Escolar Documentos
Profissional Documentos
Cultura Documentos
Cancer Center Improves Lab Specimen Labeling with Lean Six Sigma
Enviado por
drustagiDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Cancer Center Improves Lab Specimen Labeling with Lean Six Sigma
Enviado por
drustagiDireitos autorais:
Formatos disponíveis
Lessons in Labeling
Cancer center reduces lab specimen errors with lean Six Sigma
by Nina Braswell, Jill Koroseta and Amy Grogan
In 50 Words Or Less
Incomplete information on specimen-container labels at a cancer center led to errors and often meant a second round of specimen collections, representing rework and wasted time. The define, measure, analyze, improve and control method guided the center to improve the labeling part of the collection process, saving time and money.
What kind of care would you want for a loved one who is fighting cancer? This is the question the experts at Cancer Treatment Centers of America (CTCA) ask themselves every day, and its this question that motivates all employees to create a culture in which continuous improvement becomes a habit. To fully achieve this goal, CTCA recognized that it had to begin by empowering its employees, or stakeholders, to make a difference. The lean Six Sigma program at CTCA does just that: empowers employees with the tools necessary to improve their workplace and work processes, which ultimately affects patients. To have the lean Six Sigma concepts integrated into the culture, there is a portfolio of lean Six Sigma courses offered by job title. For example, front-line employees participate in a seven-week A3 performance improvement lean course and, for those who qualify, an 11-day Green Belt training course. Furthermore, supervisors, managers and executives attend Champion training to acquire the skills and learn the tools and templates needed to support employees who attend lean Six Sigma training. CTCAs lean Six Sigma vision is to have a fully integrated lean Six Sigma philosophy across the entire enterprise through empowered employees who consistently strengthen a standard model of care, which is entirely driven by advanced, whole-person treatment options and the kind of care you would want for family members. CTCA calls this "the mother standard." This standard at CTCA is designed to inspire process innovation and to effectively, efficiently and responsively drive the delivery of a superior patient experience. In June 2011, CTCA became the first institution in healthcare to receive a recommendation from the American Council on Education (ACE) for college credit for
the A3 (two lower-division semester hours) and Green Belt (six upper-division semester hours) courses. ACE is the major coordinating body for 2,200 of the nations higher education institutions. With its recommendation, CTCA has made its patient-driven program a relevant component of employees personal and professional development. The business results have been exceptional. One of the authors of this article, Nina Braswell, the laboratory quality assurance coordinator, was the Green Belt student who applied the skills and tools she learned in class while working on the following high-impact project at CTCAs Midwestern Regional Medical Center in Zion, IL, using the define, measure, analyze, improve and control (DMAIC) process.
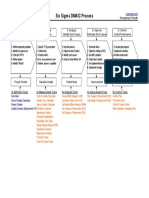
Define
The DMAIC process starts when a problem has been identified. The define phase helps to clarify the understanding of why it is a problem. The laboratory was receiving, testing and verifying results from incompletely labeled nonblood specimens. A label is considered incomplete if it does not contain one or more of the following pieces of information: patients name, medical record number, date, time of collection, specimen type and tech code, which is the identification number of the person collecting the specimen. It was determined that the specimen that had the most incomplete labels was urine for urinalysis. Standards state urine specimens must be examined within one to two hours of collection or they cannot be used for analysis. After two hours, the specimens constituents change, degrade or disappear. It was evident a new process needed to be implemented to meet standards and guarantee the quality of results for all nonblood specimens. The baseline showed that only 15% of the nonblood specimens were labeled completely.
Measure
The purpose of the measure phase is to obtain a current-state baseline of the process while collecting accurate data that truly represents the effects of the process. Data collection confirmed the most common error was missing information on the nonblood specimens. It also was clear that three primary units (as shown in the Pareto chart in Figure 1) were responsible for 79% of the incompletely labeled nonblood specimens:
Return patient clinic (RPC)36.1%. Stem cell (SC): inpatient and outpatient30.5%.
