Escolar Documentos
Profissional Documentos
Cultura Documentos
Philcare Application Form - 07302013
Enviado por
Jerry Barad SarioTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Philcare Application Form - 07302013
Enviado por
Jerry Barad SarioDireitos autorais:
Formatos disponíveis
Application No.
To our Prospective Valued Client: We are pleased to offer you the PhilCare health package! This letter intends to re-affirm with you the main features of the plan of your choice. WHAT IS PHILCARE? PhilCare puts together and causes the delivery of a package of comprehensive health services, including out-patient treatments, preventive health care and hospitalization to its members. In lieu of charging a fee for each service rendered, the Company collects regular membership fees from its members upon enrollment or membership and at fixed intervals thereafter. The organization's primary thrust is to prevent illness or at least detect and treat it at an early stage. For this reason, the Company encourages and puts emphasis on out-patient and preventive health care, while at the same time providing coverage for hospitalization expenses when needed. WHATARE YOURADVANTAGESASAMEMBER OF PHILCARE? As a member of PhilCare, you enjoy the following advantages: First, the probability of financial loss due to illness or accident is diminished if not entirely prevented. Second, your medical expenditures are determinable because most of the essential services you will be needing are covered by the regular membership fees. Third, you are guaranteed access to a team of primary physicians as well as medical specialists for the whole range of medical quality assurance programs to ensure that you are provided with accepted standards of health care. WHATARE THE LIMITATIONS OFYOUR HEALTH PLAN? Just like any other HMO, PhilCare carries with it certain limitations, which are necessary in order to maintain high quality medical services at affordable membership fees for our members. The following are the limitations of the plan. We encourage you to familiarize yourselves with these limitations. 1. Non-coverage of Pre-Existing Conditions Your contract does not cover pre-existing conditions. An illness or condition shall be considered Pre-existing if, prior to the effective date of your health care coverage (theAgreement) or the approval date of reinstatement in case of lapsation, a) any professional advise or treatment was given for such illness or condition; or b) such illness or condition was in any way evident to the Member; or c) the pathogenesis of such illness or condition has started, whether or not the member is aware of such illness or condition. In addition to the foregoing, the following conditions but not limited to, when occurring during the first year of coverage after the Effective Date or reinstatement, are considered Pre-existing: (a) endometriosis; (b) hemorrhoids; (c) diseased tonsils requiring surgery; (d) pathological abnormalities of nasal septum and turbinates; (e) thyroid conditions; (f) cataracts, glaucoma and pterygium ; (g) sinus conditions requiring surgery; (h) epilepsy; (i) asthma; (j) cirrhosis of the liver; (k) tuberculosis; (l) anal fistulae; (m) cholecystitis/choleithiasis; (n) calculi of the urinary system; (o) gastric or duodenal ulcer; (p) hallux valgus; (q) tumors, whether benign or malignant, of all organs and organ systems, including malignancies of the blood or bone marrow; (r) diabetes mellitus and other endocrine conditions; (s) hypertension; (t) collagen disease/immunologic disorders; (u) cardiovascular diseases; (v) hernia; (w) HIV/AIDS; and (x) chronic skin conditions, (y) obesity, dyslipidemia and other metabolic conditions; (z) autoimmune conditions; (aa) degenerative conditions; (ab) neurologic conditions; and (ac) cerebrovascular disease. On your second year, after 12 months of continuous coverage, the Pre-existing Condition Clause shall no longer be applicable except for illnesses and conditions which have been specifically stated as exclusions in an Endorsement form which was made part of your contract provided there is continuous coverage for the past 12 months. 2. Annual Benefit Limit (ABL) There will only be one (1) limit for all types of coverable illnesses per year to include ordinary, dreaded, ICU, or non-ICU cases. 3. Annual Renewal ofAgreement The Agreement may be renewed yearly subject to the approval of PhilCare and subject to the payment by the Member of the renewal membership fees on or before the renewal date. Further, the following conditions shall apply to the coverage of renewal years: A) Pre-existing conditions diagnosed during the first year of coverage shall permanently be excluded in the coverage of renewal years; and B) TheAnnual Benefit Limit shall be replenished. 4. Permanent and General Exclusions Some specific conditions are permanently excluded from your coverage, i.e., any claim(s) arising from such conditions will not be covered permanently by PhilCare. Such exclusions can be specific for particular members. Page 3 of hour health care contract will indicate whether or not you will be subject to a permanent exclusion. Finally, page 6 of our contract enumerates conditions that are not included in the coverage. Such conditions are referred to as General Exclusions. 