Escolar Documentos
Profissional Documentos
Cultura Documentos
Anal Fissures
Enviado por
khadzx0 notas0% acharam este documento útil (0 voto)
907 visualizações2 páginasAnal fissures are most common in infancy, and they represent the most common cause of bright rectal bleeding at any age. If not promptly diagnosed and treated, these small tears and their occasionally associated superficial infection cause severe anorectal pain during bowel movements.
Descrição original:
Direitos autorais
© Attribution Non-Commercial (BY-NC)
Formatos disponíveis
DOC, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoAnal fissures are most common in infancy, and they represent the most common cause of bright rectal bleeding at any age. If not promptly diagnosed and treated, these small tears and their occasionally associated superficial infection cause severe anorectal pain during bowel movements.
Direitos autorais:
Attribution Non-Commercial (BY-NC)
Formatos disponíveis
Baixe no formato DOC, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
907 visualizações2 páginasAnal Fissures
Enviado por
khadzxAnal fissures are most common in infancy, and they represent the most common cause of bright rectal bleeding at any age. If not promptly diagnosed and treated, these small tears and their occasionally associated superficial infection cause severe anorectal pain during bowel movements.
Direitos autorais:
Attribution Non-Commercial (BY-NC)
Formatos disponíveis
Baixe no formato DOC, PDF, TXT ou leia online no Scribd
Você está na página 1de 2
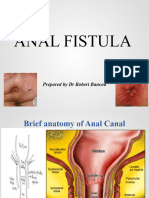
ANAL FISSURES The reflex relaxation of the internal sphincter that normally
Definition follows defecation is lost in patients with anal fissure; instead
Superficial linear tear in the squamous epithelium of the contraction of the internal sphincter occurs.
anal canal distal to the dentate line.
Most commonly caused by passage of a large, hard stool. DIAGNOSIS
History
In the short-term, usually involves only the epithelium and, in
the long-term, involves the full thickness of the anal mucosa. Relatively specific dx based usually on history alone.
Severe pain during a bowel movement, with the pain lasting
Occurrence minutes - hours afterward.
Anal fissures are common in infancy, and they represent the The pain leading to a cycle of worsening constipation, harder
most common cause of bright rectal bleeding at any age. stools, and more anal pain.
If not promptly diagnosed and treated, these small tears and Bright red blood on the toilet paper or stool but no
their occasionally associated superficial infection cause significant bleeding
severe anorectal pain during bowel movements and set in
motion a cycle of stool negativism, constipation, and Mucous anal discharge and pruritus ani are also
increasing pain with subsequent defecation. common.
History of chronic anal fissure is typically cyclical; periods
Etiology-Not exactly known But: of acute pain are followed by temporary healing, only to be
Trauma -passage of hard stool(constipation) succeeded by further acute pain.
-anal intercourse
- rectal examination speculum PHYSICAL
The patient should be examined in the left lateral position.
Low-fiber diets- lacking in raw fruits and vegetables
Visual examination may disclose a posterior oedematous
Prior anal surgery -scarring from the surgery may cause
tag and, on parting the buttocks, an associated fissure may
either stenosis or tethering of the anal canale. For example be seen.
hemorrhoidectomy, fistulotomy, condylomata ablation result
in scarring of the anoderm and loss of anoderm elasticity. Note depth of fissure and its orientation to the midline,
often described using clock orientation of hour hand.
Chronic diarrhea/explosive diarrhea
Perianal dermatitis/ or infection Majority of tears are found in the posterior midline. Goligher's
Crypt abscess rule is that 90% of fissures are posterior, 10% are anterior,
Habitual use of cathartics and less than 1% occurs simultaneously anteriorly and
posteriorly.
Abnormalities in internal sphincter tone - hypertonicity Fissures occurring off the midline should raise the possibility
and hypertrophy of the internal anal sphincter, leading to of other etiologies.
elevated anal canal and sphincter resting pressures
Sigmoidoscopy should be undertaken, under anaesthesia
Most patients with anal fissures have an elevated resting to exclude specific causes of fissure, IBD (esp. Crohn's
pressure, and this resting pressure returns to normal levels disease), anal syphilis, anal herpes, anal carcinoma,
after surgical sphincterotomy. lymphoma, anoreceptive intercourse (with or without HIV
infection), and, in children, sexual abuse.