New patient clinic (NPC)12.4%.
It was determined that the time of collection was the most frequently omitted information. Additionally, it was discovered that five different types of labels were being used: chart labels, collection manager labels, handwritten labels, temporary labels and cup labels. Data collection highlighted the need for the standardization of labels and the information to be included on them.
Analyze and improve
In the analyze phase, you examine the process, identify the root causes of defects and variations in the process, and validate these with the data collected in the measure phase. In the improve phase, you also formulate and test solutions, and implement a future state of the process that increases customer satisfaction, reduces or eliminates defects and variations within a process, and increases productivity. The root cause analysis of the incomplete specimen labels revealed there was not a standardized and uniform process for labeling nonblood specimens. Data showed and confirmed there was a need to implement a new standardized process that would guarantee quality results. Using a collection manager to draw blood had been previously implemented. With a collection manager, the patients armband is scanned, and laboratory orders for that patient are displayed. The blood is drawn and tubes are labeled at the patients bedside. This guarantees positive patient identification.
Collection managers also can be used for any type of laboratory specimen. The collection manager label provides all needed informationexcept for time of collection for urine samples. The time printed on the collection manager label is actually the time the labels print and not necessarily the time of urine collection. Because of the time-sensitive nature of urine samples, the actual time of collection is needed, so an additional time label is now affixed to the bio-bag. Patients, RNs and patient care technicians can now capture time of collection on this additional label. Using a collection manager also ensures only specimens with a physicians order will be collected. This prevents nonvalue-added time for the lab employees. Previously, lab employees needed to call an average of 15 times per week and ask for orders to be put into the electronic health record. This step also eliminates the nonvalue-added time for hospital staff to obtain orders from the physician, who may or may not want testing on the specimen collected. The time spent calling was an average of three minutes per patient for a total of 39 hours per year. A pilot program was implemented on Dec. 22, 2010, in the RPC. A training document was created, and all RPC RNs and the laboratory phlebotomy staff were trained on the new process. Auditing began on Jan. 3, 2011. Following the success of this pilot, the NPC was added to the audit on Jan. 17, 2011, and an increase in completely labeled specimen compliance from the RPC and NPC was noted. From this pilot, results improved by more 250% (see "Interim" in the staged control chart in Figure 2).
Finally, the ER, intensive care units, and the SC, infusion and inpatient oncology units were added to the program on Feb. 21, 2011. An initial decrease in compliance was noted because of a learning curve for the new units. Beginning Feb. 28, 2011, units were contacted to either re-collect the specimen or come to the lab and write the time on urine specimens. RN managers were emailed about all noncompliant issues. By Feb. 28, 2011, this new approach had resulted in a 23% increase in the compliance rate. More than one year after full implementation of the project, the compliance rate since the start of the project has increased by 287%.
Control
The purpose of this phase is to quantify the improvements that have been made, evaluate the implemented future state process, implement process controls and define the standard work instructions for the newly implemented process. Braswell, in conjunction with her project team members, decided on the following four steps to ensure the projects sustainability over time: 1. Set a threshold for properly labeled specimens. 2. Reject incompletely labeled specimens. 3. Require the lab to contact the RN manager with date, employee, patient information and issue if the number of labeled specimens falls below the threshold. An audit will take place one day or week for one month. If compliance stays above the threshold, the audit will be discontinued. 4. Add labeling requirements to new RN/patient care technician orientation. Results of the entire project included:
Increased patient satisfaction due to less re-collection of specimens. Increased label compliance by 287%. Saved 1,040 urine cups, for a total savings of $166.40. Reduced nonvalue-added time for employees from processing unnecessary specimens by 39 hours per year, yielding a soft savings of $525.
Higher patient satisfaction
Increasing labeled laboratory specimens compliance by 287% has had a positive impact in more ways than one. Most notably, patient satisfaction has increased as a result of reducing the amount of specimens that were incompletely labeled. Moreover, because most specimens are now labeled completely and uniformly, the time spent processing unnecessary specimens has decreased. Overall, the project has demonstrated how CTCA uses the model standard of care. The infusion of lean Six
Sigma methods into the culture helps employees focus on what is truly important: caring for patients.