5. Access Procedures To maximize our effectiveness and efficiency in the delivery of health care services to you, we have instituted simple procedures that you will be required to follow in availing of your benefits. The basic procedures, which you have to remember, are as follows: For non-emergency conditions proceed only to any one of our designated out-patient clinics. Emergency Rooms of hospitals are not authorized to treat non-emergency conditions. For emergency conditions, proceed to the Emergency Room of the nearest hospital, preferably a PhilCare Affiliated Hospital. You will be provided with a list of affiliated hospitals.(Emergency shall mean the sudden, unexpected onset of illness or injury, which at the time of contract reasonably appeared as having the potential of causing immediate disability or death or requiring immediate alleviation of severe pain and discomfort). Inform PhilCare CallCenter within 24 hours of your confinement especially if you are confined in a non-affiliated hospital. PhilCare will not cover expenses for emergency cases in non-affiliated hospitals if the member fails to inform this company within 24 hours about the confinement. In cases like these, members are required to apply for reimbursement. However, reimbursement will be 80% of the usual, customary reasonable expenses and standard professional fees but not to exceed 80% of what it would have cost had you been confined in an affiliated hospital and treated by an affiliated physician, or P 12,500 (for Classic Standard & Classic Executive) or P50,000 (for Classic Executive Elite & Premiere G lobal), whichever is lesser. 6. RoomAssignment You are entitled to a room accommodation corresponding to your type of program. Should you occupy a room that is higher than your room limit, you will pay only for the excess in room charges, provided that you are staying in a room classification corresponding to your plan. If you stay in a room classification higher than your plan, you will have to pay also for the excess in professional fees and other hospital ancillary charges. It is important to know that fees charged for various procedures done in the hospital, including professional fees, are based on the type of the patient's room accommodation. 7. PhilHealth (Medicare) and/or Employees Compensation Commission (ECC) In case you are covered under PHILHEALTH and/or ECC, you or your representative must submit a duly accomplished PHILHEALTH and/or ECC form prior to your discharge from the hospital. Otherwise, the hospital will require you to pay the PHILHEALTH portion, which will only be refundable to you by PHILHEALTH when you submit the required forms. Your failure to submit your PHILHEALTH and/or ECC form could result in your payment of a certain amount which should have been covered by said PHILHEALTH and/or ECC. WHATARE YOUR RESPONSIBILITIESASA PHILCARE MEMBER? A. You must be up-to-date in your payment of Membership Fees. Your membership fees are payable under the mode you have originally chosen. While PhilCare endeavors to remind you of your membership fee due either through Billing Notice sent by mail or by a phone call from PhilCare Customer Service Representatives, payment of membership fees on time remains the responsibility of the Member. Nonreceipt of billing notices or inability of respective servicing agents to collect payments shall not serve as ground to contest any decision of the company to deny benefits because the contract is no longer in force due to non-payment. B. Follow the proper procedures as earlier discussed for you to fully enjoy the benefits of the plan and prevent the occurrence of problems. C. Read your PhilCare Contract The moment you receive your PhilCare Agreement (following the approval of your application), thoroughly go through the Agreement. For any clarification, kindly consult your servicing agents or call PhilCare Customer Service Hotline at (+632) 462-1800. Our PhilCare Customer Service Representatives will be happy to answer your inquiries. (Please turn to next page)
(This portion is to be accomplished by agents)
Application No.
IE FAMILY CLASSIC STANDARD CLASSIC ELITE CLASSIC EXECUTIVE CLASSIC EXECUTIVE ELITE PREMIERE GLOBAL Enrollment Fee : P Membership Fee : P :P Rider Fee Value Added Tax : P :P TOTAL
); *- 1 +744-, ,7- 6 52--, 72 24 +0) +-551 /- 1 /) )95 4-/7 , 4-+ 4,1 / )61
DEPOSIT ON APPLICATION RECORD FOR AGENT AGREEMENT NO. EFFECTIVE DATE
Dental:
Package 1
Package 2 Package 3
APPLICANTS NAME AGENTS NAME/CODE OR Number
1
46)
6 *- 57* -+6 6 ), 756 1+)61 *-4 1 ) 7 1 65. 4) ; 6):-5 ) 9 + , 60-4 +0)4/-5 60)6 ; 60..1+1) 5) , 4 6):)61
.--5 50) )
- 574- 60)6 60- )22 6 7
*-4 15 50 /) .
44-+6
4-+-126 6
75- 60- )/4--
9 72
WHAT ARE THE OTHER BENEFITS OF YOUR PLAN?
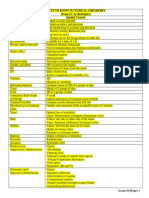
BENEFITS
Care in Foreign Territories
PREMIER / PREMIER ELITE
If you are confined or treated in a hospital outside the Philippines due to a n e m e r g e n c y, PhilamCare shall reimburse you up to 80% of the reasonable and coverable charges for medical care and services which are incurred as a result of such emergency, but not to exceed what PhilCare would have paid had you been treated by an Affiliated Physician in an Affiliated Hospital in the Philippines, or P12,500 pesos, whichever is lesser. With standard benefit package (see contract)
EXECUTIVE
If you are confined or treated in a hospital outside the Philippines due to an emergency, PhilCare shall reimburse you up to 80% of the reasonable and coverable charges for medical care and services which are incurred as a result of such emergency, but not to exceed what PhilCare would have paid had you been treated by an Affiliated Physician in an Affiliated Hospital in the Philippines, or P12,500 pesos, whichever is lesser.