Pain accompanies each bowel movement as this raw area is
stretched and the injured mucosa is abraded by the stool. Rectal examination is generally difficult to tolerate because
of sphincter spasm and pain.
The internal sphincter also begins to spasm when a bowel
movement is passed, which has 2 effects. First, the spasm Acute fissures are erythematous and bleed easily.
itself is painful; second, the spasm further reduces the blood With chronic fissures, classic fissure triad may be seen.
flow to the posterior midline and the anal fissure, contributing a. Deep ulcer
to the poor healing rate. b. Sentinel pile-skin tag-externally
c. Enlarged anal papillae- internally
Pathophysiology
Constipation thought to cause initial trauma causing acute MANAGEMENT
fissures. The goals of treatment are to relieve the constipation and pain
Acute anal fissures are superficial and are not normally thus to break the cycle of hard bowel movement, associated
associated with skin tag formation. pain, and worsening constipation and spasm of internal anal
Chronic anal fissure is associated with the development of sphincter.
both anal tags and polyps (hypertrophied anal papillae) as a
result of inflammatory edema. Medical therapy
Chronic sub epithelial infection at the fissure results in Initial therapy for an anal fissure is medical in nature, and
fibrosis and, in rare instances, anal stenosis. more than 80% of acute anal fissures resolve without
The torn edges of the anal epithelium become undermined further therapy.
and the ulcer deepens, exposing fibres of the internal Softer bowel movements are easier and less painful for the
sphincter muscle. patient to pass.
A vicious cycle ensues in which subepithelial inflammation First-line medical therapy
causes spasm of the internal sphincter, inhibiting free
drainage of the infected fissure and permitting continued Diet modification increase -water and fibres-fruits and
inflammation, resulting in a small, chronic, inadequately vegetables.
drained abscess. Stool-bulking agents/Stool softeners -such as fiber
supplementation and stool softeners-polyethylene glycol
GICHOY A JUDY WAWIRA YR 2007
Laxatives are used as needed to maintain regular bowel Sphincterotomies are normally performed in the lateral
movements.-Lactulose quadrants as most fissures are posterior or anterior and cuts
would not heal due to impaired blood supply.
Mineral oil may be added to facilitate passage of stool Only the internal sphincter is cut; the external sphincter is
without as much stretching or abrasion of the anal not used not cut and must not be injured.
for long. In chronic anal fissures, excision of the fissure in
Sitz baths after bowel movements - symptomatic relief as conjunction with the lateral sphincterotomy may be done.
they relieve painful internal sphincter muscle spasm. an advancement flap may be performed to cover the defect
in the mucosa.
2nd medical therapy
Topical application of 0.2% nitroglycerin (NTG) ointment Follow-up care
directly to the internal sphincter. stool softeners and fiber supplementation after the surgery
NTG ointment is thought to relax the internal sphincter and Complications from surgery
to help relieve some of the pain associated with sphincter Infection
spasm; it also is thought to increase blood flow to the anal Bleeding
mucosa.
Anal abscess
main adverse effects are headache and dizziness; could be
fistula development,
used directly before bedtime.
Nitroglycerin ointment is a nitric oxide source. The most feared—incontinence.
Nitric oxide is an inhibitory neurotransmitter that causes Recurrence of fissure
relaxation of the internal sphincter and improved blood flow
to the anoderm. Differential Diagnosis
Crohn's disease,
Others -hydrocortisone cream, lignocaine gels,
anal tuberculosis (TB),
Proctosedyl ointment (cinchocaine anaesthetic 0.5 per
cent and hydrocortisone 0.5 per cent). anal malignancy,
abscess/fistula disease,
Newer therapy for acute and chronic anal fissures is cytomegalovirus,
botulinum toxin.it is an injection of 20-25 units. Botox
herpes,
inhibits the release of acetylcholine from presynaptic nerve
fibers affecting a reversible paralysis that last several Chlamydia,
months. syphilis,
The toxin is injected directly into the internal anal sphincter acquired immunodeficiency syndrome,
and, in effect, performs a chemical sphincterotomy. some blood dyscrasias may all mimic anal fissure/ ulcer
The effect lasts approximately 3 months, until the nerve disease
endings regenerate. This 3-month period may allow acute Prognosis
fissures (and sometimes chronic fissures) to heal and
symptoms to resolve. Lateral internal anal sphincterotomy is successful in 90-
Recurrence indicates need for surgery. 95% of patients with chronic anal fissure/ulcer disease.