Nina Braswell is the director of laboratory services for Cancer Treatment Centers of America (CTCA) in Newnan, GA. She holds a masters degree in health sciences from Mississippi College in Clinton. She is an ASQ member and a certified Six Sigma Green Belt. Jill Koroseta is director of classroom learning and lean Six Sigma trainer at International Capital and Management Co. in St. Thomas, Virgin Islands. She holds a bachelors degree in economics and business administration from Ursinus College in Collegeville, PA. She is an ASQ member and a certified Six Sigma Black Belt. Amy Grogan is a management fellow with CTCA in Philadelphia. Grogan has a bachelors degree in English literature from the College of the Holy Cross in Worcester, MA. She is an ASQ member and a certified Six Sigma Black Belt.
Você também pode gostar
- Capstone Project: Process Improvement Specimen Lab WorkflowDocumento11 páginasCapstone Project: Process Improvement Specimen Lab Workflowapi-529869472Ainda não há avaliações
- CQI by CommitteeDocumento6 páginasCQI by CommitteeJhOy XiAinda não há avaliações
- Don't Lose PatientsDocumento9 páginasDon't Lose PatientsdrustagiAinda não há avaliações
- 1 s2.0 S0272271216300907 MainDocumento14 páginas1 s2.0 S0272271216300907 MainPUPUT PUJIANTIAinda não há avaliações
- Hospital Reduces Medication Errors Using DMAICDocumento9 páginasHospital Reduces Medication Errors Using DMAICdrustagiAinda não há avaliações
- V105 Article HanaffiDocumento15 páginasV105 Article HanaffiCarlo SacdalanAinda não há avaliações
- Lean Six Sigma Methodologies Improve Clinical Laboratory Efficiency and Reduce Turnaround TimesDocumento5 páginasLean Six Sigma Methodologies Improve Clinical Laboratory Efficiency and Reduce Turnaround TimesVipul SehgalAinda não há avaliações
- Applying Lean/Toyota Production System Principles To Improve Phlebotomy Patient Satisfaction and WorkflowDocumento6 páginasApplying Lean/Toyota Production System Principles To Improve Phlebotomy Patient Satisfaction and WorkflowHery IswantoAinda não há avaliações
- A Matrix Model For Phlebotomy Quality AssuranceDocumento15 páginasA Matrix Model For Phlebotomy Quality AssuranceandhiAinda não há avaliações
- A Review of Medical Errors in Laboratory Diagnostics and Where We Are TodayDocumento7 páginasA Review of Medical Errors in Laboratory Diagnostics and Where We Are TodayRobert MaynardAinda não há avaliações
- Modern Quality ManagementDocumento9 páginasModern Quality Managementselinasimpson1001Ainda não há avaliações
- Quality Control in HistopathologyDocumento30 páginasQuality Control in HistopathologyMuhammad Jamiu Bello78% (9)
- CPHQ ResponseSummaryDocumento21 páginasCPHQ ResponseSummaryAlex AlemanAinda não há avaliações
- Good Laboratory Practice For Waived Testing SitesDocumento4 páginasGood Laboratory Practice For Waived Testing SitesSheilaAinda não há avaliações
- Lab Audit1Documento5 páginasLab Audit1Yagna SubrmanianAinda não há avaliações
- Clinical Audit For Medical StudentsDocumento6 páginasClinical Audit For Medical StudentsAmal SaeedAinda não há avaliações
- Labman-Prelims ReviewerDocumento5 páginasLabman-Prelims ReviewerJohn Oliver AsiaAinda não há avaliações
- Clinical AuditDocumento2 páginasClinical AuditTan Choong ShenAinda não há avaliações
- Application Six Sigma Reduce Medical Errors Cathy Buck 2001Documento4 páginasApplication Six Sigma Reduce Medical Errors Cathy Buck 2001mariagianniAinda não há avaliações