EXECUTIVE ELITE
Emergency Care in Foreign Territory up to 50,000 pesos If you are confined or treated in a hospital outside the Philippines due to an emergency, PhilCare shall reimburse you up to 80% of the reasonable and coverable charges for medical care and services which are incurred as a result of such emergency, but not to exceed what PhilCare would have paid had you been treated by an Affiliated Physician in an Affiliated Hospital in the Philippines, or 50,000 pesos, whichever is lesser. Non-Emergency Treatment in the U.S.A You shall be entitled to non-emergency treatment in any registered medical facilities in the USA which is included in the UHC's US-based network of health care providers that has been contracted by PhilCare, provided that it is determined by the Medical Director or the Medical Services Officer of PhilCare that there is no professionally acceptable treatment for the said illness or condition available in the Philippines
GLOBAL CARE
Emergency Care in Foreign Territory up to 50,000 pesos (see executive plan) ( Other Benefits: Up to P 2M reimbursement for expenses incurred overseas due to sickness or accident suffered during the trip. Up to P 2M lump sum benefit for death or dismemberment due to accident suffered during the trip. Coverage for transportation and accommodation expenses of an adult family member if insured is hospitalized to take care of your minor children who are travelling with you and accompany them home in the event you are hospitalized during the trip. Coverage for arrangement and payment for the transportation and accommodation expenses of an adult family member if the insured is hospitalized for more than five (5) days during the trip and no adult family member is with you. Coverage for the arrangement and payment for the return of the mortal remains to the Philippines in the event of death due to sickness or accidents suffered during the trip. In the case of Laparoscopic Cholecystectomy, Magnetic Resonance Imaging (MRI), and Nuclear or Radioactive Isotope Scans, PhilCare shall cover the entire cost of these procedures subject to the maximum plan limit. The availment of Laparoscopic Cholecystectomy or Lithotripsy is limited only to once per contract year. When you choose these newer modalities of treatment, PhilCare shall no longer be liable for the cost of further mode of treatment/diagnostic tests for the same illness should they be necessary. Your Annual Physical Examination shall be more thorough and shall include the following additional procedures: a. Fasting Blood Sugar (FBS) b. Blood Urea Nitrogen (BUN) c. Cholesterol d. Creatinine e. Triglyceride f. Low Density Lipoprotein (LDH) High Density Lipoprotein (HDL) g. Treadmill Test The Point-of-Service (POS) Benefit allows you to avail of the services of non-affiliated doctors and/or non-affiliated hospitals in the Philippines for your hospitalization, whether emergency or non-emergency. With this, you may avail your hospitalization benefits even without prior authorization from PhilCare for the confinement as long as the hospitalization is prescribed by a qualified physician. For out-patient benefits, you may go directly to an affiliated specialist even without prior authorization from PhilCare. General medical consultations and laboratory or diagnostic exams however, must be done in PhilCare clinics. In any of the above cases where the services where rendered by a non-affiliated provider or there was no prior authorization from PhilCare, you will have to advance the payment to the doctor and hospital. You may be charged by the doctor according to the doctor's private fees. You shall then be reimbursed 100% of the health care expenses that you incurred but not to exceed 100% of what PhilCare would have paid had you been treated by an affiliated physician in an affiliated hospital Should you prefer to go directly to a PhilCare affiliated Physician in an Affiliated Hospital without any cash outlay, such may also be availed by simply getting a Letter Of Authorization (LOA) from the PhilCare PrimaryCare Physician or LOA issuing Stations in the affiliated hospital of your choice Up to P 150,000 coverage for loss of travel fare and/or accommodation expenses paid in advance and not refundable if the trip had to be cancelled within 30 days before departure date. Up to P 150,000 coverage for loss of travel fare and/or accommodation expenses paid in advance and not refundable if after commencement of the trip the insured had to return to Philippines due to pre-defined events. Up to P 2,000 per 12 hours reimbursement for the delay of flight for more than 12 hours due to severe weather conditions, strike of airline personnel or equipment failure of aircraft. Up to P 2M coverage against legal liability for bodily injury or property damage to third parties due to insured's negligence. Up to P 50,000 reimbursement for costs of additional hotel, travel and communication expenses necessary in obtaining replacement of lost passport or visa. Baggage protection Free access to Travel Guard 24-hour Emergency Hotline. In case of emergency, all you have to do is call collect (+632)878-1280 (Philippines) or (+603)2772-5672 (Malaysia) anytime from anywhere in the world.
Special Modalities of Treatment
In the case of Laparoscopic Cholecystectomy, Magnetic Resonance Imaging (MRI), and Nuclear or Radioactive Isotope Scans, PHILCARE shall cover the entire cost of these procedures subject to the maximum plan limit. The availment of Laparoscopic Cholecystectomy or Lithotripsy is limited only to once per contract year. When you choose these newer modalities of treatment, PHILCARE shall no longer be liable for the cost of further mode of treatment/diagnostic tests for the same illness should they be necessary.
More procedures for The Annual Physical Examination (APE)
With standard benefit package (see contract)
Your Annual Physical Examination shall be more thorough and shall include the following additional procedures: a. Fasting Blood Sugar (FBS) b. Blood Urea Nitrogen (BUN) c. Cholesterol d. Creatinine e. Triglyceride f. Low Density Lipoprotein (LDH) High Density Lipoprotein (HDL)
Your Annual Physical Examination shall be more thorough and shall include the following additional procedures: a. Fasting Blood Sugar (FBS) b. Blood Urea Nitrogen (BUN) c. Cholesterol d. Creatinine e. Triglyceride f. Low Density Lipoprotein (LDH) High Density Lipoprotein (HDL) g. Treadmill Test
Point-of-Service (POS) Benefit
N/A
The Point-of-Service (POS) Benefit allows you to avail of the services of nonaffiliated doctors and/or non-affiliated hospitals in the Philippines for your hospitalization, whether emergency or non-emergency. With this, you may avail your hospitalization benefits even without prior authorization from PhilCare for the confinement as long as the hospitalization is prescribed by a qualified physician. For out-patient benefits, you may go directly to an affiliated specialist even without prior authorization from PhilCare, General medical consultations and laboratory or diagnostic exams however, must be done in PhilCare clinics. In any of the above cases where the services where rendered by a non-affiliated provider or there was no prior authorization from PhilCare you will have to advance the payment to the doctor and hospital. You may be charged by the doctor according to the doctor's private fees. You shall then be reimbursed 80% of the health care expenses that you incurred but not to exceed 80% of what PhilCare would have paid had you been treated by an affiliated physician in an affiliated hospital.
Direct Access
N/A
N/A
Travel Insurance
N/A
N/A
Very truly yours,
PhilhealthCare, Inc Penthouse, PhilPlans Corporate Center 1012 North Triangle Drive Bonifacio Global City, Taguig City
MONICO V. JACOB President and CEO PhilhealthCare, Inc.
APPLICATION FOR HEALTHCARE COVERAGE
NOTE: TO FACILITATE PROCESSING OF THIS APPLICATION, PLEASE ACCOMPLISH THIS FORM COMPLETELY AND SUBMIT THIS WITH YOUR SIGNED CONFORME ON THE RE-AFFIRMATION BELOW TOGETHER WITH THE 1X1 ID PHOTO.