Fewer than 10% of surgically treated patients are
Surgical therapy: incontinent of mucous and gas.
Surgical therapy is usually reserved for acute anal fissures Fissure recurrence is less than 10%.
that remain symptomatic after 3-4 weeks of medical therapy
and for chronic anal fissures. Few chronic fissures heal
spontaneously or from medical therapy and is indication for
surgery
Sphincter dilatation
controlled anal stretch or dilatation under general anesthetic.
This is performed because one of the causative factors for
anal fissure is thought to be a tight internal anal sphincter;
stretching it helps correct the underlying abnormality, thus
allowing the fissure to heal.
Lateral internal sphincterotomy
Current surgical procedure of choice. Done under general
or spinal anesthesia.
The purpose of an internal sphincterotomy is to cut the
hypertrophied internal sphincter, thereby releasing
tension and allowing the fissure to heal.
This may be performed in "open" fashion, whereby an
incision is made in the skin and the distal one-third of the
internal sphincter is divided under direct vision.
It may also be done in a "closed" manner, whereby a scalpel
is passed in the intersphincteric plane and swept medially
dividing the internal sphincter blindly.
GICHOY A JUDY WAWIRA YR 2007
Você também pode gostar
- Anal Abscess And Fistula, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandAnal Abscess And Fistula, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNota: 1 de 5 estrelas1/5 (1)
- Anal FissureDocumento9 páginasAnal FissureaiysahmirzaAinda não há avaliações
- Anal Fissure: BY Alisha SaleemDocumento7 páginasAnal Fissure: BY Alisha Saleemashar khanAinda não há avaliações
- Anal FissureDocumento45 páginasAnal FissureMinale MenberuAinda não há avaliações
- Anal FissureDocumento8 páginasAnal Fissurenisya1982_hasibuanAinda não há avaliações
- Pruritus Ani, Hemorroidet EtjDocumento4 páginasPruritus Ani, Hemorroidet EtjKreshnik HAJDARIAinda não há avaliações
- Benign Anorectal ConditionssDocumento32 páginasBenign Anorectal ConditionssMpanso Ahmad AlhijjAinda não há avaliações
- Anal and Perianal ConditionsDocumento58 páginasAnal and Perianal ConditionsYonas YemidiralemAinda não há avaliações
- l8 Management of Perianal Pain and ConditionsDocumento51 páginasl8 Management of Perianal Pain and ConditionsMohd Johari Mohd ShafuwanAinda não há avaliações
- 24 Anorectal ConditionsDocumento55 páginas24 Anorectal ConditionsRaisa CleizeraAinda não há avaliações
- Anal ProblemsDocumento35 páginasAnal ProblemsSandip VaghelaAinda não há avaliações
- Case Study (Appendicitis)Documento8 páginasCase Study (Appendicitis)Jobelle AcenaAinda não há avaliações
- Role of Homoeopathy in The Management of Anal FissureDocumento4 páginasRole of Homoeopathy in The Management of Anal FissureSwaroopa PatilAinda não há avaliações
- Anal Fissures PPT KIDocumento20 páginasAnal Fissures PPT KIMustafa HusainAinda não há avaliações
- 3.1 Acute AppendicitisDocumento3 páginas3.1 Acute AppendicitisMavi HayalAinda não há avaliações
- Fissura AniDocumento6 páginasFissura AniSani muzakirAinda não há avaliações
- Acute Appendicitis: DR - Syed Ubaid Associate Professor of SurgeryDocumento109 páginasAcute Appendicitis: DR - Syed Ubaid Associate Professor of SurgeryRoyster CabralAinda não há avaliações
- Anal FissureDocumento17 páginasAnal FissureZoe Anna0% (1)
- Fistula PerianalDocumento25 páginasFistula PerianalHafiizh Dwi PramuditoAinda não há avaliações