- Bertholf2017 Chapter LaboratoryStructureAndFunctionDocumento23 páginasBertholf2017 Chapter LaboratoryStructureAndFunctionci8084102Ainda não há avaliações
- 2.3 WHO Competency Assessment v1Documento5 páginas2.3 WHO Competency Assessment v1edrialdeAinda não há avaliações
- Interview Information SystemDocumento9 páginasInterview Information Systemjames smithAinda não há avaliações
- Chapter 2Documento14 páginasChapter 2AdityaDhanrajSinghAinda não há avaliações
- QualityDocumento8 páginasQualityjadema14Ainda não há avaliações
- Continuous Improvement Approach Can Optimize Manufacturing OperationsDocumento15 páginasContinuous Improvement Approach Can Optimize Manufacturing OperationsMane DaralAinda não há avaliações
- Using Lean Six Sigma Techniques To Improve Efficiency in Outpatient Ophthalmology ClinicsDocumento9 páginasUsing Lean Six Sigma Techniques To Improve Efficiency in Outpatient Ophthalmology ClinicsMinh Nguyễn Phương HồngAinda não há avaliações
- New Quality Improvement Plan For Reducing Patient Assessment Errors at Health FiDocumento8 páginasNew Quality Improvement Plan For Reducing Patient Assessment Errors at Health Firexhudson100Ainda não há avaliações
- Using Lean Principles To Optimise Inpatient Phlebotomy ServicesDocumento7 páginasUsing Lean Principles To Optimise Inpatient Phlebotomy ServicesMuizzuddin MuizAinda não há avaliações
- Identification and Implementation of Quality Indicators For Improvement, Monitoring and Evaluation of Laboratory QualityDocumento56 páginasIdentification and Implementation of Quality Indicators For Improvement, Monitoring and Evaluation of Laboratory Qualityflorin020Ainda não há avaliações
- A Lean Six Sigma Approach To Reduce Waiting and Reporting Time in The Radiology Department of ADocumento9 páginasA Lean Six Sigma Approach To Reduce Waiting and Reporting Time in The Radiology Department of AH KhalifaAinda não há avaliações
- Volume 8 - Issue 4, 2008 - Healthcare Economics: Quality Management in Radiology: Defining The ParametersDocumento3 páginasVolume 8 - Issue 4, 2008 - Healthcare Economics: Quality Management in Radiology: Defining The ParametersBriane BandeiraAinda não há avaliações
- Benchmarking Clinic Wait TimesDocumento2 páginasBenchmarking Clinic Wait TimesMilton Fonseca ZuritaAinda não há avaliações
- Applying Lean and Six Sigma To Your Dermatology PracticeDocumento7 páginasApplying Lean and Six Sigma To Your Dermatology PracticedrustagiAinda não há avaliações
- Rato - Quality of Specimen NotesDocumento5 páginasRato - Quality of Specimen NotesAileen SacayAinda não há avaliações
- A Practical Guide To Using Service User Feedback Outcome ToolsDocumento99 páginasA Practical Guide To Using Service User Feedback Outcome ToolsPeter LawsonAinda não há avaliações
- Corazon: A Clinic Record Management System For PUNP TayugDocumento4 páginasCorazon: A Clinic Record Management System For PUNP TayugJames Reden Salagubang CerezoAinda não há avaliações
- Baccountingackground Researc1Documento6 páginasBaccountingackground Researc1Noor Ul AinAinda não há avaliações
- Quality ImprovementDocumento3 páginasQuality ImprovementViky SinghAinda não há avaliações
- Forum - Test SafetyDocumento2 páginasForum - Test SafetyhhhAinda não há avaliações