Application No. Agreement No.
NEW BUSINESS PART I
RENEWAL LAST NAME
RE-APPLICATION
GROUP TO INDIVIDUAL
WORKSITE (SA) FIRST NAME MI
PERMANENT ADDRESS ZIP CODE RESIDENCE TEL. NO. OFFICE ADDRESS BUSINESS TEL. NO. MOBILE NO. OCCUPATION/JOB TITLE BIRTHDATE (MM/DD/YYYY) AGE PART II TYPE OF PROGRAM CLASSIC STANDARD PROGRAM TYPE DIAMOND EMERALD PEARL MODE OF PAYMENT ANNUAL FORM OF PAYMENT OVER THE COUNTER CASH PART III CHECK CREDIT CARD AUTO DEBIT ARRANGEMENT CARD NAME CARD NUMBER 120K 65K 55K SEMI-ANNUAL IE/FAMILY CLASSIC ELITE
MAXIMUM PLAN LIMIT
NATURE OF BUSINESS PLACE OF BIRTH CITIZENSHIP: SINGLE MARRIED FILIPINO OTHERS:
WIDOWED SEPARATED
TIN
E-MAIL SEX
HEIGHT
WEIGHT CIVIL STATUS:
ESTIMATED TOTAL MONTHLY INCOME 10,000 or below 10,001 - 20,000
20,001 - 50,000 50,001 - 100,000
100,001 and up
BG+
GROUP CLASSIC EXECUTIVE CLASSIC EXECUTIVE ELITE EXECUTIVE PRIVATE EXECUTIVE SUITE Package 1 Package 2 Package 3 PREMIERE GLOBAL PREMIERE PRIVATE PREMIERE SUITE
250K 85K 75K QUARTERLY
500K 100K 90K
EXECUTIVE 150 EXECUTIVE 250
ADDITIONAL BENEFIT DESIRED MONTHLY* DENTAL
*MONTHLY MODE OF PAYMENT IS ALLOWED ONLY FOR FAMILY PLANS WITH MINIMUM OF FIVE (5) MEMBERS
CHECK THIS BOX IF YOU ARE APPLYING ONLY FOR YOUR SPOUSE AND/OR CHILDREN (with principal as Payor) DOB AGE SEX HT WT RELATIONSHIP TO PRINCIPAL / PAYOR OCCUPATION CITIZENSHIP
FAMILY MEMBERS APPLYING FOR MEMBERSHIP
IF YOU ARE NOT ENROLLING ALL YOUR CHILDREN WHO ARE SINGLE AND BELOW 21 YEARS OF AGE, PLEASE STATE REASON(S) WHY ON A SEPARATE SHEET OF PAPER
LEARNED ABOUT PHILCARE THROUGH: INTERNET PRINT AD
FRIENDS
AGENTS
PHILCARE OFFICE
OTHERS
PHILCARE RE: LETTER OF RE-AFFIRMATION Please be informed that I have read and understood the contents of the application and the limitations of my coverage. I hereby certify that the data and other information stated herein are written by me or under my supervision. I am submitting with this letter the accomplished application form and my initial payment.
Signature over Printed Name of Principal Applicant TO BE FILLED UP BY THE SERVICING AGENT: PHILCARE . RE: LETTER OF RE-AFFIRMATION
DATE
Please be informed that I have explained well to my client the contents of the application and the limitations of his/her coverage. I hereby certify that the data and other information stated herein are written by my client or by me under his/her supervision.
Signature over Printed Name of Servicing Agent AGENCY UNIT PERSONAL AGENCY
Signature over Printed Name of Servicing Agent UNIT PERSONAL
AGENTS CODE DATE: Tel. No. : Mobile No. : DATE: Email Address:
AGENTS CODE
HOW DO YOU WANT THE AGREEMENT AND MEMBERSHIP PACKAGE TO BE SENT? TO BE PICKED UP BY AGENT TO BE PICKED-UP BY MEMBER TO BE DELIVERED AT MEMBERS PERMANENT ADDRESS OFFICE ADDRESS
HOW DO YOU WANT YOUR SUCCEEDING BILLING TO BE SENT? MAILED TO PERMANENT ADDRESS MAILED TO OFFICE ADDRESS
I agree and authorize the Company to use and disclose any information (collected or held) with regards to the matters pertaining to this application to enable the Company, its associated individuals, organizations or independent third parties, to provide advice or information covering products or services which the Company believes maybe of interest to me or to communicate with me for any purpose.
Form No. M-2
FOR PHILCARE USE ONLY MEMBERSHIP WORKSHEET COMPUTATIONS CERTIFICATE # ENROLLEES NAME ISSUE AGE MEMBERSHIP FEE DENTAL FEE TOTAL
REMARKS:
TOTAL ENROLLMENT FEE VAT GRAND TOTAL
PAYMENT OR #
AMOUNT:
DATE:
BY:
UNDERWRITING ACTIONS APPROVED DATE: NAME CANCELLED DISAPPROVED SIGNATURE: REASONS RECONSIDERED ADDITIONAL REQTS.
EXCLUSIONS
CODE
EFFECTIVE DATE: ENCODED BY/DATE: DATE
EXPIRATION DATE: VERIFIED BY/DATE: REQUIREMENTS/RECOMMENDATIONS/ACTIONS NAME/SIGNATURE
MEDICAL QUESTIONNAIRE :
Answer all the following questions in the appropriate check box provided below . If you are applying for a family coverage, all questions are applicable to each applicant. Use the space provided below to give full details of items with YES answers.