- AppenDocumento25 páginasAppenFernando AnibanAinda não há avaliações
- Anal Fissure Chronic - Clinical EvidenceDocumento18 páginasAnal Fissure Chronic - Clinical EvidenceNicolás CopaniAinda não há avaliações
- Anal Fistula Dont DeleteDocumento28 páginasAnal Fistula Dont DeleteRazeen RiyasatAinda não há avaliações
- APPENDICITISDocumento18 páginasAPPENDICITISAlie DumpAinda não há avaliações
- 16 Benign Anorectal ConditionsDocumento48 páginas16 Benign Anorectal Conditionssuhaib ananzehAinda não há avaliações
- PERITONITISDocumento4 páginasPERITONITISAmoroso, Marian Corneth D.Ainda não há avaliações
- Ii. Appendicitis 1Documento3 páginasIi. Appendicitis 1lalisa manobanAinda não há avaliações
- CASE PRESENTATION Nadhirah RahimDocumento60 páginasCASE PRESENTATION Nadhirah RahimNadhirah Rahim100% (1)
- Anorectal Conditions: Prepared By: Manisha Thapa Roll No: 6 BSN 2 Year Presented To: Ms. Shristhi ShresthaDocumento25 páginasAnorectal Conditions: Prepared By: Manisha Thapa Roll No: 6 BSN 2 Year Presented To: Ms. Shristhi ShresthaManjesh Mishra XettriAinda não há avaliações
- Disease of RectumDocumento22 páginasDisease of RectumTalal AbbasiAinda não há avaliações
- Lapkas Hi 4-6-18Documento41 páginasLapkas Hi 4-6-18kalvinAinda não há avaliações
- Anal FistulaDocumento26 páginasAnal FistulaBeverly PagcaliwaganAinda não há avaliações
- Anal FissureDocumento3 páginasAnal FissureBhaveen ShethAinda não há avaliações
- Anal Fissure and FistulaDocumento21 páginasAnal Fissure and FistulaErnie SyarinaAinda não há avaliações
- LUT Trauma - DR - Agung, Sp.UDocumento42 páginasLUT Trauma - DR - Agung, Sp.UAnin DitaAinda não há avaliações
- Anal Fissure: A Frequent Reason of Anal Pain: Dr. Bhavin KothariDocumento3 páginasAnal Fissure: A Frequent Reason of Anal Pain: Dr. Bhavin KotharisebastixmasterAinda não há avaliações
- Anorectal DisorderDocumento31 páginasAnorectal DisorderSaid SalimAinda não há avaliações
- Inguinal and Femoral HerniaDocumento50 páginasInguinal and Femoral HerniaFafa NabihaAinda não há avaliações
- Hemorrhoids, ParaproctitisDocumento56 páginasHemorrhoids, ParaproctitisСандагсүрэн СандагдоржAinda não há avaliações
- Anal, Perianal, and Pilonidal Diseases - Oct - 2023 2Documento15 páginasAnal, Perianal, and Pilonidal Diseases - Oct - 2023 2qq8kx98kt2Ainda não há avaliações
- Abcesso e Fistula AnoretalDocumento5 páginasAbcesso e Fistula AnoretalDani SAinda não há avaliações
- Surgery ExamDocumento82 páginasSurgery Examrajarajachozhan139Ainda não há avaliações
- Pengendalian Rasa SakitDocumento127 páginasPengendalian Rasa SakityouareAinda não há avaliações
- Anal FistulaDocumento7 páginasAnal FistulaKate Laxamana Guina100% (1)
- Diseses of Large IntestineDocumento24 páginasDiseses of Large Intestineaastharawat1234Ainda não há avaliações
- Chapter 15 - Abdominal PainDocumento5 páginasChapter 15 - Abdominal PainSerious LeoAinda não há avaliações
- DR Kulwant SinghDocumento34 páginasDR Kulwant SinghTasyaAinda não há avaliações
- Hernia and Perianal ConditionsDocumento58 páginasHernia and Perianal ConditionsSocial Media workingAinda não há avaliações
- Pharyngeal Pouch LeafletDocumento2 páginasPharyngeal Pouch LeafletIrina Garlea-RobuAinda não há avaliações
- Acute Abdomen FinalDocumento105 páginasAcute Abdomen FinalAizul AzmiAinda não há avaliações
- Vesico-Vaginal FistulaDocumento8 páginasVesico-Vaginal FistulaBinita ShakyaAinda não há avaliações
- Other Problems in Inflammatory ResponseDocumento62 páginasOther Problems in Inflammatory ResponseJR Rolf NeuqeletAinda não há avaliações