- Critical Pathway: Clinical Pathways Have Four Main Components (Hill, 1994, Hill 1998)Documento5 páginasCritical Pathway: Clinical Pathways Have Four Main Components (Hill, 1994, Hill 1998)pooja singhAinda não há avaliações
- DR Raya Ezat Lec 4Documento16 páginasDR Raya Ezat Lec 4Djdjjd SiisusAinda não há avaliações
- MGT620 - County Hospital Ñ Process ImprovementDocumento11 páginasMGT620 - County Hospital Ñ Process Improvementmanali gupta100% (1)
- Dr. Tjan Sian Hwa's Curriculum VitaeDocumento29 páginasDr. Tjan Sian Hwa's Curriculum VitaeSamsul BahriAinda não há avaliações
- Unit 1_ Introduction to Qa (1)Documento52 páginasUnit 1_ Introduction to Qa (1)hezkiyasgashawAinda não há avaliações
- Action PlanDocumento3 páginasAction Planmy.nafi.pmp5283Ainda não há avaliações
- Corazon: A Clinic Record Management System For PUNP TayugDocumento6 páginasCorazon: A Clinic Record Management System For PUNP TayugJames Reden Salagubang CerezoAinda não há avaliações
- Purpose/Objective: of ofDocumento16 páginasPurpose/Objective: of ofSA RAIAinda não há avaliações
- Phlebotomy Preanalytic VariablesDocumento39 páginasPhlebotomy Preanalytic VariablesMahogony Scott100% (1)
- Roils Paper 2Documento3 páginasRoils Paper 2api-632146706Ainda não há avaliações
- 429-Article Text-595-1-10-20210303 (3)Documento17 páginas429-Article Text-595-1-10-20210303 (3)Christian David Comilang CarpioAinda não há avaliações
- Biochem - Med 22 3 342 9Documento10 páginasBiochem - Med 22 3 342 9Rute RibeiroAinda não há avaliações
- High RSKDocumento1 páginaHigh RSKvenkat raAinda não há avaliações
- Lesson 2. Quality AssessmentDocumento2 páginasLesson 2. Quality AssessmentdyoAinda não há avaliações
- Lean Six Sigma in HospitalDocumento10 páginasLean Six Sigma in Hospitalterrac3211Ainda não há avaliações
- Laboratory Methods For The Diagnosis of Meningitis - CHAPTER 13 - Quality Control - Quality AssuranceDocumento7 páginasLaboratory Methods For The Diagnosis of Meningitis - CHAPTER 13 - Quality Control - Quality Assuranceselvalakshmi RAinda não há avaliações
- Chpt13 Quality Control AssuranceDocumento7 páginasChpt13 Quality Control Assurancevisini100% (1)
- Evaluation & Control of Pre Analytical Errors in Required Quality Variables of Clinical Lab ServicesDocumento18 páginasEvaluation & Control of Pre Analytical Errors in Required Quality Variables of Clinical Lab ServicesIOSRjournalAinda não há avaliações
- Applying Lean Techniques to Improve Patient SchedulingDocumento7 páginasApplying Lean Techniques to Improve Patient SchedulingjessicaAinda não há avaliações
- Efficient Radiology: How to Optimize Radiology OperationsNo EverandEfficient Radiology: How to Optimize Radiology OperationsAinda não há avaliações
- SDC Course OutlineDocumento3 páginasSDC Course OutlinedrustagiAinda não há avaliações
- Top Questions Asked About SAFe ExamsDocumento2 páginasTop Questions Asked About SAFe ExamsdrustagiAinda não há avaliações
- New Blank TemplateDocumento11 páginasNew Blank TemplateAmine MoutaqiAinda não há avaliações
- Change Log TemplateDocumento3 páginasChange Log TemplatedrustagiAinda não há avaliações
- Appreciation Cards v.1.0Documento2 páginasAppreciation Cards v.1.0drustagiAinda não há avaliações
- APG Design and Development 2015Documento7 páginasAPG Design and Development 2015John RajeshAinda não há avaliações
- Create the future storyboardDocumento1 páginaCreate the future storyboarddrustagiAinda não há avaliações