Check Box YES NO
1. Have you ever had a history of, and/or treatment, consult ation or known indication for: a. Disorder of eyes, nose, or throat ? b. Dizziness, fainting, convulsion, headache, speech defect, paralysis or stroke, mental or nervous disorder ? c. Shortness of breath, persistent hoarseness or cough, blood-spitting, tuberculosis, asthma or other chronic respiratory disorders ? d. Chest pain, palpitation, high blood pressure, rheumatic fever, heart murmur, heart attack or other disorder of the heart or blood vessels ? e. Jaundice, intestinal bleeding, ulcer, hernia, appendicitis, colitis, diverticulitis, hemorrhoids, recurrent indigestion or other disorder of the stomach, intestines, liver or gall bladder ? f. Sugar, albumin, blood or pus in urine, venereal disease, stone or other disorder of kidney, bladder, prostate, or reproductive organs ? g. Diabetes, thyroid or other endocrine disorder ? h. Neuritis, sciatica, rheumatism, arthritis, gout or disorder of the muscles or bones, such as spine, back or joint s ? i. Deformity, lameness or amputation ? j. Disorder of skin, lymph glands, cysts, tumor or cancer ? k. Allergies, anemia, or other disorder of the blood ? l. Excessive use of alcohol, tobacco, or any habit forming drugs ? 2. Are you now under observation or taking treatment ? 3. Have you had any change in weight in the p ast years ? 4. Other than the above, have you: a. Had any physical disorder or any known indication thereof ? b. Had a medical examination, consultation, illness, injury, or surgery ? c. Been a patient in a hospital, clinic, sanitarium, or other medical facility ? d. Had electrocardiogram, x-ray, or other diagnostic tests ? e. Been advised to have any diagnostic test, hospitalization or surgery which was not completed ? 5. Have you ever had military service deferment, rejection or discharge because of a physical or mental condition ? 6. Have you ever applied for or received a pension payment, or benefit due to injury, sickness or disability ? 7. Do you have a parent, brother or sister who died of or had high blood pressure, tuberculosis, diabetes, cancer, heart or kidney disease, or mental illness ? If so, at what age ? 8. Do you or other members of the family smoke ? a. If yes, since when ? How many sticks a day ? b. If you have quit smoking, since when ? How long have you smoked ? How many sticks a day ? 9. Are you or any of your family members presently covered under any hospitalization or medical plan? Give details.
Check Box YES NO
10. FOR FEMALES ONLY a. Have you ever had any abnormal menstruation, pregnancy, childbirth, or disorder of the female organ or breasts ? b. Are you now pregnant ? If yes, how many months ?
* Use the space provided below to give full details of items with YES answers
NAME OF FAMILY MEMBER
DATE OF HISTORY TREATMENT, CONFINEMENT, ETC.
CHIEF COMPLAINTS AND DIAGNOSIS
TREATMENT AND RESULTS
NAME AND ADDRESS OF PHYSICIAN AND HOSPITAL
(Kindly continue on the appropriate space on the reverse side of this form, if necessary.) We hereby declare and agree that all statements and answers contained herein and in any addendum annexed to this application are full, complete and true and binds all parties in interest under the Health Care Coverage (the Agreement) herein applied for, that there shall be no contract of health care coverage unless and until an Agreement is issued on this application and the full Membership Fee according to the mode of payment is paid during the good health of proposed Member(s); that the health care coverage of any Member shall take effect only on the Effective Date as indicated in the issued Agreement or the actual date full Membership Fee was paid, whichever is later; that no information acquired by any Representative of PhilCare shall be binding upon PhilCare unless set out in writing in this application; that any physician is, by these presents, expressly authorized to disclose or give testimony at anytime relative to any information acquired by him in his professional capacity upon any question affecting the eligibility for health care coverage of the proposed Members and that the acceptance of any Agreement issued on this application shall be a ratification of any information on correction in addition to this application. We agree and authorize PhilCare and its accredited Physicians, Clinics, and the like to use and/or disclose any medical information (collected or held) in its possession after a formal written request from the requesting party (Name of Company) with regards to my medical history and that of my dependents in accordance with my healthcare coverage. We hereby affirm that we have read and understood the contents of the health care contract as discussed in the attached Re-affirmation Letter. As proof of the foregoing, we are submitting a signed conforme of the same with this Application Form. We hereby understand that we, the enrollees, will only start availing of the benefits of the program upon the effectivity of the policy.
SIGNED AT
THIS
DAY OF
PRINTED NAME AND SIGNATURE OF WITNESS
PRINTED NAME AND SIGNATURE OF PRINCIPAL APPLICANT
AUTHORIZATION TO FURNISH MEDICAL INFORMATION
(The form below should be completed for each case) I hereby authorize any person, organization, or entity that has any record or knowledge of my health and/or that of to give to the PhilhealthCare, Inc. any and all information relative to any hospitalization, consultation, treatment, or any other medical advice or examination. This authorization is in connection with the application for health care coverage or with any benefit availed and with any claim for benefits under such coverage. A photographic copy of this authorization shall be as valid as the original.
PRINTED NAME AND SIGNATURE OF WITNESS
PRINTED NAME AND SIGNATURE OF PRINCIPAL APPLICANT
PRINTED NAME AND SIGNATURE OF AGENT AND CODE NO.
APPLICATION NO.