- Testicular Torsion, Hydrocele & Fournier GangreneDocumento41 páginasTesticular Torsion, Hydrocele & Fournier GangreneNur Insyirah100% (1)
- Hernia InguinalisDocumento12 páginasHernia InguinalisAna RiantiAinda não há avaliações
- Anus and RectumDocumento140 páginasAnus and RectumJohn Paulo CatacutanAinda não há avaliações
- Common Health Problems That Develop During Infancy MPNDocumento14 páginasCommon Health Problems That Develop During Infancy MPNShaii Whomewhat GuyguyonAinda não há avaliações
- TMJ Hypermobility and Hypomobility 7Documento6 páginasTMJ Hypermobility and Hypomobility 7Somia MohmedAinda não há avaliações
- Powerpoint: Anal and Perianal DisordersDocumento66 páginasPowerpoint: Anal and Perianal Disordersj.doe.hex_8780% (5)
- PATH - Anal Fissures (2p)Documento2 páginasPATH - Anal Fissures (2p)Elvira MirandaAinda não há avaliações
- Congenital Glaucomas: 1. Primary 2. Iridocorneal DysgenesisDocumento12 páginasCongenital Glaucomas: 1. Primary 2. Iridocorneal DysgenesiskhadzxAinda não há avaliações
- Primary Angle-Closure Glaucoma: 1. Pathogenesis 2. ClassificationDocumento9 páginasPrimary Angle-Closure Glaucoma: 1. Pathogenesis 2. ClassificationkhadzxAinda não há avaliações
- 34 Idiopathic Spec Uveitis SyndromeDocumento8 páginas34 Idiopathic Spec Uveitis SyndromekhadzxAinda não há avaliações
- Congenital Cataract: 1. Important FactsDocumento13 páginasCongenital Cataract: 1. Important FactskhadzxAinda não há avaliações
- Acquired 2. Isolated Familial Ectopia Lentis 3. Associated With Systemic SyndromesDocumento8 páginasAcquired 2. Isolated Familial Ectopia Lentis 3. Associated With Systemic SyndromeskhadzxAinda não há avaliações
- 15corneal InfectionsDocumento8 páginas15corneal InfectionskhadzxAinda não há avaliações
- Abnormal Lens ShapeDocumento4 páginasAbnormal Lens ShapekhadzxAinda não há avaliações
- Chronic Osteomyelitis in Early Infancy: Presenter: DR Maina Discussant: DR Mogire (Orthopedic Surgeon)Documento27 páginasChronic Osteomyelitis in Early Infancy: Presenter: DR Maina Discussant: DR Mogire (Orthopedic Surgeon)khadzxAinda não há avaliações
- Juvenile Rheumatoid Arthritis (Jra) (Juvenile Chronic Arthritis-Jca)Documento70 páginasJuvenile Rheumatoid Arthritis (Jra) (Juvenile Chronic Arthritis-Jca)khadzxAinda não há avaliações
- 02chronic Marginal BlepharitisDocumento7 páginas02chronic Marginal BlepharitiskhadzxAinda não há avaliações
- Disorders of Eye LashesDocumento8 páginasDisorders of Eye LasheskhadzxAinda não há avaliações
- Sudden Unexpected Death FMT 400Documento11 páginasSudden Unexpected Death FMT 400khadzxAinda não há avaliações
- Classification of Injuries FMTDocumento30 páginasClassification of Injuries FMTkhadzx100% (2)
- Narcotics N HallucinogensDocumento14 páginasNarcotics N HallucinogenskhadzxAinda não há avaliações
- Ndiang'Ui: Unexpected Deaths 24 September 2009Documento25 páginasNdiang'Ui: Unexpected Deaths 24 September 2009khadzxAinda não há avaliações
- Postmortem Changes and Postmortem Time IntervalDocumento24 páginasPostmortem Changes and Postmortem Time IntervalkhadzxAinda não há avaliações
- Poisoning by MedicinesDocumento11 páginasPoisoning by MedicineskhadzxAinda não há avaliações
- Introduction To Forensic Medicine DR David Chumba MBCHB, Mmed (Human Pathology), Dip. For Med (Sa)Documento20 páginasIntroduction To Forensic Medicine DR David Chumba MBCHB, Mmed (Human Pathology), Dip. For Med (Sa)khadzxAinda não há avaliações