- Permanent Change and Temporary Deviation Request FormDocumento1 páginaPermanent Change and Temporary Deviation Request FormdrustagiAinda não há avaliações
- Lean Vs Six SigmaDocumento23 páginasLean Vs Six SigmaSiddharth ChakkarwarAinda não há avaliações
- SMC Class ScheduleDocumento1 páginaSMC Class ScheduledrustagiAinda não há avaliações
- Agile Scrum at Glance BaselineDocumento1 páginaAgile Scrum at Glance BaselinedrustagiAinda não há avaliações
- Leanmap FREE Six Sigma Tool OverviewDocumento2 páginasLeanmap FREE Six Sigma Tool OverviewdrustagiAinda não há avaliações
- Set Project Priorities - ToCDocumento4 páginasSet Project Priorities - ToCdrustagiAinda não há avaliações
- Scrum Master Certification (SMC™) Course OutlineDocumento1 páginaScrum Master Certification (SMC™) Course OutlinedrustagiAinda não há avaliações
- 6 Six Sigma Roadmap RevDocumento20 páginas6 Six Sigma Roadmap RevJuan PabloAinda não há avaliações
- Updated Agile - KanbanDocumento25 páginasUpdated Agile - Kanbandrustagi100% (1)
- Leanmap FREE Six Sigma DMAIC ProcessDocumento1 páginaLeanmap FREE Six Sigma DMAIC ProcessdrustagiAinda não há avaliações
- Six Sigma Fact SheetDocumento4 páginasSix Sigma Fact SheetMarcus Skookumchuck VanniniAinda não há avaliações
- PDSA History Ron MoenDocumento9 páginasPDSA History Ron MoenAli Shah100% (1)
- FBD, Fmea, ParetoDocumento5 páginasFBD, Fmea, ParetodrustagiAinda não há avaliações
- PDSA History Ron MoenDocumento9 páginasPDSA History Ron MoenAli Shah100% (1)
- Who Are The TOP Quality GurusDocumento8 páginasWho Are The TOP Quality GurusdrustagiAinda não há avaliações
- A Solution Template To Help in Hypothesis TestingDocumento3 páginasA Solution Template To Help in Hypothesis TestingdrustagiAinda não há avaliações
- Quality Management Gurus TheoriesDocumento6 páginasQuality Management Gurus TheoriesSyafiqah RedzwanAinda não há avaliações
- MAW KitDocumento3 páginasMAW KitdrustagiAinda não há avaliações
- A Solution Template To Help in Hypothesis TestingDocumento3 páginasA Solution Template To Help in Hypothesis TestingdrustagiAinda não há avaliações
- The Benefits of PDCADocumento2 páginasThe Benefits of PDCAdrustagiAinda não há avaliações
- Sample Chartered Accountant ResumeDocumento5 páginasSample Chartered Accountant ResumedrustagiAinda não há avaliações
- Quality Management Gurus TheoriesDocumento6 páginasQuality Management Gurus TheoriesSyafiqah RedzwanAinda não há avaliações
- Chartered Accountant Resume Sample - Best FormatDocumento4 páginasChartered Accountant Resume Sample - Best FormatdrustagiAinda não há avaliações
- 1624 - Corporate Transfer PolicyDocumento16 páginas1624 - Corporate Transfer PolicySyamsul ArifinAinda não há avaliações
- Ched Memorandum Order FinalDocumento95 páginasChed Memorandum Order Finalrvmpresas100% (3)
- Garrenton Nursing Skills Checklist 2022Documento7 páginasGarrenton Nursing Skills Checklist 2022api-507789841Ainda não há avaliações
- Group 5 Report in NCM 108Documento74 páginasGroup 5 Report in NCM 108Daniela Villanueva RosalAinda não há avaliações
- Guideline for Newly Diagnosed Epilepsy DrugsDocumento2 páginasGuideline for Newly Diagnosed Epilepsy DrugsInga CebotariAinda não há avaliações
- Management of Orthodontic Emergencies During 2019-NCOV: Editorial Open AccessDocumento4 páginasManagement of Orthodontic Emergencies During 2019-NCOV: Editorial Open Accessshatz_014Ainda não há avaliações