Você também pode gostar
- PRC Tos Board ExamDocumento10 páginasPRC Tos Board Examapi-291835787Ainda não há avaliações
- Compre-Quiz For MedtechDocumento18 páginasCompre-Quiz For MedtechynaellyAinda não há avaliações
- L5 - Nature of Clinical Lab - PMLS1Documento98 páginasL5 - Nature of Clinical Lab - PMLS1John Daniel AriasAinda não há avaliações
- MT LawsDocumento8 páginasMT LawsKathleen Javier AngcayaAinda não há avaliações
- MUST To KNOW in Clinical ChemistryDocumento53 páginasMUST To KNOW in Clinical ChemistryTristan Jay CalabiaAinda não há avaliações
- l1 Intro Pmls1Documento17 páginasl1 Intro Pmls1John Daniel AriasAinda não há avaliações
- Different Types of HazardsDocumento4 páginasDifferent Types of HazardsGNiqM100% (1)
- Medical Laws and Regulations SummaryDocumento16 páginasMedical Laws and Regulations SummaryNeririAinda não há avaliações
- Parasitology ReviewersDocumento9 páginasParasitology ReviewersLouije MombzAinda não há avaliações
- COMPLETE BLOOD COUNT Lecture GuideDocumento9 páginasCOMPLETE BLOOD COUNT Lecture GuideKaycee Gretz LorescaAinda não há avaliações
- Photo Me TryDocumento3 páginasPhoto Me TrylcrujidoAinda não há avaliações
- Lab Manual Hema 2Documento16 páginasLab Manual Hema 2Charisse Ann ValdehuezaAinda não há avaliações
- Group 1 BSMT 3A Act. 5.2Documento7 páginasGroup 1 BSMT 3A Act. 5.2Gennelyn Ross Delos ReyesAinda não há avaliações
- Lec 1 - IntroductionDocumento3 páginasLec 1 - IntroductionHaendra Mae DapilagaAinda não há avaliações
- Whats New in Blood Banking March 2013Documento41 páginasWhats New in Blood Banking March 2013violaorsinoAinda não há avaliações
- MT Laws and Lab ManDocumento8 páginasMT Laws and Lab ManGene Narune GaronitaAinda não há avaliações
- CHAPTER 8 MedtechDocumento17 páginasCHAPTER 8 MedtechKisen DiazAinda não há avaliações
- Lesson 5: Nature of The Clinical LaboratoryDocumento8 páginasLesson 5: Nature of The Clinical LaboratoryJohn Daniel AriasAinda não há avaliações
- Parasitology PRKTKLDocumento58 páginasParasitology PRKTKLmohamed100% (2)
- (MT6317) Unit 6.1 Introduction To Carbohydrates and Glucose DeterminationDocumento12 páginas(MT6317) Unit 6.1 Introduction To Carbohydrates and Glucose DeterminationJC DomingoAinda não há avaliações
- Baileys Table (Important!!!!)Documento8 páginasBaileys Table (Important!!!!)shaun lisonAinda não há avaliações
- AnemiaDocumento9 páginasAnemiaMila Canoza HerreraAinda não há avaliações
- HTMLE SEMINAR NOTES DOC. ORTEGA - CompressedDocumento35 páginasHTMLE SEMINAR NOTES DOC. ORTEGA - CompressedNISSI JUNE T. UNGABAinda não há avaliações
- Aubf LabDocumento99 páginasAubf Labhinata shoyoAinda não há avaliações
- 1.entamoeba Histolytica - Is The Major Pathogen in This GroupDocumento14 páginas1.entamoeba Histolytica - Is The Major Pathogen in This GroupJoseph De JoyaAinda não há avaliações
- Trace Elements in the BodyDocumento21 páginasTrace Elements in the BodyJunea SeeAinda não há avaliações
- ImmunoDocumento18 páginasImmunoirish o-oAinda não há avaliações
- A. B. C. D.: Send ReportDocumento4 páginasA. B. C. D.: Send ReportSp PpvAinda não há avaliações
- Gastric FluidDocumento4 páginasGastric Fluidchippai22Ainda não há avaliações
- Test Bank Exam 3Documento81 páginasTest Bank Exam 3Sajjad AhmadAinda não há avaliações
- Cc1-Task 4Documento8 páginasCc1-Task 4Joshua TrinidadAinda não há avaliações
- Manage Biological RisksDocumento4 páginasManage Biological RisksGAinda não há avaliações
- Count the sperm in the central grid and multiply by 10,000 to obtain the sperm concentration per mLDocumento81 páginasCount the sperm in the central grid and multiply by 10,000 to obtain the sperm concentration per mLAris ResurreccionAinda não há avaliações
- Compatibility Testing - BloodDocumento5 páginasCompatibility Testing - BloodMunish DograAinda não há avaliações
- AUBF Finals Vaginal SecretionsDocumento37 páginasAUBF Finals Vaginal SecretionsLyra Dennise LlidoAinda não há avaliações
- HIV Related Policies and Guidelines Issuances: Training On HIV Counseling and Testing and Facility-Based HIV ScreeningDocumento77 páginasHIV Related Policies and Guidelines Issuances: Training On HIV Counseling and Testing and Facility-Based HIV ScreeningJovania B.Ainda não há avaliações
- Chemical Examination of UrineDocumento6 páginasChemical Examination of UrinehermanskyAinda não há avaliações
- Diagnostic Microbiology - : University of Santo Tomas - Medical TechnologyDocumento6 páginasDiagnostic Microbiology - : University of Santo Tomas - Medical TechnologyWynlor AbarcaAinda não há avaliações
- M6 Histopath ImpregantionAndEmbeddingDocumento4 páginasM6 Histopath ImpregantionAndEmbeddingninaAinda não há avaliações
- HEMA 1 LAB - WatermarkDocumento133 páginasHEMA 1 LAB - WatermarkDavid WolfyAinda não há avaliações
- Chapter 1: Introduction To Urinalysis: Urine CompositionDocumento74 páginasChapter 1: Introduction To Urinalysis: Urine CompositionMegumi TadokoroAinda não há avaliações
- Micropara Final LabNotesDocumento75 páginasMicropara Final LabNotescream oAinda não há avaliações