- Fire Arm Injuries 4th Yr ForensicDocumento31 páginasFire Arm Injuries 4th Yr ForensickhadzxAinda não há avaliações
- Carbon Monoxide Poisoning 4th YrDocumento17 páginasCarbon Monoxide Poisoning 4th YrkhadzxAinda não há avaliações
- Colloidal Tin Injection - SPCDocumento15 páginasColloidal Tin Injection - SPCacbgdvAinda não há avaliações
- SafePatientHandling PDFDocumento1 páginaSafePatientHandling PDFdipraAinda não há avaliações
- Ecg ReadingsDocumento11 páginasEcg ReadingsAnton Laurenciana100% (5)
- 2018-2019 Research ProposalDocumento2 páginas2018-2019 Research Proposalapi-358143741Ainda não há avaliações
- Final Evaluation - 2021Documento12 páginasFinal Evaluation - 2021api-240864098Ainda não há avaliações
- Liver CirrhosisDocumento5 páginasLiver CirrhosisRLLTAinda não há avaliações
- InsulinomaDocumento18 páginasInsulinomaBetta BeTta0% (1)
- Myopic MaculopathyDocumento17 páginasMyopic MaculopathyjochigAinda não há avaliações
- Screening of Hemoglobinopathies in Blood DonorsDocumento17 páginasScreening of Hemoglobinopathies in Blood Donorsmansi pandyaAinda não há avaliações
- Critique of Missed Nursing Care, A Qualitative StudyDocumento6 páginasCritique of Missed Nursing Care, A Qualitative Studyclem14321100% (1)
- Winnie Koima: See Reverse For ReferencesDocumento3 páginasWinnie Koima: See Reverse For ReferencesjulialeoAinda não há avaliações
- Oxygenation: Hematologic Pathophysiology: Allen Octaviano CudiamatDocumento34 páginasOxygenation: Hematologic Pathophysiology: Allen Octaviano Cudiamatᜀᜎ᜔ᜎᜒᜈ᜔ ᜃᜓᜇᜒᜀᜋᜆ᜔100% (1)
- Extended Role of NurseDocumento7 páginasExtended Role of Nurseसपना दाहालAinda não há avaliações
- Cumulative Trauma DisorderDocumento39 páginasCumulative Trauma DisorderChanda NathaniAinda não há avaliações
- Acupuncture InformationDocumento5 páginasAcupuncture Informationsamlee65Ainda não há avaliações
- Eclinicalworks Emr Medical Assistant & Nurse Training Guide: Rachel J. Cohen PHD Dohmh Training ManagerDocumento52 páginasEclinicalworks Emr Medical Assistant & Nurse Training Guide: Rachel J. Cohen PHD Dohmh Training ManagerLaveen Chenna NaniAinda não há avaliações
- Strattera PDFDocumento5 páginasStrattera PDFToronto StarAinda não há avaliações
- CAHOCON 23 - SponsorshipBrochure PDFDocumento11 páginasCAHOCON 23 - SponsorshipBrochure PDFsubhraj7027Ainda não há avaliações
- Edan CadenceDocumento78 páginasEdan CadenceerikaAinda não há avaliações
- Skin Cancer SurgeryDocumento2 páginasSkin Cancer SurgeryContinuum Hospitals of New York100% (1)
- Neoplasia: Nomenclature Epidemiology OncogenesDocumento7 páginasNeoplasia: Nomenclature Epidemiology OncogenespriyaAinda não há avaliações
- Psychiatric Nursing SlidesDocumento27 páginasPsychiatric Nursing SlidesHazel RoseAinda não há avaliações
- 13 Otoscope UseDocumento61 páginas13 Otoscope UseJayakumar D Swamy0% (1)
- Botox EbookDocumento15 páginasBotox Ebookdoraemon100% (2)
- Ota ResumeDocumento2 páginasOta Resumeapi-336423215Ainda não há avaliações
- Rationale, Pre-Test Post-TestDocumento9 páginasRationale, Pre-Test Post-TestNina OaipAinda não há avaliações
- Dialysis Event Surveillance ManualDocumento56 páginasDialysis Event Surveillance ManualAnitha SAinda não há avaliações
- Clinical Study Report, Bioequivalence, General Concepts and OverviewDocumento48 páginasClinical Study Report, Bioequivalence, General Concepts and OverviewAhmad Abdullah Najjar100% (7)
- Pulmonary TuberculosisDocumento17 páginasPulmonary TuberculosisRobert Dominic GonzalesAinda não há avaliações
- GoutDocumento10 páginasGoutAmberAinda não há avaliações