWHO Plan of ActiontenzinAinda não há avaliações
- IUI Paper Q2. ADocumento5 páginasIUI Paper Q2. AMuhammad Ammar GhaniAinda não há avaliações
- Manual Handling of People in The Homecare EnvironmentDocumento2 páginasManual Handling of People in The Homecare EnvironmentvillarroyaAinda não há avaliações
- Emergency Surgery in Obese Patients, 2020Documento201 páginasEmergency Surgery in Obese Patients, 2020AmyandAinda não há avaliações
- HospitalsDocumento16 páginasHospitalsgemergencycareAinda não há avaliações
- Health Laws Health EthicsDocumento64 páginasHealth Laws Health EthicsEskindirAinda não há avaliações
- Basic Guide To Anesthesia For Developing CountriesDocumento242 páginasBasic Guide To Anesthesia For Developing Countriescltadams100% (4)
- Sea Ment 151Documento39 páginasSea Ment 151Irene FranzAinda não há avaliações
- Occupational Therapy in Amputee Rehabilitation.: Sue HayesDocumento23 páginasOccupational Therapy in Amputee Rehabilitation.: Sue HayesCatrinel ȘupialăAinda não há avaliações
- Emergency Care: Advocating ForDocumento39 páginasEmergency Care: Advocating Forsalza nurbaiti salamahAinda não há avaliações
- Integrated Acute Stroke Unit Care: ReviewDocumento9 páginasIntegrated Acute Stroke Unit Care: Reviewsatyagraha84Ainda não há avaliações
- Trauma Rehabilitation Clinical Guideline: Brain InjuryDocumento12 páginasTrauma Rehabilitation Clinical Guideline: Brain InjuryAhmad AliAinda não há avaliações
- ICN 2022 Disaster-Comp-Report en WEBDocumento20 páginasICN 2022 Disaster-Comp-Report en WEBJAMES ANDRE RENDONAinda não há avaliações
- 4 5893154064547450615Documento26 páginas4 5893154064547450615AyensuaAinda não há avaliações
- The OT Role in Rehabilitation For The Person With An Upper-Limb AmputationDocumento2 páginasThe OT Role in Rehabilitation For The Person With An Upper-Limb AmputationThe American Occupational Therapy AssociationAinda não há avaliações
- Code of Conduct For Anesthetists Working in Ethiopia To Be SentDocumento34 páginasCode of Conduct For Anesthetists Working in Ethiopia To Be SentyeabsraAinda não há avaliações
- Trauma and Emergency Health Care Manual: A Guide for Nursing and Medical StudentsNo EverandTrauma and Emergency Health Care Manual: A Guide for Nursing and Medical StudentsAinda não há avaliações
- The Human Challenge of Telemedicine: Toward Time-sensitive and Person-centered Ethics in Home TelecareNo EverandThe Human Challenge of Telemedicine: Toward Time-sensitive and Person-centered Ethics in Home TelecareAinda não há avaliações
- Comprehensive Geriatric AssessmentNo EverandComprehensive Geriatric AssessmentAlberto PilottoAinda não há avaliações
- TÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANONo EverandTÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANOAinda não há avaliações
- Mastering ICU Nursing: A Quick Reference Guide, Interview Q&A, and TerminologyNo EverandMastering ICU Nursing: A Quick Reference Guide, Interview Q&A, and TerminologyAinda não há avaliações
- Doroga Bahrm21s1 Pe003 Fitness Journal LogDocumento4 páginasDoroga Bahrm21s1 Pe003 Fitness Journal LogJeah Joyce LagrimasAinda não há avaliações
- Learn Sujok AcupunctureDocumento4 páginasLearn Sujok AcupunctureKarthik Kumar100% (1)
- RHIHLIA21168V012021Documento7 páginasRHIHLIA21168V012021pizza nmorevikAinda não há avaliações
- Folic Acid and Periodontal Disease PDFDocumento8 páginasFolic Acid and Periodontal Disease PDFAnonymous 8raPGW1tLAinda não há avaliações