- Clinical Chemistry BasicsDocumento15 páginasClinical Chemistry BasicsJangHanbyul100% (1)
- Online Exam - Laboratory ManagementDocumento30 páginasOnline Exam - Laboratory ManagementAngelicaAinda não há avaliações
- Immuno Sero Lec Prelim TransDocumento15 páginasImmuno Sero Lec Prelim TransLoren EscotoAinda não há avaliações
- 2.13.08 Cold Agglutinin RogersDocumento27 páginas2.13.08 Cold Agglutinin RogersJessica StewartAinda não há avaliações
- Analysis of Physical Properties of UrineDocumento2 páginasAnalysis of Physical Properties of UrineameerabestAinda não há avaliações
- Lab Evaluation of PlateletsDocumento5 páginasLab Evaluation of PlateletsDennis ValdezAinda não há avaliações
- MedtechDocumento7 páginasMedtechLyudmyla GillegoAinda não há avaliações
- Leptospires General Characteristics:: Bacteriology: SpirochetesDocumento5 páginasLeptospires General Characteristics:: Bacteriology: SpirochetesJaellah MatawaAinda não há avaliações
- Clinical MicrosDocumento28 páginasClinical MicrosKristine Jamella Maris NaragAinda não há avaliações
- Review 1 BacteDocumento9 páginasReview 1 BacteJibz MiluhonAinda não há avaliações
- Sources of Errors in Clinical ChemistryDocumento9 páginasSources of Errors in Clinical Chemistrykalantan23Ainda não há avaliações
- Disorders of Coagulation and Thrombosis NotesDocumento16 páginasDisorders of Coagulation and Thrombosis NotesleeAinda não há avaliações
- Lecture 10 AutoimmunityDocumento78 páginasLecture 10 AutoimmunitytimcarasAinda não há avaliações
- MEDICAL INSURANCE DISCLOSUREDocumento3 páginasMEDICAL INSURANCE DISCLOSURESiti Intan NabilahAinda não há avaliações
- Philhealth BenefitsDocumento2 páginasPhilhealth BenefitsjohnhenryvAinda não há avaliações
- Employee Med PolicyDocumento4 páginasEmployee Med PolicyPixie DustAinda não há avaliações
- Citibank Insurance Services - Know all about Health Forever InsuranceDocumento26 páginasCitibank Insurance Services - Know all about Health Forever InsurancekartheekbeeramjulaAinda não há avaliações
- SGPS - Travel Insurance BrochureDocumento4 páginasSGPS - Travel Insurance Brochuremackenziebromstad1265Ainda não há avaliações
- Memo For The Evaluators and RTWG 2Documento3 páginasMemo For The Evaluators and RTWG 2Jerry Barad SarioAinda não há avaliações
- Lingkod GADthering On WheelsDocumento9 páginasLingkod GADthering On WheelsJerry Barad SarioAinda não há avaliações
- ALP Chat-1 TEACHEXCELSDocumento6 páginasALP Chat-1 TEACHEXCELSJerry Barad SarioAinda não há avaliações
- ReadingDocumento44 páginasReadingJerry Barad SarioAinda não há avaliações
- TEACHeXCELS Active Learning Plan - Chat 1Documento8 páginasTEACHeXCELS Active Learning Plan - Chat 1Jerry Barad SarioAinda não há avaliações
- Certificate of Appearance RTOT RPMS TemplateDocumento1 páginaCertificate of Appearance RTOT RPMS TemplateJerry Barad SarioAinda não há avaliações
- Dear Flexible LearnersDocumento1 páginaDear Flexible LearnersJerry Barad SarioAinda não há avaliações
- Course Orientation Class 2Documento21 páginasCourse Orientation Class 2Jerry Barad SarioAinda não há avaliações
- Department of Education: Republic of The PhilippinesDocumento2 páginasDepartment of Education: Republic of The PhilippinesJerry Barad SarioAinda não há avaliações
- Teachexcels Class 30: Live Session 1Documento18 páginasTeachexcels Class 30: Live Session 1Jerry Barad SarioAinda não há avaliações
- DM s2017 080Documento11 páginasDM s2017 080Jerry Barad SarioAinda não há avaliações
- Adoption of NEAP in The Region Interim Structure and Call For Submission of ProposalsDocumento2 páginasAdoption of NEAP in The Region Interim Structure and Call For Submission of ProposalsJerry Barad SarioAinda não há avaliações
- TakeawayDocumento10 páginasTakeawayJerry Barad SarioAinda não há avaliações
- Request For VehicleDocumento2 páginasRequest For VehicleJerry Barad SarioAinda não há avaliações
- Advisory3 CYWTACDocumento1 páginaAdvisory3 CYWTACJerry Barad SarioAinda não há avaliações
- Form D.2 NEAP Daily Session - Facilitator FormDocumento2 páginasForm D.2 NEAP Daily Session - Facilitator FormJerry Barad SarioAinda não há avaliações
- Training Matrix (Women'S Artistic Gymnastics) : Mrs. Amelia B. BergoniaDocumento1 páginaTraining Matrix (Women'S Artistic Gymnastics) : Mrs. Amelia B. BergoniaJerry Barad Sario100% (3)
- RPMS LatestDocumento2 páginasRPMS LatestJerry Barad SarioAinda não há avaliações
- DepEd Region 2 assists SM City CauayanDocumento1 páginaDepEd Region 2 assists SM City CauayanJerry Barad SarioAinda não há avaliações
- Guidelines On The Preparation For The Implementation of The SHS ProgramDocumento25 páginasGuidelines On The Preparation For The Implementation of The SHS ProgramJerry Barad Sario100% (1)
- Public SHS PlanningDocumento18 páginasPublic SHS PlanningJerry Barad SarioAinda não há avaliações
- Public SHS PlanningDocumento18 páginasPublic SHS PlanningJerry Barad SarioAinda não há avaliações
- Abot Alam - Action PlanDocumento6 páginasAbot Alam - Action PlanJerry Barad SarioAinda não há avaliações