- Cdip Crosswalk 2023 FinalDocumento8 páginasCdip Crosswalk 2023 FinalRaju RajeshAinda não há avaliações
- TesisDocumento9 páginasTesisRachel SepulvedaAinda não há avaliações
- IJMS - Volume 49 - Issue 1 - Pages 1-9Documento9 páginasIJMS - Volume 49 - Issue 1 - Pages 1-9metaversajAinda não há avaliações
- Guidelines for Intensive Care ServicesDocumento252 páginasGuidelines for Intensive Care Servicesmaria carceanu salaru100% (1)
- Fredman, Christie y Bear, 2007Documento13 páginasFredman, Christie y Bear, 2007Fausto Adrián Rodríguez LópezAinda não há avaliações
- TP Leads - GurgaonDocumento32 páginasTP Leads - GurgaonDeepika Aggarwal0% (1)
- Biopsychosocial Model ApproachDocumento2 páginasBiopsychosocial Model ApproachAlifiaafpAinda não há avaliações
- Medical Marijuana RecommendationDocumento1 páginaMedical Marijuana Recommendationespinza1Ainda não há avaliações
- Peran IPCNDocumento38 páginasPeran IPCNSANITASI LINGKUNGAN RSPBGAinda não há avaliações
- 1756 9966 29 67Documento6 páginas1756 9966 29 67Yogha RyanandaAinda não há avaliações
- 1 - Normal Saline For Endotracheal SuctioningDocumento28 páginas1 - Normal Saline For Endotracheal SuctioningRena WidyaAinda não há avaliações
- PSHP 61st Anniversary and National ConventionDocumento6 páginasPSHP 61st Anniversary and National ConventionSr. Thessa Marie RamosoAinda não há avaliações
- Diagnosis and treatment approaches for excessive gingival displayDocumento9 páginasDiagnosis and treatment approaches for excessive gingival display刘雨樵Ainda não há avaliações
- The Ethics of Surgery Conflicts and Controversies 1st Edition 2015 Oxford (PRG)Documento385 páginasThe Ethics of Surgery Conflicts and Controversies 1st Edition 2015 Oxford (PRG)Eugen CerevanAinda não há avaliações
- Infection Prevention in Health Care Systems by Incorporation of Well-Equipped and Designed Isolation RoomsDocumento8 páginasInfection Prevention in Health Care Systems by Incorporation of Well-Equipped and Designed Isolation RoomsInternational Journal of Arts, Humanities and Social Studies (IJAHSS)Ainda não há avaliações
- The Evolution of MedicineDocumento7 páginasThe Evolution of MedicineEva SheikhAinda não há avaliações
- Drug Infusions in ICU Made Simple 2016Documento28 páginasDrug Infusions in ICU Made Simple 2016ta lê thanhAinda não há avaliações
- Ideal Clinic Definitions, Components and ChecklistsDocumento90 páginasIdeal Clinic Definitions, Components and ChecklistsMduduzi MbheleAinda não há avaliações
- SAP EHS - Occupational Health - EHS-HEA - V1.1 PDFDocumento87 páginasSAP EHS - Occupational Health - EHS-HEA - V1.1 PDFMukesh ChauhanAinda não há avaliações
- End of Life Choice Sponsor's ReportDocumento73 páginasEnd of Life Choice Sponsor's ReportACT Party100% (2)
- Chapter 245D Home and Community-Based Services StandardsDocumento59 páginasChapter 245D Home and Community-Based Services Standardsentreprise.tgctp2015Ainda não há avaliações
- Jama Carson 2023 SC 230002 1696973901.0012-1Documento11 páginasJama Carson 2023 SC 230002 1696973901.0012-1Luz Elena ValderramaAinda não há avaliações
- Cauti Qi PosterDocumento1 páginaCauti Qi Posterapi-219780992Ainda não há avaliações
- Perception of Nursing Students On Clinical Learning EnvironmentDocumento6 páginasPerception of Nursing Students On Clinical Learning Environmentvodem79046Ainda não há avaliações