- Revealing What Is Distinct by Recognising What Is Common: Distinguishing Between Complex PTSD and Borderline Personality Disorder Symptoms Using Bifactor Modelling 2020Documento10 páginasRevealing What Is Distinct by Recognising What Is Common: Distinguishing Between Complex PTSD and Borderline Personality Disorder Symptoms Using Bifactor Modelling 2020Nicolás MaturanaAinda não há avaliações
- Prenatal Factors Influencing Growth and Development of FetusDocumento15 páginasPrenatal Factors Influencing Growth and Development of FetusSrd Rch100% (1)
- Lawlor Et Al. (2017) Service User Satisfaction With CBTPDocumento19 páginasLawlor Et Al. (2017) Service User Satisfaction With CBTPnuriasegarramarAinda não há avaliações
- Lectures in PediatricsDocumento217 páginasLectures in PediatricsPachiappan NatarajanAinda não há avaliações
- CarcinosinDocumento42 páginasCarcinosinHilery DorrianAinda não há avaliações
- CSHPDocumento2 páginasCSHPKeren EbarleAinda não há avaliações
- Homeless CenterDocumento2 páginasHomeless CenterDelontae HullAinda não há avaliações
- Gordon's Functional PatternsDocumento2 páginasGordon's Functional PatternsFatima Love Ariate-ArcasetasAinda não há avaliações
- Medicine - IJGMP - HUMAN IMMUNO DEFFICIENCY - Adetunji Oladeni Adeniji - NigeriaDocumento10 páginasMedicine - IJGMP - HUMAN IMMUNO DEFFICIENCY - Adetunji Oladeni Adeniji - Nigeriaiaset123Ainda não há avaliações
- Recent Advances in The Development of Anti-Tuberculosis Drugs Acting On Multidrug-Resistant Strains: A ReviewDocumento18 páginasRecent Advances in The Development of Anti-Tuberculosis Drugs Acting On Multidrug-Resistant Strains: A Reviewmalik003Ainda não há avaliações
- Lichen PlanusDocumento6 páginasLichen PlanusMerry MiraAinda não há avaliações
- Solution Manual For Using Mis 7 e 7th Edition 0133546438Documento14 páginasSolution Manual For Using Mis 7 e 7th Edition 0133546438MarieHughesebgjp100% (74)
- Nursing Care of Client With Kidney CancerDocumento19 páginasNursing Care of Client With Kidney CancerancoursAinda não há avaliações
- Process of ReproductionDocumento18 páginasProcess of ReproductionAxielvie BabateAinda não há avaliações
- TI Activity 2 Getting Familiar With My Second HomeDocumento8 páginasTI Activity 2 Getting Familiar With My Second HomeSheila Mae CaballaAinda não há avaliações
- Principles of KinesioTaping 2014Documento29 páginasPrinciples of KinesioTaping 2014Wijaya Krisna I NyomanAinda não há avaliações
- Nursing Care PlanDocumento3 páginasNursing Care Plananon_984362Ainda não há avaliações
- Papa Sehat Oktober 2022 Puskesmas Sungai LimauDocumento183 páginasPapa Sehat Oktober 2022 Puskesmas Sungai LimauSeptiaAinda não há avaliações
- Quiz 2Documento3 páginasQuiz 2air france bargamentoAinda não há avaliações
- Case HistoryDocumento16 páginasCase HistoryGeena Thaploo100% (1)
- Injeksi BookDocumento13 páginasInjeksi BookSyarif SamAinda não há avaliações
- Clinical Trial Audit FDA Reg OutlinesDocumento12 páginasClinical Trial Audit FDA Reg OutlinesKateAinda não há avaliações
- Jadwal Oral & EposterDocumento8 páginasJadwal Oral & Eposteranton MDAinda não há avaliações
- Health Insurance UnderwritingDocumento59 páginasHealth Insurance UnderwritingDJR DJRAinda não há avaliações
- Global Cultural Climate (Let Us Check What You Have Read!: Week #3 Activity #2: INDIVIDUAL ACTIVITY/ ASSESSMENT (Page 35)Documento3 páginasGlobal Cultural Climate (Let Us Check What You Have Read!: Week #3 Activity #2: INDIVIDUAL ACTIVITY/ ASSESSMENT (Page 35)ElleAinda não há avaliações
- Food Contamination Worksheet 2Documento3 páginasFood Contamination Worksheet 2compilationsAinda não há avaliações