- Abot Alam - Action PlanDocumento6 páginasAbot Alam - Action PlanJerry Barad SarioAinda não há avaliações
- 17 National MancomDocumento36 páginas17 National MancomJerry Barad SarioAinda não há avaliações
- Leadership Congress USLTDocumento1 páginaLeadership Congress USLTJerry Barad SarioAinda não há avaliações
- Feedback/Status Re: Reports/Requests For Follow Up Assignment # Action TakenDocumento1 páginaFeedback/Status Re: Reports/Requests For Follow Up Assignment # Action TakenJerry Barad SarioAinda não há avaliações
- ScholarshipDocumento1 páginaScholarshipJerry Barad SarioAinda não há avaliações
- Sample Only: Competency-Based Standards For Rank-and-File Employees Assessment ToolDocumento2 páginasSample Only: Competency-Based Standards For Rank-and-File Employees Assessment ToolJerry Barad SarioAinda não há avaliações
- Abot Alam - Action PlanDocumento6 páginasAbot Alam - Action PlanJerry Barad SarioAinda não há avaliações
- Perioperative Management of Hyperglycemia and Diabetes in Cardiac Surgery PatientsDocumento24 páginasPerioperative Management of Hyperglycemia and Diabetes in Cardiac Surgery PatientsRudi HaryantoAinda não há avaliações
- Undescended TestesDocumento2 páginasUndescended TestesSamantha TarunAinda não há avaliações
- Curs DR PellegrinoDocumento1 páginaCurs DR PellegrinorfandreiAinda não há avaliações
- 328 IndexDocumento29 páginas328 IndexDafi SanAinda não há avaliações
- Four Humors Theory in Unani MedicineDocumento4 páginasFour Humors Theory in Unani MedicineJoko RinantoAinda não há avaliações
- Apollo Hospitals: Porters Generic FrameworkDocumento6 páginasApollo Hospitals: Porters Generic FrameworkVaibhav AroraAinda não há avaliações
- Diabetes TrackerDocumento1 páginaDiabetes Trackerwildlifewarrior_zrsAinda não há avaliações
- Prevalence of Soil Transmitted Helminths infection in adults in North SulawesiDocumento4 páginasPrevalence of Soil Transmitted Helminths infection in adults in North SulawesiSahrul hamidAinda não há avaliações
- Organ Systems InterviewDocumento2 páginasOrgan Systems InterviewJohn Carlo MontemayorAinda não há avaliações
- Medication Calculation Examination Study Guide: IV CalculationsDocumento2 páginasMedication Calculation Examination Study Guide: IV Calculationswaqas_xsAinda não há avaliações
- How To Protect Yourself and OthersDocumento2 páginasHow To Protect Yourself and OtherslistmyclinicAinda não há avaliações
- Maturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementDocumento10 páginasMaturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementatikahanifahAinda não há avaliações
- Eeg, PSG, Sleep DisordersDocumento48 páginasEeg, PSG, Sleep DisordersIoana MunteanuAinda não há avaliações
- Atrial Fibrillation - Diagnosis and Treatment - AAFP PDFDocumento8 páginasAtrial Fibrillation - Diagnosis and Treatment - AAFP PDFNaufal AmanullahAinda não há avaliações
- Organization of NICU ServicesDocumento45 páginasOrganization of NICU ServicesMonika Bagchi84% (64)
- Psychiatric Assessment ToolDocumento53 páginasPsychiatric Assessment ToolLori100% (4)
- Hong Kong Dental Journal - Volume 2 - Number 2 - YuLeungDocumento1 páginaHong Kong Dental Journal - Volume 2 - Number 2 - YuLeungFebySiampaAinda não há avaliações
- Antepartum Haemorrhage: Women's & Children's ServicesDocumento4 páginasAntepartum Haemorrhage: Women's & Children's ServicesYwagar YwagarAinda não há avaliações
- Sarawuth Noppiboon ID 56070700020 BioPhEPs SystemsDocumento5 páginasSarawuth Noppiboon ID 56070700020 BioPhEPs SystemsSarawuth NoppiboonAinda não há avaliações
- Nursing Care PlanDocumento2 páginasNursing Care PlanMiar QuestAinda não há avaliações
- Miliaria Pustulosa (Infetrop)Documento11 páginasMiliaria Pustulosa (Infetrop)Muhammad mukramAinda não há avaliações
- Postterm Pregnancy - UpToDateDocumento16 páginasPostterm Pregnancy - UpToDateCarlos Jeiner Díaz SilvaAinda não há avaliações
- Coliform BacteriaDocumento4 páginasColiform BacteriaLalu Novan SatriaAinda não há avaliações
- Psik Soal UtsDocumento1 páginaPsik Soal UtsNaurahSalsabil / 20Ainda não há avaliações
- Sush Unity Haemotology-1700Documento51 páginasSush Unity Haemotology-1700Dr-Jahanzaib GondalAinda não há avaliações
- US vs. Barium for Pediatric GERDDocumento6 páginasUS vs. Barium for Pediatric GERDAndreea KAinda não há avaliações
- Machine Learning Medical Imaging Market to Top $2 BillionDocumento13 páginasMachine Learning Medical Imaging Market to Top $2 BillionFrado SibaraniAinda não há avaliações
- TOPIC 3.A Bag TechniqueDocumento38 páginasTOPIC 3.A Bag TechniqueJayrelle D. Safran100% (1)
- New Technologies Related To Public Health Electronic InformationDocumento22 páginasNew Technologies Related To Public Health Electronic InformationKhams TolentinoAinda não há avaliações
- Understanding Plasma Cell Dyscrasias: MGUS, Myeloma, Waldenstrom's and AmyloidosisDocumento41 páginasUnderstanding Plasma Cell Dyscrasias: MGUS, Myeloma, Waldenstrom's and AmyloidosisDr MonikaAinda não há avaliações